
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Immunol., 29 November 2021
Sec. Vaccines and Molecular Therapeutics
Volume 12 - 2021 | https://doi.org/10.3389/fimmu.2021.781161
This article is part of the Research TopicVaccines and approaches that target trained immunity in COVID-19: immunological mechanisms of action and deliveryView all 14 articles
 Jian Wu1
Jian Wu1 Quanman Li1
Quanman Li1 Clifford Silver Tarimo1
Clifford Silver Tarimo1 Meiyun Wang2
Meiyun Wang2 Jianqin Gu3
Jianqin Gu3 Wei Wei2
Wei Wei2 Mingze Ma1
Mingze Ma1 Lipei Zhao1
Lipei Zhao1 Zihan Mu1
Zihan Mu1 Yudong Miao1*
Yudong Miao1*Globally, vaccine hesitancy is a growing public health problem. It is detrimental to the consolidation of immunization program achievements and elimination of vaccine-targeted diseases. The objective of this study was to estimate the prevalence of COVID-19 vaccine hesitancy in China and explore its contributing factors. A national cross-sectional online survey among Chinese adults (≥18 years old) was conducted between August 6, 2021 and August 9 via a market research company. We collected sociodemographic information; lifestyle behavior; quality of life; the knowledge, awareness, and behavior of COVID-19; the knowledge, awareness, and behavior of COVID-19 vaccine; willingness of COVID-19 vaccination; accessibility of COVID-19 vaccination services; skepticism about COVID-19 and COVID-19 vaccine; doctor and vaccine developer scale; and so on. Odds ratios (OR) with 95% confidence intervals (CI) were used to estimate the associations by using logistic regression models. A total of 29,925 residents (48.64% men) were enrolled in our study with mean age of 30.99 years. We found an overall prevalence of COVID-19 vaccine hesitancy at 8.40% (95% CI, 8.09–8.72) in primary vaccination and 8.39% (95% CI, 8.07–8.70) in booster vaccination. In addition, after adjusting for potential confounders, we found that women, higher educational level, married residents, higher score of health condition, never smoked, increased washing hands, increased wearing mask, increased social distance, lower level of vaccine conspiracy beliefs, disease risks outweigh vaccine risk, higher level of convenient vaccination, and higher level of trust in doctor and developer were more willing to vaccinate than all others (all p < 0.05). Age, sex, educational level, marital status, chronic disease condition, smoking, healthy behaviors, the curability of COVID-19, the channel of accessing information of COVID-19 vaccine, endorsement of vaccine conspiracy beliefs, weigh risks of vaccination against risks of the disease, making a positive influence on the health of others around you, and lower trust in healthcare system may affect the variation of willingness to take a COVID-19 vaccine (all p < 0.05). The prevalence of COVID-19 vaccine hesitancy was modest in China, even with the slight resulting cascade of changing vaccination rates between the primary and booster vaccination. Urgent action to address vaccine hesitancy is needed in building trust in medical personnel and vaccine producers, promoting the convenience of vaccination services, and spreading reliable information of COVID-19 vaccination via the Internet and other media.
Vaccination is the most cost-efficient method of avoiding infectious diseases and has been one of the most effective public health interventions to date (1–4). The effectiveness of the COVID-19 vaccination depends solely on its uptake. If there are individuals who are hesitant or unwilling to be immunized, the vaccination coverage will be limited. A study indicated that a refusal rate of more than 10% is estimated to be sufficient to weaken the population benefits of vaccination against COVID-19 (5). Since the global outbreak of COVID-19, researchers from all around the world have been working tirelessly and collaboratively to develop the vaccines against the virus. Numerous types of vaccines are currently available including inactivated vaccines, recombinant protein vaccines, adenovirus vector vaccines, attenuated influenza virus vector vaccines, and nucleic acid (mRNA and DNA vaccines) vaccines (6). However, this global effort might be hampered by vaccine hesitancy despite its availability (7).
Vaccine hesitancy has been identified as one of the greatest threats to public health at a global level (8) and a common phenomenon in the developed world for decades (9–11). However, the prevalence of COVID-19 vaccine hesitancy is chaotic globally, posing a significant obstacle to the global efforts to containing the current COVID-19 pandemic. A recent review of vaccine acceptance rates demonstrated that developed countries such as the USA, France, and Italy generally have expected vaccine acceptance rates of less than 60% (ranging from 53.7% to 58.9%). Meanwhile, low rates of COVID-19 vaccine acceptance were reported in the Middle East, Russia, Africa, and several European countries as well (11). However, the current analytics show that countries like China, Malaysia, and Ecuador are expected to have uptake rates of more than 90% (ranging from 91.3% to 97.0%) (12). In addition, another recent survey in the UK showed that 16.9% of respondents were hesitant about the vaccine (13). While a survey conducted in Hong Kong, China, showed a shift in the predicted uptake rate from 44.2% to 34.8% at different waves of local epidemic among the population (14).
The reasons for COVID-19 vaccination hesitancy are varied and, to some extent, unclear. Earlier research examined the complex nature of vaccine hesitancy by examining the epidemiologic triad of environmental, agent, and host factors (i.e., EAH framework) (15). Environmental factors include public health policies, social factors, and media messaging (16, 17) while the agent (vaccine and disease) factors include the perception of vaccine safety and effectiveness, besides the perceived susceptibility to the disease (18). Host factors are dependent on knowledge, previous experience, and educational and income levels (19). Recent research indicates that vaccine hesitation is frequently framed in terms of complacency, confidence, and convenience (3Cs framework). Vaccine hesitation occurs when there is a low perception of the necessity for vaccination (referred to as complacency), worries about the efficacy and safety of the vaccine (referred to as low confidence), and a lack of vaccine accessibility (referred to as convenience) (20). Based on the frameworks, youth, female gender, low income, low education, high informational reliance on social media, low informational reliance on print and broadcast media, membership of other than white ethnic groups, low perceived risk from COVID-19, and low trust in scientists, medics, and biomedical science, as well as (to a much lesser extent) low trust in government were all recognized as relevant factors that may affect COVID-19 vaccine hesitancy. Similar associations have been observed in countries including Canada, USA, Europe, Australia, Japan, Middle East, Russia, and Africa. The incidence of COVID-19 vaccination hesitancy has been researched, as well as how it is influenced by socioeconomic position, particularly individual psychological characteristics. However, such information is lacking in China.
