
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Glob. Womens Health , 20 November 2024
Sec. Sex and Gender Differences in Disease
Volume 5 - 2024 | https://doi.org/10.3389/fgwh.2024.1471316
This article is part of the Research Topic Gender Inequalities, Sexual and Reproductive Health, and Sustainable Development in the Global South View all 9 articles
 Derara Girma Tufa1*†
Derara Girma Tufa1*† Habteyes Hailu Tola1
Habteyes Hailu Tola1 Hiwot Dejene Dissassa1,†
Hiwot Dejene Dissassa1,† Leta Adugna Geleta1,†
Leta Adugna Geleta1,† Erean Shigign Malka1
Erean Shigign Malka1 Addisu Waleligne Tadesse1
Addisu Waleligne Tadesse1 Feyiso Bati Wariso2
Feyiso Bati Wariso2 Getahun Fetensa3,4,5
Getahun Fetensa3,4,5
Introduction: Health-related quality of life (HRQoL) is a key outcome indicator in antiretroviral therapy program. In Ethiopia, primary studies on gender disparity in HRQoL among people living with HIV/AIDS (PLHA) are conflicting, with no pooled estimation. Therefore, this study aimed to investigate gender disparity in HRQoL among PLHA in Ethiopia.
Methods: Studies were retrieved from PubMed, Web of Science, SCOPUS, Embase, MEDLINE, Science Direct, HINARI, and PsycINFO were systematically searched. In addition, Google Scholar, Google, journal homepages, bibliographies, and universities' research repositories in the country were searched by combining keywords and Medical Subject Headings (MeSH) terms with Boolean operators. Based on the primary study results, the average score of each domain was utilized as a cut-off point to classify HRQoL as poor or good. The Joanna Briggs Institute (JBI) checklist was used to assess study quality. A random-effects model was used to report the pooled estimates. Summary estimates are presented in forest plots and tables. The variation between studies was assessed using the Higgins heterogeneity test (I2). Funnel plot, Begg's test, and Egger's test were used to assess publication bias. Data were extracted using Microsoft Excel and exported to STATA 17 (Corporation, College Station, TX, USA) for analysis. The search results were managed using the EndNote X7 software.
Results: Fifteen studies with 4,867 PLHA were included. The pooled prevalence of poor HRQoL was 46.53% (95% CI: 41.96–51.10), 46.15% (95% CI: 37.05–55.24), and 36.21% (95% CI: 30.19–42.23) among PLHA, women, and men living with HIV, respectively. Moreover, a significant gender disparity in HRQoL was observed among Ethiopian women and men living with HIV. Women living with HIV were found to have 61% increased odds of poor HRQoL than men living with HIV in the country (OR = 1.61, 95% CI: 1.07, 2.15). No statistical evidence of a publication bias was observed.
Conclusion: Almost half of PLHA patients in Ethiopia had a poor HRQoL. Women living with HIV have higher odds of poor HRQoL than men living with HIV. This highlights the pressing need for gender-specific risk assessment approaches and treatment interventions aimed at optimizing HRQoL in HIV/AIDS settings.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, identifier CRD42023454810.
Human Immunodeficiency Virus (HIV) infection remains a major global public health problem. Since its occurrence, 85.6 million [65.0–113.0] individuals have been infected, and about 40.4 million [32.9–51.3] have died. By the end of 2022, 39.0 million [33.1–45.7] individuals were living with HIV worldwide. World Health Organization (WHO) African region continues to be the most seriously affected, accounting for more than two-thirds of all people living with HIV/Acquired Immuno-deficiency Virus (AIDS) (PLHA) globally (1). Specifically, HIV is a major public concern in Ethiopia, with an estimated prevalence of 1.16% in the adult population (2).
Women are disproportionately affected by HIV/AIDS (3) accounting for 53% of all PLHA (1). Gender inequality and disparities have increased the epidemic, resulting in the violation of women's reproductive rights (4, 5). Unequal power relations, sexual coercion, and violence are common experiences for women of all ages, and they have various detrimental effects on female sexual, physical, and mental health, predisposing them to HIV infection (5). Globally, HIV/AIDS infection demonstrates the destructive repercussions of gender discrimination on human health and the socioeconomic structure of society (5).
The WHO defines quality of life (QoL) as an individual's view of their position in life within the context of the culture and value systems in which they live, as well as their goals, expectations, standards, and concerns (6). Health-related quality of life (HRQoL) refers to QoL in the context of health, disease, and treatment (7). It also denotes patient reports on functioning and well-being in the physical, mental, and social dimensions of life (8). As a result, assessing HRQoL can provide an accurate assessment of how patients' lives are affected by disease and treatment (9, 10). Besides, for those living with chronic diseases, HRQoL is an important healthcare metric (11). Subsequently, among PLHA, the poor HRQoL was often defined as a score below the average in each domain and their overall summation (12–19).
