- Department of Public Health, College of Medical and Health Science, Samara University, Semera, Ethiopia
Background: Coronavirus Disease-19 pandemic had an adverse impact on the mental health of the public worldwide, but the problem is worst among pregnant women due to social distancing policies and mandatory lockdown, including prenatal care services. As a result, the prevalence of depression and anxiety could increase during the pandemic, particularly among pregnant women. Thus, the purpose of this review is to determine the magnitude of depression and anxiety and contributing factors among pregnant women during the pandemic in Ethiopia.
Methods: Web of Science, Since Direct, PubMed, Google Scholar, and African Journals Online were the electronic databases searched, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines were followed in this review. The Newcastle-Ottawa Critical Appraisal Checklist was used to assess the quality of the included studies. A predefined data extraction sheet developed in Excel was used to extract the data. The pooled prevalence of anxiety and depression was determined by a random effect model meta-analysis.
Results: 4,269 and 1,672 pregnant women were involved in depression and anxiety studies, respectively. The pooled prevalence of depression and anxiety among pregnant women during the COVID-19 pandemic in Ethiopia was 24.7% (95% CI: 18.52–30.87) and 35.19% (95% CI: 26.83–43.55), respectively. Single marital status (AOR = 2.22, 95% CI: 1.07–3.37), poor social support (AOR = 2.7, 95% CI: 1.06–4.35), unplanned pregnancies (AOR = 2.17, 95% CI: 1.34–3.0), and unsatisfied marital status (AOR = 2.16, 95% CI: 1.17–3.14) were risk factors for depression. Violence against intimate partners (AOR = 2.87, 95% CI: 1.97–3.77) and poor social support (AOR = 1.98, 95% CI: 1.24–2.71) were risk factors for anxiety.
Conclusion: One-fourth and nearly one-third of pregnant women had depression and anxiety, respectively, during COVID-19 pandemic in Ethiopia. Single or unsatisfied marital status and unplanned pregnancies were risk factors for depression. Poor social support was significantly associated with depression and anxiety. Pregnant women who experienced violence against intimate partners had higher anxiety. After COVID-19 pandemic, mental health interventions are essential for reducing depression and anxiety.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=527148, PROSPERO (CRD42024527148).
Background
Mental health is one of the major health indicators that contribute to significant morbidity (1). The most common forms of mental illness are anxiety and depression disorders, which are highly comorbid and together include the more general heading of internalizing disorders (2). Since the onset of Coronavirus Disease-19 (COVID-19) pandemic, the mental health of people has been negatively affected, especially those from vulnerable groups (3). Globally, the prevalence of depression was 32.60% for pregnant and postpartum women during COVID-19 pandemic. The rate was 31.5% for pregnant women and 27.64% for postpartum women (4). The pooled prevalence of depression and anxiety in pregnancy during COVID-19 pandemic was 25.6% and 30.5%, respectively (5). The prevalence of antenatal depression in Africa was 26.3% (6). In Kenya, depression and anxiety were 16.2% and 6.6% among pregnant women, respectively (7). In Ethiopia, the prevalence of depression ranged from 21.3% to 27.9% (8–10). Among pregnant and lactating mothers in Ethiopia, the pooled prevalence of anxiety and depression during COVID-19 pandemic were 33% and 27%, respectively (11).
Financial problem was associated with depressive and anxiety disorder (12). In low-income countries, anxiety disorder was high (13). Lifting people out of poverty improved mental health problems (14). Increased social distance was associated with increased symptoms of anxiety (15). Cultural differences exist in anxiety disorders (16). A person's social concerns need to be considered in light of their cultural, racial, and ethnic background in order to adequately assess the degree and expression of social anxiety as well as its impact on anxiety (17). Low social support was a risk factor for depression, anxiety, and self-harm during pregnancy (18). Genetics, social networks, societal levels, and adverse childhood experiences were risk factors for depression (19).
Understanding the effect of COVID-19 pandemic on psychological changes in pregnant women is essential to preventing its negative impacts and unexpected consequences (4). It is evident that depression, anxiety, and associated risk factors among pregnant women were not examined at the national level during COVID-19 pandemic in Ethiopia. The aim of the current study was therefore to determine the pooled prevalence of depression and anxiety among pregnant women during COVID-19 pandemic in Ethiopia. The present study was the first to examine the depression and anxiety experienced by pregnant women during COVID-19 pandemic at the national level in Ethiopia.
Methods
Reporting and registration
This study was registered in PROSPERO with an ID of CRD42024527148. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines were followed to report this review (20) (Supplementary File S1).
Searching strategies
Search strategy
A comprehensive electronic search of studies was carried out on the databases of Web of Science, Science Direct, PubMed, Google Scholar, and African journals online from June 4 to 17, 2024. The search strategies were then updated from November 5 to 10, 2024. For PubMed, the MeSH terms used were depression, anxiety, “pregnant women,” and Ethiopia. Database-specific subject headings were used for the other electronic databases that were linked to the terms and keywords listed in PubMed. For additional studies, references to relevant studies were searched. The search was restricted from the publication years of January 1, 2020, until June 17, 2024, with consideration of the onset of the COVID-19 pandemic. The details of the search strategies were provided in the Supplementary File (Supplementary File S2).
Eligible criteria
The inclusion criteria were as follows:
• Study design: observational studies
• Study type: both published and unpublished
• Study population: pregnant women
• Language: articles published in English
• Outcome: studies that reported either the prevalence of depression or anxiety or studies that have enough data to calculate the percentage of depression and anxiety.
• Study site and period: studies conducted in Ethiopia from January 1, 2020, to June 18, 2024.
The exclusion criteria were as follows:
• Studies dealing with depressive or anxiety disorders in nonpregnant women, such as postpartum periods.
• Studies conducted on HIV-positive pregnant women were excluded because HIV-positive women are a psychologically different target population from pregnant women without HIV-positive.
• Studies deal with generalized anxiety among pregnant women because generalized anxiety is characterized by chronic and persistent worry (21), which is different from normal anxiety that is usually short-term and related to a stressor response to some event.
• Studies without a clear outcome
• Qualitative studies, editorials, letters, reviews, commentaries, and interventional studies were excluded.
Outcome measurement
The primary outcome of this review was to determine the pooled prevalence of depression and anxiety during the COVID-19 pandemic in pregnant women using primary study data. Two parameters were required from primary studies to calculate the prevalence of depression and anxiety: the number of pregnant women with depression and anxiety as well as the total sample sizes. The prevalence was calculated by dividing the total number of pregnant women with depression by the total sample size, and the prevalence for anxiety was calculated by dividing the total number of pregnant women with anxiety by the total sample size and multiplying them by 100.
Study selection
Endnote X8.1 software was used to remove duplicate studies. Then two authors (TGW and MW) independently screened the article title and abstract. The full-text articles were retrieved after the screening of titles and abstracts. Two authors (TGW and MW) further evaluated the full-text article's eligibility for final inclusion. Disagreements were settled through dialogue and scientific consensus between the two authors (TGW and MW).
Data extraction process
A standardized data extraction checklist was developed using Microsoft Excel. The data were extracted independently by two authors (TGW and MW). Name of the first author, study year, study region, study subjects, sample size, diagnostic tools, cases with anxiety and depression, and prevalence of anxiety and depression were the extracted data. There were no discrepancies between the two authors during data extraction. The extracted data were cross-checked interchangeably by the two authors (TGW and MW). The details of data extraction were provided in the Supplementary File (Supplementary File S3).
Quality assessment of studies
Critical appraisal was carried out in the included studies by two authors (TGW and MW) independently using the Newcastle Ottawa Critical Appraisal Checklist for adapted cross sectional studies (22). Discussion and scientific consensus were used to settle disagreements between the two authors. The tool consists of three domains: selection with a maximum of 5 points (representativeness of sample*, sample size justification*, non-respondents*, ascertainment of exposure**), comparability with a maximum of 2 points (confounding control**), and outcome assessment with a maximum of 3 points (independent outcome assessment** and statistical test*). The scores were summed up and changed to percentages. When the scores were added up, the minimum score was zero and the maximum score was 10. In this systematic review, studies with quality scores higher than 50% were included.
