
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Glob. Womens Health , 12 August 2024
Sec. Contraception and Family Planning
Volume 5 - 2024 | https://doi.org/10.3389/fgwh.2024.1420476
This article is part of the Research Topic Current Advances in Contraceptive Use, Technology, and Promotion View all 11 articles
 Hailemichael Kindie Abate*
Hailemichael Kindie Abate* Abere Woretaw Azagew
Abere Woretaw Azagew Chanyalew Worku Kassahun
Chanyalew Worku Kassahun Mulugeta Wassie
Mulugeta Wassie Chilot Kassa Mekonnen
Chilot Kassa Mekonnen Yilkal Abebaw Wassie
Yilkal Abebaw Wassie Alebachew Ferede Zegeye
Alebachew Ferede Zegeye
Background: The use of long-acting contraceptives is a common health challenge in Ethiopia. Therefore, the current study aimed to assess the determinants of using long-acting contraceptive hot spots in Ethiopia using data from the Ethiopian Mini Demographic and Health Survey for 2019.
Methods: This study used data from the Ethiopia Mini Demographic and Health Survey 2019 and included a total weighted sample of 8,885 women in the analysis. The geographical variation of long-acting contraceptive usage was initially observed using hot spot analysis. Arc GIS version 10.7 was used for geographically weighted regression. Ordinarily, least squares regression was performed to identify predictors that explain the geographical variation in the use of long-acting contraceptives. Geographic weighted regression was used to predict the hot spot area of long-acting contraceptive methods.
Results: The overall prevalence of long-acting contraceptive utilization use was 6.9% (95% confidence interval: 6.4–7.45). Most of the statistically significant hot spots for long-acting contraceptives were found in lactated areas of the Oromia part of Amhara and Dire Dawa. Primary education, followers of the Muslim religion, marital status, and women with >4 children were the determinants of spatial variation use of hot spot areas for long-acting contraceptive methods.
Conclusions: A detailed map of long-acting contraceptive use hot spots and their determinants will enable decisions to target their sociodemographic-related predictors of women.
The long-acting contraceptive (LAC) method is among the most suitable and effective modern contraceptive methods that can prevent pregnancy and save money for families and the country as a whole (1). Long-acting contraceptives can be reversible or non-reversible. The reversible type of contraceptive can be hormonal (implants that prevent pregnancy for 3–5 years) and non-hormonal [an intrauterine device (IUD) that prevents pregnancy for 12 years]. The permanent type of contraceptive (vasectomy/sterilization of the man and tubal ligation of the woman) can prevent pregnancy for life (1).
In addition to the prevention of pregnancy, contraceptives have other uses, such as for adjusting the menstrual cycle, controlling premenstrual mood disturbances, and preventing endometrial cancer (1–3).
In developing countries, approximately 214 million women of reproductive age lack access to modern contraception techniques, including LAC methods. As a result, nearly half of pregnancies are unintended (4). In addition, one in three unwanted pregnancies is the consequence of contraceptive failure, which is more common with traditional and short-acting techniques than with long-acting ones (5).
Ethiopia is one of the countries with the fastest population growth, next to Nigeria (6). According to evidence from the Ethiopia Demographic Health Survey (EDHS) of 2016, 22% of women still lack access to contraceptive methods (7). Providing appropriate, accessible, and inexpensive contraceptive options is crucial to prevent unwanted pregnancies and help families achieve their desired health goals (5). Globally, 64% of women of reproductive age used different methods of contraception, of which approximately 45.2% of women in developed countries used long-acting contraceptive methods. Of them, 5.1% were in sub-Saharan Africa (8, 9). In Ethiopia, most women of reproductive age used short-acting contraceptive methods and only 10% of the women used LACs (10, 11).
To expand the lack of access to contraceptive methods, the Ethiopian Ministry of Health must plan to distribute LAC to prevent unintended pregnancy at all healthcare levels (12). Despite these attempts to increase contraceptive utilization, there was still a low level of contraceptive utilization (11).
Studies conducted on long-acting contraceptives in Ethiopia showed the simple prevalence of the utilization of long-acting contraceptives and its associated factors. As research evidence, the age of the women (13, 14), marital status, level of education (15, 16), wealth index (16, 17), number of children (18–20), and residency were factors in the use of long-acting contraceptives (17, 21). Studies were conducted on the geographical variation of modern contraceptives among reproductive age groups using data from the 2019 EDHS (22, 23). However, no studies were conducted on the determinants of long-acting contraceptive utilization hot spot analysis using 2019 mini-EDHS data applying geographic weight regression. Therefore, the current study aimed to assess the determinants of the utilization of long-acting contraceptive hot spot analysis in Ethiopia using 2019 mini-EDHS data.
The study was carried out in Ethiopia, which is located in the Horn of Africa, 3° to 14° N and 33° to 48° E. The Ethiopia Mini Demographic Health Survey (EMDHS) 2019 data were used as a data source for this study (24). According to EMDHS 2019, there are nine administrative regions [Tigray, Afar, Amhara, Oromia, Benishangul-Gumuz, Gambela, Southern Nations, Nationalities and People's Region (SNNPR), Harari, and Somoli] and two city administrations (Addis Ababa and Dire Dawa). EMDHS 2019 was the second mini-demographic survey conducted in Ethiopia. The sample was stratified into two stages and selected. A total of 305 cluster census enumeration areas (EA) stratified into urban and rural (93 urban and 212 rural) areas were selected (Figure 1).
The study was carried out between 21 March 2019 and 28 June 2019. All women of reproductive age in their late 20s were the source population, while those selected reproductive-age women who were in their late 20s were the study population. All women of reproductive age in the selected area were included in the study, while women who had never had sex and pregnant women were excluded.
In total, 8,885 women were included in the study. The dataset used to analyze this manuscript was an individual record (IR). The detailed sampling procedure is illustrated in the 2019 EMDHS report.
The dependent variable of this study was the use of one of the long-acting contraceptives (used/not used) (25).
The individual-level factors included were age, marital status, religion, educational status, wealth index, number of living children, and age at first birth, while community-level factors included community wealth index, residency, region, and community education (26, 27).
Women who are considered to be using long-acting contraceptives use one of the following long-acting contraceptive methods: IUD, implants, and male/female sterilization (25).
