
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Immunol. , 30 November 2022
Sec. Autoimmune and Autoinflammatory Disorders : Autoimmune Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fimmu.2022.1054539
Introduction: Psoriatic arthritis (PsA) is a chronic inflammatory disease that frequently develops in patients with psoriasis (PsO) but can also occur spontaneously. As a result, PsA diagnosis and treatment is commonly delayed, or even missed outright due to the manifold of clinical presentations that patients often experience. This inevitably results in progressive articular damage to axial and peripheral joints and entheses. As such, patients with PsA frequently experience reduced expectancy and quality of life due to disability. More recently, research has aimed to improve PsA diagnosis and prognosis by identifying novel disease biomarkers.
Methods: Here, we conducted a systematic review of the published literature on candidate biomarkers for PsA diagnosis and prognosis in MEDLINE(Pubmed), EMBase and the Cochrane library with the goal to identify clinically applicable PsA biomarkers. Meta-analyses were performed when a diagnostic bone and cartilage turnover biomarker was reported in 2 or moredifferent cohorts of PsA and control.
Results: We identified 1444 publications and 124 studies met eligibility criteria. We highlighted bone and cartilage turnover biomarkers, genetic markers, and autoantibodies used for diagnostic purposes of PsA, as well as acute phase reactant markers and bone and cartilage turnover biomarkers for activity or prognostic severity purposes. Serum cartilage oligometrix metalloproteinase levels were significantly increased in the PsA sera compared to Healthy Control (HC) with a standardized mean difference (SMD) of 2.305 (95%CI 0.795-3.816, p=0.003) and compared to osteoarthritis (OA) with a SMD of 0.783 (95%CI 0.015-1.551, p=0.046). The pooled serum MMP-3 levels were significantly higher in PsA patients than in PsO patients with a SMD of 0.419 (95%CI 0.119-0.719; p=0.006), but no significant difference was highlighted when PsA were compared to HC. While we did not identify any new genetic biomarkers that would be useful in the diagnosis of PsA, recent data with autoantibodies appear to be promising in diagnosis, but no replication studies have been published.
Conclusion: In summary, no specific diagnostic biomarkers for PsA were identified and further studies are needed to assess the performance of potential biomarkers that can distinguish PsA from OA and other chronic inflammatory diseases.
Psoriatic arthritis (PsA) is a chronic inflammatory disease that develops in up to 30% of patients with psoriasis (PsO), and can affect up to 0.7% of the general population (1, 2). PsA is characterized as affecting axial and peripheral joints and entheses, which can present clinically with diverse symptoms, often resulting in delayed diagnosis and treatment. PsA can lead to progressive articular damage, thus can be a source of impaired function, permanent disability, quality of life, and an increase in mortality (3, 4).
Through the Biomarkers Project, the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA) places critical emphasis on the research of biomarkers in its development strategy (5). A biomarker is defined as a characteristic that is objectively measured and evaluated as an indicator of pharmacologic responses, or normal or pathogenic biological processes, for a therapeutic intervention (6). Identification of specific biomarkers would improve early diagnosis and management of PsA in patients with joint pain and/or skin psoriasis. Although PsA can develop in up to 30% of PsO patients, the prevalence of undiagnosed PsA in patients with psoriasis is still estimated to be 10-15% (4). Although classification criteria are sometimes used by default, there are currently no diagnostic criteria or specific biomarkers available for PsA (4). Therefore, we sought to identify biomarkers for determining diagnosis and prognosis of PsA by conducting a systematic review and pairwise meta-analysis.
To conduct this research, we followed the guidelines and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for reporting on studies evaluating healthcare interventions (7). PRISMA Checklist is provided in supplementary file 1. Ethics approval was not required under local legislation for this study.
A systematic search of English-language literature was conducted in MEDLINE (via PubMed), EMBase, and the Cochrane Library dating from inception to March 1, 2022. We designed the search algorithm according to the Patient-Intervention-Comparison-Outcome-Time (PICOT) format. Search terms corresponded to MeSH or Emtree terms for “psoriatic arthritis” and “biomarkers” or “pharmacological biomarkers”. A manual search was also performed.
After searching with the pre-determined PICOT algorithm, study eligibility was ascertained after reading the title, keywords, and abstract. Once the articles of interest were identified, the full text was read to evaluate it according to the exclusion criteria, and to subsequently extract the necessary data. Inclusion criteria required the following: study must be an observational or interventional clinical trial published in English before March 2022; include an assessment of biomarker(s) in serum (including genetic biomarkers), synovial fluid, urine, or feces as diagnostic or prognostic factors; cohort must include patients with PsA according to a rheumatologist diagnosis, Moll and Wright criteria, or Classification Criteria for Psoriatic Arthritis (CASPAR).
Exclusion criteria were applied in a sequential order, and included an editorial or congress abstract; duplicates (between electronic databases or journals); non-English language full text; non-human, non-PsA, or pediatric (≤18 years old) populations; off-topic; not relevant for diagnosis and prognosis in PsA. We focused on prognostic factors of disease severity, regardless of treatment, and did not include prognostic factors of response to treatment, out of the scope.
Study results were highlighted in the main text if select biomarkers were mentioned in at least 2 publications. In addition, all included articles are presented in tabular form (Tables 1, 2).
All data was extracted into a standardized spreadsheet. For each article, we collected the data according to a pre-specified strategy. Collected information included the year of publication, name of the first author, geographical area, study design, population age and sex, disease duration, how the PsA population was determined (classification criteria used or therapist diagnosis), biomarkers investigated, primary study methodology, proportion of patients using corticosteroid and/or non-steroidal anti-inflammatory drugs (NSAIDs), proportions of patients using conventional disease modifying anti-rheumatic drugs (DMARDs; i.e., methotrexate, salazopyrine or leflunomide), and biological DMARDs. Study objectives (diagnosis or prognosis), primary outcomes, and control groups (i.e. cutaneous psoriasis, rheumatoid arthritis, spondyloarthritis, systemic lupus erythematosus, undifferentiated arthritis, osteoarthritis or healthy control (HC)) were also recorded. For all extracted data, a central value (mean or median) and variability (standard deviation or interquartile range) was collected. Study quality and risk of bias was assessed using the Newcastle Ottawa Scale for assessing the quality of non-randomized studies in meta-analysis (131).
Meta-analyses were performed when a diagnostic bone and cartilage turnover biomarker was reported in 2 or more different cohorts of PsA and control. Levels of biomarkers in PsA and control populations, means differences (MD) and standard deviation (SD) were extracted. If necessary, we converted median and interquartile in MD and SD using previously published methods (132). To perform sensitivity analyses, we applied a random effects models using the “one-study-removed” method as soon as there were more than two publications. Difference effect sizes were ascertained with the standardized mean difference (SMD) and its 95% confidence intervals (CI). A positive SMD confirmed a higher biomarker level in PsA than the control population. Magnitude of SMD was characterized as small (< 0.40), moderate (0.41 to 0.69) or large (> 0.70) (133).
We identified 1495 records extracted from the PubMed/MEDLINE (n=514), EMBASE (n=919), and Cochrane Library (n=62) databases. After a manual search, 4 additional publications were included.
After removal of 111 duplicates, 1388 articles were screened and 559 met inclusion criteria. Subsequently, 346 publications were excluded because they did not report specific diagnostic or prognostic data for the biomarkers. Ultimately, a total of 124 studies, published from 1993 to 2022, met the eligibility criteria and were included in the qualitative analysis (Figure 1).
Sixty-eight studies evaluated biomarkers for diagnostic purposes, 48 evaluated biomarkers for activity or prognostic severity purposes, and 8 publications studied both diagnostic and prognostic biomarkers (Tables 1, 2). An assessment of bias risk was performed for each study and is available in Tables 3, 4.
Sixteen articles evaluated biomarkers associated with bone and cartilage turnover for their potential as PsA diagnostic biomarkers. All the studies assessing diagnostic biomarkers in our systematic review, including those assessing biomarkers panels, are listed in chronological order of publication in Table 1. For meta-analyses, we considered only clearly identified individual biomarkers, and not panels of biomarkers. The two mainly assessed biomarkers were Cartilage Oligometrix MetalloProteinase (COMP) and Matrix MetalloProteinase-3 (MMP3).
Increases of serum COMP levels by one unit resulted in an increased PsO odds ratio (OR) of 1.001 (95% CI=1.000-1.002, p=0.04), but not for PsA (OR=1.00; 95% CI=0.999-1.002, p=0.47) when comparing PsA to both PsO and HC (10). More recently, a cross-sectional study including patients with PsA, osteoarthritis (OA) and HC demonstrated in its primary discovery phase that COMP levels were significantly higher in sera of the PsA population than that of the OA population (OR=1.24; 95% CI=1.06-1.46, p=0.0062) (15). In the validation phase, serum COMP levels were not significantly different between PsA and OA populations (217.3 ng/mL vs 210.3 ng/mL, respectively p=0.344) (15). The diagnostic value of COMP was assessed in two cross-sectional studies. In the first study, serum COMP levels were significantly higher in patients with PsA (2645.3 ± 489.5 ng/mL) than in the HC population (835.9 ± 434.6 ng/mL) and clearly distinguished the 2 populations (Area Under the Curve [AUC]=0.96, 95% CI Not Available [NA]) (17). The second study compared the biomarker in PsA, OA, and HC and reported significantly higher levels in the sera of PsA patients than in the other two populations (18). COMP levels were also reported to be significantly higher in PsA synovial fluid compared to rheumatoid arthritis (RA), even in the presence of joint destruction (8).
The four studies comparing serum COMP levels between PsA and HC were included in a meta-analysis (10, 15, 17, 18). COMP was significantly increased in the serum of the PsA population, and the effect size measured by SMD was 2.305 (95% CI=0.80-3.81, p=0.003; Figure 2). When COMP levels were compared between PsA and OA, the 3-study meta-analysis reported a significant SMD of 0.78 (95% CI=0.02-1.55, p=0.046) (15, 18).
