
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Immunol. , 02 March 2023
Sec. Mucosal Immunity
Volume 14 - 2023 | https://doi.org/10.3389/fimmu.2023.1125102
This article is part of the Research Topic Expert Opinions in Mucosal Vaccines View all 4 articles
 Richard I. Walker*
Richard I. Walker* A. Louis Bourgeois
A. Louis BourgeoisOral immunization is an effective strategy for inducing protective immunity against mucosal enteric pathogens. Although live-attenuated as well as subunit approaches have been explored for vaccination against enteric pathogens, inactivated whole bacterial cells may also be effective in introducing protective immunity. Successfully accomplishing this goal with inactivated whole bacterial cells will require that a complex antigenic repertoire be presented in controlled immunogenic amounts, in a safe and relatively simple and self-contained delivery format. The benefit from immunization with whole cell vaccines can be further enhanced through genetic engineering to over-express selected antigens and also by the use of mucosal adjuvants to direct a more robust immunologic response. These steps are being taken for the development of ETVAX, the most clinically advanced vaccine candidate against the major enteric pathogen, enterotoxigenic Escherichia coli (ETEC) with significant positive impact.
Enterotoxigenic Escherichia coli (ETEC) remains among the most common bacterial causes of diarrhea-associated morbidity and mortality and is often the first bacterial illness that children experience in endemic areas (1, 2). It is an enterotoxic non-invasive disease in which bacteria must first colonize the small intestine where they employ plasmid-encoded fimbrial colonization factors (CFs) or coli surface antigens (CS) to bind enterocytes in the upper small intestine (1, 2). Here they produce heat-stable (ST) and/or heat-labile (LT) enterotoxins, and their close association with enterocytes via their CF/CS antigens promotes transfer of ETEC enterotoxins that stimulate the release of fluid from the intestinal epithelium, resulting in watery diarrheal illness (1, 2). Even asymptomatic intestinal colonization with ETEC strains can lead to local and systemic inflammation that further highlights ETEC as a contributor to the pathogenic pathway leading to stunting EDD and poor cognitive development (1, 2).
There are no licensed vaccines for ETEC. However, field studies and human challenge studies indicate that protective immunity to ETEC develops after natural or experimental infection (1, 2). In addition, in ETEC-endemic areas, age-specific attack rates for symptomatic ETEC infection decline after three years of age (1, 2). ETEC vaccine development efforts have focused on the induction of anti-toxin and anti-colonization immunity, including using whole cell inactivated or live attenuated, purified antigens, subunit and peptide approaches (1, 2). Specifically, studies in animals and human subjects indicate that LT and CF/CS antigens contribute to protection against ETEC and have potential for use in a vaccine. The currently most advanced vaccine candidate for ETEC, ETVAX, employs these antigens (1, 2).
The development of ETVAX may provide a valuable roadmap for development of other improved inactivated whole cell enteric vaccines (1, 2), and I. Khalil, personal communication. A first-generation precursor of the current ETVAX candidate was a whole cell vaccine consisting of formalin-inactivated ETEC bacteria expressing CFA/I and CS1 to CS5, combined with cholera toxin B-subunit (CTB), which is highly homologous to the B-subunit (LTB) of LT enterotoxin produced by approximately 66% of ETEC strains (3). This 2-dose vaccine candidate was found to be immunogenic in children and adults in endemic areas. Furthermore, it protected adult travelers against moderate/severe diarrhea (4–6). In these studies, an anti-CTB serum IgA titer > 360 when trial participants arrived in Guatemala or Mexico was found to be associated with a reduced risk of developing moderate to severe ETEC traveler’s diarrhea (TD) (Table 1), suggesting that level of anti-toxoid IgA antibody may be a marker for effective vaccination in travelers. In pediatric studies, a full dose of the vaccine caused vomiting in 6–17 months old Bangladeshi children; but a quarter dose was found to be safe (7). The vaccine did not confer protection in 6–24 months old Egyptian children, but both vaccinated and unvaccinated children experienced mainly mild disease during the study period and the impact on moderate/severe diarrhea could not be evaluated (8). These data were reviewed by a WHO panel, which recommended overexpression of antigens on the cells comprising the vaccine and inclusion of an adjuvant in the formulation (9) to help improve vaccine immunogenicity in the target age-group.
