
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Immunol., 04 June 2024
Sec. Autoimmune and Autoinflammatory Disorders: Autoinflammatory Disorders
Volume 15 - 2024 | https://doi.org/10.3389/fimmu.2024.1368727
Background: Psoriasis is a chronic dermatological condition characterized by a complex pathogenesis that impacts approximately 3% of adults in the United States and brings enormous social burdens. For many diseases, the systemic immune-inflammatory index (SII), defined as neutrophils × platelets/lymphocytes, has been recognized as a prognostic indicator. Therefore, we conducted a cross-sectional study to assess the association between SII and psoriasis among outpatient US adults.
Methods: In this cross-sectional study, we used data on the US adults 20 to 59 years of age from the National Health and Nutrition Examination Survey (NHANES) spanning 2003–2006 and 2009–2014. Sample-weighted logistic regression and stratified analysis of subgroups were used.
Results: Among the 16,831 adults, there were 8,801 women and 8,030 men, with a psoriasis prevalence rate of 3.0%. A fully adjusted model revealed a positive association between a SII higher than 479.15 × 109/L and a high risk of psoriasis. According to subgroup analysis and interaction testing (p for interaction > 0.05), age, sex, alcohol drinking status, marital status, and body mass index (BMI) were not significantly correlated with this positive association.
Conclusion: Our findings suggested that SII higher than 479.15 × 109/L was positively associated with a high risk of psoriasis among outpatient US adults. To the best of our knowledge, this is the first cross-sectional study using NHANES data focused on the risk of higher SII on psoriasis among outpatient US adults. The outcomes of this cross-sectional serve to supplement previous research, indicating a need for larger-scale prospective cohorts for further validation.
Psoriasis is a chronic dermatological condition characterized by a complex pathogenesis and impacts approximately 3% of adults 20 years or older in the United States (1, 2). Research findings suggest that the prevalence of psoriasis among adults in the United States has remained relatively stable since 2003, showing no significant differences (2). Furthermore, psoriasis imposes considerable financial and social burdens, accounting for the largest global burden of disability due to skin diseases (3).
In the systemic inflammatory system of the human body, immune cells play a critical role in various diseases. Many studies have raised that integrated peripheral lymphocyte, neutrophil, and platelet counts may be more effective in predicting the inflammatory state. Importantly, SII, which possesses considerable clinical application, was calculated by counting three types of circulating immune cells: lymphocytes, platelets, and neutrophils (4, 5). Moreover, SII was initially identified as a prognosis of kidney stones, hepatic steatosis, and cancer investigations (6). Psoriasis is a chronic skin disorder with systemic involvement and inflammatory etiopathogenesis. The treatment of psoriatic skin lesions has seen notable effectiveness with interleukin-17 (IL-17), IL-23, and tumor necrosis factor-alpha (TNF-α) inhibitors (7). However, the impact of SII on psoriasis in the outpatient US population is not completely clarified, and its prognostic ability for psoriasis remains largely unknown. We hypothesized that SII could predict the risk of psoriasis, and we aimed to investigate the association between SII and psoriasis.
Information on psoriasis was only provided in the National Health and Nutrition Examination Survey (NHANES) 2003–2006 cycles for individuals aged 20–59 and in the 2009–2014 cycles for individuals aged 16–80. In this cross-sectional study, deidentified data for participants aged 20–59 were extracted from the NHANES 2003–2006 and 2009–2014 cycles. The study was deemed exempt by the Shantou University Medical College institutional review board as it used publicly available deidentified data, and informed consent was waived. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. Data were analyzed from July to November 2023.
From the NHANES 2003–2006 and 2009–2014 cycles, a total of 50,938 participants were enrolled. First, we selected 17,766 participants aged 20–59. Subsequently, we excluded 914 participants with missing SII data and 21 participants with missing psoriasis data. Finally, a total of 16,831 participants were involved. Of the 16,831 participants, there were 8,443 participants with SII lower than 479.15 × 109/L and 8,388 participants with SII higher than 479.15 × 109/L. The flowchart of participant enrollment is presented in Figure 1.
Psoriasis was defined as an affirmative response to the question, “Have you ever been told by a healthcare provider that you had psoriasis?” The SII was calculated using the peripheral neutrophil, lymphocyte, and platelet counts, defined as (platelet count × neutrophil count)/lymphocyte count (8). For all the analyses, we set the cutoff value at 479.15 × 109/L (9).
