- 1Department of Public Health, Faculty of Health Sciences, University of Limpopo, Polokwane, South Africa
- 2Department of Human Nutrition and Dietetics, Faculty of Health Sciences, University of Limpopo, Polokwane, South Africa
- 3DIMAMO Population Health Research Centre, University of Limpopo, Polokwane, South Africa
Background: Exclusive breastfeeding (EBF) for six months, with the introduction of appropriate complementary feeding thereafter, and breastfeeding continuing for up to 2 years and beyond, is highly recommended. This could save the lives of up to 1.4 million children each year worldwide. Despite this, breastfeeding rates in South Africa remain sub-optimal, with the recommended target of 50% by the World Health Assembly (WHA) not being achieved. The study aimed to investigate the reasons influencing mothers' practice of exclusive breastfeeding in the Polokwane municipality of Limpopo province in South Africa.
Methodology: A cross-sectional health facility-based quantitative and descriptive survey was conducted using a validated-structured questionnaire administered to 146 mothers. The data was analyzed using STATA. Chi-square tests were used to determine the relationship between selected demographic variables and their reasons not to breastfeed exclusively.
Results: Although 94% of the mothers had initiated breastfeeding, at the time of data collection 8% had stopped. Of those who had stopped breastfeeding, 5% did so within one month of starting. Thirty- nine percent of mothers' breastfed exclusively, while 61% practiced mixed feeding. A positive association between exclusive breastfeeding practices and the age of the mother were observed, with older mothers more likely to breastfeed. The reasons mothers stopped breastfeeding were: the mother was ill (45%) or they returned to school or work (27%). Reasons for not breastfeeding were cited as: medical conditions, not enough milk, and infant refusal to breastfeed (33%). Mothers believe that HIV-positive women should breastfeed their infants (57%), and health workers were found to be the main source of HIV information to mothers (77%).
Discussion: Exclusive breastfeeding during the first six months was less practiced. Infant formula and solid foods were introduced at an early age, usually within the first month of breastfeeding. This study sheds light on factors influencing the early initiation of breastfeeding and the practice of EBF as practiced in Polokwane.
1 Introduction
Breastfeeding is the process of feeding the infant with the mother's milk (1). It is an integral part of the reproductive process with important implications for the health of the mother and baby (2). The feeding of an infant with only breast milk and no additional food, water, or other liquids (except for medicines and vitamins, if needed) during the first six months of life is termed exclusive breastfeeding (EBF)) (3–5). This is the feeding practice for newborns and infants recommended by the World Health Organization (WHO) to reduce infant morbidity and mortality (5–7). EBF is considered superior to the mixed infant feeding method which includes a combination of breastmilk and infant formula and/or other food types (8). The importance of counselling as a strategy to improve breastfeeding practices has been highlighted in the United Nations Children's Fund (UNICEF) and WHO guidelines to improve breastfeeding. The United Nations (UN) also established targets to eliminate malnutrition and increase exclusive breastfeeding (EBF) rates to at least 50% (9, 10). It is recommended that breastfeeding should start within one hour of birth, this helps the infant with all nutrients necessary for growth from colostrum. Colostrum reduces child morbidity and mortality (1, 11).
EBF should be practiced for up to six months and breastfeeding should continue until the child is two years of age (4, 11). EBF is recommended because breast milk contains all the nutrients necessary in the first few months of life (11). Breast milk is the best nutrition for preterm infants in optimizing the growth and development of babies and young children and is an effective intervention for preventing early childhood deaths (2, 5). It is posited that EBF could prevent 1.4 million deaths worldwide among children under the age of five every year if implemented (5).
Even though EBF is the most efficacious type of infant feeding, women around the world still fail to reach the recommended target of 6 months postpartum (1, 7). Furthermore, sub optimally practiced breastfeeding, negatively affects child survival, growth, and development (1, 7). Infants less than two months old who are not breastfed are six times more likely to die from diarrhea and acute respiratory infections than their counterparts (11, 12). Those who are not exclusively breastfed have a high chance of acquiring pneumonia, meningitis, ear infections and dying from childhood-related diseases due to inadequate Timely Initiation of Breastfeeding (TIBF) (11, 12).
Mothers have numerous challenges which may influence their choice to breastfeed. These may include; a perceived lack of breastmilk, cracked or sore nipples, breast engorgement, disapproval and discomfort of breastfeeding in public, and insufficient breastfeeding support from society and healthcare providers (13). In addition, short maternity leave periods for working mothers, difficulties associated with combining breastfeeding and other maternal responsibilities, and emotional stress are also part of the challenges faced by mothers which may negatively affect their choice to breastfeed (12, 13). The South African government has committed itself to improving EBF, but there is a lack of information on reasons why mothers are not exclusively breastfeeding in rural areas of Limpopo (14). This study aimed to investigate the prevalence of EBF and barriers and enablers of EBF among mothers attending primary health care clinics around Polokwane municipality, Limpopo province.
2 Materials and methods
2.1 Study design, population, and sampling
The study was cross-sectional in design and conducted in the Capricorn District of the Limpopo Province in northern South Africa. The municipality consists of townships, suburbs, and villages within an area of 3,766 km2 and an estimated population size of 797,127, of which 2% are white, 97% African, and 1% are colored [“(15): District Municipality: Capricorn”]. The majority of residents of this district are Sepedi speaking (84.9%) followed by 2.97% Afrikaans, 2.60% Xitsonga, 2.03% English, 1.99% isiNdebele, 1.60% other, 1.41 Tshivenda, 1.05% isiZulu, 0.77 Sesotho, 0.67 Setswana [“(15): District Municipality: Capricorn”]. Polokwane Municipality has an estimated sex ratio of 92.8 males per 100 females.
In this study, a total of five primary health care (PHC) facilities were randomly selected, while the community health Centre (CHC) was automatically included as it was the only referral site within its cluster. The participants were selected using convenient sampling. The study consisted of 146 mothers, paired with their infants from a group of approximately 491 infants who attended six primary health care (PHC) facilities every month in Polokwane, South Africa.
