- 1Department of Biomedical Sciences, School of Medicine, College of Health Science, Arba Minch University, Arba Minch, Ethiopia
- 2Department of Physiology, School of Medicine, College of Health Science, Addis Ababa University, Addis Ababa, Ethiopian
- 3Department of Biomedical Sciences, College of Medicine and Health Sciences, Debre Berhan University, Debre Berhan, Ethiopia
Background: The use of contraceptives has become prevalent among women in Ethiopia. Oral contraceptive use has been suggested to trigger changes in glucose metabolism, energy expenditure, blood pressure, and body weight, among various populations and ethnic groups.
Objective: To elucidate the pattern of fasting blood glucose, blood pressure, and body mass index among combined oral contraceptive pills users compared to controls.
Methods: An institution-based cross-sectional study design was employed. A total of 110 healthy women using combined oral contraceptive pills were recruited as cases. Another 110 healthy age and sex-matched women not using any hormonal contraceptives were recruited as controls. A study was conducted between October 2018 and January 2019. Data obtained was entered and analyzed using IBM SPSS version 23 software packages. One-way ANOVA was used to identify the variation of variables in relation to the duration of use of the drug. The P-value of < 0.05 at the 95% confidence level was statistically significant.
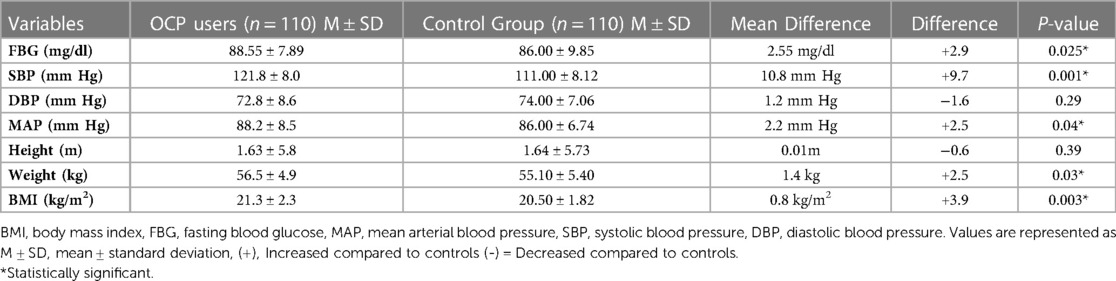
Results: Fasting blood glucose level among oral contraceptive users (88.55 ± 7.89 mg/dl) was higher than fasting blood glucose level among oral contraceptive non-users (86.00 ± 9.85 mg/dl) with a p-value of 0.025. The mean arterial pressure of oral contraceptive users (88.2 ± 8.48 mmHg) was relatively higher than their counterparts (86.0 ± 6.74 mmHg), with a p-value of 0.04. Comparatively the body weight and body mass index among oral contraceptive users were 2.5% and 3.9% higher than non-users with a p-value of 0.03 and 0.003, respectively(5). Utilization of oral contraceptive pills for prolonged period of time seemed to be a significant predictive factor for higher mean arterial pressure and body mass index with p < 0.001and p < 0.05 respectively.
Conclusions: Use of combined oral contraceptives was associated with higher fasting blood glucose (+2.9%), mean arterial pressure (+2.5%), and body mass index (3.9%) compared to controls.