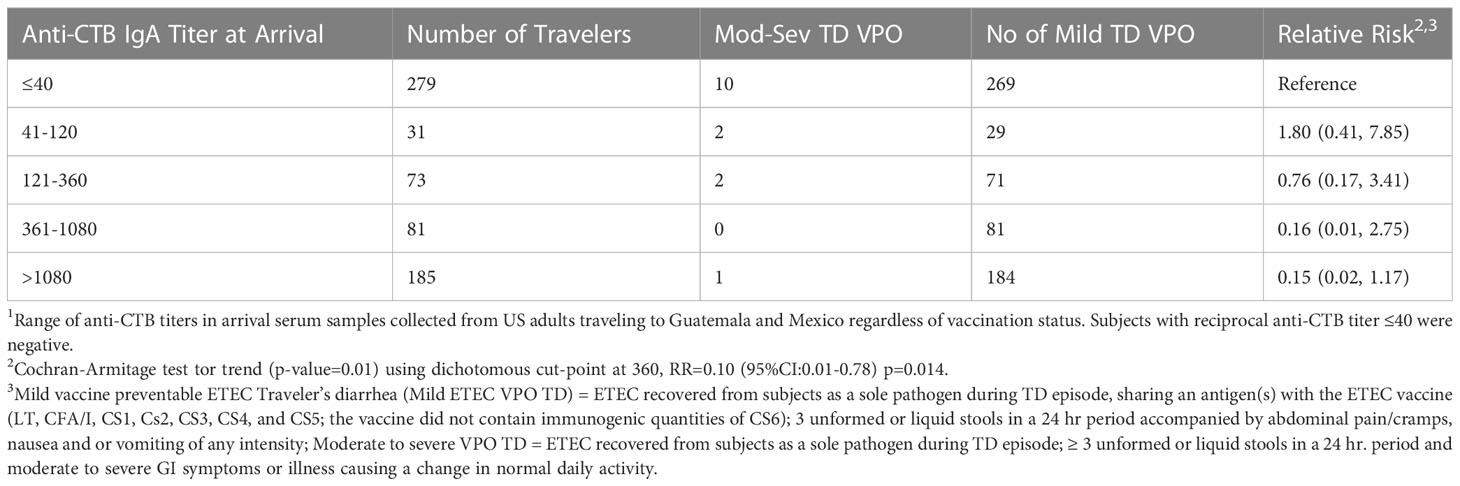
Table 1 Anti-CTB serum IgA serum IgA titer1 in U.S. travelers upon arrival in Guatemala or Mexico and the risk of developing moderate to severe ETEC traveler’s diarrhea.
ETVAX is now undergoing clinical trials as a second generation multivalent oral ETEC vaccine-containing inactivated E. coli strains over-expressing colonization factor antigens CFA/I, CS3, CS5 and CS6 (the latter was not included in the first-generation vaccine) at significantly higher levels than in naturally occurring cells (10). In addition, it was also noted that formalin inactivation of the CS6 expressing ETEC was detrimental to CS6 immunogenicity, and this was overcome in the second-generation formulation by phenol inactivation of the CS6 strain (10). The current generation vaccine is administered together with the more LT-like toxoid LCTBA (11–13). To further enhance the immunogenicity of the vaccine, it was combined with the double mutant labile toxin of ETEC (dmLT) adjuvant (10, 14, 15). When tested in Swedish adults (ISRCTN91363076), ETVAX with or without dmLT was found to be safe and to induce significant fecal SIgA responses as well as IgA antibody-secreting cell (ASC) responses against all CFs and LTB (12). Addition of 10 ug dmLT to the vaccine significantly enhanced ALS responses only to the CS6 component (12). ETVAX also induced long-lasting immunological memory in Swedish adults (16; ISRCTN27096290). Subsequent results demonstrated that ETVAX induced IgA antibody responses that cross-react with CFs belonging to the same CF families, possibly expanding the coverage of the vaccine (17). These successful results have led to clinical evaluation of ETVAX in a large phase 1/2 trial in adults and lower age groups (5 years to 6 months) in Bangladesh.