Data synthesis and statistical analysis
The relevant information from each original study was extracted using a predefined spreadsheet format developed from Microsoft Excel. Then the data were imported into STATA 15 statistical software for analysis. The random effect model meta-analysis was used to measure the pooled estimates due to the existence of heterogeneity (23). The pooled prevalence of depression and anxiety was computed. The heterogeneity of effect size was examined using the Q statistic and the I2 statistic (24). The Q-test determines whether the observed effect size is significantly different from one another than expected by chance. The I2 values of 0, 25%, 50%, and 75% were interpreted as no, low, medium, and high heterogeneity, respectively. Significant heterogeneity was taken into account in the current meta-analysis when the I2 value was greater or equal to 50%, with p-value <0.05. Sensitivity and sub-group analyses were used to investigate potential sources of heterogeneity (25). To identify associated factors, the pooled effect was computed from odds ratios. The results of the meta-analysis were presented in forest plots and tables with the support of a written explanation.
Ethics statement
Ethical approval was not required for this study since it only uses data from published studies.
Results
Search results
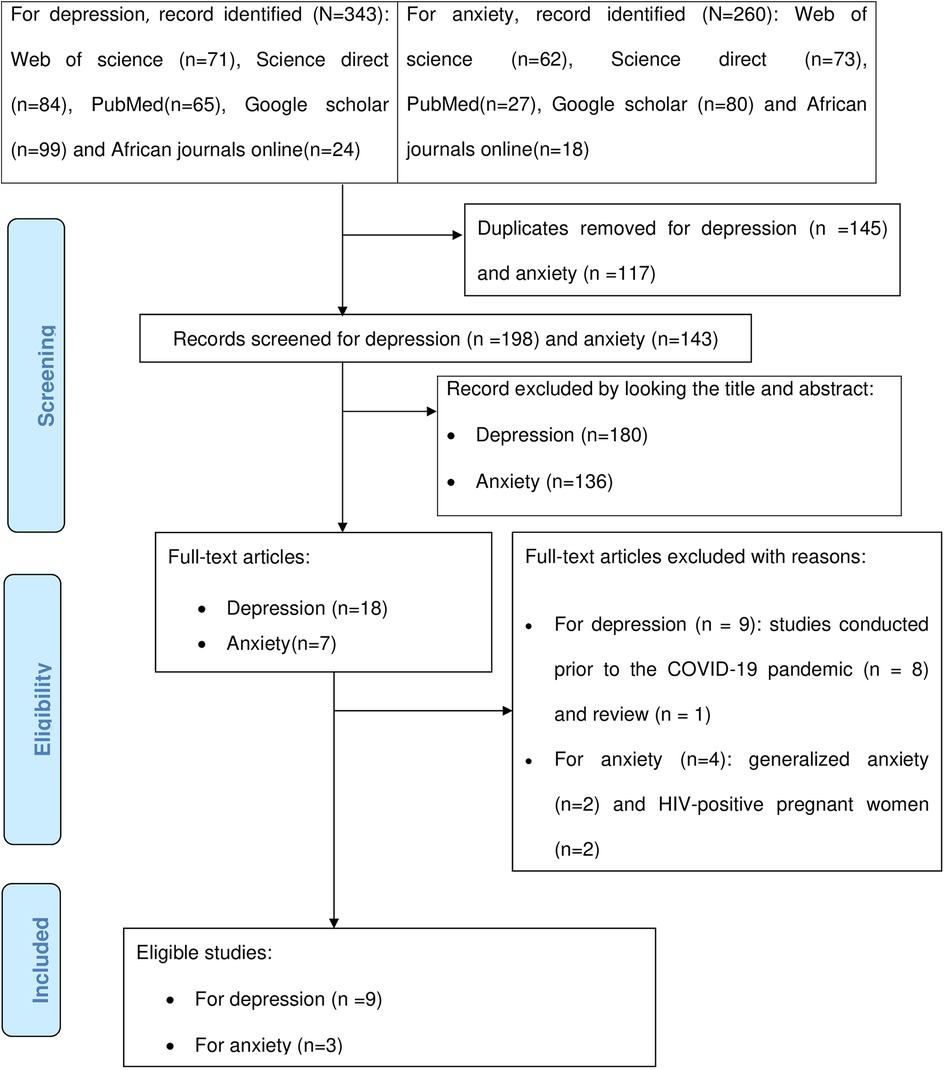
For the initial search, a total of 343 and 260 articles were retrieved for depression and anxiety, respectively. About 145 and 117 duplicate articles were removed for depression and anxiety, respectively. Irrelevant articles excluded based on abstracts and titles for depression and anxiety were 180 and 136, respectively. We excluded nine full-text articles on depression based on the following criteria: Eight studies were done before the COVID-19 pandemic, and one study was a review. Four full-text articles on anxiety were excluded for the following reasons: Two were generalized anxiety and two on HIV-positive pregnant women. Finally, nine eligible studies were found for depression, and three eligible studies were found for anxiety (Figure 1).
Study characteristics
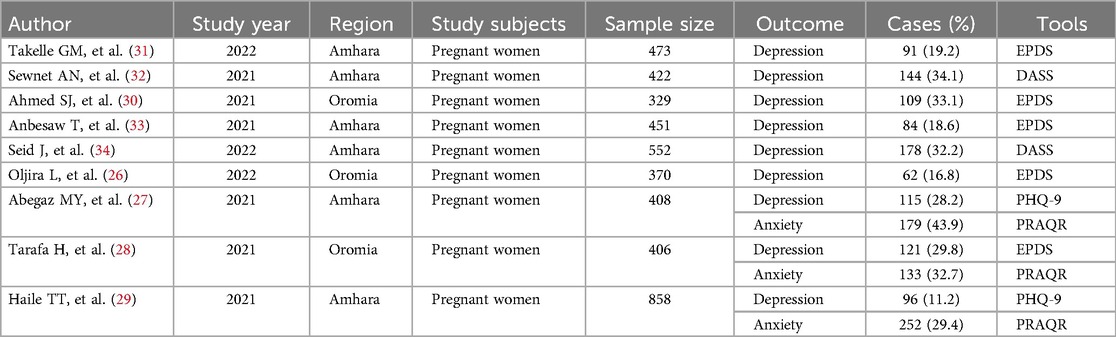
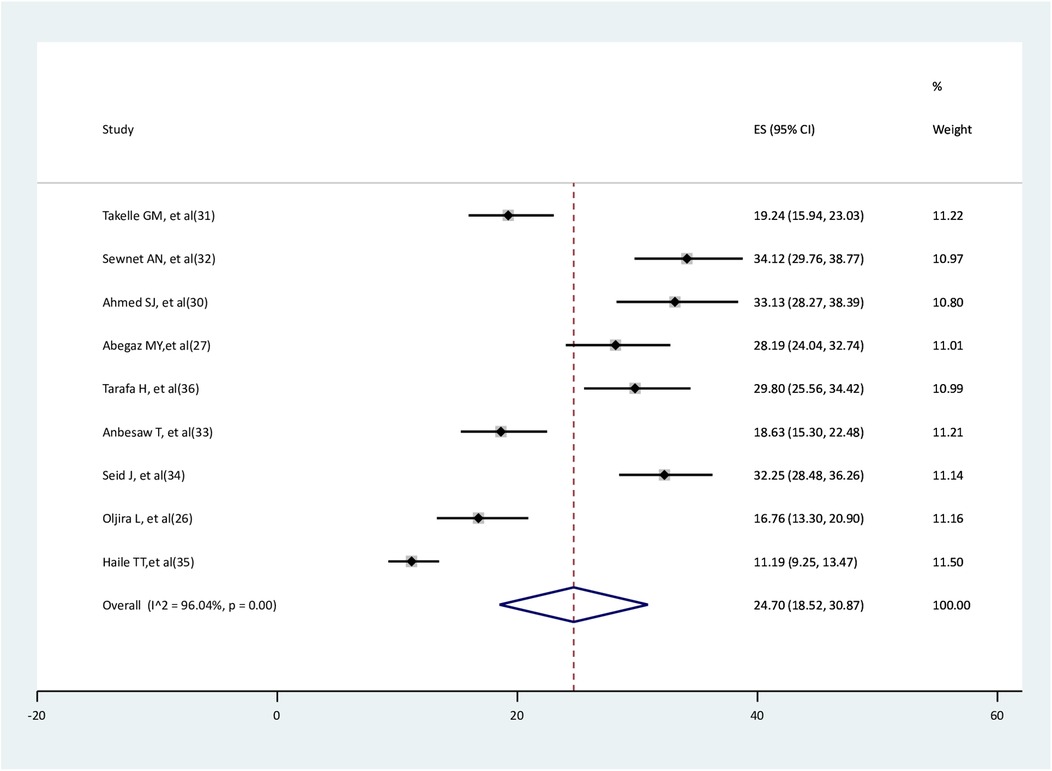
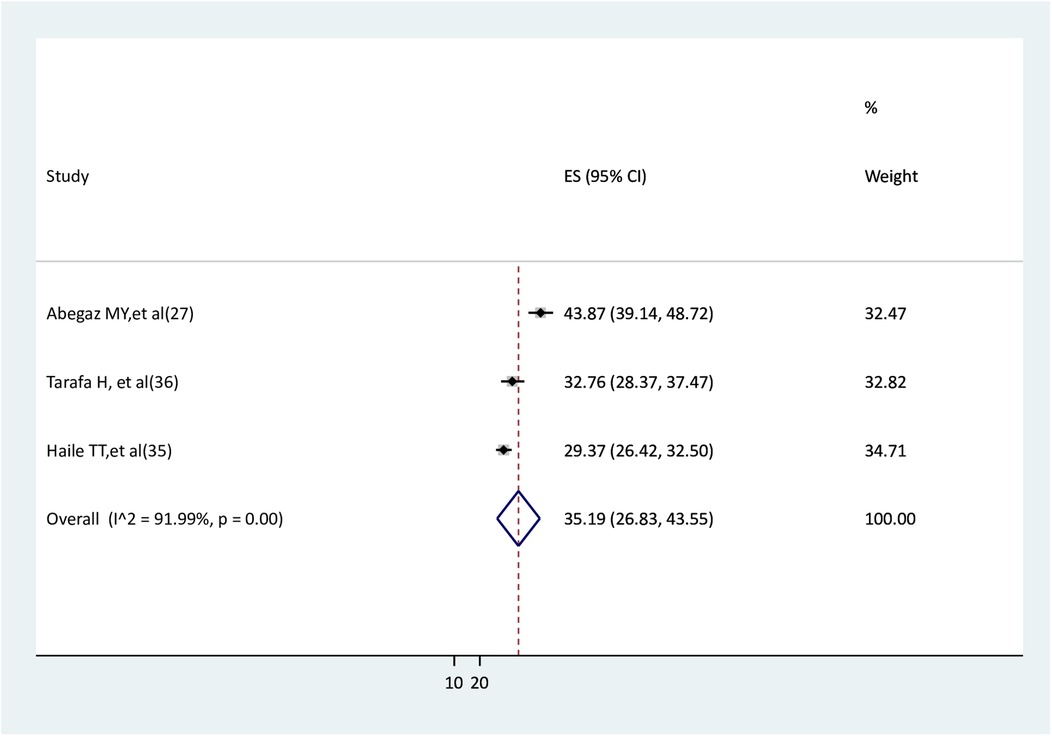
