
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Immunol. , 10 July 2023
Sec. Inflammation
Volume 14 - 2023 | https://doi.org/10.3389/fimmu.2023.1166265
This article is part of the Research Topic Immune Disorders in Diabetes and Microvascular Complications View all 14 articles
 Guanheng Chen
Guanheng Chen Leiguang Feng*
Leiguang Feng*Background: The etiology of benign prostatic hyperplasia (BPH) is still elusive. The aim of this study was to provide preventive and prognostic parameters associated with diabetes mellitus with benign prostatic enlargement (BPE).
Methods: Diabetic patients were collected retrospectively from February 2021 to December 2022, including monocyte-to-lymphocyte ratio (MLR). Diabetic patients were divided into two groups by whether the prostate volume was greater than or equal to 30 ml, which were diabetes mellitus without BPE (DM) and diabetes mellitus with BPE (DM+BPE). The baseline characteristics were compared, the risk and protective factors associated with DM+BPE were determined using univariate and multivariate logistic regression, and the parameters associated with prostate volume were determined using correlation analysis.
Results: Of the 671 patients collected, age and prostate volume were significantly higher in the DM+BPE than in the DM; MLR was higher in the DM+BPE than in the DM; and platelet was significantly lower in the DM+BPE than in the DM. Univariate logistic regression showed that age was a risk factor, while protective factors for DM+BPE were lymphocytes and platelet. Multifactorial logistic regression showed that age was a risk factor, while platelet was the protective factor for DM+BPE. In the total overall (n=671), prostate volume was positively correlated with age. Prostate volume was negatively correlated with lymphocytes and platelet. In DM+BPE (n=142), prostate volume was positively correlated with age and MLR.
Conclusion: Platelet was a protective factor for DM+BPE and was negatively correlated with prostate volume, whereas MLR was positively correlated with prostate volume in DM+BPE.
Globally, approximately 537 million adults have diabetes mellitus, 90% of which are type 2, and this number is expected to rise to 783 million by 2045 (1). In China, a research study from 2013 to 2018 showed that the estimated prevalence of diabetes mellitus increased from 10.9% to 12.4% and wasn’t significant improvement in treatment (2). The hyperglycemic state of diabetes mellitus promotes the production of intracellular mitochondrial reactive oxygen species, causing oxidative stress and inflammatory interactions leading to immune dysfunction (3, 4). In addition, it causes diabetes-related macrovascular and microvascular damage due to diabetic hypoxic response (5) as well as chronic hypoxic effects (6), which leads to various complications (7).
Benign prostatic hyperplasia (BPH) is a proliferative prostate gland disease in middle-aged and older men, increasing prostate volume (8). A common symptom is the development of lower urinary tract symptoms (9, 10), and acute urinary retention is a serious complication of BPH (11). It severely reduces the quality of life of middle-aged and older men (12). In recent years, although there has been a slight decline in the number of BPH patients with disability injury and healthy life years, due to the increasing number and advancing age, various urological complications resulting from the enlarged prostate gland have become a high burden worldwide (13, 14). The etiology of BPH is not well understood, but inflammation plays a significant role in it (15). In mouse experiments, five botanicals——Flavonoids, Dihydroartemisinin, Neferine, Curcumin, and Carica papaya leaf extract——have been shown to reduce prostate volume due to their anti-inflammatory properties to alleviate or treat prostate enlargement (16–20). Clinical guidelines state that choosing the appropriate surgical procedure according to the prostate size can reduce complications and is vital to improving patients’ quality of life (21–23). Although hyperglycemia has been reported to increase prostate volume (24, 25), and lymphocytes, free/total prostate-specific antigen (26), neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and lymphocyte-to-monocyte ratio have been associated with BPH (27), these did not analyze in detail or separately the relationship between prostate volume and hematological parameters. An analysis of platelet and monocyte-to-lymphocyte ratio and diabetes mellitus with benign prostatic enlargement is not reported in related article.
