- 1School of Rehabilitation Science, Shanghai University of Traditional Chinese Medicine, Shanghai, China
- 2Engineering Research Centre of Traditional Chinese Medicine Intelligent Rehabilitation, Ministry of Education, Shanghai, China
- 3Institute of Rehabilitation Medicine, Shanghai Academy of Traditional Chinese Medicine, Shanghai, China
Background: Tendinopathy is a growing global concern affecting many people, like athletes, workers, and the elderly. Despite its commonality among the sporting population, there is no practical clinical guideline for patellar tendinopathy (PT). Furthermore, there is conflicting evidence between clinical guidelines on shockwave therapy’s application and clinical utility for Achilles tendinopathy (AT) and plantar fasciitis (PF). Thus, our aim of this study is to evaluate the evidence for shockwave therapy; to provide a Grading of Recommendation, Assessment, Development and Evaluation (GRADE) level of the evidence and effectiveness of shockwave therapy for patellar tendinopathy, Achilles tendinopathy, and Plantar fasciitis.
Method: Medical Literature Analysis and Retrieval System Online (Medline), Embase, The Cumulative Index to Nursing and Allied Health Literature (CINAHL), Physiotherapy Evidence Database (PEDro) and China National Knowledge Infrastructure database (CNKI) were searched to find relevant studies published before December 14th, 2022.
Results: Our study showed that for PT in the short term, extracorporeal shockwave therapy (ESWT) or ESWT + eccentric exercise (EE) has a negligible effect on pain and function compared to a placebo or placebo + EE. On the contrary, ESWT significantly affects pain compared to conservative treatment (CT). For AT, ESWT has a small inconclusive effect on pain and function in the short term compared to EE. On the other hand, a placebo outperformed ESWT in improving function for AT but not pain outcomes. PF showed that ESWT significantly affects short- and long-term pain and function. When ESWT was compared to other interventions such as low laser therapy (LLLT), corticosteroid injection (CSI), or CT, there was a small inconclusive effect on pain and function in the short term.
Conclusion: There is low-moderate evidence that ESWT has a negligible effect on pain and function for PT and AT. However, high-quality evidence suggests ESWT has a large effect on pain and function for PF.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023396835, identifier CRD42023396835.
1 Introduction
Tendinopathy is a growing global concern affecting a broad spectrum of people, like athletes, workers, and the elderly (1). Surprisingly, there have been no studies to quantify the total burden of disease that tendinopathy can place on society, governments, and patients (1). Lower limb Tendinopathy (LLT) frequently occurs at the lateral to posterior hip as gluteal tendinopathy, anterior knee as patellar tendinopathy, posteriorly medial ankle as Achilles tendinopathy, or posterior tibialis tendinopathy (2, 3). According to Hopkins et al. (1), characteristics such as sex, age, occupation, physical activity level, and type of sports involved are risk factors for developing LLT. LLT increases with age and affects females more than males (3). The higher rates in females are hypothesized to be due to the metabolic changes that occur during menopause. However, studies have shown that patellar tendinopathy affects athletic men more than athletic women (4, 5).
Patellar tendinopathy (PT) is persistent patellar tendon pain and loss of function related to mechanical loading due to high-impact loading on the knee extensor during physical activities (5, 6). King et al. (4) depicted a prevalence of PT in the athletic population to account for 14.2% of the overall sports injury. Citing sports that demand a high load on the knee extensor complex had a high prevalence, while sports with a low impact on the knee extensor complex had a low prevalence. In elite male soccer/football, approximately 2.4% of players every season get affected by PT, with 61% of these athletes missing up to one week of competition or training session (7). Evidence suggests that Ultrasonographic abnormality is three times as common as clinical symptoms; hence clinical diagnosis is the preferred option for diagnosing PT (8).
Additionally, Achilles tendinopathy (AT) is persistent Achilles tendon pain and loss of function related to mechanical loading due to excessive loading on the plantar flexor complex (9, 10). AT can occur at the midportion of the Achilles tendon or the insertion of the Achilles tendon. AT can affect both the sporting population and the general population. De Jonge et al. (11) showed that the AT incidence rate is 2.53 per 1000 persons in the adult population. Of this, 35% of the cases are related to sporting activities. Although there is a higher cumulative incidence of AT before age 45, the lifetime cumulative incidence of AT is 52% for former endurance runners (12).
Moreover, Plantar fasciitis (PF) is posterior foot pain or heel pain that occurs along the calcaneus to the digits of the foot (13). The prevalence of PF in the general population is approximately 3.6% to 7%; however, PF accounts for 8% of all running-related injuries (14–16). A high body mass index and limited dorsiflexion are the most common risk factors for developing PF (17). As per the conditions mentioned above, PF is also a clinical diagnosis. The first-step pain and pain during weight-bearing activities are the main symptoms (18, 19).
Despite its commonality among the sporting population, there is no practical clinical guideline for patellar tendinopathy. The last systematic review looking at the effectiveness of shockwave therapy for PT was published more than five years ago, and therefore, new trials could have been done in the interim (20, 21). The clinical uncertainty surrounding the level of evidence for shockwave therapy use for PT persists. Furthermore, there needs to be more clarity between clinical guidelines for Achilles tendinopathy, with one clinical guideline that does not recommend shockwave therapy. In contrast, the other clinical guideline does recommend it as an adjunct modality (10, 22). This uncertainty between clinical guidelines could lead to ambiguity among clinicians on whether or not to use shockwave therapy in their clinical practice. Additionally, the latest review that looked at the effectiveness of shockwave therapy for AT used a fixed effect model in their analysis, which does not account for variations in participant characteristics between studies, the distribution of effect sizes, and differences in treatment protocols, dosages, and procedures (23). A similar situation exists in PF clinical guidelines where one guideline recommends it as a secondary approach if standard care fails while the other does not. Apart from this, an updated systematic review is needed due to the previous review investigating the effectiveness of shockwave therapy for PF being ≥ five years (24, 25).
This systematic review aimed to evaluate the evidence for shockwave therapy; to provide a Grading of Recommendations, Assessment, Development and Evaluations (GRADE) level of the evidence and effectiveness of shockwave therapy for patellar tendinopathy, Achilles tendinopathy, and Plantar fasciitis.
2 Methods
2.1 Search strategy and eligibility criteria
This systematic review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (26). This study did not require ethical approval since the data was obtained exclusively from previously published sources.
An electronic literature search was conducted via four English language databases and one Chinese database; these search databases are as follows: Medical Literature Analysis and Retrieval System Online (Medline) was searched on December 14th, 2022, Embase on December 15th, 2022, The Cumulative Index to Nursing and Allied Health Literature (CINAHL) on December 18th, 2022, Physiotherapy Evidence Database (PEDro) on December 17th, 2022 and China National Knowledge Infrastructure database (CNKI) on December 18th, 2022. The detailed search strategy is presented in the Supplementary Material. The following Boolean operators were used in Medline, Embase, and CINAHL, databases to search for patellar tendinopathy; (patellar tendinopathy) OR (jumper’s knee) OR (patellar tendinosis) OR (patellar tendinitis) OR (patellar tendonitis) AND (shockwave) OR (shockwave therapy) OR (radial shockwave) OR (focused shockwave) OR (extracorporeal shockwave) OR (ESWT). The Boolean operators for Achilles tendinopathy; (Achilles tendinopathy) OR (Mid-portion Achilles tendinopathy) OR (Insertional Achilles tendinopathy) AND (shockwave) OR (shockwave therapy) OR (radial shockwave) OR (focused shockwave) OR (extracorporeal shockwave) OR (ESWT). The Boolean operators for Plantar fasciitis (plantar fasciitis) OR (plantar fasciopathy) OR (heel pain) AND (shockwave) OR (shockwave therapy) OR (radial shockwave) OR (focused shockwave) OR (extracorporeal shockwave) OR (ESWT). Previous systematic reviews were screened for articles and checked citations through google scholar.
The inclusion criteria were: P; People between the ages of 18 or 70 with a clinical diagnosis of patellar tendinopathy, Achilles tendinopathy, and plantar fasciitis of any duration and severity with or without radiological confirmation. I; Studies that included shockwave therapy: radial shockwave therapy or focused shockwave therapy as the mode of treatment. C; Studies compared shockwave therapy to placebo, eccentric exercise, or other interventions. O; Studies that had pain and function as outcome measures. S; completed randomized controlled trials were included in this study. Studies were excluded from the analysis: non-randomized trials, case reports, observational studies, literature reviews, case series, and public conference abstracts. RCTs protocols, uncompleted and unable to access full-text of RCTs were excluded. Studies with missing information regarding the outcome data and the corresponding author who did not respond when contacted for missing data were included in the systematic review for qualitative analysis but were excluded from the quantitative analysis.