The study participants were informed about the possibility of publishing the findings of the study. The study was approved by the Turfloop Research Ethics Committee (TREC) with reference TREC/115/2017: PG under the University of Limpopo. The Department of Health (DoH) in Limpopo Province granted permission for the study to be conducted in the PHC and CHC facilities. All mothers who participated in the study did so after signing a written full informed consent. In cases where the mother was under age (<18 years) the research team sought consent from them and their legal guardian or parents.
2.1.1 Inclusion criteria
The inclusion criteria for the study were as follows:
• Mothers of infants aged 0–6 months who visited the facility for immunization on the days of data collection
• Mothers who gave written consent to take part in the study.
2.1.2 Exclusion criteria
The exclusion criteria for the study were as follows:
• Infants brought in by caregivers who are neither biological mothers nor primary caregivers
• First-time mothers with infants zero to two weeks – because they may have limited infant feeding experience
• Mothers and caregivers of children over six months of age
• Mothers with an infant with any kind of metabolic disease or genetic disease.
2.2 Data collection
A structured questionnaire was used to collect data adapted from Goosen et al. (16). This was to answer a set of closed-ended questions that sought information about the mothers and infants. The questionnaire included questions on socio-demographic information, infant feeding practices, knowledge of caregiving, and medical information. To test for the face validity of the tool, a pilot study was conducted. The questionnaire was piloted at one of the selected primary health care facilities and the results from the pilot study were used to adjust the questionnaire accordingly.
2.3 Statistical analysis
Data were analyzed using STATA statistical software (STATA Corporation, College Station, Texas) version 12. Categorical variables are presented as percentages and continuous variables are expressed as mean ± SD. χ2 tests were used to evaluate relationships between different selected variables. The critical value for significance was set at p < 0.05 for all analyses. Descriptive statistics were used to summarize the socio-demographic characteristics of the study population, the prevalence of infant feeding practices, and factors influencing these practices. Binary logistic regression was used to determine the association between exclusive breastfeeding and associated factors.
2.4 Results
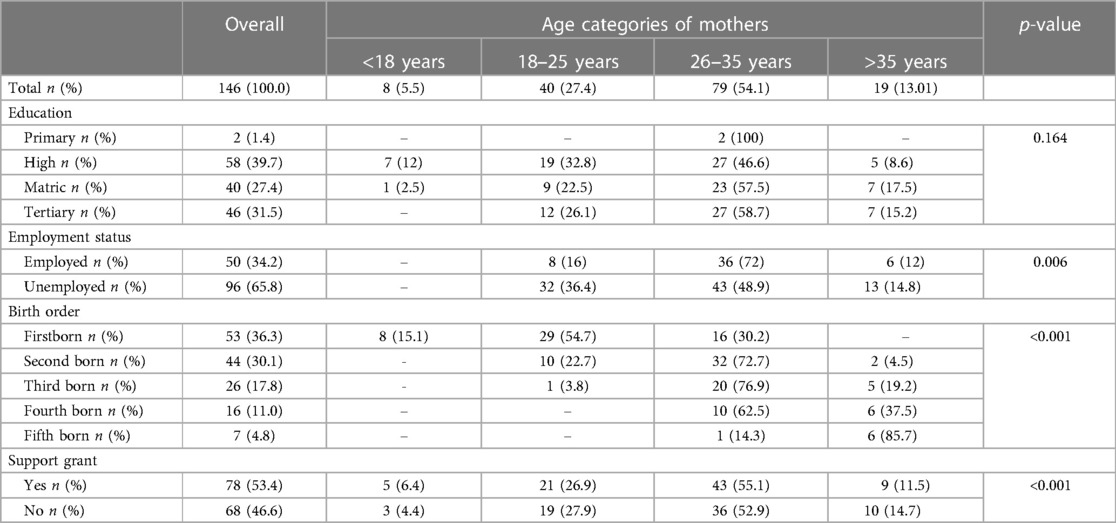
Table 1 describes the demographic characteristics of the mothers who participated in the study. Out of the 146 mothers who participated in the current study, the majority of participants (54.1%) were in the age category 26–35 years. All participants aged ≤18 years were still in high school. Overall, 65.8% of the participants were unemployed with the age group of 26–35 years having the highest percentage of both employment status categories; employed (72%) and unemployed (48.9%). About 33.2% of the participants were first-time mothers. Approximately 53% were receiving child support grants and older mothers were more likely to be receiving child support grants.
