
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Immunol. , 01 March 2022
Sec. Cancer Immunity and Immunotherapy
Volume 13 - 2022 | https://doi.org/10.3389/fimmu.2022.836338
This article is part of the Research Topic Immunotherapy with Checkpoint Inhibitors for Non-small Cell Lung Cancer, Colon Cancer and Esophageal Cancer View all 48 articles
 Zhi-Nuan Hong1,2,3,4†
Zhi-Nuan Hong1,2,3,4† Lei Gao1,2,3,4†
Lei Gao1,2,3,4† Kai Weng1,2,3,4†
Kai Weng1,2,3,4† Zhixin Huang1,2,3,4
Zhixin Huang1,2,3,4 Wu Han1,2,3,4
Wu Han1,2,3,4 Mingqiang Kang1,2,3,4*
Mingqiang Kang1,2,3,4*Objectives: The combination of neoadjuvant chemotherapy and immunotherapy (nICT) is a novel treatment for locally advanced esophageal cancer. There is concern that nICT may increase operation difficulty, postoperative morbidity, and mortality. This study aimed to compare short-term outcomes among esophagectomy after neoadjuvant chemoradiotherapy (nCRT) and nICT and for locally advanced esophageal squamous cell carcinoma (ESCC).
Methods: A retrospective analysis of a prospectively maintained database was performed to identify patients (from January 2017 through July 2021) who underwent surgery for ESCC following neoadjuvant therapy. A 1:1 propensity score matching (PSM) with a caliper 0.05 was conducted to balance potential bias.
Results: A 1:1 PSM was conducted based on clinical stage, age, body mass index (BMI), and tumor location, and then 32 comparable pairs were matched. After PSM, age, gender, BMI, American Society of Anesthesiologists (ASA) status, smoking history, clinical stage, tumor location, lymphadenectomy field, pathological stage, anastomotic position, route of gastric conduit, procedure type, and operative approach were comparable between groups. Compared with the nICT group (median, 300 min), the operation time was significantly longer in the nCRT group (median, 376 min). However, both groups were comparable in intraoperative blood loss, thoracic drainage volume, intensive care unit (ICU) stay, postoperative hospital stays, and hospital cost. Further, 30-day mortality, 30-day readmission, ICU readmission, and major complications were similar in both groups. The nCRT group had an advantage in pathological response. The pathological complete response (pCR) was 18.8% (6/32) in the nICT group and 43.8% (14/32) in the nCRT group (p = 0.03). The major pathological response (MPR) was 71.9% (23/32) in the nCRT group and 34.4% (11/32) in the nICT group (p = 0.03).
Conclusions: Based on our preliminary experience, esophagectomy appears to be safe and feasible following combined neoadjuvant immunotherapy with chemotherapy for locally advanced esophageal cancer.
Esophageal cancer (EC) is one of the most common and challenging types of cancer with 572,000 new diagnosis cases and 500,000 deaths annually. More than 50% of EC occurred in East Asia, and 90% of those patients have esophageal squamous cell carcinoma (ESCC) (1, 2). Esophagectomy plays an important role in the treatment of locally advanced EC. However, esophagectomy alone is often associated with high recurrence and metastasis rates reaching up to 43.3%–50.0% (3).
Neoadjuvant chemotherapy (nCT) or neoadjuvant chemoradiotherapy (nCRT) plus surgery had been applied to improve long-term results. Kamarajah et al. reported that nCT or nCRT followed by surgery for esophageal adenocarcinoma were equal in 5-year survival rates, and nCRT followed by surgery had an advantage in 5-year survival rates for ESCC (4). Currently, nCRT plus esophagectomy is recommended as first-line therapy for locally advanced ESCC (5). However, based on the long-term result of NEOCRTEC5010 Randomized Clinical Trial, the 5-year cumulative incidence of locoregional recurrence, distant recurrence, and overall recurrence in the nCRT group were 15.3%, 24.3%, and 32.2%, respectively, in locally advanced ESCC, which were still not promising (6). Further, a meta-analysis showed that compared with the surgery alone group, nCRT followed by surgery had an increased risk of total postoperative mortality and treatment-related mortality in patients diagnosed with ESCC (7). Thus, it is necessary to explore the novel pattern of neoadjuvant therapy for ESCC.
Based on CheckMate 577 trails results, Kelly et al. reported that nivolumab adjuvant therapy could prolong 11.4 months of disease-free survival among patients with resected esophageal or gastroesophageal junction cancer who had received nCRT (8). Further, pembrolizumab (PD-1 antagonist) plus chemotherapy has been recommended as first-line therapy for advanced EC (9). Considering the antibodies against the immune inhibitory pathway of programmed death 1 (PD-1) protein or PD-1 ligand 1 (PD-L1) checkpoint inhibitors is a new mechanism for the treatment of ESCC. nCT and immunotherapy (nICT) plus surgery may bring long-term benefits to patients diagnosed with ESCC. Recently, single-arm studies have revealed that the application of nICT in patients with locally advanced ESCC is safe and effective (10, 11).
To explore a new pattern of therapy, preoperative safety and short-term outcomes are the first concern for surgeons. However, a handful of studies focused on the comparison of short-term results and pathological response between nICT and nCRT. This study compared short-term results between nICT and nCRT to evaluate the potential effect of nICT on preoperative outcomes especially surgery safety and pathology response.