HIV is increasingly seen as a chronic disease that affects not only physical health but also the mental and social conditions of patients, due to the negative attitude of society, discrimination, and stigma, especially in developing countries (20). Evidence suggests that, in addition to underlying infection, social circumstances, relationship issues, comorbidities, and stigma affect the HRQoL of PLHA (21). Thus, HRQoL is described as one of the key factors in evaluating the health status of PLHA, and its improvement is an important treatment goal (22). In 2016, a 4th 90 target was introduced to enhance the HRQoL for PLHA by addressing comorbidities and psychosocial issues, alongside the existing triple 90 targets for clinical health monitoring. Specifically, this 4th target aims to improve the HIV care continuum in sub-Saharan Africa (SSA) by focusing on various factors to enhance HRQoL among PLHA (23).
HRQoL among PLHA is frequently assessed by the WHO Quality-of-Life Bref (QoL-HIV BREF) in six domains: physical, social relationships, level of independence, spiritual, psychological, and environmental (22, 24). The other most commonly used instruments are the Medical Outcome Survey-HIV (MOS-HIV), Short Form-36 (SF-36), European Quality-of-Life Instrument-5 Dimension (EQ-5D), Short Form-12 (SF-12), and HIV/AIDS Targeted Quality-of-Life (HAT-QOL). Furthermore, it has been shown that there is no significant variation in completion rates between the different HRQoL tools (24). Moreover, different studies have utilized below-average scores on these tools to categorize HRQoL as poor and otherwise as good status (12–15, 25).
Studies on gender disparity in HRQoL among PLHA have shown inconsistent results. Some studies have reported no disparity (16, 26, 27). However, others have suggested that there is an important gender disparity in HRQoL. Subsequently, several studies have shown that women had significantly lower scores compared to men (28–31). In contrast, a limited finding stated that women had higher HRQoL domain scores than men (32). Overall, establishing gender disparity in HRQoL can influence policies on integrating gender equality in HIV care services as an approach for improving the lives of PLHA (28).
In Ethiopia, 45.27% of PLHA had poor HRQoL (33). However, no pooled study has been conducted to identify gender disparity in HRQoL. Furthermore, different primary studies conducted in the country showed conflicting findings on the gender disparity in HRQoL (12–14, 16, 17, 25–27, 29, 31, 34). Therefore, this systematic review and meta-analysis (SRMA) aimed to estimate the pooled prevalence of poor HRQoL and gender disparity among PLHA in Ethiopia.
The protocol for this study was registered in the PROSPERO with the registration number CRD42023454810 and link https://www.crd.york.ac.uk/prospero/. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines were used to report the results of this systematic review and meta-analysis (35) (Supplementary File 1).
To conduct this SRMA, relevant articles and grey literature were searched. PubMed, Web of Science, SCOPUS, Embase, MEDLINE, Science Direct, HINARI, and PsycINFO were systematically searched. Studies were also retrieved from Google Scholar, Google, journal homepages, bibliographies, and university research repositories in the country. Keywords: “HIV”, “human immunodeficiency virus”, “acquired immunodeficiency syndrome”, “AIDS”, “HIV Infection”, “HIV positive”, “people living with HIV/AIDS”, “HIV/AIDS”, “antiretroviral therapy”, “ART”, “highly active anti-retroviral therapy”, “HAART”, “Health-related quality of life”, “Quality of Life”, “HRQOL”, “QOL”, “Ethiopia” were used in free text and MeSH terms. The search results were managed using EndNote X7 software.
This SRMA included studies conducted in Ethiopia on all adult PLHA that were accessible before November 17, 2023. Original full-text articles and studies written in English were included. Studies that did not report the prevalence of poor HRQoL and did not report on both genders were excluded.
• What is the pooled prevalence of poor HRQoL among PLHA in Ethiopia?
• Is there a gender disparity in HRQoL among PLHA in Ethiopia?
The prevalence of poor HRQoL, as determined by any of the standardized instruments used in the original studies, was considered. Based on the primary study results, the average score of each domain was utilized as a cut-off point to classify HRQoL as poor or good. Likewise, the same score was used to categorize the domains as poor or good HRQoL. Furthermore, the gender disparity in HRQoL was assessed by identifying studies reporting the association between gender and HRQoL and aggregating them using odds ratios (OR).
Data from each study were extracted by four independent authors (DGT, HDD, ESM, and AWT) in a customized format in Microsoft Excel. Inconsistencies between the authors have been resolved by other authors. The extracted data included author names, year of publication, sample size, outcome, study design, region, and settings in which the studies were conducted (Supplementary File 2).