Introduction
Oral contraceptive pills (OCPs) are one of the most common worldwide used family planning methods for preventing pregnancy and it was introduced in the early 1960s (1). Introduction of modern contraceptives has contributed significantly to avert maternal mortality by promoting the wellbeing of mothers and children (2). Modern contraceptives whether hormonal or non-hormonal, are medical procedures or products that interfere with reproduction following sexual intercourse (3). Among different methods of contraception, OCP use is common because of various factors such as reversibility, lower side effects and also its role in reducing risk of dysmenorrhea and ovarian cancers (4). Approximately one hundred million women use combined hormonal contraceptives worldwide, which are most used in the Western world (5). This could make hormonal contraceptives one of the prescription drugs most widely used in the world (5). The main contraceptive effect of OCP is inhibition of the hypothalamus-pituitary-ovarian axis via negative feedback mechanism; which is designed to suppress the secretion of pituitary gonadotropins, which, in turn, prevents follicular maturation, ovulation, and subsequently prevents pregnancy (6). Despite their benefits, hormonal contraceptive use may increase the risk of different disorders such as weight gain, hypertension, hyperglycemia, and increased BMI (7–9). Study report in Park et al. investigated that utilization of OCP for more than 24 months caused approximately two folds increase in the risk of developing hypertension (7). According to Liu et al., highest doses of OCP compared to lower doses caused approximately 50% higher risk of developing hypertension (10). Furthermore, a study from China also reported that OCP users had a nearly 40% higher risk of developing hypertension compared to OCP non users (11). In addition, clinical and experimental studies have reported that hormonal contraceptives deteriorate carbohydrate metabolism and insulin secretion of users (12, 13). Gonzale et al. investigated the influence of estradiol on insulin receptors, in which it was reported that estradiol cause the carbohydrate mechanism to deteriorate and decrease insulin sensitivity (8). These changes detected on carbohydrate mechanism are dependent on ethyl estradiol doses and androgenic effect of progestin (13). Besides the negative effects on blood pressure and carbohydrate metabolism, use of OCP has also been couple to weight gain and obesity (9). According to a study from Kenya, women who use OCP were 1.24 times more likely to be obese compared to OCP non-users (14). Similarly a study from Myanmar reported that the chance of being obese was 1.43 times more likely among OCP users as compared to their counterparts (15). Available data on effects of OCP use on blood pressure, carbohydrate metabolism, and body weight is mostly based on women from developed countries and less frequently from Africans. Specifically, no previous studies have investigated the association between OCPs use and fasting blood glucose (FBG), blood pressure, and body mass index (BMI) among users in Ethiopia. Therefore, we aimed to assess the association between OCPs use and fasting blood glucose, blood pressure, and body mass index.
Methods
Study area and period
The study was conducted at family planning services provider health centers in Chencha town, from October 2018 to January 2019.
Study design and subjects
An institution-based cross-sectional study design was employed on 220 subjects in two groups. 110 healthy women who had been using OCPs were grouped as cases and 110 healthy age and sex matched controls that were not using any hormonal contraceptive.
Eligibility criteria
Aged between 18 and 45 years; clinically stable and OCP users for more than 3 months included in the study as cases and healthy women who have the same inclusion criteria as users, but not using pills were included as controls. On the other hand, chronic alcohol and/or tobacco use; pregnancy; breastfeeding; women who were using other hormonal contraceptives; women who did not had full information on patient chart about diagnosis of chronic co-morbidities such us (thromboembolic disorders, cardiovascular disorders like hypertension, cerebrovascular accident like stroke, chronic renal disease, chronic liver disease, diabetes mellitus) before starting OCP were excluded from the study.
Sample size determination and sampling
The two-sided population proportion formula was utilized for the determination of sample size. Taking prevalence of hypertension among OCP users was 35% and among controls was 18% (7); 95% confidence interval with a 5% margin of error. By adding a 10% non-response rate the final sample size was 220. A simple random sampling technique was applied to select 110 cases. Similar numbers of controls (110) were selected by convenient sampling from a similar population.
Data collection procedure
A structured questionnaire that is a modified form of that of the World Health Organization (WHO) was used for the purpose (16). A pretested questionnaire pertinent to the study objectives was developed and used. All women were screened for eligibility based on a medical interview, and those who volunteered to participate in the study were recruited. Study participants answered questions in the questionnaire that were relevant to their socio-demographics. Afterward, systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured and mean arterial pressure (MAP) was calculated. The height and weight of each participant were measured to compute the BMI. A capillary blood sample was collected from each participant following overnight fasting for estimation of FBG.
Anthropometric measurements
The height and weight of the study participants were measured. The height was measured without shoes using a meter rule and approximated to the nearest 1 cm. Weight was measured using the weighing scale nearest to 1 kg, with light clothing, and without phones or any encumbrance that could alter their appropriate weight. BMI was calculated using the following formula: weight/squared height in kg/m2.