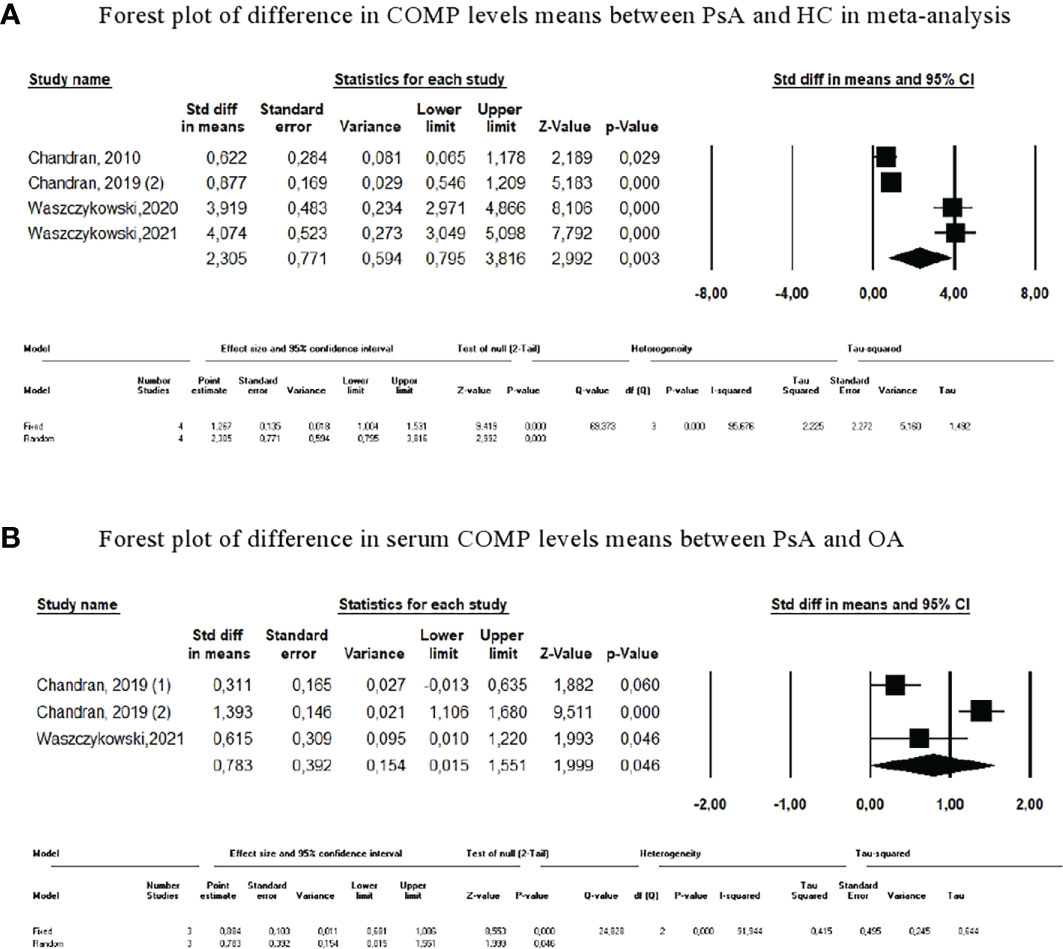
Figure 2 Meta-analysis of COMP levels. (A) Forest plot of difference in COMP levels means between PsA and HC in meta-analysis. (B) Forest plot of difference in serum COMP levels means between PsA and OA.
Due to the heterogeneity of the results, sensitivity analyses were also performed. The results remained unchanged after each study was excluded serially. The difference in COMP levels between PsA and PsO was tested in only one study (10).
The results are more discordant when considering serum levels of MMP3, also known as stromelysin-1. Five cross-sectional studies revealed that MMP3 levels were significantly higher in patients with PsA than in HC (12–14, 17, 18) or in patients with PsO (13). The accuracy of MMP3 to distinguish PsA from PsO (AUC=0.70, 95% CI=0.65-0.75) and PsA from HC (AUC=0.66, 95% CI=0.59-0.74) was moderate. Other studies did not report any difference in MMP3 levels between PsA and HC (16) or PsO (14). The latter study described an increased concentration of MMP3 in PsA sera compared to PsO, with a significant OR of 1.59 (95% CI=1.21-2.11); however, this disappeared after multivariate regression (14). In a recent study, serum MMP3 levels from PsA compared to PsO and HC were not significantly different. Only one study compared PsA and OA, and did not demonstrate any difference in serum levels of MMP3 (18).
In total, 6 studies compared serum MMP3 levels between PsA and HC (10, 13, 14, 16–18) and 4 studies compared levels between PsA and PsO (10, 13, 14, 16). The pooled results displayed a higher, but not significant, level of MMP3 in sera of PsA patients compared to HC (SMD=0.450, 95% CI=-0.080-0.981, p=0.096; Figure 3). MMP3 was significantly higher in PsA compared to PsO (SMD=0.419, 95% CI=0.119-0.719; p=0.006). Results were confirmed with sensitivity analyses. No significant SMD was found when pooled MMP3 levels of PsO and HC were compared (SMD=-0.118 [95% CI=-0.693-0.457], p=0.689).
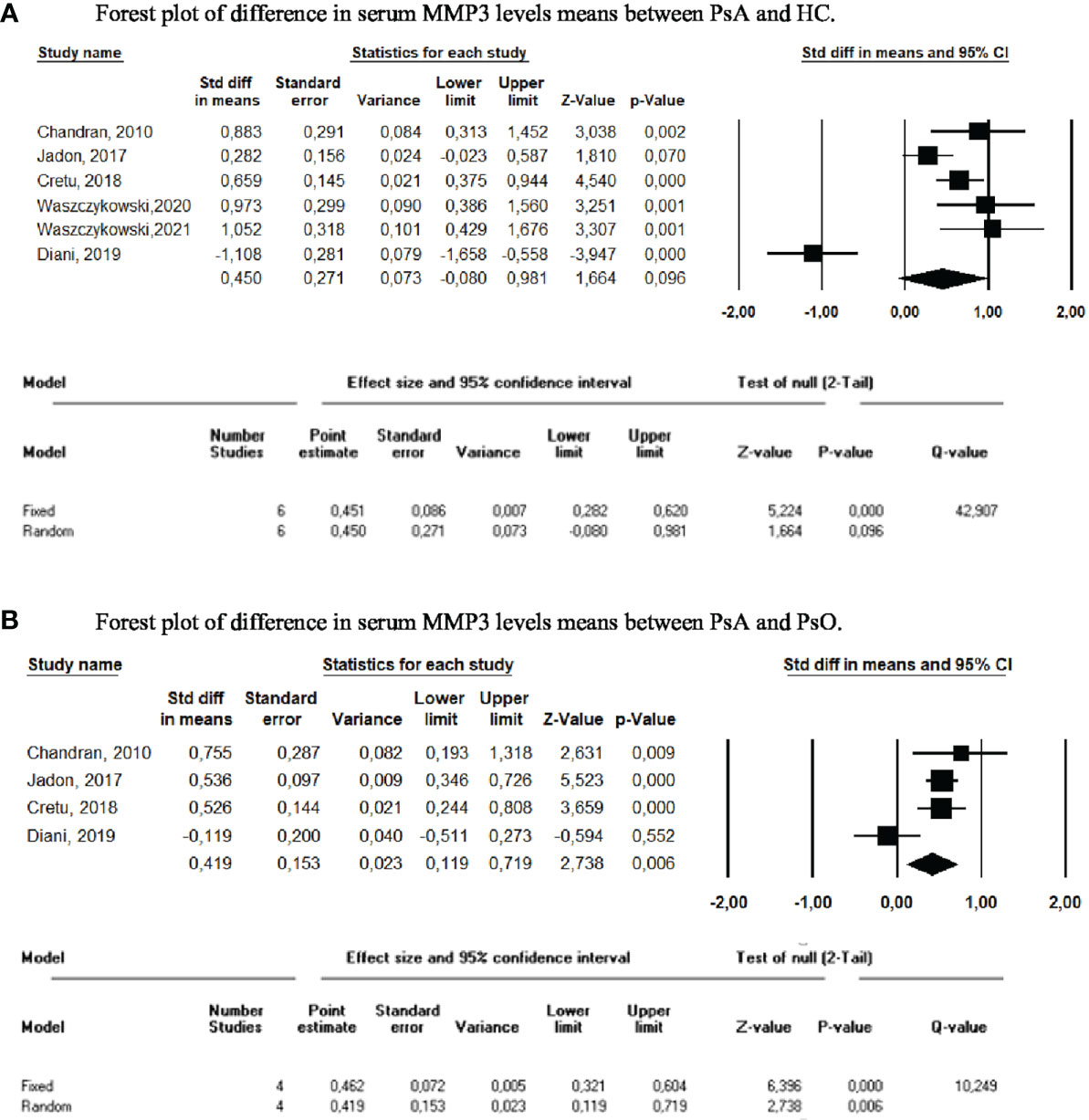
Figure 3 Meta-analysis of serum MMP3 levels. (A) Forest plot of difference in serum MMP3 levels means between PsA and HC. (B) Forest plot of difference in serum MMP3 levels means between PsA and PsO.
RANK-L was also assessed as a diagnostic biomarker in three studies. Two studies reported significantly higher serum RANK-L levels in PsA patients compared with HC (59, 134), whereas the remaining study observed the opposite (16). The same three studies also compared RANK-L levels between PsA and PsO, with little or no difference detected between the two populations. The only study reporting significantly higher levels in PsA patients concluded that RANK-L was inaccurate for differentiating PsA from PsO (AUC=0.66 [95% CI NA]) (59). In the meta-analysis of these three publications, comparison of RANKL levels between PsA and HC and between PsA and PsO (10, 16, 59), the SMDs were -0.106 (95% CI=-3.75 -3.36, p=0.952) and 0.315 (95% CI=-0.391-1.021, p=0.382), respectively (Figure 4). Results did not change upon performance of sensitivity analyses.