Adults: The safety of ETVAX alone or together with dmLT adjuvant was evaluated in Bangladeshi adults to provide the basis for studies in Bangladeshi children and infants [(3); NCT02531802]. The Bangladeshi adults received two oral doses of ETVAX with or with-out dmLT adjuvant or placebo in the initial part of a randomized, double-blind, placebo-controlled, age-descending, dose-escalation trial. This was the first clinical trial of the second generation ETVAX vaccine conducted in an ETEC endemic country. Two full doses of ETVAX, both when administered alone and with 10 ug dmLT adjuvant, were safe and well tolerated in the healthy Bangladeshi adults tested, confirming previous safety data from studies in Swedish adults (11, 12, 16). This vaccine was highly immunogenic in Bangladeshi adults, inducing intestine-derived ASC responses in all, and plasma antibody responses in a majority, of the vaccine recipients to all primary vaccine antigens (four CFs and LTB). Addition of dmLT adjuvant to the vaccine had no apparent effect on the ALS responses in the adults in this study. In contrast, in adult Swedes, 10 ug of dmLT significantly enhanced ASC responses to CS6, which is the CF present in the lowest amount in the vaccine (12).
Both the Swedish and Bangladeshi trials demonstrated that the oral ETVAX vaccine is safe in adults and induces strong mucosal as well as systemic immune responses against key vaccine antigens. These findings have provided a base for further evaluation of this vaccine in descending age groups in children and infants.
Children and infants: Healthy children in one of three age groups (24–59 months, 12–23 months, and 6–11 months) were randomly assigned with block randomization to receive either ETVAX, with or without dmLT, or placebo (18; NCT02531802). ETVAX (half [5.5 × 1010 cells, 500 ug LCTBA], quarter [2.5 × 1010 cells, 250 ug LCTBA], or eighth [1.25 × 1010 cells, 125 ug LCTBA] adult dose), with or without dmLT adjuvant (2.5 μg, 5.0 μg, or 10.0 μg), or placebo were administered orally in two doses 2 weeks apart. The primary endpoint was safety and tolerability, assessed in all children who received at least one dose of vaccine. Antibody responses to vaccine antigens, defined as at least a two-times increase in antibody levels between baseline and post-immunization, were assessed as secondary endpoints.
No solicited adverse events occurred that were greater than moderate in severity, and most were mild. The most common solicited event was vomiting which appeared related to dose and age. The addition of dmLT did not modify the safety profile. Mucosal IgA antibody responses in lymphocyte secretions were detected against all primary vaccine antigens (CFA/I, CS3, CS5, CS6, and the LCTBA toxoid) in most participants in the two older age groups, whereas such responses to four of the five antigens were less frequent and of lower magnitude in infants aged 6–11 months than in older children.
Mucosal antibody response frequencies were consistently higher in the adjuvanted vaccine group when ≥ 3, 4 or 5 antigens were considered (Table 2). Seventy-eight (56%) of 139 infants aged 6–11 months who were vaccinated developed mucosal responses against at least three of the vaccine antigens versus 14 (29%) of 49 of the infants given placebo. Addition of the adjuvant dmLT enhanced the magnitude, breadth, and kinetics (based on number of responders after the first dose of vaccine) of immune responses in infants (19). A similar positive dmLT effect was observed on the mucosal antibody response in the 12-23 month age group in this study when the antigenic breath of the responses was considered. In more in-depth immunological studies, the inclusion of dmLT in the vaccine formulation improved expression of B cell memory markers and T cell responses to key ETEC antigens as well (19–21). Subsequent findings showed that ETVAX induced mucosal and systemic immune responses against O78 LPS (present in three of the CS expressing strains in the vaccine) in all age groups and that dmLT improved intestinal immune responses among infants (19, 22). These observations may have implications for more successful use of dmLT with other oral vaccines, like cholera (OCV), which have experienced difficulty in inducing protective O antigen antibody responses in children and infants under 5 years of age (23). Also, the enhancement of protein colonization factors and 078 LPS responses in infants and young children suggests in the case of OCV that including dmLT in the formulation may make single dose vaccine strategies more protective, thereby extending available stockpiles of this vaccine (24).