Blood pressure measurement
The resting blood pressure of study participants was measured by using a recently calibrated digital sphygmomanometer. Measurements were done after 15 min of rest in a sitting position three times, giving 3 to 5 min of rest in between the measurements in the left arm. According to WHO guidelines, the mean of the 2nd and 3rd readings was taken for data analysis. The SBP and DBP readings were taken from a digital sphygmomanometer. The MAP was calculated as DBP + 1/3 (SBP- DBP) from SBP and DBP (17).
Data processing and analysis
SPSS software version 23 was used for data management and statistical analysis. Standard statistical methods were used to determine the mean, standard deviation, and range. An independent samples t-test was used to compare the results of the FBG level, MAP, and BMI of the cases with the control group. A one-way ANOVA was used to identify the variation of variables in relation to the duration of use of the drug. The P-value of < 0.05 at the 95% confidence level was statistically significant.
Ethical considerations
Our study has been approved by the departmental research and ethical committee (DRC) of the college of health sciences at Tikur Anbessa Hospital, Addis Ababa University with protocol number Anat/Phy/256/2018, September 13/2018. All participants were informed of the objective of the study and provided written approval of it.
Operational definitions
Blood pressure: The force exerted against blood vessel walls can be categorized as normal pressure below 120/80 mmHg, elevated systolic blood pressure between 120 and 129, and diastolic less than 80 mmHg, and hypertensive above 130/80 mmHg (17).
Body Mass Index (BMI): The ratio of body mass in kilograms to body height squared meter, expressed in kg/m2 units (18).
Oral Contraceptive (OCP): Often referred to as the birth control pill or colloquially as “the pill”, is a type of birth control that is designed to be taken orally by women. It includes a combination of estrogen and progesterone and alters the menstrual cycle to inhibit ovulation and prevent pregnancy (19).
Fasting Blood Glucose (FBG): Glucose level is the result of blood samples taken after the client fasts for at least eight hours or overnight, with a normal level less than 110 mg/dl, impaired fasting glucose (IFG) between 110 and 125 mg/dl and DM over 126 mg/dl (20).
Results
Socio demographic characteristics the study participants
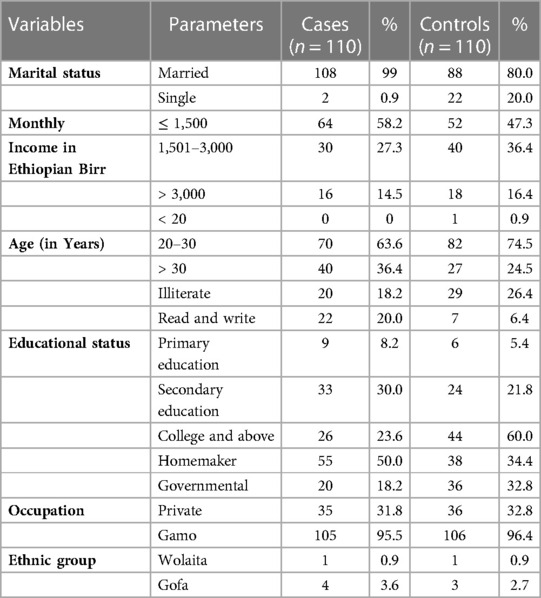
A total of 220 study participants (110 OCP users and 110 controls) were included in the study. Most participants (99% of cases and 80% of controls) were married. Sixty-four (58.2%) of OCP users and 52 (47.3%) of the control groups had monthly incomes between 500 and 1,500 Ethiopian Birr. The mean age (years) of the two groups was 29.6 ± 3.56 (OCP users) and 28.3 ± 3.86 (control). The majority of the study participants; 70 (63.6%) of OCP users and 82 (74.5%) of the controls, were aged 20–30 years. The main religion was Orthodox Christian, with 62 (56.4%) OCP users and 57 (51.8%) controls. A significant number of subjects (23.6% of OCP users and 60% of controls) attended modern education, ranging from primary up to tertiary level. About 55 (50%) of OCP users and 38 (34.4%) of controls were homemakers (as shown in Table 1).