China may be a world leader in COVID-19 vaccination coverage not only because it constitutes one-fifth of the world’s population but also because the country is becoming increasingly interconnected with the rest of the world. Although more than 62.4% (880 million) of the Chinese population have been officially confirmed to be vaccinated so far, some residents are still hesitant to get vaccinated (21). We therefore sought to expand on the EAH and 3C frameworks in order to better explain COVID-19 vaccine hesitancy among Chinese. Therefore, we conducted a nation-wide survey in 31 provinces across mainland China during the period of primary and booster vaccination of COVID-19 vaccines. We calculated the level of COVID-19 vaccine hesitancy (delay or refusal) in a large sample by analyzing expressed readiness to get an approved vaccination and identifying subgroups within the population and regions where it may be higher. Our major objective was to gain a better understanding of vaccine hesitancy on an individual psychological level to guide methods for increasing vaccination acceptance rates.
On July 10, 2021, we performed a preliminary online survey in Zhongmou County, Henan Province. We conducted a face-to-face interview with participants from a representative village and community obtained through cluster sampling approach. Basing on the vaccine hesitation rate and the reliability and validity of the questionnaire of the preliminary online survey, we estimated the minimum sample size required for the formal survey to be 6,638 participants, which was based on a prevalence of COVID-19 vaccine hesitancy of 16.57% in a preliminary online survey, an allowable error of 1%, a 95% confidence level, and an anticipated design effect of two. A subsequent national cross-sectional online survey using a snowball sampling method among Chinese adults (≥18 years old) was conducted from August 6, 2021 via a market research company. The invited respondents were unaware of the topic prior to their tentative consent to complete the survey. In order to ensure that the sample size for this study was large enough to estimate the prevalence of vaccine hesitancy, a sample saturation was monitored during the investigation. Saturation, in this study, refers to the point at which the sample size reaches a specific size whereby the vaccine hesitancy rate becomes constant and no longer varies considerably with the snowballing sample size growth. We found that when the number of valid questionnaires reached 21,780, the sample began to saturate (Appendix Figure 1). We ended the online survey when the valid sample reached 29,925 on August 9, 2021. The flowchart of participant selection and sample saturation monitoring procedures are shown in Figure 1.
Due to the absence of a uniform COVID-19 vaccine hesitancy scale in China, we designed two items to assess whether there was a delay in immunization acceptance or refusal based on the Oxford COVID-19 Vaccine Hesitancy Scale (13). The items comprised themes “In terms of COVID-19 vaccination in current stage, I would describe myself as” for estimating hesitancy rate in primary vaccination and “I would describe my attitude towards regularly receiving a COVID-19 vaccine in the future as” for predicting hesitancy rate in booster vaccination in future. For each item, item-specific response options coded from 1 to 5 were used, including (1) Vaccination, (2) Willing to get the COVID-19 vaccine, (3) Delay to getting the COVID-19 vaccine, (4) Unwilling to get the COVID-19 vaccine, and (5) Anti-vaccination.” Higher scores indicated a higher level of vaccine hesitancy. According to the definition of vaccine hesitancy, options (1) and (2) were merged into “Acceptance” and options (3), (4), and (5) were merged into “Hesitancy” during data analysis. Based on the EAH and 3C frameworks, our questionnaire subsequently collected exploratory and confirmatory factors from four aspects, namely, (1) individual characteristics (i.e., social-demographic information, subjective social status, health status), (2) COVID-19 pandemic progress perception (i.e., awareness of COVID-19 blocking, judgement of the trend, pandemic skepticism), (3) COVID-19 vaccine perception (i.e., general knowledge on vaccine, COVID-19 vaccination perception, vaccine skepticism), and (4) the healthcare system dimension (trust in doctors and vaccine developers, convenience of vaccination). All questionnaires are shown in Appendix 1.
The Chi-square goodness-of-fit test was used to monitor sample saturation throughout the formal online survey to determine sample underrepresentation error. An independent samples t-test or Chi-square test was carried out to test differences in willingness to get vaccinated across groups. Binary logistic regression analyses were conducted to examine factors associated with COVID-19 vaccine hesitancy and COVID-19 pandemic progress perception, COVID-19 vaccine perception, and trust in healthcare system after controlling for demographic and socioeconomic confounders. Multinomial logistic regression model was applied to assess between associated factors and transformations of COVID-19 vaccine hesitancy. The collinearity test was carried out to assess the correlation between independent variables using a variance inflation factor (VIF) <4, and no collinearity was detected. A sensitivity analysis was performed by excluding participants suffered from chronic diseases to test the robustness of model results and assess source of model uncertainty. We did all statistical analyses using SAS 9.4. Differences were regarded as statistically significant if p values were less than 0.05.
This study was deemed exempt by the Life Science Ethics Review Committee of Zhengzhou University.
