
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Glob. Womens Health , 29 October 2024
Sec. Sex and Gender Differences in Disease
Volume 5 - 2024 | https://doi.org/10.3389/fgwh.2024.1337553
This article is part of the Research Topic Response, Recovery, and Resilience: Mainstreaming Gender Responsive Programming Within Immunization Systems in Low-and Middle-income Countries View all 7 articles
Background: Despite global efforts, inequities in vaccine uptake remain, influenced by socioeconomic, geographic, cultural, and gender-related factors. In Eastern Sudan, gender disparities are acknowledged, particularly in livelihoods, but their impact on vaccination uptake is unclear. This study aimed to assess the effect of gender-biased parental perceptions on under-immunization among children in Kassala, Eastern Sudan.
Methods: This study was a community-based cross-sectional in rural and urban districts of Kassala locality in Kassala State, Eastern Sudan in November 2022. Data were collected from parents using a pre-tested, structured questionnaire. The Chi-square or Fisher's exact test was conducted to assess the factors associated with under-immunization among children.
Results: Data were collected from 400 parents. Our data reveal that most children were fully vaccinated with the three doses of the pentavalent vaccine (83%), while 14% were partially vaccinated. Findings showed that about one in five parents perceived male vaccination as more important than female vaccination. This parental perception of gender-based importance in vaccination was significantly associated with under-immunization among children (p-value = 0.049). Additionally, males in our study are fully vaccinated 5% more often than females. Socio-economic factors, including mothers’ education and households’ income level, were also significantly associated with the vaccination status of the children.
Conclusion: This study shed light on the effect of gender norms and related determinants on equitable access to vaccinations for boys and girls alike. More research is needed to gain a better understanding of the gender norms related to vaccination and their long-term impact on immunization demand and resilience in this region.
Despite global immunization efforts, inequities in vaccine uptake remain, influenced by socioeconomic, geographic, cultural, and gender-related factors, affecting equitable access to these crucial health services (1–3). The Immunization Agenda 2030 highlights the importance of comprehensive vaccine coverage for individual health and community disease resilience (4).
The WHO launched the Expanded Program on Immunization (EPI) in 1974 to provide vaccinations to children globally (5). However, vaccine accessibility remains problematic in Sub-Saharan Africa, where a significant number of children lack essential vaccinations, leading to high mortality rates from vaccine-preventable diseases (VPDs) (6, 7). Sudan's EPI, initiated in 1976, mandates vaccination for eligible groups, offering free immunizations to residents, including refugees (8, 9). Despite this, persistent conflicts, political upheaval, and socioeconomic disparities present considerable barriers to achieving vaccination goals in Sudan (10, 11).
Gender-based disparity in childhood immunizations is a public health challenge in some countries, with societal biases often resulting in a preference for vaccinating boys over girls (12–14). Such stereotypes, coupled with limited decision-making power for women, hinder access to vaccinations, particularly for female children, thereby increasing their vulnerability to VPDs (15–17).
A comprehensive analysis of childhood immunization in 52 countries revealed a connection between higher maternal empowerment and increased vaccination rates (18). A systematic review of factors influencing vaccination status in children (19) indicated that barriers related to gender include the cost of vaccinations, limited decision-making power for women, and time constraints due to maternal and social responsibilities. Moreover, restricted mobility, social norms, and factors related to the demand for vaccination, such as education, health literacy, and non-Western medical beliefs, also contribute to hindered access to vaccinations.
Despite the rollout of multiple vaccines in Sudan, vaccine-preventable illnesses continue to be a leading cause of mortality in children below five years of age in recent periods (20–22). In 2022, a national report indicated that the coverage for the first and the third doses of the pentavalent vaccine was 94% and 84%, respectively (23). Yet, a more detailed Simple Spatial Survey (S3M) published in 2020, which shows data specific to localities and states, revealed a lower vaccination rate, with just three-quarters of children (76%) receiving the first dose of the pentavalent vaccine (24). This survey also highlighted that Kassala state in Eastern Sudan had a significant proportion of under-immunized children (40%), in contrast, 23% of under-immunized children in Khartoum state.