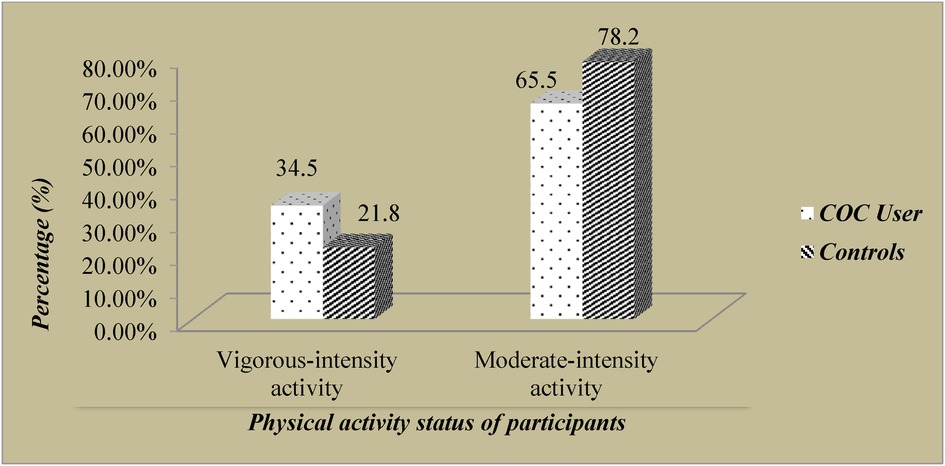
Physical activity Status of participants
All participants in both groups were physically active. 34.5% of cases and 21.8% of control groups had vigorous-intensity activity in their daily work. Majority of the study participants (65.5% of cases and 78.2% of the controls) had moderate-intensity activities in their daily work (as shown in Figure 1).
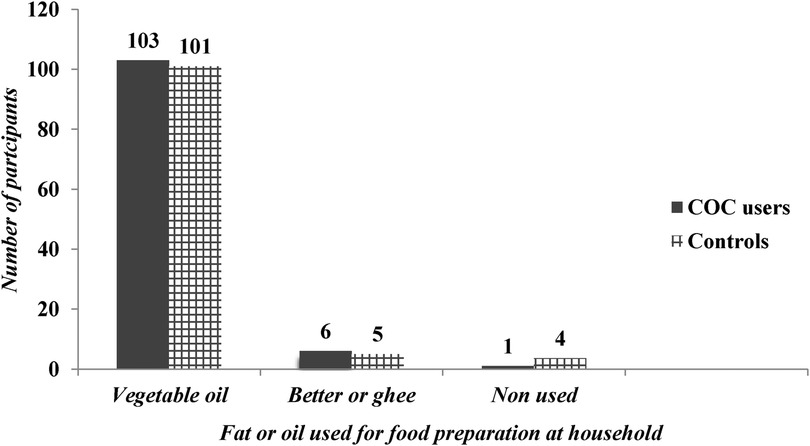
Nutritional Status of participants
Most of the time, 89% and 83% of the cases and controls ate fruit 1–3 days per week, respectively. 79% of cases and 70% of control groups were eating vegetables 4–7 days per week. The majority 93.6% of the cases and 91.8% of controls used vegetable oil for food preparation at home (as shown in Figure 2).
Use of oral contraceptives pills
In the current study, study participants used OCP on a regular basis for an average of 16 months, ranging from 3 to 36 months. About 16.4% of study participants utilized OCP for more than 25 months; 45.4% of users used it for 13–24 months; and 38.2% of users stayed on the service for 3–12 months.
Physical and biochemical measurements
The mean FBG level for cases was 88.55 ± 7.89 mg/dl and 86.00 ± 9.85 mg/dl in controls. FBG ranged from 67 to 111 mg/dl among OCP users and 64–109 mg/dl among controls. About 4.5% of OCP users had a FBG value ≥ 110 mg/dl. The MAP among OCP users was higher (88.2 ± 8.5 mmHg) than control group (86.0 ± 6.7 mmHg) with a P-value of 0.04 (as shown in Table 2). The mean SBP of cases and controls was (121.8 ± 8.0 and 111.0 ± 8.1 mm Hg) respectively with P-value of (P = 0.001). The one-way ANOVA analysis showed a significant higher (P ≤ 0.05) mean SBP, DBP, and MAP in relation to the duration of OCP utilization among pills users (as shown in Table 3).