2.2 Outcome measure
Primary outcome: One primary outcome was pain intensity, measured by a self-reporting tool such as a visual analog scale (VAS), numeric rating scale (NRS), or an equivalent pain perception scale. The other primary outcome was function measured by a self-reporting tool such as the Victorian Institute of sports assessment-patellar (VISA-P), Victorian Institute of sports assessment-Achilles (VISA-A), Foot Function Index (FFI), American Orthopaedic Foot and Ankle Society (AOFAS) and Roles and Maudsley Score (RMS). The timing of the follow-up grouped outcomes: short-term (≤3 months), mid-term (>3 months- ≤ 6 months), and long-term (≥12 months).
2.3 Selection of studies and assessment of quality
Two independent reviewers screened all titles and abstracts identified by the search strategy to pinpoint potentially eligible studies. Then, they independently assessed all full texts, and the RCTs that met the inclusion criteria were included in the systematic review. In a disagreement, the two independent reviewers discussed trying to come to a resolution. If no resolution was found, a third reviewer assessed the situation and decided whether or not the article is included or excluded. A commercial reference management software was used for retrieving studies, screening, eliminating duplicates, and managing references.
The internal validity of the included studies was assessed using the Cochrane Collaboration tool for assessing the risk of bias in randomized trials (27). Five domains from this tool were evaluated: Bias arising from the randomization process, bias due to deviation from intended interventions, bias due to missing outcome data, bias in the measurement of the outcome, and bias in the selection of the reported result. The study was classified as having a ‘low,’ ‘high,’ or ‘unclear’ risk of bias based on the two independent reviewer’s judgment of the subcomponents of the Cochrane risk of bias tool. Discrepancies were resolved through discussions. If no resolution was found, a third reviewer assessed the situation and decide on the risk of bias. The Grading of Recommendation Assessment, Development, and Evaluation (GRADE) tool was used to assess the certainty of the evidence (28). This tool comprises five main domains: risk of bias, inconsistency of results, indirectness of evidence, imprecision, and publication bias, assessed independently by two reviewers and resolved through discussion. If no resolution was found, a third reviewer assessed the situation.
2.4 Data collection and analysis
Two independent reviewers extracted the data from included studies that characterize the similarities and differences among participants: sample size, sex, age range, country, and type of population. Furthermore, shockwave therapy intervention data were extracted, such as intensity, frequency of treatment, and total duration of the intervention period. The data was compelled and then stored on commercial Microsoft office software.
The meta-analysis was conducted using Revman 5.4 software. Post-treatment means and SDs were extracted from continuous data, while dichotomous data, such as successful outcomes, were extracted. Where there were missing data, the corresponding author was contacted regarding the missing data. If requested data was not provided, attempts to calculate the SDs from CIs, SEs, or p- values were done according to the Cochrane Handbook for systematic reviews of interventions (29). For reporting continuous data, a standardized mean difference (SMD) was calculated, irrespective of whether the outcomes were similar or different. However, only outcomes of a similar construct, for example, pain intensity: VAS and NRS, were combined. The Effect sizes were 0.20-0.49 as small, 0.50-0.79 as medium, and 0.80 or above as large (30). For reporting dichotomous outcomes, odd ratios were used to represent intervention success, where a positive intervention effect >1. The random effects model with a 95% confidence interval was used, assuming variations in participant characteristics between studies, the distribution of effect sizes, and differences in treatment protocols, dosages, and procedures. An I2 test measured heterogeneity; an I2 value of 25% was low, 50% was moderate, and 75% was high heterogeneity (31). Suppose an analysis includes ten or more studies, and there is statistical significance for heterogeneity with a high percent of I2 (>75%). In that case, the prediction interval was examined to determine the estimated effect size distribution. After determining the seriousness of the heterogeneity, further subgroup analysis of the outliers may be performed if warranted. Additionally, if ten or more studies are included in an analysis, a funnel plot was be created to test for publication bias.
3 Results
3.1 Result of search
A total of 6348 articles were identified during the initial search of the above databases and through checking citations on google scholar. After the vigorous screening, sixty-three studies were eligible for this systematic review. Figure 1 depicts the flow of articles through the search, screening, and inclusion processes.
3.2 Characteristics of studies
Sixty-three studies were included in this review; ten studies on patellar tendinopathy, thirteen studies on Achilles tendinopathy, and forty articles on plantar fasciitis. Details about the characteristics of the included studies are shown in Table 1.
3.3 Risk of bias and certainty of the evidence assessment
Of the sixty-three studies included in this systematic review, the randomization process was classified as low risk of bias in fifty-five studies, high risk of bias in seven, and with some concerns of bias in one study. All Sixty-three studies had a low risk of bias for deviation from the intended intervention. Missing outcome data had twenty-four studies at low risk and thirty-nine studies at high risk. The risk of bias due to measurement was classified as low in forty-two studies and high in twenty-one studies. The risk of bias in the selection of the reported result was forty-seven articles low, three articles high, and thirteen articles with some concerns of bias. The risk of bias in the included studies is depicted below in Figure 2. The detailed GRADE quality assessment result is shown in Figures 7 to 16 on Supplementary Material.
3.4 Clinical heterogeneity
Nine out of the possible ten studies for patellar tendinopathy were done in the sporting population from varying sports such as basketball, handball, volleyball, football, and track and field. Only one study was done on the general population. In addition, all thirteen included studies looking at Achilles tendinopathy were in the general population. These studies recruited a higher number of males in studies. On the contrary, all forty studies for plantar fasciitis recruited more females than males. Also, the studies were done on the general population.
Four studies compared Extracorporeal Shockwave therapy (ESWT) to placebo only for PT. These studies had very similar shockwave impulses at 1500-3000, the frequency at 4Hz, the treatment session at three weeks, and the duration at 3-5 weeks. The two studies that compared focused ESWT + Eccentric exercise (EE) to placebo + EE showed differences in treatment sessions and durations for shockwave where one study had three treatment sessions over three weeks while the other had six treatment sessions over six weeks; however, they both had similar repetition and set ranges; however different load (intensity). A study compared focused ESWT + EE to radial ESWT + EE, and another study compared radial ESWT against conservative treatment; however, Wang et al. compared ESWT to conservative treatment. The final article for PT compared platelet-rich plasma against ESWT.
Additionally, the six articles that compared ESWT to a placebo for Achilles tendinopathy had vast variations in the treatment session, treatment duration, shockwave impulse, and frequency. Another six studies compared ESWT to EE with identical exercise prescriptions but differences in ESWT protocol. The final two trials compared ESWT to Hyaluronan injection, Cold air, and High Energy Laser Therapy.
Also, thirteen studies compared ESWT to placebo for plantar fasciitis with varying discrepancies in ESWT procedure and protocol. The seven studies that compared ESWT to Corticosteroid injection (CSI) also had variations in ESWT procedure and protocol. In addition, five articles compared ESWT to low laser therapy (LLLT), and three compared ESWT to prolotherapy with a difference in the protocol for the intervention and control groups. The remaining twelve studies that compared ESWT to conservative treatment CT depicted similar inconsistencies. Important to note that the follow-up timepoint varied from immediate (directly after the intervention) to 144 weeks after the intervention.
3.5 Evidence of effect on patellar tendinopathy
ESWT VS Placebo: based on the analysis of three studies comparing ESWT to placebo, it can be concluded with very low certainty of evidence that ESWT intervention has no superiority over placebo for reducing pain in the short-term. ESWT +EE VS Placebo+ EE: from the analysis of three studies comparing ESWT + EE and placebo + EE, it can be concluded with moderate certainty of evidence that ESWT intervention had a negligible effect in reducing pain but crosses the line of no effect; thus, no conclusive superiority over placebo. Additionally, ESWT had no superiority over placebo for improving function in the short term. ESWT VS Conservative treatment: based on the analysis of two studies comparing ESWT to conservative treatment, it can be concluded with low certainty of evidence that ESWT has a large treatment effect for reducing pain in the short term. A forest plot of the results is presented in Figures 3A, B.