The following covariates were included in this cross-sectional study: sociodemographic variables (age, sex, race and ethnicity, family income, educational level, and marital status), NHANES cycles, body mass index (BMI), alcohol drinking status, and smoking status (10–12). First, races and ethnicities were categorized into the following four groups: Mexican American, non-Hispanic White, non-Hispanic Black, and Other. Based on the family poverty income ratio, family income was categorized into the following three levels: low income (≤1.3), medium income (>1.3 to 3.5), and high income (>3.5). Educational level was categorized into the following three levels: high school or less, some college, and college graduate or higher. Marital status was categorized into the following two groups: married and not married. Smoking status was categorized into the following three groups: never smoked (or smoked <100 cigarettes), former smoker (smoked at least 100 cigarettes but has quit), and current smoker (still smoking) (13). Finally, alcohol drinking status was determined by the question, “In any 1 year, have you had at least 12 drinks of any type of alcoholic beverage?” Participants who answered “yes” were defined as alcohol drinkers (14).
In accordance with NHANES analytic guidelines, our analyses considered the complex sampling design and sampling weights (15). We calculated the sampling weight using the following formula: fasting subsample 10-year mobile examination center (MEC) weight = fasting subsample 2-year MEC weight/5 (14). We used quartiles to describe the continuous variables with non-normal distribution and performed the Wilcoxon rank-sum test for comparison. We described the categorical variables using unweighted frequency and weighted percentage and conducted a chi-square test for comparison.
We checked for multicollinearity using the variance inflation factor (VIF) method. If the VIF was 5 or higher, it meant there was multicollinearity present. Model 1 was adjusted for sociodemographic variables and NHANES cycles. Model 2 was adjusted for sociodemographic variables, NHANES cycles, BMI, alcohol drinking status, and smoking status. Additionally, we conducted interaction and subgroup analyses using logistic regression models, stratified by age group, sex, alcohol drinking status, marital status, and BMI group.
We used R version 4.3.1 for all the statistical analyses, and we considered a significance level of p < 0.05 to show that the results were statistically significant.
This cross-sectional study involved 50,938 participants from 2003–2006 and 2009–2014. First, 33,172 participants <20 and >59 years old were excluded. Then, 914 adults were excluded for missing SII data. After excluding 21 adults with missing psoriasis data, 16,831 participants were finally enrolled. As shown in Table 1, the prevalence rate of psoriasis was 3.0% in this cross-sectional study. Of the 16,831 adults, there were 8,801 women and 8,030 men. Compared with SII lower than 479.15 × 109/L, adults with SII higher than 479.15 × 109/L were more likely to be non-Hispanic White, to be current smokers, and to have an educational level of high school or less.
The results of the sample-weighted logistic regression analyses are displayed in Table 2. A positive association between a SII higher than 479.15 × 109/L and a high risk of psoriasis was revealed in model 2 (OR, 1.55; 95% CI, 1.20–2.01, p = 0.001).
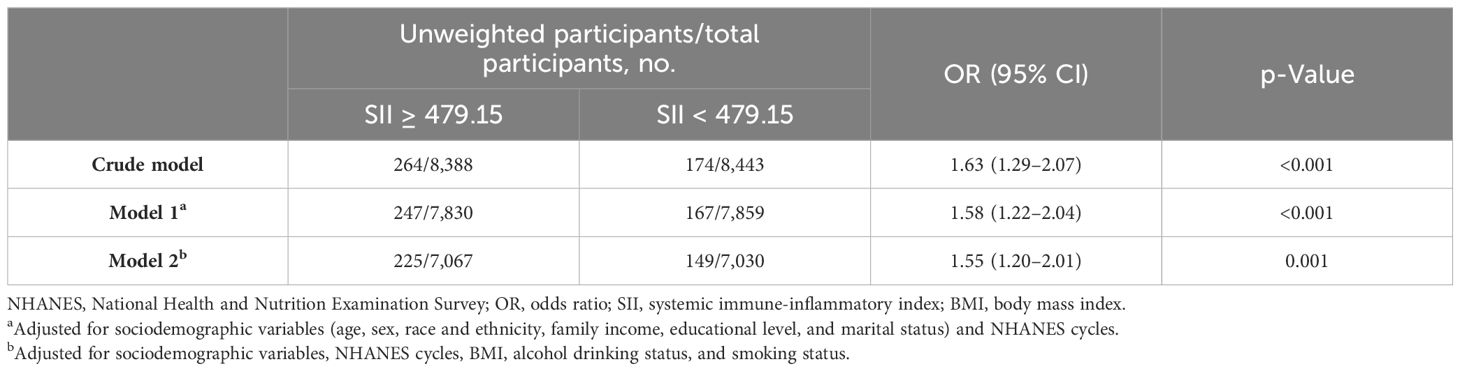
Table 2 Association of SII with psoriasis among participants in the NHANES 2003–2006 and 2009–2014 cycles.