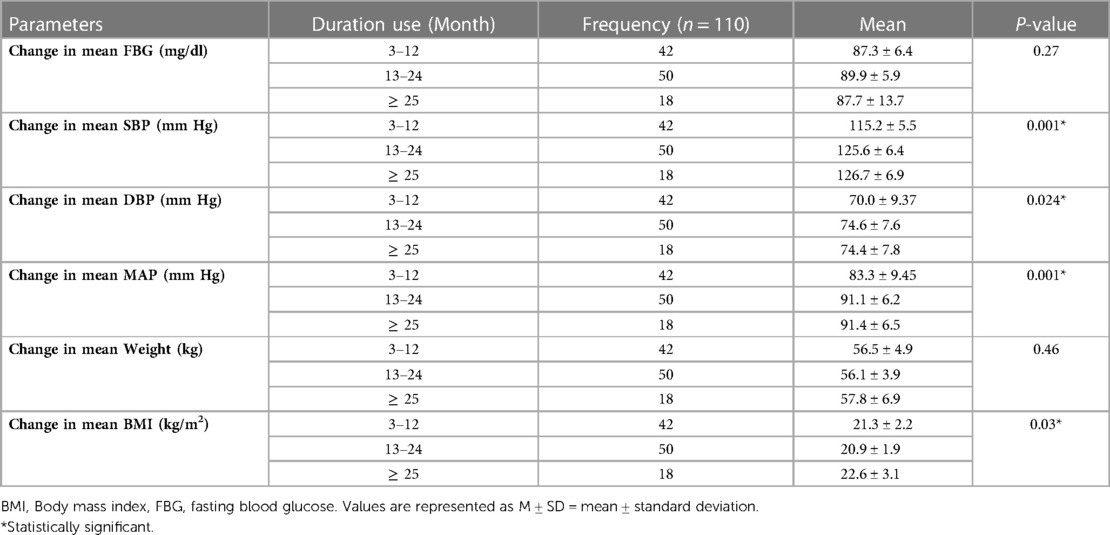
Table 3. Mean difference in serum FBG level, SBP, DBP, MAP, weight, and BMI among OCP users with relation to duration of stay on OCP utilization.
Discussions
In this comparative cross-sectional study, FBG level, MAP, mean body weight and BMI were significantly higher among OCP users as compared to their counterparts (as shown in Table 2).
Fasting blood glucose level
FBG level among OCP users (88.55 ± 7.89 mg/dl) was higher than FBG level among OCP non-users (86.00 ± 9.85 mg/dl) with p-value of 0.025. However, it remained in the normal range for all users. Similar study finding was reported by Godsland et al. (21), who observed that OCP increased the incremental areas for plasma glucose by 43% to 61% among OCP users than controls. A study in Finland also found that consumers of OCPs had significantly higher mean serum glucose levels as compared with their baseline values, with an increased risk of developing glucose metabolism abnormalities (22).
The mechanism behind OCP use leads to a higher blood glucose level has not yet been elucidated. The possible mechanism, as demonstrated in rats revealed that the high doses of estradiol decreased the sensitivity of insulin via the carbohydrate mechanism (8). Contrary to the present study finding, Berenson and co-workers' (23) reported that changes in the mean FBG level of users of OCPs were not significantly different from controls. This disparity may be due to the variation in the study protocol used in previous and current research. Berenson and co-workers' study was a cohort study involving 703 participants, whereas the current cross-sectional study involved a comparatively small sample size of 220 participants. The discrepancy may also be due to the participants' age difference between the studies. Unlike study conducted by Berenson and co-workers' (23), whose age bracket was between 25 and 33 years, our study participants were aged between 18 and 45 years. Because the women in our sample also include subjects reaching menopause that are predicted to show high FBG levels correlated with age. The disparity in food habits and behaviors can also lead to this discrepancy.
Use of OCPs and blood pressure
Our current study, showed that the MAP of OCP users (88.2 ± 8.48 mmHg) and systolic blood pressure (121.8 ± 8.0 mmHg) were relatively higher than OCPs non-users (111.00 ± 8.12), with a p-value of 0.04 and 0.001 respectively (as shown in Table 2).