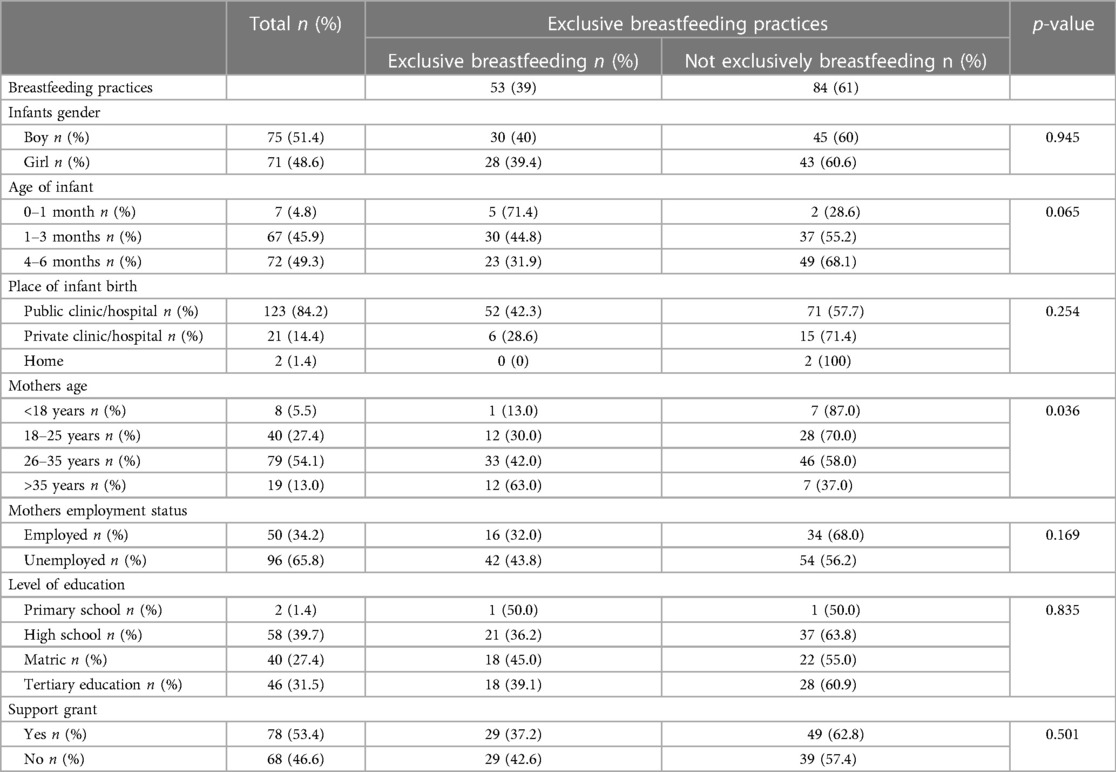
Table 2 shows the association of demographics with infant feeding practices. There was no association between the sex of the child and exclusive breastfeeding and, as expected exclusive breastfeeding decreased with the increased age of the infant (p = 0.065; insignificant) and was less significantly practiced by mothers of the age category of >35 years (p = 0.036). Most infants were delivered at public health facilities (84.22%), followed by those delivered in private health facilities (14.4%) and those delivered at home (1.4%) (p = 0.254). The present study found a significant association between an increase in the age of the mother with exclusive breastfeeding (p = 0.036), where older mothers were found to exclusively breastfeed when compared to younger mothers. In the age group <18 years, those who practiced mixed feeding were 87% as compared to 13% of EBF. In the age group 18–25 years, those who practiced mixed feeding were 70% as compared to 30% of EBF. In the age group 26–35 years, those who practiced mixed feeding were 58% as compared to 42% of EBF. On the contrary, in the age group >35 years, those who practiced mixed feeding were 37% as compared to 63% of EBF. EBF was practiced less by mothers who delivered at private health facilities (28.6%) when compared to those who delivered at public health facilities (42.3%). Although not significant, 32% of employed mothers practiced EBF and the results of the current study indicate that mothers who were full or part-time employed practiced less EBF. Even though it was not statistically significant, mothers with high school as their highest level of education practiced EBF less.
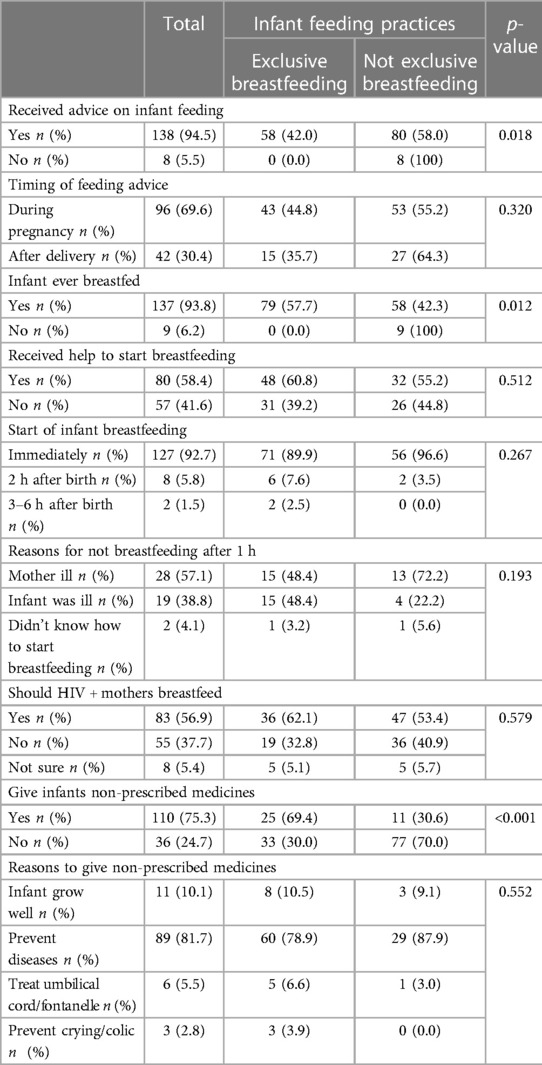
Table 3: Table 3 shows that approximately 94.5% of mothers had received advice on how to feed their infants, of which 69% had received this advice during pregnancy. Significantly more mothers (58%) who received breastfeeding advice were not exclusively breastfeeding (p = 0.018). Approximately 5% of mothers had not received advice on infant feeding and all these mothers did not exclusively breastfeed their infants. The majority (65.6%) of the mothers reported that they had received infant feeding information during pregnancy compared to 30.4% who received it after delivery. About 92.7% of mothers started breastfeeding their babies immediately after birth. Those who delayed breastfeeding stated reasons such as the mother's illness (57.1%), and infant illness (38.8%) with the last reason being lack a lack of knowledge on how to start breastfeeding (4.1%). Mothers who gave their infants non-prescribed medication were significantly more likely to practice EBF (69.4%) (p < 0.001). Reasons for giving non-prescribed medicines included perceived attributes of the medication to make the infant grow well (10.1%), prevent diseases (81.7%), treat umbilical cord/fontanelle (5.5%), and prevent crying/colic (2.8%) with no significant difference between those who practiced exclusive breastfeeding and those who did not.
