
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Immunol., 31 January 2023
Sec. Immunological Tolerance and Regulation
Volume 13 - 2022 | https://doi.org/10.3389/fimmu.2022.1020393
This article is part of the Research TopicThe Role of Epigenetic Modification in MDSC Differentiation and FunctionView all 5 articles
 Muhammad Zulqarnain1†
Muhammad Zulqarnain1† Guangxing Cui2†
Guangxing Cui2† Wen Lyu2*
Wen Lyu2* Haitao Huang2
Haitao Huang2 Xia Wang2
Xia Wang2 Hamse Mohamoud Abdi1
Hamse Mohamoud Abdi1 Lingfei Gu1
Lingfei Gu1 Shijie Fang1
Shijie Fang1 Fangzhou Liu1
Fangzhou Liu1 Liqian Ling1
Liqian Ling1To assess the effectiveness of endoscopic retrograde appendicitis therapy (ERAT) as a new technique and method for chronic fecalith appendicitis complicated by active ulcerative colitis. A 46-year-old male patient was admitted with right iliac fossa pain, tenderness, and raised inflammatory markers. A computed tomography (CT) scan of his abdomen confirmed a dilated appendix, which is considered chronic fecalith appendicitis combined with active ulcerative colitis. He was treated with an endoscopic retrograde appendicitis therapy procedure. The patient recovered well after the ERAT procedure and was discharged from the hospital in two days. On follow-up one year later, there was no recurrence of pain in his abdomen. In conclusion, ERAT could be seen as a different approach and be favored as a safer and more effective option in treating UC patients with appendicitis, especially those who are later in the course of the disease. Because of the ERAT procedure, such cases can avoid surgery and surgery-related complications. More research and issues must be addressed to demonstrate the efficacy and effectiveness of ERAT in appendicitis combined with UC.
A 46-year-old Chinese male patient was admitted because of right lower abdominal pain for over two years that had been aggravated for one month. An abdominal CT scan revealed appendicitis and ulcerative colitis, which were suspected at a local hospital. As a result, the patient was referred to our hospital for further treatment. The patient denied a history of hypertension, coronary heart disease, cerebrovascular diseases, diabetes, and hyperthyroidism. During the physical examination, the temperature was 38.1°C, the abdomen was soft, there was positive tenderness, and there was no rebound pain. The auxiliary examination after admission showed that the white blood cells (WBC) were 13.8×109/L; hemoglobin was 111 g/L; C-reactive protein (CRP) was 90 mg/L (8 mg/L); the neutrophil percentage was 81.5%; and the procalcitonin was 0.55 ng/ml (0.5). Our hospital CT scan showed that the appendix was locally thickened and enhanced, chronic fecal appendicitis was suspected, and multiple small lymph nodes were displayed in the ileocecum area (Figure 1). Under colonoscopy, the terminal ileum and the orifice of the appendix were thickened, the ileocecal valve showed a deep ulcer, and the histopathological samples presented terminal ileum, ileocecal valve crypt abscess, and cryptitis. These findings most likely suggested chronic fecalith appendicitis with active ulcerative colitis. The final diagnosis was chronic fecal appendicitis with active ulcerative colitis. The ERAT procedure was performed for the patient. When the colonoscopy reached the ileocecal valve area, the mucosa appeared ulcerated, and the surface was covered with a crypt abscess, showing “ulcerative colitis”-like changes (Figure 2).
