- 1Department of Rheumatology and Immunology, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2Department of Rheumatology and Immunology, The Fourth Affiliated Hospital of Nantong University, The First People’s Hospital of Yancheng, Yancheng, China
The catastrophic outbreak of coronavirus disease 2019 (COVID-19) is currently a public emergency. Adult-onset Still’s disease (AOSD) is an autoinflammatory disease characterized by life-threatening complications. Systemic hyperinflammation and cytokine storm play a critical role in the pathogenesis of both COVID-19 and AOSD. We aimed to compare the similarities and differences focusing on ferritin and cytokine levels between severe COVID-19 and active AOSD. A literature search was performed using the databases PubMed, EMBASE, and Web of Science to collect the levels of cytokine including IL-1β, IL-6, IL-18, TNF-α, IL-10, and ferritin in severe COVID-19 patients. After extracting available data of indicators of interest, we acquired these statistics with a single-arm meta-analysis. Furthermore, a comparison was conducted between 52 patients with active AOSD in our center and severe COVID-19 patients from databases. The levels of IL-6 and IL-10 were higher in severe COVID-19 compared with those in active AOSD. There were no significant differences on the cytokine of IL-1β and TNF-α. Fold changes of IL-18 were defined as the mean expression level ratio of severe COVID-19 to healthy controls in the COVID-19 study and active AOSD to healthy controls in our study, individually. Although the fold change of IL-18 in patients with AOSD was significantly higher than patients with severe COVID-19 (fold change: 594.00 vs 2.17), there was no statistical comparability. In addition, the level of ferritin was higher in active AOSD in comparison with severe COVID-19. Our findings suggest that severe COVID-19 and active AOSD have differences in cytokine panel and ferritin level, indicating the pathogenic role of ferritin in overwhelming inflammation. And it paves the way to make efficacy therapeutic strategy targeting the hyperinflammatory process in COVID-19 according to AOSD management, especially in severe COVID-19.
Introduction
Coronavirus disease 2019 (COVID-19), a novel virus-induced acute respiratory disease syndrome, has placed much pressure on healthcare systems with its high mortality rate (1). Intriguingly, COVID-19 demonstrates a heterogeneous course, from asymptomatic manifestations to severe respiratory involvement, multiorgan dysfunction, and even death. Accordingly, patients with COVID-19 were divided into two groups: asymptomatic or mild subset and severe subset (2). The common symptoms of COVID-19 were fever, dry cough, myalgia, and dyspnea.
A hallmark of COVID-19 is an excessive release of pro-inflammatory cytokines including interleukin-6 (IL-6), interleukin-1α (IL-1α), interleukin-1β (IL-1β), tumor necrosis factor-α (TNF-α), granulocyte-macrophage colony-stimulating factor (GM-CSF), and monocyte chemoattractant protein 1 (MCP1), which is an overwhelming inflammatory process called a cytokine storm. Compared with non-intensive care unit (ICU) patients with COVID-19, increased levels of cytokines, such as interleukin-2 (IL-2), interleukin-7 (IL-7), interleukin-10 (IL-10), and TNF-α, were observed in ICU patients with COVID-19, suggesting the potential pathogenetic role of exuberant cytokine in COVID-19 (3). Meanwhile, increasing evidence suggests that severe COVID-19 patients at higher risk of poor outcome have higher ferritin levels in serum (1297.6 ng/ml in non-survivors vs 614.0 ng/ml in survivors) (4), leading to a hypothesis that ferritin may not only act as a bystander of acute phase response but also play a pivotal role in inflammation milieu in COVID-19. Ferritin, an inflammatory protein regulated by pro-inflammatory cytokines, may further enhance pro-inflammatory process in inflammatory setting of COVID-19, contributing to the development of cytokine storm in COVID-19 (5, 6). It has spurred comparisons with other severe diseases that are associated with increased cytokines and ferritin.
Adult-onset Still’s disease (AOSD), also known as a hyperferritinemic syndrome, is a multi-system involved autoinflammatory disease. Also triggered by viral infections, AOSD is characterized by high spiking fever, evanescent skin rash, sore throat, polyarthralgia, and even life-threatening complications, including fulminant hepatitis and macrophage activation syndrome (MAS) (7, 8). Similarly, excessive and uncontrolled production of cytokines, including IL-1β, IL-6, interleukin-18 (IL-18), and TNF-α, has been recognized as a cornerstone in AOSD pathogenesis (9). It is still matter of debate about the differences of cytokine panel in COVID-19 and AOSD, the two typical conditions of cytokine storm.
Furthermore, due to the similarity of clinical presentations and high levels of ferritin, AOSD, MAS, catastrophic antiphospholipid syndrome, and septic shock are included under the umbrella of hyperferritinemic syndrome (10). In fact, AOSD patients have a largely over-abundant level of ferritin. Due to hyperferritinemia in severe COVID-19, it is hypothesized that severe COVID-19 is a new member of hyperferritinemic syndrome (6, 10). Additionally, severe COIVD-19 and AOSD might share a common pathogenesis of cytokine storm. On the basis of shared features of cytokine storm and hyperferritinemia in AOSD and severe COVID-19, it would be extremely interesting to evaluate the similarities and differences to better understanding of the pathogenesis of cytokine storm. Consequently, we performed our study to compare the similarities and differences focusing on the ferritin and cytokine level between severe COVID-19 and AOSD.
Methods
Subjects and Cytokine Assessment
A total of 52 active AOSD patients were enrolled from Department of Rheumatology and Immunology, Ruijin Hospital, Shanghai Jiao Tong University. All patients with AOSD were diagnosed according to Yamaguchi’s criteria after exclusion of infectious, neoplastic, and autoimmune diseases (11). The systemic disease activity of each AOSD patient was assessed using a modified Pouchot’s score (12). Patients with active AOSD were defined by the presence of fever and/or skin rash and/or inflammatory arthralgia/arthritis and/or sore throat (13). Forty-two age- and sex-matched health volunteers were recruited as healthy controls. Serum levels of IL-1β, IL-6, IL-18, TNF-α, and IL-10 in AOSD patients were detected using the Meso Scale Discovery electrochemiluminescence assay (MSD, Rockville, MD, USA) as described previously (13). Ferritin level in serum was quantified using commercial ELISA reagent kit following the manufacturer’s instructions.
Search Strategy and Selection Criteria
We searched PubMed, EMBASE, and Web of Science databases to identify investigations reporting COVID-19 with cytokine levels using the following search terms: (“coronavirus” OR “COVID-19” OR “SARS-CoV-2” OR “novel coronavirus” OR “coronavirus disease 2019” OR “Wuhan virus” OR “China coronavirus” OR “SARS-coronavirus-2) AND (“cytokine” OR “interleukin”). The search process was restricted to English-language articles involving humans dated from December 2019 to July 18, 2020. The search strategy conformed to the Preferred Reporting items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Table S1). Full-text of research articles was eligible if they reported exact data of cytokine level in severe COVID-19. In our study, patients with COVID-19 receiving treatment in intensive care unit or non-survivor or SpO2<90% or required mechanical ventilation or complicated with ARDS were considered severe. In some cases, hospitalized patients were also regarded as severe, compared with ambulatory patients. Review articles, editorials, comments, case reports, letters, and researches on pediatrics, pregnancy, and obstetrics were excluded. Meanwhile, articles in the MedRxiv or unaccepted articles were also excluded. During the search process, a PICOs format was used (Table S2). Owing to the characteristics of single-arm meta analysis in our study, the comparison and outcome were not required during the PICOs process.