The Joanna Briggs Institute (JBI) tools for cross-sectional and case-control studies (36) were used to assess the methodological quality and risk of bias (in design, conduct, and analysis) of the included studies (Supplementary File 3). The tools were used to evaluate the inclusion criteria, measurement of outcome variables, confounding adjustment, and appropriateness of statistical analysis. The quality of the extracted studies was evaluated by all authors who participated in data extraction.
STATA 17 (Corporation, College Station, TX, USA) was used for data analysis. The pooled prevalence of poor HRQoL was determined. To detect the gender disparity in poor HRQoL, the pooled results were presented as odds ratios (ORs) with 95% confidence intervals (CI). Heterogeneity among the included studies was checked using Cochran's Q (χ2 test) and I2 test. The heterogeneity was considered as low, moderate or high when I2 test statistics results were 25%, 50%, and 75% respectively (37). Forest plots were used to visualize heterogeneity. Because of heterogeneity, a random-effects model was used to estimate the Der Simonian and Laird's pooled effect. Subgroup and meta-regression analyses were performed to identify the sources of heterogeneity. Publication bias was assessed by using a funnel plot of symmetry. Furthermore, the statistical significance of publication bias was checked using the Egger and Begg tests (38). A p-value less than 0.05 was used to declare the presence of publication bias. Sensitivity analysis using a random-effects model was performed to assess the influence of a single study on the overall meta-analysis estimate.
Initially, 6,313 studies were retrieved by searching databases and other sources, followed by the exclusion of 1,550 studies because of duplication. Of the remaining 4,763 studies, 4,735 were removed by title and abstract screening due to different reasons including, not done in Ethiopia (3,974), unrelated population (613), not primary articles (7), and unrelated measurements (141). Then, 28 studies were eligible for the full assessment. Of these, 10 and 3 studies were removed due to unrelated purposes and did not include both genders, respectively. Finally, 15 studies that met the inclusion criteria were included in the final SRMA (Figure 1).
This SRMA included 15 original studies with a total pooled sample size of 4,867 PLHA, of which 2,857 (58.7%) were women. All studies were published articles (12–19, 25–27, 39–41), except one unpublished article (34). Furthermore, 14 studies used a cross-sectional study design (12–16, 18, 19, 25–27, 34, 39–41) and one study used a case-control study design (17). The minimum sample size was 95 (13), and the maximum was 428 (12). Six studies were conducted in the Amhara region (12, 16, 18, 34, 39, 40), five in Oromia (13–15, 17, 27), two in Benishangul-Gumuz (25, 41), one in Southwest Ethiopia (26), and one in Southern Ethiopia (19). Besides, ten studies used the WHO QOL-HIV-BREF (12–19, 34), two studies used the MOS HIV questionnaire (40, 41), one study used PROMIS-GMH (25) to measure HRQoL, and the tool was not reported in 2 studies (27, 39) (Table 1).
In the meta-analysis of 14 studies that reported on the prevalence of poor HRQoL, there was high heterogeneity (I2 = 90.1%, p-value = 0.000), and thus, a random effects model was used to analyze the results. As a result, the pooled prevalence of poor HRQoL was found to be 46.53% (95% CI: 41.96–51.10) (Figure 2). Moreover, the pooled prevalence of poor HRQoL among women and men living with HIV in Ethiopia was 44.46% (95% CI: 35.46–53.47) and 41.52% (95% CI: 29.89–53.15), respectively (Supplementary File 2).
Furthermore, the pooled estimation of the PLHA's HRQoL indicates that the domains with the highest prevalence of poor HRQoL were physical (52.19%) and environmental (50.58%). In contrast, the social relationship was identified as the domain with the highest score of good HRQoL (54.53%) (Figure 3).
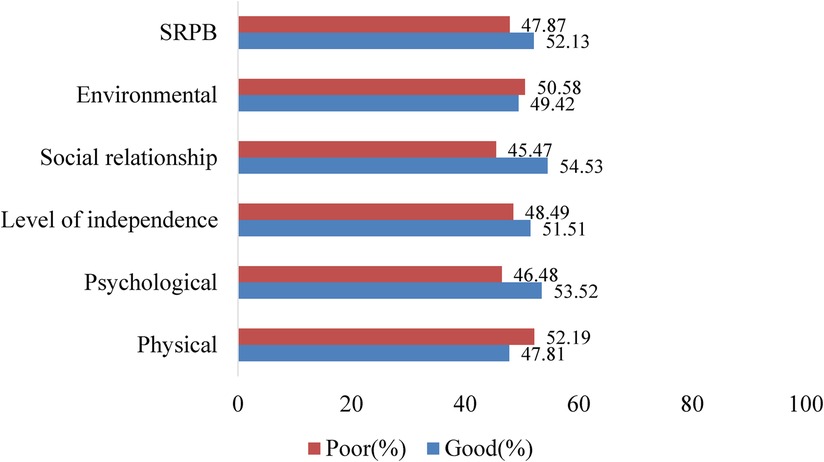
Figure 3. Pooled prevalence of the six HRQoL domains for PLHA using the wHO QOL-HIV-BREF tool in Ethiopia.