Gender disparities are acknowledged in Eastern Sudan, particularly in livelihoods, but their impact on vaccination uptake is unclear. This study aimed to assess gender-biased parental perceptions’ influence on under-immunization among children in Kassala, Eastern Sudan. We used the third dose of the DTP-containing vaccine as a measure of under-immunization. It contains diphtheria, tetanus, pertussis, hepatitis B, and Haemophilus influenzae type b (Hib) vaccine. For programmatic purposes, Gavi uses DTP as a proxy for un-vaccination and under-immunization. Children need to receive three doses of the DTP vaccine to be considered fully immunized. DTP is administered through routine national immunization programs rather than campaigns (25). These findings can inform social and behavioral strategies to increase vaccine uptake in Eastern Sudan.
This was a community-based cross-sectional study and conducted in rural and urban districts of Kassala locality in Kassala State, Eastern Sudan in November 2022. The State covers an area of 42,282 km2 with a population of approximately 2.5 million inhabitants. It is located in the eastern part of Sudan, bordered by the states of Eritrea and Ethiopia. It is subdivided into 11 localities. Most populations practice grazing in addition to agriculture.
The study population includes parents of at least one child aged (6–35 months). Either mothers or fathers were eligible for participation. Parents were asked to report about only one child to reduce the risk of recall bias. If there was more than one child in the same age range in the family, the parents/guardians were asked to report about only the youngest one. If both mother and father were available, they were asked to nominate one of themselves to complete the questionnaire.
To ensure that people from various socio-cultural and socioeconomic backgrounds (i.e., education and wealth level) are included in this study, we collected data from parents/guardians in two different rural and urban districts in Kassala; Tajouj village, and Alkhatmia district. Parents were selected in each district using consecutive sampling (convenience sample), as every parent meeting the criteria of inclusion (i.e., had a child in the age range) was included in the study until the required sample size was achieved from each district. The minimum sample size was estimated at 384. To cover for possible drop-out due to refusal to answer some crucial questions, a total of 400 parents were selected for the study (i.e., 200 per district). The sample size was computed using the following formula:
Where, n = sample size. z = (1 - α), is the z-score corresponding to a 95% confidence interval and was computed as 1.96. p = Expected probability of pentavalent vaccination coverage in the rural areas in Kassala, which is unknown, therefore it was estimated at 50%. q = (1- p) or 50%. d = desired margin of error or 0.05.
Data were collected using the Behavioral and Social Drivers of Vaccination (BeSD) survey (26), which was translated to Arabic, and adapted and pre-tested in the local context. This survey, developed by the WHO, measures four underlying factors: thoughts and feelings, social processes, motivation, and practical issues. The question about perception toward gender-biased vaccination was adapted from a question about decision-making autonomy for vaccination in the (BeSD) survey. The questionnaire was interviewer-administered. The questionnaire for the study included parent's socio-demographic characteristics, child characteristics, mother's educational level, household income (was measured as self-ranking), and perception towards gender-biased vaccination, which were used as independent variables. The uptake of the pentavalent vaccine was used as the dependent variable, which was measured as fully immunized (being vaccinated with three doses), partially immunized (being vaccinated with one or two doses) and not immunized who have not received any dose of pentavalent.
Data analysis was performed using Statistical Package for Social Sciences (SPSS) software (Version 26). The Chi-square or Fisher's exact (when the count is <5 in a cell) test was conducted to assess the factors associated with under-immunization among children. We focused on under-immunization rather than non-vaccination because we found that the proportion of under-immunized children is 14%, which is much higher than the proportion of unvaccinated children (2%). We excluded from the Chi-square test those who were not vaccinated, didn't know their vaccination status and missing data (e.g., Mother's education). A p-value of <0.05 is considered statistically significant.
Ethical approval was obtained from the Ahfad University for Women Ethical Committee (IRB). Permission to enter the communities was obtained from the community leaders in the rural districts. Written and/or verbal informed consent was obtained from each participant.
As shown in Table 1, a total of 400 parents of children aged 6–35 months were interviewed with 100% response rate. Half of them (50.0%) are from the urban district. The majority of the participants (91.8%) were mothers, and (92.5%) of them were not employed. The mean age of mothers was 27.6 (SD = 5.36). We surveyed the parents about the level of education of the mothers; results revealed that over half of the mothers (54.7%) had attended primary school, while 19.5% had never attended school. Concerning marital status, the vast majority (95.2%) of the parents are currently married. Half of the participants (50.2%) self-ranked their household income as medium. About half of the households (53.0%) have only one child under the age of five, followed by 38.3% of households having 2 children. Of the children whose vaccination status was recorded, 52.8% were male.