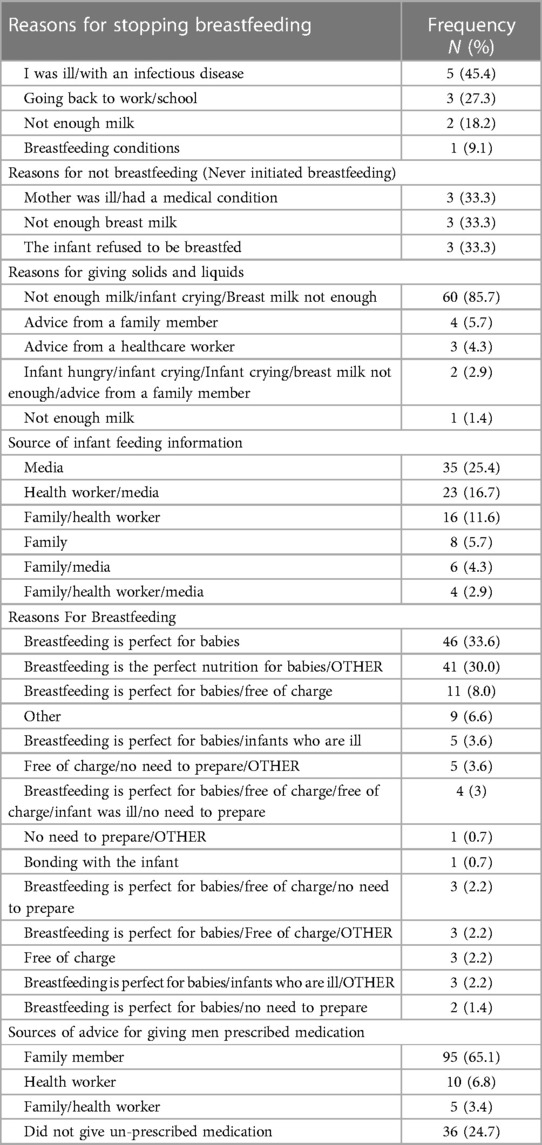
Table 4: At the time of the interview, eleven mothers, which is 8% of the participants who had initiated breastfeeding at one time, had stopped breastfeeding. Mothers who stopped breastfeeding indicated the following reasons; illness (45.5%), going back to school (27.3%), and not producing enough milk (18.2%). Mothers who did not breastfeed (never initiated breastfeeding) indicated the following reasons, illness/medical condition (33.3%), and not enough milk (33.3%), and infant refused to be breastfed 220 (33.3%). About 85.7% of mothers gave infants solids food and liquids mainly because they felt they could not produce enough milk and the infants were crying. Most mothers received their infant feeding information from health workers (33.3%), and media (25.4%), and 5.7% of the mothers received the feeding information from their families. Approximately 0.7% of the participants reported that breastfeeding promotes bonding between mother and infant. The most frequently reported reason for breastfeeding was the perception that breast milk was the perfect nutrition/food for infants, followed by that breast milk is free at 33.6% and 30.0% respectively.
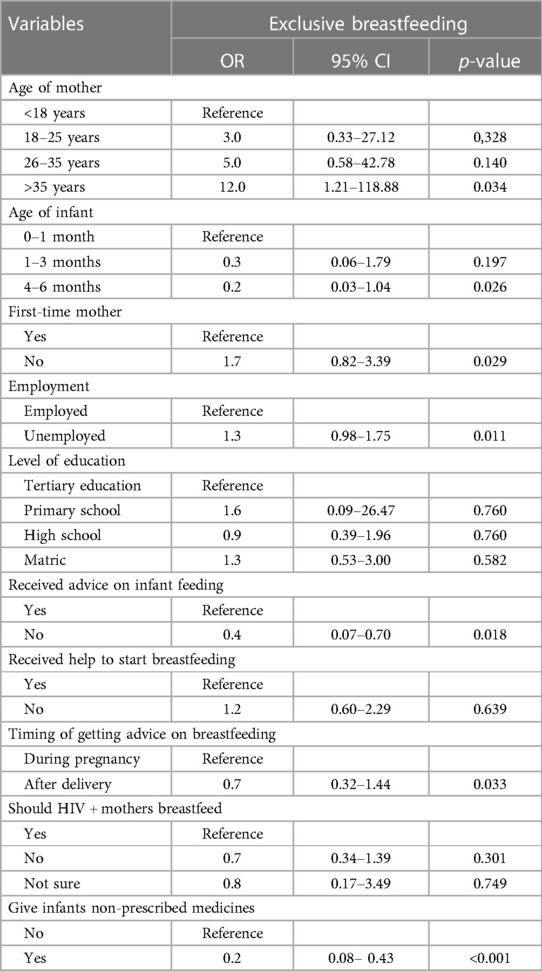
Table 5: Binary logistic regression showed that mothers aged >35 years were 12.0 times more likely to practice EBF (p = 0.034). Infants aged 4–6 months were 0.2 times less likely to be exclusively breastfed (p = 0.026). Women who were not first-time mothers (p = 0.029), unemployed (p = 0.011), and mothers who received help (p = 0.639) to start breastfeeding were more likely to practice EBF. Mothers who did not receive advice on infant feeding (p = 0.018), those who received advice on breastfeeding after delivery (p = 0.033), and those who gave their infant non-prescribed medications (p < 0.001) were less likely to practice exclusive breastfeeding.
3 Discussion
The prevalence of EBF in the present study was 39%, which is higher than the 32% national prevalence (17). However, the findings of the present study are similar to those reported in a study by du Plessis et al (18),, which reported a prevalence of 38.5% (18). On the other hand, a study conducted in the North West province, South Africa, reported a low prevalence of EBF at 9.7% in the infant age group of 20–24 weeks (19). The difference may be due to different study settings, sample sizes, EBF policies and practices, and cultural norms. Given the WHO and UNICEF targets of reaching 50% of EBF at a national level by 2025, the strong points of policies, practices, and cultural norms of countries with a high prevalence of EBF could be used to strengthen our policies and practices to meet the WHO and UNICEF targets (19). Whilst the recorded increase in exclusive breastfeeding rates for children under 6 months is positive, the continuing disparities across different reports create uncertainty about the actual progress made (20).