Of the included studies, nine studies (12–14, 16, 17, 25–27, 34) were reported on the association between gender and HRQoL. Subsequently, significant gender disparity was observed among Ethiopian women and men living with HIV/AIDS in HRQoL using the random-effects model (I2 = 90.9%, p-value = 0.000). Subsequently, women living with HIV were found to have 61% increased odds of poor HRQoL than men living with HIV in the country (OR = 1.61, 95% CI: 1.07, 2.15) (Figure 4).
Furthermore, the sources of heterogeneity were investigated using sub-group analysis and meta-regression techniques. The Sub-group analysis was done by regions. Accordingly, a significant heterogeneity was observed in Oromia and Amhara regions, while no significant heterogeneity was observed in other regions (South Ethiopia and Benishangul Gumz) (Supplementary File 4). Besides, meta-regression was performed considering the year of publication and the sample size of the studies. None of the variables were statistically significant for explaining the presence of heterogeneity. Accordingly, the meta-regression results revealed that heterogeneity in the gender disparity was unrelated to sample size variation (coefficient = 0.0042466, p-value = 0.166) or publication year (coefficient = 0.0631991, p-value = 0.437).
The presence of publication bias was assessed using funnel plot and Egger, and Begg statistical tests. In funnel plot, visual inspection showed that the presence of publication bias was less likely as there was relatively symmetrical study distribution of the study in the graph (Supplementary File 4). Also, there was no statistical evidence of publication bias in the pooled estimates using the Egger and Begg tests (p-value = 0.276 and p-value = 0.211), respectively.
To check the individual effect of included studies on the gender disparity in HRQoL among PLHA in Ethiopia, sensitivity analysis was done using random effect model. The findings revealed that there was no strong evidence that a single study had an impact on the pooled result of the meta-analysis, as the single study estimates were closer to the combined estimate (Supplementary File 4).
This SRMA estimated the prevalence and gender disparity in poor HRQoL among PLHA in Ethiopia. Thus, the pooled prevalence of poor HRQoL was 46.53% (95% CI: 41.96–51.10). A previous study from Ethiopia reported a comparable result (45.27%) (33). This might be due to the similarity in the study settings, populations, and the same articles included in both studies. Continued patterns of poor HRQoL among PLHA in the country highlight the need to recommend and implement the additional 4th UNAIDS target, ensuring 95% of PLHA experience the best possible HRQoL (42).
In contrast to the current study, the studies from other African countries revealed considerably a lower prevalence of poor HRQoL, 23.8% from Togo (43) and 21.6% from Botswana (7). The discrepancy in findings could be explained by differences in research designs and the age of the study participants. Age was depicted as having the inverse association with HRQoL in studies among PLHA (44–46). Furthermore, the need to investigate particular populations is stressed because sociodemographic variances can result in conclusions that contradict (47).
In this study, women living with HIV had significantly higher odds of poor HRQoL than men living with HIV. Various studies evinced this finding (30, 48). Different interpretations of the findings were postulated based on the domains of HRQoL. For instance, women appear to be more harmed in their physical HRQoL by personal rejection, experiencing social stigma from a variety of sources, including their communities, interpersonal encounters, and inside systems and organizations (49). Additionally, the stigma associated with HIV/AIDS could lower environment HRQoL among women who continued to be productive and the larger amount of performing chores (50). Women also reported more pain, less energy, and poor physical and mental health HRQoL (51). Furthermore, women living with HIV have a lower source of income, engage in less economic activities for their families, and have a greater burden in duties such as cooking and childcare than men (52). Cumulatively, insights into any of the dimensions could direct interventions used to improve HRQoL among PLHA taking into account gender disparity.
The current disparity in HRQoL is also confirmed by the studies demonstrating that HRQoL among older PLHA differs significantly by gender, implying high-priority interventions to reduce gender disparities in HRQoL and improve the structural conditions in which they live (53). Also, using the gender-specific HRQoL parameters in program development is suggested to improve the cost-effectiveness of interventions (54). Another study also revealed a considerably higher score of poor HRQoL among women living with HIV and recommends improving social and economic status and establishing a women's social network for women living with HIV (55).
In particular, primary studies conducted in different places in Ethiopia also reported significantly a higher risk of experiencing poor HRQoL among women living with HIV than men living with HIV (12, 29, 31, 52). This demonstrates that women living with HIV have consistently a higher prevalence of poor HRQoL than men living with HIV in the country. The spotted gaps in gender advocate for more gender mainstreaming in HIV service delivery in the country (28). Understanding these gender disparities can give important information for customizing interventions to improve HRQoL among PLHA.
