
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Immunol. , 23 November 2022
Sec. Cancer Immunity and Immunotherapy
Volume 13 - 2022 | https://doi.org/10.3389/fimmu.2022.1019638
This article is part of the Research Topic Tumor Ablation and Immunity View all 36 articles
 Qi Wang1†
Qi Wang1† Wenying Qiao1†
Wenying Qiao1† Honghai Zhang2†
Honghai Zhang2† Biyu Liu1
Biyu Liu1 Jianjun Li2
Jianjun Li2 Chaoran Zang1
Chaoran Zang1 Tingting Mei1
Tingting Mei1 Jiasheng Zheng2
Jiasheng Zheng2 Yonghong Zhang1,2*
Yonghong Zhang1,2*Purpose: To investigate the risk factors for recurrence in patients with early-stage hepatocellular carcinoma (HCC) after minimally invasive treatment with curative intent, then to construct a prediction model based on Lasso-Cox regression and visualize the model built.
Methods: Clinical data were collected from 547 patients that received minimally invasive treatment in our hospital from January 1, 2012, to December 31, 2016. Lasso regression was used to screen risk factors for recurrence. Then we established Cox proportional hazard regression model and random survival forest model including several parameters screened by Lasso regression. An optimal model was selected by comparing the values of C-index, then the model was visualized and the nomogram was finally plotted.
Results: The variables screened by Lasso regression including age, gender, cirrhosis, tumor number, tumor size, platelet-albumin-bilirubin index (PALBI), and viral load were incorporated in the Cox model and random survival forest model (P<0.05). The C-index of these two models in the training sets was 0.729 and 0.708, and was 0.726 and 0.700 in the validation sets, respectively. So we finally chose Lasso-Cox regression model, and the calibration curve in the validation set performed well, indicating that the model built has a better predictive ability. And then a nomogram was plotted based on the model chosen to visualize the results.
Conclusions: The present study established a nomogram for predicting recurrence in patients with early-stage HCC based on the Lasso-Cox regression model. This nomogram was of some guiding significance for screening populations at high risk of recurrence after treatment, by which doctors can formulate individualized follow-up strategies or treatment protocols according to the predicted risk of relapse for patients to improve the long-term prognosis.
Hepatocellular carcinoma (HCC) has the sixth-highest incidence and the third-highest mortality, with an estimated 910,000 new cases and 830,000 deaths worldwide in 2020. In China, there are 410,000 new cases and 390,000 deaths, accounting for approximately 50% of the global total (1). Hence, HCC is still a major worldwide health problem to be addressed urgently. With the development of imaging technology, more and more patients with early-stage HCC have been diagnosed, which can be treated with liver resection, local ablation, or liver transplantation. However, the high 5-year recurrence rate of about 70% leads to shorter overall survival in HCC patients (2, 3). Despite advances in these treatments, there is no effective adjuvant therapy to prevent HCC recurrence, making it crucial to improve the prognosis of HCC patients by successfully identifying and timely treating individuals at high risk of recurrence (4).
To date, several studies have published risk scoring systems combining some demographic and clinical data (5–7). Nevertheless, most of the screening processes of parameters are based on univariate and multivariate analyses, which has some limitations in dealing with multicollinearity between variables. Lasso regression with not a widely use in HCC field could build a more refined model by constructing penalty functions (8). And beyond that, few studies have performed models on account of Lasso-Cox method. In this study, Lasso regression and Cox regression are combined. The former can effectively screen variables, while the latter can be modeled and visualized for straightforward interpretation.
Therefore, this study aims to establish a new prediction model for HCC recurrence based on the Lasso-Cox method to improve the individualized prediction of recurrence risk in HCC patients at the early stage after treatment, which could identify individuals with high recurrence risk, provide a reference for the formulation of personalized diagnosis and treatment plans for HCC patients. This would be a step not to be ignored towards precision medicine.
The study included 547 patients aged 18-75 years old who were admitted with Beijing You’an Hospital affiliated to Capital Medical University from January 1, 2012, to December 31, 2016 and diagnosed with early-stage HCC by alpha-fetoprotein (AFP), enhanced imaging technology, or histological examination (diagnostic criteria recommended by AASLD) (9). Early-stage HCC was defined as a single tumor smaller than 5cm or no more than three tumors with a tumor diameter of less than 3cm. All of patients enrolled received minimally invasive treatment, namely transarterial chemoembolization (TACE) combined with locoregional ablation (hereinafter referred to as combination therapy), and achieved complete response. Patients are excluded if they met any of the following criteria:(1) secondary liver cancer; (2) Child-Pugh class C; (3) coagulation function disorders, or serious diseases of the heart, brain, lung and kidney; (4) incomplete ablation. The definition of complete ablation was that the CT scan immediately after ablation showed a safe margin of 0.5-1cm of the adjacent non-tumor tissue in the ablation area was ablated.
In 38 of the 547 patients, important data such as AFP or viral load were missing, while prognostic data were not lacking and were therefore included in the analysis of outcomes but excluded in modeling. In order to establish a more reliable and robust model, the patients included were randomly divided into a training set (N1 = 254) and a validation set (N2 = 255) in a 1:1 ratio, and the demographic characteristics, laboratory data and prognosis of patients in the two groups were compared.
Informed consent was exempted by the ethics committee because it was a minimum-risk study. The study has been approved by the ethics committee of the Beijing You’an Hospital affiliated with Capital Medical University.