Figure 3 (A): Meta-analysis results and forest plot of the effectiveness of ESWT compared to Placebo, ESWT+ Eccentric exercise versus Placebo+ Eccentric exercise, ESWT compared to Conservative treatment for Patellar tendinopathy pain in the short term. (B): ESWT+ Eccentric exercise versus Placebo+ Eccentric exercise for Patellar tendinopathy function in the short term.
3.6 Evidence of effect on Achilles tendinopathy
ESWT VS Placebo: From the analysis of four studies comparing ESWT and placebo, it can be concluded with low certainty of evidence that ESWT intervention had a large effect in improving function and reducing pain in the short term but crosses the line of no effect; thus, no conclusive superiority over placebo. ESWT VS EE: Based on the analysis of five studies comparing ESWT to EE, it can be concluded with low certainty of evidence that ESWT intervention had a small effect on reducing pain but crosses the line of no effect; thus, no conclusive superiority over EE. Additionally, ESWT had no superiority over EE for improving function in the short term. A forest plot of the results is presented in Figures 4A, B.
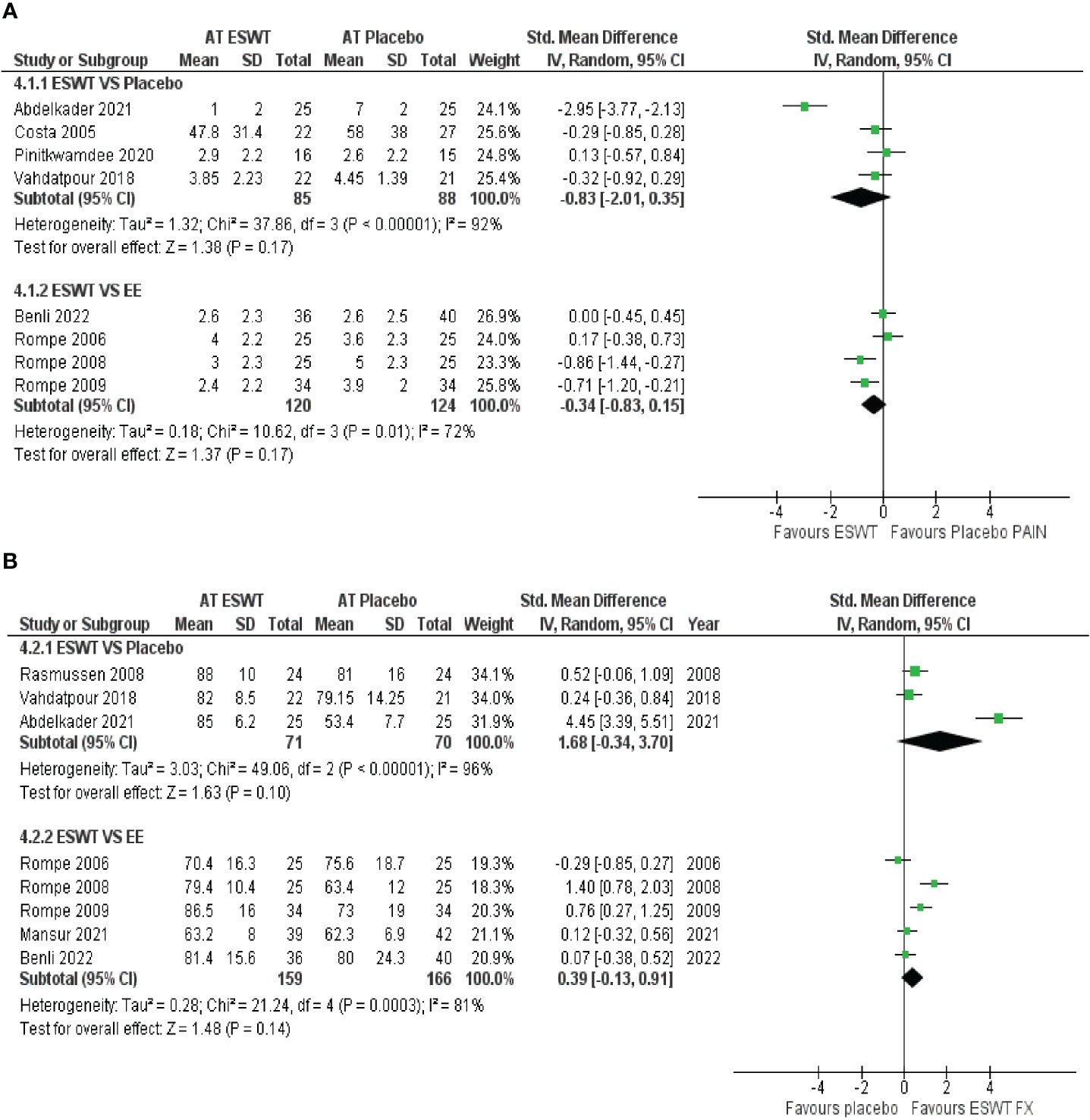
Figure 4 (A): Meta-analysis results and forest plot of the effectiveness of ESWT compared to Placebo, ESWT compared to EE for Achilles tendinopathy for function in the short-term, ESWT compared to Placebo. (B): ESWT compared to EE for Achilles tendinopathy in the short term for pain.
3.7 Evidence of effect on plantar fasciitis
ESWT VS Placebo: from the analysis of thirteen studies comparing ESWT and placebo, it can be concluded with moderate-high certainty of evidence that ESWT has a large treatment effect for improving function in the short term. Additionally, ESWT has a large treatment effect on reducing pain in the short-term, mid-term, and long-term. ESWT VS CSI: based on the analysis of six studies comparing ESWT to CSI, it can be concluded with very low certainty of evidence that ESWT had a small effect on reducing pain in the short term but crosses the line of no effect thus no conclusive superiority over CSI. ESWT VS LLLT: from the analysis of four studies comparing ESWT and LLLT, it can be concluded with low - moderate certainty of evidence that ESWT intervention had a negligible effect on improving function but crosses the line of no effect; thus, no conclusive superiority over LLLT. Additionally, ESWT had no superiority over LLLT in reducing pain in the short term. ESWT VS Prolotherapy: Based on the analysis of three studies comparing ESWT to Prolotherapy, it can be concluded with low certainty of evidence that ESWT intervention had a small effect on reducing pain in the short term but crosses the line of no effect; thus, no conclusive superiority over prolotherapy. ESWT VS CT: from the analysis of five studies comparing ESWT and CT, it can be concluded with low certainty of evidence that ESWT intervention has no superior over CT for reducing pain in the short term. A forest plot of the results is presented in Figures 5, 6.