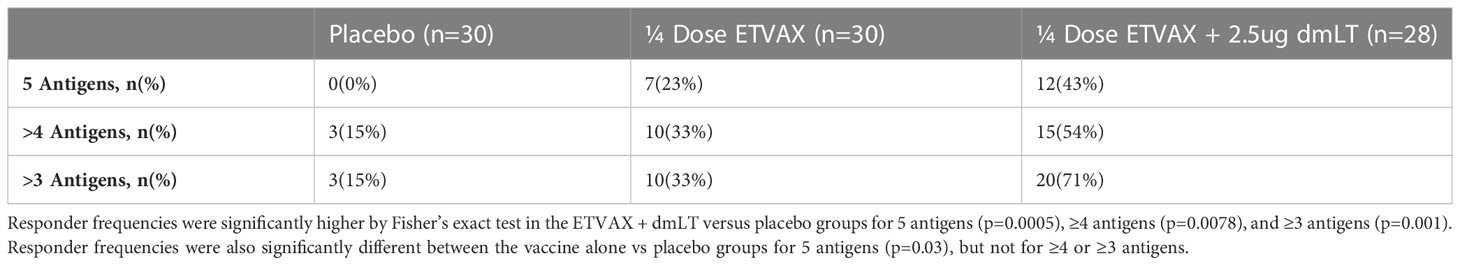
Table 2 Cumulative frequencies of 6-11 months old children given a 1/4 dose of vaccine alone or with 2.5 µg of dmLT with ≥2 fold fecal and/or ALS IgA responders against different numbers of key ETVAX vaccine antigens.
The Swedish and Bangladeshi studies showed that ETVAX could induce strong intestine-derived and/or fecal immune responses in a majority of vaccinated adults and in different age groups, including infants, in Bangladesh (21). This trial assessed for the first time the safety and immunogenicity of ETVAX in young children and infants in a low and middle income country (LMIC) and was the first analysis of dmLT adjuvant with a vaccine in this population in a LMIC. Immune responses were improved in infants aged 6–11 months by administering dmLT with the vaccine. Importantly, this study showed that occasional mild to moderate vomiting can be reduced without loss of immunogenicity by reducing the dose of vaccine, even when dmLT was included in the formulation.
A double-blind, placebo-controlled, age-descending, dose-finding trial was undertaken in 40 adults, 60 children aged 10-23 months and 146 aged 6-9 months old (25; PACTR201905764389804). Adults received a single full dose of ETVAX and children received 3 doses of either 1/4 or 1/8 of the vaccine. All vaccine doses also included 2.5 ug of dmLT. There were no differences in the frequency of solicited or unsolicited adverse events between vaccine recipients receiving 1/4 and 1/8 dose and no increase in frequency or severity of systemic reactogenicity with increasing number of vaccinations or decreasing age. The vaccine induced plasma IgA and IgG responses against LTB in 100% of the adults and 80-90% of the children. In children aged 6-9 months, IgA response rates against ≥ 4 vaccine antigens after 3 doses determined as ≥ 2-fold and ≥ 4-fold rises were significantly higher for 1/4 dose compared to placebo (65.1% vs 27.6%, p=0.004 and 32.6% vs 6.9%, p=0.01, respectively).
The Zambian studies further demonstrated that ETVAX was safe, tolerable, and immunogenic in adults and children. Using 3 doses, the maximum expected number of doses to be used in children in LMICs, the 1/4 dose was again shown to be safe and induced significant IgA responses in children.
Evaluation of pre-and post-vaccination plasma samples from 20 children aged 10-23 months was accomplished using a proteome microarray (26). Post-vaccination, reactivity to CFA/1, CS3, CS6, and LTB was stronger than baseline among the vaccinated compared to the placebo group. The CS5 protein was not included in the microarray. Three other purified non-vaccine ETEC proteins; CS4, CS14, and PCF071 had significantly higher post-vaccination responses. These data suggest that ETVAX induces cross-reactive IgG antibody responses to non-vaccine CFs CS4, CS14, and PCF071 from the class 5 fimbriae. This activity could provide some broad IgG antibody coverage beyond the core vaccine antigens (CFA/I, CS3,CS5, CS6 and LTB) themselves.
Field evidence that effective immunization with ETVAX can be protective in man.
A randomized, double-blinded, placebo-controlled phase 2b trial of ETVAX supplemented with 10 ug of dmLT was conducted among 729 Finnish volunteers (18-65 years old) randomized to receive two doses of either ETVAX or placebo two weeks apart (27; EudraCT2016-002690-35; NCT03729219). Although the data for this trial are being prepared for initial publication elsewhere, it can be said that the safety, immunogenicity and efficacy data are encouraging for moving on to Phase 3 planning for travelers and further studies among infants and young children in low to low-middle income countries (LMICs) that will lead to Phase 3 testing for both indications. The Benin Phase 2B study was a critical step in the development of the ETVAX vaccine since it was a very stringent test of its impact on ETEC TD since the burden of co-pathogens in the field proved exceptionally high and ETEC was found in 75% of all severe diarrhea cases. These data for protection are consistent with those reported for the first generation inactivated ETEC vaccine (4–6).