Risk of Bias Assessment
To critically assess the risk of bias for the included studies, the following criteria were applied in our study, which was similar to the assessment by Bao et al. (14). The criteria included a clear purpose of the study, including continuous patients, the definition of severe COVID-19, sufficient data of interest, the end-point adapted to the research goal, and a fair assessment of the end-point. The item not reported was scored 0, reported but insufficient was 1, reported and sufficient was 2. The global score of this scale was 14. Studies with a score ≥ 10 were considered high quality, and then were selected for further analysis; otherwise, they were excluded. Additionally, we drafted funnel-plots for indicators to assess publication bias if there were at least 10 included studies. When asymmetry of the funnel plots was present, the trim and fill methods were further applied to adjust publication bias.
Data Extraction and Analysis
Two independent reviewers (JM and YM) performed the literature search and assessed each article for inclusion and exclusion. Discrepancies were resolved by a third investigator (QH). The results of initial search were first screened by title and abstract. Then, the full-text of relevant articles was reviewed for inclusion and exclusion criteria. We extracted the following data from selected articles: author, publication date, journal, number of enrolled COVID-19 patients, country, study type, age, gender, ferritin, exact data of cytokine level. Data of cytokine and ferritin presented as median (interquartile, IQR) or median (Min-Max) were estimated to mean (standard deviation, SD) by Hozo group’s method (15). Additionally, we utilized I2 statistic to assess the heterogeneity of the included studies. When I2 > 75%, a random-effects model was used to minimize inter-study heterogeneity. The Stata version 16.0 was used to perform overall mean analysis. P-values less than 0.05 were considered statistically significant.
Results
Characteristics of Included Studies
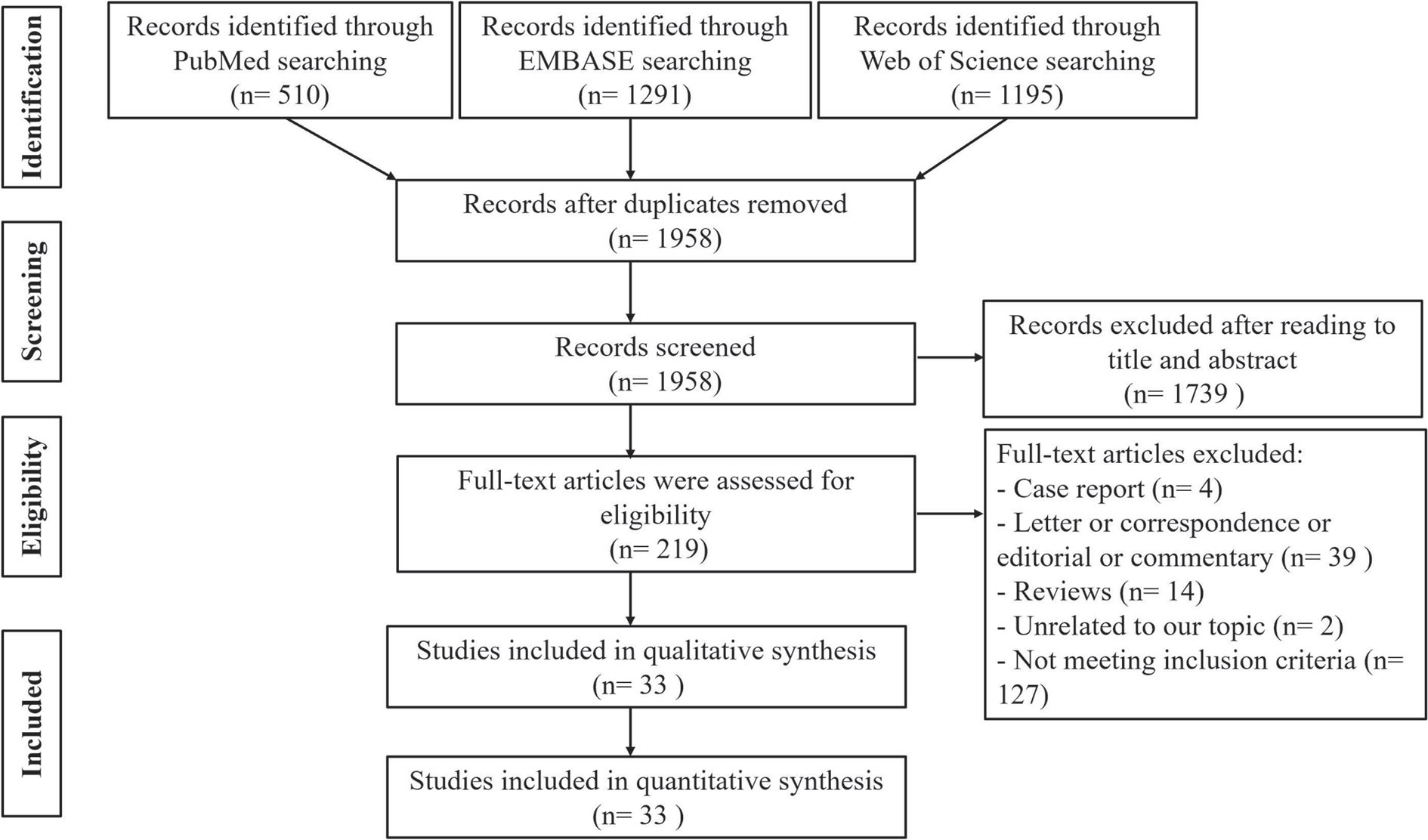
The steps of literature search are presented in Figure 1. A total of 2,996 publications were retrieved from PubMed, EMBASE, and Web of Science databases, 1,038 records of which were excluded due to duplication. After screening the remaining 1,958 publications according to title and abstraction, 219 full-text articles were further accessed for eligibility. Finally, we obtained the cytokine results of 33 articles describing 1,992 patients with COVID-19 (16–48).
Among these articles, 9 articles described the results of IL-1β, 31 articles demonstrated the results of IL-6, 16 studies presented the levels of IL-10, 17 reports showed the levels of TNF-α, and only one article depicted data of IL-18. Meanwhile, we obtained data of ferritin from 12 articles among 33 selected articles. The characteristics, cytokine profiles, and ferritin level of 33 included studies were summarized in Table 1.