We found that SII was not positively associated with psoriasis among participants aged 20–39 (OR, 1.41; 95% CI, 0.88–2.26, p = 0.147) and those not married (OR, 1.50; 95% CI, 0.98–2.29, p = 0.059). In addition, we found that SII was positively associated with psoriasis in the sex, alcohol drinking status, and obesity subgroups. The results of the subgroup analyses are displayed in Figure 2.
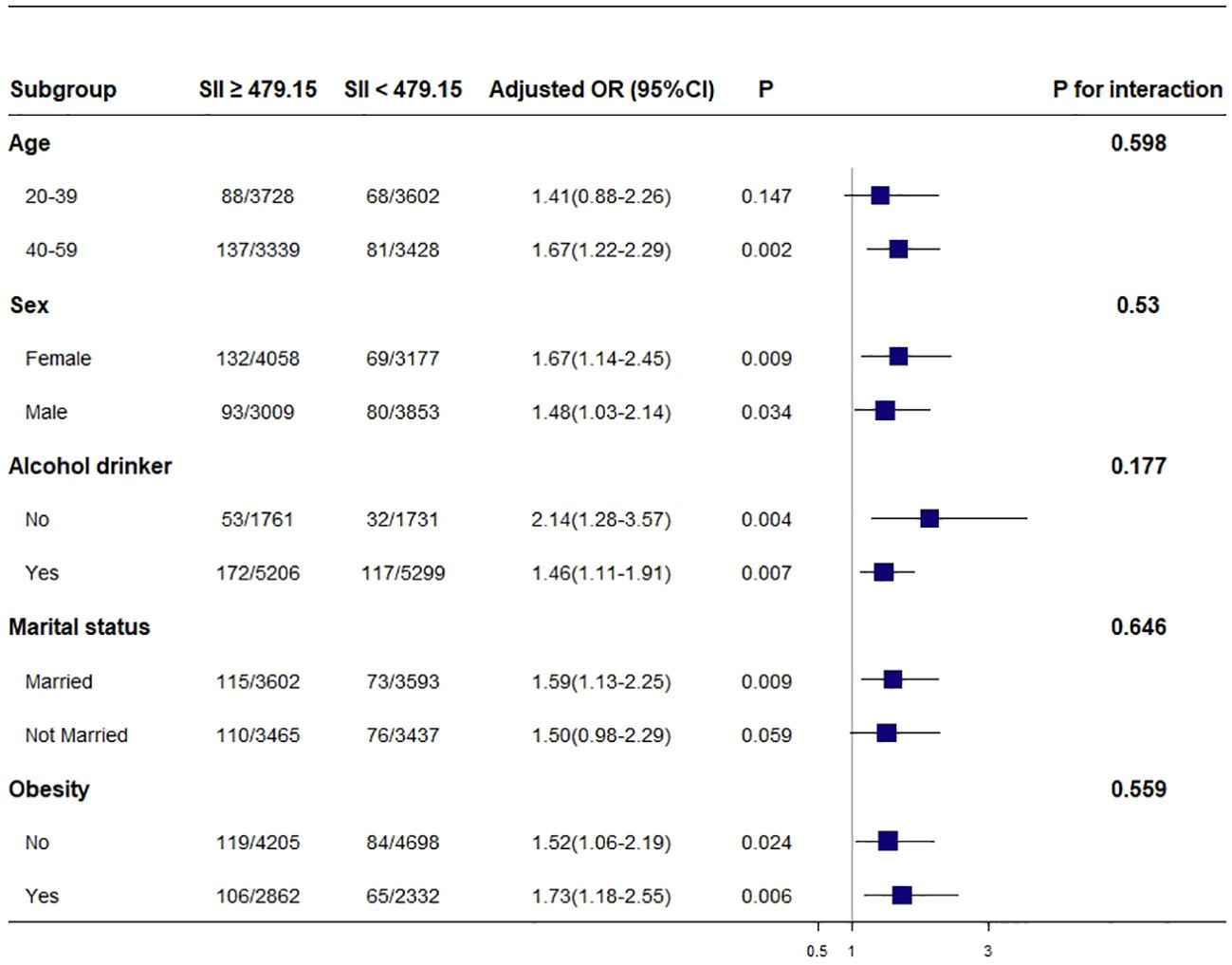
Figure 2 Association between SII and psoriasis. Each stratification was adjusted for age, sex, race and ethnicity, family income, educational level, marital status, NHANES cycles, BMI, alcohol drinking status, and smoking status except the stratification factor itself. Squares indicate odds ratios (ORs), with horizontal lines indicating 95% CIs. Obesity was defined as BMI ≥ 30. SII, systemic immune-inflammatory index; NHANES, National Health and Nutrition Examination Survey; BMI, body mass index.
