- 1Dalla Lana School of Public Health, University of Toronto, Toronto, ON, Canada
- 2Social and Behavioural Health Sciences Division, Dalla Lana School of Public Health, University of Toronto, Toronto, ON, Canada
Persistent staffing shortages in health care driven by years of inadequate funding and deficiencies in human resources planning, which overlooked the impacts of population aging, have converged into a crisis in health care settings. An essential consequence of the widespread and growing staffing shortfalls in health care has been increased pressure on nurses to work longer hours. The present rapid review has two major objectives: (1) to systematically review and synthesize evidence considering the health and human consequences of excessive work hours, work-related fatigue and associated occupational health and safety hazards; and, (2) to identify policies and practices that demonstrate efficacy in managing or mitigating the adverse effects of occupational fatigue. Findings show that shifts lasting longer than 12 h elevate the risk of occupational fatigue, leading to several fatigue-based hazards. Despite governmental restrictions on long work hours and occupational fatigue in safety-critical industries such as transport, aviation, and nuclear sectors, health care remains largely unregulated in this regard. Ensuring safe and high-quality care over the long term requires implementing adequate regulatory supports for work hour limits for nurses. These measures not only improve workplace satisfaction but also enhance patient outcomes, ultimately fostering a healthier and more resilient health care system.
1 Introduction
Nurses in Canada are increasingly grappling with significant and mounting challenges in delivering high-quality patient care. Years of inadequate health care funding, compounded by numerous failures in human resources planning that overlooked the impacts of population aging, have coalesced into a crisis in health care settings and nursing working conditions. A persistent driver of this crisis has been chronic staffing shortages, resulting in extended work hours, unsustainable increases in workload, toxic work environments, and clinical burnout (1). The onset of the COVID-19 pandemic exacerbated these pre-existing challenges in health care settings. Since 2020, the first year of the pandemic, there has been a notable rise in the proportion of nurses choosing to change jobs or leave the profession altogether. Many of those who have switched jobs opted to work for private agencies, which raises serious concerns about the long-term viability of the public health care system (2).
Nursing remains a predominantly female profession; at present, approximately nine in ten regulated nurses in Canada are women. A survey undertaken by the Canadian Federation of Nurses Unions in February 2022 found that more than half (53%) of nurses were considering leaving their current position within the coming year. Reasons cited for leaving included burnout, stress, and poor working conditions due to insufficient staffing levels (3). The shortage of nurses has become a major concern for health care systems across Canada, with many hospitals and long-term care facilities struggling to maintain adequate staffing levels. Data from Statistics Canada show that, between 2018 and 2023, job vacancies in nursing increased nearly three-fold from 10,910 to 30,790, indicating that staffing deficiencies will be very difficult to remedy in the near-term (4).
An essential consequence of the widespread and growing staffing shortages in health care is the increased pressure on nurses to work longer hours. Whether explicit through mandatory overtime or implicit through expectations from health care authorities and employers, there is a pervasive belief that nurses should fill staffing gaps by working additional shifts and extended hours. Scheduled shifts can extend up to 16 h and often deviate from the traditional day, evening, and night shift patterns. For instance, while typical 12 -hour shifts might traditionally run from 7:00 a.m. to 7:00 p.m., nurses may now be required to work shifts starting at 3:00 p.m. and ending at 3:00 a.m., depending on specific staffing needs within their unit (5). This variability can significantly impact nurses’ work-life balance and contribute to fatigue and burnout, highlighting the urgent need for effective staffing solutions and supportive work environments in health care settings (5). Nurses working in specialized units such as surgery, dialysis, or intensive care often face the expectation of being available for extra shifts beyond their regular schedules. In settings like emergency rooms, where staffing shortages are particularly severe, 24 h shifts are increasingly common (6). These scheduling practices persist despite evidence indicating that prolonged wakeful periods of 24 h or more can significantly impair cognitive and physical response times, akin to exceeding the legal blood alcohol limit for operating a motor vehicle (7). Extended hours and overwork in nursing, driven by inadequate staffing, are linked to a higher incidence of medical errors and elevated rates of patient morbidity and mortality (7–9). Excessive work hours and fatigue also heighten the risk of workplace accidents and injuries among nurses (10, 11). Furthermore, research also indicates that nurses are at increased risk of motor vehicle accidents due to drowsy driving after their shifts (12).
Despite the increasing evidence highlighting the risks of excessive work hours and occupational fatigue, the health care industry continues to rely on demanding longer hours from a shrinking pool of nurses. The lack of regulation of work hours in nursing starkly contrasts with other safety-sensitive industries like trucking, rail and nuclear where legislative standards strictly enforce work hour limits. This discrepancy raises concerns about an underlying gender-bias in the regulatory regime that must be addressed.
The present rapid review has two objectives: (1) to compile and synthesize evidence examining the health and human consequences of excessive work hours, work-related fatigue and associated occupational health and safety hazards, for the purpose of identifying safety limits for work hours; and, (2) to identify policies and practices that demonstrate efficacy in managing or mitigating the adverse effects of occupational fatigue. Rapid reviews offer a streamlined approach to synthesizing research evidence in a timely manner to deliver concise and relevant information to key decision-makers. The current review was undertaken on behalf of the Canadian Federation of Nurses Unions (CFNU) in an urgent response to the retention crisis among front-line nurses within the public health care sector.
The review proceeds in two main sections. The first is an overview of evidence on the individual and work-related impacts of excessive work hours, work-related fatigue and fatigue-based impairment, aiming to inform safety limits on work hours in nursing and the health care sector. The second section provides a summary of polices, practices and regulations related to work hours safety within safety-sensitive industries outside of health care within Canada and select peer countries (US, EU) to identify best practices.
2 Research evidence on the health and safety outcomes of long work hours and occupational fatigue
2.1 Method
A rapid review of the peer-reviewed literature on work hours safety was conducted across multiple scientific databases, including: CINAHL, Embase, ProQuest Health, Safety Science Abstracts, Medline, PubMed, Scopus, Web of Science, JSTOR, ScienceDirect, ProQuest, Directory of Open Access Journals, PLOS, and Google Scholar. Because a majority of the research on occupational fatigue safety limits in work hours has been undertaken outside of nursing and health care, topical studies across all industries and work contexts were considered. The search was structured based on the target population (workers in safety-sensitive industries and/or industries operating on a 24 h schedule), the determinant (long or excessive work hours), and the outcome (health and safety consequences of occupational fatigue). Focal keywords for the target population included: safety-sensitive industries [/transportation/trucking/rail/aviation/nuclear/health care], 24/7 operations [/manufacturing]. Key search terms for the determinant included: long [extended/excessive] work hours [/schedule], shift work, [occupational/work-related] fatigue, sleep [deprivation/deficit]. Search terms for outcomes included: occupational health [/and safety], worker health, work culture, organizational outcomes [/effects]. The search period covered approximately three decades, beginning in 1990, during which there was a significant increase in research activity on occupational fatigue, including several seminal studies on the topic. This timeframe also coincides with the implementation of regulatory limits on work hours established by the European Working Time Directive, which took effect in 1993. Some articles were identified during a search for specific authors considered experts within this domain of knowledge. Others were identified through citations and bibliographies of previously accessed professional/trade literature. Since a key objective of this review is to quantify the effects of excessive work hours to identify safe work hour limits, only quantitative research articles were considered. A sample search strategy is given in Table 1.
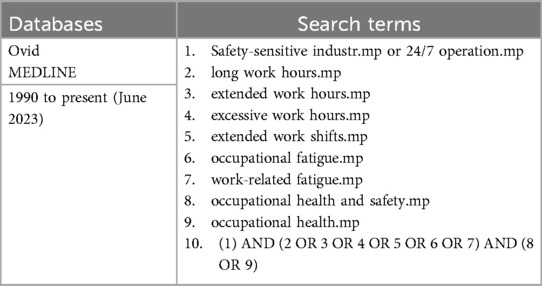
Table 1. Sample search strategy for a rapid review of the literature on the occupational health and safety effects of long work hours and work-related fatigue.
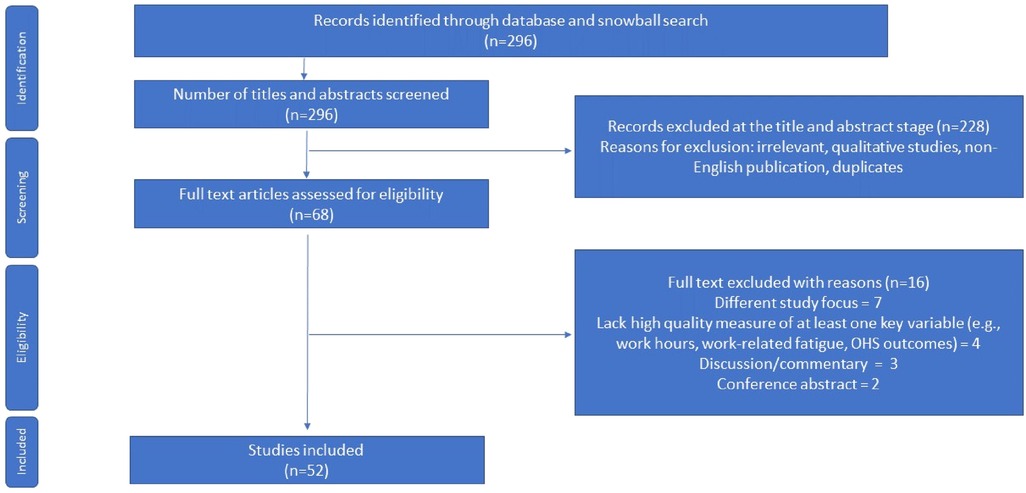
The initial search, completed in June 2023, yielded 296 articles. Adjudication of articles for inclusion in the review was informed by the a modified version of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) for rapid reviews (13). Use of this framework allows for a coherent synthesis of knowledge based on a targeted research question coupled with search strategies that make it easier to identify relevant papers. In accordance with the requirements of a rapid review, however, components of the systematic review process were simplified or omitted to produce an evidence base in a timely manner (14). Figure 1 outlines the inclusion/exclusion criteria. In all, 52 studies were deemed both relevant and of sufficiently high quality for inclusion in the main review.
The identified studies fell into two categories. First, the human factors literature examines the etiology of human fatigue rooted in neurophysiological processes, including circadian function and the homeostatic drive for sleep. These studies provide a foundation for understanding how work hours are limited by human biology. The second category is epidemiological research on the occupational health and safety effects of excessive work hours and work-related fatigue within specific work contexts, with a focus on safety-sensitive industries, including health care. These studies consider the effects of real-world factors on fatigue-based risk in situ, with implications for occupational safety outcomes at the individual and organizational levels. An overview of the selected studies and the extracted evidence by category (author, year of publication, country, outcome variable, method, relevant findings) is provided in Table 2.
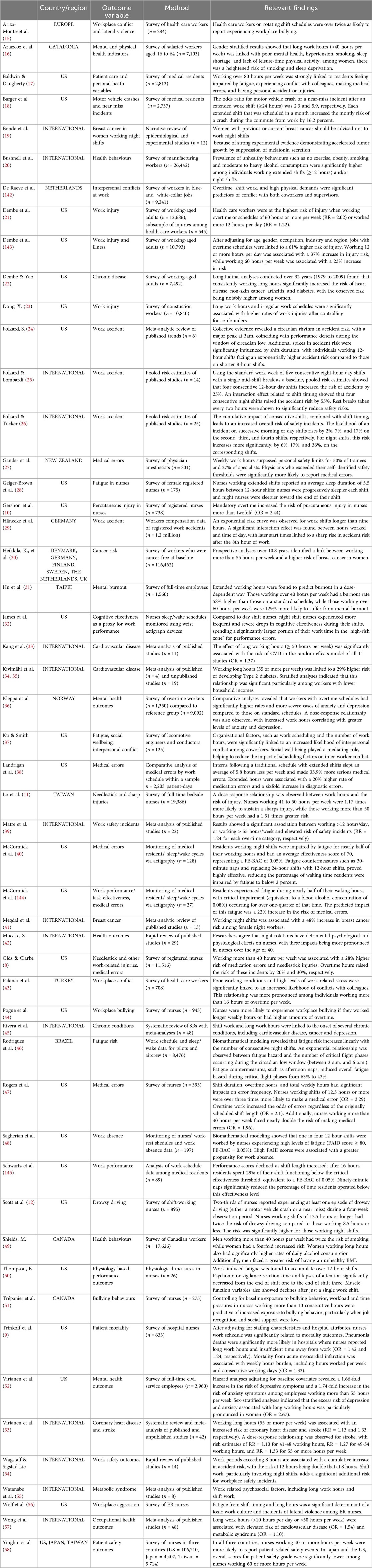
Table 2. Overview of selected studies on occupational health and safety outcomes of long work hours.