As described above, ETVAX has been shown to be safe and induce strong intestinal-mucosal IgA antibody responses to CF antigens and LTB when tested among adult Swedish volunteers, healthy Bangladeshi adults and children, and in healthy Zambian children. An ongoing trial in The Gambia is a randomized, double-blind, placebo controlled (1:1) trial to measure the safety, immunogenicity, and protective efficacy of three ETVAX doses given as 1/4 of an adult dose plus 2.5 ug of dmLT. Vaccine is given on days 1, 15, and 90 to healthy Gambian children aged 6 to 18 months (28; PACTR20201081021852). As of 17 November 2022, 4936 children have been enrolled and received at least one vaccine dose and 88% of these children received all three doses. Although safety data is blinded to group assignment, the investigational product appears safe. Active surveillance using home visits for solicited adverse events (i.e., diarrhea, vomiting, fever, acute allergic reactions) within seven days of any vaccine or placebo dose in a cohort of 350 children detected 89 events, only two events (1 vomiting, 1 fever) were severe and considered product related. Among all other children (n = 4115), there were 348 adverse events during dosing; three were severe (1 pneumonia, 1 measles, 1 bronchiolitis) and none were product related. For 32 serious adverse events, none were found product related. To 31 October 2022, 360 moderate to severe diarrhea cases have been detected and 94 (26%) were ETEC positive by multiplex PCR. Stool specimens are under testing for ETEC phenotypes and co-pathogens.
To date the only licensed inactivated whole cell vaccines against enteric diseases are against cholera, and most depend upon delivery of acid-resistant polysaccharide antigens. The presentation for these vaccines not requiring a buffer involves a cell suspension in a plastic tube that can be dispensed directly into the recipient’s mouth. A more complex presentation may be necessary to exploit the potential of whole cell vaccines containing adjuvants and conserved protein antigens. This need has been studied extensively with ETVAX so that the number of vaccine components and their presentation for administration can be simplified (N. Carlin, personal communication). The presentations now being considered for traveler and LMIC pediatric use of ETVAX will consist of a spray dried sachet (dmLT [10 ug] + antacid buffer + LCTBA) and a liquid bottle of 10 ml of bacterial cells For adults the sachet may be reconstituted in the bacterial suspension of cells in a glass containing 150 ml of water prior to consumption. For children in LMICs, the sachet contents are anticipated to be mixed directly with the bacterial suspension for administration. The two-component, self-contained formulation is a significant advance. The need for no extraneous water overcomes a delivery issue that has been problematic for widespread use of some oral inactivated whole cell vaccines (i.e.Dukorall). At this point, ETVAX has a practical formulation designed to minimize user error. Future work may be able to further reduce the footprint of this vaccine for refrigeration.
Although ETVAX promises to be an effective vaccine with broad protection against ETEC, the value proposition for this vaccine could be greatly increased by using it as a platform to immunize against other pathogens (2); I. Khalil, personal communication). For example, recombinant protective antigens against other mucosal pathogens could be cloned into one or more of the strains now comprising ETVAX. Alternatively, other whole cell vaccines alone or themselves expressing heterologous antigens could be co-formulated with ETVAX. These could include the cross-protective inactivated Shigella whole cell vaccine (29) or the Hikojima (30) or Euvichol (31) cholera vaccines. An advantage of a practical means of oral vaccine delivery compared to parenteral injections is that the other whole cell vaccines would not need to be mixed before administration to be acceptable. Instead, after administering the ETVAX with buffer and adjuvant, a second simpler plastic vial containing just the additional whole cell antigens in PBS could be used for further oral immunization, possibly benefitting from the buffer and adjuvant in ETVAX.