The major reason women gave for not practicing EBF (mixed feeding prevalence 61%) in the current study was that they perceived that they did not have enough milk. Similar findings were reported in a survey conducted in the Eastern Cape, South Africa (21). The survey found that early introduction of food, water, and infant formula milk was common despite a high breastfeeding initiation rate (21). Similarly, Goosen et al. (16), attributed the early introduction of food and water to the mother's perception that the infants needed water or other supplements (16). On the other hand, the reasons for discontinuation of breastfeeding in the current study were that the mothers were ill, returning to either school or the workplace, and breast conditions such as which concurs with other studies (22, 23). In addition, women who are affected by post-natal depression and related mental health challenges stemming from socioeconomic challenges and lack of support were reported to have a higher likelihood to stop breastfeeding in less than three months postpartum (19). On the other hand, the main reasons given by mothers in the current study for breastfeeding their infants were that breastmilk provides adequate nutrition for the infant and that breastmilk is free. Similarly, a study by Modjadji et al. (17), reported breastfeeding as economical and convenient, promoting child growth and development, protecting the infant against illness, and promoting mother-baby bonding (17). Breast milk contains all the nutrients an infant needs, and promotes child survival, health, brain, and motor development (24, 25).
Evidence shows that the prevalence of breastfeeding, including EBF declines as infants get older (6). An increase in the age of the mother was found to be an indicator of EBF in the present study, where older mothers exclusively breastfed their infants when compared to younger mothers. The Binary logistic regression showed that mothers aged >35 years were 12.0 times more likely to practice EBF. In accordance with the present study, a study conducted in the USA by Jones et al. also reported that the mother's age was strongly associated with the likelihood of breastfeeding exclusively for 6 months (26). Young mothers do not exclusively breastfeed their infants due to their busy lifestyles, being at school, and lack of confidence in breastfeeding (27). In the current study, the prevalence of EBF was high in younger infants (71.4% below 1 month) and it was much lower (31.9%) in infants aged between 3 and 6 months. These rates are still far below the targeted EBF rates of 50% (28, 29). Similarly, the low prevalence at 3–6 months was reported in a study conducted by Joshi et al. (4).
The majority of employed mothers did not practice EBF and the results of the current study indicate that mothers who were full or part-time employed practiced less EBF. In binary logistic regression, unemployed mothers were more likely to practice EBF. This finding is in accordance with the findings of a study conducted by Mandal et al., in the United States of America, which found that full-time employment status was negatively correlated with breastfeeding initiation and duration, suggesting that full-time employment remains a significant barrier to breastfeeding (30). Mothers in a study in Cape Town, South Africa, cited the lack of breastfeeding facilities in public spaces and at work as reasons for failure to exclusively breastfeed their infants (31). In addition, employed mothers face challenges such as the need to return to work early for economic reasons and an unfavorable work environment for expressing and storing milk which makes EBF a challenge for them (32).
In the current study, 64.4% of mothers initiated breastfeeding within one hour after delivery. The initiation rate in the current study is lower compared to the global target of 80% but similar to the national prevalence of 67% in 2016 (33). Initiation of breastfeeding in the first hour post-delivery is recommended as one of the interventions that have the potential to improve infants' nutritional outcomes and reduce infant mortality (34, 35). Early initiation of breastfeeding is associated with sustainable breastfeeding for up to 2 years and beyond (36–38). In the present study, failure to initiate breastfeeding within the first hour was mostly attributed to the mother's illness. Other mothers reported separation from their infants as a cause of delayed initiation as supported by Mukunya et al. (39), who also found a significant association between separation of the mother-baby pair and delayed breastfeeding initiation (39).
Another reason for the delayed initiation of breastfeeding in the current study was a lack of knowledge of how to initiate breastfeeding. Lack of breastfeeding counseling and midwife support has been previously identified as a cause for increased delay in the initiation of breastfeeding (39, 40). These authors emphasize the importance of breastfeeding education during antenatal visits and support by midwives and birth attendants post-delivery to ensure early breastfeeding initiation. Khanlari et al. (41), reported early breastfeeding initiation among mothers who received support from birth attendance immediately after delivery (41). Other challenges contributing to the lack of breastfeeding knowledge include the discrepancies in the knowledge of breastfeeding by health professionals in relation to WHO recommendations (42). A study by Zweigenthal et al. (42), highlighted the need for ongoing training in breastfeeding and infant feeding counseling, as well as community-based postnatal support initiatives addressing cultural beliefs as a way to promote knowledge of breastfeeding amongst mothers (42).
Even though only about two-thirds of mothers initiated breastfeeding within an hour post-delivery, about 94% of the mothers did initiate breastfeeding at some point post-delivery. Studies indicate that it is a common practice for most mothers to initiate breastfeeding (43, 44). Even though the rate of breastfeeding declines as the infants get older (45). These findings are consistent with the results of a study conducted by Siziba et al. (46) in four provinces of South Africa, which reported breastfeeding initiation at 90% (46). Mothers who were not first-time mothers were more likely to exclusively breastfeed. In agreement with the present study, a study by Balogun et al. (47), reported that first-time mothers with no prior experience of breastfeeding were less likely to practice exclusive breastfeeding, while women with at least one child had a higher likelihood of practicing EBF (47). First-time mothers are likely to lack experience in breastfeeding and knowledge of how to initiate it which could be the reason why in the present study mothers who are not first-time mothers were more likely to practice EBF. In addition, a study by Lutaaya et al. (48), reported the following factors as barriers to EBF in first-time mothers; mothers' perception of babies needing more than milk had the highest percentage, followed by fear of breasts losing shape, having difficulties in EBF, breastfeeding being old fashion and maternal understanding of EBF and its recommended period (48). Mothers who did not receive advice on how to initiate breastfeeding were less likely to practice EBF. Similar findings were reported by Massare et al. (49).