This is the first study in Ethiopia to examine gender disparity in HRQoL among PLHA. This finding broadens current research on gender disparity in HRQoL by offering reliable evidence from a large national sample of PLHA. However, the study did have several shortcomings. The majority of the research were done in the Oromia and Amhara areas, which may not be indicative of the country as a whole. Furthermore, because of using different HRQoL measurement tools, it was not possible to pool all dimensions used in generating HRQoL. Furthermore, this study used categorical data (odds ratios), not continuous data (β-coefficients) to analyze the relationship between gender and HRQoL.
This study revealed that nearly half of PLHA in Ethiopia had poor HRQoL, showing that it is a persistent significant public health concern in this population. Moreover, a significant gender disparity in HRQoL has been observed among PLHA. Women were more likely than men to have poor HRQoL. Therefore, this highlights the pressing need for gender-specific risk assessment approaches and treatment interventions aimed at optimizing HRQoL in the HIV/AIDS setting. Moreover, the establishment of relevant measures to track progress towards improving HRQoL of PLHA should prioritize women as part of the action plan in Ethiopia. Furthermore, this finding suggests carrying out further studies to identify the key bio-psycho-social variables driving gender disparities in HRQoL among PLHA.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
DT: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. HT: Data curation, Formal Analysis, Investigation, Methodology, Resources, Software, Validation, Visualization, Writing – review & editing. HD: Data curation, Formal Analysis, Investigation, Methodology, Resources, Software, Validation, Visualization, Writing – review & editing. LG: Data curation, Formal Analysis, Investigation, Methodology, Resources, Software, Validation, Visualization, Writing – review & editing. EM: Data curation, Formal Analysis, Investigation, Methodology, Resources, Software, Validation, Visualization, Writing – review & editing. AT: Data curation, Formal Analysis, Investigation, Methodology, Resources, Software, Validation, Visualization, Writing – review & editing. FW: Data curation, Formal Analysis, Investigation, Methodology, Resources, Software, Validation, Visualization, Writing – review & editing. GF: Data curation, Formal Analysis, Investigation, Methodology, Resources, Software, Validation, Visualization, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
GF was employed by Center for Evidence-synthesis, Support, and Development in Africa (CESDA), PLC.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2024.1471316/full#supplementary-material
CI, confidence interval; HRQoL, health-related quality of life; OR, odds ratio; PLHA, people living with HIV/AIDS; SRPB, spirituality religious and personal belief; SSA, Sub-Saharan Africa, WHO, World Health Organization.
1. UNAIDS. Global HIV & AIDS statistics - Fact sheet [Internet]. 2022 (cited 2022 August 27). Available online at: https://www.unaids.org/en/resources/fact-sheet
2. Girum T, Wasie A, Worku A. Trend of HIV/AIDS for the last 26 years and predicting achievement of the 90-90-90 HIV prevention targets by 2020 in Ethiopia: a time series analysis. BMC Infect Dis. (2018) 18(1):1–10. doi: 10.1186/s12879-018-3214-6
3. The Lancet HIV. Women lead the way in the HIV response. Lancet HIV. (2024) 11(3):e131. doi: 10.1016/S2352-3018(24)00040-7
4. Wang H, Wolock TM, Carter A, Nguyen G, Kyu HH, Gakidou E, et al. Estimates of global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2015: the global burden of disease study 2015. Lancet HIV. (2016) 3(8):e361–87. doi: 10.1016/S2352-3018(16)30087-X
5. Joint United Nations Programme on HIV/AIDS. 2024 global AIDS update thematic briefing note: HIV and adolescent girls and young women. Vol. 2024. Geneva: Joint United Nations Programme on HIV/AIDS (2024). Available online at: https://aidsinfo.unaids.org/ (accessed November 10, 2024).