The data obtained through the development of ETVAX clearly show that an effective and practical inactivated whole cell vaccine can be adapted for general use. Not only are whole cell vaccines immunogenic, but genetic engineering, as shown with ETVAX, can improve their immunogenicity in both infants and travelers. Further, the utilization of dmLT mucosal adjuvant may help overcome the weaker responses to oral vaccines often encountered with oral immunization of young children living in LMICs. The safety of Gram negative whole cell vaccines in young children can be improved with dose reduction without significant losses of immunogenicity. Finally, much progress has been made towards practical oral vaccine presentations. It is hoped that these experiences to date with ETVAX will facilitate not only its development but also the development of other much-needed whole cell-based vaccines such as for cholera and Shigella for oral administration alone or in combinations.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants given ETVAX referenced in this perspective were reviewed and approved by the appropriate institutional ethics committees:
● OEV-121 (Sweden): The Ethical Review Board in the Gothenburg Region, the Western Institutional Review Board, USA and the Swedish Medical Product Agency (Eudract no. 2011-003228-11).
● OEV-122 (Bangladesh): The Declaration of Helsinki and approved by the Research Review and Ethical Review Committees of the International Centre for Diarrhoeal Disease Research, Bangladesh; the Western Institutional Review Board, USA; and the US Food and Drug Administration (clinicaltrials.gov NCT02531802).
● OEV-123 (Benin): Coordinating Ethics Committee of Hospital District of Helsinki and Uusimaa (Finland) (clinicaltrials.gov NCT03729219).
● OEV-124 (Zambia): Ethics committee UNZABREC: University of Zambia Biomedical Research Ethics Committee (PACTR201905764389804).
● OEV-125 (Sweden): Etikprövningsmyndigheten (Swedish Ethical Review Authority) (Sweden) and Human Research Protection Office USAMRDC Office of Research Protections (ORP) (USA) (clinicaltrials.gov NCT05178134).
● OEV-128 (The Gambia): The Gambia Government/MRC Join Ethics Committee, Observational/Interventions Research Ethics Committee., London School of Hygiene and Tropical Medicine, Medical Control Agency (MCA) (PACTR202010819218562). Written informed consent to participate in these studies was provided by the patient/participants’ OR patient/participants legal guardian/next of kin.
The first draft of the manuscript was written by RW and reviewed and further edited and added to by AB. All authors contributed to the article and approved the submitted version.
This work was supported, in part, by the Bill & Melinda Gates Foundation (Opp1112376). Under the grant conditiions of Creative Commons Attribution 4.0 Generic License has already been assigned to the Author Accepted Manuscript version that might arise from this submission.
We thank Dr. Nils Carlin for technical review of the manuscript. We are grateful to Drs. M. Jahangir Hossain and Thomas Wierzba for their input describing the studies in the Gambia as well as to Drs. Nsofwa Sukwa and Cynthia Mubanga for the data from the studies in Zambia. Finally, we thank the numerous scientific teams who carried out the studies described for ETVAX.
RW and AB are employees of PATH which has used various grants to fund portions of the development of ETVAX as part of PATH’s role in promoting the development of vaccines against enteric diseases.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. World Health OrganizationWHO preferred product characteristics (PPCs) (2020)WHO (Accessed March 31, 2020).
2. Khalil I, Walker R, Porter CK, Muhib F, Chilengi R, Cravioto A, et al. Enterotoxigenic escherichia coli (ETEC) vaccines: Priority activities to enable product development, licensure, and global access. Vaccine (2021) 39:4266–77. doi: 10.1016/j.vaccine.2021.04.018
3. Akhtar M, Chowdhury MI, Bhuiyan TR, Kaim J, Ahmed T, Rafique TA, et al. Evaluation of the safety and immunogenicity of the oral inactivated multivalent enterotoxigenic escherichia coli vaccine ETVAX in Bangladeshi adults in a double-blind, randomized, placebo-controlled phase I trial using electrochemiluminescence and ELISA assays for immunogenicity analyses. Vaccine (2019) 37:5645–56. doi: 10.1016/j.vaccine.2018.11.040
4. Qadri F, Wenneras C, Ahmed F, Asaduzzaman M, Saha D, Albert MJ, et al. Safety and immunogenicity of an oral, inactivated enterotoxigenic escherichia coli plus cholera toxin b subunit vaccine in Bangladeshi adults and children. Vaccine (2000) 18(24):2704–12.
5. Qadri F, Ahmed T, Ahmed F, Sack BR, Sack DA, Svennerholm AM. Safety and immunogenicity of an oral, inactivated enterotoxigenic escherichia coli plus cholera toxin b subunit vaccine in Bangladeshi children 18–36 months of age. Vaccine (2003) 21(19–20):2394–403.