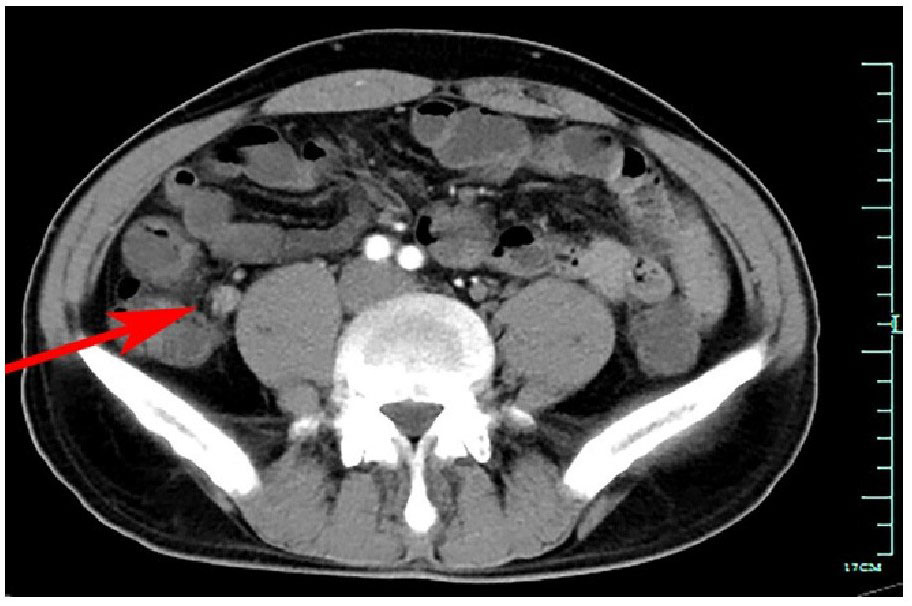
Figure 1 Abdominal contrast-enhanced computed tomography scan showing dilated appendix with high density in the lumen.
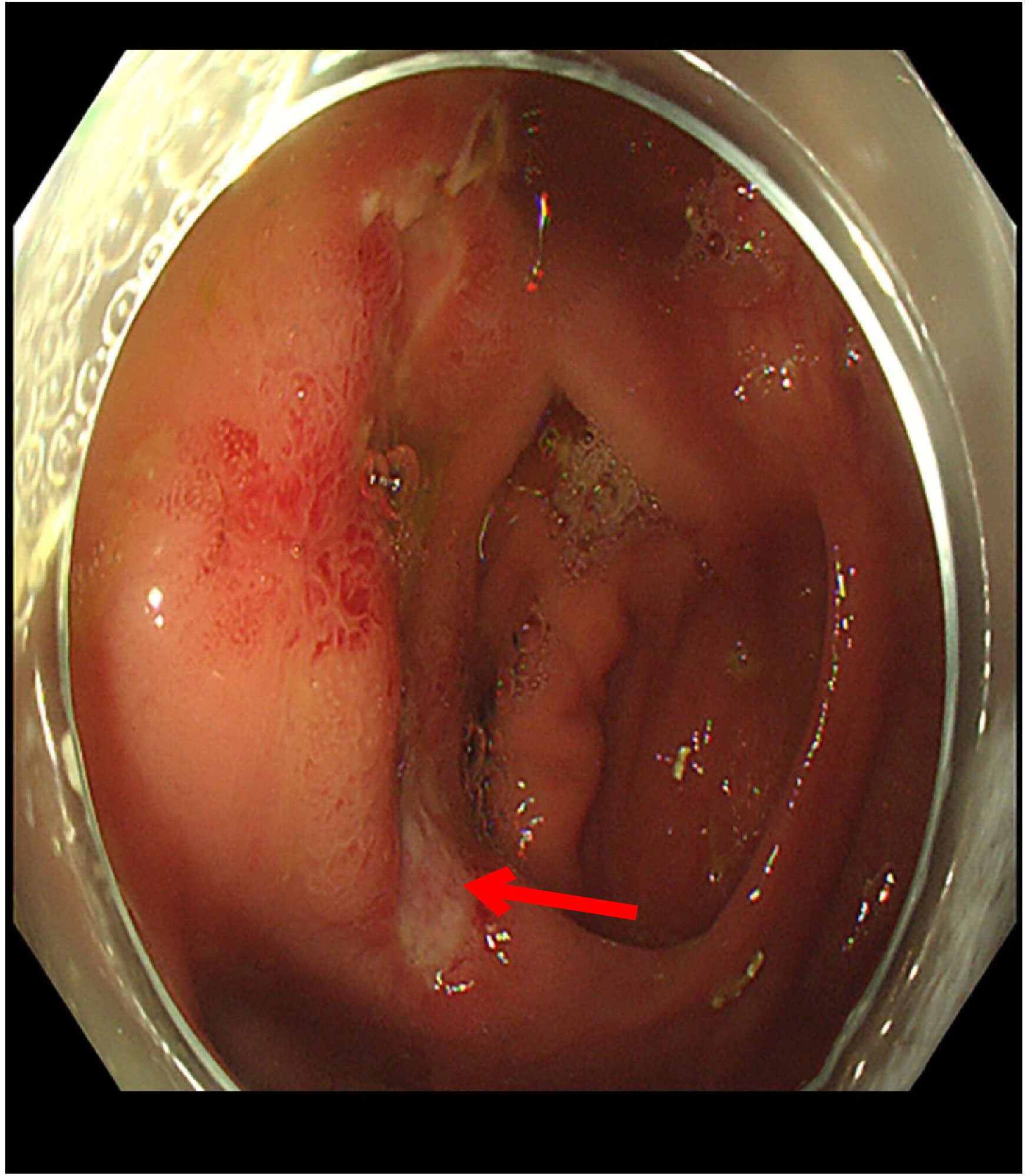
Figure 2 Large and irregular ulcer that is consistent with ulcerative colitis being seen on the ileocecal valve.