A total of 29,925 residents from 31 provinces of Chinese mainland were included in the current study. A summary of the sociodemographic, awareness of COVID-19 pandemic, COVID-19 vaccine exception, trust in healthcare system, and hesitancy of all study participants is provided in Table 1. In all, 2,514 (8.40%, 95% confidence interval (CI) 8.09% to 8.72%) participants endorsed clear vaccine hesitancy response in primary vaccination. Furthermore, 2,510 (8.39%, 95% CI 8.07% to 8.70%) expressed their hesitancy in booster vaccination of COVID-19 vaccine. We found that the prevalence of vaccine hesitancy was higher in men than women in all age groups (Appendix Figure 2). Higher prevalence in both phrases were observed among population with elders (age ≥60 years), men, lower educational level, minority, religious beliefs, not in marriage, higher subjective social status, lower self-report health condition, suffered from chronic diseases, current smoker, former drinker, extreme endorsement of COVID-19, vaccine conspiracy beliefs, medium or low possibility of curability of COVID-19, inconvenience of vaccination, and lower trust in healthcare system. The hesitancies in both phases varied substantially by the province in mainland China. More than one in 10 of the study population in Beijing, Hebei, and Tianjin were observed to be hesitant to uptake the vaccine in current stage after standardizing age and sex. In terms of predicted hesitancy in the booster vaccination, the age- and sex-standardized prevalence of hesitancy in Beijing, Tianjin, Hebei, and Hainan were more than 10%, ranging from 10.13% to 15.76% (Figure 2; Appendix Table 1).