Demographic and clinicopathological data within seven days before ablation were collected. Demographic data included age, gender, and history of smoking, drinking, antiviral, hypertension and diabetes mellitus. Clinicopathological data included following: (1) etiology: hepatitis B virus (HBV), hepatitis C virus (HCV), co-infection, and others; (2) tumor information: number, size, and AFP; (3) Liver function indicators: Child-Pugh class and cirrhosis; (4) laboratory parameters: neutrophils, platelets (PLT), lymphocytes, alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin (TBIL), albumin (ALB), γ-glutamyl transpeptidase (γ-GT), alkaline phosphatase (ALP), international normalized ratio (INR), and viral load (the number of copies of HBV-DNA or HCV-RNA quantified in serum); (5) treatment-related factors: ablation modality and the number of ablation.
Few studies have demonstrated the prognostic value of platelet-albumin-bilirubin index (PALBI) in early-stage HCC patients receiving combination therapy. Therefore, PALBI was included in this study to increase the robustness of the proposed model. The calculation formula was as follows: PALBI=(2.02*log10TBIL)+[-0.37*(log10TBIL)2]+(-0.04*ALB)+(-3.48*log10PLT)+[1.01*(logPLT)2]. PALBI were classified into three grades: PALBI-1≤-2.53, -2.53<PALBI-2≤-2.09, and PALBI-3>-2.09.
All included patients received TACE combined with locoregional ablation. The ablation modalities, such as radiofrequency ablation (RFA), microwave ablation (MWA), or argon-helium cryoablation (AHC), were performed 1-2 weeks after the TACE. Ablation in two or more sessions may be considered for patients with multiple tumors. Detailed treatment procedures have been described in previous studies and will not be described in this study.
All patients were followed up in the outpatient clinic. Physical, laboratory examinations including AFP, and ultrasound were performed every 3-6 months. Contrast‐enhanced computed tomography (CT) or magnetic resonance imaging (MRI) scan was routinely implemented every six months. When the patient relapsed, TACE and/or ablation were performed depending on the tumor conditions. Recurrence was defined as the presence of new lesions next to the original lesion or at intra-/extra-hepatic sites, which showed arterial contrast enhancement and portal phase washout on contrast-enhanced images. Recurrence-free survival (RFS) was regarded as the time span from diagnosis to the first recurrence or last follow-up. And overall survival (OS) was considered as the time span from diagnosis to death or last follow-up. Statistical analysis was performed using data available before July 1, 2020.
Continuous variables were expressed as means ± standard deviation, and differences between groups were compared using Student’s t-test. The Chi‐square test was used to perform the difference comparison of categorical variables which were reported as frequency and percentages. Lasso regression was used to screen for the risk factors. Two prediction models including parameters screened by Lasso regression were established based on Cox regression and random survival forest (RSF). The prediction abilities of the two models were compared by C-index. The hazard ratio (HR) values were calculated using a backward stepwise regression method in Cox model, which could be regarded as a weight to obtain the risk score for predicting prognosis. However, RSF was like a “black box” because it could not produce regression coefficients and, therefore, could not explain the results intuitively. We could measure the importance of each predictor in the RSF model utilizing the variable importance (VIMP) method (10). The C-index and calibration curve were used to evaluate the discrimination and consistency of the model, respectively. The K-M method was used to assess clinical applicability. All statistical analyses were performed with R software v3.6.0 (R Foundation for Statistical Computing, Vienna, Austria; random Forest SRC, party, partykit, and VIM packages).
A total of 547 patients with early-stage HCC who received TACE combined locoregional ablation at Beijing You’an Hospital affiliated with Capital Medical University from January 1, 2012, to December 31, 2016, were enrolled, including 444 (81.2%) males and 103 (18.8%) females. 448 (81.9%), 56 (10.2%), 25 (4.6%), and 18 (3.3%) patients had HBV-related, HCV-related, coinfection-related, and other HCC. 130 (23.8%) individuals were diagnosed with hypertension and 103 (18.8%) with diabetes mellitus. Among the 547 patients, 242 (44.2%) had a history of smoking, and 193 (35.3%) had a history of drinking. There were 464 (84.8%) patients with cirrhosis. 400 (73.1%) were Child-Pugh class A, and 147 (26.9%) were Child-Pugh class B.
The median follow-up was 59.3 months. By the end of follow-up, 397 had relapsed and 189 had died. The median RFS was 26.0 months, and the median OS had not been reached. The cumulative 1-, 3-, and 5-year recurrence rates were 26.0% (142/547), 57.8% (316/547), and 68.2% (373/547), and the cumulative OS rates of 1, 3, and 5 years were 98.9% (541/547), 86.8% (475/547), and 74.4% (407/547), respectively. A time-dependent recurrence curve based on the K-M method was plotted to understand whether relapse predicted patients’ poor outcomes. As shown in Supplementary Figure S1, compared with patients without relapse, patients who relapsed had a shorter OS, making it necessary to establish a prognostic model for predicting recurrence, so as to screen populations with a high risk of recurrence and take timely interventions for them.
The patients were randomly divided into the training set and the validation set in a 1:1 ratio. The training set was used to establish the model, and the validation set was used to test the model established. There were no statistically significant differences in all variables included between the two groups (p>0.05), which showed that the data grouping was random and reasonable (Table 1). Lasso regression was used to screen parameters, and the variation characteristics of the coefficient of these variables were shown in Figure 1A. The 10-fold cross-validation method was applied to the iterative analysis, and a model with excellent performance but minimum number of variables was obtained when λ was 0.063 (Log λ=-1.20) (Figure 1B). The screened variables included age, gender, liver cirrhosis, tumor number, tumor size, PALBI score, and viral load. Cox regression model was further established based on parameters screened by Lasso regression (Table 2). The C-index of the training set was 0.729 and 0.726 in the validation set.