The orifice of the appendix was thickened, so it was challenging to insert the guide wire into the appendiceal orifice (Figure 3). Finally, we reached the appendiceal cavity, in which a copious amount of pus and stones could be seen flowing out during the procedure (Figure 4). Fluoroscopy revealed that the appendiceal lumen was severely dilated after successful cannulation, with a width of 10 mm, length of 8 cm, and an irregular shape (Figure 5). The appendiceal lumen was irrigated with 100 ml of metronidazole. After clearance of the appendiceal lumen, a pigtail plastic stent with a size of 6 French widths and 5 cm in length was successfully placed into the appendix cavity. (Figure 6). Intravenous antibiotics were administered before ERAT and two days after. The patient was discharged after the procedure, and the abdominal pain was relieved.
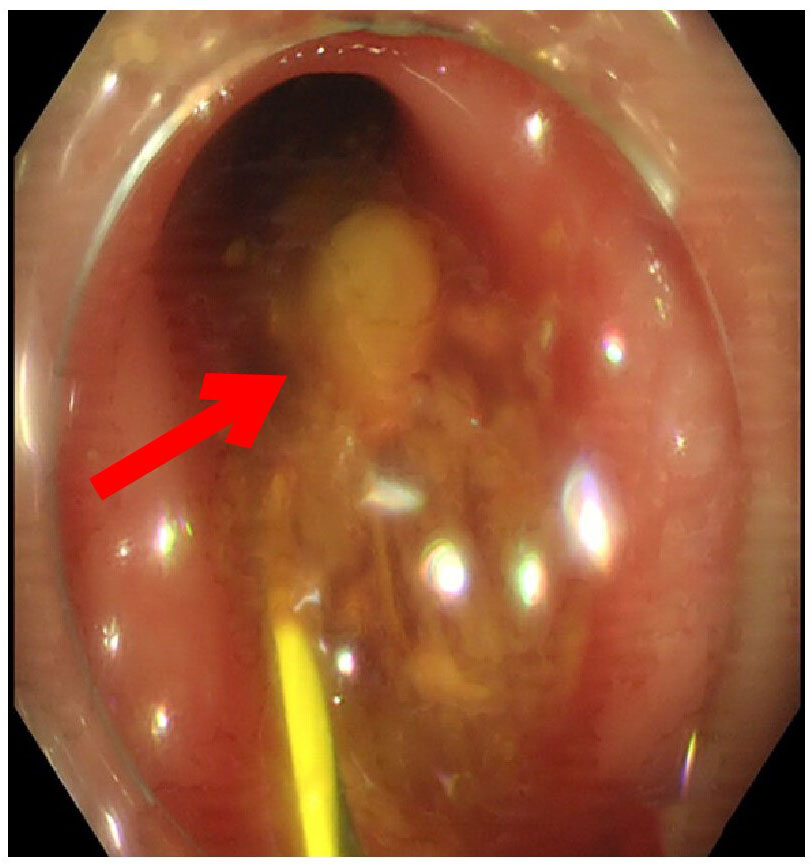
Figure 4 An appendiceal fecalith was flowing out during exchange of guidewire for balloon catheter, removal of fecalith with a balloon catheter.