Nine studies were found, with all of them providing data on depression. Three studies simultaneously reported both depression and anxiety (26–29), and the remaining six studies recorded only depression (30–34). In the Amhara and Oromia regions, six and three studies were conducted, respectively. All the included studies were cross-sectional studies. Six out of eight studies were carried out in 2021. The largest sample size was 858 in a study reporting data on both depression and anxiety (29). For depression, the smallest sample sizes were 329 (30). The minimum prevalence of depression and anxiety were 11.2% and 29.4% (29), respectively. The maximum prevalence of depression and anxiety was 34.1% (32) and 50.3% (27) respectively. Five studies measured depression using EPDS. Three studies used PRAQR to measure anxiety (Table 1).
Quality of included studies
Two reviewers (TGW and MW) assessed the quality of the included studies using the Newcastle Ottawa Critical Appraisal Checklist for adapted cross-sectional studies. Any disagreements between the two authors were resolved through dialog and scientific consensus. For depression, three studies were scored 7 out of 10 (70%), while the remaining six studies scored 10 out of 10 (100%). For anxiety, all of the included studies scored 10 out of 10 (100%). Thus, in both outcomes, all of the included studies score above 50% and were included in the final meta-analysis (Supplementary File S4).
Pooled prevalence of depression among pregnant women after the onset of COVID-19 pandemic
In this systematic review, 4,269 pregnant women were involved; of them, 1,000 had depression. According to the random effect model meta-analysis, the pooled prevalence of depression among pregnant women was 24.7% (95%CI: 18.52–30.87), with the existence of high heterogeneity (I2 = 96.04%, p < 0.001) (Figure 2).
Pooled prevalence of anxiety among pregnant women after the onset of COVID-19 pandemic
In this review, 1,672 pregnant women were involved; of them, 564 had anxiety. The random effect model meta-analysis revealed that the pooled prevalence of anxiety among pregnant women was 35.19% (95%CI: 26.83–43.55), and high heterogeneity was observed between studies (I2 = 91.99%, p < 0.001) (Figure 3).
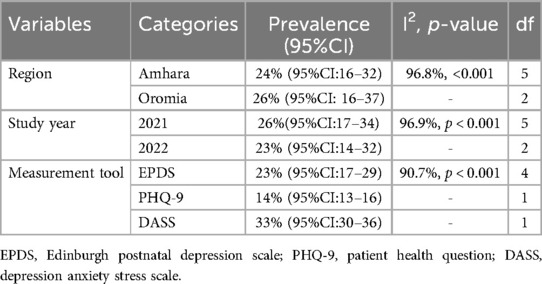
Subgroup analysis for pooled prevalence of depression
Subgroup analysis based on regions, study year, and measurement tools was conducted for the pooled prevalence of depression. The prevalence of depression in the Oromia and Amhara regions was 26% (95%CI: 16–37) and 24% (95%CI: 16–32), respectively. The pooled prevalence of depression in 2021 and 2022 was 26% (95% CI: 17–34) and 23% (95% CI: 14–32), respectively. The prevalence of depression was 14% (95% CI: 13–16), 23% (95% CI: 17–29), and 33% (95% CI: 30–36) using measurement tools of PHQ-9, EPDS, and DASS, respectively (Table 2).
