- 1Africa Research and Impact Network (ARIN), Nairobi, Kenya
- 2African Population and Health Research Center, Nairobi, Kenya
Health and climate drivers and solutions in Africa co-exist within the same social context. Primary healthcare systems are increasingly becoming impacted by climate change. Health and climate change communities still work in isolation in addition to limited multidisciplinary and integrated research on health and climate change to inform programming, and policy and unlock climate finance. Holistic and transdisciplinary approaches that make use of resources and inputs from different sectors are key to guaranteeing effective responses to the health impacts of climate change. This paper aims to understand the landscape of climate and health (C&H) research, policy capacity building, and stakeholders hence identifying models of collaboration that could be scaled up to strengthen transdisciplinary C&H research and action. A mixed method approach was used in this study that involved the combination of consultative webinars (n = 411) online surveys (n = 198), Focused Group Discussions (n = 123), and Key informant interviews (n = 25) used on targeted stakeholders. In addition, a scoping review of policy academic documents, and databases was done. It was evident that engaging partners from diverse sectors is crucial for the broad range of perspectives, interests, skills, levels of knowledge, and resources. Stakeholder engagement in C&H initiatives is increasing and yet unevenly distributed in Africa due to funding patterns and other structural patterns. Existing C&H research predominantly focuses on climate impacts on diseases, particularly vector-borne and infectious illnesses. While crucial, this disease-centric approach limits the provision of integrated solutions for complex African socio-economic contexts. In addition, Dedicated C&H capacity-building efforts are emerging, but they mainly focus on research and policy, overlooking critical areas like leadership, investment skills, and impact assessment. Health governance and climate change should be addressed through a holistic approach that is transdisciplinary and multisectoral and through the transborder framework. The approach will need innovative thinking in socio-economies, policies, ecologies, and geographies with emphasis centered on the most vulnerable groups.
Introduction
Africa faces a significant threat from climate change, with its healthcare systems being particularly vulnerable. Extreme weather events like floods and heatwaves damage infrastructure and disrupt services making it considered a global health problem of the 21st century (Opoku et al., 2021; Theron et al., 2022). Africa is disproportionately impacted due to its vulnerability and overdependent on climatically sensitive sectors despite its low emission of GHG (4%) (Wright et al., 2021; Campbell-Lendrum et al., 2023). The vulnerability is partly attributed to existing challenges such as poverty and weak health systems which restricts the capacity of nations to adequately address additional health issues caused by climate change (Owen et al., 2011). It is noteworthy that both the direct and indirect health impacts of climate change are mediated by health determinants, with heat stress, vector ecology, and air quality serving as primary exposure pathways (Africa Research and Impact Network (ARIN) and Africa Population Research Center (APHRC), 2024). According to WHO (2000), health systems refers to all the institutions, organizations, and resources that are committed to producing health actions. They form the basis of resilience at the individual and community levels. The services rendered through the health systems are usually deemed to be the first line of defense in averting negative health effects and safeguarding populations (Lugten and Hariharan, 2022). A new study conducted by the WHO revealed that 56% of the public health events documented in Africa from 2001 to 2021 were climate-related (WHO, 2000). Worth noting is that the extent of health impacts posed by climate change which varies significantly among different communities and regions because of factors like quality of existing health infrastructure, geographic and micro-climate dissimilarities, socio-economic conditions, underlying epidemiology, and communication capacity (Owen et al., 2011). According to WHO, for example, climate-related health risks intensified in the Horn of Africa as a surge of disease outbreaks was witnessed in a region where the population was already experiencing acute hunger, something that further heightens the health crisis (WHO, 2000). While the focus of climate change and health discussions has predominantly centered on communicable diseases, emerging evidence indicates that rising temperatures are exacerbating non-communicable diseases (NCDs), such as cardiovascular disease, particularly among individuals with pre-existing conditions (Siiba et al., 2024).
It is anticipated that climate change will greatly strain the global healthcare systems by 2050 causing 14.5 million extra mortalities and economic losses worth $12.5 trillion. Moreover, the induced effects of climate change will further account for $1.1 trillion additional costs to healthcare systems, something that will create a substantial extra burden to the infrastructure that is already strained as well as medical and human resources. According to the World Economic Forum (2024), the leading risk of climate-induced deaths will be caused by floods followed by droughts, which are directly associated with extreme heat, accounting for 8.5 million and 3.2 million deaths, respectively, by 2050. On the other hand, heat waves attributed to extended duration of extreme temperatures and humidity will have the greatest financial impact by 2050 due to loss in productivity, estimated at $7.1 trillion. Worth mentioning is that global health iniquities will be exacerbated by climate change with the most vulnerable populations such as the elderly, women, youth, low-income earners, and inaccessible communities being disproportionately affected by the climate-related impacts. The threats are high in regions with most dense and vulnerable populations, and which are ill equipped to adapt (World Bank, 2018).
Given that the health issues linked to climate change such as fluctuating temperature and vector-borne diseases are not restricted to geographical and political borders, a holistic and transdisciplinary approach that makes use of resources and inputs from different sectors should be adopted to guarantee effective response (Wright et al., 2021). However, despite the momentum and efforts toward addressing climate impacts on health, the roles, activities, and progress of various actors and initiatives remain unknown, and stakeholder needs are yet to be well understood. This limitation restricts opportunities for strengthening collaborations and scaling up the climate and health (C&H) agenda (Hartwell et al., 2023). While climate and health research communities are relatively well-developed, their connection is currently weak due to limited understanding of the modes of engagements for integrating health and climate change research, policy, and practice. Existing networks have focused on integrating social science into health debates (e.g., LanderNet); scoping health and climate data (e.g., the INSPIRE network); and pursuing new climate-health research (e.g., heat-related health risks in natural settings).
Besides, climate change and health research are often compartmentalized across various disciplines, resulting in a fragmented landscape of specialized discussions. This compartmentalization hinders efforts to synthesize key findings aimed at identifying trends and gaps in the evidence (Berrang-Ford et al., 2021). Additionally, the field of climate and health, which involves researchers, policy-makers, and implementation partners working collaboratively to address climate-related health issues, is still in its infancy. Notably, this field remains relatively small in low- and middle-income countries, where it currently receives only a fraction of the research funding available for climate change.
Urgent action is therefore imperative if economies are to be decarbonized and more resilient health systems developed (Wright et al., 2021). This can be accomplished by providing evidence to support action, leading in climate advocacy and leadership, guiding sectors that significantly affect health through their actions, and assuming responsibility for climate resilience and the imperative to decarbonize healthcare systems. The health community, with its influential voice, has the potential to make a distinctive and potent contribution. This can be accomplished by providing evidence to support action, leading in climate advocacy and leadership, guiding sectors that significantly affect health through their actions, and assuming responsibility for climate resilience and the imperative to decarbonize healthcare systems (Campbell-Lendrum et al., 2023). Transdisciplinary research and action agenda on climate change and health can help inform evidence given the human-environmental system problems being currently experienced by society. This is because transdisciplinary research (TDR) can address complex challenges that may not be effectively resolved through conventional science (OECD, 2020). TDR provides realistic options for dealing with highly disputed issues with high stakes. The study aimed to improve understanding of how collaborations can facilitate the integration of health considerations into climate change policies and systems.