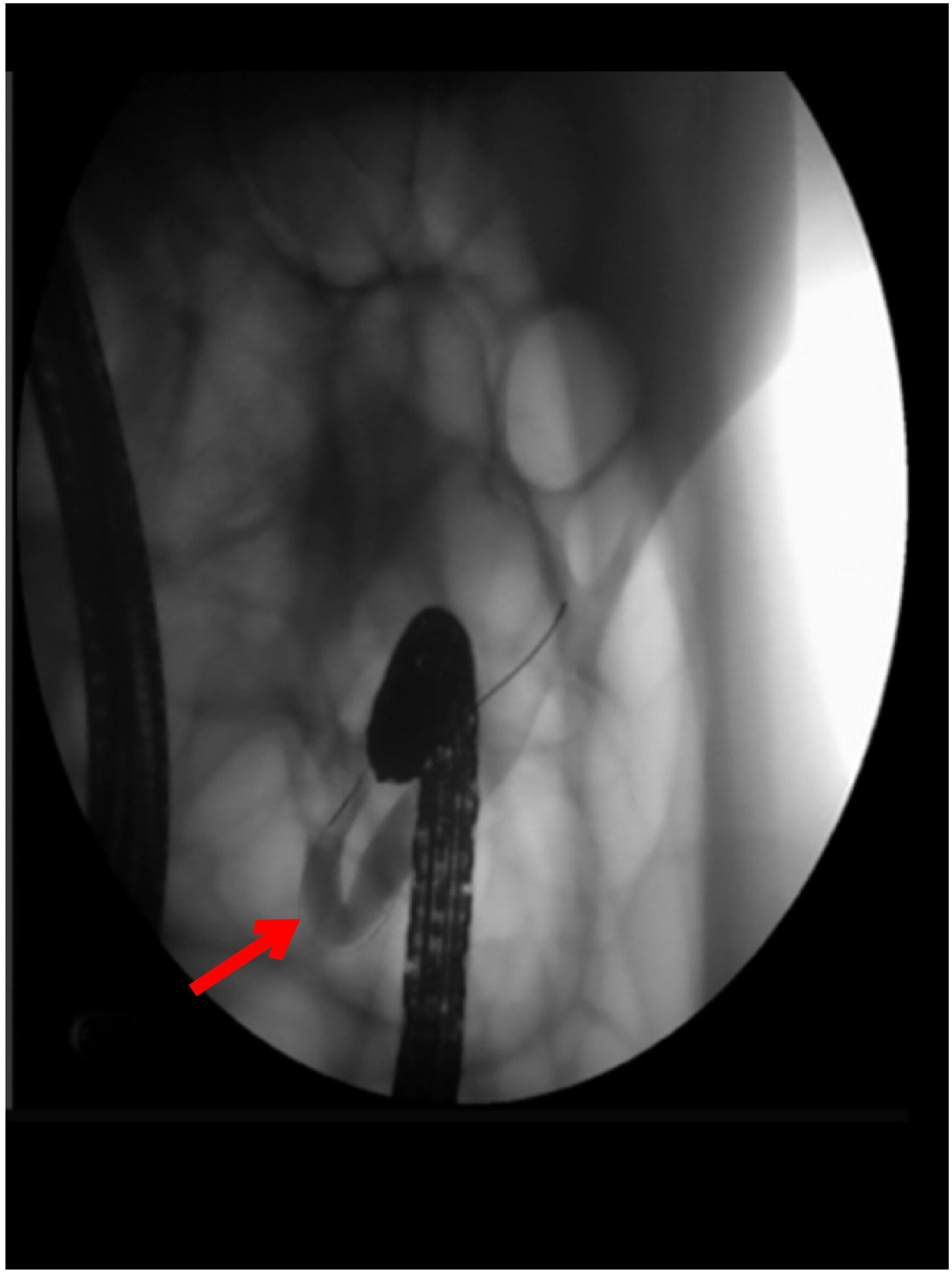
Figure 5 Fluoroscopy of the appendiceal lumen after successful cannulation showing the irregularly dilated appendiceal lumen with a diameter of 1.0cm and multiple filling defects.