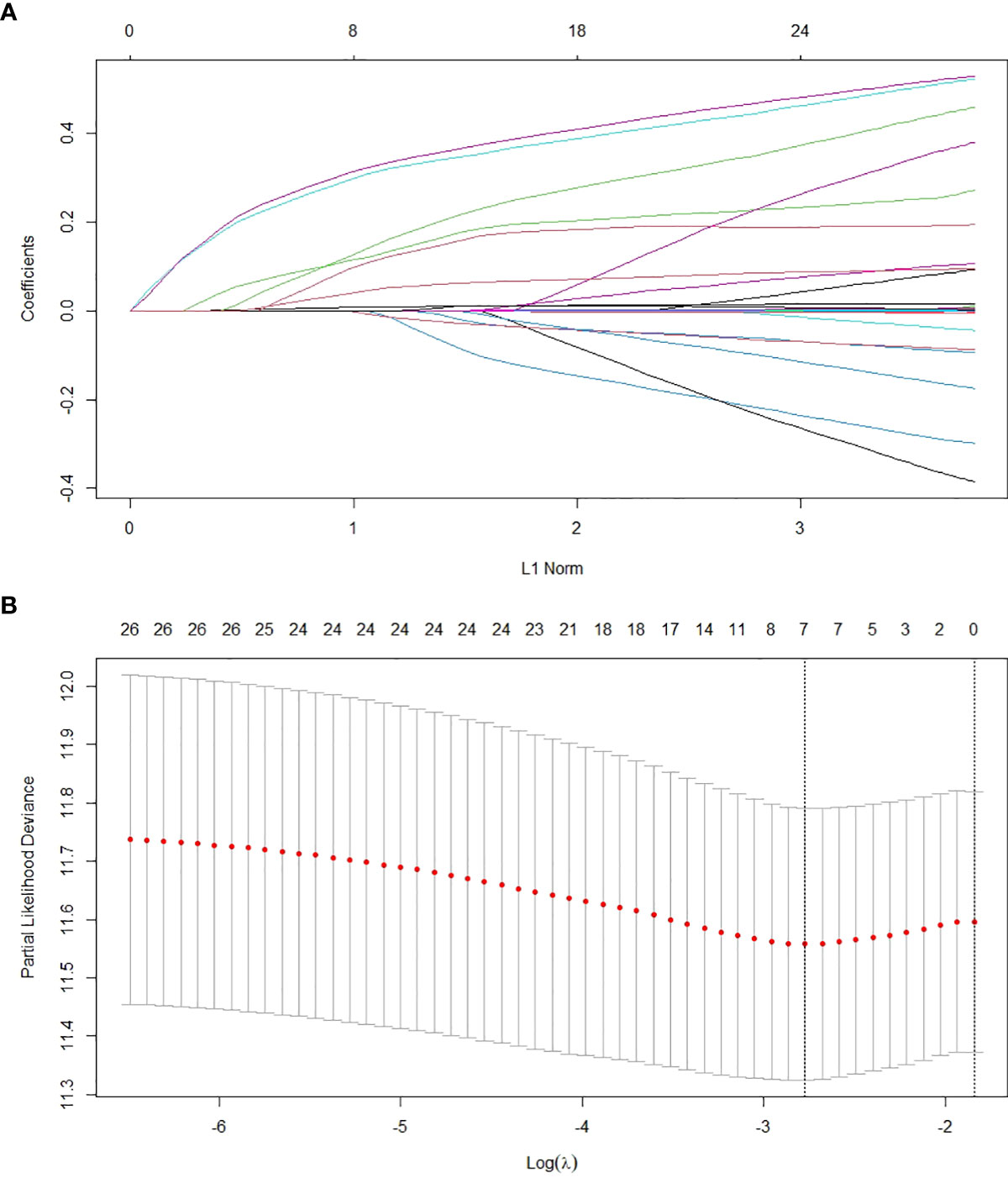
Figure 1 Screening of variables based on Lasso regression. (A) The variation characteristics of the coefficient of variables; (B) the selection process of the optimum value of the parameter λ in the Lasso regression model by cross-validation method.
Similarly, the variables selected by Lasso regression were used to build an RSF model in the training set (Figure 2A). Through parameter debugging, when ntree was 400, the error rate of the model tended to stabilize. The C-index of the training set was 0.708, and that of the validation set was 0.700. As shown in Figure 2B, the importance of variables was ranked according to the VIMP method, in the order of tumor number, tumor size, PALBI score, viral load, age, cirrhosis, and gender.