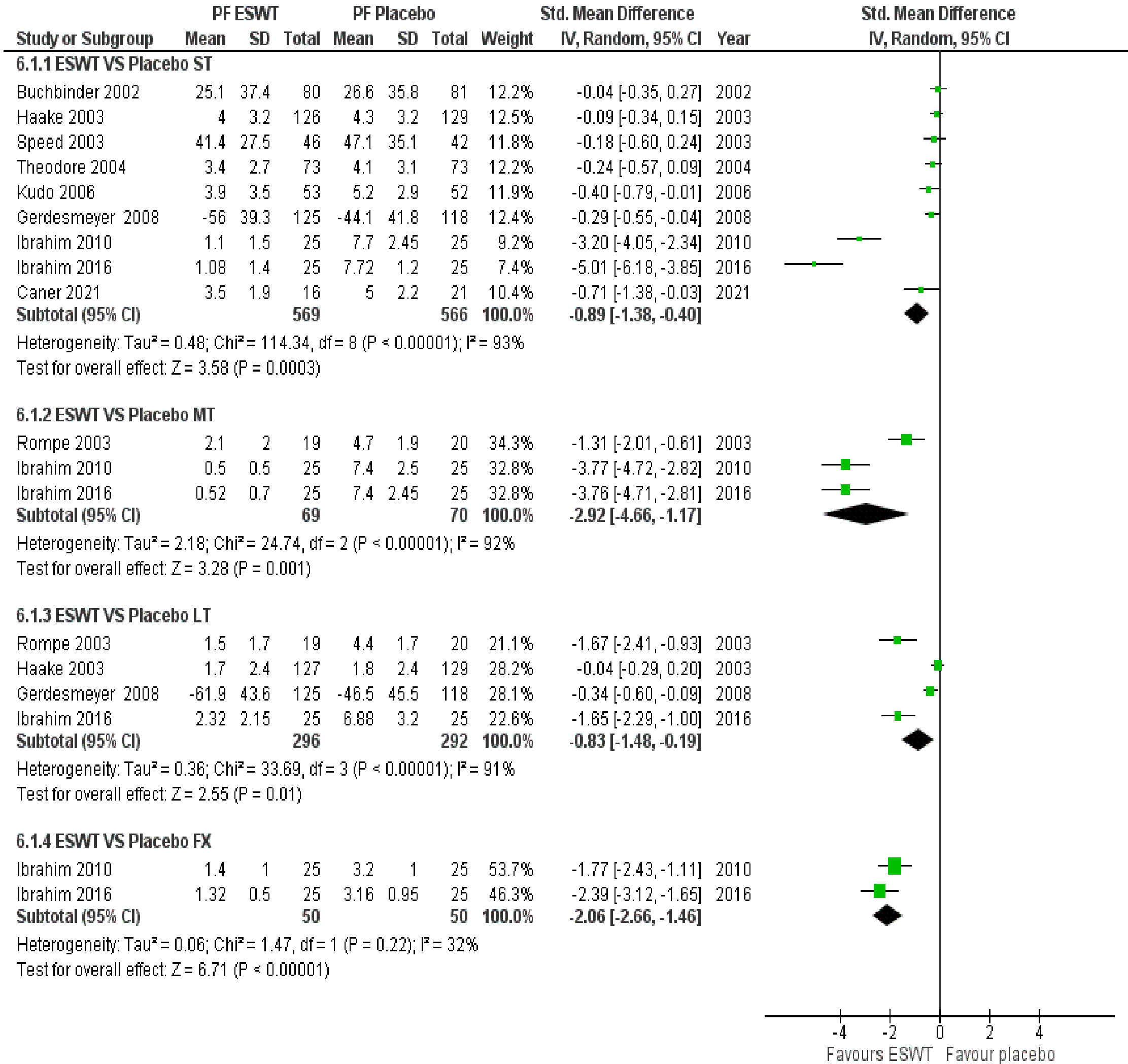
Figure 5 Meta-analysis results and forest plot of the effectiveness of ESWT compared to Placebo for Plantar Fasciitis in the short-term, mid-term and long-term for pain.
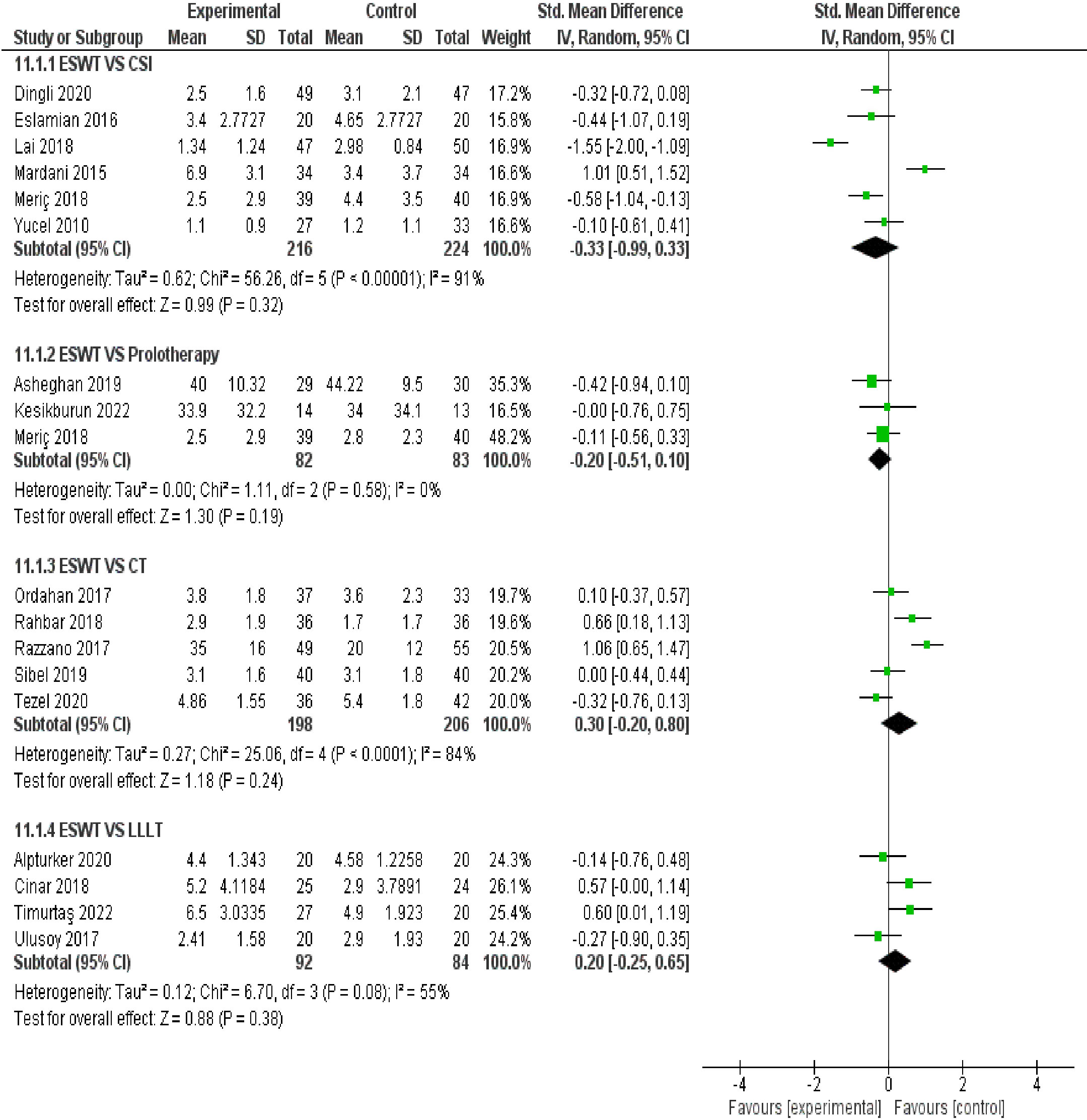
Figure 6 Meta-analysis results and forest plot of the effectiveness of ESWT compared to other treatments for Plantar Fasciitis in the short term for pain.
3.8 Publication bias
No publication bias analysis was done because fewer than ten studies were in an analysis group.
4 Discussion
4.1 Summary of effects
In this systematic review, we investigated the effectiveness of ESWT on pain and function for patellar tendinopathy, Achilles tendinopathy, and plantar fasciitis compared to a placebo, eccentric exercise, and other interventions. Our study found low to moderate-quality evidence that ESWT or ESWT + EE has a negligible effect on pain and function in the short term compared to a placebo or placebo + EE for PT. On the contrary, we found low-quality evidence that ESWT has a large effect on pain in the short term compared to conservative treatment for PT. For AT, our review found low-quality evidence that ESWT may have a small inconclusive effect on pain and function in the short term compared to EE. On the other hand, a placebo outperformed ESWT in improving function for AT but not pain outcomes. The results for PF showed moderate to high-quality evidence that ESWT has a large effect on pain and function in the short-term, mid-term, and long-term. When ESWT was compared to other interventions such as LLLT, CSI, or CT, there was low to moderate-quality evidence that suggested a small inconclusive effect on pain and function in the short term.
Most studies did not report the type of ESWT used and had vast variations in impulses, frequencies, treatment durations, and sessions. This makes it difficult to comment on an adequate protocol. Some studies did report the type of ESWT, which were Focus Extracorporeal Shockwave Therapy (fESWT) and Radial Extracorporeal Shockwave Therapy (rESWT), respectively; for PF, both fESWT and rESWT had a large effect with high-quality evidence. This implies that both fEWST and rESWT will probably give similar results on pain and function outcomes for PF. Most studies for AT and PT did not report the type of ESWT used. However, in the few studies that reported the type of intervention, negligible effects with low to moderate-quality evidence were shown in both interventions. Additionally, our findings suggest that regardless of the participants from a specific sport or general population, ESWT may have negligible effects with low to moderate quality evidence on the pain and function outcome for PT and AT patients. On the contrary, ESWT likely has a large effect, with high-quality evidence on the pain and function outcome for PF patients from a diverse population.