The community wealth index is calculated by generating the combined wealth index with its cluster number. Then, it was leveled as high community poverty and low community poverty by computing the median of the proportion (0.2777778) of the wealth index of women.
The educational level of the participants that is considered a high-level educational status of the community is generated using the media proportion of the highest educational status (0.9220659) of the participants.
Microsoft Excel was used to clean up the data. The data were further processed, cleaned, recoded, and analyzed using STATA version 14/MP. Before spatial analysis, the sample waiting for the outcome variable and the explanatory variable was performed to ensure the representativeness of the DHS data sample and to obtain reliable estimates and standard errors (28). Descriptive data were analyzed using STATA and presented in tables to describe the use of long-acting contraceptives by sociodemographic factors and maternal characteristics. STATA version 14/MP and Arc GIS v.10.8 were used for the data analysis.
The spatial autocorrelation of Global Moran's I measure was computed to assess the spatial heterogeneity of the use of long-acting contraceptives. Moran's I values close to negative 1 indicate dispersed, close to positive clustered, and 0 values indicate random use of long-acting contraceptives (29). A significant statistical Moran I value (p < 0.05) led to the rejection of the null hypothesis, which indicated the presence of spatial autocorrelation. The hot spot analysis (Getis–Ord statistics) of the z scores with significant p-values gave the characteristics with hot spot or cold spot values for the clusters. The Getis–Ord statistic z score near zero indicates that there is no clustering, the positive z score indicates a cluster of high value (hot spot), and the negative z score indicates a cluster of low value (cold spot) (30).
Ordinary least squares (OLS) regression is a global statistical model that uses a single equation to estimate the relation between the outcome and explanatory variables. The equation is given as where i = 1, 2, … n, β0, β1, β3, …, βP are the model parameters, Yi is the outcome variable for the observation i, xik is the explanatory variable, and ℰ1, ℰ2, ℰ3, …, ℰn are the error term/residuals with zero mean and with homogenous variance .
After identifying long-acting contraceptive hot spots, spatial regression modeling was performed to identify predictors of spatial patterns of long-acting contraceptives. The ordinary least squares finding is only reliable if the regression model satisfies all the assumptions that are required by this method (31). All OLS assumptions, such as multicollinearity using the variance inflation factor (VIF), the Koenker test for non-stationarity, Moran's I statistics for residual spatial autocorrelation, and statistically non-significant Jarque–Bera statistics for model bias, were checked before preceding the geographically weighted regression (GWR).
GWR is a local statistical regression model that assumes cluster variation (non-stationarity) in the relationship or heterogeneity in the relationship between the dependent and independent variables in different cluster areas. In contrast, OLS fits a single linear static equation to all data in the study area, while GWR enables an equation for each enumeration clustered area (32, 33). Therefore, the GWR coefficient assumes various values for each cluster. The coefficients were associated with each explanatory variable in the maps that were generated using the GWR. The equation of GWR was given as , where γi is the observation’s response γ, (uivi) are the geographical points of latitude and altitude, βk(uivi) (k = 0, 1, 2, …, p)p is the unknown function of geographic location (uivi), Xik is the explanatory variable at location uivi, i = 1. 2, 3, …, n, and is an error terms with zero mean and homogenous variance. To minimize potential confounders’ variable with p-value > 0.2 in OLS had to be excluded for GWR analysis.
Permission to access the data was obtained from a Demographic Health Survey (DHS) through an online request at https://dhsprogram.com/data/available-datasets.cfm. The data used for this study were freely available on request online. This study was based on secondary data from the EDHS, and we obtained a permission letter from the main Demographic Health Survey.
Among the total study participants, the majority (95.05%) of Muslim women did not use long-acting contraceptives. Among women who had not used long-acting contraceptives, the majority (98.59% and 94.18%) were not married and had no educational level, respectively. The age of respondents at first delivery (98.2%) and participants who have no living children (90.31%) did not use log-acting contraceptive methods (Table 1).
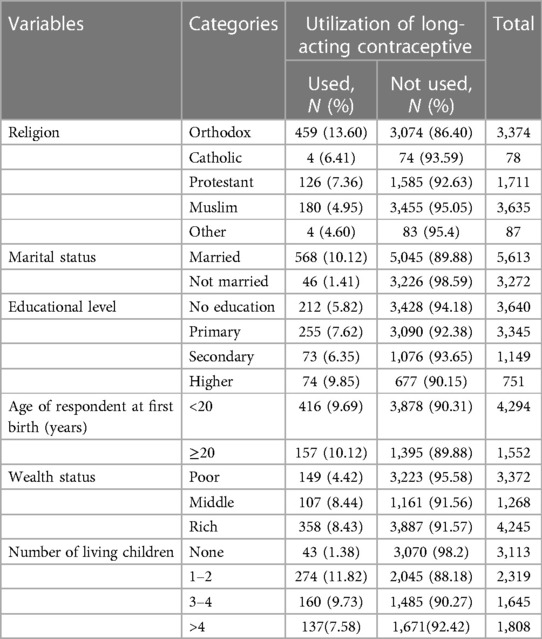
Table 1. The weighted proportion of sociodemographic factors in the use of long-acting contraceptive methods (n = 8,885).
Table 2 illustrates the weighted proportion of long-acting contraceptive use according to region and place of residence. Among women who had not used long-acting contraceptives, 93.4% were rural residents of the country. Similarly, most of the participants (99.52%) in the Somali region and 96.7% in the far region do not use the long-acting contraceptive method (Table 2). The overall prevalence of long-acting contraceptive use was 6.9% (95% confidence interval: 6.4–7.45).

Table 2. The weighted proportion of long-acting contraceptive use by place of residence and region, EMDHS 2019.
The spatial autocorrelation analysis showed a significant spatial autocorrelation of the use of long-acting contraceptives throughout the country with the Global Moran I value of 1.19 (p-value < 0.01) (Figure 2).