This is a retrospective review based on prospectively collected data conducted with consecutive patients who underwent esophagectomy followed nICT or nCRT for ESCC at Fujian Medical University Union Hospital from January 2017 to April 2021. This study was approved by the Ethics Committee of the Fujian Medical University Union Hospital, China (YF033-01). Inclusion criteria included aged between 18 and 75 years old; diagnosed with ESCC; receiving nICT or nCRT following esophagectomy; staged with cT1N1-3M0 or cT2-4aN0-3M0; and with normal hematologic, hepatic, and renal function. Exclusion criteria included patients with non-resectable tumors or metastases during exploratory surgery; patients receiving nCT or other targeted therapy; patients receiving salvage surgery; and patients with palliative surgery.
Patients in the nICT group received 2–4 cycles of intravenous PD-1 inhibitor (sintilimab at a dose of 200 mg, pembrolizumab at a dose of 200 mg, toripalimab at a dose of 240 mg, and camrelizumab at a dose of 200 mg) every 3 weeks (day 1) and simultaneous chemotherapy consisted of platinum-based drugs and paclitaxel (TP regimen). The details of the regimen are as follows: cisplatin (60 mg/m2) on day 1, albumin-bound paclitaxel (125 mg/m2) on days 1 and 8, and sintilimab/pembrolizumab/camrelizumab (200 mg) on day 1 were administered intravenously during each cycle (of 21-day duration). Docetaxel (75 mg/m2), cisplatin (60 mg/m2), and toripalimab (240 mg) were administered intravenously during each cycle (of 21-day duration) on day 1. Corticosteroids, thyroid function [including T3, T4, and thyroid-stimulating hormone (TSH)], glucose, and myocardial enzyme were routinely examined before each cycle of nICT for early detection of immunotherapy-related adverse events. When grade 2 above immunotherapy-related events occurred, we stopped the application of nICT and prioritized the management of adverse reactions. For patients who successfully received two cycles of neoadjuvant therapy, we conducted another clinical evaluation, followed by a multidisciplinary consultation to determine whether the patient should undergo surgery or continue treatment.
Patients in the nCRT group received chemotherapy (paclitaxel or 5-fluorouracil plus platinum) concurrent radiotherapy, which consisted of 40–56 Gy in daily fractions of 1.8 Gy five times a week. Radiation targets are mapped on CT using all diagnostic information by an experienced radiation oncologist.
For patients suitable for radical esophagectomy after clinical evaluation, the surgery was performed within 4–8 weeks from the end of the last neoadjuvant treatment if there were no contraindications for surgery treatment. Patients received McKeown minimally invasive esophagectomy (MIE) with or without robot-assisted, including 2-field or 3-field lymphadenectomy and gastric reconstruction. We regularly conducted 2-field lymphadenectomy, and standard three-field lymphadenectomy was performed in patients with suspected swollen lymph nodes in the neck. During the operation, patients with severe adhesion or intraoperative bleeding were transferred to thoracotomy. All operations were conducted by experienced surgeons with more than 50 cases annually, which ensured the surgery quality.
Postoperative complications were coded by Clavien–Dindo classification, and Clavien–Dindo classification grade ≧ 3 was defined as major complications. The comprehensive complication index (CCI) applied as a tool to evaluate complications systematically was calculated at www.assessurgery.com (12). The primary end point was 30-day complications (including pneumonia, anastomotic leakage, pleural infusion, chylothorax, and cardiac events). Secondary end points included pathological response, operation time, postoperative thoracic drainage, thoracic drainage tube stay, 30-day readmission rate, and 30-day mortality. Interval to surgery was defined as the last measured from the end of last neoadjuvant treatment to the date of surgery, and operative time was measured from incision to wound closure. Intensive care unit (ICU) stay was defined from the day of into ICU to the day of leaving the ICU. Postoperative hospital stay was defined from the day of operation to the day of leaving Fujian Medical University Union Hospital.
The pathological TNM stage was staged according to the 8th edition of the American Joint Committee on Cancer/Union for International Cancer Control staging system. Major pathological reaction (MPR) was defined as less than 10% residual tumor cells, and pathological complete response (pCR) was defined as evidence of no residual tumor cells.
Patients were classified into two groups based on neoadjuvant therapy patterns. Propensity score matching (PSM) was calculated based on a logistic regression model, with a caliper 0.05, matching ratio = 1:1 to balance potential bias. The minor mirror histogram of propensity scores is listed to show the matching details (13, 14). The continuous variables were expressed as median (quartile difference), and the categorical variables were expressed as numbers (percentage). χ2 test was used for classification data, and Mann–Whitney U test was used for anomaly distribution data comparison. Statistical analysis was performed in R Version 4.0.4 (R Foundation for Statistical Computing, Vienna, Austria). Bilateral p-values <0.05 were considered significant.
The patient selection chart and PSM details are shown in Figure 1. A total of 52 patients in the nICT group and 35 patients in the nCRT group were included for further analysis. Then, to balance the potential bias, a 1:1 PSM was conducted based on clinical stage, age, body mass index (BMI), and tumor location. Finally, 32 comparable pairs were matched.