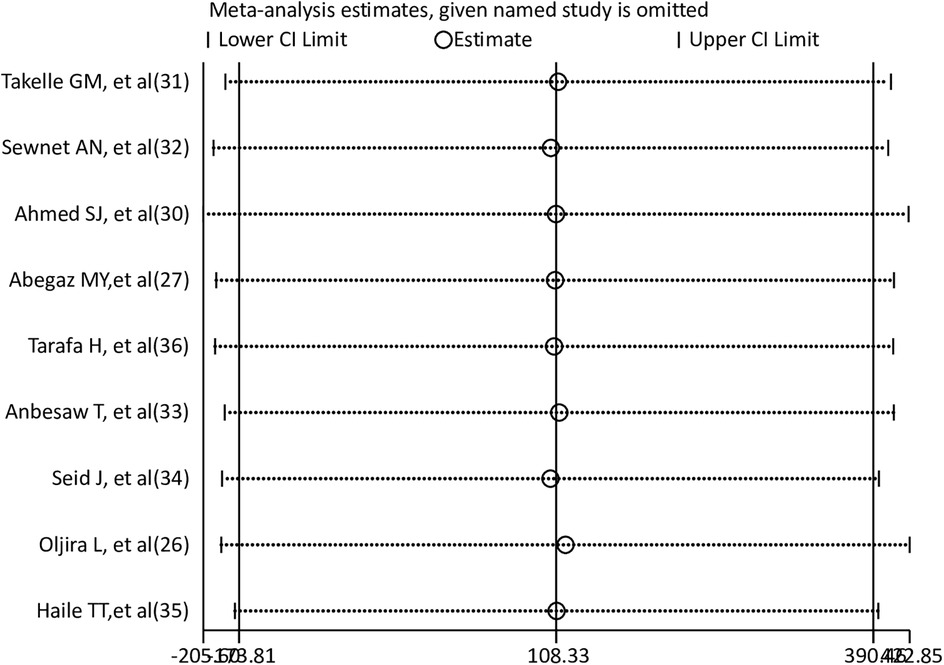
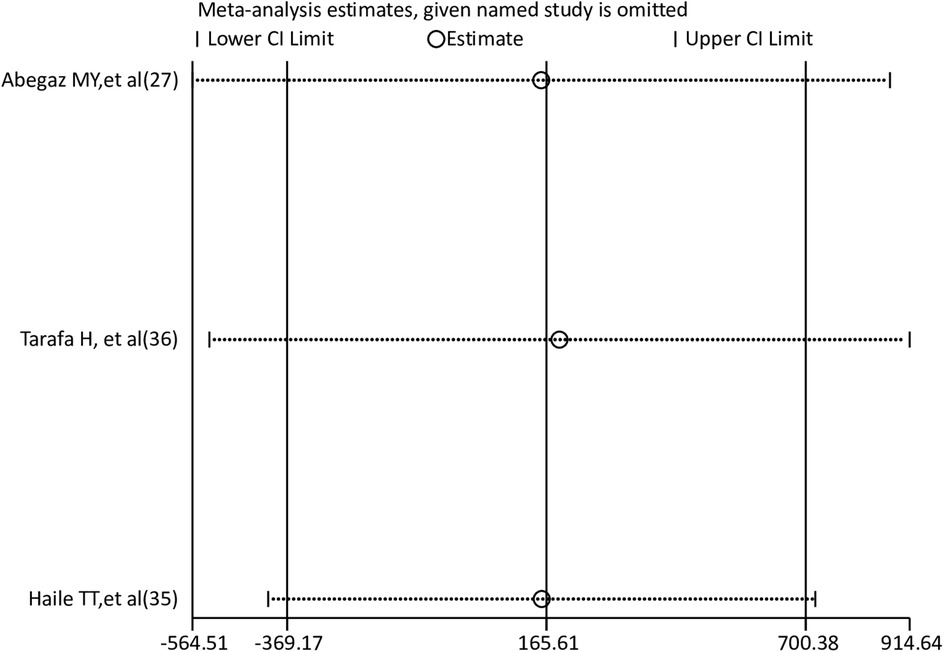
Sensitivity analysis
To find the effect of a single study on the pooled prevalence of anxiety and depression among pregnant women, a leave-one-out sensitivity analysis was carried out. The results of the sensitivity analysis showed that the findings for both depression and anxiety were robust and independent of a single study. The sensitivity analysis results were fairly stable or consistent for depression (Figure 4) and anxiety (Figure 5).
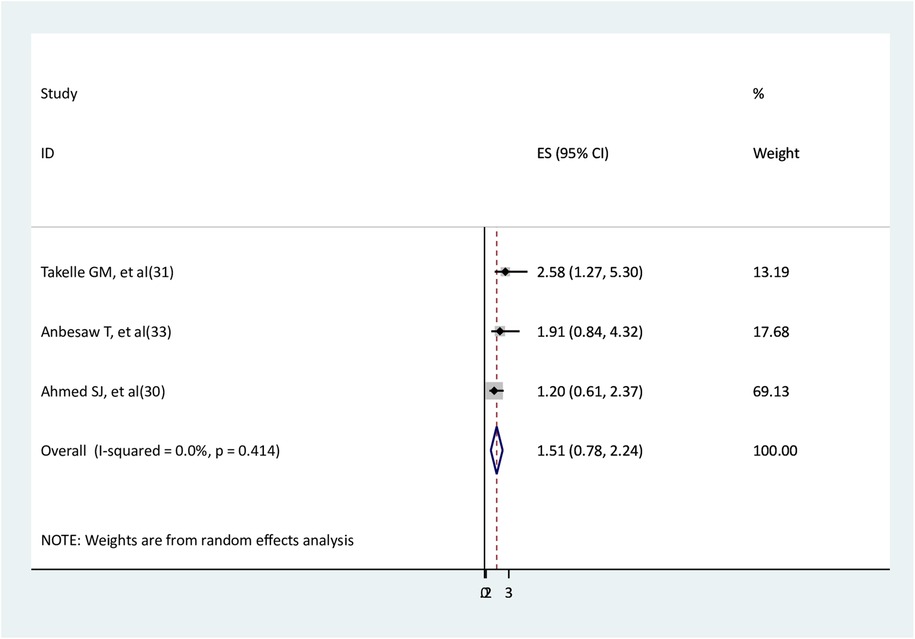
Risk factors for depression
The association between residence and depression
Three studies (30, 31, 33) were used to assess the association between residence and depression. The findings of one study (31) showed a statistically significant association, whereas the findings of the other two studies (30, 33) revealed no significant association. The results of the meta-analysis indicated that no significant association was observed between being a rural resident and depression (AOR = 1.51, 95% CI: 0.78–2.24) with no heterogeneity (Figure 6).
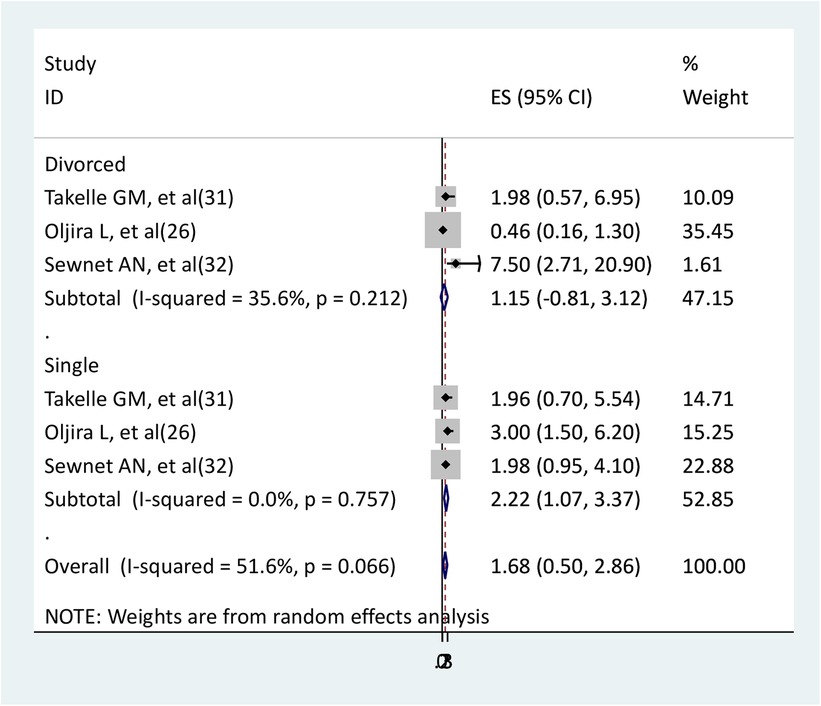
The association between marital status and depression
The relationship between marital status and depression was determined using three studies (26, 31, 32). In the relationship between divorced pregnant women and depression, two studies (26, 31) did not show statistically significant association, but one study showed significant (32). In the relationship between single marital status and depression, one study showed a significant association (26), but two studies did not show (31, 32). The findings of the meta-analysis showed that single pregnant women had higher depression than married pregnant women (AOR = 2.22, 95% CI: 1.07–3.37). However, divorced pregnant women did not have a significant association with depression compared to married pregnant women (AOR = 1.15, 95CI:-0.81–3.12) (Figure 7).