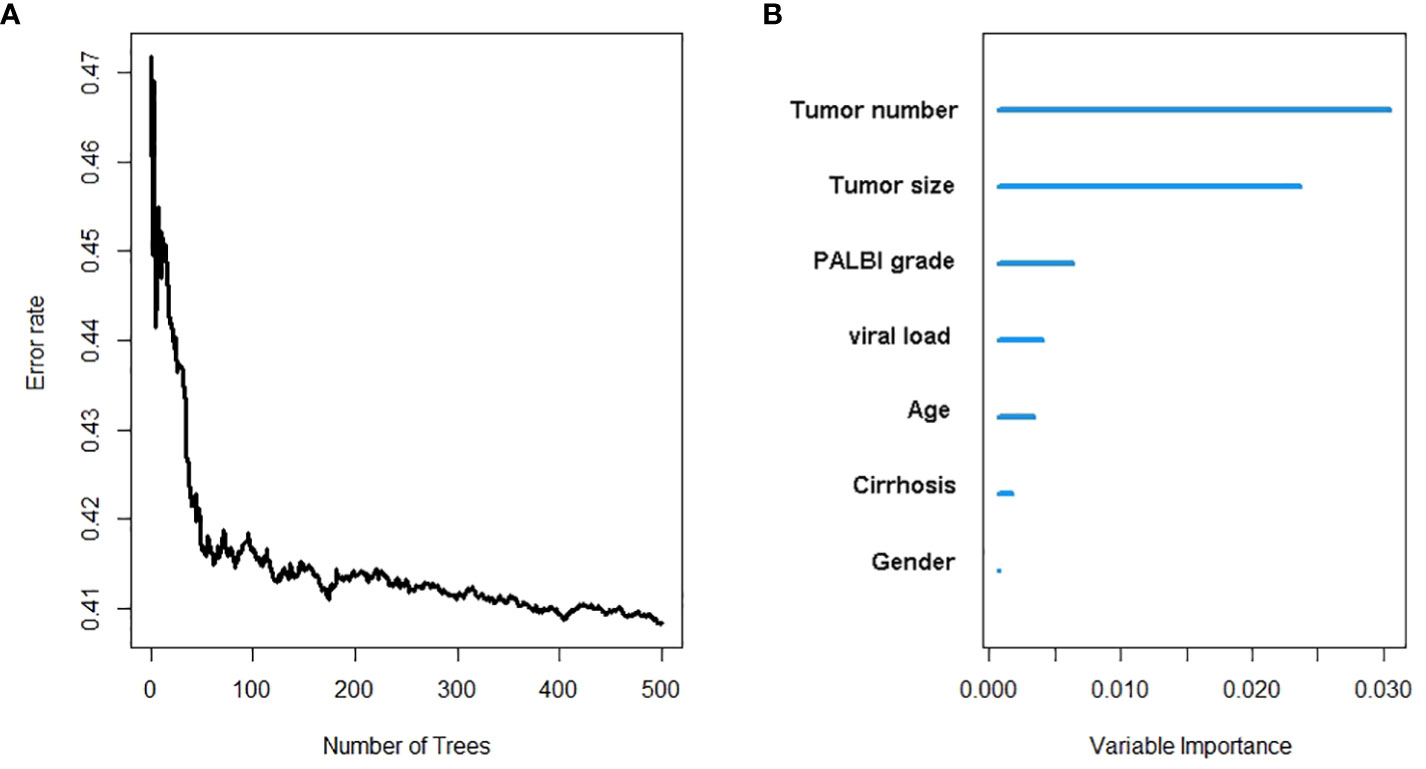
Figure 2 The recurrence risk analysis of HCC based on random survival forest. (A) Error rate of random survival forest; (B) out-of-bag variable importance ranking. HCC: hepatocellular carcinoma.
As the C-index of the Cox regression model was slightly higher than that of the RSF model, the Lasso-Cox regression model was finally used in this study to predict the recurrence of early-stage HCC patients. The calibration curves of the model built for predicting recurrence of 1, 3, and 5 years indicated a good consistency between the predicted and observed results in both the training set and validation set (Figure 3). The risk classes were generated in line with tertiles of predicted 1-, 3-, and 5-year recurrence rates and the K-M curves of recurrence were plotted based on the risk classes in the validation set. The results have showed that the model could well stratify patients according to tertiles, whether predicted 1-, 3-, or 5-year recurrence (Figures 4A–C). For comparison, the corresponding K-M curves of RSF model, whose performance was indeed not as good as the Cox regression model, made it reasonable to support the present results (Figures 4D–F).
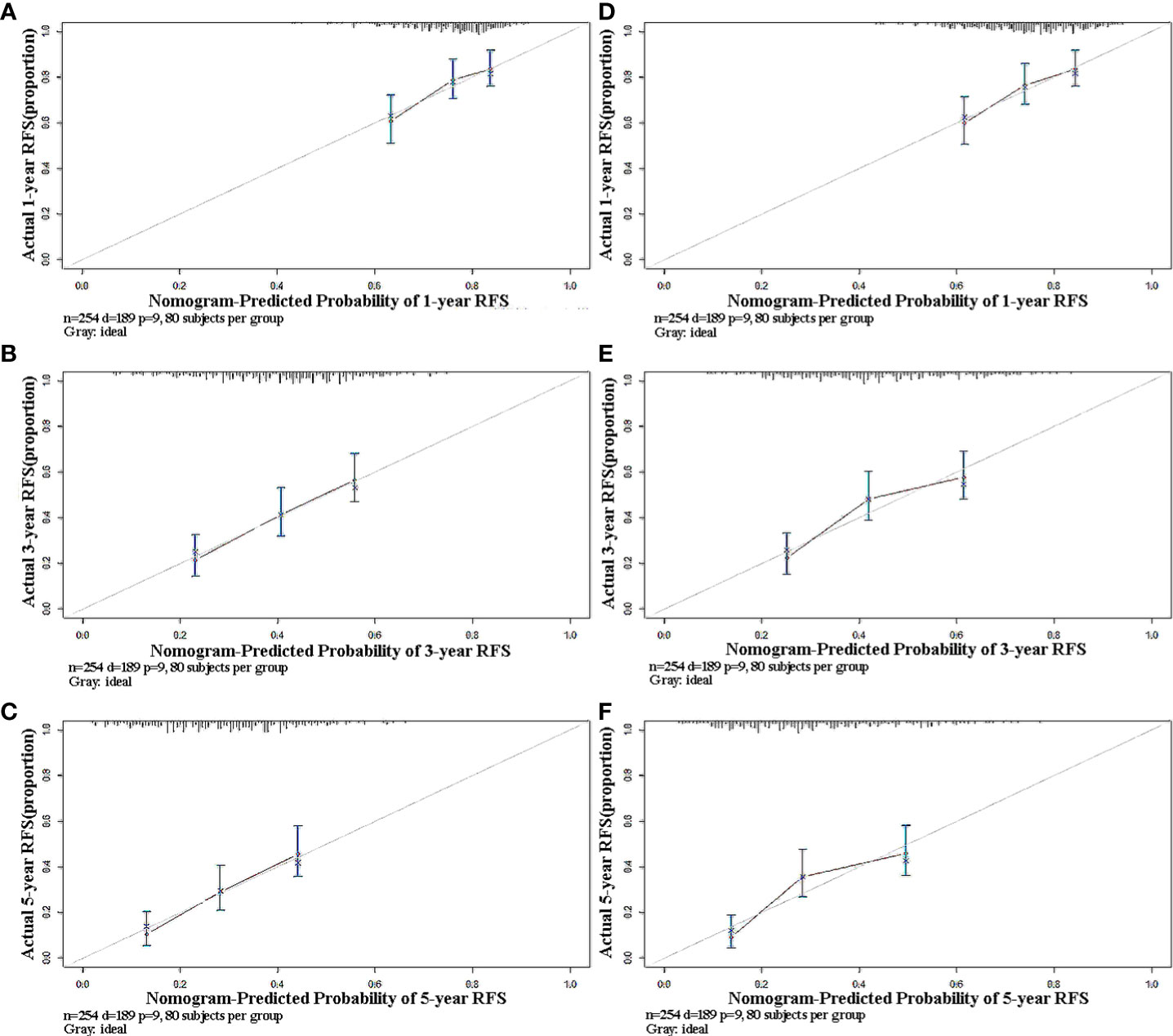
Figure 3 Calibration plots of predicted 1-, 3-, and 5-year RFS based on Cox regression modeling in the training set and validation set. (A–C) training set; (D–F) validation set. RFS, recurrence-free survival.