4 Conclusion
Exclusive breastfeeding during the first six months was less practiced. Infant formula and solid foods were introduced at an early age. This study sheds light on factors influencing the early initiation of breastfeeding following delivery and the practice of EBF as practiced in Polokwane.
5 Recommendations in light of key study findings
Given that the present study reported a low prevalence of EBF in comparison to the WHO and UNICEF goals the present study recommends that mothers be educated on the importance of EBF, particularly young ones. The study shows that there is a high use of traditional medicine among mothers; therefore, there is a need to properly implement the South African Traditional Health Act (No. 22 of 2007) with the aim of regulating the prescription of traditional medicine. It would also be beneficial to the country to speed up a review of labor regulations to increase maternity leave to six months to afford mothers more time for breastfeeding. Workplace support for breastfeeding will be more effective if it includes lactation breaks and breastfeeding rooms. Given that older mothers practice exclusive breastfeeding for a longer duration than younger mothers, there is a need to raise awareness of the significance of exclusive breastfeeding among young mothers.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was approved by the Turfloop Research Ethics Committee (TREC) with reference TREC/115/2017:PG. The University of Limpopo and the Department of Health in Limpopo Province granted permission for the study to be conducted and written full informed consent was signed all mothers who participated in the study.
Author contributions
The design of the study including the data management and writing of the article was done as a collaborative effort from all authors involved in the study. ME made substantial contributions to the conception, and design including analysis and interpretation of data while MM made substantial contributions to the acquisition of data, analysis, interpretation of data, and drafting of the manuscript. RGM, CBN, and KPS made substantial contributions to the design including revision of the manuscript. CBN played a substantial role in the data analysis, interpretation, and review of the manuscript. All authors' authors have read and approved the revised manuscript for submission.
Acknowledgments
We acknowledge all technical assistance provided to the authors by the TREC and anyone who had helpful discussions or contributed less tangible concepts. The Department of Public Health within the University of Limpopo is acknowledged for hosting the study and the Department of Health in Limpopo Province of South Africa for granting permission to conduct the study. Lastly, we would like to acknowledge the study participants for their time and efforts to make this study a success.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Alemayehu M, Abreha K, Yebyo H, Zemichael K, Gebremichael H. Factors associated with timely initiation and exclusive breast feeding among mothers of axum town, northern Ethiopia. J Public Health (2014) 2(5):394. doi: 10.11648/j.sjph.20140205.14
2. Neji OI, Nkemdilim CC, Ferdinand NF. Factors influencing the practice of exclusive breastfeeding among mothers in tertiary health facility in calabar, cross river state, Nigeria. Am J Nurs. (2015) 4(1):16. doi: 10.11648/j.ajns.20150401.13
3. Danso J. Examining the practice of exclusive breastfeeding among professional working mothers in kumasi metropolis of Ghana. Int J Nurs. (2014) 1(1):11–24.
4. Joshi PC, Angdembe MR, Das SK, Ahmed S, Faruque ASG, Ahmed T. Prevalence of exclusive breastfeeding and associated factors among mothers in rural Bangladesh: a cross-sectional study. Int Breastfeed J. (2014) 9:7. doi: 10.1186/1746-4358-9-7
5. Mekuria G, Edris M. Exclusive breastfeeding and associated factors among mothers in Debre Markos, Northwest Ethiopia: a cross-sectional study. Int Breastfeed J. (2015) 10(1):1. doi: 10.1186/s13006-014-0027-0
6. Asemahagn MA. Determinants of exclusive breastfeeding practices among mothers in azezo district, northwest Ethiopia. Int Breastfeed J. (2016) 11:22. doi: 10.1186/s13006-016-0081-x
7. Thet MM, Khaing EE, Diamond-Smith N, Sudhinaraset M, Oo S, Aung T. Barriers to exclusive breastfeeding in the ayeyarwaddy region in Myanmar: qualitative findings from mothers, grandmothers, and husbands. Appetite. (2016) 96:62–69. doi: 10.1016/j.appet.2015.08.044
8. Reni DP, Puspitaningsih R, Wati R, Nurachma E. The effectiveness combination of hypnobreastfeeding and breast exercises on breast milk production time in third trimester pregnant women. PLACENTUM: Jurnal Ilmiah Kesehatan Dan Aplikasinya. (2023) 11(1):43–51. doi: 10.20961/placentum.v11i1.66967
9. Vitalis D, Witten C, Pérez-Escamilla R. Gearing up to improve exclusive breastfeeding practices in South Africa. PLoS One. (2022) 17(3):e0265012. doi: 10.1371/journal.pone.0265012
10. Vitalis D, Vilar-Compte M, Nyhan K, Pérez-Escamilla R. Breastfeeding inequities in South Africa: can enforcement of the WHO code help address them? - a systematic scoping review. Int J Equity Health. (2021) 20(1):114. doi: 10.1186/s12939-021-01441-2
11. Tampah-Naah AM, Kumi-Kyereme A, Amo-Adjei J. Maternal challenges of exclusive breastfeeding and complementary feeding in Ghana. PLoS One. (2019) 14(5):e0215285. doi: 10.1371/journal.pone.0215285
12. Diji AK, Bam V, Asante E, Lomotey AY, Yeboah S, Owusu HA. Challenges and predictors of exclusive breastfeeding among mothers attending the child welfare clinic at a regional hospital in Ghana: a descriptive cross-sectional study. Int Breastfeed J. (2017) 12:13. doi: 10.1186/s13006-017-0104-2
13. Maastrup R, Hansen BM, Kronborg H, Bojesen SN, Hallum K, Frandsen A, et al. Factors associated with exclusive breastfeeding of preterm infants. Results from a prospective national cohort study. PLoS One. (2014) 9(2):e89077. doi: 10.1371/journal.pone.0089077
14. Jama NA, Wilford A, Masango Z, Haskins L, Coutsoudis A, Spies L, et al. Enablers and barriers to success among mothers planning to exclusively breastfeed for six months: a qualitative prospective cohort study in KwaZulu-Natal, South Africa. Int Breastfeed J. (2017) 12:43. doi: 10.1186/s13006-017-0135-8
15. Census. “Census 2011: district municipality: capricorn.” (2011). Available at: https://census2011.adrianfrith.com/place/935 (Accessed August 17, 2023).