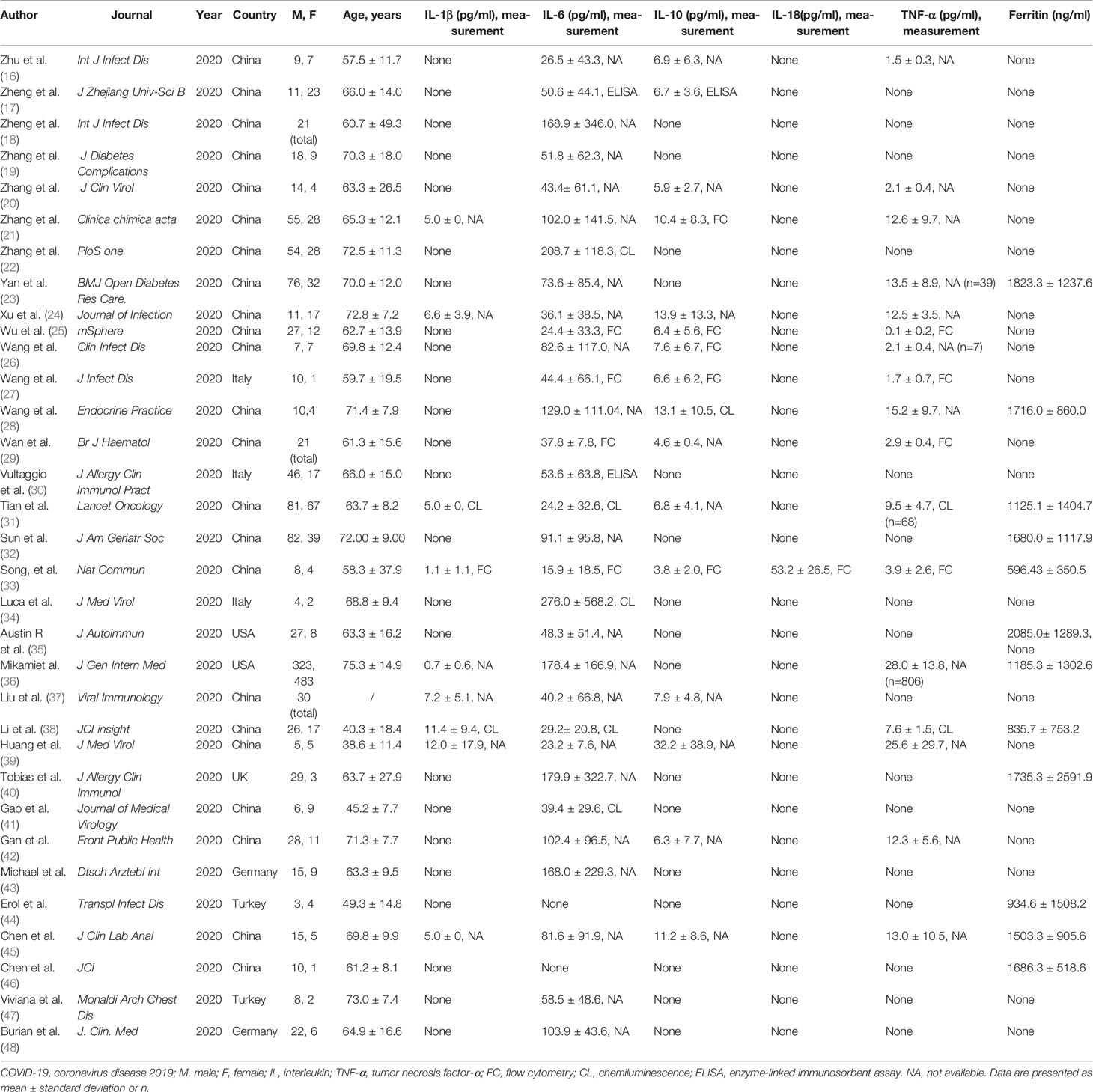
Table 1 Summary characteristics of 33 studies that demonstrated the cytokine level in patients with COVID-19.
The Differences of Clinical Manifestations and Laboratory Parameters Between COVID-19 and Active AOSD
The clinical characteristics of COVID-19 came from China, including 1,099 patients (1). Patients with active AOSD were younger than COVID-19 (38.8 ± 15.2 vs 46.7 ± 17.1 years, P = 0.0011), with high female predominance. Fever was the common manifestation in COVID-19 and active AOSD (88.7% vs 90.4%, P = 0.7095), whereas AOSD patients were characterized by sore throat (46.2% vs 13.9%, P < 0.0001), skin rash (76.9% vs 0.2%, P < 0.0001), arthralgia or myalgia (71.2% vs 14.9%, P < 0.0001), and hepatosplenomegaly or lymphadenopathy (73% vs 0.2%, P < 0.0001). The number of lung involvement assessed by chest CT was increased in patients with COVID-19 when comparing with AOSD (86.2% vs 17.3%, P < 0.0001). The occurrence of digestive symptoms, acute respiratory distress syndrome, coagulopathy, acute kidney injury, and death was higher in COVID-19, while no statistical difference was found between COVID-19 and AOSD. Regarding laboratory parameters, white blood cell (12.2 ± 6.2 vs 4.7 ± 1.9 109/L, P < 0.0001), platelets (256.5 ± 92.6 vs 169.0 ± 55.7 109/L, P < 0.0001), and lymphocyte (1.3 ± 0.75 109/L vs 1.0 ± 0.4 109/L, P < 0.0001) in AOSD were higher than those in COVID-19. Furthermore, the proportions of abnormal liver function tests (51.9% vs 22.2%, P < 0.0001) and elevated C-reactive protein level (90.2% vs 60.7%, P < 0.0001) were significantly higher in AOSD patients than in patients with COVID-19. The detailed comparison of clinical manifestations and laboratory parameters between COVID-19 and active AOSD is presented in Table 2.
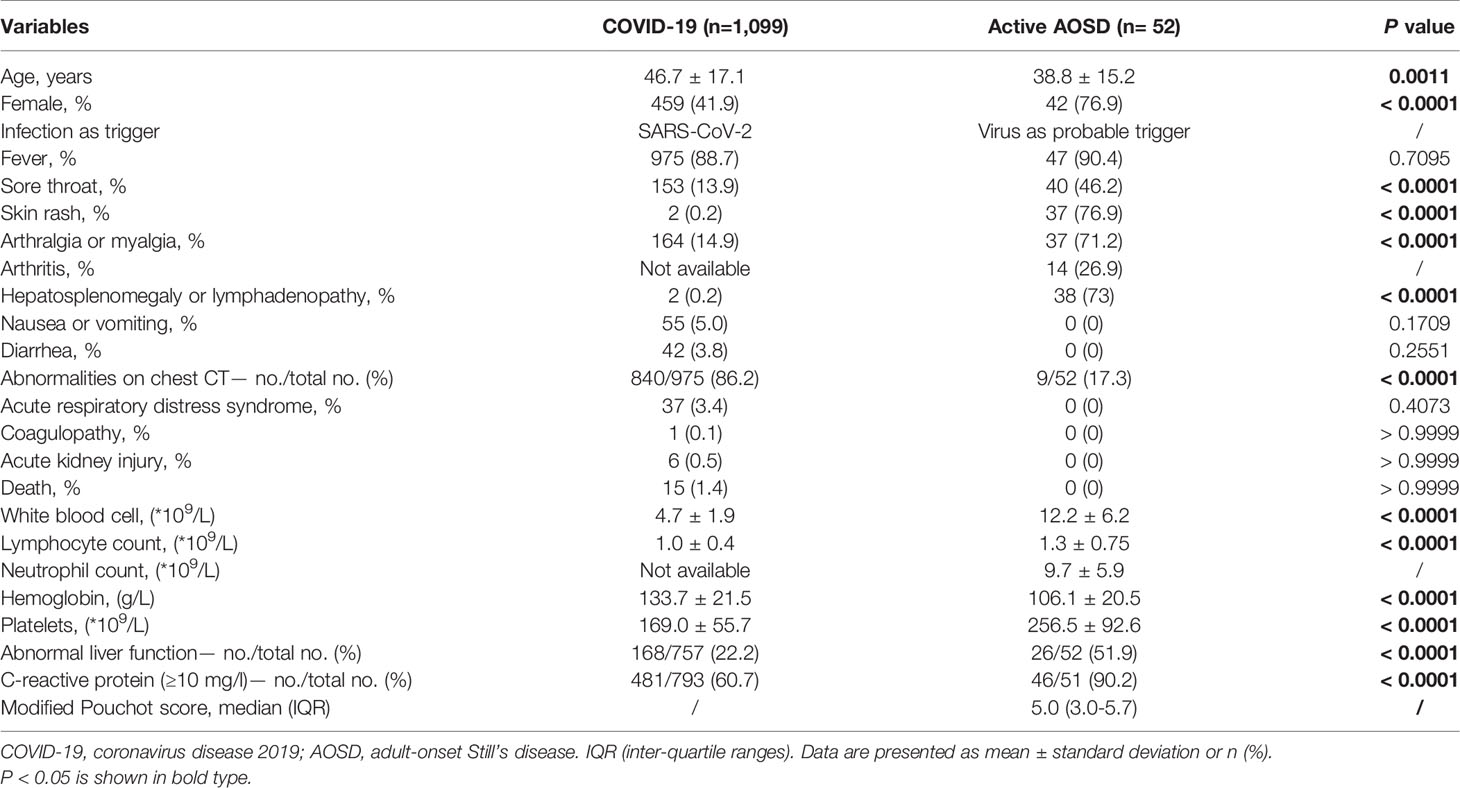
Table 2 Comparison of clinical manifestations and laboratory parameters between COVID-19 and active AOSD.