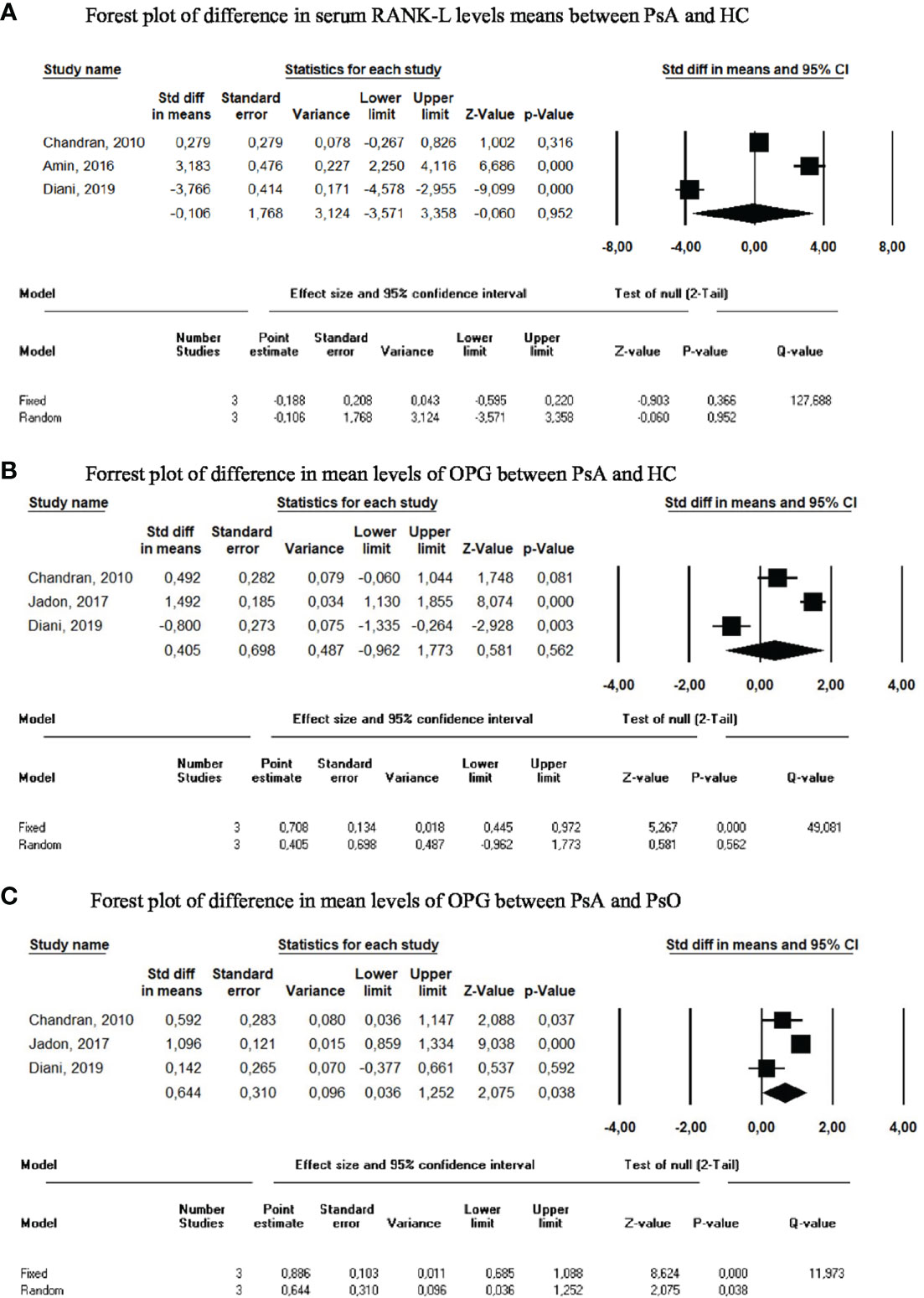
Figure 4 Meta-analysis of circulating biomarkers. (A) Forest plot of difference in serum RANK-L levels means between PsA and HC. (B) Forrest plot of difference in mean levels of OPG between PsA and HC. (C) Forrest plot of difference in mean levels of OPG between PsA and PsO.
OPG serum levels were significantly increased in a small PsA cohort (n=26 per group) compared with PsO and HC (10). However, levels were not different in a larger PsA cohort (n=200 per group) compared to PsO and HC (13), nor in another smaller PsA cohort (n=50) compared to PsO (n=50) and HC (n=20) (16). In our meta-analysis, we calculated an SMD of 0.405 (95%CI -0.962-1.773, p=0.562) when PsA was compared to HC, and an SMD of 0.644 (95%CI 0.036-1.252, p=0.038) when PsA was compared to PsO (Figure 4).
Dkk-1 serum levels were studied in two publications with opposing results (13, 16). After meta-analysis, SMD in Dkk-1 levels between PsA and HC was 3.22 (95% CI=-5.974-12.412, p=0.493; Figure 5). When patients with PsA were compared to patients with PsO, the SMD was 0.992 (95% CI=-0.89-2.87, p=0.301).
Human Leucocyte Antigen (HLA) was studied in 6 publications (19, 27–29, 35, 36). A family-based study reported an association between PsA and various HLA alleles: HLA-B*27, HLA-B*38, HLA-B*39, and HLA-C*12 (27). HLA-B*27 association with PsA was additionally described in a large cross-sectional study, while HLA-C*06 was found to be associated with skin damage and less prevalent musculoskeletal developmental phenotypes (28). Another study described an association between PsA and HLA-B*27, HLA haplotype C*12/B*38m and HLA-C*06/B*57 (29). Interestingly, HLA-B27 was not associated with PsA in the Jewish Israeli population (19), though HLA-A*01/A*01 and HLA-C*06/C*02 were risk alleles for PsA in the Chinese Han population (35).
Genetic polymorphisms were also explored in 9 different articles (20, 21, 24–26, 30, 31, 33, 41). Polymorphisms of the gene Il-13 were examined in two studies, which reported that rs1800925*C and rs20641*G were significantly associated with PsA in a PsO population (25, 26). However, one study reported the association between rs1800925 polymorphism and PsA only in the smoker population (26).
In our systematic literature review, autoantibodies were explored in 8 articles (43–50). They focused on different autoantibodies, preventing meta-analysis. Among these autoantibodies, those of interest are outlined below. It should be noted that none of these autoantibodies have been evaluated or validated in any additional PsA cohorts beyond those described here.
Anti-Cyclic citrullinated peptides (CCP) were present in some PsA patients (7.9%) (43). Anti-Mutated citrullinated vimentin (MCV) levels were significantly higher in PsA sera (24%) than PsO (8%) (45). The novel autoantibody named anti-PsA peptide was identified after screening of a random synthetic peptide library with pooled immunoglobulins derived from 30 patients with recent onset PsA. Anti-PsA shares a sequence homology with Nebullin Related Anchoring Protein (N-RAP) (46). A peptide corresponding to N-RAP sequence was synthetized and tested by ELISA. Anti-NRAP autoantibodies were recognized by 83% of PsA sera, versus 7% of rheumatoid arthritis (RA) anti-CCP positive, 4% of RA anti-CCP negative, 3.3% of PsO, and none of other rheumatic diseases included in this study (46).
Anti-A Disintegrin and MetalloproteinaSe with ThromboSpondin motifs 5 (ADAMSTS5) and anti-Cathelicidin LL37 (LL37) IgG autoantibodies were assessed for differentiating PsA from PsO. The ROC analysis reported an AUC of 0.84 (95% CI=NA, p<0.1) for anti-ADAMSTS5 autoantibodies and 0.87 (95% CI=NA, p<0.01) for anti-LL37 autoantibodies (49). Expression of Carbamethylated anti-LL37 was significantly higher in PsA sera (median=0.66, IQR=0.439) than PsO (median=0.43, IQR=0.47, p=0.02) and HC (median=0.158, IQR=0.099, p=0.0001) (48). Finally, higher IgA anti-oxidized collagen type II (oxPTMCII) autoantibodies were detected in PsA (84%, n=33/39) and axial spondyloarthritis (SpA, 47%, n=79/165) sera compared to HC (0%, n=0/28) (50).
Two additional biomarkers unrelated to the above categories were also assessed in at least 2 publications.
CXCL10 rates were overexpressed in synovial fluid of PsA versus gout or SpA, but rates were similar to those of RA (61). A prospective follow-up of patients with PsO reported both higher baseline serum CXCL10 levels in patients who subsequently developed PsA as compared with those who did not, and a significant decrease in CXCL10 levels from the year before to the year after PsA onset (70).
A serum calprotectin S100A8/S100A9 with a cut-off of 475 ng/mL was able to discriminate PsA from HC with a 93.3% specificity and 75.0% sensitivity (54). Serum calprotectin levels were increased in PsA but also in other inflammatory arthritis (RA, axial SpA) compared to controls (i.e., OA, fibromyalgia, and undifferentiated arthralgia), with good accuracy for distinguishing inflammatory arthritis from controls (AUC=0.964, 95% CI=NA) (65). Calprotectin levels in each subpopulation were not available for a meta-analysis.
Prognostic biomarkers, including markers of disease activity, were less frequently assessed than diagnostic biomarkers (Table 2). As such, the data collected were insufficient to perform meta-analyses.
One study concluded that erythrocyte sedimentation rate (ESR) was better correlated with Ritchie’s index, tender joint count (TJC) and swollen joint count (SJC) than C-Reactive Protein (CRP) in a 36 patient PsA cohort (84). These potential prognosis markers were explored in a 5-year follow-up prospective study. The 36 patients with PsA demonstrated a disease duration ranging from 1-40 years, and baseline ESR was associated with structural progression (85). Both ESR and CRP were also associated with UltraSonography (US) which are signs of active synovitis (86).