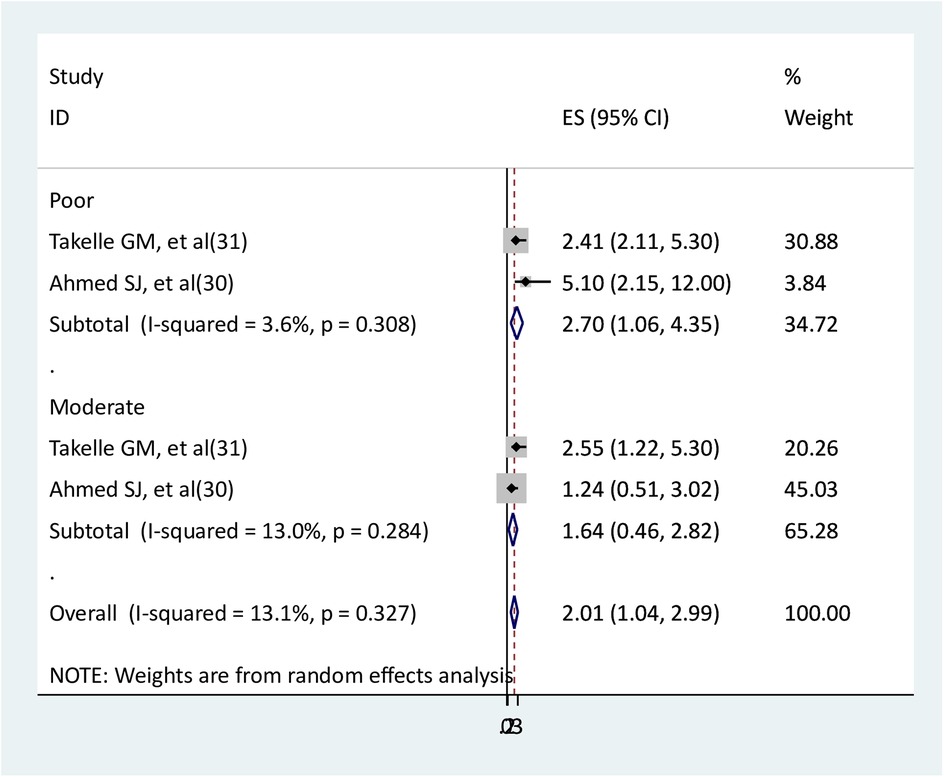
The association between social support and depression
Two studies were used to evaluate the relationship between depression and social support (30, 31). Two studies that examined the relationship between depression and poor social support found statistically significant results. One study found statistical significance (31) in the relationship between depression and moderate social support, whereas the other found no statistical significance (30). The results of meta-analysis showed that pregnant women with poor social support had 2.7 times higher rates of depression than pregnant women with strong social support (AOR = 2.7, 95% CI: 1.06–4.35); however, pregnant women with moderate social support did not have a significant association with depression (AOR = 1.64, 95% CI: 0.46–2.82). Low heterogeneities between studies were observed in both poor and moderate social support (Figure 8).
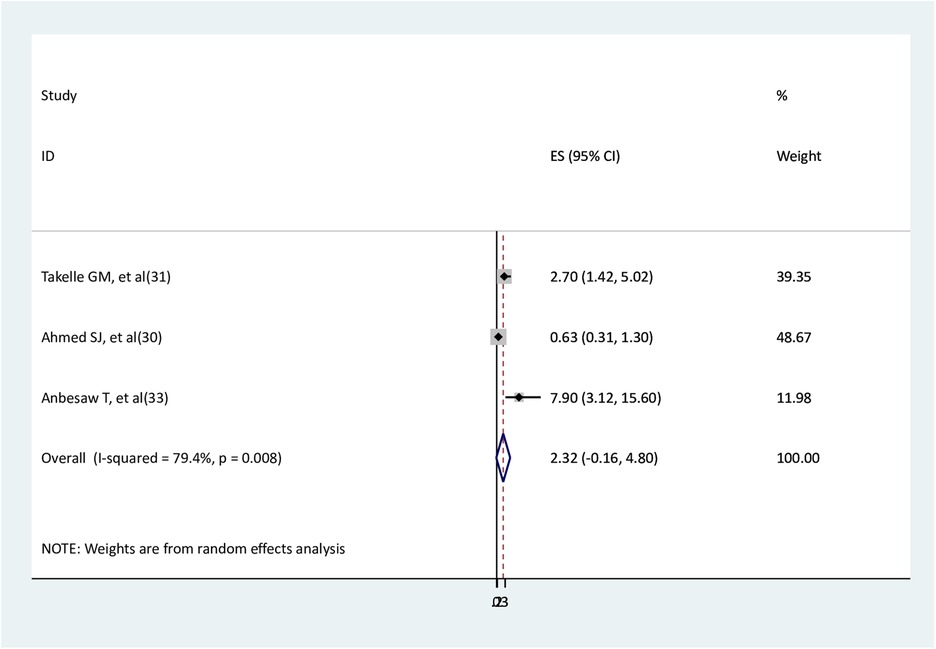
The association between intimate partner violence and depression
Three studies (30, 31, 33) were used to assess the association between intimate partners and depression. Two studies (31, 33) found a statistical association, and the other one did not show a significant association (30). The findings of the meta-analysis revealed no significant association between intimate partner violence and depression (AOR = 2.32, 95% CI: −0.16–4.8), with substantial heterogeneity between the studies (Figure 9).
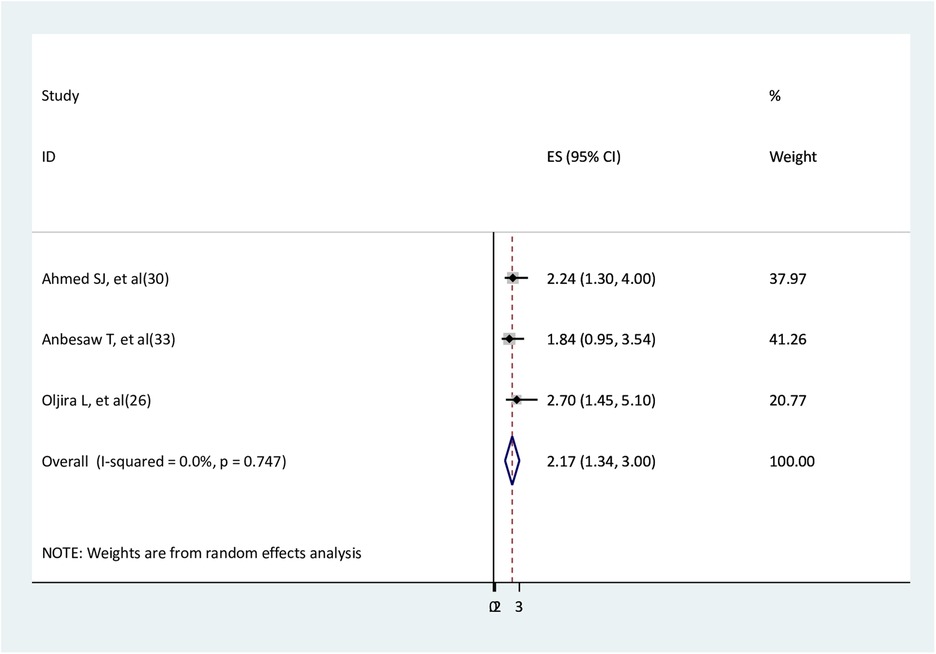
The association between unplanned pregnancy and depression
The association between unplanned pregnancy and depression was determined using three studies (26, 30, 33). Two studies (26, 30) reported significant associations, and one study (31) reported a non-significant association. Women without planned pregnancies had 2.2 times higher depression than women with planned pregnancies (AOR = 2.17, 95% CI: 1.34–3.0) (Figure 10).
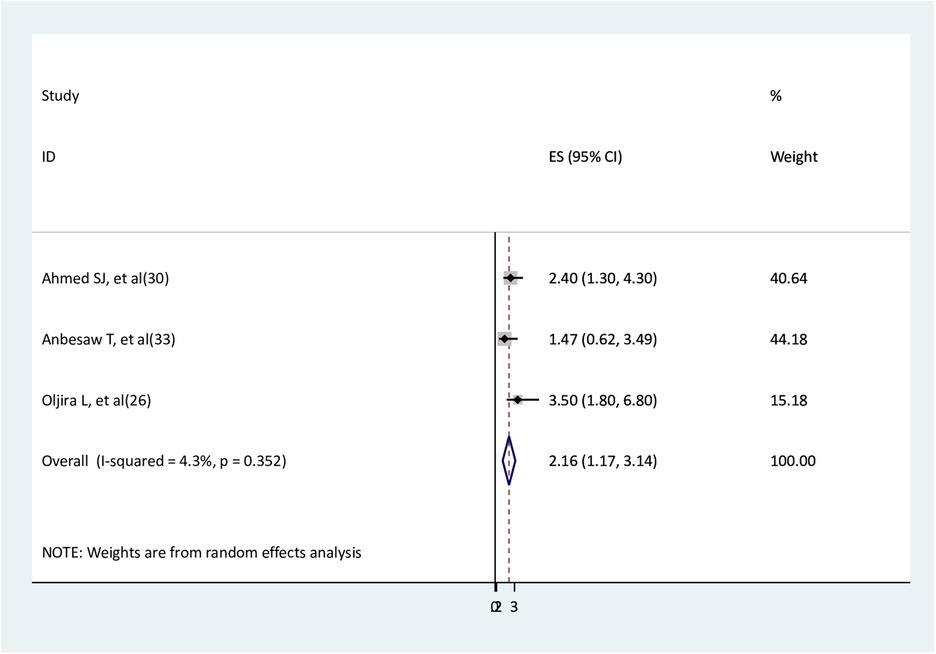
The association between unsatisfied marital status and depression
Three studies (26, 30, 33) were used to assess the relationship between unsatisfied marital status and depression. The findings of two studies (26, 30) showed significant association, while the findings of one study (33) did not show. The findings of the meta-analysis revealed that pregnant women with unsatisfied marital status had two times higher depression than pregnant women with satisfied marital status (AOR = 2.16, 95% CI: 1.17–3.14) (Figure 11).