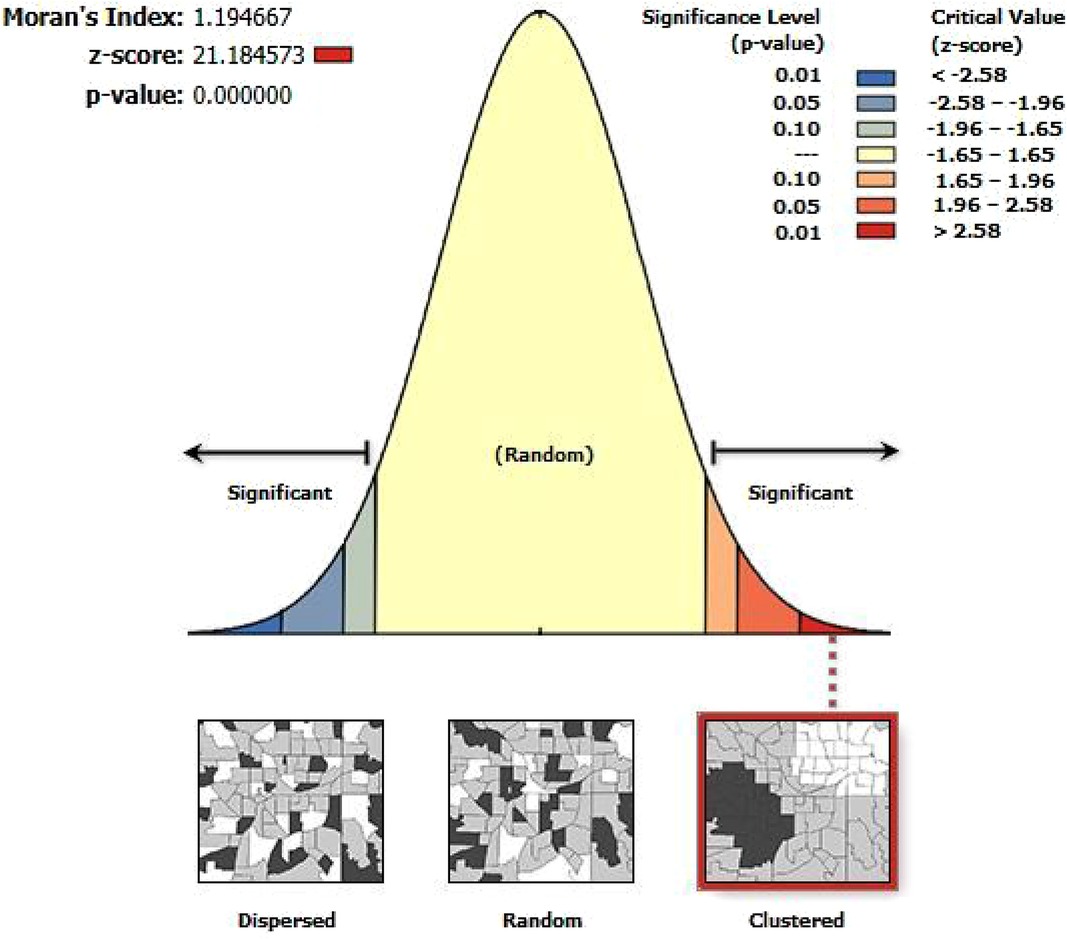
Figure 2. The global spatial autocorrelation analysis of LAC usage among women aged 15–49 years in Ethiopia, EMDHS 2019.
The significant hot spots for long-acting contraceptive use were lactated in the Oromia part of Amhara, Dire Dawa, and SNNPR (Figure 3).
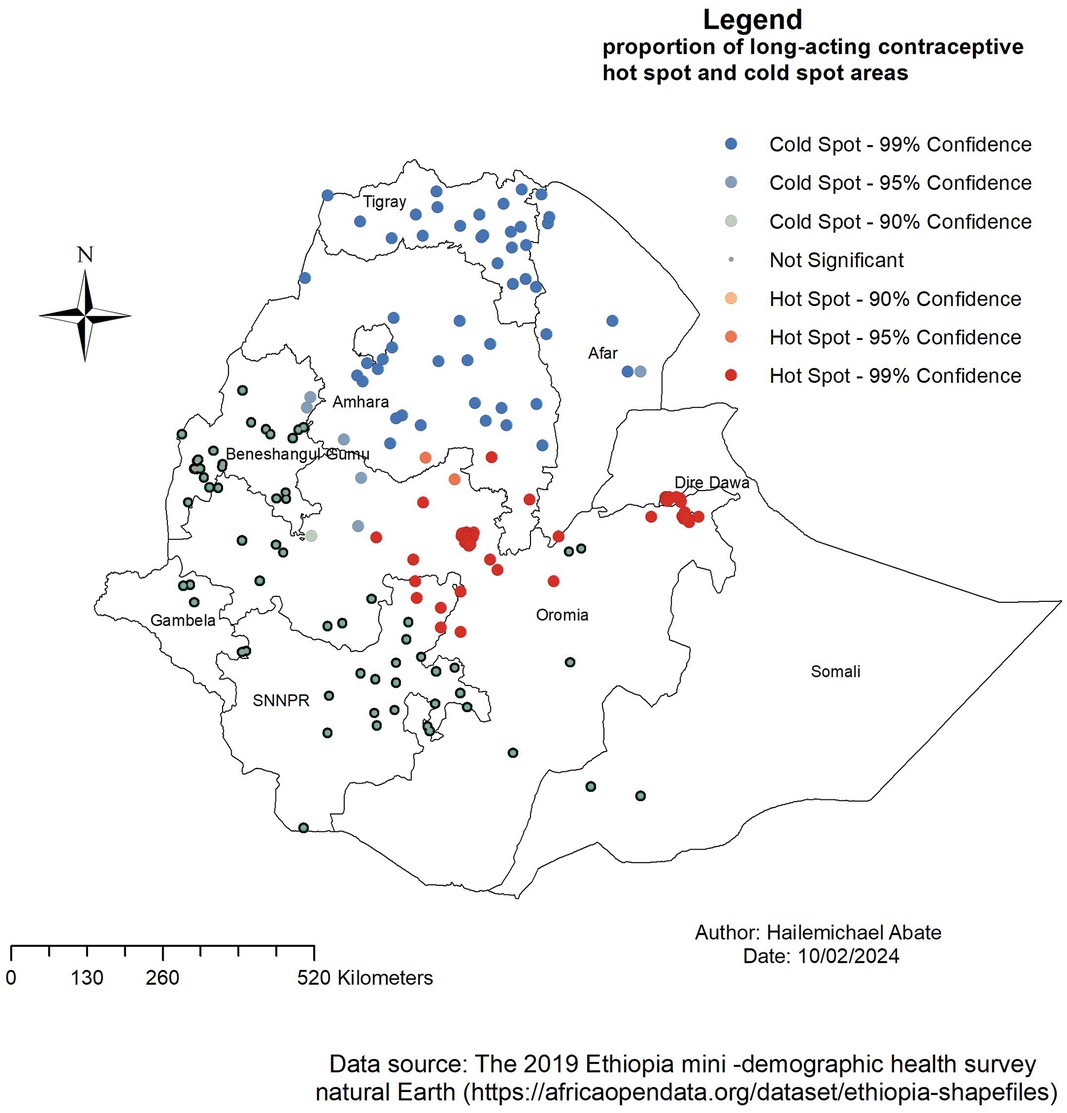
Figure 3. The Getis–Ord Gi statistical analysis of LAC usage hot spots among women aged 15–49 years in Ethiopia, EMDHS 2019.