Serum COMP levels were correlated with acute phase reactants and disease activity (TJC, r=0.60, p<0.001) and SJC, r=0.75, p<0.0001) (18, 88). A decrease in MMP3 serum levels in PsA patients receiving adalimumab was correlated with Disease Activity Score (DAS)-28 improvement (90).
In a cross-sectional study, positivity for anti-CCP antibodies was associated with more radiographic damage and polyarticular phenotypes (95). Anti-LL37 autoantibodies were also described to correlate with disease activity in PsA (48). A strong correlation between Anti-Carbamethylated Protein (CarP) antibody levels and both clinical and ultrasonographic activity was described (correlation between anti-CarP and DAS-28 (r=0.96), CRP (r=0.97), ESR (r=0.97) and US power Doppler+synovitis with a Pearson coefficient >0.97) (96).
Calprotectin S100A8/A9 plasma levels were not correlated with disease activity (122, 126). Although, one study reported calprotectin S100A8/A9 levels significantly increased in the polyarticular phenotype of PsA, and were correlated with SJC (54). Contradictory results were reported regarding correlation with US synovitis in greyscale and power Doppler analyses (115, 122). High levels of calprotectin were also associated with relapse at 1-year (118).
Serum concentration of YKL40, also named Chitinase like-3 protein (Chi3L1) was significantly correlated with disease activity (r=0.848, p<0.001) (109). It was also sensitive to changes, with a significant decrease in serum of good responders to TNF inhibitor (106).
Our systematic review of the literature shows that few biomarkers are currently available to guide clinical practice in the diagnosis and prognosis of PsA. This review has highlighted COMP and MMP3 as two potential serum biomarkers for the diagnosis of PsA. However, the discriminative qualities of these bone and cartilage remodeling markers have been revealed as insufficient for clinical use.
The meta-analysis showed that COMP was able to differentiate patients with PsA from those with OA or from healthy subjects. However, serum levels varied widely between studies. One study reported mean COMP rates were 10-fold lower in the PsA, OA, and HC populations compared with those observed in the other studies, while methodologically, only the commercial ELISA kits differed between studies (15). The success of COMP in distinguishing PsA from PsO was different across studies, and the absence of numerical data prevented performance of a meta-analysis and to deduce its efficacy in this application.
The pooled serum MMP-3 levels were significantly higher in PsA patients than in PsO patients. However, the meta-analysis showed that they did not appropriately distinguish patients with PsA from healthy subjects. Similarly, the only publication that studied MMP3 serum levels in PsA and OA reported no difference between the two (134). MMP3 levels were increased in OA when compared to HC, but do not appear to be a reliable biomarker, particularly as their assessment in a multiplex system reported results contrary to those found in this analysis (i.e., lower MMP3 serum levels in patients with PsA and PsO than in healthy subjects) (16). None of the remaining bone remodeling or cartilage markers demonstrated any ability to differentiate patients with PsA from controls. However, all the studies included in the analysis were cross-sectional studies, with patients whose diagnosis was pre-existing and whose disease duration was not considered.
We have not identified any new genetic biomarkers useful in the diagnosis of PsA since the last meta-analyses on the subject, and these analyses on genetic polymorphisms had not identified any useful biomarkers for the practical diagnosis of PsA (135, 136). Our systematic review did not identify all publications on HLA and PsA association, which may be due to the fact that our search algorithm was not specifically focused on genetics. The major loci of interest have historically been MHC region and HLA genes, of which certain alleles, primarily HLA-C*06 and HLA-B*27, are carried by about 20-35% of PsA patients (137). Recently, HLA-B27 has been identified as a marker of the axial PsA phenotype, and HLA-C*06 as a marker of the peripheral PsA phenotype (138). Furthermore, both systematic review for PsA biomarkers and a recent meta-analysis examining HLA association in PsA patients confirmed a significant increase in the risk of PsA in HLA-C*02 and C*12 populations (139, 140). Specific non-HLA PsA variants have been identified in GWAS studies, including in the IL12B, NOS2 and IFIH1 regions as reported in a systematic review published in 2015 (141). Several signaling pathways possibly implicated in the pathogenesis of PsA were presented in a recent systematic review published in 2020 (142).
Data concerning autoantibodies in PsA remains sparse in the literature. While some data appears promising, no replication studies have been published. Anti-CCP antibodies are associated with polyarticular phenotypes and structural lesions, and have been shown to be markers of severity rather than diagnosis. Indeed, a recent study reported a correlation between anti-CCP antibodies in PsA and pulmonary manifestations (143).
This systematic review of the literature has several limitations. Only patients with PsA were included while studies involving patients with SpA were excluded, which may have incidentally excluded patients with psoriatic forms of axial disease. The search algorithm also did not include imaging biomarkers, although combining imaging with other biomarkers might help to better define PsA (144). In addition, we choose to focus on diagnosis and prognosis biomarkers unrelated to treatment and did not include predictive biomarkers of treatment response. Finally, our search equation did not allow us to highlight the numerous studies concerning genetics biomarkers in psoriatic arthritis either and should be a focus of a future systemic review.
In summary, this review was broad, with more than 50 studies included since the prior systematic review on diagnostic and prognostic biomarkers in PsA (139). No specific diagnostic biomarkers for PsA were identified, despite the fact that this was the first meta-analyses to assess COMP and MMP3. The search for autoantibodies in PsA appears promising but requires additional confirmatory studies. Further studies are also needed to assess the performance of potential biomarkers that can distinguish PsA from OA and other chronic inflammatory diseases.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
TW: conception and design of the study, acquisition of data, analysis of data, original draft preparation, data curation, reviewing and editing. NB: conception and design of the study, editing LB: analysis of data, stats PL: editing, supervision TP: conception and design of the study, analysis of data, drafting manuscript, supervision, reviewing and editing All authors reviewed and approved the final draft of the manuscript.
Mrs. Catherine Weill assisted with the Embase bibliographic research. JetPub Scientific Communications LLC provided editorial assistance to the authors during preparation of this manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Scotti L, Franchi M, Marchesoni A, Corrao G. Prevalence and incidence of psoriatic arthritis: A systematic review and meta-analysis. Semin Arthritis Rheumatol (2018) 48(1):28–34. doi: 10.1016/j.semarthrit.2018.01.003
2. Mease PJ, Gladman DD, Papp KA, Khraishi MM, Thaçi D, Behrens F, et al. Prevalence of rheumatologist-diagnosed psoriatic arthritis in patients with psoriasis in European/North American dermatology clinics. J Am Acad Dermatol (2013) 69(5):729–35. doi: 10.1016/j.jaad.2013.07.023
3. Taylor WJ. Impact of psoriatic arthritis on the patient: Through the lens of the WHO international classification of functioning, health, and disability. Curr Rheumatol Rep (2012) 14(4):369–74. doi: 10.1007/s11926-012-0263-5
4. Ritchlin CT, Colbert RA, Gladman DD. Psoriatic arthritis. N Engl J Med (2017) 376(10):957–70. doi: 10.1056/nejmra1505557.
5. Duffin KC, FitzGerald O, Kavanaugh A, Mease PJ, Merola JF, Ogdie A, et al. GRAPPA 2017 project report. J Rheumatol Suppl (2018) 94:48–51. doi: 10.3899/jrheum.180139
6. Atkinson AJ, Colburn WA, DeGruttola VG, DeMets DL, Downing GJ, Hoth DF, et al. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther (2001) 69(3):89–95. doi: 10.1067/mcp.2001.113989
7. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev (2021) 10(1):1–11. doi: 10.1186/s13643-021-01626-4
8. Månsson B, Gülfe A, Geborek P, Heinegård D, Saxne T. Release of cartilage and bone macromolecules into synovial fluid: differences between psoriatic arthritis and rheumatoid arthritis. Ann Rheum Dis (2001) 60(1):27–31. doi: 10.1136/ard.60.1.27
9. Farouk HM, Mostafa AAA, Youssef SS, Elbeblawy MMS, Assaf NY, Elokda ESE. Value of entheseal ultrasonography and serum cartilage oligomeric matrix protein in the preclinical diagnosis of psoriatic arthritis. Clin Med Insights Arthritis Musculoskelet Disord (2010) 3:7–14. doi: 10.4137/CMAMD.S4461
10. Chandran V, Cook RJ, Edwin J, Shen H, Pellett FJ, Shanmugarajah S, et al. Soluble biomarkers differentiate patients with psoriatic arthritis from those with psoriasis without arthritis. Rheumatology (2010) 49(7):1399–405. doi: 10.1093/rheumatology/keq105
11. Cretu D, Prassas I, Saraon P, Batruch I, Gandhi R, Diamandis EP, et al. Identification of psoriatic arthritis mediators in synovial fluid by quantitative mass spectrometry. Clin Proteomics (2014) 11(1):1–12. doi: 10.1186/1559-0275-11-27
12. Dolcino M, Ottria A, Barbieri A, Patuzzo G, Tinazzi E, Argentino G, et al. Gene expression profiling in peripheral blood cells and synovial membranes of patients with psoriatic arthritis. PloS One (2015) 10(6):e0128262. doi: 10.1371/journal.pone.0128262
13. Jadon DR, Sengupta R, Nightingale A, Lu H, Dunphy J, Green A, et al. Serum bone-turnover biomarkers are associated with the occurrence of peripheral and axial arthritis in psoriatic disease: A prospective cross-sectional comparative study. Arthritis Res Ther (2017) 19(1):1–10. doi: 10.1186/s13075-017-1417-7
14. Cretu D, Gao L, Liang K, Soosaipillai A, Diamandis EP, Chandran V. Differentiating psoriatic arthritis from psoriasis without psoriatic arthritis using novel serum biomarkers. Arthritis Care Res (2018) 70(3):454–61. doi: 10.1002/acr.23298
15. Chandran V, Abji F, Perruccio AR, Gandhi R, Li S, Cook RJ, et al. Serum-based soluble markers differentiate psoriatic arthritis from osteoarthritis. Ann Rheum Dis (2019) 78(6):796–801. doi: 10.1136/annrheumdis-2018-214737
16. Diani M, Perego S, Sansoni V, Bertino L, Gomarasca M, Faraldi M, et al. Differences in osteoimmunological biomarkers predictive of psoriatic arthritis among a Large Italian cohort of psoriatic patients. Int J Mol Sci (2019) 20(22):5617. doi: 10.3390/ijms20225617
17. Waszczykowski M, Bednarski I, Narbutt J, Waszczykowska E, Lesiak A, Fabiś J. Interleukin-18, interleukin-20, and matrix metalloproteinases (MMP-1, MMP-3) as markers of psoriatic arthritis disease severity and their correlations with biomarkers of inflammation and turnover of joint cartilage. Adv Dermatol Allergology/Postępy Dermatologii i Alergologii (2020) 37(6):1001–8. doi: 10.5114/ada.2020.94903
18. Waszczykowski M, Fabiś-Strobin A, Bednarski I, Lesiak A, Narbutt J, Fabiś J. Serum biomarkers of inflammation and turnover of joint cartilage can help differentiate psoriatic arthritis (PsA) patients from osteoarthritis (OA) patients. Diagnostics (2021) 11(1):52. doi: 10.3390/diagnostics11010052
19. Elkayam O, Segal R, Caspi D. Human leukocyte antigen distribution in Israeli patients with psoriatic arthritis. Rheumatol Int (2004) 24(2):93–7. doi: 10.1007/s00296-003-0325-0
20. Alenius GM, Friberg C, Nilsson S, Wahlström J, Dahlqvist SR, Samuelsson L. Analysis of 6 genetic loci for disease susceptibility in psoriatic arthritis. J Rheumatol (2004) 31(11):2230–5.