4.2 Summary of previous studies
Due to the lack of clinical practice guidelines for PT, a systematic review of the literature and a GRADE quality assessment of the evidence that outlines the effectiveness of ESWT and ESWT compared to its comparators is imperative to provide clinicians with quality information to make an informed decision about the best available option in managing their patients. Additionally, this review updates the evidence of the previous reviews. Manu et al. (21) conducted a systematic review investigating the effectiveness of ESWT for PT. Their inclusion criteria included both RCTs and non-RCTs, which led to poor methodological studies that may have over or under-estimated the true effect of ESWT for PT. Also, a more recent review by Korakakis et al. (20) had similar shortcomings; hence those reviews likely did not provide a reasonable answer to the effectiveness of ESWT for PT.
Furthermore, ESWT is widely used and recommended by the International Society for Medical Shockwave Treatment (ISMST) (95) for AT; however, prestigious physical therapy practice guideline (22) has recommended against using ESWT for AT leading to uncertainty amongst clinicians on whether ESWT may provide a potential benefit to patients. A recent review (96) seeks to answer the question of ESWT effectiveness for AT, but its methodology needs to be revised. The statistical method used was the fixed model, which does not account for differences in the distribution of effect sizes between studies or participant characteristics and treatment protocols. In addition, the study also included both RCTs and non-RCT trials, which likely led to poor internal validity studies that may have over or under-estimated the actual effect of ESWT for AT; hence an updated review is needed to address these flaws and to provide high-quality evidence.
Additionally, PF faces some similar challenges as AT. Previous guidelines did not recommend ESWT as a form of treatment for PF (18); however, recent guidelines do recommend ESWT for PF (19). The recent review for PF (25) did not provide estimates of the treatment effect magnitude and used a fixed statistical model, which can potentially over or under-estimate the true effect of the intervention (97); hence an updated systematic review quantifying the effectiveness and providing a GRADE quality assessment is essential in addressing this issue.
4.3 Implication of results
ESWT is a common modality used in clinical practice to treat musculoskeletal overuse injuries such as tendinopathies and fasciopathies due to its theorized mechanism for healing degenerated soft tissue (2, 19). Our study discovered these novel findings for the effectiveness of ESWT in PT, AT, and PF. ESWT had beneficial short-term effects on pain and function for PT and AT; however, the estimated effects were small and pooled from low to moderate quality evidence, so ESWT should not be used as a primary treatment for modulating pain and function outcomes for PT and AT but as an adjunct in context-specific situations with known treatments that can provide a meaningful change to the patient. On the other hand, ESWT had a large estimated effects on PF in the short to long term, which were pooled from high quality evidence; hence ESWT can be provided as primary treatment for patients with PF.
4.4 Recommendations
The majority of the current literature reports on the short-term effectiveness of ESWT for PT, AT, and PF, so future studies with large sample sizes and placebo controls should focus on the efficacy of ESWT in the long term on changing pain and function outcomes in a diverse population. Moreover, future studies should also focus on creating and using a standardized ESWT treatment protocol. In addition, studies evaluating the potential adverse event for ESWT application in PT, AT, and PF are needed.
4.5 Limitations
This study had several limitations. First, due to the limited number of included studies in the analysis, the results must be interpreted cautiously because none of our analyses had ten or more studies; hence the results may not accurately represent the true estimated effect for the population (98). Second, Only English and Chinese databases were searched. This could have left out other vital trials relevant to the topic published in other languages. Third, the significance of the heterogeneity observed in the analysis could not be appropriately explained due to the few numbers of included studies.
5 Conclusion
In conclusion, there is a negligible effect with a low to moderate certainty of evidence that ESWT can improve function and reduce pain in the short term for PT and AT. However, ESWT had a large effect with a high certainty of evidence in improving function and reducing pain in the short-term, mid-term, and long-term for PF.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
RC: protocol design, data collection, extraction, writing, and editing. LF: protocol design, risk of bias assessment, GRADE assessment, data collection, and extraction and reviewing. RZ: risk of bias assessment, data collection and extraction, and GRADE assessment. JW: data interpretation, risk of bias assessment, GRADE assessment, and analysis. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Three-year Action Plan for the Development of TCM in the Shanghai-Highland Construction for International Standardization of TCM (No. ZY(2021–2023)-0212).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2023.1193835/full#supplementary-material
References
1. Hopkins C, Fu S-C, Eldrich C, Hu X, Rolf C, Ville M, et al. Critical review on the socio-economic impact of tendinopathy. Asia-Pacific J Sports Med Arthroscopy Rehabil Technol (2016) 4(April 2016):9–20. doi: 10.1016/j.asmart.2016.01.002
2. Millar NL, Silbernagel KG, Thorborg K, Kirwan PD, Galatz LM, Abrams GD, et al. Tendinopathy. Nat Rev Dis Primers (2021) 7(1). doi: 10.1038/s41572-020-00234-1
3. Riel H, Lindstrøm CF, Rathleff MS, Jensen MB, Olesen JL. Prevalence and incidence rate of lower-extremity tendinopathies in a danish general practice: A registry-based study. BMC Musculoskeletal Disord (2019) 20(1):239. doi: 10.1186/s12891-019-2629-6
4. King D, Yakubek G, Chughtai M, Khlopas A, Saluan P, Mont MA, et al. Quadriceps tendinopathy: A review—Part 1: epidemiology and diagnosis. Ann Trans Med (2019) 7(4):71–1. doi: 10.21037/atm.2019.01.58
5. Rudavsky A, Cook J. Physiotherapy management of patellar tendinopathy (Jumper’s knee). J Physiother (2014) 60(3):122–29. doi: 10.1016/j.jphys.2014.06.022
6. Scott A, Squier K, Alfredson H, Bahr R, Cook JL, Coombes B, et al. ICON 2019: international scientific tendinopathy symposium consensus: clinical terminology. Br J Sports Med (2020) 54(5):260–62. doi: 10.1136/bjsports-2019-100885
7. Hägglund M, Zwerver J, Ekstrand J. Epidemiology of patellar tendinopathy in elite male soccer players. Am J Sports Med (2011) 39(9):1906–11. doi: 10.1177/0363546511408877
8. Cook JL, Khan KM, Kiss ZS, Griffiths L. Patellar tendinopathy in junior basketball players: A controlled clinical and ultrasonographic study of 268 patellar tendons in players aged 14-18 years: patellar tendinopathy in junior basketball players. Scandinavian J Med Sci Sports (2000) 10(4):216–20. doi: 10.1034/j.1600-0838.2000.010004216.x
9. Silbernagel KG, Hanlon S, Sprague A. Current clinical concepts: conservative management of achilles tendinopathy. J Athletic Training (2020) 55(5):438–47. doi: 10.4085/1062-6050-356-19
