- 1Department of Obstetrics & Gynecology, New York Medical College/Westchester Medical Center, Valhalla, NY, United States
- 2Vitala Global, Vancouver, BC, Canada
- 3Fòs Feminista, New York, NY, United States
- 4Ipas, Chapel Hill, NC, United States
- 5Department of Obstetrics & Gynecology, University of Toronto, Toronto, ON, Canada
Introduction: In the last decade, Venezuela has experienced a complex humanitarian crisis that has limited access to healthcare. We set out to describe Venezuelan women's experiences accessing sexual and reproductive health services, including abortion, which is heavily restricted by law.
Methods: We fielded an online survey in July of 2020 among Venezuelan women recruited through social media advertisements. We conducted descriptive statistical analyses using Excel and STATA SE Version 16.0.
Results: We received 851 completed survey responses. Almost all respondents experienced significant hardship in the last year, including inflation (99%), worries about personal safety (86%), power outages (76%), and lack of access to clean water (74%) and medications (74%). Two thirds of respondents used contraception in the last two years, and almost half (44%) of respondents had difficulty accessing contraception during that same time period. About one fifth of respondents reported having had an abortion; of these, 63% used abortion pills, and 72% reported difficulties in the process. Half of those who had an abortion did it on their own, while the other half sought help – either from family members or friends (34%), from providers in the private health sector (14%), or from the Internet (12%).
Conclusions: Venezuelan women who responded to our survey describe a harsh context with limited access to sexual and reproductive health services. However, they report relatively high rates of contraceptive use, and abortion seems to be common despite the restrictive legal setting.
1. Introduction
For the last decade, Venezuelans have lived in crisis. In the early years of President Hugo Chavez' rule, the country experienced an oil-fueled economic boom, with promising results at the public health level, such as rising life expectancy and decreased infant mortality rates (1). When oil prices began to fall in 2008, the country's economy crashed, leading to hyper-inflation and a fall in the gross domestic product. Lack of foreign currency needed to import necessary goods and supplies led to a shortage of basic necessities – including fuel, medications and healthcare supplies (1). Many Venezuelan healthcare workers emigrated, including about half of the country's physicians, further contributing to a complete collapse of the country's healthcare system (2).
Human rights organizations have described the Venezuelan context as a “complex humanitarian emergency,” a situation in which a considerable breakdown of authority leads to human suffering on a major scale (3). According to the fragile states index, Venezuela was among the top five countries that worsened in the last decade (4). A report published in 2019 based on data collected by non-governmental organizations showed that almost all households experienced food insecurity, and rates of hospital admissions for childhood malnutrition were rising rapidly (5).
Accessing sexual and reproductive health (SRH) services in this context is challenging. For many, purchasing contraceptives can be cost-prohibitive (6). These are often unavailable due to chronic supply shortages, and are considered to be luxury items purchased on clandestine markets (6). Access to abortion is restricted by Venezuelan law, which only allows it when a woman's life is at risk (7). Although recent official government data are lacking, news organizations and civil society groups in Venezuela have described a crisis in maternal health (8). From 2015 to 2016, the last years for which official data are published, maternal deaths increased by 65% (from 456 to 756) (9). Maternal complications from unsafe abortion such as hemorrhage and infection accounted for 7% of maternal deaths reported in Venezuelan health facilities in a six-month period in 2018 (10).
News and humanitarian reports have described the challenges of accessing SRH services in Venezuela, but few if any research studies have broached this topic. We aimed to describe Venezuelan women's successes and challenges in accessing abortion and contraception in this complex humanitarian context.
2. Methods
This is a cross-sectional survey study. We conducted this survey as part of a three-phase user-centered design project aimed at developing a digital tool for self-managed abortion in Venezuela. For Phase 1 of this project, we collected quantitative and qualitative data to understand how women access sexual and reproductive health services in Venezuela, as well as their preferences for receiving information about these topics. Here, we report on the quantitative results of this phase of the project.
The research team consisted of international obstetrics & gynecology clinicians and researchers, women's rights activists, and local sexual and reproductive healthcare providers. We collaborated to design a survey, which we pilot-tested with Venezuelan women and modified accordingly.
We fielded the online survey using social media platforms. In partnership with a specialized media firm, we disseminated social media advertisements through the Facebook and Instagram accounts of PLAFAM (Asociación Civil de Planificación Familiar), a sexual and reproductive healthcare organization in Venezuela that is a partner of Fòs Feminista.