21. Ravindran JS, Owen P, Lagan A, Lewis J, Korendowych E, Welsh K, et al. Interleukin 1α, interleukin 1β and interleukin 1 receptor gene polymorphisms in psoriatic arthritis. Rheumatology (2004) 43(1):22–6. doi: 10.1093/rheumatology/keg443
22. Batliwalla FM, Li W, Ritchlin CT, Xiao X, Brenner M, Laragione T, et al. Microarray analyses of peripheral blood cells identifies unique gene expression signature in psoriatic arthritis. Mol Med (2005) 11(1–12):21–9. doi: 10.2119/2006-00003.Gulko
23. Stoeckman AK, Baechler EC, Ortmann WA, Behrens TW, Michet CJ, Peterson EJ. A distinct inflammatory gene expression profile in patients with psoriatic arthritis. Genes Immun (2006) 7(7):583–91. doi: 10.1038/sj.gene.6364334
24. Butt C, Lim S, Greenwood C, Rahman P. VEGF, FGF1, FGF2 and EGF gene polymorphisms and psoriatic arthritis. BMC Musculoskelet Disord (2007) 8(1):1–7. doi: 10.1186/1471-2474-8-1
25. Bowes J, Eyre S, Flynn E, Ho P, Salah S, Warren RB, et al. Evidence to support IL-13 as a risk locus for psoriatic arthritis but not psoriasis vulgaris. Ann Rheum Dis (2011) 70(6):1016–9. doi: 10.1136/ard.2010.143123
26. Eder L, Chandran V, Pellett F, Pollock R, Shanmugarajah S, Rosen CF, et al. IL13 gene polymorphism is a marker for psoriatic arthritis among psoriasis patients. Ann Rheum Dis (2011) 70(9):1594–8. doi: 10.1136/ard.2010.147421
27. Eder L, Chandran V, Pellett F, Shanmugarajah S, Rosen CF, Bull SB, et al. Differential human leucocyte allele association between psoriasis and psoriatic arthritis: a family-based association study. Ann Rheum Dis (2012) 71(8):1361–5. doi: 10.1136/annrheumdis-2012-201308
28. Winchester R, Minevich G, Steshenko V, Kirby B, Kane D, Greenberg DA, et al. HLA associations reveal genetic heterogeneity in psoriatic arthritis and in the psoriasis phenotype. Arthritis Rheum (2012) 64(4):1134–44. doi: 10.1002/art.33415
29. Chandran V, Bull SB, Pellett FJ, Ayearst R, Rahman P, Gladman DD. Human leukocyte antigen alleles and susceptibility to psoriatic arthritis. Hum Immunol (2013) 74(10):1333–8. doi: 10.1016/j.humimm.2013.07.014
30. Chandran V, Bull SB, Pellett FJ, Ayearst R, Pollock RA, Gladman DD. Killer-cell immunoglobulin-like receptor gene polymorphisms and susceptibility to psoriatic arthritis. Rheumatology (2014) 53(2):233–9. doi: 10.1093/rheumatology/ket296
31. Zhang Z, Yuan J, Tian Z, Xu J, Lu Z. Investigation of 36 non-HLA (human leucocyte antigen) psoriasis susceptibility loci in a psoriatic arthritis cohort. Arch Dermatol Res (2017) 309(2):71–7. doi: 10.1007/s00403-016-1706-z
32. Ciancio G, Ferracin M, Saccenti E, Bagnari V, Farina I, Furini F, et al. Characterisation of peripheral blood mononuclear cell microRNA in early onset psoriatic arthritis. Clin Exp Rheumatol (2017) 35:113–21.
33. Cascella R, Strafella C, Ragazzo M, Manzo L, Costanza G, Bowes J, et al. KIF3A and IL-4 are disease-specific biomarkers for psoriatic arthritis susceptibility. Oncotarget (2017) 8(56):95401. doi: 10.18632/oncotarget.20727
34. Abji F, Pollock RA, Liang K, Chandran V, Gladman DD. Th17 gene expression in psoriatic arthritis synovial fluid and peripheral blood compared to osteoarthritis and cutaneous psoriasis. Clin Exp Rheumatol (2017) 36(3):486–9.
35. Chen J, Yang F, Zhang Y, Fan X, Xiao H, Qian W, et al. HLA-A*01:01 in MHC is associated with psoriatic arthritis in Chinese han population. Arch Dermatol Res (2019) 311(4):277–85. doi: 10.1007/s00403-019-01902-3
36. Smith MP, Ly K, Thibodeaux Q, Beck K, Yang E, Sanchez I, et al. Evaluation of a genetic risk score for diagnosis of psoriatic arthritis. J Psoriasis Psoriatic Art (2020) 5(2):61–7. doi: 10.1177/2475530320910814
37. Caputo V, Strafella C, Termine A, Campione E, Bianchi L, Novelli G, et al. RNAseq-based prioritization revealed COL6A5, COL8A1, COL10A1 and MIR146A as common and differential susceptibility biomarkers for psoriasis and psoriatic arthritis: Confirmation from genotyping analysis of 1417 Italian subjects. Int J Mol Sci (2020) 21(8):2740. doi: 10.3390/ijms21082740
38. Lin SH, Ho JC, Li SC, Cheng YW, Yang YC, Chen JF, et al. Upregulation of miR-941 in circulating CD14+ monocytes enhances osteoclast activation via WNT16 inhibition in patients with psoriatic arthritis. Int J Mol Sci (2020) 21(12):4301. doi: 10.3390/ijms21124301
39. Pasquali L, Svedbom A, Srivastava A, Rosén E, Lindqvist U, Ståhle M, et al. Circulating microRNAs in extracellular vesicles as potential biomarkers for psoriatic arthritis in patients with psoriasis. J Eur Acad Dermatol Venereology (2020) 34(6):1248–56. doi: 10.1111/jdv.16203
40. Wade SM, McGarry T, Wade SC, Fearon U, Veale DJ. Serum MicroRNA signature as a diagnostic and therapeutic marker in patients with psoriatic arthritis. J Rheumatol (2020) 47(12):1760–7. doi: 10.3899/jrheum.190602
41. Iwaszko M, Wielińska J, Świerkot J, Kolossa K, Sokolik R, Bugaj B, et al. IL-33 gene polymorphisms as potential biomarkers of disease susceptibility and response to TNF inhibitors in rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis patients. Front Immunol (2021) 12:2168. doi: 10.3389/fimmu.2021.631603
42. Cheleschi S, Tenti S, Bedogni G, Fioravanti A. Circulating mir-140 and leptin improve the accuracy of the differential diagnosis between psoriatic arthritis and rheumatoid arthritis: a case-control study. Trans Res (2022) 239:18–34. doi: 10.1016/j.trsl.2021.08.001
43. Calzavara-Pinton PG, Franceschini F, Manera C, Zane C, Prati E. Incidence of antiperinuclear factor in patients with psoriatic arthritis. Adv Exp Med Biol (1999) 455:215–20. doi: 10.1007/978-1-4615-4857-7_31
44. Chou CL, Wu MJ, Yu CL, Lu MC, Hsieh SC, Wu TH, et al. Anti-agalactosyl IgG antibody in ankylosing spondylitis and psoriatic arthritis. Clin Rheumatol (2010) 29(8):875–81. doi: 10.1007/s10067-010-1413-7
45. Dalmády S, Kiss M, Képíró L, Kovács L, Sonkodi G, Kemény L, et al. Higher levels of autoantibodies targeting mutated citrullinated vimentin in patients with psoriatic arthritis than in patients with psoriasis vulgaris. Clin Dev Immunol (2013) 2013:474028. doi: 10.1155/2013/474028
46. Dolcino M, Lunardi C, Ottria A, Tinazzi E, Patuzzo G, Puccetti A. Crossreactive autoantibodies directed against cutaneous and joint antigens are present in psoriatic arthritis. PloS One (2014) 9(12):e115424. doi: 10.1371/journal.pone.0115424
47. Hu Q, Sun Y, Li Y, Shi H, Teng J, Liu H, et al. Anti-SIRT1 autoantibody is elevated in ankylosing spondylitis: A potential disease biomarker. BMC Immunol (2018) 19(1):1–8. doi: 10.1186/s12865-018-0280-x
48. Frasca L, Palazzo R, Chimenti MS, Alivernini S, Tolusso B, Bui L, et al. Anti-LL37 antibodies are present in psoriatic arthritis (PsA) patients: New biomarkers in PsA. Front Immunol (2018) 9(SEP):1936. doi: 10.3389/fimmu.2018.01936
49. Yuan Y, Qiu J, Lin ZT, Li W, Haley C, Mui UN, et al. Identification of novel autoantibodies associated with psoriatic arthritis. Arthritis Rheumatol (2019) 71(6):941–51. doi: 10.1002/art.40830
50. Vinci C, Infantino M, Raturi S, Tindell A, Topping LM, Strollo R, et al. Immunoglobulin a antibodies to oxidized collagen type II as a potential biomarker for the stratification of spondyloarthritis from rheumatoid arthritis. Scandinavian J Rheumatol (2020) 49(4):281–91. doi: 10.1080/03009742.2020.1713395
51. Veale D, Yanni G, Rogers S, Barnes L, Bresnihan B, Fitzgerald O. Reduced synovial membrane macrophage numbers, elam-1 expression, and lining layer hyperplasia in psoriatic arthritis as compared with rheumatoid arthritis. Arthritis Rheum (1993) 36(7):893–900. doi: 10.1002/art.1780360705
52. Szodoray P, Alex P, Chappell-Woodward CM, Madland TM, Knowlton N, Dozmorov I, et al. Circulating cytokines in Norwegian patients with psoriatic arthritis determined by a multiplex cytokine array system. Rheumatology (2007) 46(3):417–25. doi: 10.1093/rheumatology/kel306
53. Firuzi O, Spadaro A, Spadaro C, Riccieri V, Petrucci R, Marrosu G, et al. Protein oxidation markers in the serum and synovial fluid of psoriatic arthritis patients. J Clin Lab Anal (2008) 22(3):210–5. doi: 10.1002/jcla.20243
54. Hansson C, Eriksson C, Alenius GM. S-calprotectin (S100A8/S100A9): A potential marker of inflammation in patients with psoriatic arthritis. J Immunol Res (2014) 2014:696415. doi: 10.1155/2014/696415