The result of the OLS model showed that 16% of the variation in LAC utilization (adjusted R2 = 0.16) was explained by the model and met all assumptions of the OLS statistical model (34). There was no multicollinearity between the independent variables, that is, the VIF was less than 10. The Koenker test for non-stationarity was statistically significant (p-value < 0.01); therefore, it is recommended to perform a geographical weight regression. Since the Jarque–Bera statistic was non-significant (p-value > 0.01), the residual was assumed to be normally distributed. Furthermore, the combined Wald statistic was statistically significant (p-value < 0.01), which indicates that the overall model was significant. As a result of the meeting of all the OLS assumptions, GWR had to be run to obtain the local coefficient of explanatory variables of the hot spot areas (Table 3).
The proportion of followers of the Muslim religion, mothers with a primary education, married women, and women with >4 children had a significant influence on the distribution of the use of LAC. A unit increase for respondents with a primary education and marital status increases the use of long-acting contraceptives by 0.122 and 0.16, respectively. However, there was a unit decrease in followers of the Muslim religion and women with >4 children by −0.047 and −0.09 in the use of LACs, respectively (Table 4).
The OLS statistical regression model showed the LAC factors in the geographical hot spot area. However, it was a global model that showed that the relationship between each explanatory variable and LAC is stationary in the study area. The results of the GWR indicated that there was a significant improvement compared to OLS. In Table 4, the adjusted R2 (0.16) and Akaike's Information Criterion (AIC) (1,395.28) obtained in OLS were increased in GWR to 0.17 and 1,394.93, respectively. Based on this analysis, the GWR result is better than the result generated using the OLS model (Table 5).
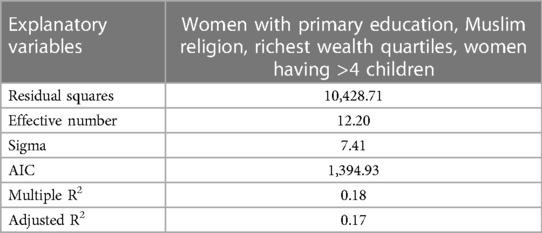
Table 5. Analysis result of significant explanatory variables using the GWR model for LAC in Ethiopia, EMDHS 2019.
The GWR analysis results showed that the explanatory variables were weak and had a strong relationship with the use of LAC.
Figures 4–7 show that the proportion of explanatory variables of LAC in the geographical areas was strong and weak predictors. The geographical area with clustered red points indicates the largest coefficient of the predictors and strong predictors in the hot spot areas in the use of long-acting contraceptives. Therefore, the largest coefficient of the predictor in the hot spot areas indicates a strong predictor in the use of LAC. Women who were married had strong and positive predictors of LAC. As the proportion of women who were married increased, the incidence of LAC usage in Tigray, Amhara, Benishangul-Gumuz, and parts of Afar increased (Figure 4).

Figure 4. Women with GWR coefficients of married marital status to predict LAC usage in Ethiopia, EMDHS 2019.
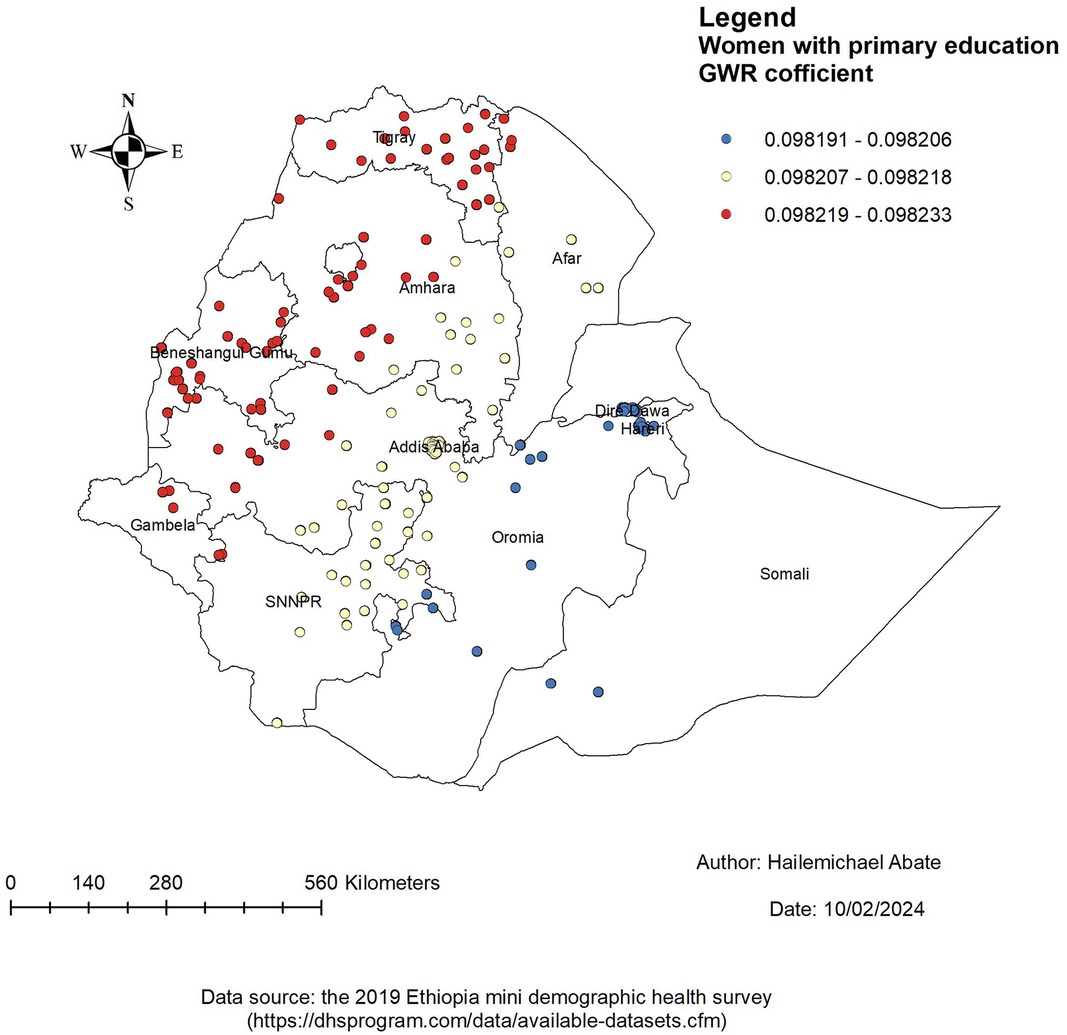
Figure 5. Women with GWR coefficients of primary education to predict LAC use in Ethiopia, EMDHS 2019.