6. Sack DA, Shimko J, Torres O, Bourgeois AL, Francia DS, Gustafsson B, et al. Safety and efficacy of a killed oral vaccine for enterotoxigenic e. coli diarrhoea of travellers to Guatemala and Mexico. Vaccine (2007) 25(22):4392–400.
7. Qadri F, Ahmed T, Ahmed F, Begum YA, Sack DA, Svennerholm AM. Reduced doses of oral killed enterotoxigenic escherichia coli plus cholera toxin b subunit vaccine is safe and immunogenic in Bangladeshi infants 6–17 months of age: dosing studies in different age groups. Vaccine (2006) 24(10):1726–33.
8. Bourgeois AL, Wierzba TF, Walker RI. Status of vaccine research and development for enterotoxigenic escherichia coli. Vaccine (2016) 34(26):2880–6.
9. World Health OrganizationWeekly epidemiological record. no. 11, Vol.81(2006)p. 97–104. Available at: https://www.who.int/wer
10. Holmgren J, Bourgeois L, Carlin N, Clements J, Gustafsson B, Lundgren A, et al. Development and preclinical evaluation of safety and immunogenicity of an oral ETEC vaccine containing inactivated e. coli bacteria overexpressing colonization factors CFA/I, CS3, CS5 and CS6 combined with a hybrid LT/CT b subunit antigen, administered alone and together with dmLT adjuvant. Vaccine (2013) 31(20):2457–64.
11. Lundgren A, Leach S, Tobias J, Carlin N, Gustafsson B, Jertborn M, et al. Clinical trial to evaluate safety and immunogenicity of an oral inactivated enterotoxigenic escherichia coli prototype vaccine containing CFA/I overexpressing bacteria and recombinantly produced LTB/CTB hybrid protein. Vaccine (2013) 31(8):1163–70.
12. Lundgren A, Bourgeois L, Carlin N, Clements J, Gustafsson B, Hartford M, et al. Safety and immunogenicity of an improved oral inactivated multivalent enterotoxigenic escherichia coli (ETEC) vaccine administered alone and together with dmLT adjuvant in a double-blind, randomized, placebo- controlled phase I study. Vaccine (2014) 32(52):7077–84.
13. Lebens M, Shahabi V, Bäckström M, Houze T, Lindblad N, Holmgren J. Synthesis of hybrid molecules between heat-labile enterotoxin and cholera toxin b subunits: potential for use in a broad-spectrum vaccine. Infect Immun (1996) 64(6):2144–50. doi: 10.1128/iai.64.6.2144-2150.1996
14. Norton EB, Lawson LB, Freytag LC, Clements JD. Characterization of a mutant escherichia coli heat-labile toxin, LT(R192G/L211A), as a safe and effective oral adjuvant. Clin Vaccine Immunol (2011) 18(4):546–51.
15. Clements JD, Norton EB. The mucosal vaccine adjuvant LT(R192G/L211A) or dmLT. mSphere (2018) 3(4):e00215–18. doi: 10.1128/mSphere.00215-18
16. Lundgren A, Jertborn M, Svennerholm AM. Induction of long term mucosal immunological memory in humans by an oral inactivated multivalent enterotoxigenic escherichia coli vaccine. Vaccine (2016) 34(27):3132–40.
17. Leach S, Lundgren A, Carlin N, Lofstrand M, Svennerholm AM. Cross-reactivity and avidity of antibody responses induced in humans by the oral inactivated multivalent enterotoxigenic escherichia coli (ETEC) vaccine ETVAX. Vaccine (2017) 35(32):3966–73.