6. Harper A, Power M, Orley J, Herrman H, Schofield H, Murphy B, et al. Development of the world health organization WHOQOL-BREF quality of life assessment. Psychol Med. (1998) 28(3):551–8. doi: 10.1017/S0033291798006667
7. Karugaba G, Thupayagale- Tshweneagae G, Moleki MM, Mabikwa OV, Matshaba M. Determinants of health-related quality of life in young adults living with perinatally acquired HIV infection in Botswana. South Afr J HIV Med. (2022) 23(1):1–10. doi: 10.4102/sajhivmed.v23i1.1362
8. Kaplan RM, Hays RD. Health-related quality of life measurement in public health. Annu Rev Public Health. (2022) 43:355–73. doi: 10.1146/annurev-publhealth-052120-012811
9. Préau M, Mora M, Puppo C, Laguette V, Sagaon-Teyssier L, Boufassa F, et al. Does quality of life and sexual quality of life in HIV patients differ between non-treated HIV controllers and treated patients in the French ANRS VESPA 2 national survey? AIDS Behav. (2019) 23(1):132–9. doi: 10.1007/s10461-018-2237-8
10. Syed IA, Syed Sulaiman SA, Hassali MA, Lee CKC. Assessing HIV and AIDS treatment safety and health-related quality of life among cohort of Malaysian patients: a discussion on methodological approach. Heal Expect. (2015) 18(5):1363–70. doi: 10.1111/hex.12116
11. Wu AW, Hays RD, Kelly S, Malitz F, Bozzette SA. Applications of the medical outcomes study health-related quality of life measures in HIV/AIDS. Qual Life Res. (1997) 6(6):531–54. doi: 10.1023/A:1018460132567
12. Koster Y, Taddele M, Aderaw Z, Tefera KT. Health-related quality of life and associated factors among HIV-positive individuals on antiretroviral therapy at Debre Markos referral hospital, northwest Ethiopia. HIV AIDS Rev. (2022) 21(3):239–49. doi: 10.5114/hivar.2022.117281
13. Zeleke Negera G, Ayele Mega T. Health-related quality of life among admitted HIV/AIDS patients in selected Ethiopian tertiary care settings: a cross-sectional study. Open Public Health J. (2020) 12(1):532–40. doi: 10.2174/1874944501912010532
14. Gesese AA, Desta YG, Behire EZ. Behavioral and psychosocial factors of quality of life among adult people living with HIV on highly active antiretroviral therapy, in public hospitals of southwest Ethiopia. PLOS Glob Public Health. (2022) 2(8):e0000822. doi: 10.1371/journal.pgph.0000822
15. Dinsa Ayeno H, Megersa Atomsa K, Melesie Taye G, Ayeno HD, Atomsa KM, Taye GM. Assessment of health-related quality of life and associated factors among HIV/AIDS patients on highly active antiretroviral therapy (Haart) at Ambo general hospital, West Shewa, Ethiopia. HIV AIDS (Auckl). (2020) 12:467–78. doi: 10.2147/HIV.S259510
16. Ayalew MB, Abdela OA, Solomon A, Adugna D, Siraj N, Yesuf JS, et al. Quality of life of HIV patients taking antiretroviral treatment in a resource limited setting: a case of University of Gondar comprehensive specialized hospital, Ethiopia. J Basic Clin Pharm. (2018) 9:302–7.
17. Gesese AA. Predictors of poor quality of life among people living with HIV/AIDS on antiretroviral therapy in Jimma zone public hospitals, south west Ethiopia: a mixed-method study. J Psychol Psychother. (2021) 11:1–9.
18. Surur AS, Teni FS, Wale W, Ayalew Y, Tesfaye B. Health related quality of life of HIV/AIDS patients on highly active anti-retroviral therapy at a university referral hospital in Ethiopia. BMC Health Serv Res. (2017) 17(1):1–8. doi: 10.1186/s12913-017-2714-1
19. Tesemma AL, Abate MG, Abebo ZH, Madebo WE. Determinants of poor quality of life among adults living with HIV and enrolled in highly active anti-retroviral therapy at public health facilities of Arba Minch town administration in southern Ethiopia. HIV AIDS (Auckl). (2019) 11:387–94. doi: 10.2147/HIV.S227244
20. Li X, Lin C, Gao Z, Stanton B, Fang X, Yin Q, et al. HIV/AIDS knowledge and the implications for health promotion programs among Chinese college students: geographic, gender and age differences. Health Promot Int. (2004) 19(3):345–56. doi: 10.1093/heapro/dah308
21. Drewes J, Gusy B, Von Rüden U. More than 20 years of research into the quality of life of people with HIV and AIDS—a descriptive review of study characteristics and methodological approaches of published empirical studies. J Int Assoc Provid AIDS Care. (2013) 12(1):18–22. doi: 10.1177/1545109712456429
22. World Health Organization. Scoring and coding for the WHOQOL-HIV instruments. WHOQOL-HIV Instrument Users Manual. Geneva: World Health Organization (2002). Available online at: http://www.who.int/msa/qol (accessed December 06, 2017).