Materials and methods
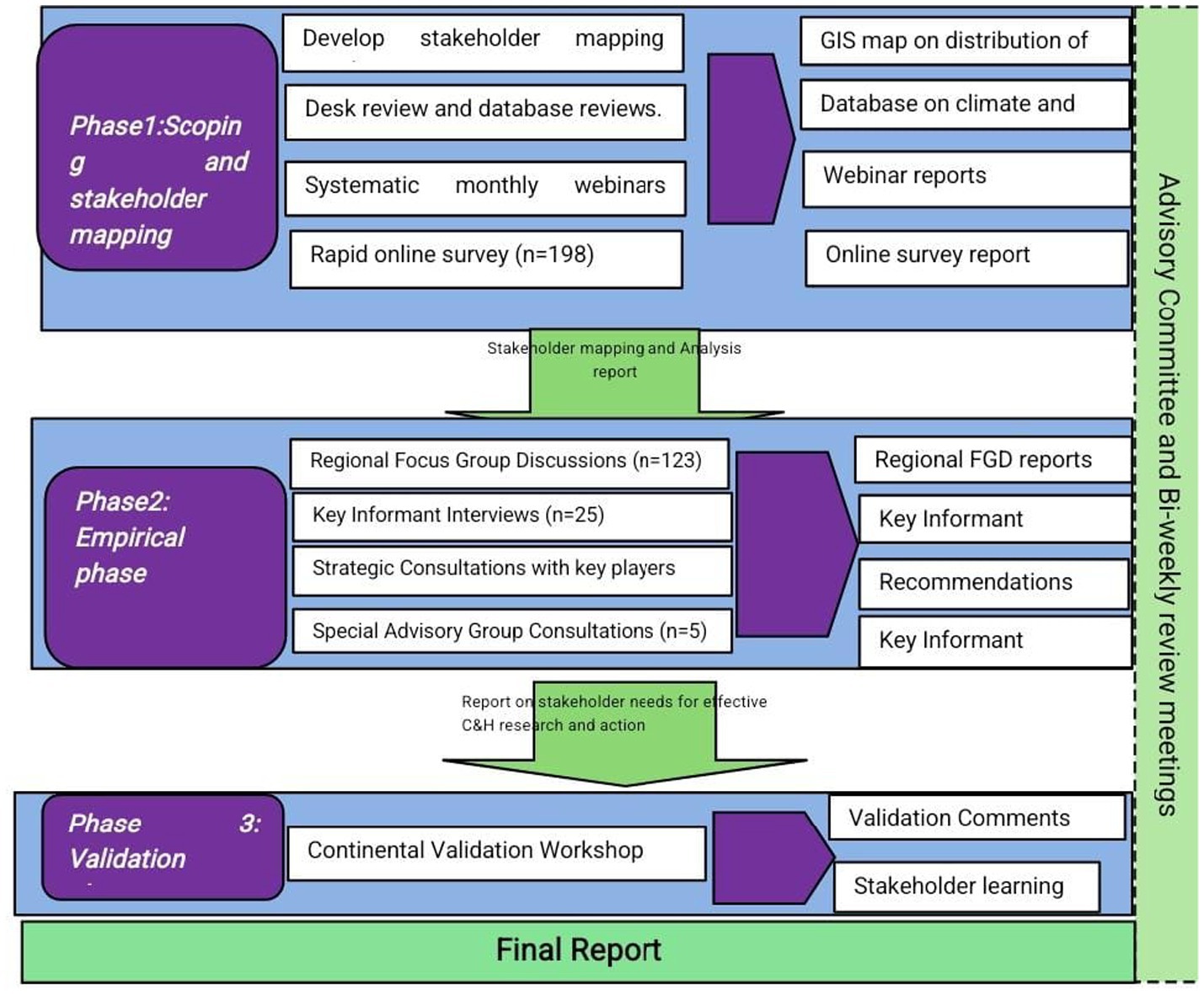
The study was conducted in three phases, as illustrated in Figure 1. Mixed method approach that involved both quantitative and qualitative approaches was used. Phase 1 involved review of policy/academic documents, databases and consultative webinars (n = 411) and an online survey (n = 198) to map the C&H policy, research and stakeholder distribution and their needs. Phase 2 involved targeted empirical engagements including regional focus group discussions (FGDs) (n = 123) and Key Informant Interviews (KIIs) (n = 25) to identify specific climate and health research, collaboration models and case studies to support suggested recommendations. The final phase involved validation of key findings by diversity stakeholders including policy makers, civil society organization, and research. The consultations process largely relied on knowledge and experience of individual stakeholders or experts representing organizations/initiatives. While these insights offer valuable perspectives, they do not necessarily provide a completely comprehensive picture of the climate and health research and policy landscape. They do, however, highlight specific aspects of practice that stakeholders believe require further attention. An advisory group was established to provide bi-monthly strategic guidance throughout the study.
Results
Climate and health policy landscape
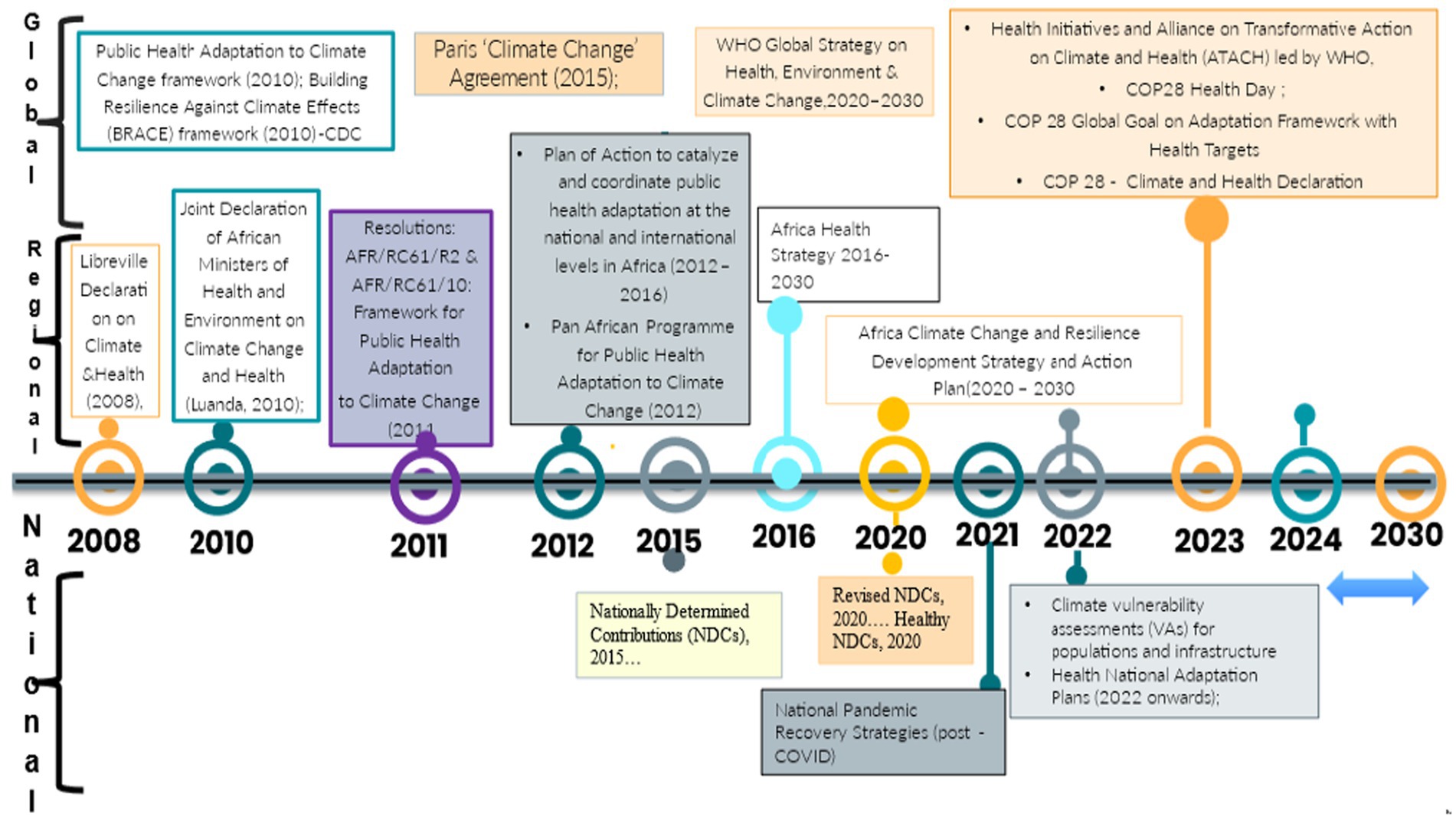
The climate and health (C&H) policy landscape is undergoing a significant transformation, shifting from multilateral agreements toward frameworks that prioritize integrated approaches and place health at the forefront of climate policy. The transformation is marked by critical junctures that reinvigorate collective action at all levels. Figure 2 illustrates this progression of the C&H policy agenda across various scales. The policy progression builds on the previous global and regional declaration decades ago that sort to foster public health resilience and overall environmental health. These efforts have culminated in the renewed focus on integrated approaches anchored in the 2015 Paris Agreement (PA). Established policies on climate change already exist under the United Nations Framework Convention on Climate Change (UNFCCC).