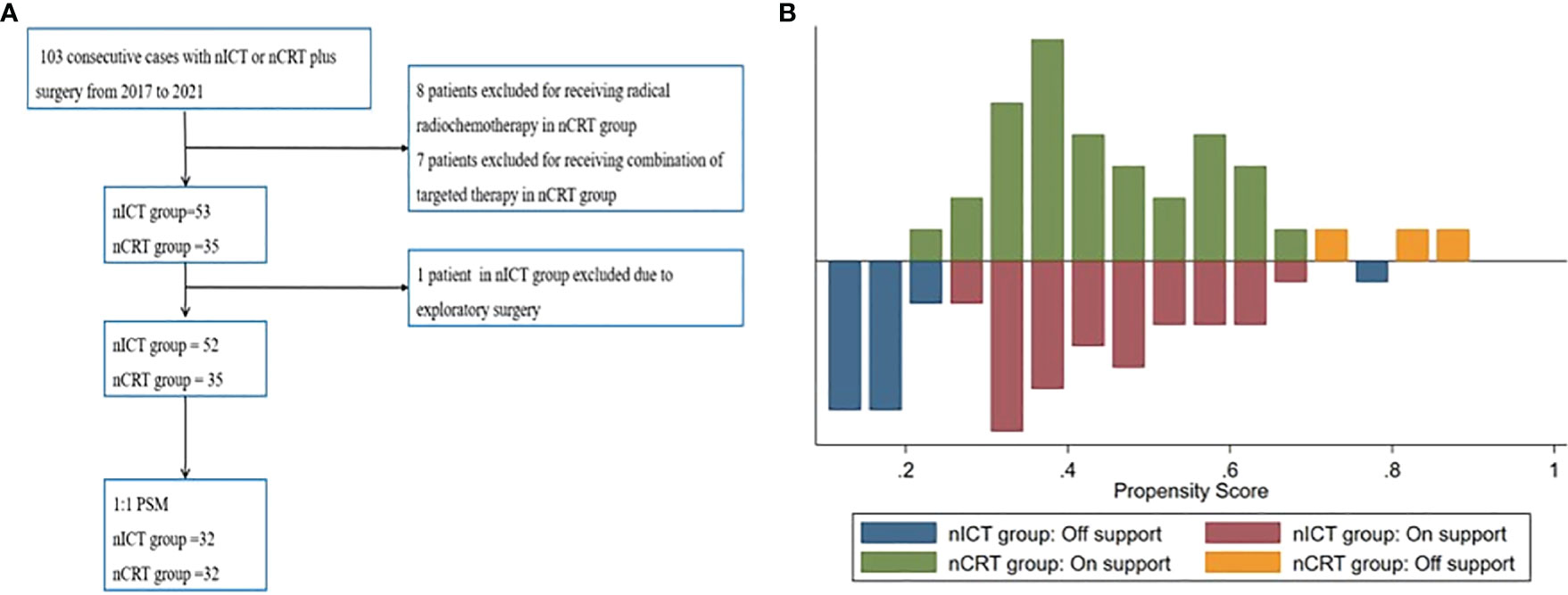
Figure 1 (A) Patient selection flowchart. (B) Mirror histogram of propensity scores for patients. PSM, propensity score matching; nICT, neoadjuvant chemotherapy and immunotherapy; nCRT, neoadjuvant chemoradiotherapy.
The baseline characteristics after PSM with 32 patients in each group are summarized in Table 1. After PSM, the clinical and demographic characteristics of the two groups were well balanced, including age, gender, BMI, American Society of Anesthesiologists (ASA) status, hypertension history, smoking history, tumor location, preoperative albumin, preoperative hemoglobin, forced expiratory volume in 1 s (FEV1), ejection fractions (EF), lymphadenectomy filed, clinical stage, histologic subtype, anastomotic position, route of gastric conduit, procedure type, clinical stage, and operative approach.
All patients in both the nICT group and nCRT group successfully received MIE without conversion into thoracotomy, although lymph nodes moved number in the nICT group (median 39) was more than that in the nCRT group (median 32). However, compared with the nICT group (319.2 ± 80.2 min), the operation time was significantly longer in the nCRT group (378.8 ± 72.7 min). Both groups were comparable in intraoperative blood loss, thoracic drainage tube stays, thoracic drainage volume, postoperative hospital stay, and hospital cost. Further, 30-day mortality, 30-day readmission, and ICU readmission were also similar in both groups. Compared with the nICT group, the nCRT group had an advantage in pathological response. The pCR was 18.8% (6/32) in the nICT group and 43.8% (14/32) in the nCRT group (p = 0.03). The major pathological response (MPR) was 71.9% (23/32) in the nCRT group and 34.4% (11/32) in the nICT group (p = 0.03). Perioperative outcomes after PSM were summarized in Table 2.
The complications within 30-day after PSM are summarized in Table 3. The incidence of pneumonia, pleural effusion, palsy of recurrent laryngeal nerve, chylothorax, and postoperative blood transfusion were comparable in both groups. Major complications and CCI were comparable in both groups. Comparison details of 30-day major complications and CCI after PSM are listed in Figure 2.