23. Mvilongo PTN, Vanhamel J, Siegel M, Nöstlinger C. The “4th 90” target as a strategy to improve health-related quality of life of people living with HIV in Sub-Saharan Africa. Trop Med Int Health. (2022) 27(12):1026–43. doi: 10.1111/tmi.13825
24. Zhang Y, He C, Peasgood T, Hulse ESG, Fairley CK, Brown G, et al. Use of quality-of-life instruments for people living with HIV: a global systematic review and meta-analysis. J Int AIDS Soc. (2022) 25(4):1–9. doi: 10.1002/jia2.25902
25. Nigusso FT, Mavhandu-Mudzusi AH. Health-related quality of life of people living with HIV/AIDS: the role of social inequalities and disease-related factors. Health Qual Life Outcomes. (2021) 19(1):1–11. doi: 10.1186/s12955-021-01702-2
26. Desta A, Biru TT, Kefale AT. Health related quality of life of people receiving highly active antiretroviral therapy in southwest Ethiopia. PLoS One. (2020) 15:1–14. doi: 10.1371/journal.pone.0237013
27. Tesfaye T, Darega J, Belachew T, Abera A. Health-Related quality of life and associated factors among people living with HIV/AIDS following ART clinic in Jimma University specialized hospital, southwest Ethiopia: a facility- based cross-sectional study. Open Public Health J. (2019) 11(1):572–83. doi: 10.2174/1874944501811010572
28. Ogaji DS, Igwebuike OP. Cross-sectional investigation of gender differences in health-related quality of life among HIV patients: implications for gender mainstreaming in HIV management. Pan Afr Med J. (2021) 39:1–16. doi: 10.11604/pamj.2021.39.201.24420
29. Gebremichael DY, Hadush KT, Kebede EM, Zegeye RT. Gender difference in health related quality of life and associated factors among people living with HIV/AIDS attending anti-retroviral therapy at public health facilities, western Ethiopia: comparative cross sectional study. BMC Public Health. (2018) 18(1):1–11. doi: 10.1186/s12889-018-5474-x
30. Briongos Figuero LS, Bachiller Luque P, Palacios Martín T, González Sagrado M, Eiros Bouza JM. Assessment of factors influencing health-related quality of life in HIV-infected patients. HIV Med. (2011) 12(1):22–30. doi: 10.1111/j.1468-1293.2010.00844.x
31. Tesfay A, Gebremariam A, Gerbaba M, Abrha H. Gender differences in health related quality of life among people living with HIV on highly active antiretroviral therapy in Mekelle town, northern Ethiopia. Biomed Res Int. (2015) 2015:1–9. doi: 10.1155/2015/516369
32. Joulaei H, Mousavi SG, Foroozanfar Z, Rakhshani T. Health-related quality of life in people living with HIV in southwest Iran in 2018: a cross-sectional study. Biomed Res Int. (2021) 2021:1–8. doi: 10.1155/2021/9935175
33. Mengistu N, Hareru HE, Shumye S, Yimer S, Sisay D, Kaso AW, et al. Health related quality of life and its association with social support among people living with HIV/AIDS receiving antiretroviral therapy in Ethiopia: a systematic review and meta-analysis. Health Qual Life Outcomes. (2022) 20(1):1–8. doi: 10.1186/s12955-022-01985-z
34. Demessie A, Wassie B, Admassu M. Assessment of Health Realted Quality of Life and Associated Factors among People Living with HIV/AIDS in South Wollo Zone, North East Ethiopia, 2011. Gondar City: University of Gondar (2011). Available online at: http://repository.iifphc.org/handle/123456789/1165
35. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71. doi: 10.1136/bmj.n71
36. JBI. Available online at: Https://Jbi.Global/Critical-Appraisal-Tools. 2024 (cited 2024 January 8). JBI Critical Appraisal Tools. Available online at: https://jbi.global/critical-appraisal-tools
37. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
38. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 50(4):1088–101. doi: 10.2307/2533446
39. Alemu A, Yenealem A, Feleke A, Meseret S. Health related quality of life assessment and associated factors among people on highly active antiretroviral therapy at Felege Hiwot referral hospital, Bahir Dar, north west Ethiopia. J AIDS Clin Res. (2014) 5(1):1–5. doi: 10.4172/2155-6113.1000272
40. Mohammed SA, Yitafr MG, Workneh BD, Hailu AD. Health-related quality of life and associated factors among people living with human immunodeficiency virus on highly active antiretroviral therapy in north east Ethiopia: cross-sectional study. PLoS One. (2021) 16:1–14. doi: 10.1371/journal.pone.0247777
41. Jaleta Wondasho P, Adimasu M. Health related quality of life and associated factors among HIV patient on highly active antiretroviral therapy at Assosa hospital, northwest Ethiopia, 2019. Am J Clin Exp Med. (2021) 9(4):102. doi: 10.11648/j.ajcem.20210904.13