Comparison of the Cytokine Profile and Ferritin Between Severe COVID-19 and Active AOSD
The comprehensive collation of the expression of cytokine profile and ferritin data is shown in Table 3. Compared with active AOSD, patients with severe COVID-19 with higher male predominance were older than active AOSD, which was parallel to the results of Table 2. The levels of IL-6 and IL-10 were higher in severe COVID-19 compared with that in active AOSD. The levels of IL-1β tended to be elevated in severe COVID-19, while there was no significant difference between severe COVID-19 and active AOSD. Also, the level of TNF-α was comparable between these two diseases. Only one investigation reported the exact raw data on IL-18 with healthy control and patients with COVID-19. Fold changes of IL-18 were defined as the mean expression level ratio of severe COVID-19 and AOSD to healthy controls. Noteworthy, the fold change of IL-18 in patients with active AOSD was approximately 594, which was much higher than that in severe COVID-19 (Fold change 2.17), without statistical comparability. In addition, the level of ferritin was significantly higher in active AOSD in comparison with severe COVID-19 (1905.0 ± 1509.00 vs 1399.0 ± 1294.5ng/ml, P=0.0413). In addition, the forest plots of age, IL-1β, IL-6, IL-10, TNF-α, and ferritin were presented in Figure S1-6.
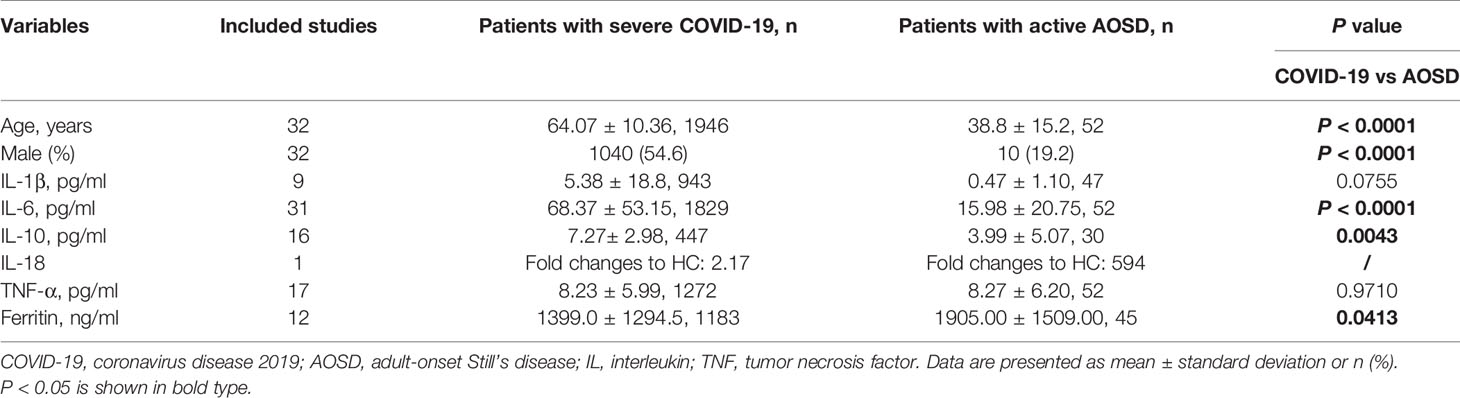
Table 3 Comparative results of cytokine and ferritin level between severe COVID-19 and active AOSD using meta-analysis.
Quality Assessment
Judging the assessment criteria, all 33 included studies were classified as high quality (Table S3). As shown in Figure S7, distribution of the funnel plot was symmetric in ferritin, indicating no evidence of publication bias. However, it was asymmetric in the funnel plots of age, IL-6, IL-10, TNF-α (Figure S8). Next, the trim and fill methods were applied to adjust publication bias. After adjustment, the distribution of the funnel plots in age (Figure S8) was more symmetric than before, indicating the results of age were relatively stable. However, the asymmetry of funnel plots of IL-6, IL-10, TNF-α still exited (Figure S8), which suggested the probable presence of the publication bias.
Discussion
COVID-19, caused by a new strain of β-coronavirus, SARS-CoV-2, is emerging as a huge threat to human health (49). SARS-CoV-2 infection invokes a hyperinflammatory state driven by multiple immune cells and mediators including IL-6, IL-1α, IL-1β, and TNF-α. Broadly speaking, cytokine storm denotes a hyperactive inflammatory response characterized by systemic inflammation, multi-organ dysfunction, elevated IL-1β, IL-18, IL-6, interferon-γ (IFN-γ), TNF-α, ferritin and other mediators, which are injurious to host cells. The imitating factors leading to cytokine storm are heterogeneous, including infections, tumor, and rheumatologic origins (50). Elevated plasma concentration of inflammatory mediators was observed in patients with COVID-19, including IL-6, IL-10, TNF-α, and other inflammatory cytokines, as well as ferritin and C-reactive protein (3, 46). Cytokine storms play a critical role in the pathogenesis of AOSD, an inflammatory disease with high serum ferritin and neutrophil activation. Severe COVID-19 patients at higher risk of poor outcome also have raised levels of ferritin. Accumulating evidences have strongly indicated the pathogenetic role of ferritin in systemic hyperinflammation, more than a bystander. For these reasons, we further investigated the similarities and differences focusing on the cytokine panel and ferritin.