Figure 1 shows that the majority of the children (83%) were fully vaccinated with the pentavalent vaccine (i.e., 3 doses), while 14% were vaccinated with either one or two doses (Partially immunized) and 2% were not vaccinated.
Figure 2 shows that about 1 in 5 participants (19.3%) perceived male vaccination as more important than female vaccination. We did further analysis to assess the association between perceiving male vaccination as more important than female vaccination and the socio-economic status of the parents, including their residence (i.e., rural or urban) and their income level, but there were no significant associations.
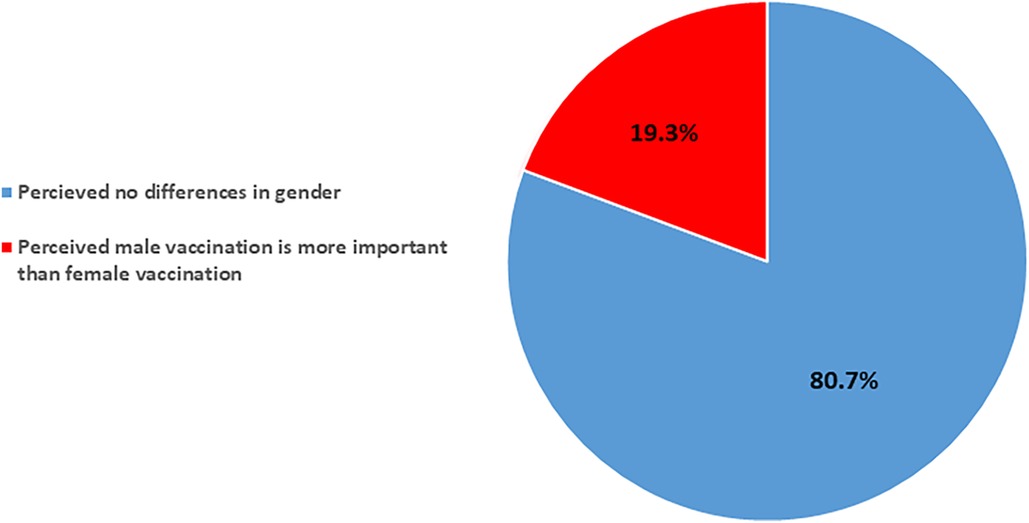
Figure 2. Parental perceptions of gender-based importance in vaccination in rural and urban Kassala, Sudan.
Table 2 shows that socioeconomic factors, including mothers’ education (p = 0.001) and household income level (p = 0.026) were significantly associated with children's vaccination status. Mothers with primary education were more likely to partially vaccinate their children with the pentavalent vaccine, followed by secondary, and non-educated mothers. Those who self-ranked their household's income as low or very low were more likely to have under-immunized children.

Table 2. Association of socioeconomic factors and parent perception with the immunization status of children in Kassala, Sudan (N = 389).
Furthermore, the parental perception of the importance of male vaccination showed a significant association with children's vaccination status (p < 0.049). Parents who perceived male vaccination as more important than female vaccination are more likely to partially vaccinate their children.
There were no significant associations between vaccination status and the residence of the household, the number of children, or the sex of the child whose vaccination status was recorded.
This paper explores the gender-specific determinants that impact the uptake of the pentavalent vaccine in rural and urban areas in Kassala State, Sudan.
The pentavalent vaccine includes diphtheria, tetanus, and pertussis (DTP), as well as hepatitis B and H. Influenzae type b (Hib). Children receive three doses of DTP as a trivalent or pentavalent vaccine within the first months of life. During vaccination sessions, oral polio vaccine (OPV) doses are administered along with DTP. Gavi linked zero-dose and under-immunization definitions with DTP vaccination for operational purposes, and it is used as a proxy for all routine childhood vaccinations (25).
Our data reveal that most children were fully vaccinated with three doses of the pentavalent vaccine (83%), while 14% were partially vaccinated, receiving one or two doses. Only 2% had received no pentavalent doses. The under-immunization in our study is lower than the state-level figure (60%) (16). This may be attributed to the area of study, which is commonly known as the capital of the Kassala state, where a relatively sufficient number of health services can be accessed.