42. Moyo RC, Sigwadhi LN, Carries S, Mkhwanazi Z, Bhana A, Bruno D, et al. Health-related quality of life among people living with HIV in the era of universal test and treat: results from a cross-sectional study in KwaZulu-Natal, South Africa. HIV Res Clin Pract. (2023) 25(1):1–10. doi: 10.1080/25787489.2023.2298094
43. Yaya I, Djalogue L, Patassi AA, Landoh DE, Assindo A, Nambiema A, et al. Health-related quality of life among people living with HIV/AIDS in Togo: individuals and contextual effects. BMC Res Notes. (2019) 12(1):1–6. doi: 10.1186/s13104-018-4038-6
44. Girma D, Dejene H, Geleta LA, Tesema M, Legesse E, Nigussie T, et al. Health related quality of life of HIV-positive women on ART follow-up in North Shewa zone public hospitals, central Ethiopia: evidence from a cross-sectional study. Heliyon. (2023) 9(2):e13318. doi: 10.1016/j.heliyon.2023.e13318
45. Kteily-Hawa R, Andany N, Wang Y, Logie CH, Tharao W, Conway T, et al. Quality of life of older women living with HIV: comparative assessment of physical and mental health-related markers using a large Canadian sexual and reproductive health cohort study. HIV Res Clin Pract. (2019) 20(2):35–47. doi: 10.1080/15284336.2018.1554373
46. Arjun BY, Unnikrishnan B, Ramapuram JT, Thapar R, Mithra P, Kumar N, et al. Factors influencing quality of life among people living with HIV in coastal south India. J Int Assoc Provid AIDS Care. (2017) 16(3):247–53. doi: 10.1177/2325957415599213
47. Lufiande J, Silva S, Reis AC, Guerra MP. Predictors of quality of life in HIV-infected persons from Mozambique: the dual role of schooling. Infect Dis Rep. (2023) 15(4):392–402. doi: 10.3390/idr15040040
48. Mrus JM, Williams PL, Tsevat J, Cohn SE, Wu AW. Gender differences in health-related quality of life in patients with HIV/AIDS. Qual Life Res. (2005) 14(2):479–91. doi: 10.1007/s11136-004-4693-z
49. Rice WS, Logie CH, Napoles TM, Walcott M, Batchelder AW, Kempf MC, et al. Perceptions of intersectional stigma among diverse women living with HIV in the United States. Soc Sci Med. (2018) 208(5):9–17. doi: 10.1016/j.socscimed.2018.05.001
50. Tran BX, Ohinmaa A, Nguyen LT, Oosterhoff P, Vu PX, Van VT, et al. Gender differences in quality of life outcomes of HIV/AIDS treatment in the latent feminization of HIV epidemics in Vietnam. AIDS Care. (2012) 24(10):1187–96. doi: 10.1080/09540121.2012.658752
51. Fumaz CR, Larrañaga-Eguilegor M, Mayordomo-López S, Gómez-Martínez S, González-García M, Ornellas A, et al. Health-related quality of life of people living with HIV infection in Spain: a gender perspective. AIDS Care. (2019) 31(12):1509–17. doi: 10.1080/09540121.2019.1597959
52. Tegegne AS. Quality of life and associated factors of HIV patients under treatment with first line regimens in public hospitals in Amhara region, north-west Ethiopia. Patient Prefer Adherence. (2023) 17:1347–59. doi: 10.2147/PPA.S413192
53. Nuño N, Martínez A, Martínez S, Cobos M, Hernández JS, Polo R. Sex differences in health-related quality of life and poverty risk among older people living with HIV in Spain: a cross-sectional study. PLoS One. (2024) 19(5):1–15. doi: 10.1371/journal.pone.0301335
54. Nuño N, Martínez A, Martínez S, Cobos M, Hernández JS, Polo R. Factors influencing the health-related quality of life of older men and women living with HIV in Spain. AIDS Care. (2024) 19:1–15. doi: 10.1080/09540121.2024.2361815
Keywords: health-related quality of life, gender disparity, HIV/AIDS, meta-analysis, Ethiopia
Citation: Tufa DG, Tola HH, Dissassa HD, Geleta LA, Malka ES, Tadesse AW, Wariso FB and Fetensa G (2024) Gender disparity in health-related quality of life among people living with HIV/AIDS in Ethiopia: a systematic review and meta-analysis. Front. Glob. Womens Health 5:1471316. doi: 10.3389/fgwh.2024.1471316
Received: 27 July 2024; Accepted: 4 November 2024;
Published: 20 November 2024.
Edited by:
Tizta Degfie, Bahir Dar University, EthiopiaReviewed by:
Venkataramana Kandi, Prathima Institute of Medical Sciences, IndiaCopyright: © 2024 Tufa, Tola, Dissassa, Geleta, Malka, Tadesse, Wariso and Fetensa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Derara Girma Tufa, ZGVyYXJhZ2lybWEyNEBnbWFpbC5jb20=
†ORCID:
Derara Girma Tufa
orcid.org/0000-0002-4905-1189
Hiwot Dejene Dissassa
orcid.org/0000-0002-5110-4075
Leta Adugna Geleta
orcid.org/0000-0002-7099-0420
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.