55. Bosè F, Capsoni F, Molteni S, Raeli L, Diani M, Altomare A, et al. Differential expression of interleukin-2 by anti-CD3-stimulated peripheral blood mononuclear cells in patients with psoriatic arthritis and patients with cutaneous psoriasis. Clin Exp Dermatol (2014) 39(3):385–90. doi: 10.1111/ced.12251
56. Maejima H, Nagashio R, Yanagita K, Hamada Y, Amoh Y, Sato Y, et al. Moesin and stress-induced phosphoprotein-1 are possible sero-diagnostic markers of psoriasis. PloS One (2014) 9(7):e101773. doi: 10.1371/journal.pone.0101773
57. Kim DS, Shin D, Lee MS, Kim HJ, Kim DY, Kim SM, et al. Assessments of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in Korean patients with psoriasis vulgaris and psoriatic arthritis. J Dermatol (2016) 43(3):305–10. doi: 10.1111/1346-8138.13061
58. Armas-González E, Díaz-Martín A, Domínguez-Luis MJ, Arce-Franco MT, Herrera-García A, Hernández-Hernández MV, et al. Differential antigen-presenting b cell phenotypes from synovial microenvironment of patients with rheumatoid and psoriatic arthritis. J Rheumatol (2015) 42(10):1825–34. doi: 10.3899/jrheum.141577
59. Amin TE, Elfar NN, Ghaly NR, Hekal MM, Hassan AM, Elsaadany HM. Serum level of receptor activator of nuclear factor kappa-b ligand in patients with psoriasis. Int J Dermatol (2016) 55(5):e227–33. doi: 10.1111/ijd.13159
60. Gudmann NS, Munk HL, Christensen AF, Ejstrup L, Sørensen GL, Loft AG, et al. Chondrocyte activity is increased in psoriatic arthritis and axial spondyloarthritis. Arthritis Res Ther (2016) 18(1):1–9. doi: 10.1186/s13075-016-1040-z
61. Muntyanu A, Abji F, Liang K, Pollock RA, Chandran V, Gladman DD. Differential gene and protein expression of chemokines and cytokines in synovial fluid of patients with arthritis. Arthritis Res Ther (2016) 18(1):1–10. doi: 10.1186/s13075-016-1196-6
62. Abji F, Pollock RA, Liang K, Chandran V, Gladman DD. Brief report: CXCL10 is a possible biomarker for the development of psoriatic arthritis among patients with psoriasis. Arthritis Rheumatol (2016) 68(12):2911–6. doi: 10.1002/art.39800
63. Reindl J, Pesek J, Krüger T, Wendler S, Nemitz S, Muckova P, et al. Proteomic biomarkers for psoriasis and psoriasis arthritis. J Proteomics. (2016) 140:55–61. doi: 10.1016/j.jprot.2016.03.040
64. Alonso A, Julià A, Vinaixa M, Domènech E, Fernández-Nebro A, Cañete JD, et al. Urine metabolome profiling of immune-mediated inflammatory diseases. BMC Med (2016) 14(1):133. doi: 10.1186/s12916-016-0681-8
65. Grossi V, Infantino M, Manfredi M, Meacci F, Bellio E, Bellio V, et al. A proposed serum calprotectin IgG cut-off level for diagnosing inflammatory arthritis. Curr Rheumatol Rev (2017) 13(2):93–97. doi: 10.2174/1573397112666160629085231
66. Ausavarungnirun R, Intarasupht J, Nakakes A, Rojanametin K. Nail abnormalities, quality of life and serum inflammatory marker in psoriatic arthritis compare to psoriasis without arthritis. J Med Assoc Thai (2017) 100:1021.
67. Maejima H, Kobayashi M, Yanagita K, Hamada Y, Nagashio R, Sato Y, et al. Valosin-containing protein is a possible sero-diagnostic marker of psoriatic arthritis. Biomed Res (2017) 28(1):442–6.
68. Farrag DA, Asaad MK, Ghobrial CK. Evaluation of IL-34 in psoriasis and psoriatic arthritis patients: Correlation with disease activity and severity. Egyptian Rheumatologist. (2017) 39(1):25–31. doi: 10.1016/j.ejr.2016.05.008
69. Sinkeviciute D, Skovlund Groen S, Sun S, Manon-Jensen T, Aspberg A, Önnerfjord P, et al. A novel biomarker of MMP-cleaved prolargin is elevated in patients with psoriatic arthritis. Sci Rep (2020) 10(1):1–10. doi: 10.1038/s41598-020-70327-0
70. Abji F, Lee KA, Pollock RA, Machhar R, Cook RJ, Chandran V, et al. Declining levels of serum chemokine (C-X-C motif) ligand 10 over time are associated with new onset of psoriatic arthritis in patients with psoriasis: a new biomarker? Br J Dermatol (2020) 183(5):920–7. doi: 10.1111/bjd.18940
71. Esawy MM, Makram WK, Albalat W, Shabana MA. Plasma gelsolin levels in patients with psoriatic arthritis: a possible novel marker. Clin Rheumatol (2020) 39(6):1881–8. doi: 10.1007/s10067-020-04959-y
72. Souto-Carneiro M, Tóth L, Behnisch R, Urbach K, Klika KD, Carvalho RA, et al. Differences in the serum metabolome and lipidome identify potential biomarkers for seronegative rheumatoid arthritis versus psoriatic arthritis. Ann Rheum Dis (2020) 79(4):499–506. doi: 10.1136/annrheumdis-2019-216374
73. Cuervo A, Celis R, Julià A, Usategui A, Faré R, Ramírez J, et al. Synovial immunohistological biomarkers of the classification of undifferentiated arthritis evolving to rheumatoid or psoriatic arthritis. Front Med (Lausanne). (2021) 8:417. doi: 10.3389/fmed.2021.656667
74. Leijten E, Tao W, Pouw J, van Kempen T, Olde Nordkamp M, Balak D, et al. Broad proteomic screen reveals shared serum proteomic signature in patients with psoriatic arthritis and psoriasis without arthritis. Rheumatology (2021) 60(2):751–61. doi: 10.1093/rheumatology/keaa405
75. Kishikawa T, Arase N, Tsuji S, Maeda Y, Nii T, Hirata J, et al. Large-Scale plasma-metabolome analysis identifies potential biomarkers of psoriasis and its clinical subtypes. J Dermatol Sci (2021) 102(2):78–84. doi: 10.1016/j.jdermsci.2021.03.006
76. Fuentelsaz-Romero S, Cuervo A, Estrada-Capetillo L, Celis R, García-Campos R, Ramírez J, et al. GM-CSF expression and macrophage polarization in joints of undifferentiated arthritis patients evolving to rheumatoid arthritis or psoriatic arthritis. Front Immunol (2021) 11:3940. doi: 10.3389/fimmu.2020.613975
77. Zhu J, Han L, Liu R, Zhang Z, Huang Q, Fang X, et al. Identification of proteins associated with development of psoriatic arthritis in peripheral blood mononuclear cells: a quantitative iTRAQ-based proteomics study. J Transl Med (2021) 19(1):1–9. doi: 10.1186/s12967-021-03006-x
78. Looby N, Roszkowska A, Reyes-Garcés N, Yu M, Bączek T, Kulasingam V, et al. Serum metabolic fingerprinting of psoriasis and psoriatic arthritis patients using solid-phase microextraction–liquid chromatography–high-resolution mass spectrometry. Metabolomics (2021) 17(7):1–12. doi: 10.1007/s11306-021-01805-3
79. Leijten EF, van Kempen TS, Olde Nordkamp MA, Pouw JN, Kleinrensink NJ, Vincken NL, et al. Tissue-resident memory CD8+ T cells from skin differentiate psoriatic arthritis from psoriasis. Arthritis Rheumatol (2021) 73(7):1220–32. doi: 10.1002/art.41652
80. Ek WE, Karlsson T, Höglund J, Rask-Andersen M, Johansson Å. Causal effects of inflammatory protein biomarkers on inflammatory diseases. Sci Adv (2021) 7(50):4359. doi: 10.1126/sciadv.abl4359
81. Wang N, Yang L, Shang L, Liang Z, Wang Y, Feng M, et al. Altered fecal metabolomics and potential biomarkers of psoriatic arthritis differing from rheumatoid arthritis. Front Immunol (2022) 13. doi: 10.3389/fimmu.2022.812996
82. Marzaioli V, Canavan M, Floudas A, Flynn K, Mullan R, Veale DJ, et al. CD209/CD14+ dendritic cells characterization in rheumatoid and psoriatic arthritis patients: Activation, synovial infiltration, and therapeutic targeting. Front Immunol (2022) 12. doi: 10.3389/fimmu.2021.722349
83. Mc Ardle A, Kwasnik A, Szentpetery A, Hernandez B, Parnell A, de Jager W, et al. Identification and evaluation of serum protein biomarkers that differentiate psoriatic arthritis from rheumatoid arthritis. Arthritis Rheumatol (2022) 74(1):81–91. doi: 10.1002/art.41899
84. Helliwell PS, Marchesoni A, Peters M, Platt R, Wright V. Cytidine deaminase activity, c reactive protein, histidine, and erythrocyte sedimentation rate as measures of disease activity in psoriatic arthritis. Ann Rheum Dis (1991) 50(6):362–5. doi: 10.1136/ard.50.6.362
85. McHugh NJ, Balachrishnan C, Jones SM. Progression of peripheral joint disease in psoriatic arthritis: a 5-yr prospective study. Rheumatology (2003) 42(6):778–83. doi: 10.1093/rheumatology/keg217
86. Bandinelli F, Denaro V, Prignano F, Collaku L, Ciancio G, Matucci-Cerinic M, et al. Ultrasonographic wrist and hand abnormalities in early psoriatic arthritis patients: correlation with clinical, dermatological, serological and genetic indices. Clin Exp Rheumatol (2015) 33(3):330–5.