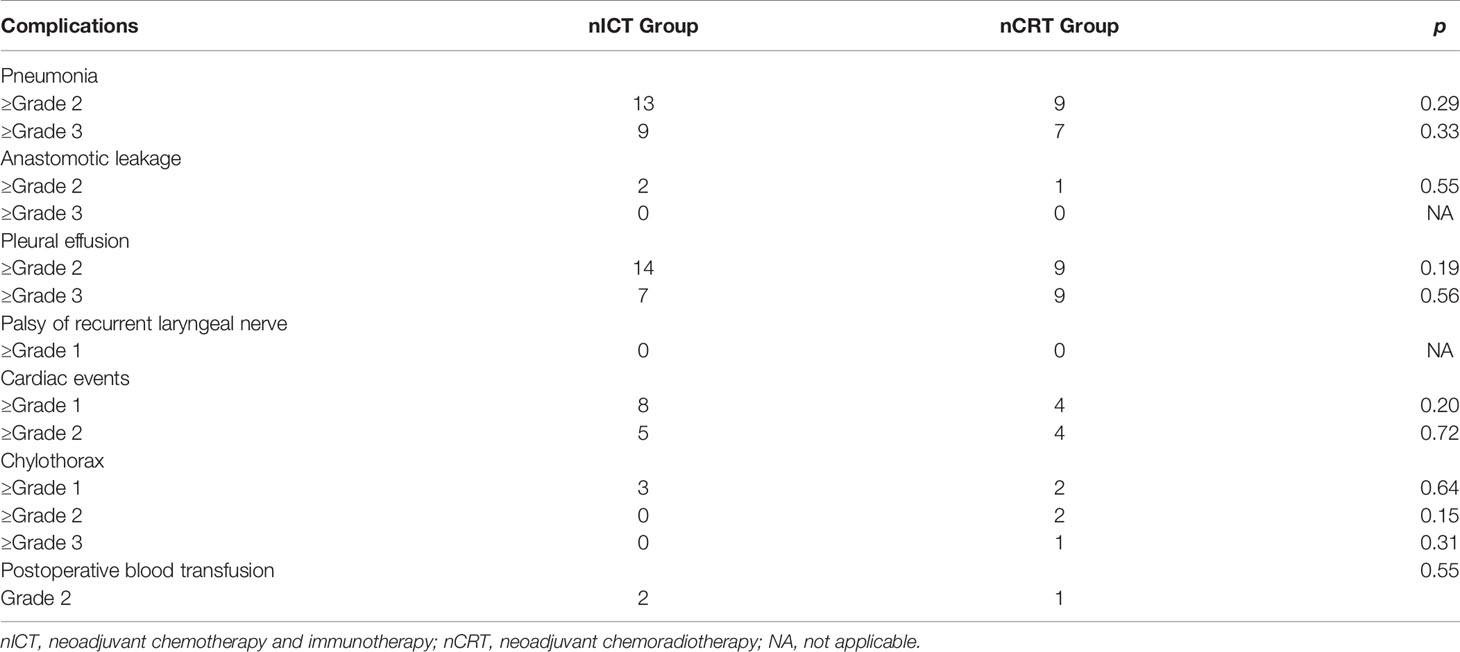
Table 3 Postoperative complications within 30-day after operation evaluated by Clavien–Dindo classification.
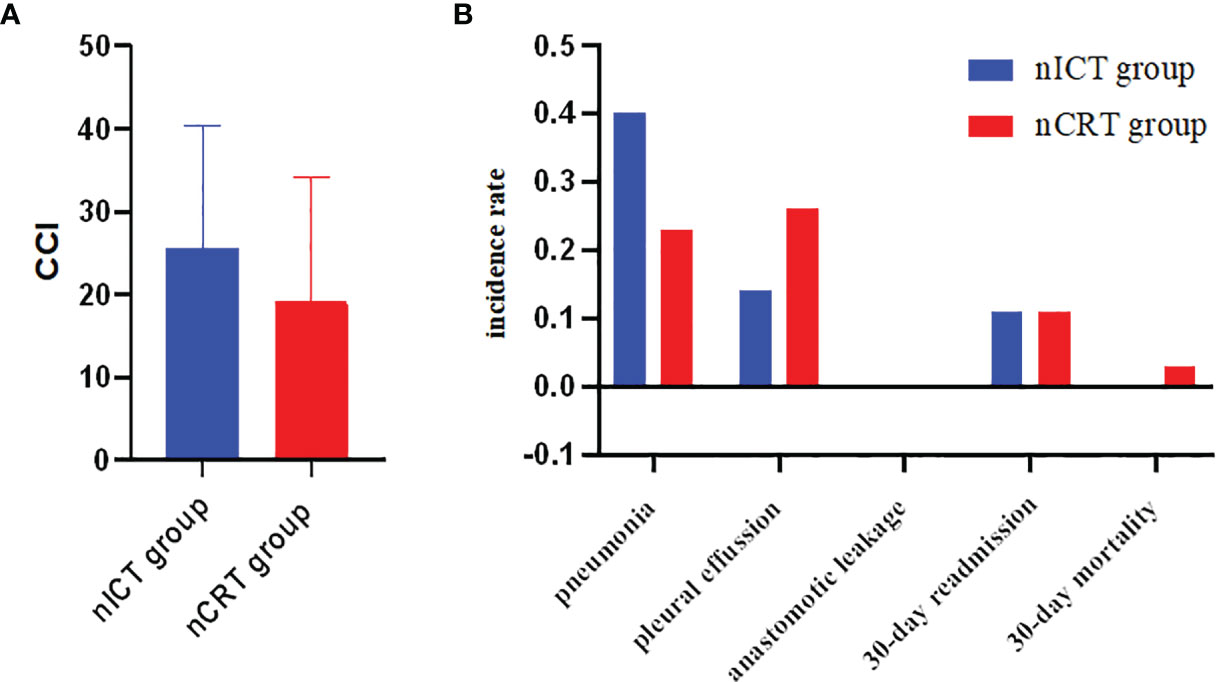
Figure 2 (A) Comparisons of CCI between nICT group and nCRT group after PSM. (B) Comparisons of major complications between nICT group and nCRT group after PSM. CCI, comprehensive complication index; nICT, neoadjuvant chemotherapy and immunotherapy; nCRT, neoadjuvant chemoradiotherapy; PSM, propensity score matching.
