- 1Health Service Quality Improvement Directorate, Gandhi Memorial Hospital, Addis Ababa, Ethiopia
- 2National Data Management & Analytic Center, Ethiopian Public Health Institute, Addis Ababa, Ethiopia
- 3Department of Nursing and Midwifery, St. Peter's Specialized Hospital, Addis Ababa, Ethiopia
- 4Department of Public Health, Menelik II Medical and Health Science College, Addis Ababa, Ethiopia
- 5Department of Public Health, Yekatit 12 Hospital Medical College, Addis Ababa, Ethiopia
Background: Obstetric violence during labor and delivery is one of the main reasons that women do not seek care from health caregivers in health facilities. Developing respectful maternity care services for women is the most important approach to ensure better newborn and maternal outcomes.
Objective: This study aimed to assess the magnitude of obstetric violence and associated factors among women who gave birth at public hospitals in Addis Adaba city administration, Ethiopia.
Methods: An institution-based cross-sectional study was carried out among 409 mothers who had given birth at two public hospitals (Gandhi Memorial Hospital and Abebech Gobena Mothers and Children's Health Hospital) in Addis Ababa, Ethiopia, from 1 to 30 May 2023. A systematic sampling method was applied and data were collected using a structured face-to-face interview questionnaire and entered into EpiData 3.1. The data were analyzed using Statistical Package for Social Science version 25. Bi-variable and multivariate analyses were performed. Statistical significance was declared at a P-value <0.05.
Results: In total, 318 mothers [77.8% with a 95% CI (73.64–81.96)] had experienced obstetric violence in the study settings. Being more educated [Adjusted Odds Ratio (AOR) = 6.43; 95% CI 2.92–14.17], having ≥4 antenatal care contacts (AOR = 3.59; 95% CI 1.91–6.75), being multiparous (AOR = 2.65; 95% CI 1.32–5.32), induction of labor (AOR = 3.39; 95% CI 1.69–6.79), vaginal delivery (AOR = 0.25; 95% CI 0.11–0.62), and female birth attendants AOR = 2.42, 95% CI (1.31–4.47) were significantly associated with obstetric violence.
Conclusion: More than three-fourths of the participants experienced obstetric violence. Thus, stakeholders need to develop interventions by taking all risk factors of obstetric violence into account.
Introduction
Obstetric violence (OV) refers to a range of abusive or dehumanizing practices and behaviors that result in women’s loss of independence and the inability to make free decisions about their own bodies and sexual activities, and can occur during pregnancy, childbirth, or the postpartum period (1, 2). According to Brower and Hills, OV can be classified into seven forms: i.e., physical abuse, non-confidential care, non-dignified care, non-consented care, abandonment/neglected care, discrimination, and detention (3–5).
Globally, approximately 140 million births occur each year and those women have been advised to give birth in healthcare institutions to ensure access to skilled healthcare providers. However, accessing labor and delivery services in healthcare institutions may not be guaranteed due to various forms of OV including physical abuse, non-confidential care, non-dignified care, non-consented care, neglected care, discrimination, and detention in many facilities (3, 6–8).
Reducing maternal and child mortality is a worldwide concern, as stated in the Millennium Development Goals (MDGs) and the Sustainable Development Goals (SDGs), which aim to limit the maternal mortality rate to less than 70 per 100,000 live births and neonatal mortality to at least 12 per 1,000 live births (9). Maternal and neonatal mortalities are unacceptably high; 303,000 and 2.7 million mortalities occurred globally in 2015 respectively. Of these, almost all of the mortalities (99%) occurred in underdeveloped countries, including sub-Saharan Africa (SSA) (10).
OV is one of the silent contributing factors to both maternal and newborn morbidity and mortality, as many women experience mistreatment during labor and delivery in health institutions around the world. Furthermore, it is more prevalent in populations with limited resources, and it is also a factor in a woman’s choice of her next child’s birthplace (11).
According to the 2019 Ethiopia Mini Demographic and Health Survey (EMDHS), the prevalence of institutional delivery was low (48%) (12). Lack of respectful care, a fear of showing one’s body to health professionals, and the perceived cost of giving birth in a health facility were identified as factors contributing to low delivery rates in facilities (13).
When women experience OV from their healthcare givers during institutionalized childbirth, it violates the laboring women's right to respectful maternity care (RMC), putting their health, life, bodily integrity, and equality at risk (14).
The fear of these non-dignified and abusive treatments that women often experience during institutional-based childbirth is the main hindrance to utilizing skilled care rather than any other recognized barriers, especially in countries with high maternal mortality (15, 16).
In developing countries, including Ethiopia, the lack of RMC during labor and delivery continues to cause problems, as shown by the maternal morbidity and mortality rates (17, 18). The poor practice of RMC, i.e., obstetric violence during labor and delivery, leads to low healthcare facility-based births and results in slow progress in the attainment of an improved healthcare delivery system in the country (17, 19, 20).
In addition to these issues, there is limited research that assesses OV during institution-based childbirth in the study area.
Assessing the prevalence of these hidden and unacceptable practices during childbirth is a critical component for strengthening maternity services in Ethiopia and reducing maternal and newborn morbidity and mortality. Thus, this study aimed to assess the prevalence and associated factors of OV among women who gave birth at public hospitals in Addis Adaba city administration, Ethiopia.
Methods
Study design and period
The study employed an institutional-based cross-sectional design in two randomly selected public hospitals in Addis Ababa, i.e., Abebech Gobena Mothers and Children's Health Hospital (AGMCHH) (an affiliate of Yekatit 12 Hospital Medical College) and Gandhi Memorial Hospital (GMH) from 1 to 30 May 2023. Addis Adaba city administration has six public hospitals and each hospital has maternity services. Both the selected hospitals provide services such as family planning, antenatal care (ANC), labor and delivery, postnatal care, a maternal intensive care unit (MICU), comprehensive abortion care (CAC), cervical pre-cancer screening and treatment, infertility treatment, a fetal-maternal subspecialty clinic, immunization, a neonatal intensive care unit (NICU), a pharmacy, and a laboratory service. The hospitals are also staffed with intern doctors, midwives, resident doctors, obstetricians, and other healthcare workers and supporting staff.