Many studies have found the significant contribution of chronic inflammation to the progression of psoriasis (16, 17). The immune system’s role as a prognostic determinant in the pathogenesis of many diseases has been recognized over a long period of time. SII was determined by tallying up the numbers of three different types of immune cells: lymphocytes, platelets, and neutrophils. The SII level, which reflects inflammatory responses, shows potential as a valuable diagnostic biomarker for evaluating overall inflammatory activity. A retrospective study suggests SII could function as a prognostic indicator for adults with psoriasis (18). However, it is still not clear if there is a link between SII levels and psoriasis among outpatient US adults. Our previous study, published in JAMA Dermatology, indicated that in outpatient US adults, psoriasis was positively associated with non-alcoholic fatty liver disease (NAFLD) (14). A recent study has shown a positive association between SII and hyperlipidemia among outpatient US adults (9). Hyperlipidemia is recognized as a risk factor for NAFLD. Therefore, it raises the question of whether there is a positive association between SII and psoriasis. In this cross-sectional study, our findings suggest that participants with SII higher than 479.15 × 109/L had a higher risk of psoriasis after fully adjusting. Furthermore, SII characterized by a non-intrusive methodology, cost-effectiveness, and easy accessibility is a widely available method. Therefore, SII can be identified as a biomarker for psoriasis in the outpatient US adult population.
This is the first cross-sectional study focused on the risk of higher SII on psoriasis in the outpatient US population. Due to our consideration of the NHANES design for obtaining nationally representative estimates in the United States, our findings should be applicable to the outpatient population of US adults.
Our subgroup analysis showed that participants with SII higher than 479.15 × 109/L and obesity had a higher risk of psoriasis. Due to the restricted sample size of participants in this cross-sectional study, it is advisable to interpret these results with caution, and more well-designed prospective studies are warranted.
As a cross-sectional study, the reliability of drawing causal conclusions is not robust, and we cannot completely rule out the potential impact of residual confounding from unmeasured variables. While NHANES is a nationally representative survey, the generalizability of our conclusions to other countries is uncertain, and further research is needed to explore the precise associations among them.
Our findings suggest a positive association between a SII higher than 479.15 × 109/L and a high risk of psoriasis among outpatient US adults. SII characterized by a non-intrusive methodology, cost-effectiveness, and easy accessibility is a widely available method. Therefore, SII can be identified as a biomarker for psoriasis in the outpatient US adult population.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
The studies involving humans were approved by National Center for Health Statistics (NCHS). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
QD: Writing – original draft, Writing – review & editing. XL: Writing – review & editing, Writing – original draft. LL: Writing – review & editing, Writing – original draft. XX: Writing – original draft, Writing – review & editing. WJ: Writing – review & editing, Writing – original draft. XC: Writing – review & editing, Writing – original draft. JC: Writing – review & editing, Writing – original draft. TL: Writing – review & editing, Writing – original draft.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Rachakonda TD, Schupp CW, Armstrong AW. Psoriasis prevalence among adults in the United States. J Am Acad Dermatol. (2014) 70:512–6. doi: 10.1016/j.jaad.2013.11.013
2. Armstrong AW, Mehta MD, Schupp CW, Gondo GC, Bell SJ, Griffiths CEM. Psoriasis prevalence in adults in the United States. JAMA Dermatol. (2021) 157(8):940–6. doi: 10.1001/jamadermatol.2021.2007