So far, this is the first article to analyze the relationship between prostate volume and hematological parameters in diabetic patients. Therefore, we performed this clinical study to provide clinicians with aid in judgment and to provide new ideas to study the etiology of BPH.
Diabetic patients were collected retrospectively from February 2021 to December 2022 in the Department of Endocrinology with diabetes mellitus from a query on the laboratory information system at the First Affiliated Hospital of Harbin Medical University.
The patients’ age, fasting blood glucose (FBG), glycated hemoglobin A1c (HbA1c), high-density lipoprotein (HDL), neutrophils, lymphocytes, monocytes, and platelet were recorded, and the patients’ anterior-posterior diameter, upper-lower diameter, and left-right diameter of the prostate were examined by abdominal ultrasound.
MLR= monocytes/lymphocytes (MLR), LHR = lymphocytes/high-density lipoprotein, and prostate volume (PV) = 0.52 × anterior-posterior diameter × upper-lower diameter × left-right diameter.
We set inclusion criteria and exclusion criteria. Inclusion criteria :(1) males older than or equal to 40 years of age;(2) diabetes mellitus diagnosis;(3) complete test data; and (4) no serious infectious diseases. Exclusion criteria:(1) diabetes mellitus complicated by eye disease;(2) acute complications of diabetes mellitus, such as diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome;(3) diagnosis of prostate cancer;(4) history of prostatectomy; and (5) history of hepatitis.
The collected diabetic group was divided into two groups according to whether the prostate volume was more significant than or equal to 30 ml, which were divided into the group with diabetes mellitus without benign prostatic enlargement (DM) and the group with diabetes mellitus with benign prostatic enlargement (DM+BPE).
SPSS 25.0 (SPSS, Inc., Chicago, IL, USA) was used for statistical analyses. All measures were tested for normality by the Kolmogorov-Smirnov normality test, and the mean ± standard deviation (SD) was used for data that conformed to a normal distribution. The median and quartiles IQR(Q3-Q1) was used for data that did not work to a normal distribution. If the chi-square test was satisfied between the two groups, the two independent samples t-test was used for the means of the two samples, and when data didn’t conform to normal distribution or didn’t satisfy the chi-square, the two independent samples’ Mann-Whitney U test was used for comparison between the two groups. The binary logistic regression model was established with DM+BPE assigned to 0 and DM set to 1. Univariate logistic regression was performed first, after which statistically significant ones were included in the multifactorial logistic regression to control for confounding factors.
Both variables were normally distributed using Pearson for linear correlation analysis, and didn’t meet normal distribution using Spearman for linear correlation analysis. A two-sided test was used, and P<0.05 was considered statistically significant.
A total of 671 patients were collected. In the comparison between DM and DM+BPE, age 64.00 [57.75-69.00] was significantly higher in the DM+BPE than in the DM 55.00 [48.50-61.50] (P<0.001); prostate volume 39.96 [34.31-51.62] was significantly higher in DM+BPE than in DM 20.37 [17.22 -24.13] (P<0.001); and MLR 0.24 [0.19-0.31] was higher in the DM+BPE than in the DM 0.22 [0.17-0.28] (P=0.029). Lymphocytes 1.82 [1.50-2.21] were lower in the DM+BPE than in the DM 1.97 [1.58-2.41] (P=0.011); platelet 201.63 ± 44.68 was significantly lower in the DM+BPE than in the DM 218.36 ± 52.64 (P<0.001); and LHR 1.84 [1.40-2.28] was lower in the DM+BPE was lower than in the DM 1.91 [1.45-2.57] (P=0.040). All other clinical parameters were not statistically significant (P>0.05), and the results were shown in Table 1.
A univariate logistic regression analysis of age, FBG, HbA1c, HDL, leukocytes, neutrophils, lymphocytes, monocytes, platelet, MLR, and LHR, which were parameters associated with DM+BPE, showed that the risk factor for DM+BPE was age (OR=1.113, 95% CI=1.086~1.140, P<0.001), while the protective factors for DM+BPE were lymphocytes (OR=0.657, 95% CI=0.482~0.896, P=0.008); platelet (OR=0.093, 95% CI=0.990~0.997, P=0.001); and LHR (OR=0.742, 95% CI=0.582~0.947, P=0.016). All other clinical parameters were not statistically significant (P>0.05), and the results were manifested in Table 2.