Alarmingly, our findings showed that about one in five parents perceived male vaccination as more important than female vaccination. This parental perception of gender-based importance in vaccination was significantly associated with under-immunization among children (p-value = 0.049). Further, males in our study are fully vaccinated 5% more often than females. This preference for male vaccination is likely rooted in societal and cultural gender norms in the Eastern Sudan communities. Additionally, these findings are a stark indicator of gender inequality in healthcare decision-making and reflect disparities in the uptake of immunization services in Sudan. This bias was significantly related to the children's vaccination status, suggesting a gender-based discrepancy in vaccination coverage that disadvantages female children. Such disparities highlight the urgent need for interventions to eliminate gender biases from health services, ensuring equitable health outcomes for all children (4, 20, 22, 27, 28).
Furthermore, the study underscores a mother's education as a pivotal factor in her child's likelihood of being vaccinated. This suggests that maternal literacy impacts health decisions, which can have gender-specific effects depending on societal norms (29, 30). Evidence shows that higher maternal empowerment is linked to increased vaccination rates (18), while limited decision-making power for women was identified as one of the gender-related barriers that influences children's vaccination status (19).
Educational initiatives directed at mothers, especially those with limited schooling, are essential not only to improving the overall childhood vaccination rate but also to bridging the knowledge gap and promoting equal vaccination opportunities for both boys and girls (31).
Household income was also identified as a significant determinant of vaccination status. However, we did not find a significant association between income level and perceiving male vaccination as more important than female vaccination. In contrast, another study suggests that economic disparities may intersect with gender disparities, as lower-income families might differentially allocate healthcare resources between sons and daughters (32). Tackling this issue requires strategies that make vaccinations accessible to all economic segments, which may help improve the vaccination rate.
We acknowledge some limitations related to our study; therefore, the study's findings should be interpreted within the context of this study. One of the limitations of this study is that there was unintentional selection bias due to consecutive sampling to recruit participants until the pre-determined sample size was reached from both districts. Additionally, from a gender perspective, most of the participants were female; this may be attributed to the time when the interviews were conducted (i.e., men at work). It was observed that fathers’ perceptions, perspectives, and decision-making roles regarding vaccination were missing due to their absence during the study. However, in Sudanese culture, like many other African countries, mothers are primarily responsible for the health and well-being of their children and family and, hence, have a better understanding of the health situation (33). Therefore, some parents preferred that the study should include mothers rather than fathers. We suggested future research to explore the perspectives of a broader range of parents, including fathers.
Given the study's purpose of shedding light on the role of gender norms on vaccination and its possible impact on children's vaccination, we performed only the chi-square test to examine the relationship between independent variables and the dependent variable. However, we did not go further in doing a logistic regression, which could be helpful in analyzing categorical variables and better understanding the predictors of immunization status.
This study emphasizes the importance of confronting gender biases in healthcare to guarantee equitable access to vaccinations for boys and girls alike. Gender norms related to vaccination in Sudan are not well-documented. However, data collectors anecdotally reported that some participants believe that male children should be vaccinated to protect them, as they tend to spend more time outside the house. More qualitative research is needed to gain a better understanding of the gender norms related to vaccination and their long-term impact on immunization demand and resilience in this region.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study was approved by Ahfad University for Women Ethical Committee. The study was conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
MA: Conceptualization, Investigation, Writing – original draft. TJ: Conceptualization, Investigation, Methodology, Writing – original draft. YE: Validation, Visualization, Writing – review & editing. MS: Conceptualization, Formal Analysis, Methodology, Supervision, Validation, Visualization, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
We would like to express our gratitude to the managers at Kassala State's Ministry of Health and the community leaders in both districts for facilitating data collection. We would also like to extend a special thank you to Professor Julie Leask from the University of Sydney for her support to the research project.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2024.1337553/full#supplementary-material
1. Greenwood B. The contribution of vaccination to global health: past, present and future. Philos Trans R Soc B Biol Sci. (2014) 369(1645). doi: 10.1098/rstb.2013.0433
2. Ali HA, Hartner AM, Echeverria-Londono S, Roth J, Li X, Abbas K, et al. Vaccine equity in low and middle income countries: a systematic review and meta-analysis. Int J Equity Health. (2022) 21(1):82. doi: 10.1186/s12939-022-01678-535701823
3. Bocquier A, Ward J, Raude J, Peretti-Watel P, Verger P. Socioeconomic differences in childhood vaccination in developed countries: a systematic review of quantitative studies. Expert Rev Vaccines. (2017) 16(11):1107–18. doi: 10.1080/14760584.2017.138102028914112
4. O’Brien KL, Lemango E, Nandy R, Lindstrand A. The immunization agenda 2030: a vision of global impact, reaching all, grounded in the realities of a changing world. Vaccine. (2022) 42 Suppl 1:S1–S4. doi: 10.1016/j.vaccine.2022.02.073
5. Henderson RH. The expanded programme on immunization of the world health organization. Reviwes Infect Dis. (1984) 6:475–80. doi: 10.1093/clinids/6.Supplement_2.S475
6. Barrow A, Afape AO, Cham D, Azubuike PC. Uptake and determinants of childhood vaccination status among children aged 0–12 months in three West African countries. BMC Public Health. (2023) 23(1):1–12. doi: 10.1186/s12889-023-15863-w36624437
7. World Health Organization Regional Office for Africa. Business case for WHO immunization activities on the African continent 2018–2030.