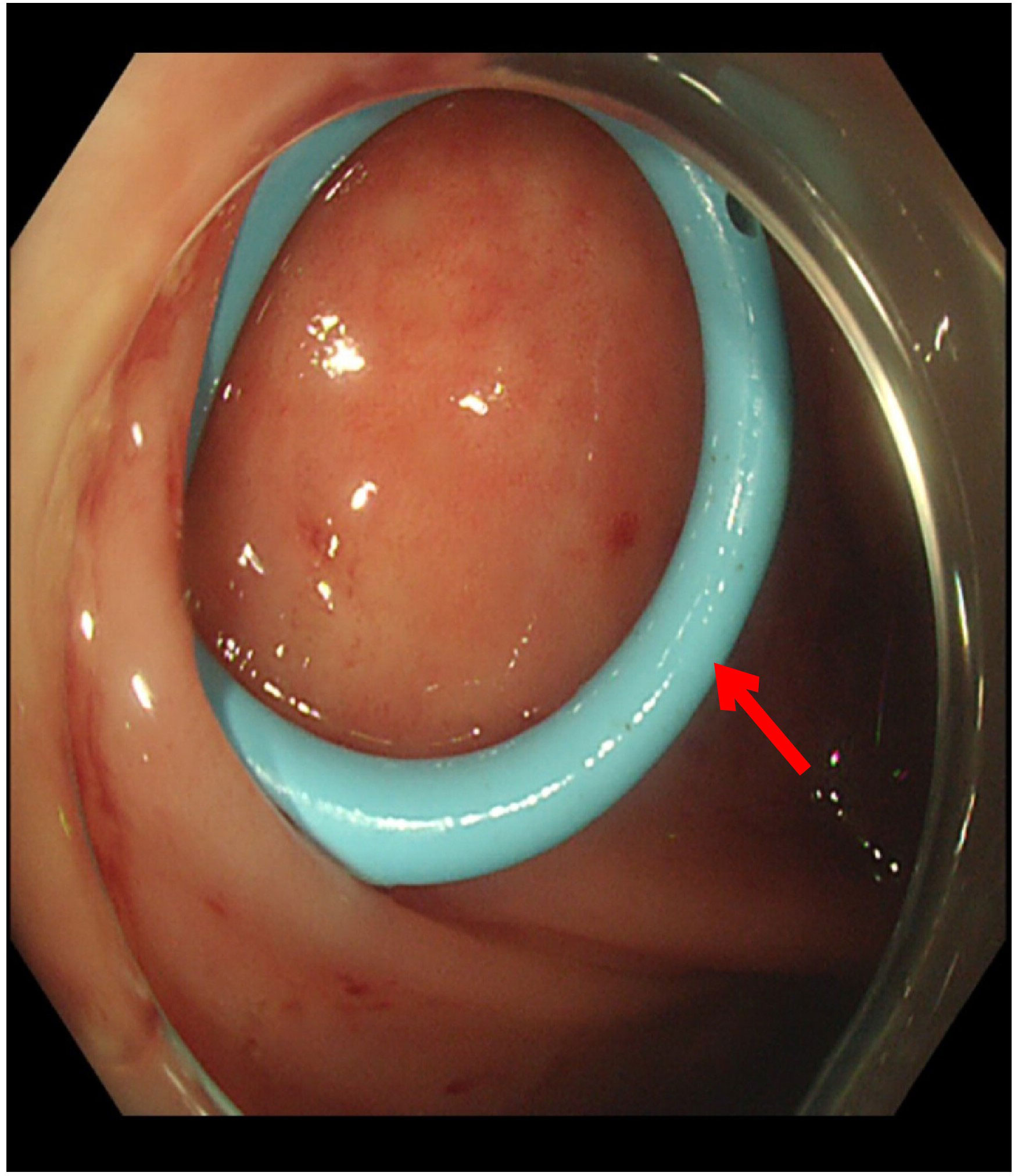
Figure 6 After clearance of the appendiceal lumen, a pigtail plastic stent with a size of 6 *French widths and 5 cm in length was successfully placed into the appendix cavity.