87. Foell D, Kane D, Bresnihan B, Vogl T, Nacken W, Sorg C, et al. Expression of the pro-inflammatory protein S100A12 (EN-RAGE) in rheumatoid and psoriatic arthritis. Rheumatology (2003) 42(11):1383–9. doi: 10.1093/rheumatology/keg385
88. Skoumal M, Haberhauer G, Fink A, Steiner A, Klingler A, Varga F, et al. Increased serum levels of cartilage oligomeric matrix protein in patients with psoriasis vulgaris: a marker for unknown peripheral joint involvement? Clin Exp Rheumatol (2008) 26(6):1087–90.
89. Dalbeth N, Pool B, Smith T, Callon KE, Lobo M, Taylor WJ, et al. Circulating mediators of bone remodeling in psoriatic arthritis: Implications for disordered osteoclastogenesis and bone erosion. Arthritis Res Ther (2010) 12(4):1–9. doi: 10.1186/ar3123
90. van Kuijk AWR, DeGroot J, Koeman RC, Sakkee N, Baeten DL, Gerlag DM, et al. Soluble biomarkers of cartilage and bone metabolism in early proof of concept trials in psoriatic arthritis: effects of adalimumab versus placebo. PloS One (2010) 5(9):1–5. doi: 10.1371/journal.pone.0012556
91. Ramonda R, Modesti V, Ortolan A, Scanu A, Bassi N, Oliviero F, et al. Serological markers in psoriatic arthritis: promising tools. Exp Bio Med (2013) 238(12):1431–6. doi: 10.1177/1535370213506435
92. Chung Y, Li ZC, Sun XL, Liu YY, Shao M, Gan YZ, et al. Elevated serum dickkopf-1 is a biomarker for bone erosion in patients with psoriatic arthritis. Chin Med J (2021) 134(21):2583–8. doi: 10.1097/CM9.0000000000001612
93. Alenius GM, Jidell E, Nordmark L, Rantapää Dahlqvist S. Disease manifestations and HLA antigens in psoriatic arthritis in northern Sweden. Clin Rheumatol (2002) 21(5):357–62. doi: 10.1007/s100670200097
94. Korendowych E, Owen P, Ravindran J, Carmichael C, McHugh N. The clinical and genetic associations of anti-cyclic citrullinated peptide antibodies in psoriatic arthritis. Rheumatology (2005) 44(8):1056–60. doi: 10.1093/rheumatology/keh686
95. Perez-Alamino R, Garcia-Valladares I, Cuchacovich R, Iglesias-Gamarra A, Espinoza LR. Are anti-CCP antibodies in psoriatic arthritis patients a biomarker of erosive disease? Rheumatol Int (2014) 34(9):1211–6. doi: 10.1007/s00296-014-2956-8
96. Ibrahim SE, Morshedy NA, Farouk N, Louka AL. Anti-carbamylated protein antibodies in psoriatic arthritis patients: Relation to disease activity, severity and ultrasonographic scores. Egyptian Rheumatologist. (2018) 40(1):17–21. doi: 10.1016/j.ejr.2017.08.002
97. Elkayam O, Yaron I, Shirazi I, Yaron M, Caspi D. Serum levels of hyaluronic acid in patients with psoriatic arthritis. Clin Rheumatol (2000) 19(6):455–7. doi: 10.1007/s100670070005
98. Elkayam O, Yaron I, Shirazi I, Yaron M, Caspi D. Serum levels of IL-10, IL-6, IL-1ra, and sIL-2R in patients with psoriatic arthritis. Rheumatol Int (2000) 19(3):101–5. doi: 10.1007/s002960050111
99. Rooney T, Murphy E, Benito M, Roux-Lombard P, FitzGerald O, Dayer JM, et al. Synovial tissue interleukin-18 expression and the response to treatment in patients with inflammatory arthritis. Ann Rheum Dis (2004) 63(11):1393–8. doi: 10.1136/ard.2003.016428
100. Fink AM, Cauza E, Hassfeld W, Dunky A, Bayer PM, Jurecka W, et al. Vascular endothelial growth factor in patients with psoriatic arthritis. Clin Exp Rheumatol (2007) 25(2):305–8.
101. Madland TM, Larsen A, Brun JG. S100 proteins calprotectin and S100A12 are related to radiographic changes rather than disease activity in psoriatic arthritis with low disease activity. J Rheumatol (2007) 34(10):2089–92.
102. Alenius GM, Eriksson C, Rantapää Dahlqvist S. Interleukin-6 and soluble interleukin-2 receptor alpha-markers of inflammation in patients with psoriatic arthritis? Clin Exp Rheumatol (2009) 27(1):120–3.
103. Pongratz G, Straub RH, Schölmerich J, Fleck M, Härle P. Serum BAFF strongly correlates with PsA activity in male patients only–is there a role for sex hormones? Clin Exp Rheumatol (2010) 28(6):813–9.
104. Celis R, Planell N, Fernández-Sueiro JL, Sanmartí R, Ramírez J, González-Álvaro I, et al. Synovial cytokine expression in psoriatic arthritis and associations with lymphoid neogenesis and clinical features. Arthritis Res Ther (2012) 14(2):1–9. doi: 10.1186/ar3817
105. Przepiera-Będzak H, Fischer K, Brzosko M, Reumatologii K, Wewnętrznych C. Serum levels of angiogenic cytokines in psoriatic arthritis and SAPHO syndrome. Polish Arc Int Med (2013) 123:Pol Arch Med Wewn. doi: 10.20452/pamw.1772
106. Jensen P, Wiell C, Milting K, Poggenborg RP, Østergaard M, Johansen JS, et al. Plasma YKL-40: a potential biomarker for psoriatic arthritis? J Eur Acad Dermatol Venereol (2013) 27(7):815–9. doi: 10.1111/j.1468-3083.2012.04570.x
107. Eissa A, Cretu D, Soosaipillai A, Thavaneswaran A, Pellett F, Diamandis A, et al. Serum kallikrein-8 correlates with skin activity, but not psoriatic arthritis, in patients with psoriatic disease. Clin Chem Lab Med (2013) 51(2):317–25. doi: 10.1515/cclm-2012-0251/html
108. Kayikçi Ö, Pamuk ÖN, Pamuk GE, Arican Ö, Dönmez S. T Helper 17 cytokine profile in psoriatic arthritis and their relations with clinical findings. Yeni Tıp Dergisi (2014) 31(3):163–7.