Source and study population
The source population was all the mothers who had given birth at Addis Adaba city administration public hospitals during the study period.
Inclusion and exclusion criteria
Women who had given birth at GMH and AGMCHH and women who had completed their hospital stay just after a discharge decision had been made (i.e., to prevent the underreporting of OV during their hospital stay) during the study period were included in the study while women who had experienced a loss of consciousness or were unable to remember their labor and delivery process were excluded.
Sample size determination
The minimum sample size required for this study was determined using both specific objectives and the largest sample size was taken to include all forms of OV. Thus, a single population proportion formula was used which considered the following assumptions: proportion of physical abuse (46.9%), non-consented care (63.6%), non-dignified care (55.3%), stigma and discrimination (9.3%), non-confidential care (32.3%), neglected care (12.7%), and no mothers who reported any form of detention in the healthcare facility. These figures were taken from a previous study conducted at the University of Gondar Comprehensive Specialized Hospital (17). The level of confidence was 95% and the margin of error was 5% (d = 0.05). The sample size for each form of OV was calculated as follows, and the largest number was used:
where p is the proportion of women who experienced obstetric violence during childbirth, q is the proportion of women who experienced no obstetric violence during childbirth, and d is the margin of error.
Thus, the final sample size was found to be 421 after allowing for a 10% non-response rate.
Sample size determination for the second objective, i.e., factors associated with OV, was calculated using OpenEpi by using some variables from previous studies (19, 21, 22) (Supplementary Table S1).
Sampling technique and procedure
To include 421 women in this study, a proportional allocation method was used based on the number of women who gave birth at the two hospitals in the month preceding the data collection period. Thus, 208 and 213 women were enrolled from GMH and AGMCHH, respectively. A systematic random sampling technique was used for the enrollment of the 421 postpartum mothers who gave birth in the study area. Using the assumptions of N (the estimated deliveries in the two hospitals in a month) = 1,780 and n (the required minimum sample size including 10% non-response rate) = 421, we calculated the sampling fraction (k): where k = N/n ⇒ 1,780/421 ≈ 4. Thus, the study participants were selected using a sampling interval of 4.
Dependent and independent variables
The outcome variable was obstetric violence and the explanatory variables included socio-demographic characteristics and provider-related, client-related, and obstetric factors.
Operational definitions
Obstetric violence was defined as having occurred when the participants answered “yes” for at least one type or form of OV. Each form of OV has its own verification criteria, and a total of 25 verification criteria were used. Thus, the women who answered “yes” to at least one type/form/of OV were considered to have been victims of OV (3, 23) (Annex: verification criteria in the Supplementary Material).
Data collection tools and procedures
Data were collected in face-to-face interviews using a structured questionnaire adapted from the WHO intrapartum care recommendations for a positive childbirth experience and other related literature (3, 23). OV was measured using seven performance standards or forms of violence including physical abuse, non-confidential care, non-dignified care, non-consented care, neglected care, discrimination, and detention using the verification criteria (a total of 25 criteria) developed by the Maternal and Child Health Integrated Program (MCHIP). The reliability of the tool was checked by computing Cronbach's alpha with a normal range value (0.8).
The questionnaire was first prepared in English, translated into the local language (Amharic), and then translated back into English by the principal investigator to check the consistency. Four midwives who provide free services outside the study facilities, along with two professional midwives, were recruited as data collectors and supervisors, respectively.
Data quality assurance
A daylong training session was conducted for data collectors and supervisors (four data collectors and two supervisors) on the objectives and benefits of the study, individuals’ rights, informed consent, and data collecting techniques. Further pre-testing of the tool with 5% of the sample size, i.e., 21 mothers at Zewditu Memorial Hospital (one of the six hospitals in Addis Adaba city administration) which was not included in the study, was done. To prevent non-reporting or underreporting of OV during their hospital stay, postpartum mothers were interviewed just after they received their discharge decision.
Data processing and analysis
Data was entered into EpiData version 3.1 and exported to the Statistical Package for Social Science (SPSS) version 25 software package for analysis. Before analysis, data processing (cleaning, counting, categorizing, and computing) was performed. Descriptive statistics were employed by computing summary statistics such as frequency, mean, percentages, and standard deviations. Assumptions of logistic regression were checked before analysis. The Hosmer–Lemeshow test was used to test the model's goodness of fit. Binary logistic regression was conducted to assess the crude relationship between the independent variables and the dependent variable. All variables with a P-value <0.25 were considered candidates for the multivariate logistic regression. Multivariate logistic regression was conducted to assess the independent effect of each variable on the outcome variable. The results were presented in the form of texts, tables, and/or figures. The degree of association between the variables was demonstrated by the odds ratio and significance level using a 95% confidence interval.
Results
Socio-demographic characteristics of the study population
A total of 421 postpartum women were invited, of which 409 were interviewed with a 97.1% response rate. The socio-demographic information provided by the respondents was not significantly different between the two hospitals. Of the respondents, 219 (53.5%) were aged between 25 and 34 years with a mean age of 27.58 years (±SD 4.85) and minimum and maximum ages of 19 and 40, respectively. Furthermore, 274 (67.0%) study participants were permanently living in urban areas and 371 (90.7%) of the mothers were married. Regarding the educational status of the participants, 218 (53.3%) had attended secondary school and above and 63 (15.4%) had no formal education. Finally, 192 (46.9%) participants were private employees whereas 23 (5.6%) mothers were merchants, students, or daily laborers by occupation (Table 1).