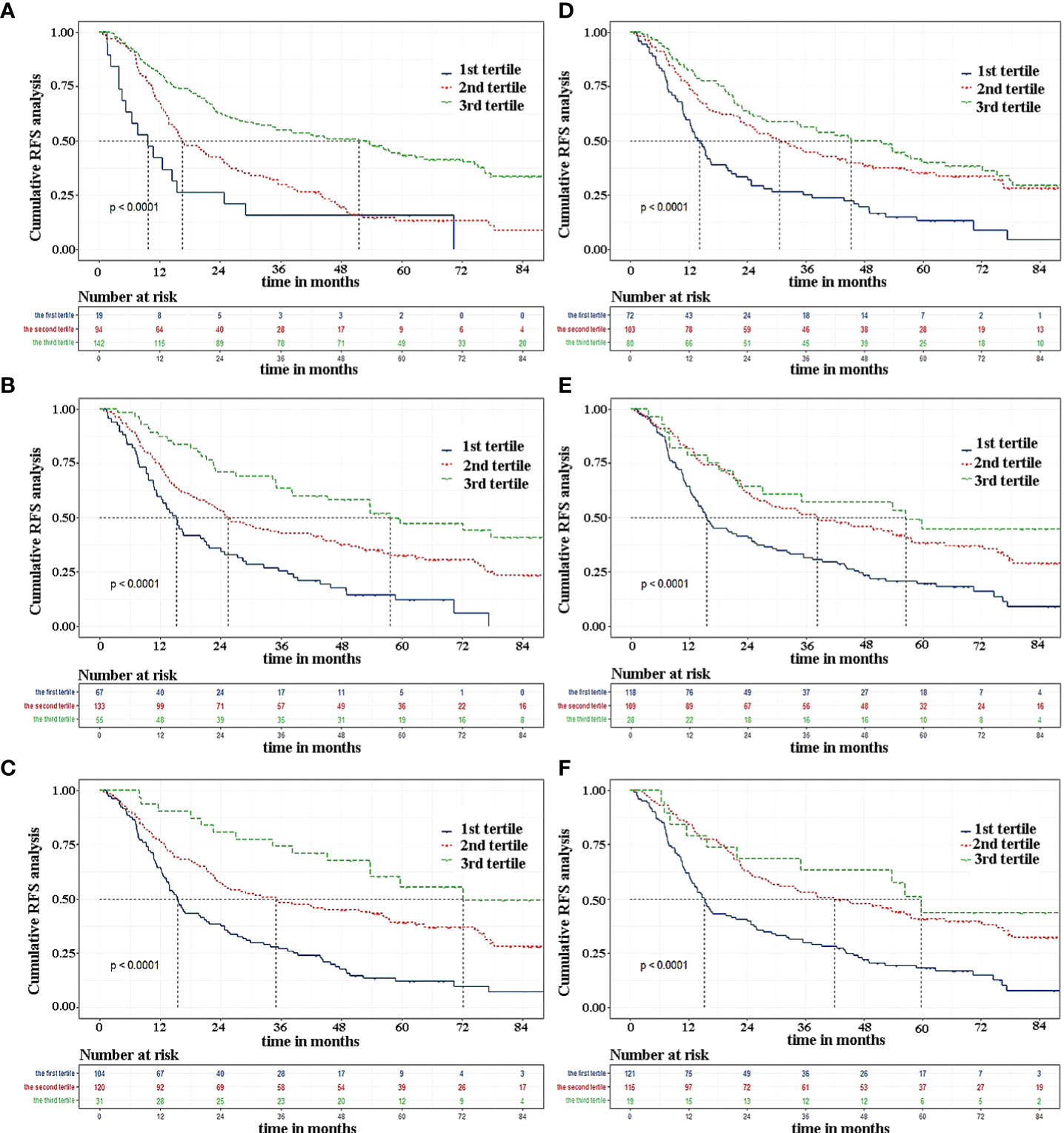
Figure 4 The Kaplan-Meier curves by tertiles of predicted 1-, 3, and 5-year RFS according to the two modeling approaches in validation set. (A–C) Cox regression modeling; (D–F) random survival forest. RFS, recurrence-free survival.