8. Tibin I, Ismail A, Mahgoob El-Tayeb E, Diaaeldin M, Omer FA, Eltahir YM, et al. Assessment of routine immunization coverage in Nyala locality, reasons behind incomplete immunization in South Darfur state, Sudan. Asian J Med Sci. (2014) 6(1):1. doi: 10.3126/ajms.v6i1.1019925729558
9. Abaker S. Review of expanding program on immunization (EPI) in Sudan 2018. Acta Sci Microbiol. (2020) 3(3):01–4. doi: 10.31080/ASMI.2020.03.0520
10. Mohamed AE, Elhadi YAM, Mohammed NA, Ekpenyong A, Lucero-Prisno DE. Exploring challenges to COVID-19 vaccination in the darfur region of Sudan. Am J Trop Med Hyg. (2022) 106(1):17–20. doi: 10.4269/ajtmh.21-0782
11. Sabahelzain MM, Tagelsir A, Elhadi YAM, Abdalla O. Perceived vaccine availability and the uptake of measles vaccine in Sudan: the mediating role of vaccination hesitancy. Vaccines (Basel). (2022) 10(10):1674. doi: 10.3390/vaccines1010167436298539
12. Feletto M, Sharkey A. The influence of gender on immunisation: using an ecological framework to examine intersecting inequities and pathways to change. BMJ Glob Health. (2019) 4(5):1711. doi: 10.1136/bmjgh-2019-001711
13. Antai D. Gender inequities, relationship power, and childhood immunization uptake in Nigeria: a population-based cross-sectional study. Int J Infect Dis. (2012) 16(2):e136–45. doi: 10.1016/j.ijid.2011.11.00422197748
14. Fuertes CV, Johns NE, Goodman TS, Heidari S, Munro J, Hosseinpoor AR. The association between childhood immunization and gender inequality: a multi-country ecological analysis of zero-dose DTP prevalence and DTP3 immunization coverage. Vaccines (Basel). (2022) 10(7):1032. doi: 10.3390/vaccines1007103235891196
15. Feletto M, Sharkey A, Rowley E, Gurley N, Sinha A, Champions E, et al. A Gender Lens to Advance Equity in Immunisation. New York, NY, USA: Equity Reference Group for Immunisation (2018). Available online at: https://www.gavi.org/our-alliance/strategy/gender-and-immunisation
16. Hay K, McDougal L, Percival V, Henry S, Klugman J, Wurie H, et al. Disrupting gender norms in health systems: making the case for change. Lancet. (2019) 393(10190):2535. doi: 10.1016/S0140-6736(19)30648-831155270
17. Jayachandran S. The roots of gender inequality in developing countries. Annu Rev Econ. (2015) 7(1):63–88. doi: 10.1146/annurev-economics-080614-115404
18. Johns NE, Santos TM, Arroyave L, Cata-Preta BO, Heidari S, Kirkby K, et al. Gender-related inequality in childhood immunization coverage: a cross-sectional analysis of DTP3 coverage and zero-dose DTP prevalence in 52 countries using the SWPER global index. Vaccines (Basel). (2022) 10(7):988. doi: 10.3390/vaccines1007098835891152
19. Merten S, Martin Hilber A, Biaggi C, Secula F, Bosch-Capblanch X, Namgyal P, et al. Gender determinants of vaccination status in children: evidence from a meta-ethnographic systematic review. PLoS One. (2015) 10(8):e0135222. doi: 10.1371/journal.pone.013522226317975
20. Ministry of Health in Sudan: Annual Statistical Report 2017. Available online at: www.sho.gov.sd (accessed December 15, 2022).