Such results from this research were consistent with a study in Pakistan (24) that found significantly higher SBP and DBP among pill users than controls. A related follow-up analysis by Azima and Mousavi (4) found that one year after pill intake, SBP was significantly higher compared to the baseline level. Likewise, the study conducted in Korea (7) found similar results with current research, that prolonged use of OCP is related to higher blood pressure than in non-users. A study on blood pressure in women using OCPs in England (25) found that blood pressure among OCPs users was significantly higher than the controls. A similar study of hypertension among users of OCPs conducted in Texas, United States showed an increased blood pressure in both over-the-counter and clinic users of the pills (26). The reason behind for higher blood pressure among OCPs users might be due to the fact that estrogen containing hormonal contraceptives always change the blood pressure by increasing hepatic production of angiotensinogen, which in turn causes the renin-angiotensin-aldosterone system to elevate the blood pressure (27–29). Furthermore, hypertension has been linked to OCP, especially when used over a prolonged period of time (30).
OCPs use and body weight and BMI
In our current study, significantly higher mean values of body weight (56.5 ± 4.9) and BMI (21.3 ± 2.3) were recorded among OCP users as compared with non-user controls (55.10 ± 5.40 and 20.50 ± 1.82), with a p-value of 0.03 and 0.003 respectively, as shown in Table 2. This is in line with a study conducted in Thailand (31) on the effect of the use of OCPs on BMI and blood pressure, according to which, the use of pills containing estrogen and progestin tends to increase BMI and body weight. Another study of the effect of OCPs on lipid profile, blood pressure, and BMI in Pakistan (24) also showed similar results to this report. Contraceptives induced weight gain could be attributed to fluid retention secondary to the activation of the mineralocorticoid and/or renin-angiotensin-aldosterone system and/or an increase in subcutaneous fat secondary to an increase in appetite and food intake caused by hormones (32) On the other hand, study in Minnesota found that pill users have a higher body weight than their controls, but not statistically significant (33). The disparity found between the studies could be attributed to the difference in race associated with a genetic weight gain predisposition, where black women had a higher mean weight gain compared to white (34).
Limitations of the study
The potential confounders including total daily calorie intake, physical activity, and intake of cholesterol-rich diets were not measured objectively and the outcome was not compared with the outcomes blood glucose, BP, and BMI. The FBG, MAP, and BMI of OCPs users were not compared with their respective pretreatment values because they were not found on the client's card and registration book. This study is cross-sectional rather than cohort in design, with relatively small sample sizes. So, further longitudinal study with a larger sample size is needed to evaluate the changes in glucose metabolism, blood pressure, and BMI that are associated with use of OCP.
Conclusions
OCP use for in average more than two years was associated with higher fasting glucose, MAP, body weight and BMI compare to controls. The higher MAP, body weight and BMI among OCP users seemed to be dependent on the duration of OCP use.
Data availability statement
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by departmental research and ethical committee (DRC) of college of health sciences, Tikur-Anbessa Hospital, Addis Ababa University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
ZK designed the study, participated in data collection, performed analysis and interpretation of data, and drafted the paper and manuscript. YS and DH designed, approved the proposal with some revisions, participated in data analysis and revised subsequent drafts of the paper and the manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