The establishment of global frameworks such as the Alliance for Transformative Action on Climate and Health (ATACH) by the World Health Organization (WHO) during the 26th Conference of parties (COP 26) provide some guidelines, governments are adopting contextual approaches in the implementation of global targets at national levels. Countries are currently advancing Health National Adaptation Plans (HNAPS) guided by the ATACH framework. However, localized tools and skills are necessary to support the development of implementation plans for HNAPs. Consultations revealed challenges in translating HNAPs into action, even in countries with seemingly advanced plans. By early 2024, 17 countries were engaged in national consultations for HNAPs. These processes foster collaboration among health-determining sectors, stimulating demand for and uptake of transdisciplinary research and evidence. The inclusion of health as a key focus area in the Global Goal on Adaptation Framework provides a foundation for setting targets and monitoring policy progress. Notably, Paragraph 9 of the Global Goal on Adaptation Framework, established at COP 28, identified health as a target sector for developing adaptation targets and reporting. For instance, Uganda and Tanzania have integrated health considerations into their climate plans. Burundi and Côte d’Ivoire exemplify leadership in this area (Global Climate and Health Alliance, 2023). Moreover, countries like Egypt, Rwanda, and Zambia have developed specific health sector response plans to address heat-related illnesses. However, these plans lack concrete implementation details, such as specific tasks, timelines, and assigned responsibilities. This can hinder progress in translating policy into action.
Pan-African declarations and strategies, such as the African Union Climate Change and Resilient Development Strategy and Action Plan (2022–2032), also promote these objectives through the One Health Agenda (African Union, 2022). At the national level, a multi-sectoral approach to developing health adaptation plans is gaining momentum, although a dearth of transdisciplinary evidence remains a challenge. Operationalizing global climate and health frameworks at national and regional levels presents significant challenges. Policymakers struggle to adapt global data platforms to inform national vulnerability assessments and HNAPs. Regional focus groups and consultations with policymakers identified key obstacles, including sectoral tensions between climate and health