Ulcerative colitis (UC) is a chronic colon inflammation that has a variable clinical course (1). Although the etiology of UC is still unclear, genetic susceptibility and environmental factors are involved in the pathogenesis of UC. The results of a large, multi-center study demonstrate that appendectomy, regardless of the timing of the UC diagnosis, does not decrease the severity of the UC disease course compared to UC patients who did not undergo appendectomy. The results suggested that performing an appendectomy after a UC diagnosis may be harmful, as they showed a 2.2-fold increased risk of colectomy. An updated systematic review and meta-analysis confirmed the findings, which showed appendectomy did not affect colectomy rates in UC patients (2). Indications for surgery are intractability (49%), stricture, dysplasia, toxic colitis, bleeding, and perforation (3). Parian et al.’s retrospective database study of 2714 UC patients found a higher risk of colectomy in 48 patients who had appendectomy after UC diagnosis and concluded that appendectomy should not be recommended as a treatment for UC. However, recently published data show contradictory findings after appendectomy in UC patients, with an increased colectomy rate and, moreover, an increased risk of colorectal cancer (CRC) (4). If an appendectomy is associated with an increased risk of the subsequent development of CRC, this would have considerable implications for ongoing clinical studies and daily clinical practice. More research is necessary to understand this possible link and how the immune system might be involved. For over 100 years, appendectomy has been the first choice for treating acute appendicitis (5). It is now believed that the appendix has secretion and immune function (6, 7) and maintains the normal colonic flora (8). Appendectomy is not perfect because, overall, in-hospital complications of appendectomy occur as much as 11% (9). And the negative appendectomy rate remains as high as 8% (10). Endoscopic retrograde appendicitis therapy (ERAT) is an endoscopic therapy used to manage acute appendicitis (AA) and is an alternative to laparoscopic appendectomy. This method was first reported by Liu et al. in 2012. The recurrence rate of appendicitis following ERAT was low, with an average rate of 6.01 percent (11). The previous study reported a colonoscopic diagnosis of acute appendicitis and described the colonoscopic features of the appendiceal orifice during acute appendicitis (12–15). ERAT has several advantages. First of all, ERAT resulted in almost immediate relief from abdominal pain. Patients can resume normal activities after stent drainage and avoid postoperative pain from the incision. Second, ERAT is minimally invasive and allows patients with acute appendicitis to get treatment without a residual scar. ERAT is a simple and quick procedure that could be carried out in the outpatient department, thus further reducing medical expenses. Finally, ERAT retains the potential physiological function of the appendix. During the procedure, ulcerative colitis was seen in an operational condition, and inflammation was observed at the appendiceal orifice. Under fluoroscopy, the lumen was irregular and had no stricture. After the procedure, the patient’s abdominal pain disappeared. In addition to relieving the obstruction and removing Fecalith from the appendix lumen, draining the pus and flushing the lumen could control the inflammation. It also permits the insertion of a drainage tube into the lumen to ensure smooth drainage through the appendiceal orifice and reduce the risk of appendicitis recurrence caused by the blockage.