In our study, cytokines including IL-1β, IL-6, IL-10, and TNF-α were elevated in severe COVID-19 and active AOSD, compared with healthy controls, indicating the potential contribution of cytokine storm in pathogenesis of COVID-19 and AOSD. As a whole, the levels of IL-6 and IL-10 were significantly higher in severe COVID-19 from our results, suggesting a more serious cytokine storm underlying the pathogenesis of COVID-19. Consistent with the aforementioned results, the mortality of overall patients with COVID-19 was higher than active AOSD despite no statistical significance. The reported mortality of severe COVID-19 over 10% further indicated the contribution of cytokine storm to severe COVID (51). Previous reports showed that COVID-19 patients with worse prognosis had higher levels of IL-6 (3, 26, 52). Furthermore, targeting IL-6 signaling, i.e., tocilizumab, an IL-6 receptor antagonist, showed promising and encouraging results in the treatment of COVID-19 (53). Similarly, tocilizumab was effective on systemic manifestations of AOSD in a double-blinded randomized clinical trial (54). Based on the results from this trial, tocilizumab is approved for the treatment of AOSD. In a word, IL-6 is increased in COVID-19 and AOSD and the therapy targeting it is effective, indicating a potential and potent role in the pathogenesis of cytokine storm. IL-10, an anti-inflammatory cytokine, which was increased in severe COVID-19 patients (55), was correlated with disease activity of AOSD (56). The compensatory role of anti-inflammatory cytokine might be a shared phenomenon in the pathogenesis of inflammatory disease characterized by a cytokine storm. Although IL-18 was elevated in COVID-19 (33), the levels of IL-18 in AOSD of our study were significantly higher than in severe COVID-19 patients, indicating the potential distinguishing feature of cytokine profiles between COVID-19 and AOSD. Nearly two decades ago, IL-18 was first identified as a diagnostic marker and was an indicator of disease activity in AOSD (57). Blocking IL-18 with recombinant human IL-18 BP (tadekinig alfa) appears to have treatment efficacy in AOSD (58). As we know, IL-18 is derived from the inflammasome activation, which might be a contributor of the pathogenesis of AOSD (59). Due to lack of researches on inflammasome and COVID-19 currently, we speculate that inflammasome activation might play a minimal role in COVID-19 pathogenesis. IFN-γ, an important cytokine of cytokine storm, were not assessed in our study as serum samples of some AOSD patients in our study are not available. In COVID-19, enhanced levels of IFN-γ was correlated with the viral load and was considered a marker of poor outcome (3, 60). Similarly, serum level of IFN-γ and IFN-γ expression in natural killer cell were enhanced in acute AOSD and reduced in remission AOSD (12, 61). IFN-γ was released by hematopoietic cells during viral infection, where IFN-γ might boost the amplification of inflammation (62). Consequently, enhanced expression of IFN-γ was found in SARS-CoV-2 infection and AOSD triggered probably by virus. However, whether the levels of IFN-γ are comparable need further investigation. With regards to ferritin, several investigations have confirmed that ferritin was elevated in patients with COVID-19 and was correlated with disease severity (63, 64). Due to the similarities in clinical manifestations and high level of ferritin in serum, severe COVID-19 was regarded as a fifth member of hyperferritinemic syndromes (65). Ferritin, the common denominator of COVID-19 and AOSD, comprises 24 subunits of two types, heavy and light subunits. Beyond its iron storage role, ferritin functions in a pathogenic role in inflammation. Under inflammatory conditions, such as COVID-19 and AOSD, ferritin is upregulated in response to IL-1β, IL-6, and IFN-γ. Furthermore, ferritin further stimulates inflammatory pathways to amply the inflammatory process (5, 66–68). Interestingly, the expression of ferritin was dramatically increased in AOSD when comparing with COVID-19, which was consistent with the analysis from Colafrancesco et al. (65). In vitro experiments showed that ferritin might be secreted by hepatocytes and macrophages (69). A previous study demonstrated that ferritin levels are correlated with disease activity and macrophage activation in AOSD (70). Accordingly, we hypothesize that the contribution of macrophage activation is more crucial to AOSD compared with COVID-19, resulting in the higher levels of ferritin in AOSD.
Besides denominators of hyperferritinemia and cytokine storm in COVID-19 and AOSD, there are also shared clinical manifestations. Fever, as a result of cytokine storm, is not surprisingly the most prominent common feature of COVID-19 and AOSD. Meanwhile, sore throat, arthralgia, or arthritis are relatively common in these two diseases. From our comparative results, digestive symptoms, such as nausea or vomiting, and diarrhea are comparable. AOSD, unlike COVID-19, is frequently triggered by viral infections with uncertain origins, while SARS-CoV-2 is the leading cause of COVID-19. The cardinal target organ of COVID-19 is lung, causing an acute respiratory distress syndrome. Recently, Ruscitti et al. conducted a study to compare the difference of clinical manifestation, laboratory tests, and radiological imaging in patients with lung involvement between severe COVID-19 and MAS secondary to AOSD (71). More patients in the COVID-19 group presented with ground-glass opacities (GGOs) compared with those in the group of MAS secondary to AOSD. And higher proportions of apical, basal, bilateral, and peripheral distributions of GGOs were observed in COVID-19 patients than in MAS. Consistent with this feature, SARS-CoV-2 is transmitted by droplets that come into the respiratory system, which widely express the angiotensin-converting enzyme-related carboxypeptidase as receptors of SARS-CoV-2. This may be the underlying reason why more COVID-19 patients suffered from lung involvement. The clinical manifestations, including arthralgia or arthritis, skin rashes, hepatomegaly, splenomegaly as distinctive clinical manifestations of AOSD haven’t been reported in COVID-19 so far. Furthermore, increased count of leukocyte and neutrophil is remarkable in AOSD, which is opposite to COVID-19 in which leukopenia are common. Besides these features mentioned above, diffused intravascular coagulopathy (DIC) is a rare but serious complication in patients with COVID-19 and AOSD. Regarding treatment, glucocorticoids, which are not recommended in COVID-19 unless severe patients, have been considered as the first-line therapy of AOSD patients.
Our study has several limitations. First, relatively few studies with exact data of IL-1β and IL-18 were included in this analysis, resulting in the difficulty of interpretation of the results. And the I2 statistics of our meta-analysis were high, indicating large heterogeneity, probably secondary to the difference of measurement in our selected studies. Therefore, the conclusion of our study needs to be verified by unified measurement of cytokines in more COVID-19 patients and healthy controls. Second, in the majority of patients with COVID-19 in our meta-analysis, the article described clinical manifestation and our AOSD cohort came from China, suggesting an underlying ethnic bias. Additional data from all over the world would provide a more comprehensive picture to better understand the similarities and differences between COVID-19 and AOSD. Whether the conclusion in our study is consistent with other studies consisting of more ethnicities remains to be investigated. Third, IL-18 binding protein (IL-18BP), a naturally IL-18 inhibitor in the circulation, can distinguish free bioactive IL-18 from total IL-18. The level of IL-18BP is not usually detected in COVID-19, thus a comparison of IL-18 binding protein (IL-18BP) level is not performed in our study (72). Last, potential publication bias and availability of data are mainly common limitations of all meta-analyses, leading us to explain the results cautiously.
Conclusions
In conclusion, our findings suggest that both COVID-19 and AOSD have elevated level of ferritin and cytokines, including IL-1β, IL-6, IL-10, IL-18, and TNF-α, indicating systemic inflammation in the pathogenesis of COVID-19 and AOSD. Importantly, all triggered by virus, COVID-19 and AOSD have differences in cytokine panel and ferritin level, indicating the diverse pathogenic role of cytokines and ferritin in overwhelming inflammation. And it paves the way to make efficacy therapeutic strategy targeting the hyperinflammatory process in COVID-19 according to AOSD management, especially severe COVID-19.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Ethics Statement
Information on demographic and clinical data were obtained under a protocol approved by the Institutional Research Ethics Committee of Ruijin Hospital (ID: 2016-62), Shanghai, China. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
Study conception or design: QH, CY, JM. Acquisition of the data: JM, YM, JJ, MW, JT, HS, HL, YTS, JY, YS, XBC, HC, TL, DZ, ZZ, LW, ZW, FW, XQ, XC, HZ, and ZT. Analysis and interpretation of the data: JM, YM, JJ, MW, and QH. Drafting and revising the article: QH, CY, and JM. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (82001704), Shanghai Sailing Program (20YF1427100), Shanghai Pujiang Young Rheumatologists Training program (SPROG201901), and Shanghai Science and Technology Innovation Action (20Y11911500).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2020.603389/full#supplementary-material
Abbreviations
COVID-19, Coronavirus disease 2019; IL-6, interleukin-6; IL-1α, interleukin-1α; IL-1β, interleukin-1β; TNFα, tumor necrosis factor-α; GM-CSF, granulocyte-macrophage colony-stimulating factor; MCP1, monocyte chemoattractant protein 1; ICU, non-intensive care unit, IL-2, interleukin-2; IL-7, interleukin-7; IL-10, interleukin-10; IL-18, interleukin-18; AOSD, Adultonset Still’s disease; MAS, macrophage activation syndrome; PRISMA, Preferred Reporting items for Systematic Reviews and Meta-Analyses statement; IQR, interquartile; SD, standard deviation; IFN-γ, interferon-γ; GGOs, ground-glass opacities, DIC, diffused intravascular coagulopathy.