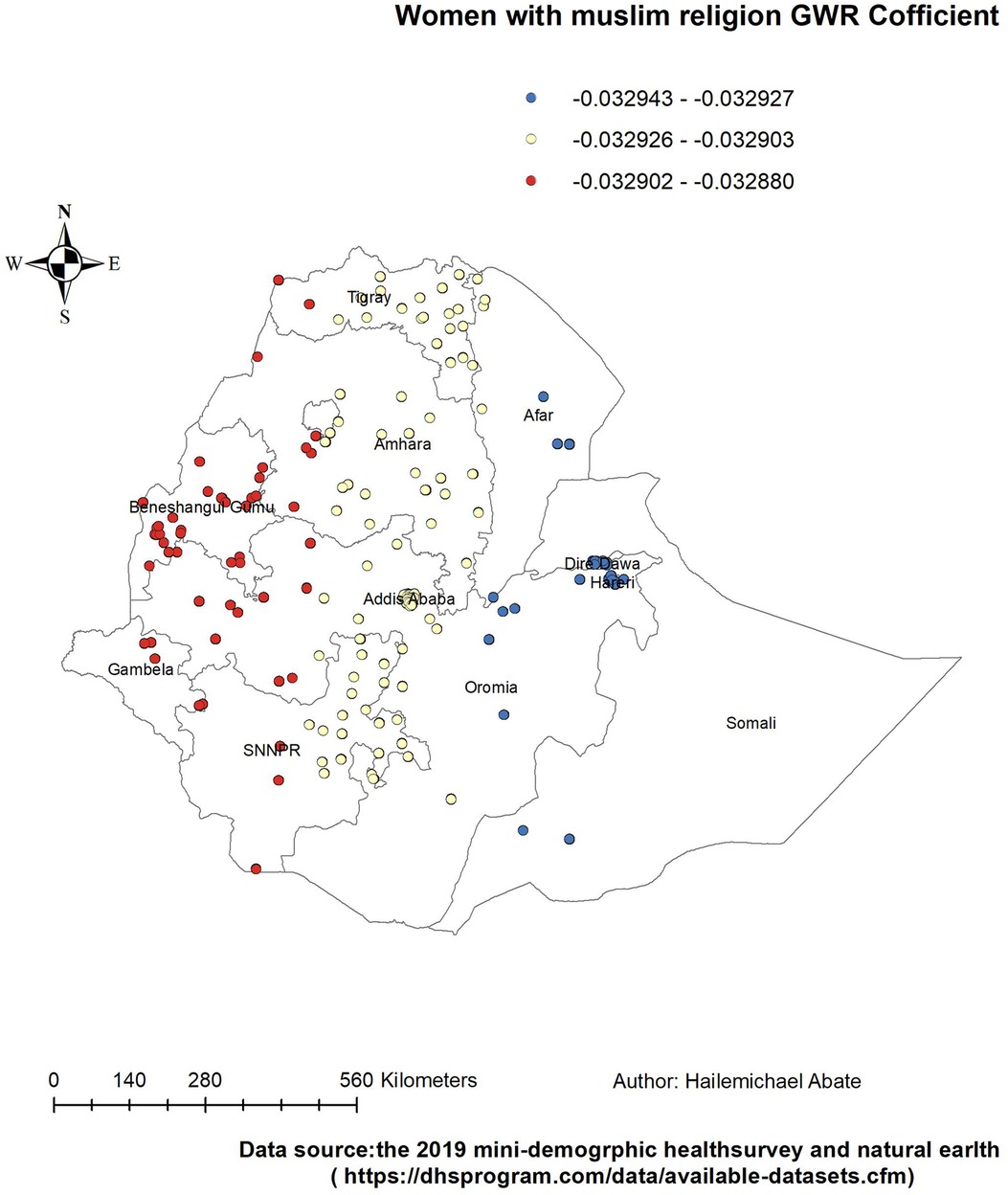
Figure 6. Women with GWR coefficients of Muslim religion to predict LAC usage in Ethiopia, EMDHS 2019.
Women with a primary education had a positive and weak predictor of LAC. As the proportion of women with a primary education increased, the existence of LAC in Tigray, Amhara, Benishangul-Gumuz, Gambela, west Oromia, and the northern part of Afar increased (Figure 5).
Women who were followers of the Muslim religion had a negative and weak relationship with the use of LAC. Therefore, the Muslim religion was a protective factor in the use of LAC hot spot areas. The proportion of Muslim women decreased in the LAC hot spot areas of West Amhara and Oromia; in the entire Benishangul-Gumuz; and in parts of Tigray, Gambela, and SNNPR (Figure 6).