3. Vanderpuye-Orgle J, Zhao Y, Lu J, Shrestha A, Sexton A, Seabury S, Lebwohl M. Evaluating the economic burden of psoriasis in the United States. J Am Acad Dermatol. (2015) 72(6):961–7.e5. doi: 10.1016/j.jaad.2015.02.1099
4. Tang Y, Peng B, Liu J, Liu Z, Xia Y, Geng B. Systemic immune-inflammation index and bone mineral density in postmenopausal women: a cross-sectional study of the national health and nutrition examination survey (NHANES) 2007–2018. Front Immunol. (2022) 13:975400. doi: 10.3389/fimmu.2022.975400
5. Hu B, Yang X-R, Sun YF, Sun C, Guo W, Zhang X, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res Off J Am Assoc Cancer Res. (2014) 20(23):6212–22. doi: 10.1158/1078-0432.CCR-14-0442
6. Di X, Liu S, Xiang L, Jin X. Association between the systemic immune-inflammation index and kidney stone: a cross-sectional study of NHANES 2007–2018. Front Immunol. (2023) 14:1116224. doi: 10.3389/fimmu.2023.1116224
7. van de Kerkhof PC. From empirical to pathogenesis-based treatments for psoriasis. J Invest Dermatol. (2022) 142:1778–85. doi: 10.1016/j.jid.2022.01.014
8. Guo W, Song Y, Sun Y, Du H, Cai Y, You Q, et al. Systemic immune-inflammation index is associated with diabetic kidney disease in Type 2 diabetes mellitus patients: evidence from NHANES 2011–2018. Front Endocrinol. (2022) 13:1071465. doi: 10.3389/fendo.2022.1071465
9. Mahemuti N, Jing X, Zhang N, Liu C, Li C, Cui Z, et al. Association between systemic immunity-inflammation index and hyperlipidemia: a population-based study from the NHANES (2015–2020). Nutrients. (2023) 15(5):1177. doi: 10.3390/nu15051177
10. Liu N, Zhang C, Hua W. Dietary inflammatory potential and psoriasis: A cross-sectional study. J Dermatol. (2023) 50:692–9. doi: 10.1111/1346-8138.16731
11. Wei J, Jaleel T, MacLeod AS, Ji JS. Inverted U-shaped relationship between vitamin D and ever-reported eczema in US adults. Allergy. (2019) 74(5):964–75. doi: 10.1111/all.13708
12. Ma C, Schupp CW, Armstrong EJ, Armstrong AW. Psoriasis and dyslipidemia: a population-based study analyzing the National Health and Nutrition Examination Survey (NHANES). J Eur Acad Dermatol Venereol JEADV. (2014) 28(8):1109–12. doi: 10.1111/jdv.12232
13. Zhao L, Sun Y, Liu Y, Yan Z, Peng W. A J-shaped association between Dietary Inflammatory Index (DII) and depression: A cross-sectional study from NHANES 2007–2018. J Affect Disord. (2023) 323:257–63. doi: 10.1016/j.jad.2022.11.052
14. Ruan Z, Lu T, Chen Y, Yuan M, Yu H, Liu R, et al. Association between psoriasis and nonalcoholic fatty liver disease among outpatient US adults. JAMA Dermatol. (2022) 158(7):745–53. doi: 10.1001/jamadermatol.2022.1609
15. Kabadi SM, Lee BK, Liu L. Joint effects of obesity and vitamin D insufficiency on insulin resistance and type 2 diabetes: results from the NHANES 2001–2006. Diabetes Care. (2012) 35:2048–54. doi: 10.2337/dc12-0235
16. Griffiths CEM, Armstrong AW, Gudjonsson JE, Barker JNWN. Psoriasis. Lancet Lond Engl. (2021) 397(10281):1301–15. doi: 10.1016/S0140-6736(20)32549-6
17. Boehncke W-H. Systemic inflammation and cardiovascular comorbidity in psoriasis patients: causes and consequences. Front Immunol. (2018) 9:579. doi: 10.3389/fimmu.2018.00579
Keywords: psoriasis, systemic immune-inflammatory index (SII), cross-sectional study, National Health and Nutrition Examination Survey (NHANES), outpatient US adults
Citation: Ding Q, Li X, Lin L, Xie X, Jing W, Chen X, Chen J and Lu T (2024) Association between systemic immunity-inflammation index and psoriasis among outpatient US adults. Front. Immunol. 15:1368727. doi: 10.3389/fimmu.2024.1368727
Received: 11 January 2024; Accepted: 15 May 2024;
Published: 04 June 2024.
Edited by:
Giusto Trevisan, University of Trieste, ItalyReviewed by:
Jing Luo, Tsinghua University, ChinaCopyright © 2024 Ding, Li, Lin, Xie, Jing, Chen, Chen and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tao Lu, bHV0YW9paEAxMjYuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.