References
1. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med (2020) 382:1708–20. doi: 10.1056/NEJMoa2002032
2. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA (2020) 323:1061–9. doi: 10.1001/jama.2020.1585
3. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (2020) 395:497–506. doi: 10.1016/s0140-6736(20)30183-5
4. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Medicine (2020) 46:846–8. doi: 10.1007/s00134-020-05991-x
5. Ruscitti P, Berardicurti O, Barile A, Cipriani P, Shoenfeld Y, Iagnocco A, et al. Severe COVID-19 and related hyperferritinaemia: more than an innocent bystander? Ann Rheum Dis (2020) 79:1515–6. doi: 10.1136/annrheumdis-2020-217618
6. Ruscitti P, Berardicurti O, Di Benedetto P, Cipriani P, Iagnocco A, Shoenfeld Y, et al. Severe COVID-19, Another Piece in the Puzzle of the Hyperferritinemic Syndrome. An Immunomodulatory Perspective to Alleviate the Storm. Front Immunol (2020) 11:1130. doi: 10.3389/fimmu.2020.01130
7. Hu QY, Zeng T, Sun CY, Luo CN, Liu S, Ding TT, et al. Clinical features and current treatments of adult-onset Still’s disease: a multicentre survey of 517 patients in China. Clin Exp Rheumatol (2019) 37(Suppl. 121):S52–7.
8. Li Z, Liu HL, Chen J, Zeng T, He L, Li M, et al. Both HLA class I and II regions identified as genome-wide significant susceptibility loci for adult-onset Still’s disease in Chinese individuals. Ann Rheum Dis (2019) 79(1):161–3. doi: 10.1136/annrheumdis-2019-215239
9. Hu Q, Shi H, Zeng T, Liu H, Su Y, Cheng X, et al. Increased neutrophil extracellular traps activate NLRP3 and inflammatory macrophages in adult-onset Still’s disease. Arthritis Res Ther (2019) 21:9. doi: 10.1186/s13075-018-1800-z
10. Rosario C, Zandman-Goddard G, Meyron-Holtz EG, D’Cruz DP, Shoenfeld Y. The hyperferritinemic syndrome: macrophage activation syndrome, Still’s disease, septic shock and catastrophic antiphospholipid syndrome. BMC Med (2013) 11:185. doi: 10.1186/1741-7015-11-185
11. Feist E, Mitrovic S, Fautrel B. Mechanisms, biomarkers and targets for adult-onset Still’s disease. Nat Rev Rheumatol (2018) 14:603–18. doi: 10.1038/s41584-018-0081-x
12. Rau M, Schiller M, Krienke S, Heyder P, Lorenz H, Blank N. Clinical manifestations but not cytokine profiles differentiate adult-onset Still’s disease and sepsis. J Rheumatol (2010) 37:2369–76. doi: 10.3899/jrheum.100247
13. Chi H, Liu D, Sun Y, Hu Q, Liu H, Cheng X, et al. Interleukin-37 is increased in adult-onset Still’s disease and associated with disease activity. Arthritis Res Ther (2018) 20:54. doi: 10.1186/s13075-018-1555-6
14. Bao J, Li C, Zhang K, Kang H, Chen W, Gu B. Comparative analysis of laboratory indexes of severe and non-severe patients infected with COVID-19. Clinica Chimica Acta (2020) 509:180–94. doi: 10.1016/j.cca.2020.06.009
15. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol (2005) 5:13. doi: 10.1186/1471-2288-5-13
16. Zhu Z, Cai T, Fan L, Lou K, Hua X, Huang Z, et al. Clinical value of immune-inflammatory parameters to assess the severity of coronavirus disease 2019. Int J Infect Diseases (2020) 95:332–9. doi: 10.1016/j.ijid.2020.04.041
17. Zheng Y, Sun L-J, Xu M, Pan J, Zhang Y-T, Fang X-L, et al. Clinical characteristics of 34 COVID-19 patients admitted to intensive care unit in Hangzhou. China J Zhejiang Univ Sci B (2020) 21:378–87. doi: 10.1631/jzus.B2000174
18. Zheng C, Wang J, Guo H, Lu Z, Ma Y, Zhu Y, et al. Risk-adapted Treatment Strategy For COVID-19 Patients. Int J Infect Diseases (2020) 94:74–7. doi: 10.1016/j.ijid.2020.03.047
19. Zhang Q, Wei Y, Chen M, Wan Q, Chen X. Clinical analysis of risk factors for severe COVID-19 patients with type 2 diabetes. J Diabetes its Complications (2020), 107666–6. doi: 10.1016/j.jdiacomp.2020.107666
20. Zhang J, Yu M, Tong S, Liu L-Y, Tang L-V. Predictive factors for disease progression in hospitalized patients with coronavirus disease 2019 in Wuhan, China. J Clin Virol (2020) 127:104392. doi: 10.1016/j.jcv.2020.104392
21. Zhang D, Zhou X, Yan S, Tian R, Su L, Ding X, et al. Correlation between cytokines and coagulation-related parameters in patients with coronavirus disease 2019 admitted to ICU. Clinica Chimica Acta; Int J Clin Chem (2020) 510:47–53. doi: 10.1016/j.cca.2020.07.002
22. Zhang B, Zhou X, Qiu Y, Song Y, Feng F, Feng J, et al. Clinical characteristics of 82 cases of death from COVID-19. PLoS One (2020) 15:e0235458–e0235458. doi: 10.1371/journal.pone.0235458
23. Yan Y, Yang Y, Wang F, Ren H, Zhang S, Shi X, et al. Clinical characteristics and outcomes of patients with severe covid-19 with diabetes. BMJ Open Diabetes Res Care (2020) 8(1):e001343. doi: 10.1136/bmjdrc-2020-001343
24. Xu B, Fan C-Y, Wang A-L, Zou Y-L, Yu Y-H, He C, et al. Suppressed T cell-mediated immunity in patients with COVID-19: A clinical retrospective study in Wuhan. China J Infect (2020) 81:E51–60. doi: 10.1016/j.jinf.2020.04.012
25. Wu Y, Huang X, Sun J, Xie T, Lei Y, Muhammad J, et al. Clinical Characteristics and Immune Injury Mechanisms in 71 Patients with COVID-19. mSphere (2020) 5(4):e00362-20. doi: 10.1128/mSphere.00362-20
26. Wang Z, Yang B, Li Q, Wen L, Zhang R. Clinical Features of 69 Cases With Coronavirus Disease 2019 in Wuhan, China. Clin Infect Dis (2020) 71:769–77. doi: 10.1093/cid/ciaa272
27. Wang W, Liu X, Wu S, Chen S, Li Y, Nong L, et al. The Definition and Risks of Cytokine Release Syndrome in 11 COVID-19-Affected Critically Ill Patients with Pneumonia: Analysis of Disease Characteristics. J Infect Dis (2020) 222(9):1444–51. doi: 10.1093/infdis/jiaa387
28. Wang F, Yang Y, Dong K, Yan Y, Zhang S, Ren H, et al. Clinical Characteristics of 28 Patients with Diabetes and Covid-19 In Wuhan, China. Endocr Pract (2020) 26:668–74. doi: 10.4158/ep-2020-0108
29. Wan S, Yi Q, Fan S, Lv J, Zhang X, Guo L, et al. Relationships among lymphocyte subsets, cytokines, and the pulmonary inflammation index in coronavirus (COVID-19) infected patients. Br J Haematol (2020) 189:428–37. doi: 10.1111/bjh.16659