We are grateful to all supervisors, data collectors, and study participants for taking part in our study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Brynhildsen J. Combined hormonal contraceptives: prescribing patterns, compliance, and benefits versus risks. Ther Adv Drug Saf. (2014) 5(5):201–13. doi: 10.1177/2042098614548857
2. Ahmed S, Li Q, Liu L, Tsui AO. Maternal deaths averted by contraceptive use: an analysis of 172 countries. Lancet. (2012) 380(9837):111–25. doi: 10.1016/S0140-6736(12)60478-4
3. Hubacher D, Trussell J. A definition of modern contraceptive methods. Contraception. (2015) 92(5):420–1. doi: 10.1016/j.contraception.2015.08.008
4. Azima S, Mousavi S. Oral contraceptive pills use and hypertension. Int J Pharmaceut Sci Invention. (2017) 6(1):47–9. International journal of pharmaceutical science invention ISSN (Online): 2319–6718, ISSN (Print): 2319–670X www.ijpsi.org 6(1) (2017) P. 47–9
5. Margolis KL, Adami HO, Luo J, Ye W, Weiderpass E. A prospective study of oral contraceptive use and risk of myocardial infarction among Swedish women. Fertil Steril. (2007) 88(2):310–16. doi: 10.1016/j.fertnstert.2006.11.206
6. Edelman AB, Carlson NE, Cherala G, Munar MY, Stouffer RL, Cameron JL, et al. Impact of obesity on oral contraceptive pharmacokinetics and hypothalamic–pituitary–ovarian activity. Contraception. (2009) 80(2):119–27. doi: 10.1016/j.contraception.2009.04.011
7. Park H, Kim K. Associations between oral contraceptive use and risks of hypertension and prehypertension in a cross-sectional study of Korean women. BMC women's Health. (2013) 13(1):39. doi: 10.1186/1472-6874-13-39
8. González C, Alonso A, Grueso NA, Díaz F, Esteban MM, Fernández S, et al. Role of 17β-estradiol administration on insulin sensitivity in the rat: implications for the insulin receptors. Steroids. (2002) 67(13):993–1005. doi: 10.1016/S0039-128X(02)00073-9
9. Sugiharti S, Hadi H, Julia M. Hormonal contraception as a risk factor for obesity. Med J Indones. (2005) 14(3):163–168. doi: 10.13181/mji.v14i3.191
10. Liu H, Yao J, Wang W, Zhang D. Association between duration of oral contraceptives use and risk of hypertension: meta analysis. J Clin Hypertens. (2017) 19:1032–41. doi: 10.1111/jch.13042
11. Wang C, Li Y, Bai J, Qian W, Zhou J, Sun Z, et al. General and central obesity, combined oral contraceptive use and hypertension in Chinese women. Am J Hypertens. (2011) 24(12):1324–30. doi: 10.1038/ajh.2011.157
12. Ordóñez P, Moreno M, Alonso A, Llaneza P, Díaz F, González C. 17beta-Estradiol And/or progesterone protect from insulin resistance in STZ-induced diabetic rats. J Steroid Biochem Mol Biol. (2008) 111(3-5):287–94. doi: 10.1016/j.jsbmb.2008.07.001
13. Sutter-Dub MT. Rapid non-genomic and genomic responses to progestogens, estrogens, and glucocorticoids in the endocrine pancreatic B cell, the adipocyte and other cell types. Steroids. (2002) 67:77–93. doi: 10.1016/S0039-128X(01)00142-8
14. Mkuu RS, Epnere K, Chowdhury MAB. Prevalence and predictors of overweight and obesity among Kenyan women. Prev Chronic Dis. (2018) 15:E44. doi: 10.5888/pcd15.170401
15. Hong SA, Peltzer K, Lwin KT. The prevalence of underweight, overweight and obesity and their related socio-demographic and lifestyle factors among adult women in Myanmar, 2015-16. PLoS One. (2018) 13(3):e0194454. doi: 10.1371/journal.pone.0194454
16. World Health Organization, WHO STEPS surveillance manual: the WHO STEPwise approach to chronic disease risk factor surveillance, (No. WHO/NMH/CHP/SIP/05.02). Geneva: World Health Organization (2005)
17. Schwartzbard AZ, Newman JD, Weintraub HS, Baum SJ. The 2017 high blood pressure clinical practice guideline: the old and the new. Clin Cardiol. (2018) 41(3):279. doi: 10.1002/clc.22905
18. Nuttall FQ. Body mass index: obesity, BMI, and health: a critical review. Nutr Today. (2015) 50(3):117. doi: 10.1097/NT.0000000000000092
19. Villavicencio J, Allen RH. Unscheduled bleeding and contraceptive choice: increasing satisfaction and continuation rates. Journal of Contraception. (2016) 7(1):43–52. doi: 10.2147/OAJC.S85565.