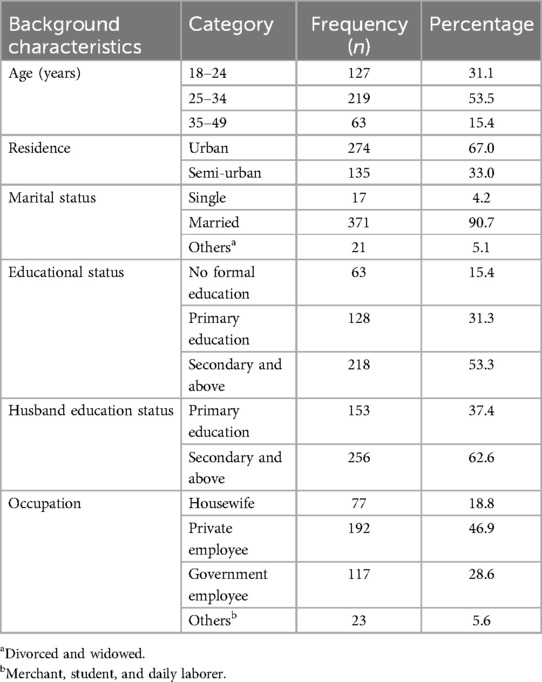
Table 1. Socio-demographic characteristics of the women who gave birth at public hospitals in Addis Ababa, Ethiopia, 2023 (n = 409).
Obstetric characteristics of mothers
Of the total number of respondents, 395 (96.6%) of mothers had ANC contact during their recent pregnancy, and among these, 280 (70.9%) had four or more ANC contacts and 218 (55.2%) had received it from midwives. Furthermore, 208 (50.9%) respondents were multiparous and 238 (58.2%) mothers gave birth through spontaneous vaginal delivery (SVD). For 142 (34.7%) of the respondents, labor was induced or augmented and 95% of the mothers (n = 218) had a previous history of institutional delivery (Table 2).
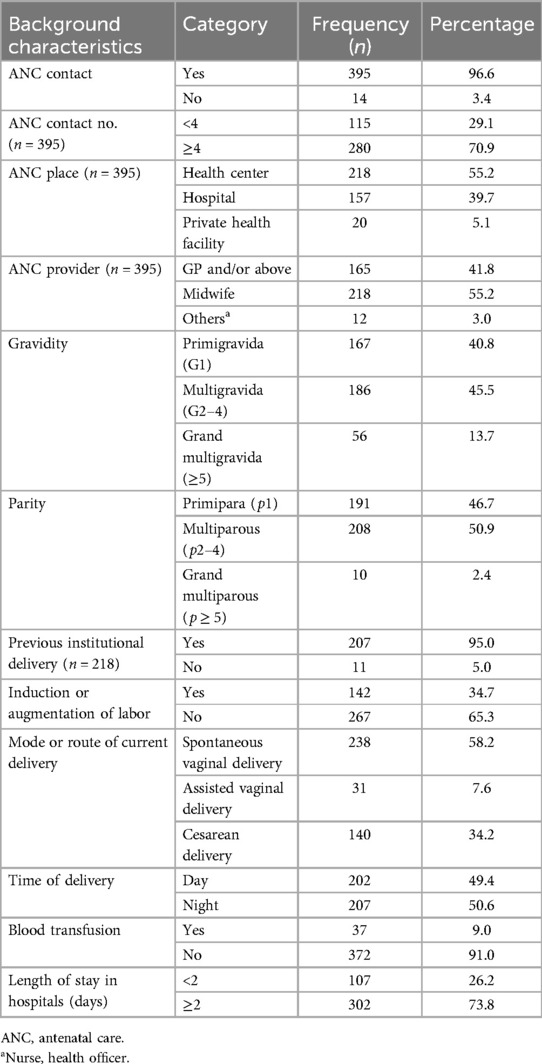
Table 2. Obstetric characteristics of the mothers who gave birth at public hospitals in Addis Ababa, Ethiopia, 2023 (n = 409).
Individual and provider-related characteristics
From the total respondents, almost three in five (249, 60.9%) of the mothers were not involved in decisions regarding their labor and delivery process, whereas half (50.4%) of the mothers normalized obstetric violence. More than half of the interviewed mothers, (215, 52.6%) were attended by female health professionals and three in seven of them (43.3%) were attended by midwives (Table 3).
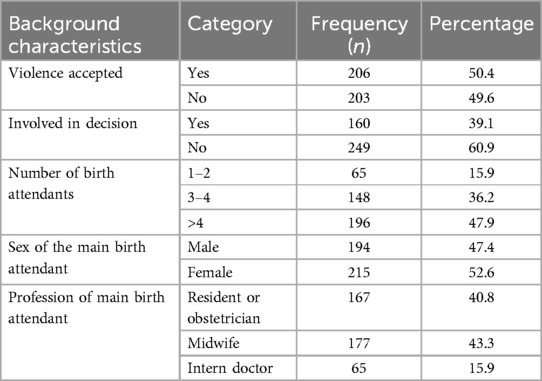
Table 3. Individual and provider-related characteristics of mothers who gave birth at public hospitals in Addis Ababa, Ethiopia, 2023 (n = 409).
Prevalence and forms of obstetric violence
Among the 409 interviewed mothers, 318 [77.8% with a 95% CI (73.64–81.96)], reported having experienced at least one form of obstetric violence (see Figure 1).
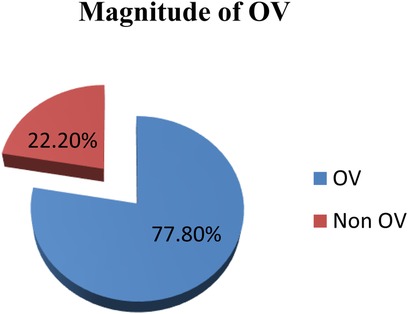
Figure 1. Prevalence of obstetric violence among mothers who gave birth at public hospitals in Addis Ababa, Ethiopia, 2023 (n = 409).