2.2 Human factors research on the etiology of occupational fatigue
Human factors research is a broad multidisciplinary field that focuses on understanding and optimizing the interaction between humans and aspects of their environment. With respect to work and workplace settings, the goal is to develop work systems that enhance human well-being, performance and satisfaction while minimizing errors, accidents, and adverse effects (59).
A key area of human factors research is understanding how to minimize the onset and consequences of work-related fatigue. Broadly, fatigue at work arises from an imbalance between the intensity, duration, and timing of work, coupled with an insufficient allotment of time for recovery (60). In real-life work environments, this imbalance is linked to poor scheduling practices that require workers to stay on task for extended periods without sufficient rest-breaks either during or between shifts, and is compounded by high-intensity workloads. From an occupational standpoint, fatigue is commonly described as an individualized experience of lack of energy or tiredness with physical, cognitive and/or psychological manifestations (48). Work-related fatigue is a significant workplace hazard since it leads to diminished cognitive and physical acuity, which raises the risk of safety incidences on the job (25, 61–63). While there are different dimensions of fatigue (e.g., muscular, mental, psychomotor), human factors studies primarily focus on fatigue related to the “drive to sleep,” which stems from the neurobiological processes regulating sleep and circadian rhythm (64). Sleep is essential to recovery after prolonged work-related activity. Its functional benefits include restoration and repair of both physical and cognitive systems, conserving energy, and strengthening the immune system. In the short term, sleep deprivation leads to reduced attention, slower reaction times, impaired memory consolidation, and diminished emotional regulation (65). Over the long term, accumulating sleep deficits are linked to declines in physical and mental health, contributing chronic conditions such as cardiovascular disease, diabetes, and depression (66, 67).
Bio-mathematical models of fatigue (BMMF) have been used to isolate the basic human factors that give rise to fatigue among workers across a range of settings. The models are designed around assumptions regarding the interaction of basic neurobiological functions, namely homeostatic drive for sleep and processes of circadian regulation (61). Drawing on information related to work-rest patterns, BMMF constitute predictive tools with respect to the level of fatigue associated with different work schedules, and are able to quantify the inferred risk on performance and safety outcomes arising from fatigue (60).
Several studies have used BMMF to evaluate the degree of “hazard exposure” associated with work-related fatigue. These studies quantify the relative risk arising from fatigue across a range of work practices and industry settings. Within health care, studies have used bio-mathematical modeling to examine the association between long hours, fatigue and fatigue-related risks (e.g., medical errors). Sagherian et al. (48) used FAID (Fatigue Audit Inter Dyne) to estimate fatigue in pediatric nurses. FAID scales are calibrated such that a fatigue score of 40 represents a standard work schedule of 40 h per week, Monday to Friday 9:00 a.m. to 5:00 p.m. Scores of 80 to 100 represent work-related fatigue arising from 23 to 24 h of continuous sleep deprivation; scores higher than 120 represent a permanent night shift schedule of six consecutive 12 h night shifts, with one day off between shifts. Nurses working 12 h shifts generated FAID scores of seven to 154 with nearly one in four (23%) shifts worked by nurses experiencing very high levels of fatigue [i.e., FAID scores of 80 or more indicating a Fatigue Equivalent BAC (FE-BAC) of 0.05%]. James et al. (32) used another BMMF approach known as SAFTE (Sleep Activity Fatigue Task Effectiveness) to analyze nurses’ sleep/wake schedules. Significant differences in cognitive effectiveness between shift-type were found with night shift nurses exhibiting frequent substantial declines into the “high risk” zone throughout their shifts (32).
Schwartz et al. (145) examined the effects of duty-hours on performance in surgical residents using SAFTE software to predict fatigue risk and performance outcomes. Performance scores decreased with increased shift length; after 16 h, residents spent over one-fourth of their shift (29%) below the “critical effectiveness threshold” (FE-BAC = 0.05%). Additional analyses found that naps lasting 90 min significantly reduced the predicted percentage of time residents spent below the critical threshold. Similar studies study by McCormick et al. (40, 144) found that medical residents experience fatigue nearly half (48%) of their waking hours, with their fatigue levels reaching the “impaired” threshold (FE-BAC of 0.08%) 27% of the time (144). Fatigue in residents was associated with a 22% increased risk of medical errors. Additionally, residents working night shifts were more fatigued and faced a greater risk of medical errors compared to those on day shifts. Fatigue countermeasures such as 30 min naps and substituting 24 h shifts with 12 h shifts were found to be highly effective, reducing the percentage of waking time residents were impaired by fatigue to below 2 percent (40). Other studies have demonstrated the risk-mitigating effects of limiting the number of critical work tasks performed during the window of circadian low (WOCL), which occurs between about 2 a.m. and 6 a.m. (46).
2.3 Epidemiological studies on the health and safety risks of long work hours
A substantial body of epidemiological evidence demonstrates the risks associated with long work hours across various work contexts. In general, these studies are concerned with fatigue resulting from sleep deprivation caused by work scheduling factors, such as overtime and extended shifts lasting more than eight hours. Studies tend to focus on the impacts of occupational fatigue within safety-critical industries such as aviation, transportation, heavy manufacturing and health care. Focal outcomes generally fall into three categories: (1) the risk of workplace safety incidents (i.e., accidents, including errors, or injuries); (2) the risk of workplace conflict and lateral violence; and (3) risks to individual health and wellbeing.
2.3.1 Long hours and the risk of workplace safety incidents
The elevated risk of a workplace safety incident can result from a combination of total successive work hours coupled with shift timing. Several high-profile industrial disasters have been partly attributed to occupational fatigue from long nighttime hours, including the Exxon Valdez oil spill disaster, the Challenger Space Shuttle explosion, and system failures at Three Mile Island and Chernobyl (68–70). In health care, Canadian data show that one in 17 hospital stays involved at least one harmful event (71). A portion of iatrogenic incidents may be due to work hours and fatigue among health care providers (72).
Research on the impact of prolonged work hours and the timing of work has quantified the effects of fatigue and associated workplace risks. A notable early study by Folkard (24) examined the effects of shift timing and duration on the risk of accident in transport operations. Sleep propensity data identified peak accident risk occurs at 3am due to lower performance during the window of circadian low. Time-on-task was also a significant factor with shifts lasting 12 h or more at twice the accident risk of 8 h shifts (24). Other studies have reported similar findings with respect to the exponential risk of accident beyond the 9th hour of work. Using a sample of 1.2 million registered workplace accidents, Hänecke et al. (29) reported a significant interaction between hour at work and time of day with later start times predictive of a drastic increase in accident risk beyond the eighth hour at work (29).
A prospective study drawing on a large representative panel of US workers found that the odds of injury after 12 h of work nearly doubled, while shifts lasting longer than 16 h produced a hazard rate of 3.5. Workweeks of ≥50 h nearly doubled the risk of workplace accident (OR = 1.98) (23). In another analysis of the same panel, Dembe et al. (143) observed that, after controlling for factors like age, gender, occupation, industry and region, jobs involving overtime schedules were associated with a 61% higher injury risk. Furthermore, working 12 or more hours per day was increased injury risk by 37%, while working 60 h per week elevated the risk by 23% (143). Another study involving health care professionals demonstrated a clear dose-response relationship between weekly work hours and risk of injury. No additional risk was found to be associated with extended shifts lasting 12 h. The authors concluded that the most potent source of fatigue in health care workers arises from accumulated hours over the course of a week, rather than from occasional 12 h shifts worked a few days each week (21).
Folkard and Lombardi (25) employed an advanced analytic approach to investigating the risk of long work hours by pooling data across several studies (25). Pooled risk estimates were used to construct a “Risk Index” based on different combinations of aspects of work scheduling—i.e., shift duration, number of successive shifts, shift timing, intervals between breaks. Using the “normal work week” comprised of five successive eight-hour day shifts with a single mid-shift break as a baseline, the study found that four successive 12 h day shifts increased accident risk by 25%. There was an interaction effect for shift-timing with four successive night shifts increasing accident risk by 55%. The authors concluded that work schedules should follow the general guideline that for any given workweek, a long span of short shifts tends to be safer than a short span of long shifts (e.g., six eight-hour shifts vs. four consecutive 12 h shifts). Furthermore, properly timed rest breaks—ideally every two-hours—can significantly reduce safety risk (Figure 2).
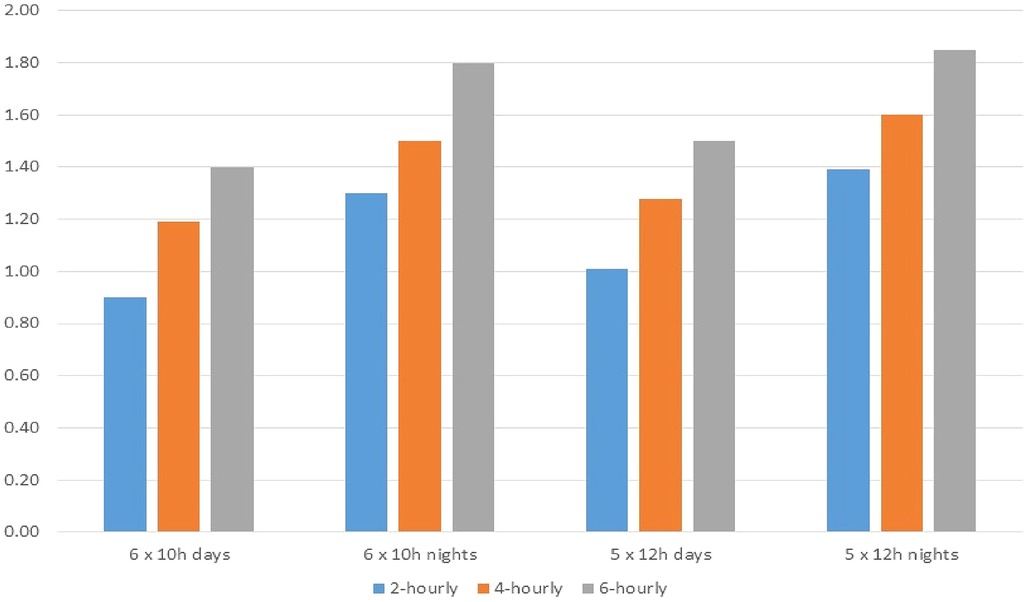
Figure 2. Risk of accident by type of work shift including rest breaks. Source: Folkard & Lombardi (25).
Folkard and Tucker (26) reported similar findings regarding the cumulative effects of multiple shifts and shift timing showing that, on average, the risk of incident on successive morning/day shifts is 2%, 7% and 17% higher for the second, third and fourth work shift respectively, whereas for night shifts the respective risk is elevated to 6%, 17% and 36% (26). Furthermore, at least two systematic reviews provide strong evidence of the cumulative safety risk associated with long work hours. The risk of safety incident for shifts lasting 12 h can be as high as twice that of shifts lasting eight hours (39, 54). Among nurses, Thompson (50) has shown that extended 12 h work shifts lasting 12 h were linked to reduced muscle strength, slower reaction time and decreased attention. Additionally, both reaction time and attention continued to deteriorate over successive work shifts (50).
Other studies have confirmed the relationship between long work hours and safety risk with respect to the commission of medical errors. Gander, Merry, Millar, & Weller (27) has reported that physicians who exceed self-defined safety limits for consecutive work hours were significantly more likely to report medical errors (27). Landrigan et al. (38) used a prospective, randomized design to investigate the impact of long hours on medical interns in critical care units. Interns following a traditional schedule with extended shifts slept an average of 5.8 h less per week and made serious medical errors 35.9% often compared to the intervention group, which eliminated extended shifts and reduced weekly work hours. Additionally, extended hours were linked with a 20% higher rate of medication errors and a six fold increase in serious diagnostic errors (38). Rogers et al. (47) investigated nursing care outcomes in relation to work hours and shift timing. Shift duration and number of hours worked per week had a significant effect on error frequency. Shifts of 12.5 h or more were associated with an error rate more than times that of eight-hour shifts. Overtime hours were predictive of a two-fold increase in the odds of making at least one error. Dose-response between work hours and incident risk was reported with shifts of 8 h, 8–12 h and 12 h increasing error risk by 34%, 53% and 326%, respectively. Nurses working more than 40 h per week were at nearly twice the risk of patient errors and at almost 50% higher risk of near errors (47). Another study of the effects of extended work hours on critical care nurses reported similar findings with shifts lasting 12.5 predictive of nearly twice the probability of medical error occurrence (7). The probability of near errors also increased significantly during extended shifts. Nurses working more than 40 h per week were at significantly higher risk of both errors and near errors (46% and 93%, respectively). At least one study has directly linked long work hours in nurses with mortality outcomes in patients (9). Adjusting for staffing (e.g., levels and skill mix) and hospital characteristics, work schedule was found to be significantly associated with mortality outcomes. Deaths from pneumonia were 42% more likely in hospitals where nurses worked extended hours and lacked time away from work. Mortality from acute myocardial infarction was significantly associated with weekly work hours burden. A review by Muecke (42) examining 10-years of scientific literature on the effects of rotating night shifts in nurses reported evidence of a relationship between extended shifts, inferior levels of alertness and performance, failures in attending to changes in patient condition, medication errors, and patient mortality (42).