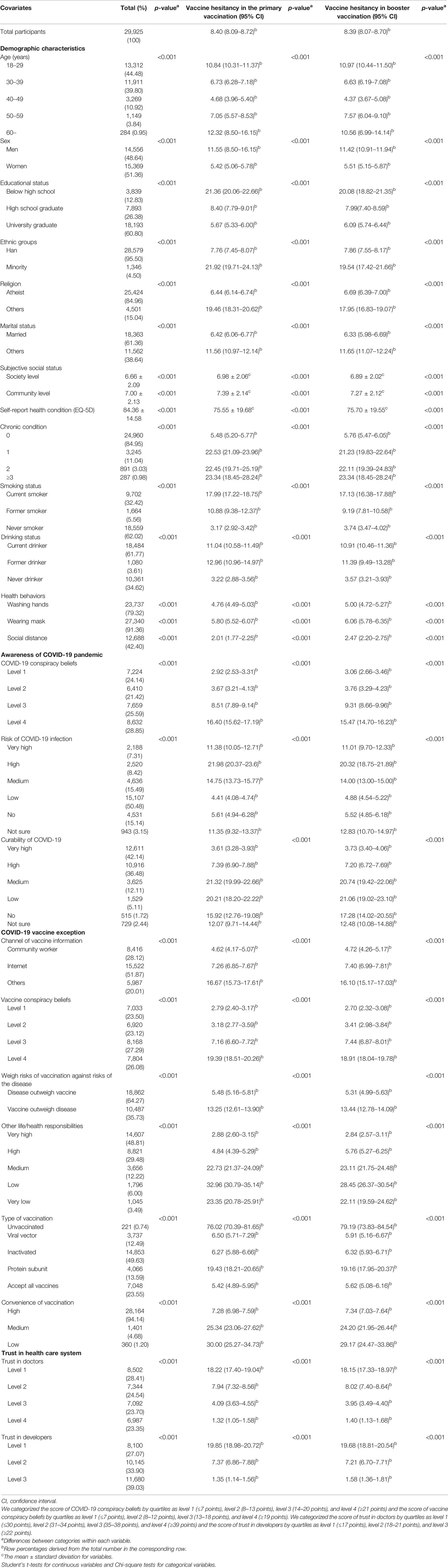
Table 1 Sociodemographic, awareness of COVID-19 pandemic, COVID-19 vaccine exception, trust in healthcare system, and COVID-19 vaccine hesitancy of all study participants.
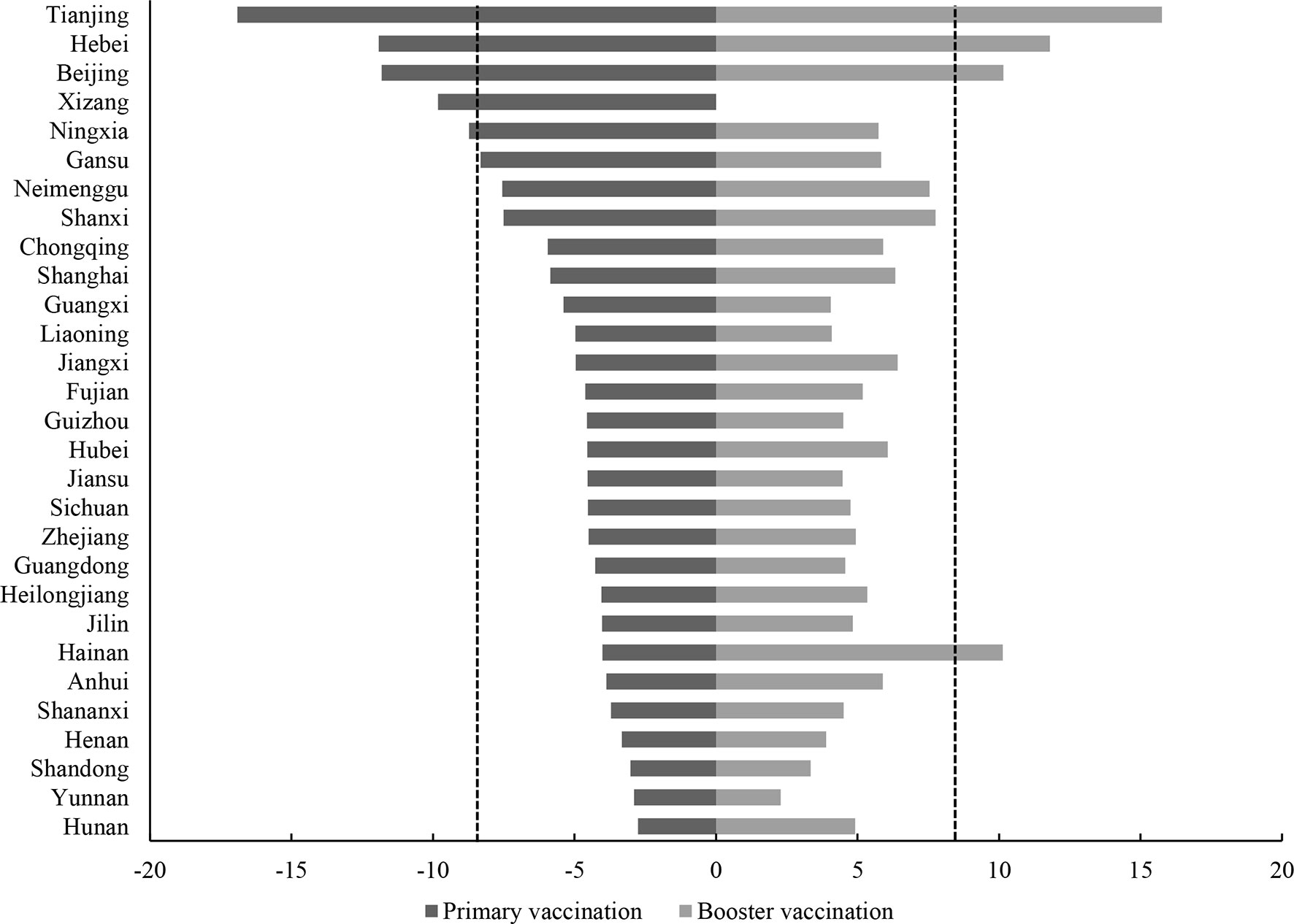
Figure 2 Age- and sex-standardized prevalence of COVID-19 vaccine hesitancy by province in primary vaccination (left) and booster vaccination (right). Qinghai and Xinjiang province were not shown.
In the binary logistic regression model among all study participants, age, sex, educational level, marital status, self-report health condition, subjective social status in community level, smoking status, drinking status, healthy behaviors, the risk of COVID-19 infection, the curability of COVID-19, the channel of accessing information of COVID-19 vaccine, endorsement of vaccine conspiracy beliefs, weigh risks of vaccination against risks of the disease, other life/health responsibilities, inconvenience of vaccination, and lower trust in healthcare system were independent factors associated with hesitancy on COVID-19 primary vaccination. A similar pattern of hesitancy in the booster vaccination was also shown among the subjects (Table 2).
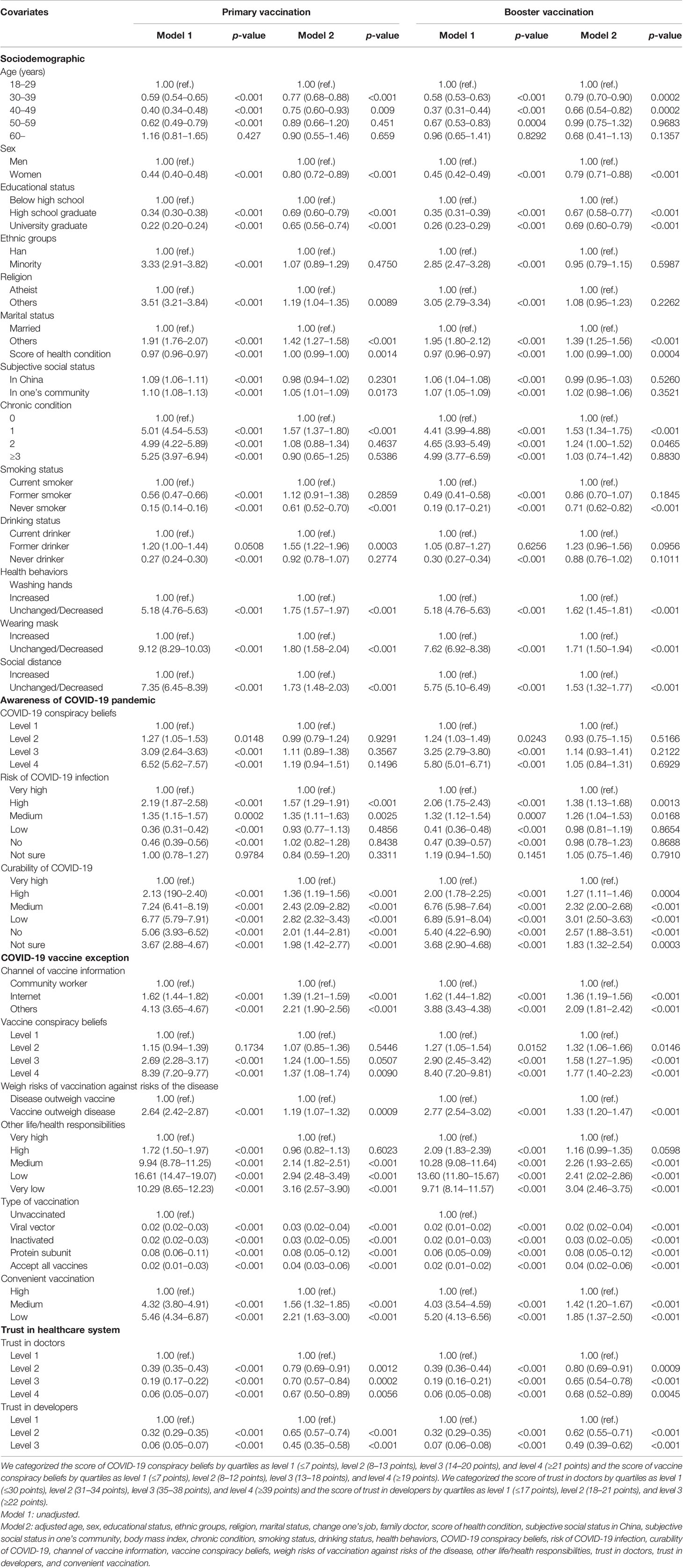
Table 2 Associations between COVID-19 vaccine hesitancy and sociodemographic, awareness of COVID-19 pandemic, COVID-19 vaccine exception, and trust in healthcare system.