The most commonly experienced form of obstetric violence was non-consented care as 264 [64.5% with a 95% CI (59.7–69.3)] mothers reported having experienced it. This was followed by non-confidential care with 172 [42.1% with a 95% CI (37.3–46.9)] and physical abuse with 156 [38.1% with a 95% CI (33.4–42.9)] participants. Non-dignified care, neglected care, and discriminated care were reported by 110 (26.9%), 107 (26.2%), and 54 (13.2%) mothers, respectively, and no mother reported any form of detention in the healthcare facilities during childbirth (see Figure 2).
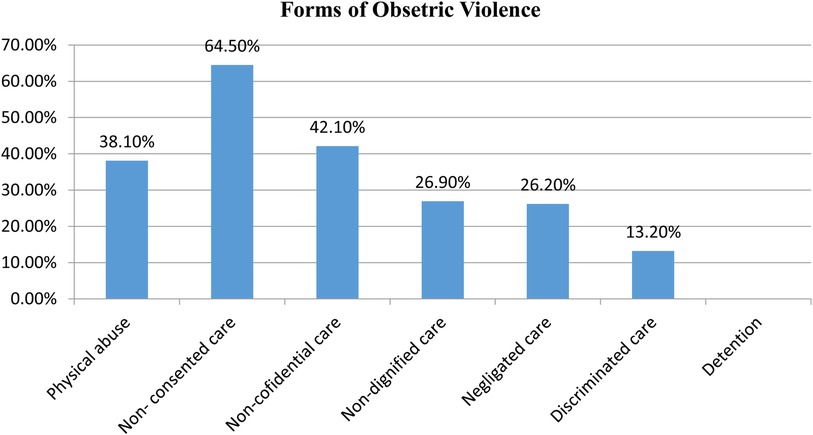
Figure 2. Percentage of each form of OV among mothers who gave birth at public hospitals in Addis Ababa, Ethiopia, 2023 (n = 409).
The most frequently reported criterion of OV was women not being allowed to give consent to healthcare providers before any procedure which was reported by 167 (40.8%) women. The healthcare provider not using curtains or other visual barriers to protect their privacy was reported by 148 (36.2%) mothers and the healthcare provider using fundal pressure was reported by 79 (19.3%). Furthermore, healthcare providers making negative comments toward them was reported by 54 (13.2%) participants, 87 (21.3%) reported healthcare providers ignoring them during labor while they were calling for help, and healthcare providers discriminating against them due to their socio-demographic status was reported by 47 (11.5%). These were reported in the domains of non-consented care, non-confidential care, physical abuse, non-dignified care, neglected care, and discriminated care (Supplementary Table S5).
Factors associated with obstetric violence during institutional childbirth
In the bi-variable analysis, the age of the mother, educational status of the mother, number of ANC contacts of the mother, parity, induction or augmentation of labor, route of delivery, time of delivery, length of stay in the hospital, involvement in decisions, sex of main birth attendant, and profession of main birth attendant were associated with OV with P-values <0.25. Thereafter, in the multivariate logistic regression, a total of 11 explanatory variables with a P-value <0.25 in the bivariate logistic regression analysis were regressed against OV. As a result, in the multivariable logistic regression analysis, maternal educational status, ANC contact number, parity, induction or augmentation of labor, route of delivery, and sex of main birth attendant were significantly associated with OV at a P-value of <0.05.
Accordingly, mothers who had received a primary school education were two times more likely to report obstetric violence as compared to those who had no formal education [Adjusted Odds Ratio (AOR) = 2.42; 95% CI (1.10–5.35)]; while mothers who received secondary school education and above were six times more likely to report OV as compared to those who had no formal education [AOR = 6.43; 95% CI (2.92–14.17)].
Mothers who had four or more ANC contacts were 3.59 times more likely to report obstetric violence than their counterparts [AOR = 3.59, 95% CI (1.91–6.75)], whereas obstetric violence among multiparous mothers was 2.65 times higher than their counterparts [AOR = 2.65, 95% CI (1.32–5.32)].
The odds of experiencing obstetric violence among mothers whose labor had started with induction or augmentation were three times higher than those mothers who started labor spontaneously [AOR = 3.39, 95% CI (1.69–6.79)].
Mothers who delivered through cesarean delivery were 74.6% less likely to report obstetric violence as compared to women who gave birth through spontaneous vaginal delivery [AOR = 0.25, 95% CI (0.11–0.62)]. Finally, mothers who delivered with female birth attendants were two times more likely to experience OV as compared to mothers who delivered with male birth attendants [AOR = 2.42, 95% CI (1.31–4.47)] (Table 4).