109. Ahmed SF, Attia EAS, Saad AA, Sharara M, Fawzy H, el Nahrery EMA. Serum YKL-40 in psoriasis with and without arthritis; correlation with disease activity and high-resolution power Doppler ultrasonographic joint findings. J Eur Acad Dermatol Venereology (2015) 29(4):682–8. doi: 10.1111/jdv.12653
110. Husakova M, Lippert J, Stolfa J, Sedova L, Arenberger P, Lacinova Z, et al. Elevated serum prolactin levels as a marker of inflammatory arthritis in psoriasis vulgaris. BioMed Pap Med Fac Univ Palacky Olomouc Czech Repub (2015) 159(4):562–8. doi: 10.5507/bp.2015.033
111. Matt P, Lindqvist U, Kleinau S. Up-regulation of CD64-expressing monocytes with impaired FcγR function reflects disease activity in polyarticular psoriatic arthritis. Scandinavian J Rheumatol (2015) 44(6):464–73. doi: 10.3109/03009742.2015.1020864
112. Peled M, Strazza M, Azoulay-Alfaguter I, Mor A. Analysis of programmed death-1 in patients with psoriatic arthritis. Inflammation (2015) 38(4):1573–9. doi: 10.1007/s10753-015-0132-2
113. Dikbas O, Tosun M, Bes C, Tonuk SB, Aksehirli OY, Soy M. Serum levels of visfatin, resistin and adiponectin in patients with psoriatic arthritis and associations with disease severity. Int J Rheum Dis (2016) 19(7):672–7. doi: 10.1111/1756-185X.12444
114. Munk HL, Gudmann NS, Christensen AF, Ejstrup L, Sorensen GL, Loft AG, et al. Cartilage collagen type II seromarker patterns in axial spondyloarthritis and psoriatic arthritis: associations with disease activity, smoking and HLA-B27. Rheumatol Int (2016) 36(4):541–9. doi: 10.1007/s00296-015-3397-8
115. Inciarte-Mundo J, Ramirez J, Hernández MV, Ruiz-Esquide V, Cuervo A, Cabrera-Villalba SR, et al. Calprotectin and TNF trough serum levels identify power Doppler ultrasound synovitis in rheumatoid arthritis and psoriatic arthritis patients in remission or with low disease activity. Arthritis Res Ther (2016) 18(1):1–10. doi: 10.1186/s13075-016-1032-z
116. Przepiera-Będzak H, Fischer K, Brzosko M. Serum interleukin-18, fetuin-a, soluble intercellular adhesion molecule-1, and endothelin-1 in ankylosing spondylitis, psoriatic arthritis, and SAPHO syndrome. Int J Mol Sci (2016) 17(8):1255. doi: 10.3390/ijms17081255
117. Kiliç S, Reşorlu H, Işik S, Oymak S, Akbal A, Hiz MM, et al. Association between mean platelet volume and disease severity in patients with psoriasis and psoriatic arthritis. Adv Dermatol Allergol (2017) 34(2):126–30. doi: 10.5114/ada.2017.67076
118. Inciarte-Mundo J, Ramirez J, Hernández MV, Ruiz-Esquide V, Cuervo A, Cabrera-Villalba SR, et al. Calprotectin strongly and independently predicts relapse in rheumatoid arthritis and polyarticular psoriatic arthritis patients treated with tumor necrosis factor inhibitors: A 1-year prospective cohort study. Arthritis Res Ther (2018) 20(1):1–11. doi: 10.1186/s13075-018-1764-z
119. Wade SM, Canavan M, McGarry T, Low C, Wade SC, Mullan RH, et al. Association of synovial tissue polyfunctional T-cells with DAPSA in psoriatic arthritis. Ann Rheum Dis (2019) 78(3):350–4. doi: 10.1136/annrheumdis-2018-214138
120. Coras R, Kavanaugh A, Boyd T, Huynh Q, Pedersen B, Armando AM, et al. Pro- and anti-inflammatory eicosanoids in psoriatic arthritis. Metabolomics (2019) 15(4):1–9. doi: 10.1007/s11306-019-1527-0
121. Colak S, Omma A, Sandikci SC, Yucel C, Omma T, Turhan T. Vaspin, neutrophil gelatinase-associated lipocalin and apolipoprotein levels in patients with psoriatic arthritis. Bratisl Lek Listy (2019) 120(1):65–9. doi: 10.4149/BLL_2019_010
122. Sakellariou G, Lombardi G, Vitolo B, Gomarasca M, Faraldi M, Caporali R, et al. Serum calprotectin as a marker of ultrasound-detected synovitis in early psoriatic and rheumatoid arthritis: results from a cross-sectional retrospective study. Clin Exp Rheumatol (2019) 37(3):429–36.
123. Coras R, Kavanaugh A, Boyd T, Huynh D, Lagerborg KA, Xu YJ, et al. Choline metabolite, trimethylamine n-oxide (TMAO), is associated with inflammation in psoriatic arthritis. Clin Exp Rheumatol (2019) 37(3):481–4.
124. Ozisler C, Sandikci SC. Evaluation of red blood cell distribution width in patients with psoriatic arthritis. Egyptian Rheumatologist. (2020) 42(4):309–12. doi: 10.1016/j.ejr.2019.06.001
125. Arias de la Rosa I, Font P, Escudero-Contreras A, López-Montilla MD, Pérez-Sánchez C, Ábalos-Aguilera MC, et al. Complement component 3 as biomarker of disease activity and cardiometabolic risk factor in rheumatoid arthritis and spondyloarthritis. Ther Adv Chronic Dis (2020) 11:2040622320965067. doi: 10.1177/2040622320965067
126. Jarlborg M, Courvoisier DS, Lamacchia C, Martinez Prat L, Mahler M, Bentow C, et al. Serum calprotectin: A promising biomarker in rheumatoid arthritis and axial spondyloarthritis. Arthritis Res Ther (2020) 22(1):1–11. doi: 10.1186/s13075-020-02190-3
127. Medvedeva I v., Stokes ME, Eisinger D, LaBrie ST, Ai J, Trotter MWB, et al. Large-Scale analyses of disease biomarkers and apremilast pharmacodynamic effects. Sci Rep (2020) 10(1):1–11. doi: 10.1038/s41598-020-57542-5
128. Wcisło-Dziadecka D, Grabarek B, Kruszniewska-Rajs C, Swinarew A, Jasik K, Rozwadowska B, et al. Analysis of molecular and clinical parameters of 4-year adalimumab therapy in psoriatic patients. Adv Dermatol Allergol (2020) 37(5):736–45. doi: 10.5114/ada.2020.100484
129. Boyd TA, Eastman PS, Huynh DH, Qureshi F, Sasso EH, Bolce R, et al. Correlation of serum protein biomarkers with disease activity in psoriatic arthritis. Expert Rev Clin Immunol (2020) 16(3):335–41. doi: 10.1080/1744666X.2020.1729129
130. Coras R, Kavanaugh A, Kluzniak A, Holt D, Weilgosz A, Aaron A, et al. Differences in oxylipin profile in psoriasis versus psoriatic arthritis. Arthritis Res Ther (2021) 23(1):1–13. doi: 10.1186/s13075-021-02575-y
131. Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute (2021). Available at: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
132. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol (2005) 5(1):1–10. doi: 10.1186/1471-2288-5-13
133. Cohen J. Statistical power analysis for the behavioral sciences. In: Statistical power analysis for the behavioral sciences, 2nd ed. New York: Routledge (1988). doi: 10.4324/9780203771587/statistical-power-analysis-behavioral-sciences-jacob-cohen
134. Chandran V, Cook R, Pollock RA, Pellet F, Hua S, Gladman D. Soluble biomarkers predict response to anti-tumour necrosis factor (TNF) therapy in psoriatic arthritis (PsA). J Rheumatol (2010) 37(6):1282–3. doi: 10.1093/rheumatology/keq105
135. Loures MAR, Alves HV, de Moraes AG, Santos T da S, Lara FF, Neves JSF, et al. Association of TNF, IL12, and IL23 gene polymorphisms and psoriatic arthritis: meta-analysis. Expert Rev Clin Immunol (2019) 15(3):303–13. doi: 10.1080/1744666X.2019.1564039
136. Villalpando-Vargas FV, Rivera-Valdés JJ, Alvarado-Navarro A, Huerta-Olvera SG, Macías-Barragán J, Martínez-López E, et al. Association between IL-17A, IL-17F and IL-17RA gene polymorphisms and susceptibility to psoriasis and psoriatic arthritis: a meta-analysis. Inflammation Res (2021) 70(10–12):1201–10. doi: 10.1007/s00011-021-01514-6
137. Queiro R, Morante I, Cabezas I, Acasuso B. HLA-B27 and psoriatic disease: a modern view of an old relationship. Rheumatology (2016) 55(2):221–9. doi: 10.1093/rheumatology/kev296
138. Massy E, Pedini P, Pollet E, Martin M, Roudier J, Picard C, et al. Association study between HLA-a, -b, -c, -DRB1 alleles and psoriatic arthritis in southern France. Hum Immunol (2022) 83(6):515–20. doi: 10.1016/j.humimm.2022.04.001
139. Generali E, Scirè CA, Favalli EG, Selmi C. Biomarkers in psoriatic arthritis: a systematic literature review. Exp Rev Clin Immunol (2016) 12(6):651–60. doi: 10.1586/1744666X.2016.1147954
140. Shao LN, Wang N, Zhou SH, Wang Z. Associations between human leukocyte antigen c locus polymorphism and psoriatic arthritis in populations of European and middle Eastern descent: a meta-analysis. Ann Saudi Med (2020) 40(4):338–46. doi: 10.5144/0256-4947.2020.338
141. Stuart PE, Nair RP, Tsoi LC, Tejasvi T, Das S, Kang HM, et al. Genome-wide association analysis of psoriatic arthritis and cutaneous psoriasis reveals differences in their genetic architecture. Am J Hum Genet (2015) 97(6):816–36. doi: 10.1016/j.ajhg.2015.10.019
142. Chen J, Yuan F, Fan X, Wang Y. Psoriatic arthritis: A systematic review of non-HLA genetic studies and important signaling pathways. Int J Rheum Dis (2020) 23(10):1288–96. doi: 10.1111/1756-185X.13879
143. Hagiwara S, Tsuboi H, Terasaki T, Terasaki M, Toko H, Shimizu M, et al. Association of anti-cyclic citrullinated peptide antibody with clinical features in patients with psoriatic arthritis. Mod Rheumatol (2020) 30(2):365–72. doi: 10.1080/14397595.2019.1586085
Keywords: psoriatic arthritis, psoriatic biomarker, psoriasis, arthritis, meta-analysis
Citation: Wirth T, Balandraud N, Boyer L, Lafforgue P and Pham T (2022) Biomarkers in psoriatic arthritis: A meta-analysis and systematic review. Front. Immunol. 13:1054539. doi: 10.3389/fimmu.2022.1054539
Received: 26 September 2022; Accepted: 07 November 2022;
Published: 30 November 2022.
Edited by:
Durga Prasanna Misra, Sanjay Gandhi Post Graduate Institute of Medical Sciences (SGPGI), IndiaReviewed by:
Ajesh Maharaj, University of KwaZulu-Natal, South AfricaCopyright © 2022 Wirth, Balandraud, Boyer, Lafforgue and Pham. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Theo Wirth, d2lydGh0aGVvQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.