Our study highlighted that the prevalence of vaccine hesitancy among Chinese residents remains at a low and stable level, with a slight shift from 8.40% to 8.39% (95% CI, 8.07 to 8.70) that was observed between the primary and booster vaccinations. In detail, 88.02% and 4.81% of the population responded in a consistent acceptance and hesitancy towards taking a COVID-19 vaccine in both phases, respectively. Notably, there were also individuals who showed varying levels of willingness to take vaccines. In summary, 3.58% of respondents declared an acceptance of rejection, whereas 3.59% of those who were previously hesitant became willing to receive vaccination (Table 3). The associations of COVID-19 vaccine hesitancy transformations and socio-demographic, awareness of COVID-19 pandemic, COVID-19 vaccine exception, and trust in healthcare system were summarized in Table 3. The variation of willingness (i.e., acceptance to hesitancy, hesitancy to acceptance, hesitancy to hesitancy) to take a COVID-19 vaccine was associated with age, sex, educational level, marital status, chronic disease condition, smoking, healthy behaviors, the curability of COVID-19, the channel of accessing information of COVID-19 vaccine, endorsement of vaccine conspiracy beliefs, weigh risks of vaccination against risks of the disease, other life/health responsibilities, and lower trust in healthcare system were independent.
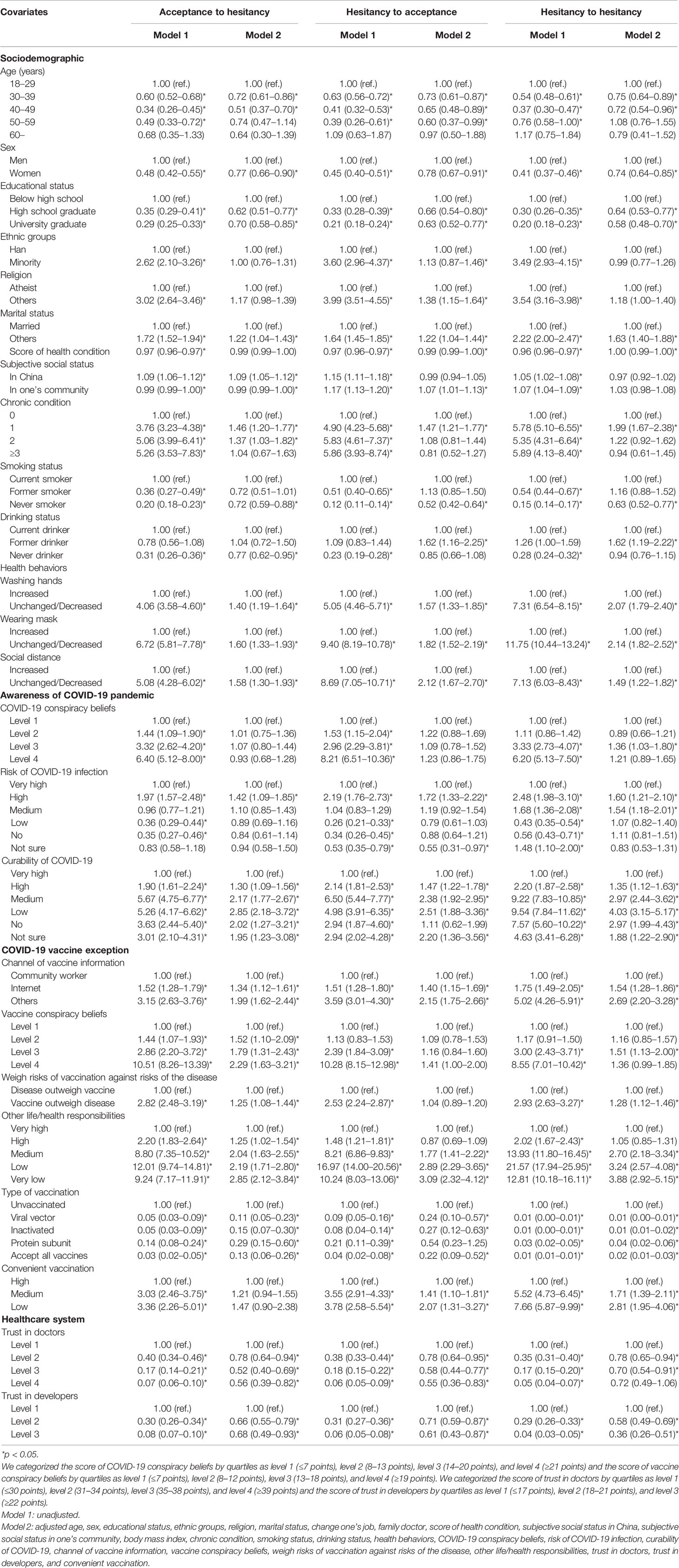
Table 3 Associations between COVID-19 vaccine hesitancy transformations and sociodemographic, awareness of COVID-19 pandemic, COVID-19 vaccine exception, and trust in healthcare system.
In sensitivity analyses, exclusion of cases with chronic disease did not appreciably alter the findings for vaccine hesitancy. The effect estimates remained similar for the main results (Appendix Table 2).