16. Goosen C, McLachlan M, Schübl C. Infant feeding practices during the first 6 months of life in a low-income area of the western cape province. South Afr J Child Health. (2014) 8(2):50. doi: 10.7196/sajch.675
17. Modjadji P, Seabela ES, Ntuli B, Madiba S. Beliefs and norms influencing initiation and sustenance of exclusive breastfeeding: experiences of mothers in primary health care facilities in ermelo, South Africa. Int J Environ Res Public Health. (2023) 20(2):1513. doi: 10.3390/ijerph20021513
18. Du Plessis LM, Herselman MG, McLachlan MH, Nel JH. Selected facets of nutrition during the first 1000 days of life in vulnerable South African communities. South Afr J Child Health. (2016) 10(1):37–42. doi: 10.7196/SAJCH.2016.v10i1.984
19. Witten C, Claasen N, Kruger HS, Coutsoudis A, Grobler H. Psychosocial barriers and enablers of exclusive breastfeeding: lived experiences of mothers in low-income townships, North West province, South Africa. Int Breastfeed J. (2020) 15(1):76. doi: 10.1186/s13006-020-00320-w
20. Martin-Wiesner P. “A Policy-Friendly Environment for Breastfeeding.” A Review of South Africa's Progress in Systematising Its International and National Responsibilities to Protect, Promote and Support Breastfeeding. Johannesburg: DST-NRF Centre of Excellence in Human Development. (2018).
21. Sayed N, Burger R, Harper A, Swart EC. Lockdown-associated hunger may be affecting breastfeeding: findings from a large SMS survey in South Africa. Int J Environ Res Public Health. (2021) 19(1):351. doi: 10.3390/ijerph19010351
22. Lima APE, Castral TC, Leal LP, Javorski M, Sette GCS, Scochi CGS, et al. Exclusive breastfeeding of premature infants and reasons for discontinuation in the first month after hospital discharge. Rev Gaucha Enferm. (2019) 40:e20180406. doi: 10.1590/1983-1447.2019.20180406
23. Rozga MR, Kerver JM, Olson BH. Self-reported reasons for breastfeeding cessation among low-income women enrolled in a peer counseling breastfeeding support program. J Hum Lact. (2015) 31(1):129–37; quiz 189–90. doi: 10.1177/0890334414548070
24. Jensen SK, Bouhouch RR, Walson JL, Daelmans B, Bahl R, Darmstadt GL, et al. Enhancing the child survival agenda to promote, protect, and support early child development. Semin Perinatol. (2015) 39(5):373–86. doi: 10.1053/j.semperi.2015.06.002
25. Vaivada T, Gaffey MF, Bhutta ZA. Promoting early child development with interventions in health and nutrition: a systematic review. Pediatrics. (2017) 140(2):e20164308. doi: 10.1542/peds.2016-4308
26. Jones JR, Kogan MD, Singh GK, Dee DL, Grummer-Strawn LM. Factors associated with exclusive breastfeeding in the United States. Pediatrics. (2011) 128(6):1117–25. doi: 10.1542/peds.2011-0841
27. Liben ML, Gemechu YB, Adugnew M, Asrade A, Adamie B, Gebremedin E, et al. Factors associated with exclusive breastfeeding practices among mothers in dubti town, afar regional state, northeast Ethiopia: a community based cross-sectional study. Int Breastfeed J. (2016) 11:4. doi: 10.1186/s13006-016-0064-y
28. Dhami MV, Ogbo FA, Akombi-Inyang BJ, Torome R, Agho KE. On behalf of the global maternal and child health research collaboration GloMACH. Understanding the enablers and barriers to appropriate infants and young child feeding practices in India: a systematic review. Nutrients. (2021) 13(3):825. doi: 10.3390/nu13030825
29. World Health Organization. Reducing Stunting in Children: Equity Considerations for Achieving the Global Nutrition Targets 2025. Geneva: World Health Organization (2018).