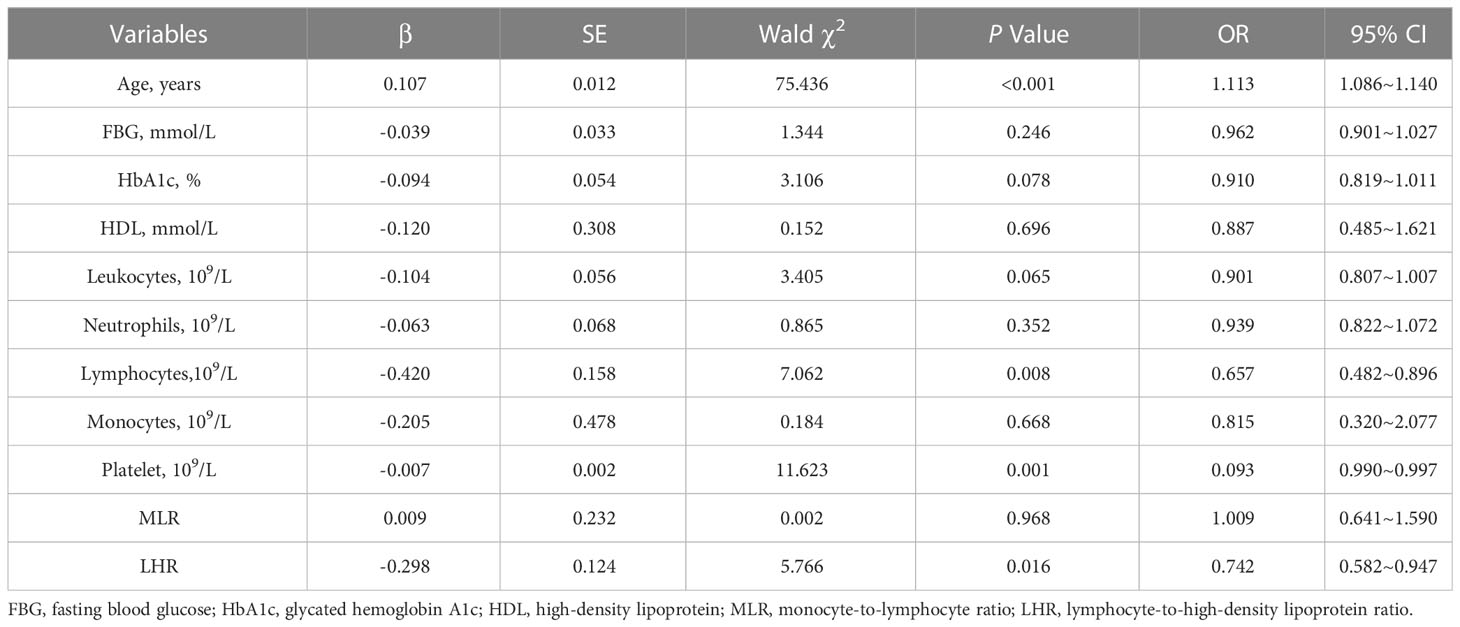
Table 2 Univariate logistic regression analysis of diabetes mellitus with and without benign prostatic enlargement.
Age, lymphocytes, platelet, and LHR were statistically significant in univariate logistic regression. Considering age as a confounding factor for BPH, we performed multifactorial logistic regression analysis for the above parameters. The results showed that the risk factor for DM+BPE was age (OR=1.109, 95% CI=1.082~1.137, P<0.001), and the protective factor for DM+BPE was platelet (OR=0.995, 95% CI=0.991~0.999, P=0.017). All other clinical parameters were not statistically significant (P>0.05), and the results were exhibited in Table 3.