Immune dermatitis was relatively common, with an incidence of 6.25% (2/32). Only one patient underwent grade 3 pneumonitis on the 10th day after the operation. This patient was admitted into ICU and treated with 40 mg of methylprednisolone for 7 days. Then, the symptoms were relieved, and this patient recovered without intubation. The chest scan changes are summarized in Figure 3.

Figure 3 (A) Chest CT scan before surgery. (B) Chest scan on 5th day after operation. (C) Chest scan after application of methylprednisolone for 7 days. (D) Chest scan in 3 months after discharge.
Compared with the nICT group (median, 300 min), the operation time was significantly longer in the nCRT group (median, 376 min). The 30-day complications measured by CCI and major complications were comparable between the nICT group and nCRT group after PSM. The 30-day mortality, 30-day readmission, and ICU readmission were similar in both groups. The nCRT group had an advantage in both pCR and MPR (p < 0.03).
The postoperative mortality and morbidity were comparable between the nICT group and the nCRT group. Additional neoadjuvant immunotherapy did not increase postoperative mortality and morbidity, and our finding was consistent with the previous report. Sihag et al. compared the major complications between patients receiving neoadjuvant immunotherapy and chemoradiotherapy and nCRT and found that additional neoadjuvant immunotherapy was not associated with a statistically significantly increased risk of developing major complications (including pulmonary complications, anastomotic leakage, and other complications) (15). However, additional neoadjuvant immunotherapy brings additional immune-related AEs. In this study, one patient had grade 3 pneumonitis on the 7th day after the operation and finally recovered by administration of methylprednisolone treatment. A recent meta‐analysis including 12,876 patients from 23 randomized control trials showed that the incidence of pneumonitis associated with PD‐1 inhibitors was 5.17%, with an incidence of grade 3–5 pneumonitis of 4.14% (16). The time to onset pneumonitis had a really wide time window ranging from 9 days to 19.2 months (17). Pneumonia is one of the most common complications after esophagectomy. However, due to the various radiological subtypes of pneumonia, sometimes distinguishing pneumonia from pneumonitis is really a challenge. Thus, it is necessary to be vigilant for the incidence of pneumonitis when patients’ symptoms do not correspond to sputum, serum etiology, and inflammatory markers. Antibiotic treatment is recommended before pneumonitis is diagnosed.
Operation time is an indicator of surgical difficulty, and moved lymph number is an indicator of surgical quality in esophagectomy. Operation time in the nCRT group was longer than that in the nCRT group, and moved lymph nodes in nICT were more than that in the nCRT group (both above 15), although previous studies indicated that surgical resection of non-small cell lung cancer (NSCLC) following neoadjuvant immunotherapy increased surgical difficulty and challenge due to dense fibrosis, especially in mediastinal and hilar dissection (18, 19). Further, there was also a possibility of unexpected conversion into thoracotomy in patients following immunotherapy (20). For patients with NSCLC, there was a reduction of moved lymph nodes in the neoadjuvant immunotherapy group (21). However, there was still no similar report in esophagectomy following nICT. In this study, all patients in the nICT group received McKeown MIE without any transformation thoracotomy. We admitted that after the application of nICT, the primary tumor shrunk, and there was fibrous scarring in the esophageal mesentery, which led to difficulty in distinguishing the boundary between the tumor and surrounding organs or tissues. Clinical practice showed that after nICT, the fibrosis was not dense, and for experienced surgeons, MIE was still applicable. For patients receiving nCRT, the primary tumor site of esophageal cancer often exhibits necrosis, fibrosis, and organizational alterations (Figure 4). Further, in some cases, the normal tissue gap disappears and transforms into dense fibrosis. Adhesive fibrosis is more serious in patients with obvious tumor invasion before radiotherapy (22). Thus, resection in the nCRT group is more difficult and requires more time to separate the esophagus from surrounding tissues and organs. In summary, for resection following nICT or nCRT, the surgical procedures have high technical requirements for surgeons. Such procedures should be conducted by experienced surgeons. Based on the present evidence, it seems that compared with nCRT, esophagectomy following nICT had a lower operation difficulty.