10. De Vos R-J, van der Vlist AC, Zwerver J, Meuffels DE, Smithuis F, Van Ingen R, et al. Dutch multidisciplinary guideline on achilles tendinopathy. Br J Sports Med (2021) 55(20):1125–34. doi: 10.1136/bjsports-2020-103867
11. De Jonge S, Van Den Berg C, De Vos RJ, van der Heide HJL, Weir A, Verhaar JAN, et al. Incidence of midportion achilles tendinopathy in the general population. Br J Sports Med (2011) 45(13):1026–28. doi: 10.1136/bjsports-2011-090342
12. Kujala UM, Sarna S, Kaprio J. Cumulative incidence of achilles tendon rupture and tendinopathy in male former elite athletes. Clin J Sport Med (2005) 15(3):133–35. doi: 10.1097/01.jsm.0000165347.55638.23
13. McPoil TG, Martin RL, Cornwall MW, Wukich DK, Irrgang JJ, Godges JJ. Heel pain—Plantar fasciitis. J Orthop Sports Phys Ther (2008) 38(4):A1–18. doi: 10.2519/jospt.2008.0302
14. Dunn JE. Prevalence of foot and ankle conditions in a multiethnic community sample of older adults. Am J Epidemiol (2004) 159(5):491–98. doi: 10.1093/aje/kwh071
15. Hill CL, Gill TK, Menz HB, Taylor AW. Prevalence and correlates of foot pain in a population-based study: the north west adelaide health study. J Foot Ankle Res (2008) 1(1):2. doi: 10.1186/1757-1146-1-2
16. Taunton JE. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med (2002) 36(2):95–101. doi: 10.1136/bjsm.36.2.95
17. Hamstra-Wright KL, Huxel Bliven KC, Curtis Bay R, Aydemir B. Risk factors for plantar fasciitis in physically active individuals: A systematic review and meta-analysis. Sports Health: A Multidiscip Approach (2021) 13(3):296–303. doi: 10.1177/1941738120970976
18. Martin RL, Davenport TE, Reischl SF, McPoil TG, Matheson JW, Wukich DK, et al. Heel pain—Plantar fasciitis: revision 2014. J Orthop Sports Phys Ther (2014) 44(11):A1–33. doi: 10.2519/jospt.2014.0303
19. Morrissey D, Cotchett M, Said J’Bari A, Prior T, Griffiths IB, Rathleff MS, et al. Management of plantar heel pain: A best practice guide informed by a systematic review, expert clinical reasoning and patient values. Br J Sports Med (2021) 55(19):1106–18. doi: 10.1136/bjsports-2019-101970
20. Korakakis V, Whiteley R, Tzavara A, Malliaropoulos N. The effectiveness of extracorporeal shockwave therapy in common lower limb conditions: A systematic review including quantification of patient-rated pain reduction. Br J Sports Med (2018) 52(6):387–407. doi: 10.1136/bjsports-2016-097347
21. Mani-Babu S, Morrissey D, Waugh C, Screen H, Barton C. The effectiveness of extracorporeal shock wave therapy in lower limb tendinopathy: A systematic review. Am J Sports Med (2015) 43(3):752–61. doi: 10.1177/0363546514531911
22. Martin RL, Chimenti R, Cuddeford T, Houck J, Matheson JW, McDonough CM, et al. Achilles pain, stiffness, and muscle power deficits: midportion achilles tendinopathy revision 2018: clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American physical therapy association. J Orthop Sports Phys Ther (2018) 48(5):A1–38. doi: 10.2519/jospt.2018.0302
23. Barili F, Parolari A, Kappetein PA, Freemantle N. Statistical primer: heterogeneity, random- or fixed-effects model analyses? Interactive Cardiovasc Thorac Surg (2018) 27(3):317–21. doi: 10.1093/icvts/ivy163
24. Li H, Xiong Y, Zhou W, Liu Y, Liu J, Xue H, et al. Shock-wave therapy improved outcome with plantar fasciitis: A meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg (2019) 139(12):1763–70. doi: 10.1007/s00402-019-03262-z
25. Xiong Y, Wu Q, Mi B, Zhou W, Liu Y, Liu J, et al. Comparison of efficacy of shock-wave therapy versus corticosteroids in plantar fasciitis: A meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg (2019) 139(4):529–36. doi: 10.1007/s00402-018-3071-1
26. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (2021), n71. doi: 10.1136/bmj.n71
27. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ (2019), l4898. doi: 10.1136/bmj.l4898
28. Brożek JL, Akl EA, Alonso-Coello P, Lang D, Jaeschke R, Williams JW, et al. Grading quality of evidence and strength of recommendations in clinical practice guidelines. Allergy (2009) 64(5):669–77. doi: 10.1111/j.1398-9995.2009.01973.x
29. Higgins JPT, Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions. In: Cochrane Book Series, 2nd ed. Hoboken, NJ: Wiley-Blackwell (2020).
30. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hoboken: Taylor and Francis (2013).
31. Higgins JPT. Measuring inconsistency in meta-analyses. BMJ (2003) 327(7414):557–60. doi: 10.1136/bmj.327.7414.557
32. Taunton J, Taunton K, Khan K. Treatment of patellar tendinopathy with extracorporeal shock wave therapy. BC Med J (2003) 45(10).
33. Zwerver J, Hartgens F, Verhagen E, van der Worp H, Van Den Akker-Scheek I, Diercks RL. No effect of extracorporeal shockwave therapy on patellar tendinopathy in jumping athletes during the competitive season: A randomized clinical trial. Am J Sports Med (2011) 39(6):1191–99. doi: 10.1177/0363546510395492
34. Zhang ZJ, Lee WC, Fu SN. One session of extracorporeal shockwave therapy-induced modulation on tendon shear modulus is associated with reduction in pain. J Sports Sci Med (2020) 19:309–16.
35. Persson Krogh T, Astrup JK, Kyed C, Fredberg U. Extracorporeal shockwave therapy in the treatment of patellar tendinopathy: A randomized, double-blind, placebo-controlled trial. Trans Sports Med (2021) 4(4):534–44. doi: 10.1002/tsm2.246
36. Thijs KM, Zwerver J, Backx FJG, Steeneken V, Rayer S, Groenenboom P, et al. Effectiveness of shockwave treatment combined with eccentric training for patellar tendinopathy: A double-blinded randomized study. Clin J Sport Med (2017) 27(2):89–96. doi: 10.1097/JSM.0000000000000332
37. Lee W-C, Ng GY-F, Zhang Z-J, Malliaras P, Masci L, Fu S-N. Changes on tendon stiffness and clinical outcomes in athletes are associated with patellar tendinopathy after eccentric exercise. Clin J Sport Med Publish Ahead Print (2007). 46(5):348–357. doi: 10.1097/JSM.0000000000000562
38. Cheng L, Chang S, Qian L, Wang Y, Yang M. Extracorporeal shock wave therapy for isokinetic muscle strength around the knee joint in athletes with patellar tendinopathy. J Sports Med Phys Fitness (2019) 59(5). doi: 10.23736/S0022-4707.18.09023-0
39. Wang C-J, Ko J-Y, Chan Y-S, Weng L-H, Hsu S-L. Extracorporeal shockwave for chronic patellar tendinopathy. Am J Sports Med (2007) 35(6):972–78. doi: 10.1177/0363546506298109
40. Van Der Worp H, Zwerver J, Hamstra M, Van Den Akker-Scheek I, Diercks RL. No difference in effectiveness between focused and radial shockwave therapy for treating patellar tendinopathy: A randomized controlled trial. Knee Surg Sports Traumatol Arthroscopy (2014) 22(9):2026–32. doi: 10.1007/s00167-013-2522-z
41. Vetrano M, Castorina A, Vulpiani MC, Baldini R, Pavan A, Ferretti A. Platelet-rich plasma versus focused shock waves in the treatment of jumper’s knee in athletes. Am J Sports Med (2013) 41(4):795–803. doi: 10.1177/0363546513475345
42. Abdelkader NA, Helmy MNK, Fayaz NA, Saweeres ESB. Short- and intermediate-term results of extracorporeal shockwave therapy for noninsertional achilles tendinopathy. Foot Ankle Int (2021) 42(6):788–97. doi: 10.1177/1071100720982613
43. Demir Benli M, Tatari H, Balcı A, Peker A, Şimşek K, Yüksel O, et al. A comparison between the efficacy of eccentric exercise and extracorporeal shock wave therapy on tendon thickness, vascularity, and elasticity in achilles tendinopathy: A randomized controlled trial. Turkish J Phys Med Rehabil (2022) 68(3):372–80. doi: 10.5606/tftrd.2022.8113