Research has shown that nurses working extended hours face a heightened risk of work-related injuries. In an analysis of reports from over 11,000 nurses, Olds and Clarke found that both needlestick injuries and medication errors were 28% more common among nurses working more than 40 h per week. Overtime hours also increased the risk of needlestick injuries by 20% and medication errors by 30% (8). Another study involving over 19,000 bedside nurses revealed that those working more than 40 h per week were 17% more likely to experience needlestick injuries and 29% more likely to suffer sharps injuries. For nurses working over 50 h per week, these risks increased to 51% and 37%, respectively (11).
Studies have also demonstrated that the risks associated with long work hours are not constrained to accidents at the workplace. Several studies have demonstrated the risks of post-shift fatigue on drowsy driving and motor vehicle accidents (18, 73, 74). Scott et al. (12) examined the effects of shift work on drowsy driving in nurses. Two-thirds of nurses reported at least one episode of drowsy driving; ∼5% of nurses reported struggling to stay awake while driving home after every shift. The risk of reporting a drowsy driving episode doubled among nurses working 12.5 h or more. Night shifts nurses reported difficulty staying awake driving home 30% of post-shift periods (12).
2.3.2 Long hours and the risk of workplace conflict and lateral violence
Long work hours have been linked with mental and emotional exhaustion, increasing the likelihood of workplace conflict. In nursing, excessive work hours are a critical factor within a broader set of work-related conditions—such as high intensity work, heavy workloads, and high stakes outcomes—that are strongly predictive of elevated stress and burnout (75, 76). These stressors can significantly influence the organizational climate, creating an environment that fosters interpersonal conflict and psychological bullying (77, 78). Studies of workplace conflict in health care workers have found factors including shift work, long work hours, high stress work settings, heavy workloads, and poor working conditions are associated with inter-peer conflict and lateral violence (15, 51, 79, 142). Excessive work hours tend to increase stress and fatigue, causing breakdowns in communications among staff, reduced empathy and patience for the collaborative needs of others, and an increase in general irritability and conflict triggers (37, 80).
Studies have shown that the poor working conditions of nurses can deplete mental and emotional resources, making them more prone to negative mood (51, 81). Collectively, the impoverished psycho-social conditions of the work environment can significantly diminish the quality of the relationships within nursing units and increase the likelihood of hostile and abusive behaviour among staff (51, 58). One study found that average scores for teamwork, based on supportiveness, respect and cooperation, were significantly lower among nurses working longer hours (≥60 h per week), compared to those working <40 h per week. Other studies have demonstrated similar effects of long hours and overtime on occupational stress and the tendency for workplace conflict (43, 56). The degradation of key aspects of teamwork—such as treating coworkers with empathy and respect, and demonstrating a willingness to collaborate on tasks—constitutes a crucial leading indicator of a potential breakdown in healthy work relations, with implications for the quality of nursing care and patient safety (17, 43, 58, 82).
There is a growing body of evidence that a lack of control over work schedule coupled with high workloads can produce a work climate wherein lateral violence, or bullying, among nurses can flourish (77, 83, 84). Trépanier et al. (51) followed nurses over one-year to examine the effects of workload and work-related time pressures on bullying incidents. Controlling for frequency of bullying encounters at baseline, workload was found to be positively predictive of exposure to bullying behaviours over time when both job recognition (i.e., perceived social rewards from others at work) and social support were low (51). A recent study by Pogue and colleagues found that that nurses were more likely to experience workplace bullying the more hours they worked per week. Nurses who experienced bullying were significantly less likely to report good or excellent quality of care within their units, as well as a favourable grade for patient safety (44).
2.3.3 Long hours and the risks to individual health and wellbeing
Long hours and compressed work schedules are common in nursing; still, accumulating evidence indicates the potential negative effects on both mental and physical well-being resulting from these scheduling practices. Extensive epidemiological studies have established associations between non-traditional work hours, such as extended shifts and shift work, and the increased risk of various chronic health issues.
2.3.3.1 Sleep disorders
Long work hours and overtime diminish the available time for sleep, leading to fatigue (85). Among shift workers, quantity of sleep can be reduced by up to two hours a day; moreover, the quality of sleep tends to be diminished due to a lack of REM and Stage 2 sleep (86). Evidence suggests that few shift-working nurses obtain the recommended seven to eight hours of sleep during recovery periods (87). Self-reported sleep times range between 4.3 and 6.7 h, with night shift nurses generally getting less sleep than their daytime counterparts, averaging 5.7 h compared to 6.7 h, respectively (88). Consequently, night-shift nurses typically report heightened levels of fatigue and can are more susceptible to cumulative adverse effects (89). An investigation of sleep habits among nurses working extended shifts found that sleep duration averaged 5.5 h between 12 h shifts (28). Other key studies on the impacts of shift work among nurses have shown that sleep deficits resulting from extended work hours can induce sleepiness during shifts and increase the likelihood of involuntary napping, both of which are associated with a higher risk of medical errors (7). Over time, disordered sleep patterns can lead to chronic insomnia, a significant problem among shift-working nurses (11).
2.3.3.2 Mood disorders
A growing body of evidence has established a connection between extended work hours and the development of mood disorders. Research findings from this literature indicate that individuals working more than the standard 40 h per week are at an elevated risk of experiencing anxiety and depression (45, 52, 90). One longitudinal study of the psychological impacts of long work hours, utilizing an exceptionally robust sample of 2,960 workers, examined outcomes over a five-year period (52). Adjusting for baseline covariates, hazard analyses revealed a 1.66-fold increase in the risk of depressive symptoms, and a 1.74-fold increase in risk of anxiety symptoms among employees working more than 55 h per week, compared to those working 35–40 h per week. Sex-stratified analyses showed that the excess risk of depression and anxiety due to long work hours was especially pronounced in women (OR = 2.67) (52). Kleppa et al. (36) have reported similar results. Findings from comparative analyses showed that individuals who worked overtime hours exhibited both a higher prevalence and a greater severity of anxiety and depressive symptoms relative to those working standard hours. A dose-response relationship was also evident, with more work hours associated with higher levels of anxiety and depression (36). Hu et al. (31) have reported a dose-dependent association between long working hours and mental burnout. The odds of burnout was significantly greater in individuals working over 40 h per week (OR = 1.58). The odds of burnout substantially higher among those working more than 60 h per week (OR = 2.29). The authors recommend policies restricting weekly work hours to 40 to help prevent the onset of burnout (31).
2.3.3.3 Cardiovascular disease
Many studies have documented the relationship between long work hours and an increased risk of cardiovascular disease. Rivera et al. (45) conducted a review of 48 individual systematic reviews investigating the links between work schedule and several chronic conditions. The review found low grade evidence that long work hours and shift work are associated with low to moderate increases in the risk of cardiovascular disease (45). A meta-analytic review by Kivimäki et al. (34, 35), using data from over 600,000 participants in the US, Europe, and Australia, reported similar findings. After adjusting for age, sex, and socio-economic status, long work hours (≥55 h per week) was predictive of an increased risk of coronary heart disease (RR = 1.13) and incident stroke (RR = 1.33) (34). Convergent conclusions were reached by at least two earlier meta-analytic reviews. Using results from 42 observational studies, Virtanen et al. (53) found that working long hours (>50 h per week) is associated with a 40% increased risk of coronary heart disease (53). Similarly, Kang et al. (33) analyzed evidence from 11 separate studies, with follow-up periods ranging from 42 months to 30 years on average, and concluded that individuals working long hours (≥50 per week) had a 37% higher risk of developing cardiovascular disease (33). Dembe & Yao (22) utilized data from an unusually large cohort of participants (n = 7,492) to investigate chronic disease outcomes over a period of more than three decades. The authors identified a dose-response relationship between average weekly work hours and reported prevalence of heart disease. Compared to those working the standard 40 h per week, those working 51 to 60 h had a 1.68 times higher risk, while working more than 60 h per week increased the risk by 1.74 times (22).
2.3.3.4 Cancer
Several studies have linked long work hours and shift work with various types of cancer. In their longitudinal study tracking health outcomes in workers over three decades, Dembe & Yao (22) found that long work hours were associated with an elevated risk of non-skin cancers. Moreover, the relationship was cumulative, with individuals working 51 to 60 h per week experiencing a two-fold increase in the likelihood of cancer diagnosis (OR = 2.03), and workers exposed to more than 60 h per week exhibiting a risk increase of nearly three-fold (OR = 2.83). A multi-cohort study by Heikkila et al. (30) investigated the effects of excess work hours and shift work on incident cancer risk among workers who were cancer-free at baseline. Drawing on data from 12 separate prospective studies, the authors employed random effects meta-analysis to examine cancer rates among a total of 116,462 workers over an average period of 10.8 years. While the study did not show clear evidence of an association between working hours and overall cancer risk, the authors did find an association between working ≥55 h per week and an increased risk of female breast cancer (OR = 1.60) (30). Another meta-analytic review by Megdal et al. (41) found that exposure to night work was associated with a 48% increased risk of developing breast cancer (41). Bonde et al. (19) has also reported that statistically significant increases in risk for breast cancer were seen in people working night shift for 20 years or more; in turn, they conclude that women with previous or current be advised not to work night shifts because of strong experimental evidence demonstrating accelerated tumor growth by suppression of melatonin secretion (19).
In 2007, the International Agency for Research on Cancer (IARC) of the World Health Organization declared that there is sufficient evidence to support that shift work is a probable carcinogen. This designation is due to the disruption of the body's circadian rhythm caused by shiftwork (91). In their analysis of 17 systematic reviews on cancer outcomes in individuals working non-standard schedules, Rivera et al. (45) found moderate grade evidence linking shift work with female breast cancer.
2.3.3.5 Poor health behaviours and metabolic syndrome
Research indicates that long work hours and shift work are associated with an increased risk of deleterious health behaviours. Bushnell et al. (20) tracked the effects of different types of work schedules on the rate of poor health behaviours over a period of nine years. After adjusting for potential confounders, the authors found that, compared to a standard 8 h day shift, a 12 h rotation schedule was predictive of higher rates of smoking (RR = 1.60), lack of physical activity and exercise (RR = 1.30), and short sleep duration of six hours or less per night (RR = 1.30) (20).
Artazcoz et al. (16) examined the relationship between weekly work hours and health-related behaviours among more than 7,000 salaried workers aged 16–64. Gender-stratified findings revealed that, among men, working 51–60 h per week was predictive of an elevated risk of hypertension (OR = 1.60), smoking (OR = 1.33), shortage of sleep (OR = 1.42), and no leisure-time physical activity (OR = 2.43). Among women, long work hours were associated with an increased risk of shortage of sleep (OR = 2.21) (16). Other studies have demonstrated an elevated risk of smoking in both sexes as a result of long work hours. Shields (49) has reported that, for both sexes, changing from standard work hours to long work hours (>40 h per week) is associated with increases in smoking behaviour. Among men, long work hours were predictive of more than twice the odds of increased daily smoking, while among women, the corresponding odds were more than four times higher (49).
Metabolic syndrome and its attendant risk factors have also been linked to work schedules. Shields (49) has reported that, among men, increased work hours are associated with unhealthy weight gain (49). Other studies have likewise linked increases in body mass index to shift work and excessive work hours (92, 93). A meta-analysis on the health effects of work-related factors by Watanabe et al. (55) demonstrated a significant positive relationship between shift work and metabolic syndrome (RR = 1.59) (55). A meta-analysis by Wong et al. (57) reported an association between long work hours and a heightened risk of metabolic syndrome (OR = 1.10) (57).
A handful of studies have identified work schedule as a risk factor in the onset of Type 2 diabetes. In a meta-analysis of data from more than 200,000 participants, Kivimäki et al. (34, 35) found that long work hours (≥55 h per week) were associated with an elevated risk of a Type 2 diabetes diagnosis in lower income populations (RR = 1.29) (35). Dembe & Yao (22) have reported that exposure to excessive work hours is predictive of an elevated risk of diabetes onset (22). Possible mechanisms underlying this relationship may include poor sleep quality and reduced sleep duration, which can cause an imbalance in appetite hormones, increasing feelings of hunger. These factors can lead to metabolic changes, resulting in obesity, insulin resistance and reduced lipid tolerance (94).