In the same way, women with >4 children had a negative and weak relationship with the use of LAC. Therefore, the factor of women with >4 children was protective in the use of LAC hot spot areas. The proportion of women with >4 children decreased in the LAC hot spot areas of Tigray, Amhara, Gambela, Benishangul-Gumuz, northwest Tigray, southwest Amhara, and parts of Gambela (Figure 7).
This baseline study shows the geographical variation of LACs and their associated factors in Ethiopia. LAC hot spots were located in Tigray, Amhara, Benishangul-Gumuz, Afar, Tigray, Oromia, SNNPR, and Gambela. Based on the findings of this study, the potential disparity in the use of LACs across the region could be due to different sociodemographic factors. In the GWR analysis, statistically significant determinant factors are identified that had strong and weak relationships with the use of LACs.
The proportion of women who were married, who had a primary education, who were Muslim, and who had >4 children were the predictors of the geographic areas of the LAC hot spots. From these predictors, the GWR coefficient of primary education relatively indicated that strong predictors of LAC were in the range of 0.098219–0.098233. The findings of this study can be used to emphasize the distribution use of LAC in the least used area of Ethiopia by addressing the predictors in the use of LAC.
The GWR coefficient of those women who were married varied from region to region in the range of 0.0938558–0.095068. The proportion of women who were married in the state increased the incidence of LAC use in Tigray, Amhara, Benishangul-Gumuz, and parts of Afar. This study's findings differed from the studies conducted in the 2016 EDHS (27, 35) in Ghana (36). A possible justification might be because of the difference in use of the dataset and method of analysis. Furthermore, participants in the current study might have knowledge in the use of LAC during pregnancy follow-up visits, the exchange of information with their couples, and the participation of husbands in reproductive services (37, 38).
The finding of this study also indicated that the proportion of women who had a primary education had a positive relationship and increased the prevalence of LAC use in Tigray, Amhara, Benishangul-Gumuz, Gambela West, and the northern part of Afar. This finding was supported by studies conducted in Ethiopia (39–41), Nigeria (42), and sub-Saharan Africa (43). A possible explanation might be that educated women would have information about the importance of the use of LAC through different social media and reading different articles (44, 45).
However, religious Muslim women had a negative and weak relationship with the use of LAC. Therefore, the Muslim religion was a protective factor in the use of LAC hot spot areas. The proportion of religious Muslim women decreased in the use of LAC hot spots area of West Amhara and Oromia, in the entire Benishangul-Gumuz, and in some parts of Tigray, Gambela, and SNNPR. The finding in this study is consistent with studies conducted in Ethiopia (46), Nigeria (47), and Nepal (48). A possible justification could be that religious opposition to contraceptive use may be more problematic for Muslim women (49).
Similarly, women who had >4 children had a negative and weak relationship with the use of LAC. Therefore, the factor of women who had >4 children was protective in the use of LAC hot spot areas. The proportion of women who had >4 children decreased in the use of LAC hot spot areas of Tigray, Amhara, Gambela, Benishangul-Gumuz, northwest Tigray, southwest Amhara, and parts of Gambela. This finding is supported by the study conducted in sub-Saharan Africa (50). This could be because women who had more children could be approaching physiological menopause and thus experience decreased sexual desire so there is no need for the use of long-acting contraceptives (51).
The present study has some limitations. The geographical coordinate cluster area was displaced by 2 km in urban areas, 10 km for 1% of the clusters in rural areas, and 5 km for most of the clusters in rural areas to avoid anonymized respondents of the community. This may influence the estimated cluster effects in the spatial analysis. Furthermore, in the two EMDHS 2019, some maternal factors were not available; this could be a potential determinant of LAC. However, despite these limitations, the study also had its strengths. The study used a nationally representative dataset that covers all regions of the country. In addition, the spatial regression modeling analysis using GWR was the strength of this study.
The study showed that there was spatial variation in the use of long-acting contraceptives among women in Ethiopia. Significant hot spot areas of long-acting contraceptive use were lactated in Oromia, part of Amhara, Dire Dawa, and SNNPR.
Women who were married and had a primary education had a positive predictor of LAC. On the other hand, religious Muslim women and women with >4 children had a negative relationship with the use of LAC.
Decision makers and the government should emphasize in women’s health information about the use of contraceptives and cooperate with religious and community leaders as strategies to improve the use of long-acting contraceptives. Organizing campaigns with religious leaders on the use of contraceptives is a good strategy to improve the use of contraceptives by women. In addition, education about the factors that influence the negative attitude toward the use of contraceptives is another effective means to increase the use of contraceptives. Furthermore, researchers should investigate other cultural and social factors that hinder the geographical variation of the use of long-acting contraceptives.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
HA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AA: Formal Analysis, Investigation, Methodology, Project administration, Validation, Writing – original draft, Writing – review & editing. CK: Formal Analysis, Project administration, Validation, Writing – original draft, Writing – review & editing. MW: Data curation, Formal Analysis, Methodology, Project administration, Validation, Writing – original draft, Writing – review & editing. CM: Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Validation, Writing – original draft, Writing – review & editing. YW: Data curation, Investigation, Methodology, Project administration, Software, Validation, Writing – original draft, Writing – review & editing. AZ: Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors express their thanks to the DHS data archivist, who allowed access to the dataset.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2024.1420476/full#supplementary-material
1. Joshi R, Khadilkar S, Patel M. Global trends in use of long-acting reversible and permanent methods of contraception: seeking a balance. Int J Gynaecol Obstet. (2015) 131:S60–S3. doi: 10.1016/j.ijgo.2015.04.024
2. Kallner HK. Benefits of reversible contraception. F1000Res. (2018) 7:14370–81. doi: 10.12688/f1000research.14370.1
3. Bahamondes L, Valeria Bahamondes M, Shulman LP. Non-contraceptive benefits of hormonal and intrauterine reversible contraceptive methods. Hum Reprod Update. (2015) 21(5):640–51. doi: 10.1093/humupd/dmv023
4. World Health Organization. World health statistics, institutional repository journal (iris). (2020). Available online at: https://www.who.int/publications/i/item/9789240005105 (Accessed March 8, 2024).