domains, a dearth of domestic expertise to interpret climate-health linkages, and a lack of contextual data. While countries like Uganda and Tanzania have integrated health into climate plans, concrete implementation steps, such as defined tasks, timelines, and accountability, remain elusive (Africa Research and Impact Network (ARIN) and Africa Population Research Center (APHRC), 2024). In Kenya for instance, a functional Climate, Energy and Health working group exists that is spearheading the formulation of Household Air Pollution Strategy.
Climate and health stakeholders in Africa
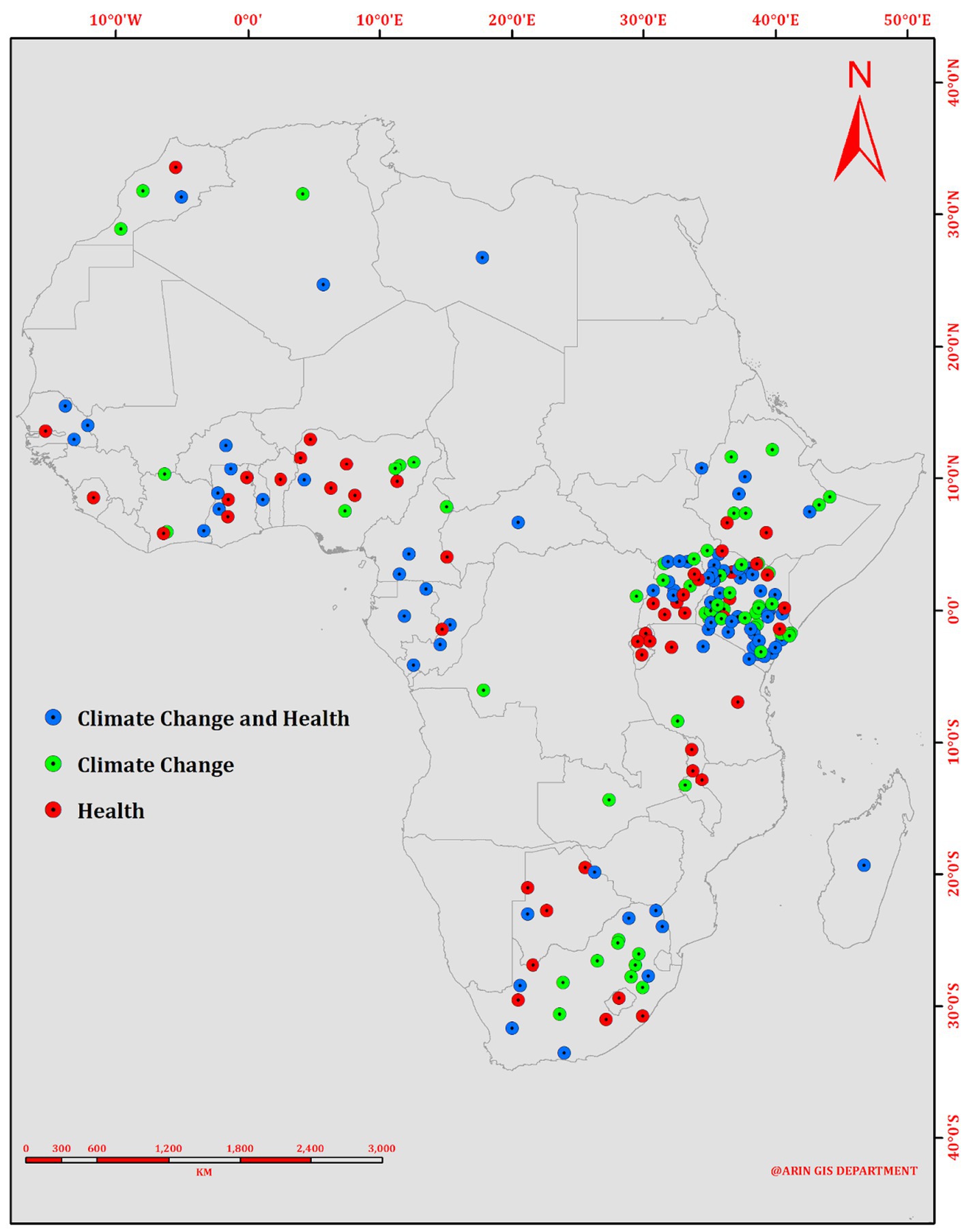
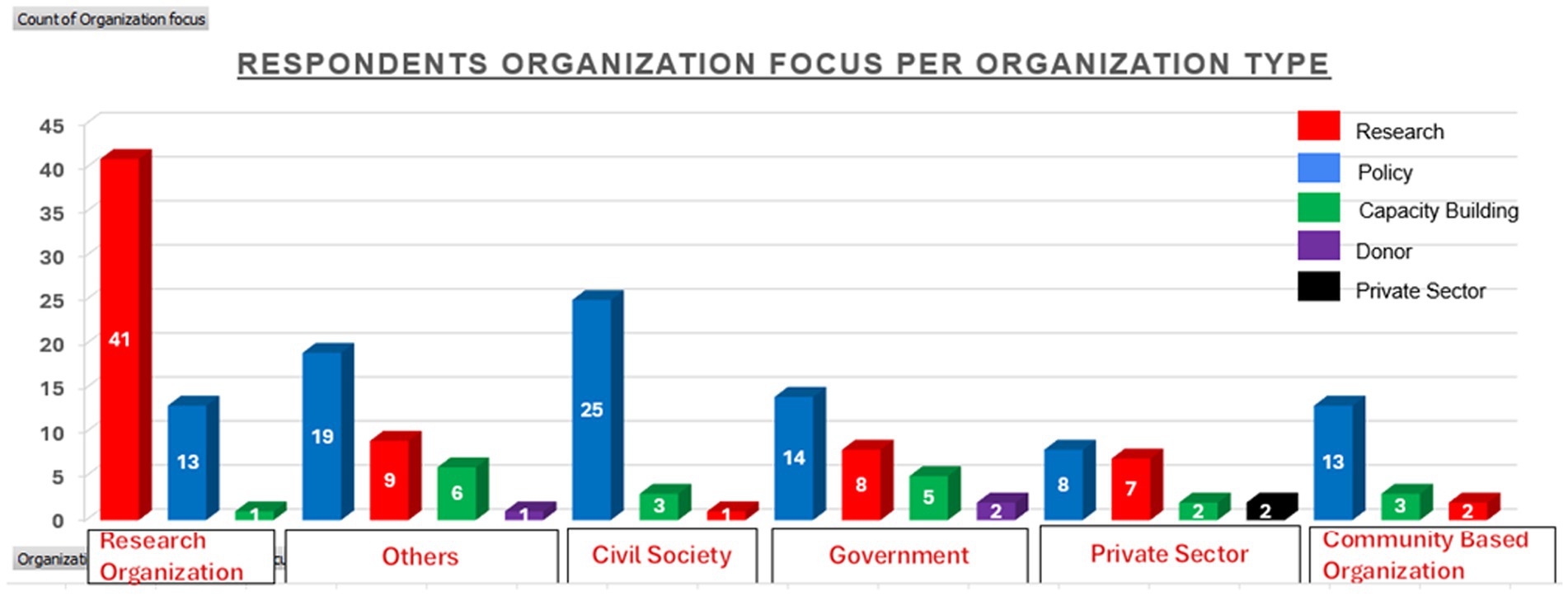
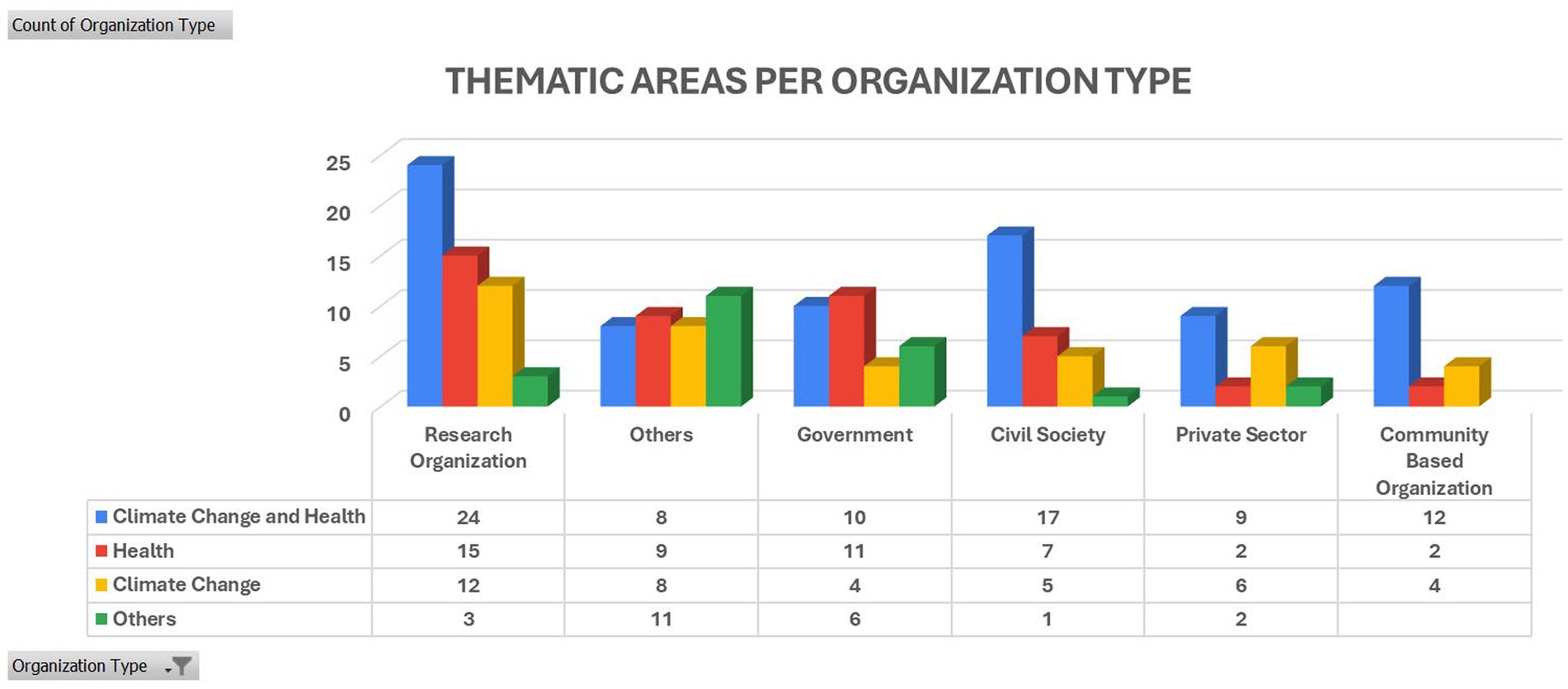
The climate and health landscape is increasingly complex, comprising stakeholders from research, policy, advocacy, capacity building, and funding. Figure 3 illustrates the spatial distribution of the stakeholders mapped in climate change and health. This is purely by design of the study where the focus was to identify organizations working the C&H intersection. It is worth mentioning that some of the organizations listed under the C&H thematic area may not necessarily have C&H as their focus but have short-term based project(s) focusing on C&H. The imbalance in geographical distribution in stakeholders involved in climate change and health work in Africa is influenced by funding, vulnerability and geopolitics. Of the (N = 188) stakeholders mapped, (n = 52) focused solely on climate change, (n = 57) on health, and (n = 79) on the climate-health nexus. Stakeholder concentration is highest in East, West, and Southern Africa, with under-representation in central and northern Africa. Many stakeholders engage in multiple thematic areas across research, policy, and capacity building, creating potential synergies for transdisciplinary research and action (TDR). As illustrated in Figure 4, most research organizations prioritize research while incorporating policy elements. However, capacity-building initiatives within these organizations are limited, suggesting potential gaps in translating research into practical solutions. Conversely, civil society organizations predominantly focus on policy advocacy with less emphasis on research, highlighting the need to bridge the gap between advocacy and evidence-based action. Government organizations primarily address policy issues with limited research and capacity building, hindering the development of actionable programs based on existing policies.