2.3.3.6 Individual and organization-level factors affecting fatigue risk
Empirically-established thresholds regarding the effects of working hours on fatigue offer essential guidance for constructing safety limits. However, various individual and organizational factors can exacerbate occupational fatigue, thereby accelerating fatigue-based risk. At the individual level, factors influencing the onset of occupational fatigue include age, biological sex, health status, sleep habits, and personal circumstances that can affect opportunities for sleep and recovery, such as caregiving responsibilities. Within organizations, the structure of work systems can contribute to work-related fatigue and fatigue-related risks, including factors such as working conditions, heavy workloads, and work schedules that do not allow for adequate recovery time between shifts.
2.3.3.6.1 Age
As individuals age, sleep patterns often change, characterized by shorter and more fragmented periods of sleep, with insomnia becoming more common (85, 95). Consequently, older workers may find it increasingly challenging to attain adequate recovery between work shifts (96, 97). Research on sleep deprivation indicates that performance deficits equivalent to a blood alcohol concentration (BAC) of up to 0.10% can occur, with more mature nurses reaching this performance limit in less time compared to their younger colleagues (98). Additional studies indicate that the range of adverse physical and psychological effects resulting from shiftwork-related fatigue is more pronounced in nurses over the age of 40 (42). While certain research suggests potential protective effects of experience and enhanced safety performance associated with older age and longer work tenure (99), it is important to note that the cumulative effects of fatigue stemming from shift work and extended work hours might counterbalance any incremental benefits linked with age (100, 101).
2.3.3.6.2 Biological sex
Some evidence suggests that hormonal differences and gender-specific health issues can influence fatigue-levels, leading to differences in the ability of men and women to tolerate long hours and shift work. Studies examining the sex-stratified effects of non-standard work schedules have found that women working shift work or long hours experience shorter and lower quality sleep periods compared to their male counterparts (16, 96, 102, 103). Long work hours have been associated with a greater likelihood of the onset of depressive symptoms (49, 52, 104) and diabetes (105) in women, though at least one study has reported that adverse mental and physical outcomes resulting from excessive work hours tend to be more pronounced in men (16). Weekly work hours have also been demonstrated to have a stronger association with women's risk of work injury (106, 107). Some of the differences in susceptibility to the effects of extended work hours between women and men likely arise from disparities in childcare, other caregiving responsibilities, and domestic workloads, which disproportionately limit the amount of time women can dedicate to sleep and recovery from work (108).
2.3.3.6.3 Health status
Research has demonstrated that certain chronic diseases can contribute to daytime sleepiness and compromise cognitive functioning. Chronic conditions known to impact fatigue include arthritis, asthma, chronic fatigue syndrome, chronic obstructive pulmonary disease (COPD), and rhinitis (109). As the population ages, the incidence of chronic morbidity due to various health conditions has increased. Currently, approximately one in three Canadians (33.7%) lives with a chronic condition, including cardiovascular disease, cancer, diabetes, or mood and/or anxiety disorders (110). The physical and psychosocial stresses linked with non-standard work schedules are known to be less well tolerated by individuals with chronic health issues (96, 108). One study observed that night shift workers with Type 2 diabetes had greater difficulty controlling glucose levels compared to their counterparts working day shifts (111). Other research has demonstrated lower tolerance of non-standard work hours among workers with mood disorders such as anxiety (112). The presence of chronic conditions is believed to deplete the body of critical physiological and psychic resources, resulting in greater risk of fatigue (85). Moreover, the relationship between work hours and health is likely circular, as long-term exposure to excessive work hours has been identified as a significant causal factor in the onset of chronic health problems (113).
2.3.3.6.4 Sleep habits
The need for good sleep hygiene practices is heightened among individuals working extended hours or shift work. Insufficient or poor sleep, often linked to inadequate recovery, can serve as a common pathway from long work hours, shift work and work stress to various forms of illness (114). Non-work factors such as domestic and caregiving responsibilities can significantly impact the opportunity for recovery, as well as the quality and duration of sleep during recovery periods. Competing work and family responsibilities give rise to physical and psychological strain that can exacerbate fatigue (115). Studies investigating the effects of work scheduling on nurses have identified work-family conflict as a significant predictor of poor sleep quality (116). Additionally, sleep disruption resulting from the strain of work-life conflict has been demonstrated to have deleterious impacts on nurses’ mental health (115, 117).
2.3.3.6.5 Work demands/stressors
Hectic work characterized by high work demands under fast-changing circumstances is physically and psychologically draining and can lead to high levels of fatigue in nurses (118, 119). Work that is hectic or physically strenuous is linked to poor sleep quality with deleterious effects on recovery (96). A synthesis of studies on work-related fatigue reported strong positive associations between work demands and the need for recovery across six different occupations (120). Nurses typically contend with heavy physical workloads and circumstances that demand a high level of emotional regulation to sustain attention and focus. The level of intensity of work demands in nursing can accelerate the onset of occupational fatigue and attendant fatigue-based risks (121). Nurses working in acute care environments, particularly those with a high proportion of patients at risk of rapid deterioration, often experience heightened strain and are more susceptible to fatigue (122, 123). Consequently, research on managing stress and fatigue in nurses recommends monitoring individual nurses’ level of fatigue during a work shift, as well as utilizing tools to predict fatigue risk (118, 124).
2.3.3.6.6 Work schedule
Shift work, especially rotating schedules and night shifts, is known to contribute to poor sleep quality and work-related fatigue (42, 74). Long work shifts of 12 h or more have been linked with various fatigue-related safety risks (23, 25, 47), particularly shifts occurring at night (54). The number of consecutive work shifts and total weekly work hours are also associated with an increased risk of work-related accidents and injuries in a cumulative fashion (58, 125). One aspect of nurses’ work schedules that has been linked with higher risk of fatigue is the “quick return,” where nurses are given less than 11 h between the end of one shift and the start of the next. Considering optimal sleep periods (typically recommended as seven to eight hours for most adults), schedules that mandate quick returns to work do not allow for adequate recovery between shifts (118). Research has linked quick returns to a higher incidence of sick leave, a relationship likely influenced by the reduced amount of time nurses have available to sleep and recover from fatigue (126).
The significant positive effects of scheduled rest breaks during a shift are well-documented. In their study of workers hospitalized with severe injuries, Lombardi et al. (127) demonstrated that even minimal rest breaks of less than 30 min had a significant effect on delaying the onset of work-related injury (127). Likewise, Tucker et al. (128) reported that regular rest breaks constitute an effective method of controlling the accumulation of injury risk during a work shift (128).
3 Regulations on work hours and fatigue-risk management within safety-critical industries
The impact of long work hours on occupational health and safety outcomes is a major concern for employers, leading to the increased adoption of regulations across various industries (25). Governments in developed countries have increasingly set limits on work hours to minimize the adverse effects of fatigue on occupational health and safety outcomes. A review of these policies suggest that for the most part these conform to the research evidence on work hours safety; however, there are some notable exceptions, including within the Canadian health care sector.
A review of the regulations on work hours within Canada focused on the active regulatory limits enforced by government or another regulatory body within safety-sensitive industries including, transport, nuclear, aviation, health care. Policies concerning the safety limits on work hours within the US and the EU focus on restrictions enforced by regulatory bodies within the health care sector.
3.1 Work hours regulations in safety-sensitive industries in Canada
In Canada, certain classes of workers within federally regulated safety-sensitive industries are subject to specific restrictions on work hours. Motor vehicle operations/trucking, rail, nuclear and aviation are each governed by a set of restrictions on work hours to help maintain worker performance, forestall the onset of fatigue, and reduce the risk of accidents. The specific policies regarding work hours for each domain are described in turn. In general, work hours regulations focus on three key aspects of the work schedule: (1) total number of consecutive work hours; (2) number of successive [night] shifts; and, (3) mandatory minimum periods for recovery.
3.1.1 Motor vehicle operators
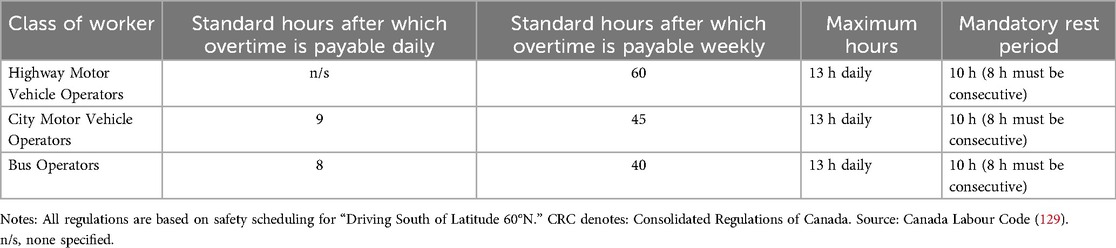
Under Part III of the Canada Labour Code (CLC), motor vehicle operators are governed by the Motor Vehicle Operators Hours of Work Regulations (CRC, c.990). This classification encompasses city and highway vehicle operators involved in interprovincial and international transport of goods or passengers, as well as the transport of mail, and bus operators (129). This category includes commercial vehicles and trucking. The general limits on work hours for each class of worker as stipulated by the regulations are provided in Table 3.
3.1.2 Railway operators
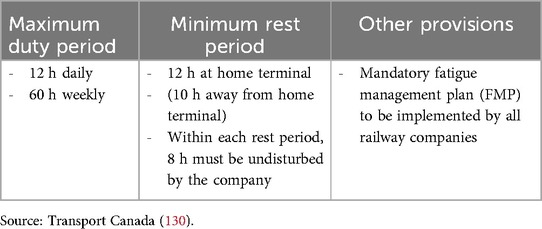
Transport Canada has set limits on work hours to protect the health and safety of railway operators under the Railway Safety Act. These types of employees include: locomotive engineers, conductors, trainmen, yardmen, pilots, operators of remote-control locomotives, and operators of light rail passenger equipment.
Notably, unlike regulations covering motor vehicle operators, legislation regarding work hour limits for railway operators specifically identifies its purpose as “fatigue management” so as to mitigate “fatigue-related risk that may affect safe railway operations.” Fatigue management is considered a “shared responsibility” between the railway company and the employees. In turn, the term “fit for duty” with respect to work hours limits and rest breaks appears multiple times in the legislation. An objective measure of fatigue/duty-fitness is taken prior to shift periods using the Karolinska Sleepiness Scale, a ten-item self-report measure of one's current level of fatigue (130). Specific directives of the regulation are given in Table 4.
Relevant excerpts from the policy as to specific strategies for fatigue management include:
Where an employee's duty period is scheduled to last more than 10 h and to end between 00:01 and 06:00, an employee shall report to the railway company, in accordance with the company's fatigue management plan, that they believe themselves to be fit for duty in accordance with the fatigue self-assessment training provided by the railway company and that they have met the following requirements:
• Obtained at least five hours of sleep in the 24 h prior to commencing the duty period;
• Obtained at least 12 h of sleep in the 48 h prior to commencing the duty period; and,
• Assessed themselves as scoring a seven or lower on the Karolinska Sleepiness Scale (scored on 1–10 scale, where is “extremely alert” and 10 is “extremely sleepy”).
In an effort to achieve maximal mitigation of fatigue-based risk, the policy also explicitly allows for “use of controlled napping protocols,” where appropriate (130).
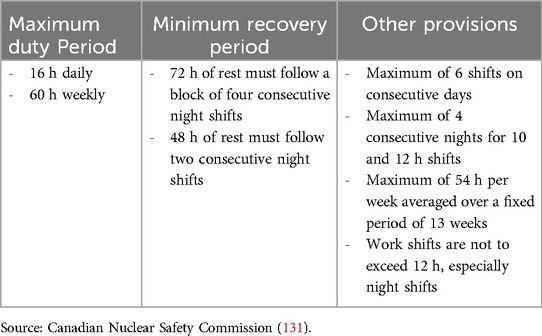
3.1.3 Nuclear
The work hours of employees in the nuclear energy industry are governed by the Canadian Nuclear Safety Commission under the Nuclear Safety and Control Act (NSCA). Like the railway industry, regulations for nuclear employees stipulate that the goal is to ensure “fitness for duty” by effectively “managing worker fatigue.” In particular, the regulation requires that nuclear operators “shall document and implement limits on hours of work and recovery periods that:
1. Provide sufficient time for sleep daily
2. Restrict consecutive shifts to limit the build-up of sleep debt
3. Provide sufficient time off to allow for recovery from sleep debt
4. Limit average weekly hours as a safeguard against cumulative fatigue.”
Moreover, nuclear operators must “document the rationale that justifies their limits on hours of work and recovery periods” and that “the rationale shall be based on scientific principles and knowledge.” In turn, it is required that all nuclear operators must “define and implement a range of measures to manage risks associated with fatigue, including those to manage the level of fatigue workers experience at work and to reduce the likelihood and consequences of fatigue-related errors” (131). The range of measures recommended for mitigating worker fatigue include: allowing rest periods or an opportunity to sleep, nurturing an environment that includes self-reporting when workers believe they are too fatigued to perform their duties competently and safely; employing additional supervisory oversight and independent verification when the risk of fatigue is highest (e.g., during the night shift, near the end of a shift, working beyond 12 h); rotating workers between tasks of varying cognitive and physical workloads; and, scheduling safety-critical tasks outside of peak times for fatigue (especially between the hours of 2:00 a.m. and 6:00 a.m.—referred to in the research as the “window of circadian low”). Specific limits on work hours as set forth by the NSCA are outlined in Table 5.