5. Bradley SE, Croft T, Rutstein SO. The Impact of Contraceptive Failure on Unintended Births and Induced Abortions: Estimates and Strategies for Reduction. Calverton, MD, USA: ICF Macro (2011).
6. World population data sheet, Population Reference Bureau (PRB). (2007). Available online at: https://www.prb.org/resources/2007 (Accessed February 8, 2024).
7. ORC Macro. Central Statistical Agency: Ethiopia Demographic and Health Survey 2016. Calverton, MD, USA: ORC Macro (2016). Vol. 3. p. 6–59.
8. Kantorova V, Molitoris J, Ueffing P. Global changes in contraceptive method-mix and outlook to 2030. Available online at: https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/undesa_pd_2021_method-mix_iussp_ipc_2021.pdf (Accessed February 8, 2024).
9. United Nations. Trends in Contraceptive Use Worldwide 2015. New York: United Nations, Department of Economic and Social Affairs (2015). Available online at: https://www.un.org/development/desa/pd/content/trends-contraceptive-use-worldwide-2015-report (Accessed March 9, 2024).
10. Csace I. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, MD, USA: CSA and ICF (2016). p. 1–551.
11. Kesetebirhan A. National Guideline for Family Planning Services in Ethiopia. Addis Ababa, Ethiopia: Ministry of Health (2011).
12. Asnake M, Henry EG, Tilahun Y, Oliveras E. Addressing unmet need for long-acting family planning in Ethiopia: uptake of single-rod progestogen contraceptive implants (Implanon) and characteristics of users. Int J Gynaecol Obstet. (2013) 123:e29–32. doi: 10.1016/j.ijgo.2013.07.003
13. Mekonnen G, Enquselassie F, Tesfaye G, Semahegn A. Prevalence and factors affecting use of long acting and permanent contraceptive methods in Jinka Town, Southern Ethiopia: a cross sectional study. Pan Afr Med J. (2014) 18:98. doi: 10.11604/pamj.2014.18.98.3421
14. Mohammed E, Tadese L, Agero G. Acceptance of long acting reversible contraceptive methods and associated factors among reproductive age women in Adama Town, Oromia Regional State, Ethiopia. Clin Med Res. (2017) 6(2):53. doi: 10.11648/j.cmr.20170602.15
15. Mambo S, Oyore J, Obare F, Maingi J, Shisanya C, Gitonga N. Assessing long-acting and permanent family planning methods uptake among women of reproductive age in Kilifi Sub-County, Kilifi County. Int J Innov Res Stud. (2014) 3:19–31.
16. Teferra AS, Wondifraw AA. Determinants of long acting contraceptive use among reproductive age women in Ethiopia: evidence from EDHS 2011. Sci J Public Health. (2015) 3(1):143–9.
17. Palamuleni ME, Adebowale AS. Women empowerment and the current use of long acting and permanent contraceptive: evidence from 2010 Malawi Demographic and Health Survey. Malawi Med J. (2014) 26(3):63–70.27529015
18. Melka AS, Tekelab T, Wirtu D. Determinants of long acting and permanent contraceptive methods utilization among married women of reproductive age groups in Western Ethiopia: a cross-sectional study. Pan Afr Med J. (2015) 21:246. doi: 10.11604/pamj.2015.21.246.5835
19. Sahilemichael A, Temesgen K, Gemechukejela . Determinants of long acting reversible contraceptives use among child bearing age women in Dendi District, Western Ethiopia. J Women’s Health Care. (2015) 4:242. doi: 10.4172/2167-0420.1000242
20. Azmoude E, Behnam H, Barati-Far S, Aradmehr M. Factors affecting the use of long-acting and permanent contraceptive methods among married women of reproductive age in East of Iran. Womens Health Bull. (2017) 4(3):1–8. doi: 10.5812/whb.44426
21. Alemayehu M, Kalayu A, Desta A, Gebremichael H, Hagos T, Yebyo H. Rural women are more likely to use long acting contraceptive in Tigray Region, Northern Ethiopia: a comparative community-based cross sectional study. BMC Womens Health. (2015) 15(1):1–8. doi: 10.1186/s12905-015-0229-7
22. Merid MW, Kibret AA, Alem AZ, Asratie MH, Aragaw FM, Chilot D, et al. Spatial variations and multi-level determinants of modern contraceptive utilization among young women (15–24 years) in Ethiopia: spatial and multi-level analysis of mini-EDHS 2019. Contracept Reprod Med. (2023) 8(1):26. doi: 10.1186/s40834-023-00224-0
23. Terefe B, Getnet M, Akalu Y, Belsti Y, Diress M, Gela YY, et al. Geospatial variations and determinants of contraceptive utilization among married reproductive age women in Ethiopia: spatial and multilevel analysis of Ethiopian Demographic and Health Survey, 2019. Front Global Womens Health. (2023) 4:1151031. doi: 10.3389/fgwh.2023.1151031
24. Central Statistical Agency (CSA) and ICF. Ethiopia Demographic and Health Survey. Addis Ababa, Ethiopia and Calverton, MD, USA: Central Statistical Agency (CSA) and ICF (2016). p. 1.
25. Ethiopia—Mini Demographic and Health Survey (2019). Available online at: https://microdataworldbankorg/indexphp/catalog/2886 (Accessed January 8, 2024).
26. Ebrahim OA, Zeleke EG, Muluneh AG. Geographic variation and associated factors of long-acting contraceptive use among reproductive-age women in Ethiopia: a multi-level and spatial analysis of Ethiopian Demographic and Health Survey 2016 data. Reprod Health. (2021) 18(1):122. doi: 10.1186/s12978-021-01171-2
27. Chekol YM, Jemberie SB, Goshe BT, Tesema GA, Tessema ZT, Gebrehewet LG. Geographic weighted regression analysis of hot spots of modern contraceptive utilization and its associated factors in Ethiopia. PLoS One. (2023) 18(11):e0288710. doi: 10.1371/journal.pone.0288710
29. Anselin L. GIS research infrastructure for spatial analysis of real estate markets. J Hous Res. (1998) 9(1):113–33. doi: 10.1080/10835547.1998.12091930
30. Getis A, Ord JK. The analysis of spatial association by use of distance statistics. Geogr Anal. (1992) 24(3):189–206. doi: 10.1111/j.1538-4632.1992.tb00261.x
31. ESRI. Common Regression Problems, Consequences, and Solutions in Regression Analysis Basics. California: Esri company (2011).