20. World Health Organization & International Diabetes Federation, Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation. Geneva: World Health Organization (2006). https://apps.who.int/iris/handle/10665/43588
21. Godsland IF, Crook D, Simpson R, Proudler T, Felton C, Lees B, et al. The effects of different formulations of oral contraceptive agents on lipid and carbohydrate metabolism. N Engl J Med. (1990) 323(20):1375–81. doi: 10.1056/NEJM199011153232003
22. Piltonen T, Puurunen J, Hedberg P, Ruokonen A, Mutt SJ, Herzig KH, et al. Oral, transdermal and vaginal combined contraceptives induce an increase in markers of chronic inflammation and impair insulin sensitivity in young healthy normal-weight women: a randomized study. Hum Reprod. (2012) 27(10):3046–56. doi: 10.1093/humrep/des225
23. Berenson AB, van den Berg P, Williams KJ, Rahman M. Effect of injectable and oral contraceptives on glucose and insulin levels. Obstet Gynecol. (2011) 117(1):41. doi: 10.1097/AOG.0b013e318202ac23
24. Mohammad NS, Nazli R, Khan A, Akhtar T, Ahmad J, Zafar Z. Effect of combined oral contraceptive pills on lipid profile, blood pressure and body mass index in women of childbearing age. Khyber Med Uni J. (2013) 5(1):22–6. Available from: https://www.kmuj.kmu.edu.pk/article/view/11148
25. Dong W, Colhoun HM, Poulter NR. Blood pressure in women using oral contraceptives: results from the health survey for England 1994. J Hypertens. (1997) 15(10):1063–8. doi: 10.1097/00004872-199715100-00003
26. White K, Potter JE, Hopkins K, Amastae J, Grossman D. Hypertension among oral contraceptive users in El Paso, Texas. J Health Care Poor Underserved. (2013) 24(4):1511. doi: 10.1353/hpu.2013.0172
27. Szwarcwald CL, Costa SH, de Azeredo Costa E, Klein CH, do Carmo Leal M. Anticoncepcionais orais e pressão arterial: pesquisa epidemiológica de hipertensão arterial no Rio Grande do sul. Cadernos de Saúde Pública. (1985) 1(2):177–91. doi: 10.1590/S0102-311X1985000200005
28. Brito MB, Nobre F, Vieira CS. Hormonal contraception and cardiovascular system. Arq Bras Cardiol. (2011) 96(4):e81–9. doi: 10.1590/S0066-782X2011005000022
29. Oelkers WK. Effects of estrogens and progestogens on the renin-aldosterone system and blood pressure. Steroids. (1996) 61(4):166–71. doi: 10.1016/0039-128X(96)00007-4
30. Afshari M, Alizadeh-Navaei R, Moosazadeh M. Oral contraceptives and hypertension in women: results of the enrolment phase of tabari cohort study. BMC Women's Health. (2021) 21(1):1–7. doi: 10.1186/s12905-021-01376-4
31. Murayama N, Matsunaga A, Tangbanluekal L, Tantawiwat S, Ohtsuka R. Effects of oral contraceptive use on body mass index and blood pressure among female villagers in north-east Thailand. J Biosoc Sci. (2003) 35(2):243–61. doi: 10.1017/S0021932003002438
32. Gallo MF, Grimes DA, Schulz KF, Helmerhorst FM. Combination estrogen–progestin contraceptives and body weight: systematic review of randomized controlled trials. Obstet Gynecol. (2004) 103(2):359–73. doi: 10.1097/01.AOG.0000107298.29343.6a
33. Kharbanda EO, Parker ED, Sinaiko AR, Daley MF, Margolis KL, Becker M, et al. Initiation of oral contraceptives and changes in blood pressure and body mass index in healthy adolescents. J Pediatr. (2014) 165(5):1029–33. doi: 10.1016/j.jpeds.2014.07.048
Keywords: contraceptives, pills, BMI, family planning, chencha
Citation: Kofole Z, Haile D and Solomon Y (2023) Fasting blood glucose, blood pressure and body mass index among combined oral contraceptive users in Chencha town Southern Ethiopia, 2019. Front. Glob. Womens Health 4:992750. doi: 10.3389/fgwh.2023.992750
Received: 13 July 2022; Accepted: 7 April 2023;
Published: 28 April 2023.
Edited by:
Anne E. Burke, Johns Hopkins University, United States© 2023 Kofole, Haile and Solomon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zelalem Kofole a3plbGFsZW0yMDA4QGdtYWlsLmNvbQ== Yerukneh Solomon eWVydWtuZXNvbG9tb25AZ21haWwuY29t
 Zelalem Kofole
Zelalem Kofole Diresbachew Haile
Diresbachew Haile Yerukneh Solomon
Yerukneh Solomon