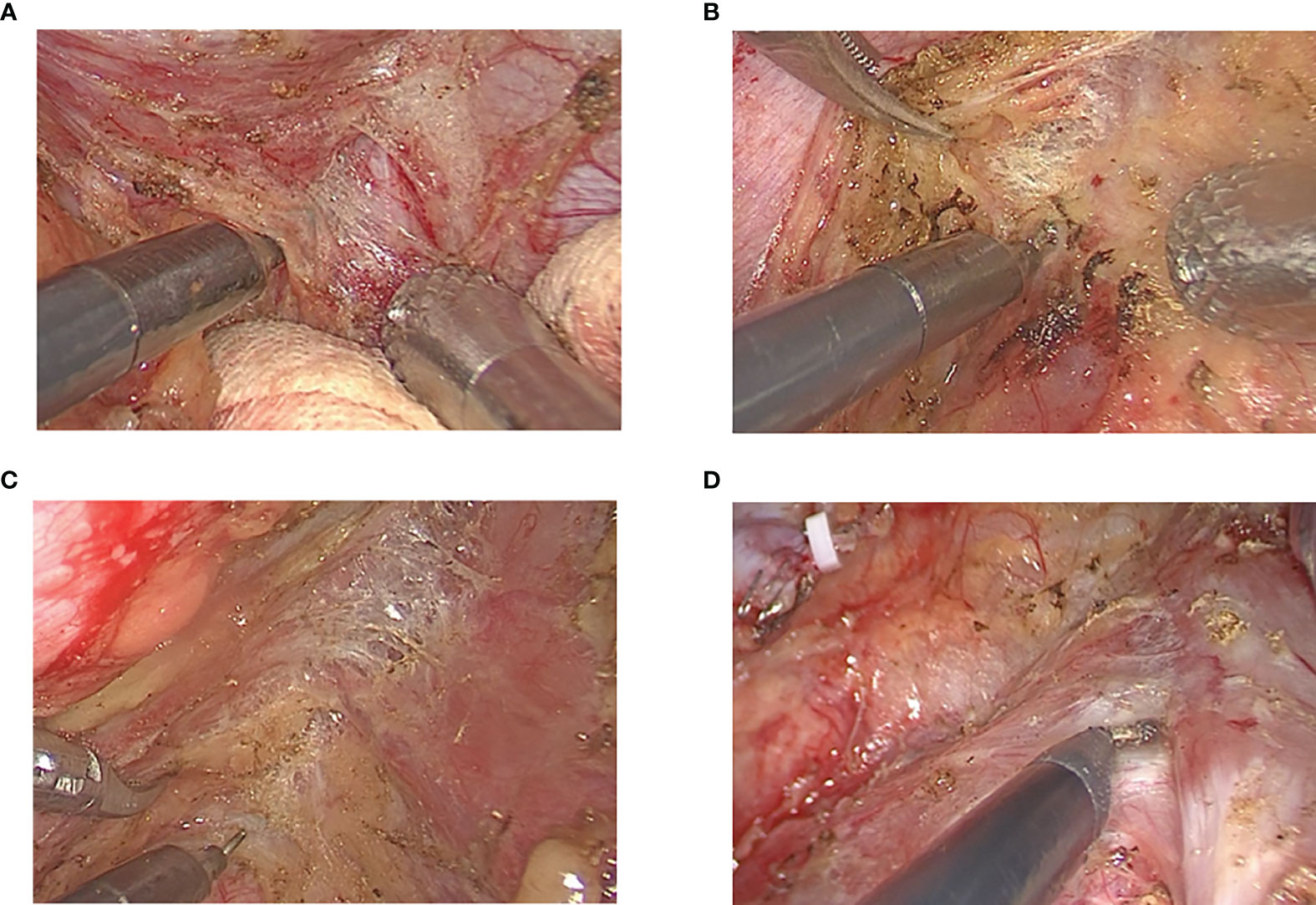
Figure 4 (A) Fibrosis in esophageal mesentery near primary tumor. (B) Fibrosis in esophageal mesentery near pericardium. (C) Fibrosis in esophageal mesentery near thoracic aorta. (D) Fibrosis in esophageal mesentery near trachea.
The nCRT group had an advantage in pathological response. The pCR rate was 18.8% (6/32) in the nICT group and 43.8% (14/32) in the nCRT group (p = 0.03). pCR was proved to be associated with long-term survival. Kamarajah et al. analyzed the National Cancer Database (2006–2015) including 2,367 with ESCC (nCRT 2,155 and nCT 212) and found that for ESCC, nCRT followed by surgery had advantage in pCR rate (50.9% versus 30.4%; p < 0.001), margin-negative resections (92.8% versus 82.4%, p < 0.001), and a statistically significant overall survival benefit (hazard ratio (HR) 0.78, 0.62 to 0.97) (23). A recent meta-analysis including 4,529 patients (nCT 2,035 and nCRT 2,494) showed that compared with nCT, nCRT could provide a higher 3-year survival benefit, higher R0 resection, and pCR rates, but no increase in 5-year survival (24). Zhang et al. conducted a propensity score-matched study from the National Cancer Center to compare the long-term results between nCRT and nCT and found that significantly higher pCR rates in the nCRT group did not lead to a longer survival (25). Thus, considering the different mechanisms of immunotherapy, it is worth conducting a long-term follow-up to evaluate the effect of nICT. Whether nICT could challenge nCRT or nCT in the first-line treatment of locally advanced ESCC requires the evaluation of long-term results in a cohort with a sufficient sample size.