Climate change health research landscape
While existing research has strengthened the evidence base for climate change’s impact on health, a greater emphasis on solution-oriented research is required. A rapid mapping of African C&H literature revealed that over 80% of initiatives explore the impact of climate events on disease prevalence, particularly vector-borne diseases. Focus Group Discussion (FGD) results indicated that while a lot of research is being conducted, it is being done in silos, something that may help explain why there is insufficient evidence on the relationship between climate and health. This claim equally aligned with the findings of the online survey as can be seen in Figure 4. Besides, the stakeholder mapping exercise revealed that most of the C&H initiatives mainly focused on vector-borne diseases, such as Malaria, in diverse climatic contexts. Participants targeted for the Focus Group Discussion and Key Informant Interviews (KIIs) session asserted that a need exist to enhance data collection on health impacts of climate change through demographic and health surveys targeting aspects such as temperature and heat effect. It is imperative to sensitize and engage the public, deploying tools to routinely gather information and increase the availability of short videos showcasing the impacts of climate change on health for dissemination, especially targeting youth audiences. Data should equally be centralized to facilitate access at both local and international levels, while also avoiding duplication of efforts. A need also exist to transition from research activities to the practical implementation of evidence-based practices. Moreover, it was noted that most of the existing C & H data is generated by international organizations, with limited regional contributions due to lack of funding and relevant expertise. This was equally corroborated by the findings of the online survey (Figure 5).
Based on this finding, it was agreed that regional research should be generated to inform local action. Research interventions should start from basic needs assessments, environmental and community scoping on climate change issues, and generate enough evidence that involves the community in the study considering that climate change impacts various fields including biodiversity, energy efficiency, environmental issues, and renewable energy. In Nigeria and much of West Africa for example, it was noted that drought has led to insecurity forcing people to move to places they are not sure they will be welcomed. As a defense mechanism, they become aggressive when relating with the people in the new places they have settled. As such, drought is a climate change impact that has to be addressed collectively with communities and governments given the impact it has on health.
Key stakeholder needs
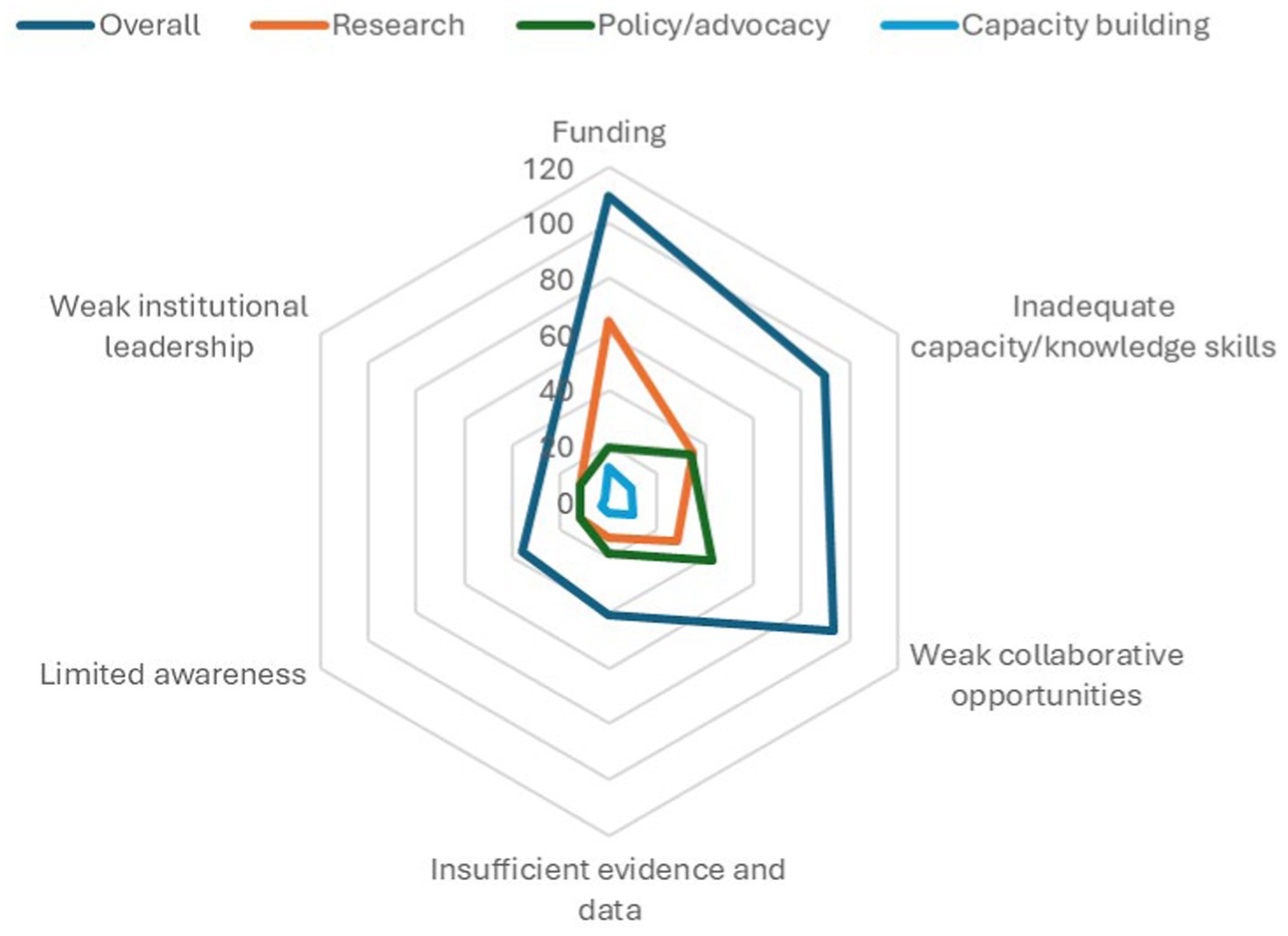
We applied both surveys and webinars to identify preliminary stakeholder needs. As for the surveys, we asked respondents about the pressing barriers/challenges to integrated C&H research and action. In this section, we interpret these barriers to be synonymous to the needs of these stakeholders triangulated through the webinars and document reviews. Figure 6 illustrates several key stakeholder needs derived from an online survey encompassing responses from 198 respondents. The counts have been established based on the number of times a particular need/barrier occurred within the top three mentioned barriers by all respondents. This data was cross-referenced with insights gathered during webinar discussions. While some of these needs have been previously emphasized in the preceding sections, here we offer concise overviews explaining why stakeholders consider them significant.