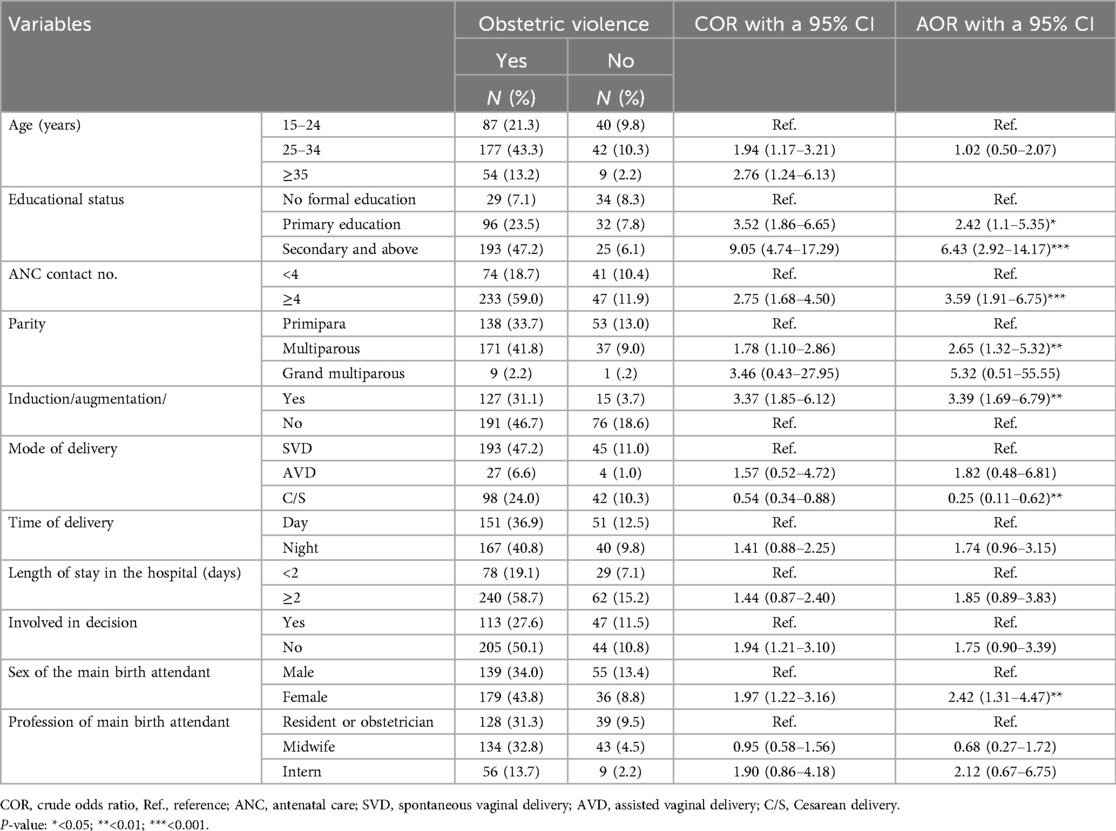
Table 4. Factors associated with OV among mothers during institutional childbirth at public hospitals in Addis Ababa, Ethiopia, 2023 (n = 409).
Discussion
This study aimed to assess obstetric violence and its associated factors among women who gave birth in the selected health institutions. The study showed a high prevalence of OV as nearly four out of five [77.8% with a 95% CI (73.64–81.96)] of the women who participated reported having experienced at least one type of OV. OV was significantly associated with having received a secondary school and above education, ≥4 ANC contacts, being multiparous, labor started with induction, vaginal delivery, and being attended by a female birth attendant. The prevalence of OV in the current study is similar to other studies done in Ethiopia such as in South Wollo (79.4%) (3), Gondar University Comprehensive Specialized Hospital (75.1%) (17), and the Gedeo zone (79.7%) (19), as well as studies done in Mozambique (80%) (24), Italy (78.4%) (25), and Europe (76.3%) (26).
However, the prevalence of OV in this study is higher than a previous study conducted in Malawi (42.5%) (27) and a systematic review in SSA (44.09%) (28) as well as other previous studies in Spain (Part I, 38.3%) (29), Mexico (33.3%) (30), and Brazil (18.3%) (31). This finding is also higher than that reported in other studies conducted in Ethiopia such as in Tigray (22%) (32) and north Shewa (51.4%) (33), as well as the overall pooled prevalence of a systematic review and meta-analysis in Ethiopia (51.56%) (5). This difference might be due to variations in the types of data collection methods, study settings, and sample size (27, 28, 34). Unlike the current study settings (tertiary level), which had high case flows and many complicated referral situations, the majority of the aforementioned studies were conducted in low-level settings with limited client flow, which might mean healthcare providers are more likely to act abusively when there are too many clients and complicated problems. Other reasons might be due to differences in the study subjects, study period, and the timing of the interview after childbirth as in previous studies interviewees might have been affected by recall bias (29, 30, 34).
In contrast, the prevalence of OV in this study is lower than that reported in studies conducted in fourteen hospitals in Peru and Pakistan which showed a prevalence of 97.4% and 99.7%, respectively (35, 36). This difference might be due to the data in this study being collected through direct interviews with the mothers but in the previous studies, data was collected through direct observation. Hence, when data is collected through interviews, the prevalence of OV might be affected by the participants’ recall capacity and level of perception. The difference in prevalence could also be related to variations in the study settings and sample size. The current study's finding is also lower than that of studies done in Hawassa and in the North Showa zone of Ethiopia, both of which showed OV was experienced by all the study subjects (6, 37). This discrepancy might be attributed to the timing of the interview after childbirth and the verification criteria for the outcome variable that the researchers used. In this study, physical abuse was measured by six verification criteria while in the study done in North Showa, it was measured by 10 verification criteria. This study used as dependent variables the seven forms of OV women experience during facility-based childbirth but in the study done in Hawassa, Ethiopia, the domain of OV that was measured was different.
Regarding factors associated with OV during institutional delivery, mothers who had received education were more likely to report obstetric violence as compared to those who had no formal education (two times and six times more among mothers who had a primary school education and mothers who had a secondary school and above education, respectively). This finding is similar to studies conducted in Mexico and Nigeria, and other studies conducted in Ethiopia such as those in the Gedeo zone and at the University of Gondar Comprehensive Specialized Hospital (17, 19, 20, 30). This association could be due to the fact that educated women are more aware of their rights, are more perceptive, and thus more likely to report experiencing any sort of OV. It might be also as women become more educated, they become less accepting of any form of mistreatment during labor and delivery as a normal procedure and thus they become confident enough to report it (30, 38).
This study showed that as the number of ANC contacts increased, mothers were more likely to report OV. Accordingly, women who had four or more ANC contacts were 3.6 times more likely to report OV than their counterparts. However, this finding is opposed to studies conducted in Addis Ababa and Assosa, Ethiopia (22, 39), and the variation might be related to the data collection methods and study subjects’ differences. The association in this study could be related to the fact that women with a higher number of ANC contacts can easily ascertain the standard of birth care, are informed of their rights, and have an improved level of awareness of how to report the occurrence of any form of OV. However, even if more ANC contacts are typically encouraged and are linked to better health outcomes for both women and their babies, this may not be guaranteed due to systemic and contextual problems, such as frequent rushed interactions between healthcare providers, which can exacerbate power imbalances and cause them to feel abused (7).