3.1.4 Aviation
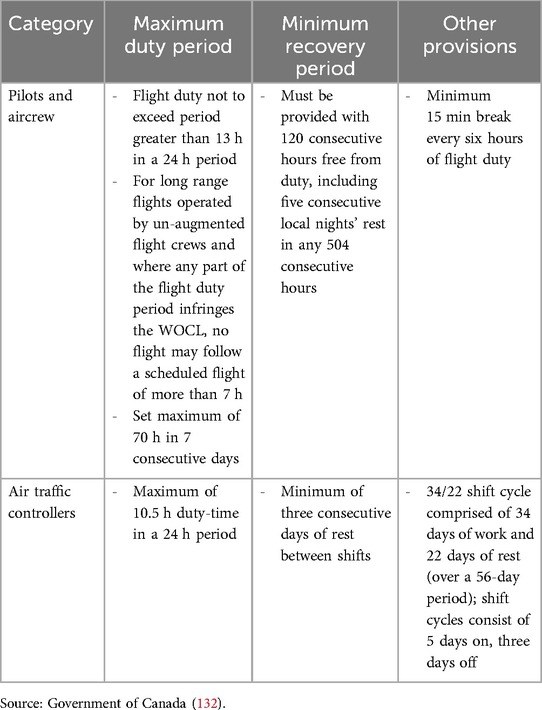
Work hour limits for air crews and air traffic controllers are governed by Transport Canada's Canadian Aviation Regulations (CAR). As part of a comprehensive approach to safety management, CAR also requires that all air operators have a fatigue risk management program in place for flight crew members as part of a comprehensive approach to safety management. Table 6 provides an overview of work hour restrictions and mandatory rest periods set forth in the regulation.
The regulations also require that air operators implement a specific protocol for managing fatigue risk in employees—i.e., Fatigue Risk Management System for the Canadian Aviation Industry. The policy stipulates that, among other requirements, employers must provide aviation workers training in each of the following areas: personal fatigue management strategies relating to sleep hygiene, lifestyle, exercise and diet; sleep requirements and the science of fatigue; how to recognize fatigue in themselves and others; awareness of human and organizational factors causing fatigue such as sleep quality and duration, the impact of shift work and overtime, and the effects of changes in time zones.
3.1.5 Health care
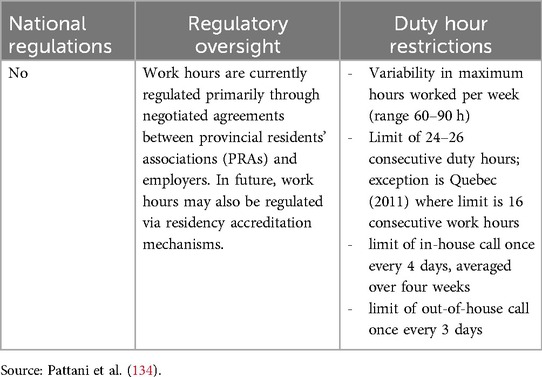
At present, there are no federal regulations governing the work hours of health care employees. The work hours of medical residents, however, are governed through negotiated agreements between the Provincial Residents’ Associations (PRAs) and employers. The PRAs currently set limits for residents at between 24 and 26 consecutive work hours. The exception is Quebec where, since July 1, 2012, residents’ time on duty has been restricted to 16 h due to result an arbitration ruling in the province that a 24 h duty period is a violation of the Canadian Charter of Rights and Freedoms and the Quebec Charter of Human Rights and Freedoms (133). Weekly work hour limits vary widely across provinces, ranging from 60 to 90 h per week (134). General regulations and restrictions pertaining to resident duty hours in Canada are outlined in Table 7.
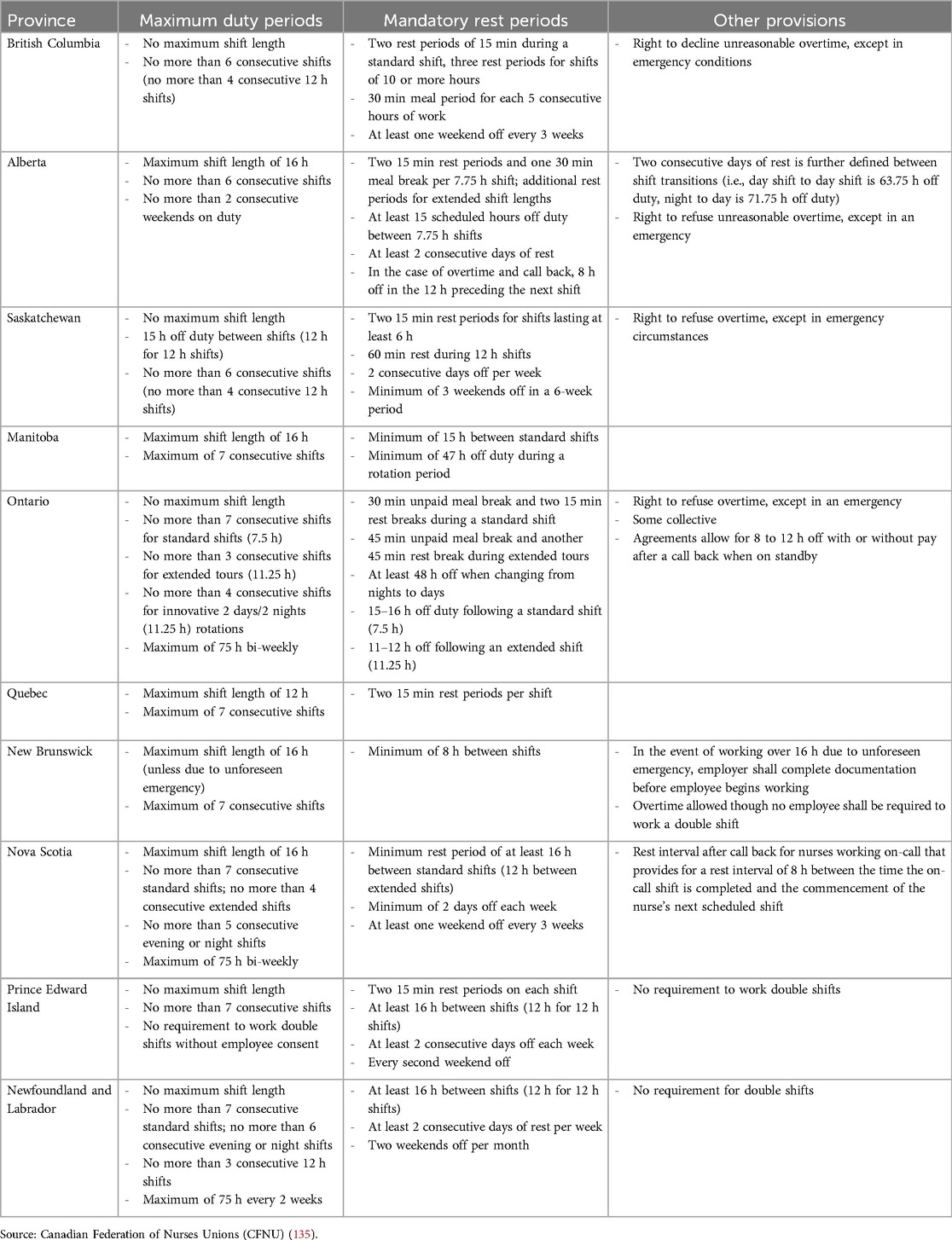
Like medical residents, currently there is no pan-Canadian limitation on nurses’ work hours. Where regulations exist, these are primarily through collective agreements with employers. There are currently dozens of collective agreements in effect within each province covering a range of nurse practice types—e.g., hospital, community health, and long-term care. Table 8 provides an overview of the key policies with respect to work hour limits contained within the master agreements for each province.
Notably, although five provinces—Alberta, Manitoba, Quebec, Nova Scotia, and New Brunswick—only Quebec sets the limit at 12 h, which the literature suggests is the safety maximum. Still, Quebec allows for up to a maximum seven consecutive work shifts, which the evidence indicates could be problematic for nurses working extended shifts. Only Nova Scotia and Newfoundland and Labrador have limited the number of consecutive night or evening shifts. Four provinces—British Columbia, Alberta, Saskatchewan and Ontario—have explicitly provided for the right to refuse overtime hours, though New Brunswick, PEI and Newfoundland and Labrador have agreements that stipulate no requirement to work double shifts. Four provinces, Ontario, Nova Scotia, PEI and Newfoundland have mandated a minimum break of 11 h (i.e., no “quick returns”) after an extended shift.
3.2 Work hours regulations in health care in the United States
Like its peer countries, in the United States the work hours of truck drivers, locomotive engineers, and pilots are regulated to protect the public from fatigue-related errors, though hospitalized patients lack similar protection (70). At present, there are no restrictions on the number of hours a nurse may voluntarily work in a 24 h or a seven-day period in the United States, while only minimal restrictions exist on hours worked by physicians (70).
As of 2011, the Accreditation Council for Graduate Medical Education (ACGME) recommended the following work hour limits for medical residents: interns were allowed a maximum of 16 continuous work hours, with an overall workweek limit of 80 h; shifts could last up to 24 h, plus an additional six hours for transitioning care; residents were entitled to one day off per week, averaged over a four-week period; and on-call duties could be scheduled no more than once every three nights (136).
In contrast, nurses’ work hours are regulated by state governmental agencies known as nursing regulatory bodies (NRBs), leading to variations in work hour limits across states. It should be noted, however, that none of these jurisdictional restrictions address the duration nurses may work on a voluntary basis (70). An overview of work hours regulations for health care professionals in the US is provided in Table 9.

Table 9. Work hours regulations for health care professionals, select jurisdictions (United States).
Research on the impact of state regulations on nurses’ work hours demonstrates their effectiveness in reducing overwork (138, 139). In one study, Bae and Yoon (139) found that government regulations on mandatory overtime and consecutive work hours led to a 3.9 percentage point decrease in the likelihood of mandated overtime and an 11.5 percentage point reduction in the likelihood of nurses working 40 h per week (139).
3.3 Work hours regulations in health care in Europe
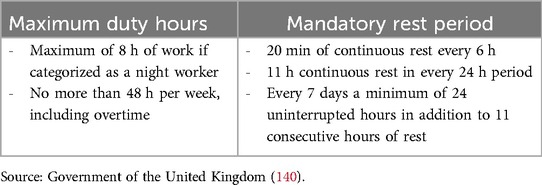
As in all safety-sensitive industries in the EU, work hours in health care are regulated by the European Working Time Directive (EWTD). Instituted in 1993, the EWTD introduced specific measures for scheduling shifts and rest periods to limit work hours, based on evidence that shift work and excessive hours can pose significant occupational health and safety risks (95). The work hours of both medical residents and nurses are governed by the EWTD. The specific requirements of this legislation are detailed in Table 10.
4 Discussion
A rapid review of the evidence regarding the occupational health and safety impacts of excessive work hours is both clear and compelling. Extended shifts exceeding 12 h significantly increase the risk of occupational fatigue, leading to various fatigue-related hazards. Likewise, working more than 40 h per week is associated with higher health and safety risks. The cumulative effect of work-related fatigue raises the likelihood of accidents and injuries, both during work and after shifts (e.g., due to drowsy driving). Chronic fatigue also negatively impacts workplace culture and team cohesion, as fatigued employees often show reduced empathy toward peers and a lower willingness to cooperate. The health consequences of excessive work hours include sleep disturbances, mood disorders, and serious chronic conditions such as cardiovascular disease, metabolic disorders, and cancer. Fatigue from extended work hours is further exacerbated by shift work, especially rotating schedules that involve night shifts, which disrupt circadian rhythms. The body's neurophysiological rhythms, particularly during the “window of circadian low” (2:00 a.m.–6:00 a.m.), reduce the ability to work effectively at night, leading to a higher risk of workplace injuries and long-term health problems for night shift workers. Extensive research, particularly in nursing, has highlighted the detrimental effects of long work hours and shift work schedules on both personal and patient safety.