18. Qadri F, Akhtar M, Bhuiyan TR, Chowdhury MI, Ahmed T, Rafique TA, et al. Safety and immunogenicity of the oral, inactivated, enterotoxigenic escherichia coli vaccine ETVAX in Bangladeshi children and infants: a double-blind, randomised, placebo-controlled phase 1/2 trial. Lancet Infect Dis (2020) 20(2):208–19. doi: 10.1016/S1473-3099(19)30571-7
19. Akhtar M, Nizam NN, Basher SR, Hossain L, Akter S, Bhuiyan TR, et al. dmLT adjuvant enhances cytokine responses to T cell stimuli, whole cell vaccine antigens and lipopolysaccharide in both adults and infants. Front Immunol (2021) 12:654872. doi: 10.3389/fimmu.2021.654872
20. Mottram L, Lundgren A, Svennerholm. A-M, Leach S. A systems biology approach identifies b cell maturation antigen (BCMA) as a biomarker reflecting oral vaccine induced IgA antibody responses in humans. Front Immunol (2021) 12:647873. doi: 10.3389/fimmu.2021.647873
21. Svennerholm AM, Lundgren A, Leach S, Akhtar M, Qadri F. Mucosal immune responses against an oral enterotoxigenic escherichia coli vaccine evaluated in clinical trials. J Infect Dis (2021) 224(12 Suppl 2):S821–8. doi: 10.1093/infdis/jiab475
22. Svennerholm AM, Qadri F, Lundgren A, Kaim J, Bhuiyan TR, Akhtar M, et al. Induction of mucosal and systemic immune responses against the common O78 antigen of an oral inactivated ETEC vaccine in Bangladeshi children and infants. Vaccine (2022) 40(2):380–9. doi: 10.1016/j.vaccine.2021.10.056
23. Qifang B, Ferreras E, Pezzoli L, Legros D, Ivers LC, Date K, et al. Protection against cholera from killed whole-cell oral cholera vaccines: a systematic review and meta-analysis. Lancet Infect Dis (2017) 17:1080–1088. doi: 10.1016/S1473-3099(17)30359-6
24. Qadri F, Wierzba TF, Ali M, Chowdhury F, Khan AI, Saha A, et al. Efficacy of a single-dose, inactivated oral cholera vaccine in Bangladesh. N Engl J Med (2016) 374:1723–32. doi: 10.1056/NEjMoa1510330
25. Sukwa N, Mubanga C, Hatyoka LM, Chilyabanyama ON, Mundia S, Chibuye M, et al. (2022). Safety, tolerability, and immunogenicity of an oral inactivated ETEC vaccine (ETVAX®) with dmLT adjuvant in healthy adults and children in Zambia: An age descending randomised, placebo- controlled trial, in: 2022 VASE meeting, Washington, DC, November 29 to December 1, 2022.
26. Mubanga C, Mwape K, Simuyandi M, Chibesa K, Chisenga C, Chilya O, et al. (2022). Cross-reactivity of the ETVAX® vaccine-induced antibodies to non-vaccine ETEC antigens and diarrhoeagenic escherichia coli specific antigens: A microarray analysis, in: 2022 VASE meeting, Washington, DC, November 29 to December 1, 2022.
27. Kantele A. (2021). A phase 2b placebo controlled clinical trial of the oral vaccine ETVAX® to examine safety, immunogenicity, diagnostic methods and protective efficacy against travelers’ diarrhea among Finnish travelers to Benin, West Africa, in: 2022 VASE Virtual Symposium, Washington, DC, September 28 to September 30, 2021.
28. Hossain JM, Secka F, Sanyang LC, Taiwo R, Okoh EC, Olubiyi OA, et al. (2022). A field trial examining the safety, immunogenicity, and efficacy of ETVAX vaccine against enterotoxigenic e. coli-associated diarrhea in Gambian children aged 6 to 18 months, in: 2022 VASE meeting, Washington, DC, November 29 to December 1, 2022.
29. Kim MJ, Moon YH, Kim H, Rho S, Shin YK, Song M, et al. Cross-protective Shigella whole-cell vaccine with a truncated O-polysaccharide chain. Front Microbiol (2018) 9:2609. doi: 10.3389/fmicb.2018.02609
30. Sharma T, Joshi N, Kumar MA, Nordqvist SL, Lebens M, Kanchan V, et al. Development of hillchol®, a low-cost inactivated single strain hikojima oral cholera vaccine. Vaccine (2020) 38(50):7998–8009. doi: 10.1016/j.vaccine.2020.10.043
Keywords: immunity, oral immunization, adjuvant, vaccine, ETEC vaccine
Citation: Walker RI and Bourgeois AL (2023) Oral inactivated whole cell vaccine for mucosal immunization: ETVAX case study. Front. Immunol. 14:1125102. doi: 10.3389/fimmu.2023.1125102
Received: 15 December 2022; Accepted: 03 February 2023;
Published: 02 March 2023.
Edited by:
Andreas Frey, Research Center Borstel (LG), GermanyReviewed by:
Nicholas J. Mantis, Wadsworth Center, United StatesCopyright © 2023 Walker and Bourgeois. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Richard I. Walker, cndhbGtlcjIwMTlAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.