30. Vultaggio A, Vivarelli E, Virgili G, Lucenteforte E, Bartoloni A, Nozzoli C, et al. Prompt Predicting of Early Clinical Deterioration of Moderate-to-Severe COVID-19 Patients: Usefulness of a Combined Score Using IL-6 in a Preliminary Study. J Allergy Clin Immunol: In Pract (2020) 8(8):2575–81. doi: 10.1016/j.jaip.2020.06.013
31. Tian J, Yuan X, Xiao J, Zhong Q, Yang C, Liu B, et al. Clinical characteristics and risk factors associated with COVID-19 disease severity in patients with cancer in Wuhan, China: a multicentre, retrospective, cohort study. Lancet Oncol (2020) 21:893–903. doi: 10.1016/s1470-2045(20)30309-0
32. Sun H, Ning R, Tao Y, Yu C, Deng X, Zhao C, et al. Risk Factors for Mortality in 244 Older Adults With COVID-19 in Wuhan, China: A Retrospective Study. J Am Geriatr Society (2020) 68:E19–23. doi: 10.1111/jgs.16533
33. Song JW, Zhang C, Fan X, Meng FP, Xu Z, Xia P, et al. Immunological and inflammatory profiles in mild and severe cases of COVID-19. Nat Commun (2020) 11:3410. doi: 10.1038/s41467-020-17240-2
34. Quartuccio L, Sonaglia A, Pecori D, Peghin M, Fabris M, Tascini C, et al. Higher levels of IL-6 early after tocilizumab distinguish survivors from non-survivors in COVID-19 pneumonia: a possible indication for deeper targeting IL-6. J Med Virol (2020) 92(11):2852–6. doi: 10.1002/jmv.26149
35. Morrison AR, Johnson JM, Griebe KM, Jones MC, Stine JJ, Hencken LN, et al. Clinical characteristics and predictors of survival in adults with coronavirus disease 2019 receiving tocilizumab. J Autoimmun (2020) 102512–2. doi: 10.1016/j.jaut.2020.102512
36. Mikami T, Miyashita H, Yamada T, Harrington M, Steinberg D, Dunn A, et al. Risk Factors for Mortality in Patients with COVID-19 in New York City. J Gen Internal Medicine (2020) 30:1–10. doi: 10.1007/s11606-020-05983-z
37. Liu Y, Liao W, Wan L, Xiang T, Zhang W. Correlation Between Relative Nasopharyngeal Virus RNA Load and Lymphocyte Count Disease Severity in Patients with COVID-19. Viral Immunol (2020) 37(Suppl. 121):S52–7. doi: 10.1089/vim.2020.0062
38. Li S, Jiang L, Li X, Lin F, Wang Y, Li B, et al. Clinical and pathological investigation of patients with severe COVID-19. JCI Insight (2020) 5(12):e138070. doi: 10.1172/jci.insight.138070
39. Huang H, Zhang M, Chen C, Zhang H, Wei Y, Tian J, et al. Clinical Characteristics of COVID-19 in patients with pre-existing ILD: A retrospective study in a single center in Wuhan, China. J Med Virol (2020) 92(11):2742–50. doi: 10.1002/jmv.26174
40. Herold T, Jurinovic V, Arnreich C, Lipworth BJ, Hellmuth JC, Bergwelt-Baildon MV, et al. Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19. J Allergy Clin Immunol (2020) 146:128–36.e124. doi: 10.1016/j.jaci.2020.05.008
41. Gao Y, Li T, Han M, Li X, Wu D, Xu Y, et al. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J Med Virol (2020) 92:791–6. doi: 10.1002/jmv.25770
42. Gan J, Li J, Li S, Yang C. Leucocyte Subsets Effectively Predict the Clinical Outcome of Patients With COVID-19 Pneumonia: A Retrospective Case-Control Study. Front Public Health (2020) 8:299. doi: 10.3389/fpubh.2020.00299
43. Dreher M, Kersten A, Bickenbach J, Balfanz P, Hartmann B, Cornelissen C, et al. The Characteristics of 50 Hospitalized COVID-19 Patients With and Without ARDS. Deutsches Arzteblatt Int (2020) 117:271–+. doi: 10.3238/arztebl.2020.0271
44. Demir E, Uyar M, Parmaksiz E, Sinangil A, Yelken B, Dirim AB, et al. COVID-19 in kidney transplant recipients: A multicenter experience in Istanbul. Transplant Infect Disease (2020), e13371–1. doi: 10.1111/tid.13371
45. Chen X, Yan L, Fei Y, Zhang C. Laboratory abnormalities and risk factors associated with in-hospital death in patients with severe COVID-19. J Clin Lab Anal (2020), e23467–7. doi: 10.1002/jcla.23467
46. Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest (2020) 130:2620–9. doi: 10.1172/jci137244
47. Carlino MV, Valenti N, Cesaro F, Costanzo A, Cristiano G, Guarino M, et al. Predictors of Intensive Care Unit admission in patients with coronavirus disease 2019 (COVID-19). Monaldi Arch chest Dis = Archivio Monaldi per le malattie del torace (2020) 90:430–6. doi: 10.4081/monaldi.2020.1410
48. Burian E, Jungmann F, Kaissis GA, Lohoefer FK, Spinner CD, Lahmer T, et al. Intensive Care Risk Estimation in COVID-19 Pneumonia Based on Clinical and Imaging Parameters: Experiences from the Munich Cohort. J Clin Med (2020) 9(5):1514. doi: 10.3390/jcm9051514
49. Moore JB, June CH. Cytokine release syndrome in severe COVID-19. Science (2020) 368:473–4. doi: 10.1126/science.abb8925
50. Behrens EM, Koretzky GA. Review: Cytokine Storm Syndrome: Looking Toward the Precision Medicine Era. Arthritis Rheumatol (2017) 69:1135–43. doi: 10.1002/art.40071
51. Simonovich VA, Burgos Pratx LD, Scibona P, Beruto MV, Vallone MG, Vazquez C, et al. A Randomized Trial of Convalescent Plasma in Covid-19 Severe Pneumonia. N Engl J Med (2020). doi: 10.1056/NEJMoa2031304
52. Fernandez-Ruiz M, Lopez-Medrano F, Asin M A P-J, de la Calle GM, Bueno H, Caro-Teller JM, et al. Tocilizumab for the treatment of adult patients with severe COVID-19 pneumonia: a single-center cohort study. J Med Virol (2020). doi: 10.1002/jmv.26308
53. Toniati P, Piva S, Cattalini M, Garrafa E, Regola F, Castelli F, et al. Tocilizumab for the treatment of severe COVID-19 pneumonia with hyperinflammatory syndrome and acute respiratory failure: A single center study of 100 patients in Brescia, Italy. Autoimmun Rev (2020) 19:102568. doi: 10.1016/j.autrev.2020.102568
54. Kaneko Y, Kameda H, Ikeda K, Ishii T, Murakami K, Takamatsu H, et al. Tocilizumab in patients with adult-onset still’s disease refractory to glucocorticoid treatment: a randomised, double-blind, placebo-controlled phase III trial. Ann Rheum Dis (2018) 77:1720–9. doi: 10.1136/annrheumdis-2018-213920