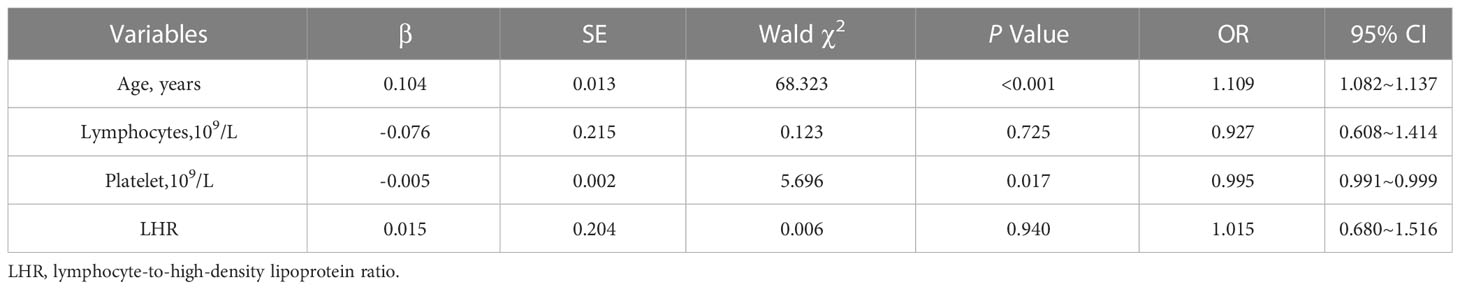
Table 3 Multifactorial logistic regression analysis of diabetes mellitus with and without benign prostatic enlargement.
In the correlation analysis, we subjected the total overall (n=671) to Spearman correlation analysis, and the positive correlation identified in this analysis was prostate volume with age (r=0.309, P<0.001). The negative correlations were prostate volume with lymphocytes (r=-0.091, P=0.018) and platelet (r=-0.098, P=0.011). In the DM+BPE (n=142) Spearman correlation analysis, the positive correlations identified in this analysis were prostate volume with age (r=0.182, P=0.030), MLR (r=0.236, P=0.005), and no other clinical parameters were statistically significant (P>0.05), as demonstrated in Table 4.
The hyperglycemic state of diabetes mellitus may affect BPH (28). The systemic chronic low-grade inflammation of diabetes mellitus promotes the development of prostatic enlargement (29). The inflammation increases the size of the prostate (30), which leads to bladder outlet obstruction (31). It severely reduces sleep quality in middle-aged and older men (32) and sometimes causes depression (33). Lower urinary tract symptoms are caused by prostatic enlargement blocking the bladder outlet (34). If not properly managed, it causes the development of urinary tract infections (35, 36). Increasing age is one of the risk factors for BPH (37). The increase in prostate volume with increasing age in our present analysis is consistent with previous reports in the literature (38). This confounding factor must be controlled for in our current study.
Lymphocytes have a scavenging effect on foreign antigens, and the LHR reflects the body’s inflammatory status. Increased HDL is negatively associated with the risk of developing BPH (39). Lipid-lowering drugs have a therapeutic effect on BPH (40). Thus, in this study, lymphocytes and LHR levels were reduced in Table 1 but not statistically significant in the analysis of Tables 2, 3, probably because age was among the confounding factors. Platelet and MLR parameters have been shown to have a prognostic role in idiopathic pulmonary fibrosis (41), acute ischemic stroke (42), and immunoglobulin A nephropathy (43). However, there need to be more reports on DM+BPE. In our study, platelet was a protective factor for BPE, and prostate volume was negatively correlated with platelet counts. Some substances secreted by platelet may have an imbalance that positively regulates cell proliferation in the prostate. Although MLR wasn’t statistically significant in Tables 2, 3, in Tables 1, 4, there was a positive correlation between prostate volume and MLR in DM+BPE, probably due to an inflammatory response caused by monocyte infiltration leading to an increase in prostate volume (44, 45).