Despite the well-documented occupational health and safety risks linked to long work hours and occupational fatigue—risks that have prompted governmental regulations in safety-critical industries like transportation, aviation, and the nuclear sector—the health care industry remains largely unregulated in this area. In Canada, the only exception is the work hour restrictions for medical residents, enforced by provincial regulatory bodies. However, there are no governmental restrictions currently exist on the number of hours a nurse can work within a 24 h period or over a 7-day interval. Protections against overwork for nurses are provided solely through individual collective agreements, within only five provinces placing limits on shift-length under normal (non-emergency) conditions. Of these, only Quebec enforces a 12 h maximum, which aligns with evidence-based recommendations. Considering the longstanding history of regulatory limits on work hours in safety-critical industries outside of health care, the lack of governmental protections for nurses’ working conditions raises the question of gender-bias as a potential underlying factor. It is crucial to bring this disparity to the forefront for policy makers, not only in the interest of equity, but also to ensure public safety. In Europe, comprehensive worker protections regarding work hour limits set a valuable precedent for other Western countries, and could offer a straightforward solution in this context.
Additionally, fatigue risk management programs are standard practice within safety-critical industries and should be adopted in health care settings as well. Occupational health and safety management systems such as the ISO-45001 provide specific guidelines for employers to identify potential fatigue hazards and strategies to mitigate fatigue risks. These standards encompass crucial safeguards related to work hour limits, including shift duration, properly timed rest breaks, the number of consecutive shifts, weekly work hour loads, and systems for fatigue management and monitoring. Fatigue monitoring enables employers to consider individual factors like age and health status, which can vary over time. These frameworks also provide guidance on educating workers to understand the causes and consequences of fatigue, as well as how to recognize fatigue in themselves and others. Health care employers can reinforce these standards by adopting practices such as providing designated napping spaces for nurses working extended or overnight shifts and offering transportation home for those fatigued after their shifts. These actions help reduce the risks associated with fatigue, enhance overall safety, and improve working conditions for nurses—key steps in addressing staffing shortages by boosting both retention and recruitment.
This review marks the first direct application of research evidence on the occupational health and safety impacts of excessive work hours and occupational fatigue to gain a clearer understanding of safe work hour limits in nursing. It also offers a foundational framework for designing work schedules and establishing work hour targets to promote safe nursing practices. The primary strength of the review lies in its comprehensive approach, synthesizing findings from the academic literature and linking them to current policy recommendations across multiple safety-critical sectors beyond health care. Further research on the effects of long work hours in nursing could, in the future, enable a more extensive systematic review of the evidence. However, a limitation of this review is the short timeframe allotted for the study—less than six months—arising from the urgent need to deliver a rapid overview of the evidence to Canadian health care regulators. Additionally, the involvement of only a single investigator could be considered a weakness, as the absence of multiple reviewers may have reduce the capacity to check for potential bias. In the future, additional studies on the occupational health and safety consequences of long work hours should also include qualitative investigations into workers’ experiences with work hour regulations, particularly assessing the extent to which these regulations are enforced in practice. Furthermore, research on resilience among nurses (141) should place greater emphasis on working conditions and work hours as key factors contributing to psychological harm and reduced well-being.
Still, given the well-documented effects of excessive work hours on both individual and public health, there is ample evidence supporting the need for stricter regulations on nurses’ work hours. Ensuring safe and high-quality care over the long term requires providing nurses with robust support systems and implementing fair scheduling practices. These measures will not only improve nurses’ work satisfaction and overall wellbeing but also help address staffing shortages by fostering better working conditions. This, in turn, creates a virtuous cycle that leads to better patient outcomes and a more resilient health care system.
Author contributions
HS-M: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Funding for this research was provided by the Canadian Federation of Nurses Unions (CFNU).
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bagwell GA, Cesario SK, Fraser D, Kenner C, Walker K. Breaking the cycle of nursing chaos: the need to address the nursing shortage. Adv Neonatal Care. (2023) 23(6):495–8. doi: 10.1097/anc.0000000000001126
2. Drost A, Ben-Ahmed HE, Sweetman A. The trajectory of agency-employed nurses in Ontario, Canada: a longitudinal analysis (2011–2021). Policy Polit Nurs Pract. (2024) 25(2):70–82. doi: 10.1177/15271544241240489
4. Statistics Canada. Job vacancy and wage survey (2023). Available online at: https://www150.statcan.gc.ca/t1/tbl1/en/cv.action?pid=1410032801 (retrieved April 23, 2024).
5. Peršolja M. Effects of nurses’ schedule characteristics on fatigue: an integrative review. Nurs Manage. (2023) 54(4):28–37. doi: 10.1097/01.Numa.0000921904.11222.11
6. Canadian Union of Public Employees. 24-hour shifts for nurses at North Bay hospital puts patients at risk. (2023).
7. Scott LD, Rogers AE, Hwang WT, Zhang Y. Effects of critical care nurses’ work hours on vigilance and patients’ safety. Am J Crit Care. (2006) 15(1):30–7. doi: 10.4037/ajcc2006.15.1.30
8. Olds DM, Clarke SP. The effect of work hours on adverse events and errors in health care. J Saf Res. (2010) 41(2):153–62. doi: 10.1016/j.jsr.2010.02.002
9. Trinkoff A, Johantgen M, Storr C, Gurses A, Liang Y, Han K. Nurses’ work schedule characteristics, nurse staffing, and patient mortality. Nurs Res. (2011) 60(1):1–8. doi: 10.1097/NNR.0b013e3181fff15d
10. Gershon RR, Pearson JM, Sherman MF, Samar SM, Canton AN, Stone PW. The prevalence and risk factors for percutaneous injuries in registered nurses in the home health care sector. Am J Infect Control. (2009) 37(7):525–33. doi: 10.1016/j.ajic.2008.10.022
11. Lo W-Y, Chiou S-T, Huang N, Chien L-Y. Long work hours and chronic insomnia are associated with needlestick and sharps injuries among hospital nurses in Taiwan: a national survey. Int J Nurs Stud. (2016) 64:130–6. doi: 10.1016/j.ijnurstu.2016.10.007
12. Scott LD, Hwang WT, Rogers AE, Nysse T, Dean GE, Dinges DF. The relationship between nurse work schedules, sleep duration, and drowsy driving. Sleep. (2007) 30(12):1801–7. doi: 10.1093/sleep/30.12.1801
13. Khayyat S, Walters P, Whittlesea C, Nazar H. Patient and public perception and experience of community pharmacy services post-discharge in the UK: a rapid review and qualitative study. BMJ Open. (2021) 11(3):e043344. doi: 10.1136/bmjopen-2020-043344
14. Tricco AC, Antony J, Zarin W, Strifler L, Ghassemi M, Ivory J, et al. A scoping review of rapid review methods. BMC Med. (2015) 13:224. doi: 10.1186/s12916-015-0465-6
15. Ariza-Montes A, Muniz N, Montero-Simó M, Araque-Padilla R. Workplace bullying among healthcare workers. Int J Environ Res Public Health. (2013) 10(8):3121–39. doi: 10.3390/ijerph10083121
16. Artazcoz L, Cortès I, Escribà-Agüir V, Cascant L, Villegas R. Understanding the relationship of long working hours with health status and health-related behaviours. J Epidemiol Community Health. (2009) 63(7):521. doi: 10.1136/jech.2008.082123
17. Baldwin D, Daugherty S. Interprofessional conflict and medical errors: results of a national multi-specialty survey of hospital residents in the US. J Interprof Care. (2008) 22(6):573–86. doi: 10.1080/13561820802364740
18. Barger LK, Cade BE, Ayas NT, Cronin JW, Rosner B, Speizer FE, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. (2005) 352(2):125–34. doi: 10.1056/NEJMoa041401
19. Bonde JP, Hansen J, Kolstad HA, Mikkelsen S, Olsen JH, Blask DE, et al. Work at night and breast cancer–report on evidence-based options for preventive actions. Scand J Work Environ Health. (2012) 38(4):380–90. doi: 10.5271/sjweh.3282
20. Bushnell PT, Colombi A, Caruso CC, Tak S. Work schedules and health behavior outcomes at a large manufacturer. Ind Health. (2010) 48(4):395–405. doi: 10.2486/indhealth.mssw-03
21. Dembe A, Delbos R, Erickson J. Estimates of injury risks for healthcare personnel working night shifts and long hours. Qual Saf Health Care. (2009) 18(5):336–40. doi: 10.1136/qshc.2008.029512
22. Dembe A, Yao X. Chronic disease risks from exposure to long-hour work schedules over a 32-year period. J Occup Environ Med. (2016) 58(9):861–7. doi: 10.1097/jom.0000000000000810
23. Dong X. Long workhours, work scheduling and work-related injuries among construction workers in the United States. Scand J Work Environ Health. (2005) 31(5):329–35. doi: 10.5271/sjweh.915
24. Folkard S. Black times: temporal determinants of transport safety. Accid Anal Prev. (1997) 29(4):417–30. doi: 10.1016/S0001-4575(97)00021-3
25. Folkard S, Lombardi D. Modeling the impact of the components of long work hours on injuries and “accidents”. Am J Ind Med (2006) 49(11):953–63. doi: 10.1002/ajim.20307
26. Folkard S, Tucker P. Shift work, safety and productivity. Occup Med (Chic Ill). (2003) 53(2):95–101. doi: 10.1093/occmed/kqg047
27. Gander PH, Merry A, Millar MM, Weller J. Hours of work and fatigue-related error: a survey of New Zealand anaesthetists. Anaesth Intensive Care. (2000) 28(2):178–83. doi: 10.1177/0310057(0002800209
28. Geiger-Brown J, Rogers VE, Trinkoff AM, Kane RL, Bausell RB, Scharf SM. Sleep, sleepiness, fatigue, and performance of 12-hour-shift nurses. Chronobiol Int. (2012) 29(2):211–9. doi: 10.3109/07420528.2011.645752
29. Hänecke K, Tiedemann S, Nachreiner F, Grzech-Sukalo H. Accident risk as a function of hour at work and time of day as determined from accident data and exposure models for the German working population. Scand J Work Environ Health. (1998) 24(Suppl 3):43–8.