Risk factors for anxiety
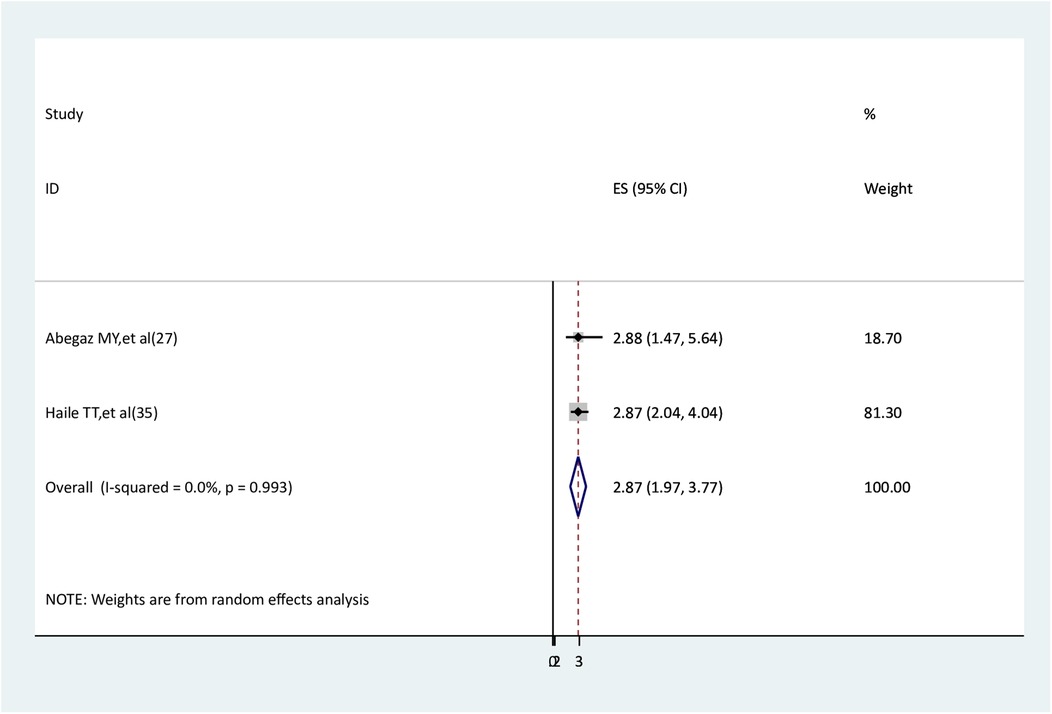
The association between intimate partner violence and anxiety
The association between intimate partner violence and anxiety was examined by two studies (27, 29). Both studies found a statistically significant association. The findings of the meta-analysis showed that pregnant women who experienced intimate partner violence had higher anxiety than pregnant women who did not (AOR = 2.87, 95% CI: 1.97–3.77) (Figure 12).
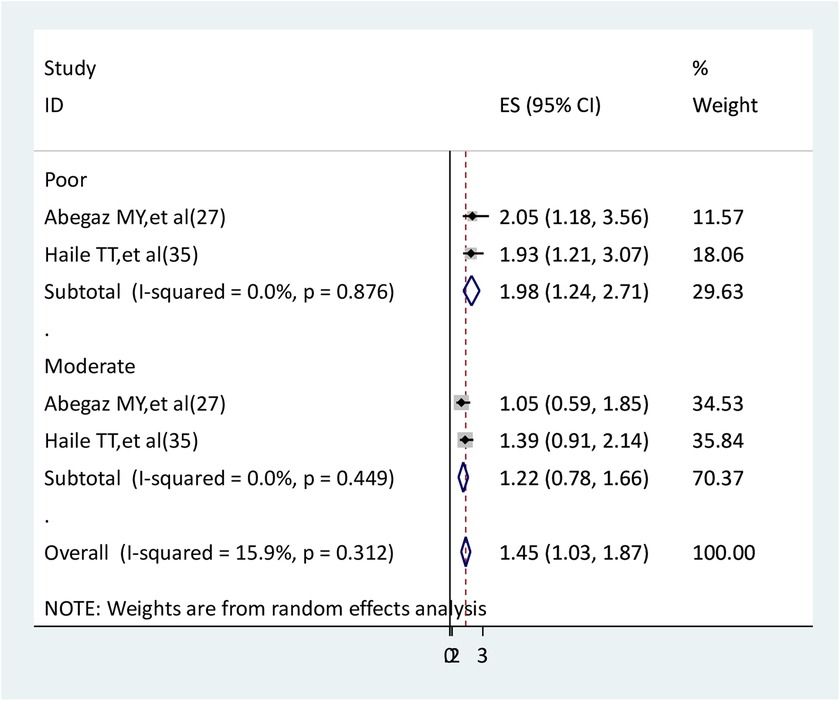
The association between social support and anxiety
Two studies were identified to determine the relationship between social support and anxiety (27, 29). In the findings of two studies, there is a statistically significant association between poor social support and anxiety but not between moderate social support and anxiety. The results of the meta-analysis indicated that pregnant women with poor social support had nearly two times higher anxiety than pregnant women with strong social support (AOR = 1.98, 95% CI: 1.24–2.71). Pregnant women with moderate social support did not have a statistically significant association with anxiety (AOR = 1.22, 95% CI: 0.78–1.66). There was no heterogeneity between studies (Figure 13).
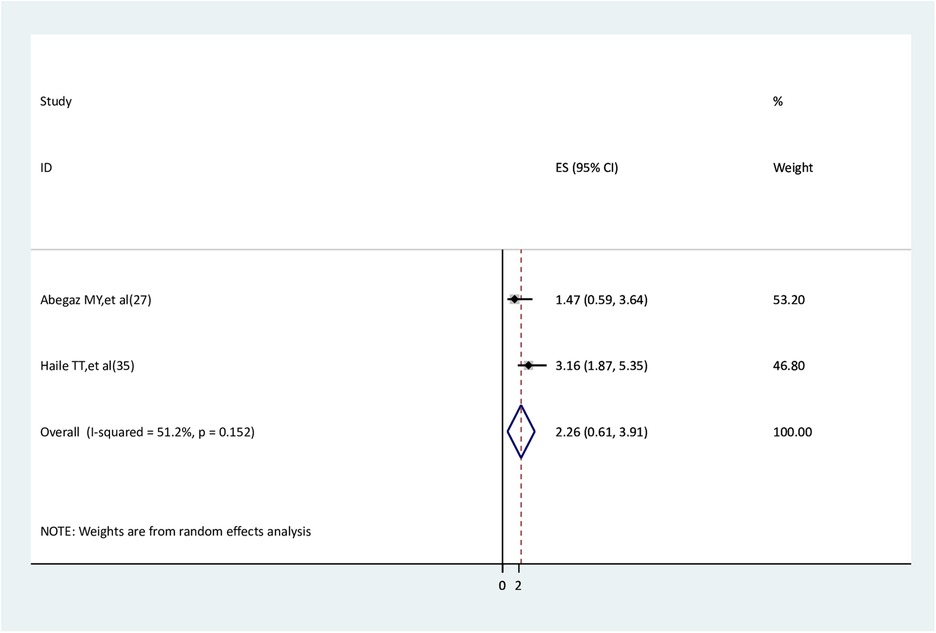
History of medical illness and anxiety
The association between a history of medical illness and anxiety was assessed using two studies (27, 29). One study had a significant association (29), but the other one did not (27). The results of the meta-analysis did not find a significant association between a history of medical illness and anxiety (AOR = 2.26, 95% CI: 0.61–3.91) (Figure 14).