Our study has some advantages: On the one hand, this study provides valuable parameters for prevention, treatment, and determination of prognosis valid for patients with DM+BPE. On the other hand, because platelet and MLR are readily available in the physical blood test, they have a relatively low price and are more suitable for widespread use. However, some shortcomings must be addressed: Firstly, because this was a retrospective study, data were collected without specimens corresponding to all patients, lacking the indicator of prostate-specific antigen, which is associated with prostate volume (46, 47). An increased prostate-specific antigen concentration is a risk for enlarged prostate volume (48). Secondly, this single-center clinical study may influence ethnicity, geography, and social and economic conditions. Finally, this study could not prove causality because it was retrospective. Therefore, prostate-specific antigen parameters should be increased in the future, and prospective and multicenter studies should be conducted to provide evidence-based surgical treatment for patients with BPH.
Platelet was a protective factor for DM+BPE and was negatively correlated with prostate volume in the overall patient analysis. In DM+BPE, MLR was positively correlated with prostate volume.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Ethics Committee of the First Affiliated Hospital of Harbin Medical University (202247). The patients/participants provided their written informed consent to participate in this study.
GC Data acquisition, Data analysis, and Writing. LF Funding acquisition, Conceptualization, and Supervision. Both authors contributed to the article and approved the submitted version.
This study was supported by the National Key Research and Development Program of China (ProjectNo.2021YFC2009300 and 2021YFC2009306).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ahmad E, Lim S, Lamptey R, Webb DR, Davies MJ. Type 2 diabetes. Lancet (2022) 400(10365):1803–20. doi: 10.1016/s0140-6736(22)01655-5
2. Wang L, Peng W, Zhao Z, Zhang M, Shi Z, Song Z, et al. Prevalence and treatment of diabetes in China, 2013-2018. JAMA (2021) 326(24):2498–506. doi: 10.1001/jama.2021.22208
3. Fajgenbaum DC, June CH. Cytokine storm. N Engl J Med (2020) 383(23):2255–73. doi: 10.1056/NEJMra2026131
4. Hotamisligil GS. Inflammation, metaflammation and immunometabolic disorders. Nature (2017) 542(7640):177–85. doi: 10.1038/nature21363
5. Sousa Fialho MDL, Purnama U, Dennis K, Montes Aparicio CN, Castro-Guarda M, Massourides E, et al. Activation of Hif1alpha rescues the hypoxic response and reverses metabolic dysfunction in the diabetic heart. Diabetes (2021) 70(11):2518–31. doi: 10.2337/db21-0398
6. West JB. Physiological effects of chronic hypoxia. N Engl J Med (2017) 376(20):1965–71. doi: 10.1056/NEJMra1612008
7. Catrina SB, Zheng X. Hypoxia and hypoxia-inducible factors in diabetes and its complications. Diabetologia (2021) 64(4):709–16. doi: 10.1007/s00125-021-05380-z
8. Devlin CM, Simms MS, Maitland NJ. Benign prostatic hyperplasia - what do we know? BJU Int (2021) 127(4):389–99. doi: 10.1111/bju.15229
9. Xiong Y, Zhang Y, Li X, Qin F, Yuan J. The prevalence and associated factors of lower urinary tract symptoms suggestive of benign prostatic hyperplasia in aging males. Aging Male (2020) 23(5):1432–39. doi: 10.1080/13685538.2020.1781806