Results show that different stakeholder groups have different needs. Overall, limited funding had the highest rank followed by weak collaboration and inadequate capacity. The ranks were different for different stakeholders. For research-focused stakeholders, funding remains highly ranked as a key barrier/need while for policy-focused stakeholders, weak collaborations and inadequate capacity are key barriers. Funding remains a key barrier for capacity building- focused stakeholders.
Discussion
Climate and health policy
Existing climate policies and other health-determining sectoral policies, such as those in energy and agriculture, can enhance health outcomes. These include National Climate Change Action Plans (NCCAPs), Nationally Determined Contributions (NDCs), National Adaptation Plans (NAPs), Renewable Energy Strategies, Agricultural Development Strategies, and Air Quality Strategies. By identifying the most urgent and immediate needs for adapting to climate change across sectors, these policies lay a strong foundation for integrating health considerations into climate action (Africa Research and Impact Network (ARIN) and Africa Population Research Center (APHRC), 2024). The commitment by over 80 countries globally and 33 in Africa to the ATACH is an indication of the need of the countries to address climate change effects in the health sector. The development of HNAPs by countries also affirms its support to orient policies toward transdisciplinarity in addressing climate change effects on health. This in turn also goes hand in hand with commitment by countries to commit part of their budgets to climate change and health aspects and source for more funding to address gap deficits in funding. Efforts to address the health impacts of climate change are evolving rapidly supported by the contributions from a diverse range of stakeholders. These include governments implementing policies, research organizations generating data and evidence, civil societies promoting advocacy, and funders and private sector bodies providing investments. The 2010 Building Resilience Against Climate Effects (BRACE) framework (Marinucci et al., 2014) was developed by the United State Center for Disease Control (CDC) to encourage the engagement of local and national public health systems and actors in climate change adaptation. Similarly, the Africa Union Climate Change and Resilient Development Strategy and Action Plan (2022–2032) (African Union, 2022) recognizes the role of health in building healthy and resilient economies and calls for integrated efforts by all sectors and stakeholders to strengthen resilient health systems.
Overall, there is a significant momentum in the C&H policy agenda. The World Health Organization remains a key player in propelling the global policy momentum that spurs action at the national level, with both the Ministries of Health and Environment in various countries playing critical roles. While policy readiness appears to be taking shape, implementing these policies requires more than just the documents. Stakeholders emphasize the need to build a cadre of skills and expertise capable of translating policies into actionable programs and interventions that can yield the desired outcomes. Additionally, there appears to be an increasing availability of funding opportunities for C&H, but the institutional arrangements for disbursing these funds need careful consideration and design to inspire transdisciplinary collaboration necessary for creating impact.
The multi-sectoral approach to addressing climate change impacts on health is critical given that health is interconnected with other sectors where climate change impacts and actions are most strongly felt. Evidence shows that responses in various sectors impact health outcomes in different ways. This has inspired a diversity of stakeholders drawn from different sectors to respond to this call. More recently, a number of actors are turning their attention to integrated Climate and Health (C&H) research and action.
Climate and health research
Health is increasingly becoming a sector at the forefront of climate change impacts in Africa, alongside agriculture (Opoku et al., 2021). This heightened susceptibility is exacerbated by an already strained healthcare system and the absence of robust adaptation actions, which are further compounded by the region’s fragile socio-economic conditions (Theron et al., 2022; Opoku et al., 2021). Numerous climate change impacts on health have been documented, ranging from an increase in vector-borne diseases to respiratory illnesses resulting from inhaling toxic greenhouse gases (GHGs), as well as, heat-related conditions among others. Vulnerable populations are particularly susceptible to heatwaves attributed to rapidly rising temperatures, and mortalities related to heat increased by 68% between 2000 and 2021. Due to the changing climate, certain ecosystems that were initially pathogen-free, such as coastal waters, are progressively becoming suitable for the spread of Vibrio pathogens. The expanding breeding conditions for pathogens have led to an increase in the number of cholera cases (Baker-Austin et al., 2013). Other Vibrio species have been noted in non-endemic areas due to the rise in sea surface temperatures, particularly evident in cold/temperate regions that have been significantly impacted by global warming (Vezzulli et al., 2015). The transmission of malaria in the highland areas of Africa also increased by 13.8 and 31.3%, respectively, between 1951 to 1960 and 2012 to 2021 (Romanello et al., 2022). Additionally, air pollution, partly caused by greenhouse gases (GHGs), claims over a million lives annually across Africa (United Nations Environment Programme, 2022). These vulnerabilities pose severe implications to the health sector, including overall impacts on health systems such as reduced access to primary healthcare, especially by vulnerable groups whose income levels continue to decrease. There is also the destruction of healthcare facilities, especially in flood-prone areas, and overall shifts in health-related budgets to support climate action.
So far, there is sufficient evidence that climate change significantly impacts health outcomes. This is attributed to climate change and health research often operating in silos, hindering knowledge synthesis and the identification of evidence gaps (Berrang-Ford et al., 2021). A major gap identified during our initial consultations, especially in the research and policy context, is the limited evidence on attribution to help clarify C&H linkages in an actionable manner. With increasing demand for evidence including indicators and tools that can clarify the C&H linkages and inform strategies, efforts have been channeled toward the development of indicators (CCHIs) that represent C&H relationships (Kenney et al., 2018; Murray et al., 2020; Hambling et al., 2011; Liu et al., 2021).
The data, so far, shows that the severity of climate impacts on health are increasing yet adaptation measures remain unclear and uncoordinated. In terms of heat, the indicators show increasing suitable areas for anopheles’ mosquitoes for transmission of Plasmodium falciparum in the 2013–2022 period, compared to 1951–1960. The data also shows that drought is a major climate risk, which alters the hydrological cycle, threatening drinking water supplies and sanitation, crop and livestock productivity, nutrition, wellbeing, and health. The increase in heat wave and drought seasons in 2021 compared to 1981–2010, is associated with a double increase in the number of people facing food insecurity and malnutrition in Africa. Data from Lancet provides indicative information and framework on general trends even though such efforts could benefit from more evidence and contextual data attributed to the C&H relationship.