The study has also found that multiparous mothers were at 2.65 times higher risk of experiencing OV than their counterparts. This is similar to studies conducted in Kenya and four regions of Ethiopia (16, 21) and in contrast with the study done in North Showa, Ethiopia (33). This association might be due to the fact that multiparous women have already given birth and are thus more aware of their rights and the standards of obstetric care and are therefore more likely to report OV. Another finding in this study was that OV among mothers whose labor had been started with induction or augmentation was more than three times higher than among those who started labor spontaneously. This might be because inducing labor is related to the risk of failure of induction, the requirement of more medical intervention compared to spontaneous vaginal delivery such as instrumental delivery, the need for cesarean delivery, and the fear of additional obstetric complications such as uterine rupture, postpartum hemorrhage, infection, and neonatal loss (40–42).
Moreover, mothers who delivered through cesarean section were 74.6% less likely to experience obstetric violence as compared to those women who gave birth through spontaneous vaginal delivery. Studies in Peru and the Hadiya zone of Ethiopia shared similar results (10, 35). Even though indications for cesarean section were not included as part of the data in this study, the reason might be that mothers who deliver through a cesarean delivery have fewer procedures than those who give birth vaginally, as the latter may experience repeated vaginal examination, prolonged labor, other birth-related complications, and an episiotomy without anesthesia.
In contrast, other studies showed that mothers who gave birth through SVD were less likely to experience OV compared to those women who gave birth through cesarean delivery (18, 43). This might be due to the fact that mothers who had a cesarean birth are more likely to have postpartum pain and a more difficult and longer recovery.
Finally, the results of this study also revealed that mothers who delivered with female birth attendants were also two times more likely to face OV as compared to mothers who delivered with male birth attendants. This finding is in line with the studies conducted in Hawassa and Addis Ababa (22, 37). The finding may be because male providers were more commonly considered to participate in RMC activities than female providers (44).
Limitations of the study
Since it was a cross-sectional study design, it is difficult to establish temporal relationships between the explanatory variables and the outcome variable.
Conclusion
The prevalence of obstetric violence was high in the study setting and was significantly associated with having a secondary school and above education, having four and more ANC contacts, being multiparous, induction or augmentation of labor, vaginal delivery, and a delivery attended with female birth attendants.
The Ministry of Health needs to strengthen initiatives to reduce obstetric violence by incorporating healthcare providers’ attitudes toward respectful maternity care and considering all risk factors. Healthcare providers should handle all mothers with compassion and a respectful manner, taking into account that mothers are different regardless of their mode of delivery and parity. The continuous provision of education and counseling throughout their ANC follow-up should be strengthened and awareness raised to increase the number of ANC contacts. Furthermore, maternity care providers should prioritize reducing OV among mothers whose labor had been started with induction or augmentation by providing proper information about the indication of inducing labor, its risks, and its complications. Female birth attendants have to meet respectful maternity care standards. We recommend additional research using a mixed approach in different study settings.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical clearance was obtained from Yekatit 12 Hospital Medical College, School of Public Health; Institutional Review Board (IRB), protocol number 170/23. The study was also granted permission by the Addis Ababa City Administration Health Bureau (AACAHB). Written informed consent was also obtained from each study respondent after a clear explanation about the benefits and harm of the study.
Author contributions
GS: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. GT: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. BS: Conceptualization, Formal Analysis, Methodology, Writing – original draft, Writing – review & editing. NT: Conceptualization, Formal Analysis, Project administration, Visualization, Writing – review & editing. AH: Conceptualization, Formal Analysis, Methodology, Visualization, Writing – review & editing. FS: Data curation, Methodology, Visualization, Writing – review & editing. DN: Conceptualization, Data curation, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
Above all, we would like to acknowledge the Yekatit 12 Hospital Medical College for facilitating the ethical clearance and also the Addis Ababa Health Bureau for granting permission. We would like to also express our sincere thanks and appreciation to data collectors, supervisors, and all the study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2024.1417676/full#supplementary-material
Abbreviations
AGMCHH, Abebech Gobena Mothers and Children's Health Hospital; GMH, Gandhi Memorial Hospital; OV, obstetric violence; RMC, respectful maternity care.
References
1. Azzam OA, Sindiani AM, Eyalsalman MM, Odeh MK, AbedAlkareem KY, Albanna SA, et al. Obstetric violence among pregnant Jordanian women: an observational study between the private and public hospitals in Jordan. Healthc. (2023) 11(5):1–10. doi: 10.3390/healthcare11050654
2. Mena-Tudela D, Iglesias-Casás S, González-Chordá VM, Valero-Chillerón MJ, Andreu-Pejó L, Cervera-Gasch Á. Obstetric violence in Spain (Part III): healthcare professionals, times and areas. Int J Environ Res Public Health. (2021) 18(7):3359. doi: 10.3390/ijerph18073359
3. Maldie M, Egata G, Chanie MG, Muche A, Dewau R, Worku N, et al. Magnitude and associated factors of disrespect and abusive care among laboring mothers at public health facilities in Borena District, South Wollo, Ethiopia. PLoS One. (2021) 16(11 November):1–18. doi: 10.1371/journal.pone.0256951
4. Minckas N, Gram L, Smith C, Mannell J. Disrespect and abuse as a predictor of postnatal care utilisation and maternal-newborn well-being: a mixed-methods systematic review. BMJ Glob Heal. (2021) 6(4):1–14. doi: 10.1136/bmjgh-2020-004698
5. Habte A, Tamene A, Woldeyohannes D, Endale F, Bogale B, Gizachew A. The prevalence of respectful maternity care during childbirth and its determinants in Ethiopia: a systematic review and meta-analysis. PLoS One. (2022) 17(11 November):1–23. doi: 10.1371/journal.pone.0277889
6. Adinew YM, Hall H, Marshall A, Kelly J. Disrespect and abuse during facility-based childbirth in central Ethiopia. Glob Health Action. (2021) 14(1). doi: 10.1080/16549716.2021.1923327
7. Mengesha MB, Desta AG, Maeruf H, Hidru HD. Disrespect and abuse during childbirth in Ethiopia: a systematic review. Biomed Res Int. (2020) 2020:4–10. doi: 10.1155/2020/8186070
8. World Health Organization. Intrapartum Care for a Positive Childbirth Experience. Geneva: World Health Organization (2018). p. 212.