Discussion
Understanding COVID-19 pandemic effects on the psychological well-being of pregnant women is essential to preventing negative impacts and unexpected consequences for the mother and the fetus (4). Thus, the aim of this systematic review was to determine the pooled prevalence of depression and anxiety during the COVID-19 pandemic in Ethiopia.
In this systematic review, the pooled prevalence of depression among pregnant women during COVID-19 pandemic in Ethiopia was 24.7%. This magnitude is consistent with previous studies conducted at the global level (5), in Africa (6), and in Ethiopia (8–11). We did not find any differences in the pooled prevalence of depression in the present and the prior studies that did not take into account the pandemic in Ethiopia (9, 10). The World Health Organization discovered that the COVID-19 pandemic impacted mental health outcomes for women during and after pregnancy (35); therefore, this discovery was unexpected. The current depression magnitude, however, is lower than that of a previous study conducted globally (4) but higher than that of a previous study conducted in Kenya (7). This could be explained by the role of chance because of the small sample size, which makes it difficult to accurately detect the outcome of a single institute study conducted in Kenya. Other factors that may contribute to the variation in depression magnitude include societal level, social networks, genetics, cultural disparities (16, 17, 19), and variations in income levels (12–14). In the present meta-analysis, the pooled prevalence of anxiety among pregnant women after the onset of COVID-19 was 35.19%, which is higher than the previous studies conducted at the global level (5) and Kenya (7). This discrepancy may result from variations in cultural norms and income levels (12–14, 16, 17, 19). Moreover, there was a slightly higher magnitude of anxiety in the current study compared to a previous study in Ethiopia (11). This could be due to differences in how the social distancing strategy was implemented across Ethiopia during the COVID-19 epidemic, which could have an impact on the rise in anxiety symptoms (15).
The prevalence of depression was 26% and 24% in the Oromia and Amhara regions, respectively. This slight difference in the magnitude of depression between Oromia and Amhara region could be variations of genetic, societal (19) and financial levels (12–14) among study participants. The other explanation could be a sample size difference. A higher prevalence of depression was observed in 2021 at 26%, and then slightly decreased to 23% in 2022 by 3%. This may be because the COVID-19 immunization reduced COVID-19 mortality from 2020 to 2022 (36). Using DASS measurement tools, the prevalence of depression was 33%, while using EPDS and PHQ-9, the prevalence of depression was 23% and 14%, respectively. This variation could be a difference in the effectiveness of these tools in the diagnosis of depression.
Single and unsatisfied marital statuses were risk factors for depression. These findings were in line with the previous findings that reported that non-married and dissatisfied marital status had higher depression symptoms (30, 37). Unplanned pregnancy was a cause for depression. This evidence is consistent with a previous study done by Muskens L, et al. (38) that stated that women with an unplanned pregnancy were more vulnerable to developing depression. Pregnant women with poor social support had a higher depression and anxiety than pregnant women with strong social support. This finding was in line with a previous study (18). It might be attributed to having a poor social network (19), which is possibly based on increased social distance (15), which in turn worsens feelings of depression and anxiety. Pregnant women with intimate partner violence were more likely to have anxiety than pregnant women without intimate partners. This finding was in line with a previous study conducted by Wu F. et al. (39), which stated that intimate partner violence was significantly associated with anxiety.
All of the included studies were cross-sectional and, hence, had a lower level of evidence compared to other analytical studies. This systematic review only covered a small number of regions, making it impossible to generalize to the remaining regions. For the pooled prevalence of depression, heterogeneities were observed only in the Amhara region and in the study year 2021. Therefore, the heterogeneity in this region and study period should require further investigation. For other subgroup analyses, there was no heterogeneity. In general, the number of included studies was insufficient, resulting in inadequate power to detect the outcome in each subgroup. For the pooled prevalence of anxiety, subgroup analyses were not generally conducted as a result of the existence of few studies per category (one or two per category). Small numbers of studies were used to assess the association of risk factors with depression and anxiety, which led to insufficient evidence. Therefore, these results should be interpreted with caution, considering the small number of studies included, leading to the inadequate power of the study and its inability to detect the outcome accurately. However, this study found that the high rate of depression and anxiety in pregnant women during the COVID-19 pandemic in Ethiopia had significant implications for the mental and physical health of the woman as well as the wellbeing of her fetus. It is vital, therefore, to address them as a public health priority.
Conclusion
One-fourth and nearly one-third pregnant women developed depression and anxiety, respectively, during the COVID-19 pandemic in Ethiopia. As a result, action is needed to incorporate perinatal mental health into policy and integrate mental health services, such as those for anxiety and depression, into routine prenatal care. Pregnant women with single and unsatisfied marital status required early antenatal screening and treatment to reduce depression. Unplanned pregnancy should also be given special attention. Poor social support is a cause of depression and anxiety. Pregnant women with violent intimate partners were more likely to develop anxiety.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
TG: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MW: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to express our gratitude to all of the primary authors of the included studies in this review.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2024.1453157/full#supplementary-material
Abbreviations
COVID-19, coronavirus disease-19; HIV, human immunodeficiency viruses; EPDS, Edinburgh postnatal depression scale; PHQ-9, patient health question; DASS, depression anxiety stress scale; PRAQR, pregnancy related anxiety questionnaires-revised; AOR, adjusted odd ratio; CI, confidence interval; Fig, figure; S, supplementary.
References
1. Mirzaei M, Yasini Ardekani SM, Mirzaei M, Dehghani A. Prevalence of depression, anxiety and stress among adult population: results of Yazd health study. Iran J Psychiatry. (2019) 14(2):137–46.31440295
2. Kalin NH. The critical relationship between anxiety and depression. Am J Psychiatry. (2020) 177(5):365–7. doi: 10.1176/appi.ajp.2020.20030305
3. Dule A. Psychological distress among Ethiopian pregnant women during COVID-19: negative correlation with self-efficacy. Psychol Res Behav Manag. (2021) 14:1001–10. doi: 10.2147/PRBM.S317961
4. Adrianto N, Caesarlia J, Pajala FB. Depression in pregnant and postpartum women during COVID-19 pandemic: systematic review and meta-analysis. Obstet Gynecol Sci. (2022) 65(4):287–302. doi: 10.5468/ogs.21265
5. Tomfohr-Madsen LM, Racine N, Giesbrecht GF, Lebel C, Madigan S. Depression and anxiety in pregnancy during COVID-19: a rapid review and meta-analysis. Psychiatry Res. (2021) 300:113912. doi: 10.1016/j.psychres.2021.113912
6. Wegbom AI, Edet CK, Ogba AA, Osaro BO, Harry AM, Pepple BG, et al. Determinants of depression, anxiety, and stress among pregnant women attending tertiary hospitals in urban centers, Nigeria. Women. (2023) 3(1):41–52. doi: 10.3390/women3010003