To our best knowledge, this is the first study that compares the short-term outcomes between nICT and nCRT. We tried to solve the potential selection and detection bias by strict patient selection and PSM. However, this study was still limited by its retrospective nature, and it was also only conducted in a single institution with a relatively limited case number. Due to the lack of patients’ compliance and the quality control of radiotherapy, the application of nCRT was relatively limited, and nCT was a more popular pattern in China. Some patients received nCRT in other hospitals and then received surgery in our institution. Thus, the case number of the nCRT group in our institution was limited with potential bias. We used pCR to evaluate the antitumor effect of neoadjuvant therapy. Although pCR has been proved to be associated with long-term survival, long-term follow-up is necessary for further confirming the effect of nICT. To determine whether nICT could challenge the status of nCRT in the treatment of locally advanced ESCC and to establish a new treatment model based on immunotherapy, there is an urgent need for more phase III clinical trials and more convincing research results.
Compared with nCRT, esophagectomy following nICT had a lower operation difficulty, similar postoperative complications, and similar mortality. Esophagectomy following nICT is safe and feasible for locally advanced ESCC. Long-term follow-up is necessary to evaluate the effect of nICT.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Fujian Medical University Union Hospital. The patients/participants provided their written informed consent to participate in this study.
Z-NH conceived the concept and coordinated the design. Z-NH drafted the manuscript with significant contributions from LG and KW. All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
This study was sponsored by the Key Laboratory of Cardio-Thoracic Surgery (Fujian Medical University), Fujian Province University.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We deeply appreciate Toedit for its excellent language service.
1. Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer Statistics in China, 2015. CA Cancer J Clin (2016) 66(2):115–32. doi: 10.3322/caac.21338
2. He F, Wang J, Liu L, Qin X, Wan Z, Li W, et al. Esophageal Cancer: Trends in Incidence and Mortality in China From 2005 to 2015. Cancer Med (2021) 10(5):1839–47. doi: 10.1002/cam4.3647
3. Lagergren J, Smyth E, Cunningham D, Lagergren P. Oesophageal Cancer. Lancet (2017) 390(10110):2383–96. doi: 10.1016/S0140-6736(17)31462-9
4. Ajani JA, D’Amico TA, Bentrem DJ, Chao J, Corvera C, Das P, et al. Esophageal and Esophagogastric Junction Cancers, Version 2.2019, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw (2019) 17(7):855–83. doi: 10.6004/jnccn.2019.0033
5. van Hagen P, Hulshof MC, van Lanschot JJ, Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BP, et al. Preoperative Chemoradiotherapy for Esophageal or Junctional Cancer. N Engl J Med (2012) 366(22):2074–84. doi: 10.1056/NEJMoa1112088
6. Yang H, Liu H, Chen Y, Zhu C, Fang W, Yu Z, et al. Neoadjuvant Chemoradiotherapy Followed by Surgery Versus Surgery Alone for Locally Advanced Squamous Cell Carcinoma of the Esophagus (NEOCRTEC5010): A Phase III Multicenter, Randomized, Open-Label Clinical Trial. J Clin Oncol (2018) 36(27):2796–803. doi: 10.1200/JCO.2018.79.1483
7. Ando N, Kato H, Igaki H, Shinoda M, Ozawa S, Shimizu H, et al. A Randomized Trial Comparing Postoperative Adjuvant Chemotherapy With Cisplatin and 5-Fluorouracil Versus Preoperative Chemotherapy for Localized Advanced Squamous Cell Carcinoma of the Thoracic Esophagus (JCOG9907). Ann Surg Oncol (2012) 19(1):68–74. doi: 10.1245/s10434-011-2049-9
8. Yarchoan M, Johnson BA 3rd, Lutz ER, Laheru DA, Jaffee EM. Targeting Neoantigens to Augment Antitumour Immunity. Nat Rev Cancer (2017) 17(9):569. doi: 10.1038/nrc.2017.74
9. Smyth EC, Gambardella V, Cervantes A, Fleitas T. Checkpoint Inhibitors for Gastroesophageal Cancers: Dissecting Heterogeneity to Better Understand Their Role in First-Line and Adjuvant Therapy. Ann Oncol (2021) 32(5):590–9. doi: 10.1016/j.annonc.2021.02.004
10. Shen D, Chen Q, Wu J, Li J, Tao K, Jiang Y. The Safety and Efficacy of Neoadjuvant PD-1 Inhibitor With Chemotherapy for Locally Advanced Esophageal Squamous Cell Carcinoma. J Gastrointest Oncol (2021) 12(1):1–10. doi: 10.21037/jgo-20-599