9. World Health Organization. Maternal Mortality Evidence Brief. Geneva: World Health Organization (2020), No. 1, p. 1–4.
10. Mengistie T, Mulatu T, Alemayehu A, Yadeta TA, Dheresa M. Respectful maternity care among women who gave birth at public hospitals in Hadiya Zone, Southern Ethiopia. Front Public Heal. (2022) 10:949943. doi: 10.3389/fpubh.2022.949943
11. Ribeiro DO, Gomes GC, Oliveira AMN, Alvarez SQ, Gonçalves BG, Acosta DF. Obstetric violence in the perception of multiparous women. Rev Gauch Enferm. (2020) 41:e20190419. doi: 10.1590/1983-1447.2020.20190419
12. Ethiopian Public Health Institute (EPHI), ICF. Ethiopia Mini Demographic and Health Survey 2019: Final Report. (2021). p. 1–207. Available online at: https://dhsprogram.com/pubs/pdf/FR363/FR363.pdf (accessed May 2021).
13. Asres GD. Satisfaction and associated factors among mothers delivered at Asrade Zewude Memorial Primary Hospital, Bure, West Gojjam, Amhara, Ethiopia: a cross sectional study. Prim Heal Care Open Access. (2018) 8:14–28. doi: 10.5897/JPHE2018.1013
14. Vogel JP, Bohren MA, Tunçalp O, Oladapo OT, Gülmezoglu AM. Promoting respect and preventing mistreatment during childbirth. BJOG An Int J Obstet Gynaecol. (2016) 123(5):671–4. doi: 10.1111/1471-0528.13750
15. Chadwick RJ. Obstetric violence in South Africa. South African Med J. (2016) 106(5):423–4. doi: 10.7196/SAMJ.2016.v106i5.10708
16. Abuya T, Warren CE, Miller N, Njuki R, Ndwiga C, Maranga A, et al. Exploring the prevalence of disrespect and abuse during childbirth in Kenya. PLoS One. (2015) 10(4):e0123606. doi: 10.1371/journal.pone.0123606
17. Mihret MS. Obstetric violence and its associated factors among postnatal women in a specialized comprehensive hospital, Amhara Region, Northwest Ethiopia. BMC Res Notes. (2019) 12(1):1–7. doi: 10.1186/s13104-019-4614-4
18. Ferede WY, Gudayu TW, Gessesse DN, Erega BB. Respectful maternity care and associated factors among mothers who gave birth at public health institutions in South Gondar Zone, Northwest Ethiopia 2021. Women’s Heal. (2022) 18. 17455057221116505
19. Molla W, Wudneh A, Tilahun R. Obstetric violence and associated factors among women during facility based childbirth at Gedeo Zone, South Ethiopia. BMC Pregnancy Childbirth. (2022) 22(1):1–14. doi: 10.1186/s12884-022-04895-6
20. Ogunlaja OA, Fehintola OA, Ogunlaja IP, Popoola G, Idowu A, Awotunde OT, et al. “Respectful maternity care” or “Disrespect and abuse during maternity care”; experience of pregnant women in Ogbomoso, South West Nigeria. Rwanda Med J. (2017) 74(3):6–9. Available online at: https://www.researchgate.net/publication/325555880 (accessed November 01, 2022).
21. Sheferaw ED, Kim YM, Van Den Akker T, Stekelenburg J. Mistreatment of women in public health facilities of Ethiopia. Reprod Health. (2019) 16(1):1–10. doi: 10.1186/s12978-019-0781-y
22. Assefa AW. Obstetric violence and associated factors among HIV-infected women receiving birth care at public health facilities in Addis Ababa, Ethiopia. Res Sq. (2022):1–15. doi: 10.21203/rs.3.rs-1740887/v1
23. WHO. The prevention and elimination of disrespect and abuse during facility-based childbirth: WHO statement. World Health Organization. (2015) 4. https://iris.who.int/handle/10665/134588 (accessed November 01, 2022).
24. Galle A, Manaharlal H, Cumbane E, Picardo J, Griffin S, Osman N, et al. Disrespect and abuse during facility-based childbirth in southern Mozambique: a cross-sectional study. BMC Pregnancy Childbirth. (2019) 19(1):1–13. doi: 10.1186/s12884-018-2145-y
25. Scandurra C, Zapparella R, Policastro M, Continisio GI, Ammendola A, Bochicchio V, et al. Obstetric violence in a group of Italian women: socio-demographic predictors and effects on mental health. Cult Heal Sex. (2021) 11(2022):1466–80. doi: 10.1080/13691058.2021.1970812
26. Reuther ML. Prevalence of obstetric violence in Europe: exploring associations with trust, and care-seeking intention. (Student theses). (2021):1–54. Corpus ID: 238162146. Available online at: https://purl.utwente.nl/essays/87962 (accessed August 03, 2021).