Therefore, addressing the impacts of climate change on health requires a multi-sectoral and multi-stakeholder approach. An integrated multi-stakeholder and multi-sectoral approach to tackling the impacts of climate change on health can leverage sector opportunities and avoid the risk of relieving one sector while exacerbating another, a situation otherwise referred to as maladaptation in the health sector (Romanello et al., 2022). Such a situation was witnessed in the wake of COVID-19 where response mechanisms failed to deliver the green recovery, livelihoods, and social welfare proposed by the health community but instead worsened the health risks associated with climate change.
Effective approaches to foster transdisciplinary research in advancing C & H
Advancing the climate and health agenda in Africa will depend on how well the linkages between research, policy, and society are strengthened in addition to tackling existing inequalities in research. While research evidence has been identified to be key in furthering sustainable development in policy documents like the 2030 United Nations Agenda and the 2063 African Union Agenda, data generated from the Global North may fail to effectively foster the much needed transformative change in Africa (Schneider et al., 2023). Though data from the Global North may help inform researchers, policymakers, and communities on how to address C & H issues, they may not be context-relevant, and thus the need to support and augment the capacity of African researchers to enable them to produce context-specific data for action. The following are some of the ways in which stakeholders can be supported to undertake transdisciplinary research and advance climate and health action:
1 Funding
Providing transdisciplinary funding encourages researchers to focus on areas that directly influence policy. Encouraging and supporting transdisciplinary research projects that involve researchers, policy-makers, and practitioners working together from the inception of a project promotes a holistic approach to addressing climate and health issues. This ensures that research findings are relevant and applicable to real-world policy and practice. According to Schneider et al. (2023) donors can promote the integration of C & H in Africa by actively encouraging research-policy-society interactions through transdisciplinary research (TDR). This can be achieved by permitting African researchers to steer high-quality TDR projects, enabling them to pursue TDR research careers, and improving the environment for doing TDR in the region.
2 Establishing Collaborative Networks
Creating platforms and networks that bring together researchers, policy-makers, and practitioners from various disciplines and sectors is key. This allows for the exchange of knowledge, sharing of best practices, and collaboration on research and policy development. FGD results indicated that collaboration mechanisms should be utilized to inform evidence-based programming and advocacy for interventions aimed at strengthening the intersection of climate and health. Collaboration between Global South and Global North countries can help advance shared goals in addressing climate and health challenges. South–South collaboration fosters enhanced data sharing and information exchange due to similarities of the interconnected issues faced. On the other hand, North–North collaboration facilitates the vertical transfer of tools, technology, funding, approaches, and knowledge. However, while acknowledging the importance of North–South collaborations, the significance of South–South collaborations was also underscored by the FDG participants. This is particularly crucial given that Africa’s indexed research findings are predominantly shaped by international collaborations, with North–South collaborations reinforcing Africa’s position in the global scientific landscape. For instance, between 2017 and 2019, Central and East Africa cumulatively accounted for 88% of the scientific publications with international co-authors, while Southern Africa represented 85% of the scientific publications with foreign co-authors (Lewis et al., 2021). South–South collaboration thus represents an opportunity for African researchers to assert control over their research agenda and establish their priorities.
3 Facilitating Regular Communication
Encouraging regular communication channels such as meetings, conferences, and webinars helps to foster dialogue and information sharing between different stakeholders. This ensures that all parties are up-to-date with the latest research, policy updates, and field experiences. More information ought to be provided on the connection between climate and health as most people view them separately. This can be done by sharing evidence of how climate change can affect the health sector, and similarly how the health sector can get prepared and minimize the negative effects of climate change. From the 4 online C & H webinar series that were conducted, participants expressed interest to be involved in future engagements, “it’s a great honor to contribute for change and do not miss out to get back for any session arranged” while others expressed interest to partner with ARIN to help advance the C & H agenda in the region, “Is there a formal pathway for joining up with ARIN on our climate/health in Africa portfolios?” Funders should give attention too to support such activities.
4 Capacity Building and Knowledge Translation
Supporting capacity-building initiatives that enhance the skills and understanding of researchers, policy-makers, and practitioners across different disciplines and sectors is crucial. This can include training programs, workshops, and mentoring opportunities. Findings from the FGD indicate that collaborative efforts involving different stakeholders are essential for curriculum development. It was suggested that climate change and health courses should be developed either as standalone programs or integrated into existing courses. Moreover, there should be dedicated centers within universities focused on climate change and health to encourage further research and capacity building in this field. Recognizing this need, Aga Khan University has shown interest in developing an environmental health curriculum aimed at imparting knowledge to healthcare professionals on the interrelation between climate change and health.
Additionally, translating research findings into accessible formats and disseminating them widely helps to bridge the gap between research and policy/practice. Besides, results from the online survey indicated that the healthcare industry has the potential to make a positive impact on the planet by promoting sustainable policies, educating the public, and investing in research on sustainable healthcare practices by sharing best practices, advocating for sustainability policies, and building partnerships with other organizations. This claim is supported by Wright et al. (2021) who asserts that the general public is more persuaded to mitigate climate change if it is devised as a health problem with the information propagated by health professionals. A need also exist for capacity building and empowerment of new researchers on health and climate in addition to need for adequate financing for research on Health and climate.
5 Engaging Stakeholders in Co-creation Processes
Involving stakeholders, such as community members, advocacy groups, and non-governmental organizations, in the co-creation of research projects, policies, and interventions fosters a sense of ownership and ensures that their voices and perspectives are included. This increases the likelihood of successful implementation and sustainable outcomes. Researchers can equally work closely with policymakers and practitioners to identify pressing knowledge gaps and prioritize research that will have a direct impact on policy and practice. According to Shackleton et al. (2023), the transformation needed to address the health impacts of climate change in Africa demands innovative approaches of mobilizing resources, working jointly, and applying knowledge. To efficiently address the diverse C & H challenges as well as the varied needs and interests of actors in the different sectors, research must be effectively interlinked with policymaking, planning, and action. The co-generation of data across disciplines is one approach that can foster such transformations. By providing timely and policy-relevant research, researchers can support evidence-based decision making and effective implementation of climate and health policies.
Overall, fostering strong connections and coordination among researchers, policy-makers, and practitioners working on climate and health issues requires ongoing communication, collaboration, and an inclusive approach that values the contributions of all stakeholders involved.
Conclusion
Engaging partners from diverse sectors is crucial for the broad range of perspectives, interests, skills, levels of knowledge, and resources that it brings. Health governance and climate change should be viewed and addressed collectively as a human and population concern besides being considered as a matter of health promotion and disease prevention only. Consequently, a more effective response will necessitate a holistic systems approach that is transdisciplinary and multisectoral, which integrates climate change and health governance in a transborder framework. The approach will need innovative thinking on socio-economies, policies, ecologies, and geographies with emphasis centered on the most vulnerable groups.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by National Commission for Science Technology and Innovation. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft. EB: Formal analysis, Methodology, Writing – original draft. HA: Validation, Writing – review & editing. KM: Investigation, Supervision, Writing – review & editing. ST: Software, Writing – review & editing. EG: Formal analysis, Writing – review & editing. AW: Conceptualization, Writing – original draft, Writing – review & editing. HG: Methodology, Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research received funding from the Wellcome Trust.
Acknowledgments
The authors greatly acknowledges all stakeholders that made this research successful.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Africa Research and Impact Network (ARIN) and Africa Population Research Center (APHRC) (2024). Consultation on communities of practice for transdisciplinary research and action in climate change and health in Africa (technical report no. 9).