30. Heikkila K, Nyberg ST, Madsen IEH, de Vroome E, Alfredsson L, Bjorner JJ, et al. Long working hours and cancer risk: a multi-cohort study. Br J Cancer. (2016) 114(7):813–8. doi: 10.1038/bjc.2016.9
31. Hu NC, Chen JD, Cheng TJ. The associations between long working hours, physical inactivity, and burnout. J Occup Environ Med. (2016) 58(5):514–8. doi: 10.1097/jom.0000000000000715
32. James L, James S, Wilson M, Brown N, Dotson E, Dan Edwards C, et al. Sleep health and predicted cognitive effectiveness of nurses working 12-hour shifts: an observational study. Int J Nurs Stud. (2020) 112:103667. doi: 10.1016/j.ijnurstu.2020.103667
33. Kang MY, Park H, Seo JC, Kim D, Lim YH, Lim S, et al. Long working hours and cardiovascular disease: a meta-analysis of epidemiologic studies. J Occup Environ Med. (2012) 54(5):532–7. doi: 10.1097/JOM.0b013e31824fe192
34. Kivimäki M, Jokela M, Nyberg ST, Singh-Manoux A, Fransson EI, Alfredsson L, et al. Long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603,838 individuals. Lancet. (2015) 386(10005):1739–46. doi: 10.1016/s0140-6736(15)60295-1
35. Kivimäki M, Virtanen M, Kawachi I, Nyberg ST, Alfredsson L, Batty GD, et al. Long working hours, socioeconomic status, and the risk of incident type 2 diabetes: a meta-analysis of published and unpublished data from 222 120 individuals. Lancet Diabetes Endocrinol. (2015) 3(1):27–34. doi: 10.1016/s2213-8587(14)70178-0
36. Kleppa E, Sanne B, Tell GS. Working overtime is associated with anxiety and depression: the hordaland health study. J Occup Environ Med. (2008) 50(6):658–66. doi: 10.1097/JOM.0b013e3181734330
37. Ku C-H, Smith MJ. Organisational factors and scheduling in locomotive engineers and conductors: effects on fatigue, health and social well-being. Appl Ergon. (2010) 41(1):62–71. doi: 10.1016/j.apergo.2009.04.006
38. Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med. (2004) 351(18):1838–48. doi: 10.1056/NEJMoa041406
39. Matre D, Skogstad M, Sterud T, Nordby KC, Knardahl S, Christensen JO, et al. Safety incidents associated with extended working hours. A systematic review and meta-analysis. Scand J Work Environ Health. (2021) 47(6):415–24. doi: 10.5271/sjweh.3958
40. McCormick F, Kadzielski J, Evans B, Landrigan C, Herndon J, Rubash H. Fatigue optimization scheduling in graduate medical education: reducing fatigue and improving patient safety. J Grad Med Educ. (2013) 5(1):107–11. doi: 10.4300/JGME-D-12-00021.1
41. Megdal SP, Kroenke CH, Laden F, Pukkala E, Schernhammer ES. Night work and breast cancer risk: a systematic review and meta-analysis. Eur J Cancer. (2005) 41(13):2023–32. doi: 10.1016/j.ejca.2005.05.010
42. Muecke S. Effects of rotating night shifts: literature review. J Adv Nurs. (2005) 50(4):433–9. doi: 10.1111/j.1365-2648.2005.03409.x
43. Palancı Y, Mengenci C, Bayraktaroğlu S, Emhan A. Analysis of workplace health and safety, job stress, interpersonal conflict, and turnover intention: a comparative study in the health sector. Health Psychol Rep. (2021) 9(1):76–86. doi: 10.5114/hpr.2020.99971
44. Pogue CA, Li P, Swiger P, Gillespie G, Ivankova N, Patrician PA. Associations among the nursing work environment, nurse-reported workplace bullying, and patient outcomes. Nurs Forum. (2022) 57(6):1059–68. doi: 10.1111/nuf.12781
45. Rivera AS, Akanbi M, O'Dwyer LC, McHugh M. Shift work and long work hours and their association with chronic health conditions: a systematic review of systematic reviews with meta-analyses. PLoS One. (2020) 15(4):e0231037. doi: 10.1371/journal.pone.0231037
46. Rodrigues T, Fischer F, Helene O, Antunes E, Furlan E, Morteo E, et al. Modelling the root causes of fatigue and associated risk factors in the Brazilian regular aviation industry. Saf Sci. (2023) 157:105905. doi: 10.1016/j.ssci.2022.105905
47. Rogers A, Hwang W, Scott L, Aiken L, Dinges D. The working hours of hospital staff nurses and patient safety. Health Aff. (2004) 23(4):202–12. doi: 10.1377/hlthaff.23.4.202
48. Sagherian K, Zhu S, Storr C, Hinds PS, Derickson D, Geiger-Brown J. Bio-mathematical fatigue models predict sickness absence in hospital nurses: an 18 months retrospective cohort study. Appl Ergon. (2018) 73:42–7. doi: 10.1016/j.apergo.2018.05.012
50. Thompson B. Does work-induced fatigue accumulate across three compressed 12 h shifts in hospital nurses and aides? PLoS One. (2019) 14(2):e0211715. doi: 10.1371/journal.pone.0211715
51. Trépanier S, Peterson C, Fernet C, Austin S, Desrumaux P. When workload predicts exposure to bullying behaviours in nurses: the protective role of social support and job recognition. J Adv Nurs. (2021) 77(7):3093–103. doi: 10.1111/jan.14849
52. Virtanen M, Ferrie JE, Singh-Manoux A, Shipley MJ, Stansfeld SA, Marmot MG, et al. Long working hours and symptoms of anxiety and depression: a 5-year follow-up of the whitehall II study. Psychol Med. (2011) 41(12):2485–94. doi: 10.1017/s0033291711000171
53. Virtanen M, Heikkilä K, Jokela M, Ferrie JE, Batty GD, Vahtera J, et al. Long working hours and coronary heart disease: a systematic review and meta-analysis. Am J Epidemiol. (2012) 176(7):586–96. doi: 10.1093/aje/kws139
54. Wagstaff AS, Sigstad Lie JA. Shift and night work and long working hours–a systematic review of safety implications. Scand J Work Environ Health. (2011) 37(3):173–85. doi: 10.5271/sjweh.3146
55. Watanabe K, Sakuraya A, Kawakami N, Imamura K, Ando E, Asai Y, et al. Work-related psychosocial factors and metabolic syndrome onset among workers: a systematic review and meta-analysis. Obes Rev. (2018) 19(11):1557–68. doi: 10.1111/obr.12725
56. Wolf LA, Perhats C, Delao AM, Clark PR. Workplace aggression as cause and effect: emergency nurses’ experiences of working fatigued. Int Emerg Nurs. (2017) 33:48–52. doi: 10.1016/j.ienj.2016.10.006
57. Wong K, Chan AHS, Ngan SC. The effect of long working hours and overtime on occupational health: a meta-analysis of evidence from 1998 to 2018. Int J Environ Res Public Health. (2019) 16:12. doi: 10.3390/ijerph16122102
58. Yinghui W, Fujita S, Seto K, Ito S, Matsumoto K, Huang C-C, et al. The impact of nurse working hours on patient safety culture: a cross-national survey including Japan, the United States and Chinese Taiwan using the hospital survey on patient safety culture. BMC Health Serv Res. (2013) 13:394. doi: 10.1186/1472-6963-13-394
59. Vogt J, Leonhardt J, Köper B, Pennig S. Human factors in safety and business management. Ergonomics. (2010) 53(2):149–63. doi: 10.1080/00140130903248801
60. Dawson D, Ian Noy Y, Härmä M, Åkerstedt T, Belenky G. Modelling fatigue and the use of fatigue models in work settings. Accid Anal Prev. (2011) 43(2):549–64. doi: 10.1016/j.aap.2009.12.030
61. Abe T, Mollicone D, Basner M, Dinges DF. Sleepiness and safety: where biology needs technology. Sleep Biol Rhythms. (2014) 12(2):74–84. doi: 10.1111/sbr.12067
62. Fan J, Smith A. Effects of occupational fatigue on cognitive performance of staff from a train operating company: a field study. Front Psychol (2020) 11:558520. doi: 10.3389/fpsyg.2020.558520
63. Williamson A, Lombardi DA, Folkard S, Stutts J, Courtney TK, Connor JL. The link between fatigue and safety. Accid Anal Prev. (2011) 43(2):498–515. doi: 10.1016/j.aap.2009.11.011
64. Dinges D. An overview of sleepiness and accidents. J Sleep Res. (1995) 4:4–14. doi: 10.1111/j.1365-2869.1995.tb00220.x
65. Zielinski MR, McKenna JT, McCarley RW. Functions and mechanisms of sleep. AIMS Neurosci. (2016) 3(1):67–104. doi: 10.3934/Neuroscience.2016.1.67
66. Liew SC, Aung T. Sleep deprivation and its association with diseases- a review. Sleep Med. (2021) 77:192–204. doi: 10.1016/j.sleep.2020.07.048
67. Roberts RE, Duong HT. The prospective association between sleep deprivation and depression among adolescents. Sleep. (2014) 37(2):239–44. doi: 10.5665/sleep.3388
68. Alaska Oil Spill Commission. Spill: The wreck of the Exxon (1990). Available online at: https://www.arlis.org/docs/vol1/EVOS/1990/21337991.pdf (retrieved June 27, 2023).
69. Mitler MM, Carskadon MA, Czeisler CA, Dement WC, Dinges DF, Graeber RC. Catastrophes, sleep, and public policy: consensus report. Sleep. (1988) 11(1):100–9. doi: 10.1093/sleep/11.1.100
70. Page A. editor. Keeping Patients Safe: Transforming the Work Environment of Nurses. Washington, DC: The National Academies Press (2004).
71. Canadian Institute for Health Information. Patient harm in Canadian hospitals? It does happen (2022). Available online at: https://www.cihi.ca/en/patient-harm-in-canadian-hospitals-it-does-happen (retrieved June 19, 2023).
72. Rodziewicz TL, Houseman B, Hipskind JE. Medical Error Reduction and Prevention. Treasure Island, FL: StatPearls Publishing (2023).
73. James S, Vila B. Police drowsy driving: predicting fatigue-related performance decay. Policing. (2015) 38(3):517–38. doi: 10.1108/PIJPSM-03-2015-0033
74. Lee ML, Howard ME, Horrey WJ, Liang Y, Anderson C, Shreeve MS, et al. High risk of near-crash driving events following night-shift work. Proc Natl Acad Sci U S A. (2016) 113(1):176–81. doi: 10.1073/pnas.1510383112
75. Shah MK, Gandrakota N, Cimiotti JP, Ghose N, Moore M, Ali MK. Prevalence of and factors associated with nurse burnout in the US. JAMA Netw Open. (2021) 4(2):e2036469. doi: 10.1001/jamanetworkopen.2020.36469
76. Stimpfel AW, Sloane DM, Aiken LH. The longer the shifts for hospital nurses, the higher the levels of burnout and patient dissatisfaction. Health Aff. (2012) 31(11):2501–9. doi: 10.1377/hlthaff.2011.1377
77. Baillien E, De Cuyper N, De Witte H. Job autonomy and workload as antecedents of workplace bullying: a two-wave test of Karasek's Job demand control model for targets and perpetrators. J Occup Organ Psychol. (2011) 84(1):191–208. doi: 10.1348/096317910X508371
78. Salin D, Hoel H. Organizational risk factors of workplace bullying. In: Einarsen SV, Hoel H, Zapf D, Cooper CL, editors. Bullying and Harassment in the Workplace: Theory, Research and Practice. Boca Raton: CRC Press (2020). p. 25.
79. Baldwin D, Daugherty S, Tsai R, Scotti MJ. A national survey of residents’ self-reported work hours: thinking beyond specialty. Acad Med. (2003) 78(11):1154–63. doi: 10.1097/00001888-200311000-00018
80. Rosta J, Gerber A. Excessive working hours and health complaints among hospital physicians: a study based on a national sample of hospital physicians in Germany. Ger Med Sci. (2007) 5:Doc09.19675717
81. Healy CM, McKay MF. Nursing stress: the effects of coping strategies and job satisfaction in a sample of Australian nurses. J Adv Nurs. (2000) 31(3):681–8. doi: 10.1046/j.1365-2648.2000.01323.x
82. Almost J, Wolff AC, Stewart-Pyne A, McCormick LG, Strachan D, D'Souza C. Managing and mitigating conflict in healthcare teams: an integrative review. J Adv Nurs. (2016) 72(7):1490–505. doi: 10.1111/jan.12903
83. Giorgi G, Mancuso S, Fiz Perez F, Castiello D'Antonio A, Mucci N, Cupelli V, et al. Bullying among nurses and its relationship with burnout and organizational climate. Int J Nurs Pract. (2016) 22(2):160–8. doi: 10.1111/ijn.12376
84. Notelaers G, De Witte H, Einarsen S. A job characteristics approach to explain workplace bullying. Eur J Work Org Psychol. (2010) 19(4):487–504. doi: 10.1080/13594320903007620
85. Caruso C. Negative impacts of shiftwork and long work hours. Rehabil Nurs. (2014) 39(1):16–25. doi: 10.1002/rnj.107
86. Akerstedt T. Psychological and psychophysiological effects of shift work. Scand J Work Environ Health. (1990) 16(Suppl 1):67–73. doi: 10.5271/sjweh.1819
87. Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American academy of sleep medicine and sleep research society. Sleep. (2015) 38(6):843–4. doi: 10.5665/sleep.4716
88. Stimpfel A, Fatehi F, Kovner C. Nurses’ sleep, work hours, and patient care quality, and safety. Sleep Health. (2020) 6(3):314–20. doi: 10.1016/j.sleh.2019.11.001
89. Rogers A. Nurses' work schedules, quality of care, and the health of the nurse workforce remain significant issues. Washington State Nurses Association (2019). Available online at: https://cdn.wsna.org/assets/entry-assets/3215/Nurses-work-schedules-quality-of-care-and-fatigue_200622_172628.pdf (retrieved June 14, 2023).