27. Hughes CS, Kamanga M, Jenny A, Zieman B, Warren C, Walker D, et al. Perceptions and predictors of respectful maternity care in Malawi: a quantitative cross-sectional analysis. Midwifery. (2022) 112:103403. doi: 10.1016/j.midw.2022.103403
28. Kassa ZY, Tsegaye B, Abeje A. Disrespect and abuse of women during the process of childbirth at health facilities in sub-Saharan Africa: a systematic review and meta-analysis. BMC Int Health Hum Rights. (2020) 20(1):1–9. doi: 10.1186/s12914-020-00242-y
29. Mena-Tudela D, Iglesias-Casás S, González-Chordá VM, Cervera-Gasch Á, Andreu-Pejó L, Valero-Chilleron MJ. Obstetric violence in Spain (Part I): Women’s perception and interterritorial differences. Int J Environ Res Public Health. (2020) 17(21):1–14. doi: 10.3390/ijerph17217726
30. Castro R, Frías SM. Obstetric violence in Mexico: results from a 2016 national household survey. Violence Against Women. (2020) 26(6–7):555–72. doi: 10.1177/1077801219836732
31. Mesenburg MA, Victora CG, Jacob Serruya S, De León RP, Damaso AH, Domingues MR, et al. Disrespect and abuse of women during the process of childbirth in the 2015 Pelotas birth cohort. Reprod Health. (2018) 15(1):1–8. doi: 10.1186/s12978-018-0495-6
32. Gebremichael MW, Worku A, Medhanyie AA, Berhane Y. Mothers’ experience of disrespect and abuse during maternity care in northern Ethiopia. Glob Health Action. (2018) 11(1):1465215. doi: 10.1080/16549716.2018.1465215
33. Amare NS, Mekuriyaw AM, Tesema GW, Ambaw YL. Proportion and associated factors of respectful maternity care during childbirth in North Showa zone public health institutions, North Showa, Ethiopia: an institutional-based cross-sectional study. Front Public Heal. (2022) 10. doi: 10.3389/fpubh.2022.878019
34. Diamond-Smith N, Treleaven E, Murthy N, Sudhinaraset M. Women’s empowerment and experiences of mistreatment during childbirth in facilities in Lucknow, India: results from a cross-sectional study. BMC Pregnancy Childbirth. (2017) 17(2):1–13. doi: 10.1186/s12884-017-1501-7
35. Montesinos-Segura R, Urrunaga-Pastor D, Mendoza-Chuctaya G, Taype-Rondan A, Helguero-Santin LM, Martinez-Ninanqui FW, et al. Disrespect and abuse during childbirth in fourteen hospitals in nine cities of Peru. Int J Gynecol Obstet. (2018) 140(2):184–90. doi: 10.1002/ijgo.12353
36. Azhar Z, Oyebode O, Masud H. Disrespect and abuse during childbirth in district Gujrat, Pakistan: a quest for respectful maternity care. PLoS One. (2018) 13(7):1–11. doi: 10.1371/journal.pone.0200318
37. Tagesse B, Mayisso K. Prevalence and associated factors of disrespectful and abusive care during childbirth among women who gave birth in health facilities in Hawassa city, Southern Ethiopia. A cross-sectional study. Health Biomed Sci. (2018) 11(1):1–22. doi: 10.20372/ejhbs.v11i01.276
38. Lansky S, De Souza KV, De Morais Peixoto ER, Oliveira BJ, Diniz CSG, Vieira NF, et al. Obstetric violence: influences of the senses of birth exhibition in pregnant women childbirth experience. Cienc e Saude Coletiva. (2019) 24(8):2811–24. doi: 10.1590/1413-81232018248.30102017
39. Abamila NM, Agago TA, Garedew MG. Disrespect and abusive maternity care and associated factors in the labor and delivery wards of public health facilities in Assosa Zone, Ethiopia. Ethiop J Reprod Heal. (2022) 14(1):29–37. doi: 10.69614/ejrh.v14i01.534
40. Falk M, Nelson M, Blomberg M. The impact of obstetric interventions and complications on women’s satisfaction with childbirth a population based cohort study including 16,000 women. BMC Pregnancy Childbirth. (2019) 19(1):1–9. doi: 10.1186/s12884-019-2633-8
41. Debele TZ, Cherkos EA, Badi MB, Anteneh KT, Demssie FW, Abdo AA, et al. Factors and outcomes associated with the induction of labor in referral hospitals of Amhara regional state, Ethiopia: a multicenter study. BMC Pregnancy Childbirth. (2021) 21(1):1–8. doi: 10.1186/s12884-021-03709-5
42. Yosef T, Getachew D. Proportion and outcome of induction of labor among mothers who delivered in teaching hospital, Southwest Ethiopia. Front Public Heal. (2021) 9(December):1–7. doi: 10.3389/fpubh.2021.686682
43. Wassihun B, Zeleke S. Compassionate and respectful maternity care during facility based child birth and women’s intent to use maternity service in Bahir Dar, Ethiopia. BMC Pregnancy Childbirth. (2018) 18(1):1–9. doi: 10.1186/s12884-018-1909-8
Keywords: obstetric violence, women, labor and delivery, Ethiopia, respectful maternity care, childbirth
Citation: Simeneh GT, Tesema GW, Seifu BA, Tafesse N, Hailemariam AZ, Suleyiman FM and Nigatu DT (2024) Obstetric violence and associated factors among women who gave birth at public hospitals in Addis Ababa city administration, Ethiopia. Front. Glob. Womens Health 5:1417676. doi: 10.3389/fgwh.2024.1417676
Received: 15 April 2024; Accepted: 30 September 2024;
Published: 25 October 2024.
Edited by:
Shimelash Bitew Workie, Wolaita Sodo University, EthiopiaReviewed by:
Redempta Mbatia, Tanzania Health Promotion Support (THPS), TanzaniaDavid Ramiro-Cortijo, Autonomous University of Madrid, Spain
Copyright: © 2024 Simeneh, Tesema, Seifu, Tafesse, Hailemariam, Suleyiman and Nigatu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Getinet Tilahun Simeneh, Z2V0dGlsYWh1bjdAZ21haWwuY29t
†These authors share first authorship
 Getinet Tilahun Simeneh
Getinet Tilahun Simeneh Getaye Worku Tesema
Getaye Worku Tesema Befikad Assefa Seifu3
Befikad Assefa Seifu3 Nebiyou Tafesse
Nebiyou Tafesse