ERAT is a different approach and is favored as a safer and more effective option in treating UC patients with appendicitis, especially those later in the course of the disease. Because of the ERAT procedure, such cases can avoid surgery and surgery-related complications. Follow-up one year later, the patient has no recurrent episodes of appendicitis. More research and issues must be addressed to demonstrate the efficacy and effectiveness of ERAT in appendicitis combined with UC.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
MZ and GC drafted the manuscript. GC and HH performed the ERAT procedure and designed the study. LG, SF, FL, LL and WX revised the manuscript. and HA is responsible for the collection of data and analysis. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Katz J. The course of inflammatory bowel disease. Med Clinics North Am (1994) 78(6):1275–80. doi: 10.1016/S0025-7125(16)30100-6
2. Lee HS, Park SH, Yang SK, Kim SO, Soh JS, Lee S, et al. Appendectomy and the clinical course of ulcerative colitis: a retrospective cohort study and a nested case-control study from Korea. J Gastroenterol Hepatol (2015) 30(3):470–7. doi: 10.1111/jgh.12707
3. Longo WE, Virgo KS, Bahadursingh AN, Johnson FE. Patterns of disease and surgical treatment among united states veterans more than 50 years of age with ulcerative colitis. Am J Surg (2003) 186(5):514–8. doi: 10.1016/j.amjsurg.2003.07.001
4. Parian A, Limketkai B, Koh J, Brant SR, Bitton A, Cho JH, et al. Appendectomy does not decrease the risk of future colectomy in UC: Results from a large cohort and meta-analysis. Gut. (2017) 66(8):1390–7. doi: 10.1136/gutjnl-2016-311550
5. McBurney C IV. The incision made in the abdominal wall in cases of appendicitis, with a description of a new method of operating. Ann Surg (1894) 20(1):38–43. doi: 10.1097/00000658-189407000-00004
6. Zahid A. The vermiform appendix: not a useless organ. J Coll Physicians Surgeons–Pakistan JCPSP. (2004) 14(4):256–8. doi: 04.2004/jcpsp.256258
7. Bazar KA, Lee PY, Joon Yun A. An "eye" in the gut: the appendix as a sentinel sensory organ of the immune intelligence network. Med Hypotheses (2004) 63(4):752–8. doi: 10.1016/j.mehy.2004.04.008
8. Randal Bollinger R, Barbas AS, Bush EL, Lin SS, Parker W. Biofilms in the large bowel suggest an apparent function of the human vermiform appendix. J Theor Biol (2007) 249(4):826–31. doi: 10.1016/j.jtbi.2007.08.032
9. Guller U, Hervey S, Purves H, Muhlbaier LH, Peterson ED, Eubanks S, et al. Laparoscopic versus open appendectomy: outcomes comparison based on a large administrative database. Ann Surg (2004) 239(1):43–52. doi: 10.1097/01.sla.0000103071.35986.c1
10. Seetahal SA, Bolorunduro OB, Sookdeo TC, Oyetunji TA, Greene WR, Frederick W, et al. Negative appendectomy: A 10-year review of a nationally representative sample. Am J Surg (2011) 201(4):433–7. doi: 10.1016/j.amjsurg.2010.10.009
11. Liu BR, Song JT, Han FY, Li H, Yin JB. Endoscopic retrograde appendicitis therapy: a pilot minimally invasive technique (with videos). Gastrointest Endoscopy (2012) 76(4):862–6. doi: 10.1016/j.gie.2012.05.029
12. Minocha A. An endoscopic view of appendicitis. New Engl J Med (1998) 339(20):1481. doi: 10.1056/NEJM199811123392015
13. Chen YY, Soon MS, Yen HH. Images of interest. gastrointestinal: colonoscopic features of acute appendicitis. J Gastroenterol Hepatol (2005) 20(12):1940. doi: 10.1111/j.1440-1746.2005.04184.x
14. Zimmer V, Juengling B, Lammert F. Colonoscopy in acute appendicitis. Internal Med (Tokyo Japan) (2010) 49(20):2273. doi: 10.2169/internalmedicine.49.3891
Keywords: chronic fecalith appendicitis, active ulcerative colitis, endoscopic retrograde appendicitis therapy (ERAT), antibiotics, inflammation
Citation: Zulqarnain M, Cui G, Lyu W, Huang H, Wang X, Abdi HM, Gu L, Fang S, Liu F and Ling L (2023) Endoscopic retrograde appendicitis therapy in the management of chronic fecalith appendicitis in a patient with ulcerative colitis: The first human case report. Front. Immunol. 13:1020393. doi: 10.3389/fimmu.2022.1020393
Received: 16 August 2022; Accepted: 27 December 2022;
Published: 31 January 2023.
Edited by:
Shengjun Wang, Jiangsu University Affiliated People’s Hospital, ChinaReviewed by:
Catherine Hunter, University of Oklahoma, United StatesCopyright © 2023 Zulqarnain, Cui, Lyu, Huang, Wang, Abdi, Gu, Fang, Liu and Ling. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wen Lyu, NjcwOTYwOTEyQHFxLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.