10. Sarma AV, Wei JT. Clinical practice. benign prostatic hyperplasia and lower urinary tract symptoms. N Engl J Med (2012) 367(3):248–57. doi: 10.1056/NEJMcp1106637
11. Bengtsen MB, Heide-Jorgensen U, Borre M, Knudsen JS, Norgaard M. Acute urinary retention in men: 21-year trends in incidence, subsequent benign prostatic hyperplasia-related treatment and mortality: a Danish population-based cohort study. Prostate (2022) 83(1):87–96. doi: 10.1002/pros.24440
12. Huang J, Chan CK, Yee S, Deng Y, Bai Y, Chan SC, et al. Global burden and temporal trends of lower urinary tract symptoms: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis (2022) 26(2):421–28. doi: 10.1038/s41391-022-00610-w
13. Zeng Z, Zhan J, Zhang K, Chen H, Cheng S. Global, regional, and national burden of urinary tract infections from 1990 to 2019: an analysis of the global burden of disease study 2019. World J Urol (2022) 40(3):755–63. doi: 10.1007/s00345-021-03913-0
14. Xu XF, Liu GX, Guo YS, Zhu HY, He DL, Qiao XM, et al. Global, regional, and national incidence and year lived with disability for benign prostatic hyperplasia from 1990 to 2019. Am J men’s Health (2021) 15(4):15579883211036786. doi: 10.1177/15579883211036786
15. Zhang J, Zhang M, Tang J, Yin G, Long Z, He L, et al. Animal models of benign prostatic hyperplasia. Prostate Cancer Prostatic Dis (2021) 24(1):49–57. doi: 10.1038/s41391-020-00277-1
16. Cao X, Shang Y, Kong W, Jiang S, Liao J, Dai R. Flavonoids derived from anemarrhenae rhizoma ameliorate inflammation of benign prostatic hyperplasia Via modulating Cox/Lox pathways. J Ethnopharmacol (2022) 284:114740. doi: 10.1016/j.jep.2021.114740
17. Zhang B, Chen X, Gan Y, Li BS, Wang KN, He Y. Dihydroartemisinin attenuates benign prostatic hyperplasia in rats by inhibiting prostatic epithelial cell proliferation. Ann Transl Med (2021) 9(15):1246. doi: 10.21037/atm-21-3296
18. Jahan N, Chowdhury A, Li T, Xu K, Wei F, Wang S. Neferine improves oxidative stress and apoptosis in benign prostate hyperplasia Via Nrf2-are pathway. Redox report: Commun Free Radical Res (2021) 26(1):1–9. doi: 10.1080/13510002.2021.1871814
19. Liu Y, Wang Z, Gan Y, Chen X, Zhang B, Chen Z, et al. Curcumin attenuates prostatic hyperplasia caused by inflammation Via up-regulation of bone morphogenetic protein and activin membrane-bound inhibitor. Pharm Biol (2021) 59(1):1026–35. doi: 10.1080/13880209.2021.1953539
20. Jin BR, Ju JY, Nugroho A, Lee M, An HJ. Carica papaya leaf extract inhibits prostatitis-associated prostatic hyperplasia Via the Traf6/Tak1/Mek/Nf-kappab pathway. BioMed Pharmacother (2021) 135:111197. doi: 10.1016/j.biopha.2020.111197
21. Tian Y, Liu HM, Yang B, Yang XS, Sun ZL, Sun F, et al. Prostatic anatomical parameters correlate with clinical characteristics suggestive of benign prostatic hyperplasia. Asian J androl (2021) 23(1):64–8. doi: 10.4103/aja.aja_47_20
22. Foster HE, Dahm P, Kohler TS, Lerner LB, Parsons JK, Wilt TJ, et al. Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: aua guideline amendment 2019. J Urol (2019) 202(3):592–98. doi: 10.1097/JU.0000000000000319
23. Lerner LB, McVary KT, Barry MJ, Bixler BR, Dahm P, Das AK, et al. Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: aua guideline part ii-surgical evaluation and treatment. J Urol (2021) 206(4):818–26. doi: 10.1097/JU.0000000000002184