32. Raza O, Mansournia MA, Foroushani AR, Holakouie-Naieni K. Geographically weighted regression analysis: a statistical method to account for spatial heterogeneity. Arch Iran Med. (2019) 22(3):155–60. PMID: 31029072.31029072
33. Mennis J. Mapping the results of geographically weighted regression. Landmarks Mapp. (2017):204–17. doi: 10.4324/9781351191234-20
34. Shifti DM, Chojenta C, Holliday EG, Loxton D. Application of geographically weighted regression analysis to assess predictors of short birth interval hot spots in Ethiopia. PLoS One. (2020) 15(5):e0233790. doi: 10.1371/journal.pone.0233790
35. Hailegebreal S, Seboka BT, Ahmed MH, Teferi GH, Regasa Z, Tekabe B, et al. Individual and community-level factors associated with modern contraceptive use among adolescent girls and young women in Ethiopia: a multilevel analysis of 2016 Ethiopia Demographic and Health Survey. Arch Public Health. (2021) 79(1):204. doi: 10.1186/s13690-021-00736-8
36. Beson P, Appiah R, Adomah-Afari A. Modern contraceptive use among reproductive-aged women in Ghana: prevalence, predictors, and policy implications. BMC Womens Health. (2018) 18(1):157. doi: 10.1186/s12905-018-0649-2
37. Prata N, Bell S, Fraser A, Carvalho A, Neves I, Nieto-Andrade B. Partner support for family planning and modern contraceptive use in Luanda, Angola. Afr J Reprod Health. (2017) 21(2):35–48. doi: 10.29063/ajrh2017/v21i2.5
38. Worku AG, Tessema GA, Zeleke AA. Trends of modern contraceptive use among young married women based on the 2000, 2005, and 2011 Ethiopian Demographic and Health Surveys: a multivariate decomposition analysis. PLoS One. (2015) 10(1):e0116525. doi: 10.1371/journal.pone.0116525
39. Negash BT, Chekol AT, Wale MA. Modern contraceptive method utilization and determinant factors among women in Ethiopia: multinomial logistic regression mini-EDHS-2019 analysis. Contracept Reprod Med. (2023) 8(1):40. doi: 10.1186/s40834-023-00235-x
40. Hailegebreal S, Dileba Kale T, Gilano G, Haile Y, Endale Simegn A. Modern contraceptive use and associated factors among reproductive-age women in Ethiopia: multilevel analysis evidence from 2019 Ethiopia mini demographic and health survey. J Mater Fetal Neonatal Med. (2023) 36(2):2234067. doi: 10.1080/14767058.2023.2234067
41. Belachew TB, Negash WD. Modern contraceptive utilisation and its associated factors among reproductive age women in high fertility regions of Ethiopia: a multilevel analysis of Ethiopia Demographic and Health Survey. BMJ Open. (2023) 13(2):e066432. doi: 10.1136/bmjopen-2022-066432
42. Bolarinwa OA, Ajayi KV, Okeke SR, Hailegebreal S, Odimegwu C. Spatial distribution and multilevel analysis of factors associated with long-acting reversible contraceptive use among sexually active women of reproductive age in Nigeria. Arch Public Health. (2023) 81(1):99. doi: 10.1186/s13690-023-01110-6
43. Sambah F, Aboagye RG, Seidu AA, Tengan CL. Long-acting reversible contraceptives use among adolescent girls and young women in high fertility countries in sub-Saharan Africa. Reprod Health. (2022) 19(1):209. doi: 10.1186/s12978-022-01494-8
44. Aychew EW, Bekele YA, Ayele AD, Dessie AM, Dagnew GW. Utilization of long-acting contraceptive methods and associated factors among married women in Farta Woreda, Northwest Ethiopia: a community-based mixed method study. BMC Women’s Health. (2022) 22(1):533. doi: 10.1186/s12905-022-02092-3
45. Pazol K, Zapata LB, Dehlendorf C, Malcolm NM, Rosmarin RB, Frederiksen BN. Impact of contraceptive education on knowledge and decision making: an updated systematic review. Am J Prev Med. (2018) 55(5):703–15. doi: 10.1016/j.amepre.2018.07.012
46. Tigabu S, Demelew T, Seid A, Sime B, Manyazewal T. Socioeconomic and religious differentials in contraceptive uptake in western Ethiopia: a mixed-methods phenomenological study. BMC Women’s Health. (2018) 18:1–10. doi: 10.1186/s12905-018-0580-6
47. Obasohan PE. Religion, ethnicity and contraceptive use among reproductive age women in Nigeria. Int J MCH AIDS. (2015) 3(1):63.27621987
48. Thakuri DS, Singh YKC, Karkee R, Khatri RB. Knowledge and practices of modern contraceptives among religious minority (Muslim) women: a cross-sectional study from Southern Nepal. PLoS One. (2022) 17(12):e0278899. doi: 10.1371/journal.pone.0278899
49. Omran A-R. Family Planning in the Legacy of Islam. United Kingdom: Taylor and Francis group (2012).
50. Adedini SA, Omisakin OA, Somefun OD. Trends, patterns and determinants of long-acting reversible methods of contraception among women in sub-Saharan Africa. PLoS One. (2019) 14(6):e0217574. doi: 10.1371/journal.pone.0217574
Keywords: long-acting contraceptive, geographically weighted regression, predictors, contraceptive, Ethiopia
Citation: Abate HK, Azagew AW, Kassahun CW, Wassie M, Mekonnen CK, Wassie YA and Zegeye AF (2024) Predictors of long-acting contraceptive utilization hot spots in Ethiopia: using geographical weighted regression analysis. Front. Glob. Womens Health 5:1420476. doi: 10.3389/fgwh.2024.1420476
Received: 20 April 2024; Accepted: 1 July 2024;
Published: 12 August 2024.
Edited by:
Allen Kabagenyi, Makerere University, UgandaReviewed by:
Lingli Sun, Peking University, China© 2024 Abate, Azagew, Kassahun, Wassie, Mekonnen, Wassie and Zegeye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hailemichael Kindie Abate, aGFpbGUyMDZrQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.