21. Ministry of Health in Sudan: Annual Statistical Report 2018. Available online at: www.sho.gov.sd (accessed December 15, 2022).
22. Ministry of Health in Sudan: Annual Statistical Report 2019. Available online at: www.sho.gov.sd (accessed December 15, 2022).
23. Sudan: WHO and UNICEF Estimate of Immunization Coverage: 2018 Revision. Available online at: www.sho.gov.sd (accessed March 27, 2020).
24. FMOH. Simple Spatial Survey Method (S3M II) for Sudan—2018. (2018). Available online at: http://sho.gov.sd (accessed March 2, 2022).
25. Linked Immunisation. Zero-Dose Analysis Card. Gavi, the Vaccine Alliance. (2021). Available online at: https://www.linkedimmunisation.org/wp-content/uploads/2021/08/Gavi_Zero-dose_AnalysisCard.pdf (accessed October 10, 2022).
26. World Health Organization. Behavioural and Social Drivers of Vaccination: Tools and Practical Guidance for Achieving High Uptake. Geneva: World Health Organization (2022). Licence: CC BY-NC-SA 3.0 IGO.
27. Azad AD, Charles AG, Ding Q, Trickey AW, Wren SM. The gender gap and healthcare: associations between gender roles and factors affecting healthcare access in Central Malawi, June–August 2017. Arch Public Health. (2020) 78(1):1–11. doi: 10.1186/s13690-020-00497-w31908777
28. Wonodi C, Farrenkopf BA. Defining the zero dose child: a comparative analysis of two approaches and their impact on assessing the zero dose burden and vulnerability profiles across 82 low- and middle-income countries. Vaccines (Basel). (2023) 11(10):1543. doi: 10.3390/vaccines1110154337896946
29. Greenaway ES, Leon J, Baker DP. Understanding the association between maternal education and use of health services in Ghana: exploring the role of health knowledge. J Biosoc Sci. (2012) 44(6):733. doi: 10.1017/S002193201200004122377424
30. Kibreab F, Lewycka S, Tewelde A. Impact of mother’s education on full immunization of children aged 12–23 months in Eritrea: population and health survey 2010 data analysis. BMC Public Health. (2020) 20(1):1–10. doi: 10.1186/s12889-020-8281-031898494
31. Forshaw J, Gerver SM, Gill M, Cooper E, Manikam L, Ward H. The global effect of maternal education on complete childhood vaccination: a systematic review and meta-analysis. BMC Infect Dis. (2017) 17(1):1–16. doi: 10.1186/s12879-017-2890-y28049444
32. McMaughan DJ, Oloruntoba O, Smith ML. Socioeconomic Status and access to healthcare: interrelated drivers for healthy aging. Front Public Health. (2020) 8:231. doi: 10.3389/fpubh.2020.0023132626678
33. Caldwell JC, Caldwell P. Roles of women, families, and communities in preventing illness and providing health services in developing countries. In: National Research Council (US) Committee on Population, Gribble JN, Preston SH, editors. The Epidemiological Transition: Policy and Planning Implications for Developing Countries: Workshop Proceedings. Washington, DC, USA: National Academies Press (US) (1993). p. 252–71. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK236452/ (accessed May 6 6, 2023)
Keywords: gender norms, vaccination, under-immunization, Kassala, Sudan
Citation: Abdallah MS, Jumma T, Elhadi YAM and Sabahelzain MM (2024) Impact of gender-biased parental perceptions on under-immunization in Eastern Sudan: a cross-sectional study. Front. Glob. Womens Health 5:1337553. doi: 10.3389/fgwh.2024.1337553
Received: 13 November 2023; Accepted: 16 October 2024;
Published: 29 October 2024.
Edited by:
Sara Clements, Centers for Disease Control and Prevention (CDC), United StatesReviewed by:
Madeeha Malik, Cyntax Health Projects, PVT Ltd., CRO & Corporate Firm, PakistanCopyright: © 2024 Abdallah, Jumma, Elhadi and Sabahelzain. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Majdi M. Sabahelzain, bWFqZGkuZGFmYWxsYWhAc3lkbmV5LmVkdS5hdQ==; bWFqZGlzYWJhaGVsemFpbkBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.