24. Zhao MJ, Huang Q, Wang XH, Ren XY, Jin YH, Zeng XT. Comparing clinical parameters of abnormal and normal fasting blood glucose in benign prostatic hyperplasia patients. Aging Male (2020) 23(5):655–62. doi: 10.1080/13685538.2019.1570493
25. Wu Y, Ding Y, Cao QF, Qian SB, Wang C, Duan HQ, et al. The relationship between glucose homeostasis status and prostate size in aging Chinese males with benign prostatic hyperplasia. World J Urol (2020) 38(11):2923–31. doi: 10.1007/s00345-020-03084-4
26. Zhang H, Lu L, Wan S, Wang Z. Relationship among lymphocytes, Free/Total prostate specific antigen, lower urinary tract symptoms and prostatic inflammation in benign prostatic hyperplasia patients. Asian J Surg (2021) 44(6):921–22. doi: 10.1016/j.asjsur.2021.04.006
27. Kang JY, Choi JD, Cho JM, Yoo TK, Park YW, Lee JH. Association of neutrophil-to-Lymphocyte ratio, platelet-to-Lymphocyte ratio, and lymphocyte-to-Monocyte ratio with benign prostatic hyperplasia: a propensity score-matched analysis. Urologia internationalis (2021) 105(9-10):811–16. doi: 10.1159/000512894
28. Berger AP, Deibl M, Halpern EJ, Lechleitner M, Bektic J, Horninger W, et al. Vascular damage induced by type 2 diabetes mellitus as a risk factor for benign prostatic hyperplasia. Diabetologia (2005) 48(4):784–9. doi: 10.1007/s00125-005-1678-6
29. Gandaglia G, Briganti A, Gontero P, Mondaini N, Novara G, Salonia A, et al. The role of chronic prostatic inflammation in the pathogenesis and progression of benign prostatic hyperplasia (Bph). BJU Int (2013) 112(4):432–41. doi: 10.1111/bju.12118
30. Sreenivasulu K, Nandeesha H, Dorairajan LN, Nachiappa Ganesh R. Over expression of Pi3k-akt reduces apoptosis and increases prostate size in benign prostatic hyperplasia. Aging Male (2020) 23(5):440–46. doi: 10.1080/13685538.2018.1519014
31. Pandolfo SD, Del Giudice F, Chung BI, Manfredi C, De Sio M, Damiano R, et al. Robotic assisted simple prostatectomy versus other treatment modalities for Large benign prostatic hyperplasia: a systematic review and meta-analysis of over 6500 cases. Prostate Cancer Prostatic Dis (2022). doi: 10.1038/s41391-022-00616-4
32. Xiong Y, Zhang Y, Zhang F, Wu C, Qin F, Yuan J. Reduced sleep duration increases the risk of lower urinary tract symptoms suggestive of benign prostatic hyperplasia in middle-aged and elderly males: a national cross-sectional study. Aging Male (2022) 25(1):159–66. doi: 10.1080/13685538.2022.2079627
33. Vartolomei L, Cotrus A, Tataru SO, Vartolomei MD, Man A, Ferro M, et al. Lower urinary tract symptoms are associated with clinically relevant depression, anxiety, and stress symptoms. Aging Male (2022) 25(1):62–6. doi: 10.1080/13685538.2022.2040981
34. Homma Y, Gotoh M, Kawauchi A, Kojima Y, Masumori N, Nagai A, et al. Clinical guidelines for Male lower urinary tract symptoms and benign prostatic hyperplasia. Int J Urol (2017) 24(10):716–29. doi: 10.1111/iju.13401
35. Choi JB, Min SK. Complicated urinary tract infection in patients with benign prostatic hyperplasia. J infection chemother (2021) 27(9):1284–87. doi: 10.1016/j.jiac.2021.06.006
36. Cao Q, Wu Y, Guan W, Zhu Y, Qi J, Xu D. Diagnosis of chronic prostatitis by noninvasive methods in elderly patients with benign prostatic hyperplasia in China. Andrologia (2021) 53(6):e14055. doi: 10.1111/and.14055
37. Qian S, Sheng X, Xu D, Shen H, Qi J, Wu Y. Variation of prostatic morphology in Chinese benign prostatic hyperplasia patients of different age decades. Aging Male (2020) 23(5):457–63. doi: 10.1080/13685538.2018.1522626