30. Mandal B, Roe BE, Fein SB. The differential effects of full-time and part-time work status on breastfeeding. Health Policy. (2010) 97(1):79–86. doi: 10.1016/j.healthpol.2010.03.006
31. Sowden M, Marais D, Beukes R. Factors influencing high socio-economic class mothers’ decision regarding formula-feeding practices in the cape metropole. South Afr J Clin Nutr. (2009) 22(1):37–44. doi: 10.1080/16070658.2009.11734215
32. Maponya N, van Rensburg ZJ, Du Plessis-Faurie A. Understanding South African mothers’ challenges to adhere to exclusive breastfeeding at the workplace: a qualitative study. Int J Nurs Sci. (2021) 8(3):339–46. doi: 10.1016/j.ijnss.2021.05.010
33. Nieuwoudt S, Manderson L, Norris SA. Infant feeding practices in soweto, South Africa: implications for healthcare providers. S Afr Med J. (2018) 108(9):756–62. doi: 10.7196/SAMJ.2018.v108i9.13358
34. Christian P, Mullany LC, Hurley KM, Katz J, Black RE. Nutrition and maternal, neonatal, and child health. Semin Perinatol. (2015) 39(5):361–72. doi: 10.1053/j.semperi.2015.06.009
35. John JR, Mistry SK, Kebede G, Manohar N, Arora A. Determinants of early initiation of breastfeeding in Ethiopia: a population-based study using the 2016 demographic and health survey data. BMC Pregnancy Childbirth. (2019) 19(1):69. doi: 10.1186/s12884-019-2211-0
36. Ezeh OK, Ogbo FA, Stevens GJ, Tannous WK, Uchechukwu OL, Ghimire PR, et al. Factors associated with the early initiation of breastfeeding in economic community of West African states (ECOWAS). Nutrients. (2019) 11(11):2765. doi: 10.3390/nu11112765
37. Gebretsadik GG, Tkuwab H, Berhe K, Mulugeta A, Mohammed H, Gebremariam A. Early initiation of breastfeeding, colostrum avoidance, and their associated factors among mothers with under one year old children in rural pastoralist communities of Afar, Northeast Ethiopia: a cross sectional study. BMC Pregnancy Childbirth. (2020) 20(1):448. doi: 10.1186/s12884-020-03151-z
38. Raihana S, Dibley MJ, Rahman MM, Tahsina T, Siddique MAB, Rahman QS, et al. Early initiation of breastfeeding and severe illness in the early newborn period: an observational study in rural Bangladesh. PLoS Med. (2019) 16(8):e1002904. doi: 10.1371/journal.pmed.1002904
39. Mukunya D, Tumwine JK, Nankabirwa V, Ndeezi G, Odongo I, Tumuhamye J, et al. Factors associated with delayed initiation of breastfeeding: a survey in Northern Uganda. Glob Health Action. (2017) 10(1):1410975. doi: 10.1080/16549716.2017.1410975
40. Syam A, Amiruddin R. Inhibitor factors of early initiation of breastfeeding among mothers in rural district bone, South Sulawesi, Indonesia. Asian J Epidemiol. (2014) 8(1):1–8. doi: 10.3923/aje.2015.1.8
41. Khanlari S, Barnett Am B, Ogbo FA, Eastwood J. Re-examination of perinatal mental health policy frameworks for women signalling distress on the Edinburgh postnatal depression scale (EPDS) completed during their antenatal booking-in consultation: a call for population health intervention. BMC Pregnancy Childbirth. (2019) 19(1):221. doi: 10.1186/s12884-019-2378-4
42. Zweigenthal V, Strebel A, Hunter-Adams J. Adolescent girls’ perceptions of breastfeeding in two low-income periurban communities in South Africa. Health Care Women Int. (2019) 40(7-9):995–1011. doi: 10.1080/07399332.2018.1549043
43. Nkoka O, Ntenda PAM, Kanje V, Milanzi EB, Arora A. Determinants of timely initiation of breast milk and exclusive breastfeeding in Malawi: a population-based cross-sectional study. Int Breastfeed J. (2019) 14:37. doi: 10.1186/s13006-019-0232-y
44. Wu Y, Wang Y, Huang J, Zhang Z, Wang J, Zhou L, et al. The association between caesarean delivery and the initiation and duration of breastfeeding: a prospective cohort study in China. Eur J Clin Nutr. (2018) 72(12):1644–54. doi: 10.1038/s41430-018-0127-9
45. Salih M. Why mothers are not exclusively breast feeding their babies till 6 months of age? Knowledge and practices data from two large cities of the kingdom of Saudi Arabia. Sudan J Paediatr. (2018) 1:28–38. doi: 10.24911/SJP.2018.1.5
46. Siziba LP, Jerling J, Hanekom SM, Wentzel-Viljoen E. Low rates of exclusive breastfeeding are still evident in four South African provinces. South Afr J Clin Nutr. (2015) 28(4):170–79. doi: 10.1080/16070658.2015.11734557
47. Balogun OO, Dagvadorj A, Anigo KM, Ota E, Sasaki S. Factors influencing breastfeeding exclusivity during the first 6 months of life in developing countries: a quantitative and qualitative systematic review. Matern Child Nutr. (2015) 11(4):433–51. doi: 10.1111/mcn.12180
48. Lutaaya MA. Prevalence and factors hindering first time mothers from exclusively breast feeding in kyabugimbi health centre IV (Bushenyi district Uganda Thesis). (2017). Kampala International University, Kampala (2017).
49. Massare BA, Hackman NM, Sznajder KK, Kjerulff KH. Helping first-time mothers establish and maintain breastfeeding: access to someone who can provide breastfeeding advice is an important factor. PLoS One. (2023) 18(6):e0287023. doi: 10.1371/journal.pone.0287023
50. Behzadifar M, Saki M, Behzadifar M, Mardani M, Yari F, Ebrahimzadeh F, et al. Prevalence of exclusive breastfeeding practice in the first six months of life and its determinants in Iran: a systematic review and meta-analysis. BMC Pediatr. (2019) 19(1):384. doi: 10.1186/s12887-019-1776-0
51. Burns N, Grove SK. 2010. Understanding Nursing Research-EBook: Building an Evidence-Based Practice. Maryland Heights, MO, United States: Elsevier Health Sciences.
52. Motee A, Ramasawmy D, Pugo-Gunsam P, Jeewon R. An assessment of the breastfeeding practices and infant feeding pattern among mothers in Mauritius. J Nutr Metab. (2013) 2013:243852. doi: 10.1155/2013/243852
Keywords: breastfeeding, feeding practices, factors, barriers, enablers
Citation: Makwela MS, Mashaba RG, Ntimana CB, Seakamela KP and Maimela E (2024) Barriers and enablers to exclusive breastfeeding by mothers in Polokwane, South Africa. Front. Glob. Womens Health 5:1209784. doi: 10.3389/fgwh.2024.1209784
Received: 21 April 2023; Accepted: 31 January 2024;
Published: 13 February 2024.
Edited by:
Julia Lopez, Washington University in St. Louis, United States© 2024 Makwela, Mashaba, Ntimana, Seakamela and Maimela. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Reneilwe Given Mashaba Z2l2ZW4ubWFzaGFiYUB1bC5hYy56YQ==
 Maishataba Solomon Makwela
Maishataba Solomon Makwela Reneilwe Given Mashaba
Reneilwe Given Mashaba Cairo Bruce Ntimana
Cairo Bruce Ntimana Kagiso Peace Seakamela
Kagiso Peace Seakamela Eric Maimela
Eric Maimela