African Union (2022). African union climate change and resilient development strategy and action plan (2022-2032). Available at: https://au.int/en/documents/20220628/african-union-climate-change-andresilient-development-strategy-and-action-plan
Baker-Austin, C., Trinanes, J. A., Taylor, N. G., Hartnell, R., Siitonen, A., and Martinez-Urtaza, J. (2013). Emerging Vibrio risk at high latitudes in response to ocean warming. Nat Clim Chang 3, 73–77.
Berrang-Ford, L., Sietsma, A., Callaghan, M., Minx, J., Scheelbeek, P., and Haddaway, N. (2021). Systematic mapping of global research on climate and health: a machine learning review. Lancet 5, 514–525. doi: 10.1038/s41558-021-01170-y
Campbell-Lendrum, D., Neville, T., Schweizer, C., and Neira, M. (2023). Climate change and health: three grand challenges. Nat. Med. 29, 1631–1638. doi: 10.1038/s41591-023-02438-w
Global Climate and Health Alliance (2023). 2023 healthy NDC scorecard. Available at: https://climateandhealthalliance.org/initiatives/healthy-ndcs/ndcScorecards
Hambling, T., Weinstein, P., and Slaney, D. (2011). A review of frameworks for developing environmental health indicators for climate change and health. Int. J. Environ. Res. Public Health 8, 2854–2875. doi: 10.3390/ijerph8072854
Hartwell, C., Lovell, S., Hess, J. J., Dolan, K., Vickery, J., and Errett, N. A. (2023). Barriers and facilitators to state public health agency climate and health action: a qualitative assessment. BMC Public Health 23:145. doi: 10.1186/s12889-023-14996-2
Kenney, M. A., Janetos, A. C., and Gerst, M. D. (2018). A framework for national climatndicators. Clim. Chang. 163, 1705–1718. doi: 10.1007/s10584-018-2307-y
Liu, A. Y., Trtanj, J. M., Lipp, E. K., and Balbus, J. M. (2021). Toward an integrated system of climate change and human health indicators: a conceptual framework. Clim. Chang. 166, 1–16. doi: 10.1007/s10584-021-03125-w
Lugten, E., and Hariharan, N. (2022). Strengthening health Systems for Climate Adaptation and Health Security: key considerations for policy and programming. Health Secur. 20, 435–439. doi: 10.1089/hs.2022.0050
Marinucci, G., Luber, G., Uejio, C., Saha, S., and Jeremy, J. H. (2014). Building resilience against climate effects—a novel framework to facilitate climate readiness in public. Health agencies. Int. J. Environ. Res. Public Health 11, 6433–6458. doi: 10.3390/ijerph110606433
Murray, K. A., Escobar, L. E., Lowe, R., Rocklov, J., Semenza, J. C., and Watts, N. (2020). Tracking infectious diseases in a warming world. BMJ 371:m3086. doi: 10.1136/bmj.m3086
OECD. (2020). (Organisation for Economic Co-operation and Development). Addressing societal challenges using transdisciplinary research in OECD Science, Technology and Industry Policy Paper 88. Paris: OECD Publishing. doi: 10.1787/0ca0ca45-en
Opoku, S., Filho, W., Hubert, F., and Adejumo, O. (2021). Climate change and health preparedness in Africa: analysing trends in six African countries. Int J Environ Res Public Health. 18:4672. doi: 10.3390/ijerph18094672
Owen, O., Okereke, C., Webb, J., and Musa, M. (2011). “Climate change and health across Africa: issues and options” in United Nations Economic Commission for Africa African Climate Policy Centre. Working Paper 20.
Schneider, S., Fürsich, F. T., Werner, W., and Pierce, C. S. (2023). Comment on: Magalhães et al., Middle Jurassic multiscale transgressive–regressive cycles: An example from the Lusitanian Basin. Depositional Record.
Shackleton, C., Matsuoka, K., Moholdt, G., Liefferinge, B. V., and Paden, J. (2023). Stochastic Simulations of Bed Topography Constrain Geothermal Heat Flow and Subglacial Drainage Near Dome Fuji, East Antarctica. J. Geophys. Res. Earth. Surf, 128:e2023JF007269. doi: 10.1029/2023JF007269
Siiba, A, Kangmennaang, J, Baatiema, L, and Luginaah, I. (2024). The relationship between climate change, globalization and non-communicable diseases in Africa: A systematic review. PLoS ONE. 19:e0297393. doi: 10.1371/journal
Romanello, M., Di Napoli, C., Drummond, P., Freen, C., Kennard, H., and Lampard, P. (2022). The 2022 report of the lancet countdown on health and climate change: health at the mercy of fossil fuels. Lancet 400, 1619–1654. doi: 10.1016/S0140-6736(22)01540-9
Theron, E., Bills, C., Hynes, E., Stassen, W., and Rublee, C. (2022). Climate change and emergency care in Africa: a scoping review. Afr. J. Emerg. Med. 12, 121–128. doi: 10.1016/j.afjem.2022.02.003
Lewis, J., Schneegans, S., and Straza, T. (2021). UNESCO Science Report: The race against time for smarter development (Vol. 2021). Unesco Publishing.
Vezzulli, L., Pezzati, E., Brettar, I., Höfle, M., and Pruzzo, C. (2015). Effects of global warming on vibrio ecology. Microbiol. Spectr. 3, 25–36. doi: 10.1128/microbiolspec.VE-0004-2014
WHO (2000). The world health report 2000: health systems: improving performance. The Amazon: World Health Organization.
World Bank. (2018). A Country-Based Approach for Assessing Risks and Investing in Climate-Smart Health Systems. Available at: https://shorturl.at/senUi
World Economic Forum. (2024). Quantifying the Impact of Climate Change on Human Health. Geneva, Switzerland: World Economic Forum. Available at: https://www3.weforum.org/docs/WEF_Quantifying_the_Impact_of_Climate_Change_on_Human_Health_2024.pdf.
Keywords: climate change, health, transdisciplinary, holistic, healthcare systems, stakeholder engagement
Citation: Atela J, Bolo E, Agevi H, Muindi K, Thiam S, Gordon E, Wanjiru Irungu A and Gitau H (2024) Stakeholder analysis towards unpacking communities of practice for transdisciplinary research and action in climate change and health in Africa. Front. Hum. Dyn. 6:1454597. doi: 10.3389/fhumd.2024.1454597
Edited by:
Happy Mathew Tirivangasi, University of Jyväskylä, FinlandReviewed by:
Shingirai S. Mugambiwa, University of Limpopo, South AfricaPeter Omemo, Maseno University, Kenya
David Chikwaza, Dublin City University, Ireland
Copyright © 2024 Atela, Bolo, Agevi, Muindi, Thiam, Gordon, Wanjiru Irungu and Gitau. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joanes Atela, ai5hdGVsYUBhcmluLWFmcmljYS5vcmc=
 Joanes Atela
Joanes Atela Emily Bolo
Emily Bolo Humphrey Agevi
Humphrey Agevi Kanyiva Muindi2
Kanyiva Muindi2 Sokhna Thiam
Sokhna Thiam Ezekiel Gordon
Ezekiel Gordon Ann Wanjiru Irungu
Ann Wanjiru Irungu