From what has been discussed above, we finally chose the Lasso-Cox regression model to predict the recurrence risk in early-stage HCC patients after treatment. To facilitate the clinical service, we converted the complex mathematical model into a nomogram (Figure 5). It was necessary to sum the scores of variables included in the model. And then a vertical line at the total score was drawn and making it intersect with the three lines representing the predicted RFS. The corresponding values of the point of intersection were the predicted 1-, 3-, and 5-year RFS of individuals. For example, a 75-year-old female patient with a history of cirrhosis, single tumor with tumor diameter more than 3cm, PALBI grade 2, and viral load less than1000 IU/mL, had about a total score of 202, with a 1-year RFS of 77%, a 3-year RFS of 48%, and 5-year RFS of 33%, respectively (Table 3). It could be seen that nomogram was more convenient to use in clinical practice than mathematical formulas.
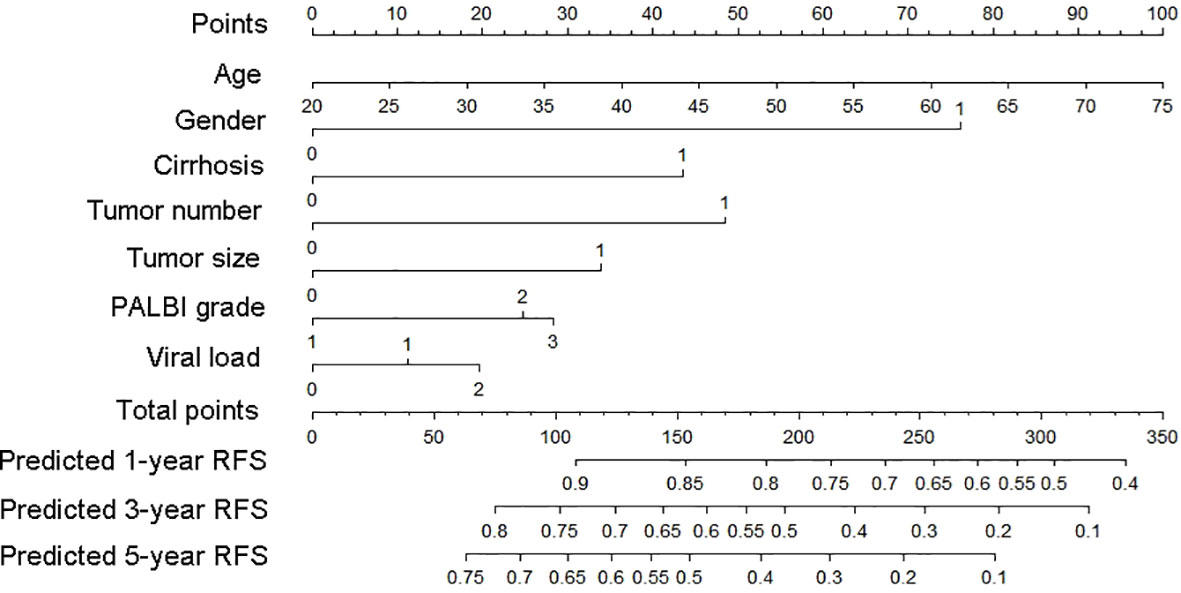
Figure 5 Nomogram used to predict time-related recurrence in patients with early-stage HCC. HCC, hepatocellular carcinoma.
As one of the most common malignant tumors in the world, HCC has posed a serious threat to human health. HCC patients in the early stage can be effectively treated with surgical resection, ablation, and liver transplantation. The 5-year OS of patients with early-stage HCC in our hospital who received TACE combined with ablation and achieved complete remission is about 75%. However, it cannot be ignored that the recurrence rate is as high as 70% after radical locoregional treatment, which is consistent with our results (2, 3). Therefore, it is necessary to analyze the risk factors affecting the recurrence of early-stage HCC patients and establish a prognostic model to make the individualized prediction of recurrence risk.
This study including 509 patients established a nomogram based on several variables screened by the Lasso regression. The model established involved seven clinically used indicators representing tumor burden (number and size of the tumor), viral replication strength (viral load), liver function status (cirrhosis and PALBI score), and demographic data (gender and age). A wide range of indicators could be used to comprehensively evaluate the specific situation of individuals, so as to well predict the risk of relapse. Variables were scored according to their contribution to the outcome, and the scores of these indicators included were summed. A vertical line at the position of the corresponding total scores was drawn to make it intersect with the three lines representing the predicted risk of recurrence. The values displayed at the intersection point were the predicted 1-, 3-, and 5-year RFS.
The established prediction model based on Lasso-Cox regression performed well in predicting relapse at both 3 and 5 years, and was able to clearly stratify patients into three groups according to personalized recurrence risk. However, as shown in Figure 4A, the model did not perform well in predicting 1-year recurrence and could only screen out patients at high risk of recurrence. But overall, this model still had large predictive advantages. To validate our result again, OS survival curves were plotted to explore whether patients with different predicted recurrence risks had different outcomes (Supplementary Figure S2). As we suspected, a high risk of relapse did predict a poor prognosis, which in turn confirmed the robustness of our model.
ALBI score, which included serum ALB and TBIL that represented synthetic and metabolic functions of the liver, was first proposed by Johnson et al. in 2015 (11). In the same year, Roayaie et al. improved on this basis by adding PLT indicating the degree of portal vein hypertension, namely the PALBI score (12). The PALBI and ALBI scores were initially used to assess the degree of liver decompensation in HCC patients. Both scoring systems, having higher accuracy of prediction than Child-Pugh classification and MELD score, could predict the prognosis of HCC patients undergoing surgery, ablation, or TACE and perform risk stratification, among which PALBI score was the best in predicting the survival of patients with poor liver function and patients receiving different treatments (13–15). In 2019, Ni et al. confirmed that the PALBI score had better predictive value than the ALBI score or Child-Pugh classification for HCC patients with large tumors receiving TACE combined with MWA (16). Similarly, Zhong et al. in 2021 also demonstrated that the PALBI score could better predict the risk of postoperative liver failure for patients undergoing hepatectomy (17). However, few studies discussed the predictive abilities of the PALBI score for early recurrence of HCC patients after radical minimally-invasive treatment, for which we took the PALBI score into consideration and confirmed its outstanding value in predicting recurrence.