The current study examined the prevalence of COVID-19 vaccine hesitancy in a large representative sample of 31 provinces of mainland China. Our findings indicated that a sizable majority (88.02%) of mainland Chinese citizens express their readiness to be vaccinated. It is possible that this proportion will remain robust throughout the upcoming COVID-19 vaccine booster, but this is likely to be researched and confirmed. Our predicted vaccine hesitancy rate is comparable with earlier research conducted on the majority of the Chinese residents. According to these surveys, the vaccination rate among Chinese residents was found to be around 80%. The reason for the lower vaccination hesitancy rate, or for the greater vaccine acceptance rate, is mostly attributable to the following factors: Firstly, China has established a vaccine management law and successfully passed the World Health Organization’s evaluation of its National Vaccine Regulatory System (NRS) which guarantees its quality and supply of the vaccine (22, 23). Secondly, China has consistently enhanced postmarket surveillance of vaccinations, with an emphasis on the safety and effectiveness of the vaccine while making a consistent follow-up on the incidences of vaccine-preventable disease as well as public acceptance of the vaccines. In addition, tracking the experience of vaccine use together with the development of vaccine big data are still ongoing (24). Thirdly, China has strengthened risk communication to ensure that recipients and the public have a consciousness of the benefits and risks of vaccination and to actively disseminate the scientific concept that the overall benefits of the vaccination greatly outweigh the risks. Finally, China has engaged in expanding vaccine availability, which requires vaccination services to be tailored to the characteristics of the jurisdiction area and population, as well as a reasonable distribution of vaccination clinics.
At the provincial level, the prevalence of COVID-19 vaccine hesitation varies greatly. Our results show that among the 31 provinces, the prevalence of vaccine hesitancy was more than 10% in three provinces. The reason for this level of hesitancy is not yet clear, and a variety of factors may be involved. Since the first vaccine was approved for marketing in mainland China on December 31, 2020, various provinces have made strenuous efforts to increase primary vaccination rates, but there are significant differences in the demographic structure, health literacy, prevalence of chronic diseases, and vaccination service supply capacity among provinces. It is likely that the combination of these factors has led to the uneven distribution of vaccine hesitation rates among provinces. With 4.81% of the population refusing to receive a COVID-19 vaccination, in the current study, the timeline for eradicating the pandemic may be delayed, resulting in widespread of vaccine hesitancy, wreaking havoc on individuals and the healthcare systems. Thus, in the future, policy development in China should prioritize minimizing existing inequalities among provinces when it comes to vaccination.
COVID-19 vaccine hesitancy increases with inconvenience of vaccination. Although China established tens of thousands of temporary vaccination sites in a relatively short time, vaccination service is provided through appointments and the waiting time at the vaccination site is frequently longer due to limited health personnel resources and a shortage of vaccines. This situation brings a lot of inconvenience to vaccinators and may have played a significant role towards vaccine acceptance rate. In order to effectively prevent the spread of the virus, vaccinators have to be registered through a reliable and user-friendly appointment system. Additionally, the majority of residents in China are not yet accustomed to vaccine appointments, which creates a considerable “sense of inconvenience” for vaccinators, which in turn causes some people to have doubts about whether to receive a vaccination. Therefore, for improving COVID-19 vaccination uptake, it is particularly important to improve the experience of vaccination services. Key measures that should also be considered include increasing the number of vaccination personnel, vaccine supply, encouraging qualified medical institutions to provide vaccination services, and actively using digital technologies to reduce waiting time (25–27).
There is a considerable link between doctor and vaccine developer distrust and COVID-19 vaccine hesitation. In essence, willingness to take a vaccination is a matter of trust: that the vaccine is necessary, that it will function, and that it is safe. Due to recent vaccination-related adverse events and instances of counterfeit vaccine, the public’s trust in medical professionals and vaccine developers has decreased significantly (28). To build faith in the vaccine, the vaccination service organization should, on the one hand, expand the number of vaccination medical personnel, train and develop doctor-patient communication skills, and improve the quality of vaccination service evaluation. China should also accelerate the development of a vaccine industry credibility system, encourage vaccine production, and encourage companies to take the lead in vaccine production and circulation while ensuring the quality and safety of vaccine products from development stage to circulation. In addition, recommending the one vaccine in which at the given moment is with the highest level of the public willingness will likely result in a less prevalence of COVID-19 vaccination hesitancy.
It is worth mentioning that when the role of gender in COVID-19 vaccine hesitancy was assessed, males were shown to be more likely to reject the vaccine. The finding was consistent with a previous research in which a higher vaccine acceptance rate was associated with men’s increased perception of COVID-19 vaccine and decreased belief in disease-related conspiracy theories (11). However, our research was carried out at the stage when the vaccination rate had already exceeded 60%. As information about the COVID-19 vaccination circulated, women may have become fully aware of the implications of the disease and so lost belief in conspiratorial claims, implying that their vaccine hesitancy rate was found to be lower than that of males. In the future COVID-19 vaccination, attention should be paid to increasing the vaccination rate of men. Additionally, age, men, educational level, marital status, self-report health condition, subjective social status, smoking status, healthy behaviors, the curability of COVID-19, the channel of accessing information of COVID-19 vaccine, endorsement of vaccine conspiracy beliefs, weigh risks of vaccination against risks of the disease, and other life/health responsibilities were all found to be independently associated with COVID-19 vaccine hesitancy. Numerous reports show that the mechanism underlying vaccine hesitancy is exceedingly complicated, and that effective countermeasures should be implemented concurrently (17, 20, 29, 30). Firstly, we think that assisting persons with poor information and insufficient health literacy in obtaining a correct understanding of vaccines through education may play a critical role. Government authorities should also communicate clearly and consistently in order to instill public confidence in vaccination programs. This involves describing how vaccines function and are created, from recruiting to regulatory approval based on safety and efficacy. Effective campaigns should also carefully describe the level of effectiveness of a vaccine, the duration of protection (with multiple doses if necessary), and the critical nature of population-wide coverage in order to attain the herd immunity. Secondly, vaccine information transmitted by the Internet and the media should be effectively identified and any misleading information must be eliminated. The Internet and other forms of media should serve as a link between vaccination services and the general population through disseminating vaccine knowledge received through official channels and eradicating social misconceptions about the vaccines.