7. Adina J, Morawska A, Mitchell AE, Haslam D, Ayuku D. Depression and anxiety in second and third trimesters among pregnant women in Kenya: a hospital-based prevalence study. J Affect Disord. (2022) 10:100447. doi: 10.1016/j.jadr.2022.100447
8. Ayen SS, Kasahun AW, Zewdie A. Depression during pregnancy and associated factors among women in Ethiopia: a systematic review and meta-analysis. BMC Pregnancy Childbirth. (2024) 24(1):220. doi: 10.1186/s12884-024-06409-y
9. Zegeye A, Alebel A, Gebrie A, Tesfaye B, Belay YA, Adane F, et al. Prevalence and determinants of antenatal depression among pregnant women in Ethiopia: a systematic review and meta-analysis. BMC Pregnancy Childbirth. (2018) 18(1):462. doi: 10.1186/s12884-018-2101-x
10. Ayano G, Tesfaw G, Shumet S. Prevalence and determinants of antenatal depression in Ethiopia: a systematic review and meta-analysis. PLoS One. (2019) 14(2):e0211764. doi: 10.1371/journal.pone.0211764
11. Demissie DB, Bitew ZW. Mental health effect of COVID-19 pandemic among women who are pregnant and/or lactating: a systematic review and meta-analysis. SAGE Open Med. (2021) 9:20503121211026195. doi: 10.1177/20503121211026195
12. Dijkstra-Kersten SM, Biesheuvel-Leliefeld KE, van der Wouden JC, Penninx BW, van Marwijk HW. Associations of financial strain and income with depressive and anxiety disorders. J Epidemiol Community Health. (2015) 69(7):660–5. doi: 10.1136/jech-2014-205088
13. Roddy Mitchell A, Gordon H, Atkinson J, Lindquist A, Walker SP, Middleton A, et al. Prevalence of perinatal anxiety and related disorders in low- and middle-income countries: a systematic review and meta-analysis. JAMA Network Open. (2023) 6(11):e2343711. doi: 10.1001/jamanetworkopen.2023.43711
14. Thomson RM, Igelström E, Purba AK, Shimonovich M, Thomson H, McCartney G, et al. How do income changes impact on mental health and wellbeing for working-age adults? A systematic review and meta-analysis. The Lancet Public Health. (2022) 7(6):e515–e28. doi: 10.1016/S2468-2667(22)00058-5
15. Harville EW, Wood ME, Sutton EF. Social distancing and mental health among pregnant women during the coronavirus pandemic. BMC women’s Health. (2023) 23(1):189. doi: 10.1186/s12905-023-02335-x
16. Hofmann SG, Hinton DE. Cross-cultural aspects of anxiety disorders. Curr Psychiatry Rep. (2014) 16(6):450. doi: 10.1007/s11920-014-0450-3
17. Hofmann SG, Anu Asnaani MA, Hinton DE. Cultural aspects in social anxiety and social anxiety disorder. Depress Anxiety. (2010) 27(12):1117–27. doi: 10.1002/da.20759
18. Bedaso A, Adams J, Peng W, Sibbritt D. The relationship between social support and mental health problems during pregnancy: a systematic review and meta-analysis. Reprod Health. (2021) 18(1):162. doi: 10.1186/s12978-021-01209-5
19. Remes O, Mendes JF, Templeton P. Biological, psychological, and social determinants of depression: a review of recent literature. Brain Sci. (2021) 11(12). doi: 10.3390/brainsci11121633
20. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
21. Stein Murray B, Sareen J. Generalized anxiety disorder. N Engl J Med. (2015) 373(21):2059–68. doi: 10.1056/NEJMcp1502514
22. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
23. DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. (2007) 28(2):105–14. doi: 10.1016/j.cct.2006.04.004
24. Israel H, Richter RR. A guide to understanding meta-analysis. J Orthop Sports Phys Ther. (2011) https://www.jospt.org/doi/epdfplus/10.2519/jospt.2011.3333; 41(7):496–504. doi: 10.2519/jospt.2011.3333
25. Mathur MB, VanderWeele TJ. Sensitivity analysis for publication bias in meta-analyses. J R Stat Soc Ser C Appl Stat. (2020) 69(5):1091–119. doi: 10.1111/rssc.12440
26. Oljira L, Abdissa E, Lema M, Merdassa E, Wakoya Feyisa J, Desalegn M. Antenatal depression and associated factors among pregnant women attending antenatal care at public health facilities in the Gida Ayana district, Oromia region, West Ethiopia, in 2022. Front Public Health. (2023) 11:1176703. doi: 10.3389/fpubh.2023.1176703
27. Abegaz MY, Muche HA, Aynalem GL. Determinants of pregnancy-related anxiety among women attending antenatal checkup at public health institutions in Debre Markos town, Ethiopia. Depress Res Treat. (2022) 2022:6935609. doi: 10.1155/2022/6935609
28. Tarafa H, Alemayehu Y, Nigussie M. Factors associated with pregnancy-related anxiety among pregnant women attending antenatal care follow-up at Bedelle general hospital and Metu Karl comprehensive specialized hospital, Southwest Ethiopia. Front Psychiatry. (2022) 13:938277. doi: 10.3389/fpsyt.2022.938277
29. Haile TT, Kebede AA, Gessesse DN, Tsega NT, Aklil MB, Temesgan WZ, et al. Anxiety and associated factors in Northwest Ethiopian pregnant women: a broad public health concern. Front Public Health. (2024) 11:1300229. doi: 10.3389/fpubh.2023.1300229
30. Ahmed SJ, Merid M, Edessa D, Usso AA, Adem HA, Tariku M, et al. Prenatal depression among pregnant women attending public health facilities in Babile district, Eastern Ethiopia: a cross-sectional study. BMC Psychiatry. (2024) 24(1):339. doi: 10.1186/s12888-024-05732-0
31. Takelle GM, Nakie G, Rtbey G, Melkam M. Depressive symptoms and associated factors among pregnant women attending antenatal care at comprehensive specialized hospitals in Northwest Ethiopia, 2022: an institution-based cross-sectional study. Front Psychiatry. (2023) 14:1148638. doi: 10.3389/fpsyt.2023.1148638
32. Sewnet Amare N, Nibret Gessesse D, Solomon Kinfu Y, Melesew Mekuriyaw A, Amera Tizazu M, Mossie Menalu M, et al. Prevalence of antenatal depression and associated factors among pregnant women during COVID-19 pandemic in North Shewa zone, Amhara region, Ethiopia. Int J Afr Nurs Sci. (2022) 17:100459. doi: 10.1016/j.ijans.2022.100459
33. Anbesaw T, Ejigu H, Abegaz Z, Arefaynie M. Antenatal depressive symptoms and its associated factors among pregnant women in Northeast, Ethiopia. Sage Open. (2024) 14(3):21582440241271132. doi: 10.1177/21582440241271132
34. Seid J, Mohammed E, Cherie N, Yasin H, Addisu E. The magnitude of perinatal depression and associated factors among women in Kutaber Woreda public health institution and Boru Meda general hospital, Ethiopia, 2022: a cross-sectional study. Front Psychiatry. (2024) 14:1302168. doi: 10.3389/fpsyt.2023.1302168
35. USAID. A Shared Vision for Improving Perinatal Mental Health in Low- and Middle-Income Countries: A Theory of Change and Prioritized Implementation Research Questions. United States: USAID MOMENTUM (2022). Available online at: https://pdf.usaid.gov/pdf_docs/PA00ZQN5.pdf (accessed September 25, 2023).
36. Viscusi WK. The global COVID-19 mortality cost report card: 2020, 2021, and 2022. PLoS One. (2023) 18(5):e0284273. doi: 10.1371/journal.pone.0284273
37. Bedaso A, Adams J, Peng W, Xu F, Sibbritt D. An examination of the association between marital status and prenatal mental disorders using linked health administrative data. BMC Pregnancy Childbirth. (2022) 22(1):735. doi: 10.1186/s12884-022-05045-8
38. Muskens L, Boekhorst M, Kop WJ, van den Heuvel MI, Pop VJM, Beerthuizen A. The association of unplanned pregnancy with perinatal depression: a longitudinal cohort study. Archives of Women’s Mental Health. (2022) 25(3):611–20. doi: 10.1007/s00737-022-01225-9
Keywords: depression, anxiety, pregnant women, COVID 19 pandemic, Ethiopia
Citation: Gebeyehu Wondmeneh T and Wogris M (2024) Depression and anxiety among pregnant women during COVID 19 pandemic in Ethiopia: a systematic review and meta-analysis. Front. Glob. Womens Health 5:1453157. doi: 10.3389/fgwh.2024.1453157
Received: 22 June 2024; Accepted: 20 November 2024;
Published: 3 December 2024.
Edited by:
Jayashri Kulkarni, Monash University, AustraliaReviewed by:
Ana I. Flores, Research Institute Hospital 12 de Octubre, SpainLenka Kramska, Na Homolce Hospital, Czechia
Copyright: © 2024 Gebeyehu Wondmeneh and Wogris. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Temesgen Gebeyehu Wondmeneh, dG9taWdlYjIwMDZAZ21haWwuY29t
 Temesgen Gebeyehu Wondmeneh
Temesgen Gebeyehu Wondmeneh Mohhamed Wogris
Mohhamed Wogris