90. Afonso P, Fonseca M, Pires JF. Impact of working hours on sleep and mental health. Occup Med (Lond). (2017) 67(5):377–82. doi: 10.1093/occmed/kqx054
91. Erren TC, Falaturi P, Morfeld P, Knauth P, Reiter RJ, Piekarski C. Shift work and cancer: the evidence and the challenge. Dtsch Arztebl Int. (2010) 107(38):657–62. doi: 10.3238/arztebl.2010.0657
92. Antunes LC, Levandovski R, Dantas G, Caumo W, Hidalgo MP. Obesity and shift work: chronobiological aspects. Nutr Res Rev. (2010) 23(1):155–68. doi: 10.1017/s0954422410000016
93. Nakamura K, Shimai S, Kikuchi S, Takahashi H, Tanaka M, Nakano S, et al. Increases in body mass index and waist circumference as outcomes of working overtime. Occup Med (Lond). (1998) 48(3):169–73. doi: 10.1093/occmed/48.3.169
94. Spiegel K, Tasali E, Leproult R, Van Cauter E. Effects of poor and short sleep on glucose metabolism and obesity risk. Nat Rev Endocrinol. (2009) 5(5):253–61. doi: 10.1038/nrendo.2009.23
95. Harrington J. Health effects of shift work and extended hours of work. Occup Environ Med. (2001) 58(1):68. doi: 10.1136/oem.58.1.68
96. Åkerstedt T, Fredlund P, Gillberg M, Jansson B. Work load and work hours in relation to disturbed sleep and fatigue in a large representative sample. J Psychosom Res. (2002) 53(1):585–8. doi: 10.1016/S0022-3999(02)00447-6
97. Hulsegge G, Loef B, van Kerkhof LW, Roenneberg T, van der Beek AJ, Proper KI. Shift work, sleep disturbances and social jetlag in healthcare workers. J Sleep Res. (2019) 28(4):e12802. doi: 10.1111/jsr.12802
98. Dawson D, Reid K. Fatigue, alcohol and performance impairment. Nature. (1997) 388(6639):235. doi: 10.1038/40775
99. Namian M, Ghorbani Z, Taherpour F, Ghiasvand E, Karji A. Demystifying the impact of age on safety performance of construction workers: examining the mediating roles of experience and fatigue. Pract Period Struct Des Constr. (2022) 27(4). doi: 10.1061/(ASCE)SC.1943-5576.00007
100. Brighenti-Zogg S, Mundwiler J, Schüpbach U, Dieterle T, Wolfer DP, Leuppi JD, et al. Physical workload and work capacity across occupational groups. PLoS One. (2016) 11(5):e0154073. doi: 10.1371/journal.pone.0154073
101. Clendon J, Walker L. Nurses aged over 50 years and their experiences of shift work. J Nurs Manag. (2013) 21(7):903–13. doi: 10.1111/jonm.12157
102. Gander P, Briar C, Garden A, Purnell H, Woodward A. A gender-based analysis of work patterns, fatigue, and work/life balance among physicians in postgraduate training. Acad Med. (2010) 85(9):1526–36. doi: 10.1097/ACM.0b013e3181eabd06
103. Lecca R, Figorilli M, Casaglia E, Cucca C, Meloni F, Loscerbo R, et al. Gender and nightshift work: a cross sectional study on sleep quality and daytime somnolence. Brain Sci. (2023) 13(4):1–12. doi: 10.3390/brainsci13040607
104. Choi E, Choi KW, Jeong HG, Lee MS, Ko YH, Han C, et al. Long working hours and depressive symptoms: moderation by gender, income, and job status. J Affect Disord. (2021) 286:99–107. doi: 10.1016/j.jad.2021.03.001
105. Gilbert-Ouimet M, Ma H, Glazier R, Brisson C, Mustard C, Smith PM. Adverse effect of long work hours on incident diabetes in 7065 Ontario workers followed for 12 years. BMJ Open Diabetes Res Care. (2018) 6(1):e000496. doi: 10.1136/bmjdrc-2017-000496
106. Smith PM, Ibrahim-Dost J, Keegel T, MacFarlane E. Gender differences in the relationship between shiftwork and work injury: examining the influence of dependent children. J Occup Environ Med. (2013) 55(8):932–6. doi: 10.1097/JOM.0b013e31829178e1
107. Wirtz A, Lombardi DA, Willetts JL, Folkard S, Christiani DC. Gender differences in the effect of weekly working hours on occupational injury risk in the United States working population. Scand J Work Environ Health. (2012) 38(4):349–57. doi: 10.5271/sjweh.3295
108. Caruso C, Bushnell T, Eggerth D, Heitmann A, Kojola B, Newman K, et al. Long working hours, safety, and health: toward a national research agenda. Am J Ind Med. (2006) 49(11):930–42. doi: 10.1002/ajim.20373
109. Smolensky MH, Di Milia L, Ohayon MM, Philip P. Sleep disorders, medical conditions, and road accident risk. Accid Anal Prev. (2011) 43(2):533–48. doi: 10.1016/j.aap.2009.12.004
110. Branchard B, Deb-Rinker P, Dubois A, Lapointe P, O'Donnell S, Pelletier L, et al. At-a-glance—how healthy are Canadians? A brief update. Health Promot Chronic Dis Prev Can. (2018) 38(10):385–7. doi: 10.24095/hpcdp.38.10.05
111. Manodpitipong A, Saetung S, Nimitphong H, Siwasaranond N, Wongphan T, Sornsiriwong C, et al. Night-shift work is associated with poorer glycaemic control in patients with type 2 diabetes. J Sleep Res. (2017) 26(6):764–72. doi: 10.1111/jsr.12554
112. Costa G, Lievore F, Casaletti G, Gaffuri E, Folkard S. Circadian characteristics influencing interindividual differences in tolerance and adjustment to shiftwork. Ergonomics. (1989) 32(4):373–85. doi: 10.1080/00140138908966104
113. Bannai A, Tamakoshi A. The association between long working hours and health: a systematic review of epidemiological evidence. Scand J Work Environ Health. (2014) 40(1):5–18. doi: 10.5271/sjweh.3388
114. Härmä M. Workhours in relation to work stress, recovery and health. Scand J Work Environ Health. (2006) 32(6):502–14. doi: 10.5271/sjweh.1055
115. Mohamed BES, Ghaith RFAH, Ahmed HAA. Relationship between work–family conflict, sleep quality, and depressive symptoms among mental health nurses. Middle East Curr Psychiatry. (2022) 29(1):19. doi: 10.1186/s43045-022-00183-3
116. Berkman LF, Liu SY, Hammer L, Moen P, Klein LC, Kelly E, et al. Work–family conflict, cardiometabolic risk, and sleep duration in nursing employees. J Occup Health Psychol. (2015) 20(4):420–33. doi: 10.1037/a0039143
117. Zhang Y, Punnett L, Nannini A. Work-family conflict, sleep, and mental health of nursing assistants working in nursing homes. Workplace Health Saf. (2016) 65(7):295–303. doi: 10.1177/2165079916665397
118. Gifkins J, Johnston A, Loudoun R, Troth A. Fatigue and recovery in shiftworking nurses: a scoping literature review. Int J Nurs Stud. (2020) 112:103710. doi: 10.1016/j.ijnurstu.2020.103710
119. Ross A, Geiger-Brown J, Yang L, Flynn S, Cox R, Wehrlen L, et al. Acute and chronic fatigue in nurses providing direct patient care and in non-direct care roles: a cross-sectional analysis. Nurs Health Sci. (2021) 23(3):628–38. doi: 10.1111/nhs.12862
120. Sluiter JK, de Croon EM, Meijman TF, Frings-Dresen MHW. Need for recovery from work related fatigue and its role in the development and prediction of subjective health complaints. Occup Environ Med. (2003) 60:i62–70. doi: 10.1136/oem.60.suppl_1.i62
121. Barker LM, Nussbaum MA. Fatigue, performance and the work environment: a survey of registered nurses. J Adv Nurs. (2011) 67(6):1370–82. doi: 10.1111/j.1365-2648.2010.05597.x
122. Cochran KR. An examination of work characteristics, fatigue, and recovery among acute care nurses. J Nurs Adm. (2021) 51(2):89–94. doi: 10.1097/NNA.0000000000000975
123. Wu Y, Jiang F, Ma J, Tang YL, Wang M, Liu Y. Experience of medical disputes, medical disturbances, verbal and physical violence, and burnout among physicians in China. Front Psychol. (2020) 11:556517. doi: 10.3389/fpsyg.2020.556517
124. Steege LM, Pinekenstein BJ, Rainbow JG, Arsenault Knudsen É. Addressing occupational fatigue in nurses: current state of fatigue risk management in hospitals, part 2. J Nurs Adm. (2017) 47(10):484–90. doi: 10.1097/nna.0000000000000519
125. Karhula K, Härmä M, Sallinen M, Hublin C, Virkkala J, Kivimäki M, et al. Association of job strain with working hours, shift-dependent perceived workload, sleepiness and recovery. Ergonomics. (2013) 56(11):1640–51. doi: 10.1080/00140139.2013.837514
126. Vedaa Ø, Mørland E, Larsen M, Harris A, Erevik E, Sivertsen B, et al. Sleep detriments associated with quick returns in rotating shift work: a diary study. J Occup Environ Med. (2017) 59(6):522–7. doi: 10.1097/jom.0000000000001006
127. Lombardi DA, Jin K, Courtney TK, Arlinghaus A, Folkard S, Liang Y, et al. The effects of rest breaks, work shift start time, and sleep on the onset of severe injury among workers in the People's Republic of China. Scand J Work Environ Health. (2014) 40(2):146–55. doi: 10.5271/sjweh.3395
128. Tucker P. The impact of rest breaks upon accident risk, fatigue and performance: a review. Work Stress. (2003) 17:123–37. doi: 10.1080/0267837031000155949
130. Transport Canada. Duty and rest periods for railway operating employees. In G. o. Canada (Ed.) (2023).
131. Canadian Nuclear Safety Commission. REGDOC-2.2.4. In Fitness for Duty: Managing Worker Fatigue (2023).
132. Government of Canada. Canadian Aviation Regulations (SOR/96-433). In Commercial Air Services, Maximum Number of Hours of Work—700.29 (2023).
133. Dussault C, Saad N, Carrier J. 16-hour Call duty schedules: the Quebec experience. BMC Med Educ. (2014) 14(1):S10. doi: 10.1186/1472-6920-14-S1-S10
134. Pattani R, Wu PE, Dhalla IA. Resident duty hours in Canada: past, present and future. CMAJ. (2014) 186(10):761–5. doi: 10.1503/cmaj.131053
136. Burchiel KJ, Zetterman RK, Ludmerer KM, Philibert I, Brigham TP, Malloy K, et al. The 2017 ACGME common work hour standards: promoting physician learning and professional development in a safe, humane environment. J Grad Med Educ. (2017) 9(6):692–6. doi: 10.4300/jgme-d-17-00317.1
138. Bae S-H, Brewer CS, Kovner CT. State mandatory overtime regulations and newly licensed nurses’ mandatory and voluntary overtime and total work hours. Nurs Outlook. (2012) 60(2):60–71. doi: 10.1016/j.outlook.2011.06.006
139. Bae SH, Yoon J. Impact of states’ nurse work hour regulations on overtime practices and work hours among registered nurses. Health Serv Res. (2014) 49(5):1638–58. doi: 10.1111/1475-6773.12179
140. Government of the United Kingdom. European Working Time Directive Regulations. In D. o. Health (Ed.) (2023).
141. Cooper AL, Brown JA, Leslie GD. Nurse resilience for clinical practice: an integrative review. J Adv Nurs. (2021) 77(6):2623–40. doi: 10.1111/jan.14763
142. De Raeve J, van den Brandt V, Kant . Risk factors for interpersonal conflicts at work. Scand J Work Environ Health. (2008) 34(2):96–106. doi: 10.5271/sjweh.1223
143. Dembe A, Erickson J, Delbos R, Banks S. The impact of overtime and long work hours on occupational injuries and illnesses: new evidence from the United States. Occup Environ Med. (2005) 62(9):588–97. doi: 10.1136/oem.2004.016667
144. McCormick F, Kadzielski J, Landrigan C, Evans B, Herndon J, Rubash H. Surgeon fatigue: a prospective analysis of the incidence, risk, and intervals of predicted fatigue-related impairment in residents. Arch Surg. (2012) 147(5):430–5. doi: 10.1001/archsurg.2012.84
Keywords: nursing, health care, long work hours, shift work, occupational fatigue, occupational health risk factors, safety-sensitive work
Citation: Scott-Marshall HK (2024) Safe limits on work hours for the nursing profession: a rapid evidence review. Front. Glob. Womens Health 5:1455422. doi: 10.3389/fgwh.2024.1455422
Received: 26 June 2024; Accepted: 7 October 2024;
Published: 31 October 2024.
Edited by:
Anju Devianee Keetharuth, The University of Sheffield, United KingdomReviewed by:
Ashlesha Bagadia, The Green Oak Initiative, IndiaJaqui Long, The University of Sheffield, United Kingdom
Copyright: © 2024 Scott-Marshall. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Heather Katherine Scott-Marshall, aGVhdGhlci5zY290dEB1dG9yb250by5jYQ==
 Heather Katherine Scott-Marshall
Heather Katherine Scott-Marshall