11. Yang G, Su X, Yang H, Luo G, Gao C, Zheng Y, et al. Neoadjuvant Programmed Death-1 Blockade Plus Chemotherapy in Locally Advanced Esophageal Squamous Cell Carcinoma. Ann Transl Med (2021) 9(15):1254. doi: 10.21037/atm-21-3352
12. Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA. The Comprehensive Complication Index: A Novel Continuous Scale to Measure Surgical Morbidity. Ann Surg (2013) 258(1):1–7. doi: 10.1097/SLA.0b013e318296c732
13. Zhan C, Yang X, Song X, Yan L. Radiotherapy vs Surgery for T1-2N0M0 Laryngeal Squamous Cell Carcinoma: A Population-Based and Propensity Score Matching Study. Cancer Med (2018) 7(7):2837–47. doi: 10.1002/cam4.1525
14. Yang X, Sun F, Chen L, Shi M, Shi Y, Lin Z, et al. Prognostic Value of Visceral Pleural Invasion in non-Small Cell Lung Cancer: A Propensity Score Matching Study Based on the SEER Registry. J Surg Oncol (2017) 116(3):398–406. doi: 10.1002/jso.24677
15. Sihag S, Ku GY, Tan KS, Nussenzweig S, Wu A, Janjigian YY, et al. Safety and Feasibility of Esophagectomy Following Combined Immunotherapy and Chemoradiotherapy for Esophageal Cancer. J Thorac Cardiovasc Surg (2021) 161(3):836–43.e1. doi: 10.1016/j.jtcvs.2020.11.106
16. Su Q, Zhu EC, Wu JB, Li T, Hou YL, Wang DY, et al. Risk of Pneumonitis and Pneumonia Associated With Immune Checkpoint Inhibitors for Solid Tumors: A Systematic Review and Meta-Analysis. Front Immunol (2019) 10:108. doi: 10.3389/fimmu.2019.00108
17. Naidoo J, Wang X, Woo KM, Iyriboz T, Halpenny D, Cunningham J, et al. Pneumonitis in Patients Treated With Anti-Programmed Death-1/Programmed Death Ligand 1 Therapy. J Clin Oncol (2017) 35(7):709–17. doi: 10.1200/JCO.2016.68.2005
18. Kitagawa S, Hakozaki T, Kitadai R, Hosomi Y. Switching Administration of Anti-PD-1 and Anti-PD-L1 Antibodies as Immune Checkpoint Inhibitor Rechallenge in Individuals With Advanced Non-Small Cell Lung Cancer: Case Series and Literature Review. Thorac Cancer (2020) 11(7):1927–33. doi: 10.1111/1759-7714.13483
19. Chaft JE, Hellmann MD, Velez MJ, Travis WD, Rusch VW. Initial Experience With Lung Cancer Resection After Treatment With T-Cell Checkpoint Inhibitors. Ann Thorac Surg (2017) 104(3):e217–8. doi: 10.1016/j.athoracsur.2017.03.038
20. Bott MJ, Cools-Lartigue J, Tan KS, Dycoco J, Bains MS, Downey RJ, et al. Safety and Feasibility of Lung Resection After Immunotherapy for Metastatic or Unresectable Tumors. Ann Thorac Surg (2018) 106(1):178–83. doi: 10.1016/j.athoracsur.2018.02.030
21. Zhang F, Qiu B, Ji Y, Guo W, Li N, Xue Q, et al. Comparison of Surgical Difficulty in Patients With Resectable Non-Small Cell Lung Cancer Under Different Neoadjuvant Treatment Modes: A Retrospective Cohort Study. J Thorac Dis (2021) 13(10):5604–16. doi: 10.21037/jtd-21-1007
22. Liu G, Han Y, Peng L, Wang K, Fan Y. Reliability and Safety of Minimally Invasive Esophagectomy After Neoadjuvant Chemoradiation: A Retrospective Study. J Cardiothorac Surg (2019) 14(1):97. doi: 10.1186/s13019-019-0920-0
23. Kamarajah SK, Phillips AW, Ferri L, Hofstetter WL, Markar SR. Neoadjuvant Chemoradiotherapy or Chemotherapy Alone for Oesophageal Cancer: Population-Based Cohort Study. Br J Surg (2021) 108(4):403–11. doi: 10.1093/bjs/znaa121
24. Han J, Wang Z, Liu C. Survival and Complications After Neoadjuvant Chemotherapy or Chemoradiotherapy for Esophageal Cancer: A Meta-Analysis. Future Oncol (2021) 17(17):2257–74. doi: 10.2217/fon-2021-0021
25. Zhang G, Zhang C, Sun N, Xue L, Yang Z, Fang L, et al. Neoadjuvant Chemoradiotherapy Versus Neoadjuvant Chemotherapy for the Treatment of Esophageal Squamous Cell Carcinoma: A Propensity Score-Matched Study From the National Cancer Center in China. J Cancer Res Clin Oncol (2021). doi: 10.1007/s00432-021-03659-7
Keywords: esophagectomy, neoadjuvant chemotherapy and immunotherapy, neoadjuvant chemoradiotherapy, esophageal squamous cell carcinoma, propensity score matching (PSM)
Citation: Hong Z-N, Gao L, Weng K, Huang Z, Han W and Kang M (2022) Safety and Feasibility of Esophagectomy Following Combined Immunotherapy and Chemotherapy for Locally Advanced Esophageal Squamous Cell Carcinoma: A Propensity Score Matching Analysis. Front. Immunol. 13:836338. doi: 10.3389/fimmu.2022.836338
Received: 15 December 2021; Accepted: 31 January 2022;
Published: 01 March 2022.
Edited by:
Hubing Shi, Sichuan University, ChinaReviewed by:
Chen-Yuan Lin, China Medical University Hospital, TaiwanCopyright © 2022 Hong, Gao, Weng, Huang, Han and Kang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mingqiang Kang, a2FuZ21pbmdxaWFuZzA3OTlAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.