The number and size of tumors suggested strong tumor aggressiveness and poor prognosis of HCC, which was currently uncontroversial and needed not be described here. Liver function impairment in patients with cirrhosis was a major risk factor for the occurrence of HCC. Even after radical treatment, the presence of unimproved liver tissue would still rise to recurrences. The International Liver Cancer Association has pointed out that cirrhosis was the only risk factor for the recurrence of HCC patients who survived more than 2 years after surgery, which indicated the adverse effect of liver cirrhosis on the prognosis of HCC (18). Some studies have shown that the elderly have decreased liver weight and blood flow velocity of portal vein, which together resulted in weaker liver repairability than that of young patients (19, 20). In addition, due to the low immunity of the elderly, the tumor progression after treatment was faster than in young patients, leading to a higher recurrence rate and poor prognosis. The present study also demonstrated that male patients had a higher recurrence rate compared to female patients, which might be due to discrepancies in biological, environmental, and behavioral factors between different genders. For example, estrogen might have a potential protective effect on HCC (21, 22). Long-term smoking and alcohol consumption in men often led to impaired liver function, which in turn contributed to a worse prognosis. It was well known that the risk factors of HCC recurrence included advanced age, maleness, tumor number, tumor size, cirrhosis, and the presence of microvascular invasion, all of which were irreversible. However, viral load was the only reversible parameter reflecting the level of viral replication, which was the key driver of liver injury and hepatocarcinogenesis (23). A high level of viral load was a potential adverse factor for prognosis, for which it was essential to take antiviral drugs for HCC patients with active viral replication.
Lasso regression, with an advantage over univariate analysis, could address the problem of multicollinearity among variables. And it was confirmed in the present study that compared with the Cox regression, the random survival forest did not have a better C-index. Therefore, a nomogram based on the Lasso-Cox regression model was established, which possessed a particular reference value for medical workers to analyze the individual risk of recurrence intuitively and had instructive significance for screening high-risk patients with relapse after locoregional treatment. In order to reduce the rate of recurrence and prolong overall survival, the decision maker could formulate individualized follow-up strategies or treatment plans according to the predicted recurrence risk. Although this study had a large sample size and external validation, the generalization ability of the model established was slightly weak since the data was from the same hospital. Therefore, a multi-center study with a large sample size was required for verification in the future.
The present study established a nomogram for predicting recurrence in patients with early-stage HCC based on the Lasso-Cox regression model. This nomogram was of some guiding significance for screening populations at high risk of recurrence after treatment, by which doctors could formulate individualized follow-up strategies or treatment protocols according to the predicted risk of relapse for patients to improve the long-term prognosis.
The original data supporting the results of this study are available from the corresponding author upon request.
The study has been approved by the ethics committee of the Beijing You’an Hospital affiliated to Capital Medical University. As a minimum risk study that was in accordance with the Helsinki protocol, the requirement for patients’ informed consent was waived by the same ethics committee that approved the study (Beijing You’an Hospital affiliated to Capital Medical University), and all methods were carried out in accordance with relevant guidelines and regulations.
YZ and JZ conceived and designed the protocol; JL and CZ collected the data; QW, WQ and HZ wrote the manuscript; JL and BL analyzed the data; TM and QW critically revised the manuscript. All authors contributed to the article and approved the submitted version.
This study was funded by a grant Beijing Municipal Natural Science Foundation (7191004), Capital Health Development Project (2020-1-2182 and 2020-2-1153), Beijing Key Laboratory (BZ0373), Beijing Municipal Administration of Hospitals’ Ascent Plan (DFL20181701), Key Medical Professional Development Plan of Beijing Municipal Administration of Hospitals (ZYLX201711), and Beijing Municipal Administration of Hospitals’ Incubating Program (PX2018059), and the National Key R&D Program of China (2020YFE0202400).