This is the first large-scale study to assess the prevalence and associated factors of COVID-19 vaccination hesitancy in a large, saturated sample of the Chinese population. Due to the saturation of the sample, we can be certain that our estimate of vaccine hesitancy is accurate. To provide more extensive explanatory variables, we adopted the most widely accepted international definition of vaccine hesitancy and collected data using the EAH and 3C frameworks. One of the major limitations of the current study is that it relies on self-reports of willingness to take a COVID-19 vaccination to assess vaccine hesitancy, and we were unable to develop a standard for validation due to the lack of a universal scale to assess COVID-19 vaccine hesitancy in China. Due to the fact that an accurate assessment of COVID-19 vaccine hesitancy can serve as an important basis for vaccine development and production, as well as the estimation of market demand, the development of a global scale for COVID-19 vaccine hesitancy assessment will become one of the important directions of future research. However, the COVID-19 vaccine hesitancy was assessed from a reliable questionnaire and the results of it was similar with previous studies according to the Oxford COVID-19 Vaccine Hesitancy Scale (13, 31). Another shortcoming of the study includes its cross-sectional design, which precluded the establishment of a cause-and-effect link. Finally, despite the fact that we used data from a large saturation sample of the population from 31 provinces, due to the epidemic, we were forced to collect data via online questionnaires utilizing the snowball sampling approach. Therefore, these research findings may differ from those estimated using probability sampling. In addition, the influence of socioeconomic level on COVID-19 vaccination hesitancy observed in this study may not be applicable to persons without Internet access.
Despite the aforementioned constraints, COVID-19 vaccination hesitancy prevalence in China is modest in comparison with other countries. This will lay a solid foundation for future booster vaccinations. However, interprovincial disparities in COVID-19 vaccine hesitation may delay the onset of herd immunity, and local vaccination efforts should be stepped up in Tianjin, Hebei, Beijing, and Hainan provinces due to their significantly greater frequency of COVID-19 vaccine hesitancy. Emphasis should be placed on building trust in medical personnel and vaccine producers, promoting the convenience of vaccination services, and spreading reliable COVID-19 vaccine information via the Internet and other media.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Conceptualization: YM, JW, QL, MW, and JG. Data curation: YM, QL, WW, and MM. Formal analysis: JW, QL, and YM. Funding acquisition: MW and JG. Investigation: JW, YM, QL, MM, LZ, and ZM. Methodology: YM, JW, QL, and CT. Project administration: JW. Resources: JW and YM. Software: QL, LZ, and ZM. Writing—original draft: JW, YM, QL, and CT. Writing—review and editing: YM, CT, MW, and JG. All authors contributed to the article and approved the submitted version.
This study is supported by the National Social Science Fund of China (number 21BGL222); the Collaborative Innovation Key Project of Zhengzhou (number 20XTZX05015); Joint Project of National Health Commission and Henan Province (number SB201901072); 2021 Postgraduate Education Reform and Quality Improvement Project of Henan Province (number YJS2021KC07); Performance Evaluation of New Basic Public Health Service Projects in Henan Province (number 2020130B).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2021.781161/full#supplementary-material
1. Abbas K, Procter SR, van Zandvoort K, Clark A, Funk S, Mengistu T, et al. Routine Childhood Immunisation During the COVID-19 Pandemic in Africa: A Benefit–Risk Analysis of Health Benefits Versus Excess Risk of SARS-CoV-2 Infection. Lancet Global Health (2020) 8(10):e1264–72. doi: 10.1016/s2214-109x(20)30308-9
2. Debellut F, Clark A, Pecenka C, Tate J, Baral R, Sanderson C, et al. Evaluating the Potential Economic and Health Impact of Rotavirus Vaccination in 63 Middle-Income Countries Not Eligible for Gavi Funding: A Modelling Study. Lancet Global Health (2021) 9(7):e942–56. doi: 10.1016/s2214-109x(21)00167-4
3. Jentsch PC, Anand M, Bauch CT. Prioritising COVID-19 Vaccination in Changing Social and Epidemiological Landscapes: A Mathematical Modelling Study. Lancet Infect Dis (2021) 21(8):1097–106. doi: 10.1016/s1473-3099(21)00057-8
4. Sandmann FG, Davies NG, Vassall A, Edmunds WJ, Jit M. The Potential Health and Economic Value of SARS-CoV-2 Vaccination Alongside Physical Distancing in the UK: A Transmission Model-Based Future Scenario Analysis and Economic Evaluation. Lancet Infect Dis (2021) 21(7):962–74. doi: 10.1016/s1473-3099(21)00079-7
5. Schaffer DeRoo S, Pudalov NJ, Fu LY. Planning for a COVID-19 Vaccination Program. JAMA (2020) 323(24):2458–59. doi: 10.1001/jama.2020.8711
6. Amanat F, Krammer F. SARS-CoV-2 Vaccines: Status Report. Immunity (2020) 52(4):583–89. doi: 10.1016/j.immuni.2020.03.007
7. MacDonald NE. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine (2015) 33(34):4161–4. doi: 10.1016/j.vaccine.2015.04.036