55. Zhao Y, Qin L, Zhang P, Li K, Liang L, Sun J, et al. Longitudinal COVID-19 profiling associates IL-1RA and IL-10 with disease severity and RANTES with mild disease. JCI Insight (2020) 5(13):e139834. doi: 10.1172/jci.insight.139834
56. Sun Y, Wang Z, Chi H, Hu Q, Ye J, Liu H, et al. Elevated serum levels of interleukin-10 in adult-onset Still’s disease are associated with disease activity. Clin Rheumatol (2019) 38:3205–10. doi: 10.1007/s10067-019-04642-x
57. Kawaguchi Y, Terajima H, Harigai M, Hara M, Kamatani N. Interleukin-18 as a novel diagnostic marker and indicator of disease severity in adult-onset Still’s disease. Arthritis Rheumatol (2001) 44:1716–7. doi: 10.1002/1529-0131(200107)44:7<1716::AID-ART298>3.0.CO;2-I
58. Gabay C, Fautrel B, Rech J, Spertini F, Feist E, Kotter I, et al. Open-label, multicentre, dose-escalating phase II clinical trial on the safety and efficacy of tadekinig alfa (IL-18BP) in adult-onset Still’s disease. Ann Rheum Dis (2018) 77:840–7. doi: 10.1136/annrheumdis-2017-212608
59. Hsieh CW, Chen YM, Lin CC, Tang KT, Chen HH, Hung WT, et al. Elevated Expression of the NLRP3 Inflammasome and Its Correlation with Disease Activity in Adult-onset Still Disease. J Rheumatol (2017) 44:1142–50. doi: 10.3899/jrheum.161354
60. Pedersen SF, Ho YC. SARS-CoV-2: a storm is raging. J Clin Invest (2020) 130:2202–5. doi: 10.1172/JCI137647
61. Shimojima Y, Kishida D, Ueno K II, Ushiyama S, Ichikawa T, Sekijima Y. Characteristics of Circulating Natural Killer Cells and Their Interferon-gamma Production in Active Adult-onset Still Disease. J Rheumatol (2019) 46:1268–76. doi: 10.3899/jrheum.181192
62. Canna SW, Behrens EM. Making sense of the cytokine storm: a conceptual framework for understanding, diagnosing, and treating hemophagocytic syndromes. Pediatr Clin North Am (2012) 59:329–44. doi: 10.1016/j.pcl.2012.03.002
63. Sun Y, Dong Y, Wang L, Xie H, Li B, Chang C, et al. Characteristics and prognostic factors of disease severity in patients with COVID-19: The Beijing experience. J Autoimmun (2020) 102473–3. doi: 10.1016/j.jaut.2020.102473
64. Liao D, Zhou F, Luo L, Xu M, Wang H, Xia J, et al. Haematological characteristics and risk factors in the classification and prognosis evaluation of COVID-19: a retrospective cohort study. Lancet Haematol (2020) 7:e671–8. doi: 10.1016/S2352-3026(20)30217-9
65. Colafrancesco S, Alessandri C, Conti F, Priori R. COVID-19 gone bad: A new character in the spectrum of the hyperferritinemic syndrome? Autoimmun Rev (2020) 19:102573. doi: 10.1016/j.autrev.2020.102573
66. Ruscitti P, Di Benedetto P, Berardicurti O, Panzera N, Grazia N, Lizzi AR, et al. Pro-inflammatory properties of H-ferritin on human macrophages, ex vivo and in vitro observations. Sci Rep (2020) 10:12232. doi: 10.1038/s41598-020-69031-w
67. Ruddell RG, Hoang-Le D, Barwood JM, Rutherford PS, Piva TJ, Watters DJ, et al. Ferritin functions as a proinflammatory cytokine via iron-independent protein kinase C zeta/nuclear factor kappaB-regulated signaling in rat hepatic stellate cells. Hepatology (2009) 49:887–900. doi: 10.1002/hep.22716
68. Ruscitti P, Cipriani P, Di Benedetto P, Ciccia F, Liakouli V, Carubbi F, et al. Increased level of H-ferritin and its imbalance with L-ferritin, in bone marrow and liver of patients with adult onset Still’s disease, developing macrophage activation syndrome, correlate with the severity of the disease. Autoimmun Rev (2015) 14:429–37. doi: 10.1016/j.autrev.2015.01.004
69. Cohen LA, Gutierrez L, Weiss A, Leichtmann-Bardoogo Y, Zhang DL, Crooks DR, et al. Serum ferritin is derived primarily from macrophages through a nonclassical secretory pathway. Blood (2010) 116:1574–84. doi: 10.1182/blood-2009-11-253815
70. Colafrancesco S, Priori R, Alessandri C, Astorri E, Perricone C, Blank M, et al. sCD163 in AOSD: a biomarker for macrophage activation related to hyperferritinemia. Immunol Res (2014) 60:177–83. doi: 10.1007/s12026-014-8563-7
71. Ruscitti P, Bruno F, Berardicurti O, Acanfora C, Pavlych V, Palumbo P, et al. Lung involvement in macrophage activation syndrome and severe COVID-19: results from a cross-sectional study to assess clinical, laboratory and artificial intelligence-radiological differences. Ann Rheum Dis (2020) 79(9):1152–5. doi: 10.1136/annrheumdis-2020-218048
Keywords: coronavirus disease 2019, adult-onset Still’s disease, cytokine storm, hyperferritinemia, inflammation
Citation: Meng J, Ma Y, Jia J, Wang M, Teng J, Shi H, Liu H, Su Y, Ye J, Sun Y, Cheng X, Chi H, Liu T, Zhu D, Zhou Z, Wan L, Wang Z, Wang F, Qiao X, Chen X, Zhang H, Tang Z, Yang C and Hu Q (2021) Cytokine Storm in Coronavirus Disease 2019 and Adult-Onset Still’s Disease: Similarities and Differences. Front. Immunol. 11:603389. doi: 10.3389/fimmu.2020.603389
Received: 06 September 2020; Accepted: 09 December 2020;
Published: 19 January 2021.
Edited by:
Luca Quartuccio, University of Udine, ItalyReviewed by:
Piero Ruscitti, University of L’Aquila, ItalyOnorina Berardicurti, University of L’Aquila, Italy
Copyright © 2021 Meng, Ma, Jia, Wang, Teng, Shi, Liu, Su, Ye, Sun, Cheng, Chi, Liu, Zhu, Zhou, Wan, Wang, Wang, Qiao, Chen, Zhang, Tang, Yang and Hu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiongyi Hu, aHVxaW9uZ3lpMTMxQDE2My5jb20=; Chengde Yang, eWFuZ2NoZW5nZGVAc2luYS5jb20=
†These authors have contributed equally to this work
 Jianfen Meng
Jianfen Meng Yuning Ma
Yuning Ma Jinchao Jia
Jinchao Jia Mengyan Wang
Mengyan Wang Jialin Teng
Jialin Teng Hui Shi
Hui Shi Honglei Liu
Honglei Liu Yutong Su
Yutong Su Junna Ye
Junna Ye Yue Sun
Yue Sun Xiaobing Cheng1
Xiaobing Cheng1 Huihui Chi
Huihui Chi Tingting Liu
Tingting Liu Dehao Zhu
Dehao Zhu Zhuochao Zhou
Zhuochao Zhou Liyan Wan
Liyan Wan Zhihong Wang
Zhihong Wang Fan Wang
Fan Wang Xin Qiao
Xin Qiao Xia Chen
Xia Chen Zihan Tang
Zihan Tang Chengde Yang
Chengde Yang Qiongyi Hu
Qiongyi Hu