44. Gatz M, Schweda S, Betsch M, Dirrichs T, de laFuente M, Reinhardt N, et al. Line- and point-focused extracorporeal shock wave therapy for achilles tendinopathy: A placebo-controlled RCT study. Sports Health: A Multidiscip Approach (2021) 13(5):511–18. doi: 10.1177/1941738121991791
45. Vahdatpour B, Forouzan H, Momeni F, Ahmadi M, Taheri P. Effectiveness of extracorporeal shockwave therapy for chronic achilles tendinopathy: A randomized clinical trial. J Res Med Sci (2018) 23(1):37. doi: 10.4103/jrms.JRMS_413_16
46. Lynen N, De Vroey T, Spiegel I, Ongeval FV, Hendrickx N-J, Stassijns G. Comparison of peritendinous hyaluronan injections versus extracorporeal shock wave therapy in the treatment of painful achilles’ Tendinopathy: A randomized clinical efficacy and safety study. Arch Phys Med Rehabil (2017) 98(1):64–71. doi: 10.1016/j.apmr.2016.08.470
47. Notarnicola A, Maccagnano G, Tafuri S, Forcignanò MI, Panella A, Moretti B. CHELT therapy in the treatment of chronic insertional achilles tendinopathy. Lasers Med Sci (2014) 29(3):1217–25. doi: 10.1007/s10103-013-1510-3
48. Rasmussen S, Christensen M, Mathiesen I, Simonson O. Shockwave therapy for chronic achilles tendinopathy: A double-blind, randomized clinical trial of efficacy. Acta Orthop (2008) 79(2):249–56. doi: 10.1080/17453670710015058
49. Rompe JD, Nafe B, Furia JP, Maffulli N. Eccentric loading, shock-wave treatment, or a wait- and-see policy for tendinopathy of the main body of tendo achillis: A randomized controlled trial. Am J Sports Med (2007) 35(3):374–83. doi: 10.1177/0363546506295940
50. Rompe JD, Furia J, Maffulli N. Eccentric loading compared with shock wave treatment for chronic insertional achilles tendinopathy: A randomized, controlled trial. J Bone Joint Surgery-American (2008) 90(1):52–61. doi: 10.2106/JBJS.F.01494
51. Rompe JD, Furia J, Maffulli N. Eccentric Loading versus Eccentric Loading plus Shock-Wave Treatment for Midportion Achilles Tendinopathy: A Randomized Controlled Trial. Am J Sports Med (2009) 37(3):463–70. doi: 10.1177/0363546508326983
52. Costa ML, Shepstone L, Donell ST, Thomas TL. Shock wave therapy for chronic achilles tendon pain: A randomized placebo-controlled trial. Clin Orthop related Res (2005) 440:199–204. doi: 10.1097/01.blo.0000180451.03425.48
53. Mansur NSB, Matsunaga FT, Carrazzone OL, Schiefer Dos Santos B, Nunes CG, Aoyama BT, et al. Shockwave therapy plus eccentric exercises versus isolated eccentric exercises for achilles insertional tendinopathy: A double-blinded randomized clinical trial. J Bone Joint Surg (2021) 103(14):1295–302. doi: 10.2106/JBJS.20.01826
54. Pinitkwamdee S, Laohajaroensombat S, Orapin J, Woratanarat P. Effectiveness of extracorporeal shockwave therapy in the treatment of chronic insertional achilles tendinopathy. Foot Ankle Int (2020) 41(4):403–10. doi: 10.1177/1071100719898461
55. Armagan Alpturker K, Cerrahoglu ABL, Orguc IS. Evaluation effects of laser therapy and extracorporeal shock wave therapy with clinical parameters and magnetic resonance imaging for treatment of plantar fasciitis in patients with spondyloarthritis: A randomized controlled trial. Int J Rheumatol (2020) 2020:1–8. doi: 10.1155/2020/4386361
56. Asheghan M, Hashemi SE, Hollisaz MT, Roumizade P, Hosseini SM, Ghanjal A. Dextrose prolotherapy versus radial extracorporeal shock wave therapy in the treatment of chronic plantar fasciitis: A randomized, controlled clinical trial. Foot Ankle Surg (2021) 27(6):643–49. doi: 10.1016/j.fas.2020.08.008
57. Bagcier F, Yilmaz N. The impact of extracorporeal shock wave therapy and dry needling combination on pain and functionality in the patients diagnosed with plantar fasciitis. J Foot Ankle Surg (2020) 59(4):689–93. doi: 10.1053/j.jfas.2019.09.038
58. Bahar-Ozdemir Y, Atan T. Effects of adjuvant low-dye kinesio taping, adjuvant sham taping, or extracorporeal shockwave therapy alone in plantar fasciitis: A randomised double-blind controlled trial. Int J Clin Pract (2021) 75(5). doi: 10.1111/ijcp.13993
59. Buchbinder R, Ptasznik R, Gordon J, Buchanan J, Prabaharan V, Forbes A. Ultrasound-guided extracorporeal shock wave therapy for plantar fasciitis: A randomized controlled trial. JAMA (2002) 288(11):1364. doi: 10.1001/jama.288.11.1364
60. Caner ÖC, Güneş S, Gökmen D, Ataman Ş, Kutlay Ş. The efficacy and safety of extracorporeal shock wave therapy on plantar fasciitis in patients with axial spondyloarthritis: A double-blind, randomized controlled trial. Rheumatol Int (2022) 42(4):581–89. doi: 10.1007/s00296-022-05098-0
61. Chew KTL, Leong D, Lin CY, Lim KK, Tan B. Comparison of autologous conditioned plasma injection, extracorporeal shockwave therapy, and conventional treatment for plantar fasciitis: A randomized trial. PM&R (2013) 5(12):1035–43. doi: 10.1016/j.pmrj.2013.08.590
62. Cinar E, Saxena S, Uygur F. Combination therapy versus exercise and orthotic support in the management of pain in plantar fasciitis: A randomized controlled trial. Foot Ankle Int (2018) 39(4):406–14. doi: 10.1177/1071100717747590
63. Cinar E, Saxena S, Akkurt HE, Uygur F. Extracorporeal shockwave therapy in the management of plantar fasciitis: A randomized controlled trial. Foot (2020) 44:101679. doi: 10.1016/j.foot.2020.101679
64. Yinilmez Sanmak ÖD. Comparison of effects of low-level laser therapy and extracorporeal shock wave therapy in plantar fasciitis treatment: A randomized, prospective, single-blind clinical study. Turkish J Phys Med Rehabil (2019) 65(2):184–90. doi: 10.5606/tftrd.2019.3528
65. Xu D, Jiang W, Huang D, Hu X, Wang Y, Li H, et al. Comparison between extracorporeal shock wave therapy and local corticosteroid injection for plantar fasciitis. Foot Ankle Int (2020) 41(2):200–5. doi: 10.1177/1071100719891111
66. Eslamian F, Shakouri SK, Jahanjoo F, Hajialiloo M, Notghi F. Extra corporeal shock wave therapy versus local corticosteroid injection in the treatment of chronic plantar fasciitis, a single blinded randomized clinical trial. Pain Med (2016) 17(9):1722–31. doi: 10.1093/pm/pnw113
67. Gerdesmeyer L, Frey C, Vester J, Maier M, Lowell W, Weil L, et al. Radial extracorporeal shock wave therapy is safe and effective in the treatment of chronic recalcitrant plantar fasciitis: results of a confirmatory randomized placebo-controlled multicenter study. Am J Sports Med (2008) 36(11):2100–9. doi: 10.1177/0363546508324176
68. Gollwitzer H, Diehl P, Korff AV, Rahlfs VW, Gerdesmeyer L. Extracorporeal shock wave therapy for chronic painful heel syndrome: A prospective, double blind, randomized trial assessing the efficacy of a new electromagnetic shock wave device. J Foot Ankle Surg (2007) 46(5):348–57. doi: 10.1053/j.jfas.2007.05.011
69. Gollwitzer H, Saxena A, DiDomenico LA, Galli L, Bouché RT, Caminear DS, et al. Clinically relevant effectiveness of focused extracorporeal shock wave therapy in the treatment of chronic plantar fasciitis: A randomized, controlled multicenter study. J Bone Joint Surgery-American (2015) 97(9):701–8. doi: 10.2106/JBJS.M.01331
70. Haake M. Extracorporeal shock wave therapy for plantar fasciitis: randomised controlled multicentre trial. BMJ (2003) 327(7406):75–0. doi: 10.1136/bmj.327.7406.75
71. Ibrahim MI, Donatelli RA, Schmitz C, Hellman MA, Buxbaum F. Chronic plantar fasciitis treated with two sessions of radial extracorporeal shock wave therapy. Foot Ankle Int (2010) 31(5):391–97. doi: 10.3113/FAI.2010.0391
72. Ibrahim MI, Donatelli RA, Hellman M, Hussein AZ, Furia JP, Schmitz C. Long-term results of radial extracorporeal shock wave treatment for chronic plantar fasciopathy: A prospective, randomized, placebo-controlled trial with two years follow-up: RADIAL ESWT FOR PLANTAR FASCIOPATHY. J Orthop Res (2017) 35(7):1532–38. doi: 10.1002/jor.23403