8. WHO. (2019). Available at: https://www.who.int/news-room/feature-stories/ten-threats-to-global-health-in-2019.
9. Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM, et al. Attitudes Toward a Potential SARS-CoV-2 Vaccine : A Survey of U.S. Adults. Ann Intern Med (2020) 173(12):964–73. doi: 10.7326/M20-3569
10. Gardner L, Dong E, Khan K, Sarkar S. Persistence of US Measles Risk Due to Vaccine Hesitancy and Outbreaks Abroad. Lancet Infect Dis (2020) 20(10):1114–15. doi: 10.1016/s1473-3099(20)30522-3
11. Solis Arce JS, Warren SS, Meriggi NF, Scacco A, McMurry N, Voors M, et al. COVID-19 Vaccine Acceptance and Hesitancy in Low- and Middle-Income Countries. Nat Med (2021) 27(8):1385–94. doi: 10.1038/s41591-021-01454-y
12. Sallam M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines (Basel) (2021) 9(2):160. doi: 10.3390/vaccines9020160
13. Freeman D, Loe BS, Yu L-M, Freeman J, Chadwick A, Vaccari C, et al. Effects of Different Types of Written Vaccination Information on COVID-19 Vaccine Hesitancy in the UK (OCEANS-III): A Single-Blind, Parallel-Group, Randomised Controlled Trial. Lancet Public Health (2021) 6(6):e416–27. doi: 10.1016/s2468-2667(21)00096-7
14. Wang K, Wong EL-Y, Ho K-F, Cheung AW, Yau PS, Dong D, et al. Change of Willingness to Accept COVID-19 Vaccine and Reasons of Vaccine Hesitancy of Working People at Different Waves of Local Epidemic in Hong Kong, China: Repeated Cross-Sectional Surveys. Vaccines (2021) 9(1):62. doi: 10.3390/vaccines9010062
15. Kumar D, Chandra R, Mathur M, Samdariya S, Kapoor N. Vaccine Hesitancy: Understanding Better to Address Better. Isr J Health Policy Res (2016) 5:2. doi: 10.1186/s13584-016-0062-y
16. Dube E, Ward JK, Verger P, MacDonald NE. Vaccine Hesitancy, Acceptance, and Anti-Vaccination: Trends and Future Prospects for Public Health. Annu Rev Public Health (2021) 42:175–91. doi: 10.1146/annurev-publhealth-090419-102240
17. Broadbent JJ. Vaccine hesitancy: Misinformation on Social Media. BMJ (2019) 3(366):14457. doi: 10.1136/bmj.l4457
18. Quinn SC, Andrasik M. Addressing Vaccine Hesitancy in BIPOC Communities - Toward Trustworthiness, Partnership, and Reciprocity. N Engl J Med (2021) 385(2):97–100. doi: 10.1056/NEJMp2103104
19. Simas C, Larson HJ. Overcoming Vaccine Hesitancy in Low-Income and Middle-Income Regions. Nat Rev Dis Primers (2021) 7(1):41. doi: 10.1038/s41572-021-00279-w
20. Razai MS, Chaudhry UAR, Doerholt K, Bauld L, Majeed A. Covid-19 Vaccination Hesitancy. BMJ (2021) 373:n1138. doi: 10.1136/bmj.n1138
21. Our World in Data (2021). Available at: https://ourworldindata.org/covid-vaccinations.
22. The National People’s Congress of the People’s Republic of China. Available at: http://www.npc.gov.cn/npc/c30834/201907/11447c85e05840b9b12c62b5b645fe9d.shtml.
23. WHO. (2021). Available at: https://extranet.who.int/pqweb/sites/default/files/documents/Status_COVID_VAX_20Jan2021_v2.pdf.
24. Su S, Du L, Jiang S. Learning From the Past: Development of Safe and Effective COVID-19 Vaccines. Nat Rev Microbiol (2021) 19(3):211–19. doi: 10.1038/s41579-020-00462-y
25. Phelan AL, Eccleston-Turner M, Rourke M, Maleche A, Wang C. Legal Agreements: Barriers and Enablers to Global Equitable COVID-19 Vaccine Access. Lancet (2020) 396(10254):800–02. doi: 10.1016/s0140-6736(20)31873-0
26. Ratzan S, Schneider E, Hatch H, Cacchione J. Missing the Point - How Primary Care Can Overcome Covid-19 Vaccine "Hesitancy". N Engl J Med (2021) 384(25):e100. doi: 10.1056/NEJMp2106137
27. Wouters OJ, Shadlen KC, Salcher-Konrad M, Pollard AJ, Larson HJ, Teerawattananon Y. Challenges in Ensuring Global Access to COVID-19 Vaccines: Production, Affordability, Allocation, and Deployment. Lancet (2021) 397(10278):1023–34. doi: 10.1016/s0140-6736(21)00306-8
28. Du F, Chantler T, Francis MR, Sun FY, Zhang X, Han K, et al. The Determinants of Vaccine Hesitancy in China: A Cross-Sectional Study Following the Changchun Changsheng Vaccine Incident. Vaccine (2020) 38(47):7464–71. doi: 10.1016/j.vaccine.2020.09.075
29. Hofer U. Make It Personal to Beat Vaccine Hesitancy. Nat Rev Microbiol (2021) 19(7):406. doi: 10.1038/s41579-021-00579-8
30. Tanne JH. Covid-19: US Doctors Suggest New Ways to Target Vaccine Hesitancy. BMJ (2021) 25(373):n1640. doi: 10.1136/bmj.n1640
Keywords: COVID-19 vaccine hesitancy, China, primary vaccination, booster vaccination, factors (individual factors, contextual factors)
Citation: Wu J, Li Q, Silver Tarimo C, Wang M, Gu J, Wei W, Ma M, Zhao L, Mu Z and Miao Y (2021) COVID-19 Vaccine Hesitancy Among Chinese Population: A Large-Scale National Study. Front. Immunol. 12:781161. doi: 10.3389/fimmu.2021.781161
Received: 22 September 2021; Accepted: 29 October 2021;
Published: 29 November 2021.
Edited by:
George Kenneth Lewis, University of Maryland, United StatesReviewed by:
Lucy Ochola, Institute of Primate Research, KenyaCopyright © 2021 Wu, Li, Silver Tarimo, Wang, Gu, Wei, Ma, Zhao, Mu and Miao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yudong Miao, bWVsZG9uQHp6dS5lZHUuY24=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.