The authors highly appreciate all the patients who were involved in the present study and our team from Beijing You’an Hospital.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2022.1019638/full#supplementary-material
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin (2021) 71(3):209–49. doi: 10.3322/caac.21660
2. Villanueva A. Hepatocellular carcinoma. N Engl J Med (2019) 380:1450–62. doi: 10.1056/NEJMra1713263
3. Llovet JM, Kelley RK, Villanueva A, Singal AG, Pikarsky E, Roayaie S, et al. Hepatocellular carcinoma. Nat Rev (2021) 7:6. doi: 10.1038/s41572-020-00240-3
4. Wong JS, Wong GL, Tsoi KK, Ye R, Zhu Y, Zhou L, et al. Meta-analysis: the efficacy of antiviral therapy in prevention of recurrence after curative treatment of chronic hepatitis b-related hepatocellular carcinoma. Aliment Pharmacol Ther (2011) 33:1104–12. doi: 10.1111/j.1365-2036.2011.04634.x
5. Wen L, Weng S, Yan C, Ye R, Zhu Y, Zhou L, et al. A radiomics nomogram for preoperative prediction of early recurrence of small hepatocellular carcinoma after surgical resection or radiofrequency ablation. Front Oncol (2021) 11:657039. doi: 10.3389/fonc.2021.657039
6. Yang Y, Chen Y, Zhang XY, Xin Y, Wang Y, Li X, et al. Predictors and patterns of recurrence after radiofrequency ablation for hepatocellular carcinoma within up-to-seven criteria: A multi-center retrospective study. Eur J Radiol (2021) 138:109623. doi: 10.1016/j.ejrad.2021.109623
7. Zhang F, Lu SX, Hu KS, Gan YH, Chen Y, Ge NL, et al. Albumin-to-alkaline phosphatase ratio as a predictor of tumor recurrence and prognosis in patients with early-stage hepatocellular carcinoma undergoing radiofrequency ablation as initial therapy. Int J Hyperthermia (2021) 38(1):1–10. doi: 10.1080/02656736.2020.1850885
8. Tibshirani R. Regression shrinkage and selection via the lasso. J R Stat Soc Ser B Stat Methodol (1996) 58(1):267–88. doi: 10.1111/j.2517-6161.1996.tb02080.x
9. Heimbach JK, Kulik LM, Finn RS, Sirlin CB, Abecassis MM, Roberts LR, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. (2018) 67(1):358–80. doi: 10.1002/hep.29086
10. Strobl C, Boulesteix AL, Kneib T, Augustin T, Zeileis A. Conditional variable importance for random forests. BMC Bioinf (2008) 9:307. doi: 10.1186/1471-2105-9-307
11. Johnso PJ, BerhaneE S, Kagebayashi C, Satomura S, Teng M, Reeves HL, et al. Assessment of liver function in patients with hepatocellular carcinoma: A new evidence-based approach-the ALBI grad. J Clin Oncol (2015) 33(6):550 –558. doi: 10.1200/JCO.2014.57.9151
12. Roayaie S, Jibara G, Berhane S, Tabrizian P, Park JW, Yang J, et al. 851 PALBI-an objective score based on platelets, albumin bilirubin stratifies HCC patients undergoing resection & ablation better than child’s classification. Hepatology. (2015) 62:624A –690A. doi: 10.1002/hep.27745
13. Hansmann J, Evers MJ, Bui JT, Lokken RP, Lipnik AJ, Gaba RC, et al. Albumin-bilirubin and platelet-albumin- bilirubin grades accurately predict overall survival in high-risk patients undergoing conventional transarterial chemoembolization for hepatocellular carcinoma. J Vasc Interv Radiol (2017) 28(9):1224 –1231. doi: 10.1016/j.jvir.2017.05.020
14. Liu PH, Hsu CY, Hsia CY, Lee YH, Chiou YY, Huang YH, et al. ALBI and PALBI grade predict survival for HCC across treatment modalities and BCLC stages in the MELD era. J Gastroenterol Hepatol (2017) 32(4):879 –886. doi: 10.1111/jgh.13608
15. Lee SK, Song MJ, Kim SH, Park M. Comparing various sco ring system for predicting overall survival according to treatment modalities in hepatocellular carcinoma focused on platelet-albumin-bilirubin(PALBI) and albumin-bilirubin(ALBI) grade: A nationwide cohort study. PLos One (2019) 14(5):e0216173. doi: 10.1371/journal.pone.0216173
16. Ni JY, Fang ZT, An C, Sun HL, Huang ZM, Zhang TQ, et al. Comparison of albumin-bilirubin grade, platelet-albumin-bilirubin grade and child-Turcotte-Pugh class for prediction of survival in patients with large hepatocellular carcinoma after transarterial chemoembolization combined with microwave ablation. Int J Hyperthermia (2019) 36(1):841–53. doi: 10.1080/02656736.2019.1646927
17. Zhong WH, Zhang F, Huang KJ, Zou Y, Liu Y. Development and validation of a nomogram based on noninvasive liver reserve and fibrosis (PALBI and FIB-4) model to predict posthepatectomy liver failure grade b-c in patients with hepatocellular carcinoma. J Oncol (2021) 2021:6665267. doi: 10.1155/2021/6665267
18. Imamura H, Matsuyama Y, Tanaka E, Ohkubo T, Hasegawa K, Miyagawa S, et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol (2003) 38(2):200–7. doi: 10.1016/S0168-8278(02)00360-4
19. Schmucker DL. Aging and the liver: An update. J Gerontol A Biol Sci Med Sci (1986) 53(5):B315–20. doi: 10.1093/gerona/53a.5.b315
20. Zoli M, Iervese T, Abbati S, Bianchi GP, Marchesini G, Pisi E, et al. Portal blood velocity and flow in aging man. Gerontology. (1989) 35:61–5. doi: 10.1159/000213000
21. Ladenheim MR, Kim NG, Nguyen P, Le A, Stefanick ML, Garcia G, et al. Sex differences in disease presentation, treatment and clinical outcomes of patients with hepatocellular carcinoma: a single-centre cohort study. BMJ Open Gastroenterol (2016) 3(1):e000107. doi: 10.1136/bmjgast-2016-000107
22. Wu EM, Wong LL, Hernandez BY, Ji JF, Jia W, Kwee SA, et al. Gender differences in hepatocellular cancer: disparities in nonalcoholic fatty liver disease/steatohepatitis and liver transplantation. Hepatoma Res (2018) 4:66. doi: 10.20517/2394-5079.2018.87
Keywords: nomogram, Lasso-Cox regression, hepatocellular carcinoma, prediction, recurrence
Citation: Wang Q, Qiao W, Zhang H, Liu B, Li J, Zang C, Mei T, Zheng J and Zhang Y (2022) Nomogram established on account of Lasso-Cox regression for predicting recurrence in patients with early-stage hepatocellular carcinoma. Front. Immunol. 13:1019638. doi: 10.3389/fimmu.2022.1019638
Received: 15 August 2022; Accepted: 31 October 2022;
Published: 23 November 2022.
Edited by:
Ming Kuang, The First Affiliated Hospital of Sun Yat-sen University, ChinaCopyright © 2022 Wang, Qiao, Zhang, Liu, Li, Zang, Mei, Zheng and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yonghong Zhang, emhhbmd5aEBjY211LmVkdS5jbg==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.