73. Kesikburun S, Şan AU, Kesikburun B, Aras B, Yaşar E, Tan AK. Comparison of ultrasound-guided prolotherapy versus extracorporeal shock wave therapy in the treatment of chronic plantar fasciitis: A randomized clinical trial. J Foot Ankle Surg (2022) 61(1):48–52. doi: 10.1053/j.jfas.2021.06.007
74. Kudo P, Dainty K, Clarfield M, Coughlin L, Lavoie P, Lebrun C. Randomized, placebo-controlled, double-blind clinical trial evaluating the treatment of plantar fasciitis with an extracoporeal shockwave therapy (ESWT) device: A north american confirmatory study. J Orthop Res (2006) 24(2):115–23. doi: 10.1002/jor.20008
75. Lai T-W, Li H, Lee M-S, Chen P-M, Ku M-C, Lai T-W. Ultrasonography and clinical outcome comparison of extracorporeal shock wave therapy and corticosteroid injections for chronic plantar fasciitis: A randomized controlled trial. J Musculoskeletal Neuronal Interact (2017) 18:47–54. doi: 10.1053/j.jfas.2006.04.007
76. Malay DS, Pressman MM, Assili A, Kline JT, York S, Buren B, et al. Extracorporeal shockwave therapy versus placebo for the treatment of chronic proximal plantar fasciitis: results of a randomized, placebo-controlled, double-blinded, multicenter intervention trial. J Foot Ankle Surg (2006) 45(4):196–210. doi: 10.1053/j.jfas.2006.04.007
77. Mardani-Kivi M, Mobarakeh MK, Hassanzadeh Z, Mirbolook A, Asadi K, Ettehad H, et al. Treatment outcomes of corticosteroid injection and extracorporeal shock wave therapy as two primary therapeutic methods for acute plantar fasciitis: A prospective randomized clinical trial. J Foot Ankle Surg (2015) 54(6):1047–52. doi: 10.1053/j.jfas.2015.04.026
78. Uğurlar M, Sönmez MM, Uğurlar ÖY, Adıyeke L, Yıldırım H, Eren OT. Effectiveness of four different treatment modalities in the treatment of chronic plantar fasciitis during a 36-month follow-up period: A randomized controlled trial. J Foot Ankle Surg (2018) 57(5):913–18. doi: 10.1053/j.jfas.2018.03.017
79. Ordahan B. Extracorporeal shockwave therapy versus kinesiology taping in the management of plantar fasciitis: A randomized clinical trial. Arch Rheumatol (2017) 32(3):227–33. doi: 10.5606/ArchRheumatol.2017.6059
80. Porter MD, Shadbolt B. Intralesional corticosteroid injection versus extracorporeal shock wave therapy for plantar fasciopathy. Clin J Sport Med (2005) 15(3):119–24. doi: 10.1097/01.jsm.0000164039.91787.dc
81. Rahbar M, Eslamian F, Toopchizadeh V, Jahanjoo F, Kargar A, Dolatkhah N. A comparison of the efficacy of dry-needling and extracorporeal shockwave therapy for plantar fasciitis: a randomized clinical trial. Iran Red Crescent Med J (2018) 20(9):e68908. doi: 10.5812/ircmj.68908
82. Razzano C, Carbone S, Mangone M, Iannotta MR, Battaglia A, Santilli V. Treatment of chronic plantar fasciitis with noninvasive interactive neurostimulation: A prospective randomized controlled study. J Foot Ankle Surg (2017) 56(4):768–72. doi: 10.1053/j.jfas.2017.02.015
83. Roca B, Mendoza MA, Roca M. Comparison of extracorporeal shock wave therapy with botulinum toxin type A in the treatment of plantar fasciitis. Disability Rehabil (2016) 38(21):2114–21. doi: 10.3109/09638288.2015.1114036
84. Rompe JD, Decking J, Schoellner C, Nafe B. Shock wave application for chronic plantar fasciitis in running athletes: A prospective, randomized, placebo-controlled trial. Am J Sports Med (2003) 31(2):268–75. doi: 10.1177/03635465030310021901
85. Rompe J, Meurer A, Nafe B, Hofmann A, Gerdesmeyer L. Repetitive Low-Energy Shock Wave Application without Local Anesthesia Is More Efficient than Repetitive Low-Energy Shock Wave Application with Local Anesthesia in the Treatment of Chronic Plantar Fasciitis. J Orthop Res (2005) 23(4):931–41. doi: 10.1016/j.orthres.2004.09.003
86. Rompe JD, Cacchio A, Weil L, Furia JP, Haist J, Reiners V, et al. Plantar fascia-specific stretching versus radial shock-wave therapy as initial treatment of plantar fasciopathy. J Bone Joint Surgery-American (2010) 92(15):2514–22. doi: 10.2106/JBJS.I.01651
87. Rompe JD, Furia J, Cacchio A, Schmitz C, Maffulli N. Radial shock wave treatment alone is less efficient than radial shock wave treatment combined with tissue-specific plantar fascia-stretching in patients with chronic plantar heel pain. Int J Surg (2015) 24:135–42. doi: 10.1016/j.ijsu.2015.04.082
88. Okur S, Aydın A. Comparison of extracorporeal shock wave therapy with custom foot orthotics in plantar fasciitis treatment: A prospective randomized one-year follow-up study. J Musculoskeletal Neuronal Interact (2019) 18:178–86.
89. Speed CA, Nichols D, Wies J, Humphreys H, Richards C, Burnet S, et al. Extracorporeal shock wave therapy for plantar fasciitis. A double blind randomised controlled trial. J Orthop Res (2003) 21(5):937–40. doi: 10.1016/S0736-0266(03)00048-2
90. Tezel N, Umay E, Bulut M, Cakci A. Short-term efficacy of kinesiotaping versus extracorporeal shockwave therapy for plantar fasciitis: A randomized study. Saudi J Med Med Sci (2020) 8(3):181. doi: 10.4103/sjmms.sjmms_624_19
91. Theodore GH, Buch M, Amendola A, Bachmann C, Fleming LL, Zingas C. Extracorporeal shock wave therapy for the treatment of plantar fasciitis. Foot Ankle Int (2004) 25(5):290–97. doi: 10.1177/107110070402500503
92. Timurtaş E, Çinar E, Selçuk H, Avci EE, Batar S, Demirbüken İ, et al. Extracorporeal shock wave therapy versus low level laser therapy in the treatment of plantar fasciitis: A randomized controlled trial. J Am Podiatr Med Assoc (2022), 1–27. doi: 10.7547/22-095
93. Ulusoy A, Cerrahoglu L, Orguc S. Magnetic resonance imaging and clinical outcomes of laser therapy, ultrasound therapy, and extracorporeal shock wave therapy for treatment of plantar fasciitis: A randomized controlled trial. J Foot Ankle Surg (2017) 56(4):762–67. doi: 10.1053/j.jfas.2017.02.013
94. Yucel I, Ozturan KE, Demiraran Y, Degirmenci E, Kaynak G. Comparison of high-dose extracorporeal shockwave therapy and intralesional corticosteroid injection in the treatment of plantar fasciitis. J Am Podiatr Med Assoc (2010) 100(2):105–10. doi: 10.7547/1000105
95. The International Society for Medical Shockwave Treatment. Available at: https://www.shockwavetherapy.org/fileadmin/user_upload/ISMST_Guidelines.pdf.
96. Paantjens MA, Helmhout PH, Backx FJG, Van Etten-Jamaludin FS, Bakker EWP. Extracorporeal shockwave therapy for mid-portion and insertional achilles tendinopathy: A systematic review of randomized controlled trials. Sports Med - Open (2022) 8(1):68. doi: 10.1186/s40798-022-00456-5
97. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods (2010) 1(2):97–111. doi: 10.1002/jrsm.12
Keywords: extracorporeal shockwave therapy, patellar tendinopathy, Achilles tendinopathy, tendinopathy, plantar fasciitis
Citation: Charles R, Fang L, Zhu R and Wang J (2023) The effectiveness of shockwave therapy on patellar tendinopathy, Achilles tendinopathy, and plantar fasciitis: a systematic review and meta-analysis. Front. Immunol. 14:1193835. doi: 10.3389/fimmu.2023.1193835
Received: 25 March 2023; Accepted: 28 July 2023;
Published: 16 August 2023.
Edited by:
Howe Liu, Allen College, United StatesReviewed by:
Xuan Zhang, Hong Kong Baptist University, Hong Kong SAR, ChinaJuan Li, Chengdu University of Traditional Chinese Medicine, China
Copyright © 2023 Charles, Fang, Zhu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lei Fang, ZmFuZ2xlaTU4NkAxMjYuY29t
 Ravon Charles
Ravon Charles Lei Fang
Lei Fang Ranran Zhu
Ranran Zhu Jinxiang Wang
Jinxiang Wang