38. Fiard G, Stavrinides V, Chambers ES, Heavey S, Freeman A, Ball R, et al. Cellular senescence as a possible link between prostate diseases of the ageing Male. Nat Rev Urol (2021) 18(10):597–610. doi: 10.1038/s41585-021-00496-8
39. Yoo S, Oh S, Suh J, Park J, Cho MC, Jeong H, et al. Optimal high-density lipoprotein cholesterol level for decreasing benign prostatic hyperplasia in men not taking statin medication: a historical cohort study. Prostate (2020) 80(7):570–76. doi: 10.1002/pros.23970
40. Cakir SS, Ozcan L, Polat EC, Besiroglu H, Kocaaslan R, Otunctemur A, et al. Statins are effective in the treatment of benign prostatic hyperplasia with metabolic syndrome. Aging Male (2020) 23(5):538–43. doi: 10.1080/13685538.2018.1541979
41. Chen Y, Cai J, Zhang M, Yan X. Prognostic role of nlr, plr and mhr in patients with idiopathic pulmonary fibrosis. Front Immunol (2022) 13:882217. doi: 10.3389/fimmu.2022.882217
42. Sun YY, Wang MQ, Wang Y, Sun X, Qu Y, Zhu HJ, et al. Platelet-to-Lymphocyte ratio at 24h after thrombolysis is a prognostic marker in acute ischemic stroke patients. Front Immunol (2022) 13:1000626. doi: 10.3389/fimmu.2022.1000626
43. Tan J, Song G, Wang S, Dong L, Liu X, Jiang Z, et al. Platelet-to-Albumin ratio: a novel iga nephropathy prognosis predictor. Front Immunol (2022) 13:842362. doi: 10.3389/fimmu.2022.842362
44. Roumeguere T, Van Antwerpen P, Vanhamme L, Delporte C, Rousseau A, Wespes E, et al. Myeloperoxidase and prostate volume: a preliminary study. Prog Urol (2018) 28(10):482–87. doi: 10.1016/j.purol.2018.06.004
45. Lloyd GL, Marks JM, Ricke WA. Benign prostatic hyperplasia and lower urinary tract symptoms: what is the role and significance of inflammation? Curr Urol Rep (2019) 20(9):54. doi: 10.1007/s11934-019-0917-1
46. Avci S, Onen E, Caglayan V, Kilic M, Sambel M, Oner S. Free prostate-specific antigen outperforms total prostate-specific antigen as a predictor of prostate volume in patients without prostate cancer. Archivio italiano di urologia andrologia: organo ufficiale [di] Societa italiana di ecografia urologica e nefrologica (2020) 92(1):1–6. doi: 10.4081/aiua.2020.1.1
47. Jia L, Strand DW, Goueli RS, Gahan JC, Roehrborn CG, Mauck RJ. Psa density is associated with bph cellular composition. Prostate (2022) 82(12):1162–69. doi: 10.1002/pros.24367
48. Kusuma Duarsa GW, Sari YA, Gde Oka AA, Santosa KB, Yudiana IW, Wisnu Tirtayasa PM, et al. Serum testosterone and prostate-specific antigen levels are major risk factors for prostatic volume increase among benign prostatic hyperplasia patients. Asian J Urol (2021) 8(3):289–97. doi: 10.1016/j.ajur.2020.06.001
Keywords: diabetes mellitus, benign prostatic enlargement, benign prostatic hyperplasia, platelet, monocyte-to-lymphocyte ratio, inflammation
Citation: Chen G and Feng L (2023) Analysis of platelet and monocyte-to-lymphocyte ratio and diabetes mellitus with benign prostatic enlargement. Front. Immunol. 14:1166265. doi: 10.3389/fimmu.2023.1166265
Received: 15 February 2023; Accepted: 26 June 2023;
Published: 10 July 2023.
Edited by:
Yuanzeng Min, University of Science and Technology of China, ChinaReviewed by:
Aixia Sun, Michigan State University, United StatesCopyright © 2023 Chen and Feng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Leiguang Feng, bGVpZ3VhbmdmZW5nQDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.