We only included completed responses in the analysis. We used Microsoft Excel and Stata SE Version 16.0 to conduct descriptive statistical analyses of survey responses.
The Allendale Institutional Review Board approved this study.
3. Results
We advertised the survey during six days in July of 2020, and received a total of 851 completed survey responses. Table 1 shows the demographic characteristics of survey respondents. Most were young women (27% were 19–25, and 36% were 26–35). Almost half (360, 42%) of respondents had completed university and a third (279, 32.8%) had some university education. Most respondents had encountered social and economic challenges in the past year, with the most common being inflation (99%), worrying about personal safety (86%), and power outages (76%).

Table 1. Characteristics of individuals who responded to an online survey conducted in 2020 about sexual and reproductive health in Venezuela.
3.1. Contraception
When asked about contraceptive use, approximately two thirds of respondents (565, 66.4%) reported having used a contraceptive method in the last two years. The most popular methods were the male condom (240, 43.9%) and the implant (212, 37.5%), followed by contraceptive pills (151, 26.7%) and the IUD (141, 25.0%). Most respondents obtained contraceptives from PLAFAM (56.3%) or from a pharmacy (40.7%). Almost half of respondents who used contraception (247, 44.0%) had difficulties accessing contraceptive methods in the last two years. The most common difficulties experienced were high cost (239, 96.8%), lack of availability of their preferred method (193, 78.1%), and transportation issues (77, 31.2%). Table 2 shows contraceptive use and difficulty accessing contraception.
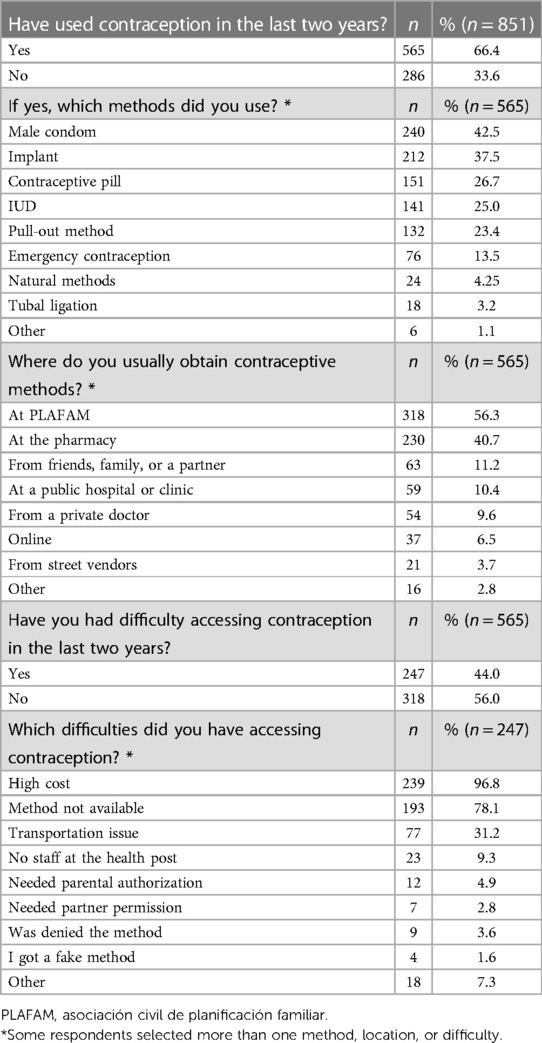
Table 2. Contraceptive access, use and challenges among individuals who responded to an online survey conducted in 2020 in Venezuela.
3.2. Abortion
Almost half of survey respondents (364, 42.8%) experienced an unplanned pregnancy in their lifetime, and one fifth had an abortion at some point in their life (169, 19.9%). Two thirds of respondents (563, 66.2%) reported they knew a friend or family member who has had an abortion. Of the 169 respondents who had an abortion, roughly two thirds did so using abortion pills (106, 62.7%), while about one third had a procedure performed by a physician (61, 36.1%). Other abortion methods such as herbal remedies and procedures performed by non-physicians were less frequent. Some respondents selected more than one abortion method. Approximately half of respondents who had an abortion experienced difficulties accessing one, with the most common difficulty being fear that something bad would happen (82, 48.5%). Half those who had an abortion (via any method) sought help from other people, while the other half did not. Table 3 shows access to abortion and difficulties experienced in this process.
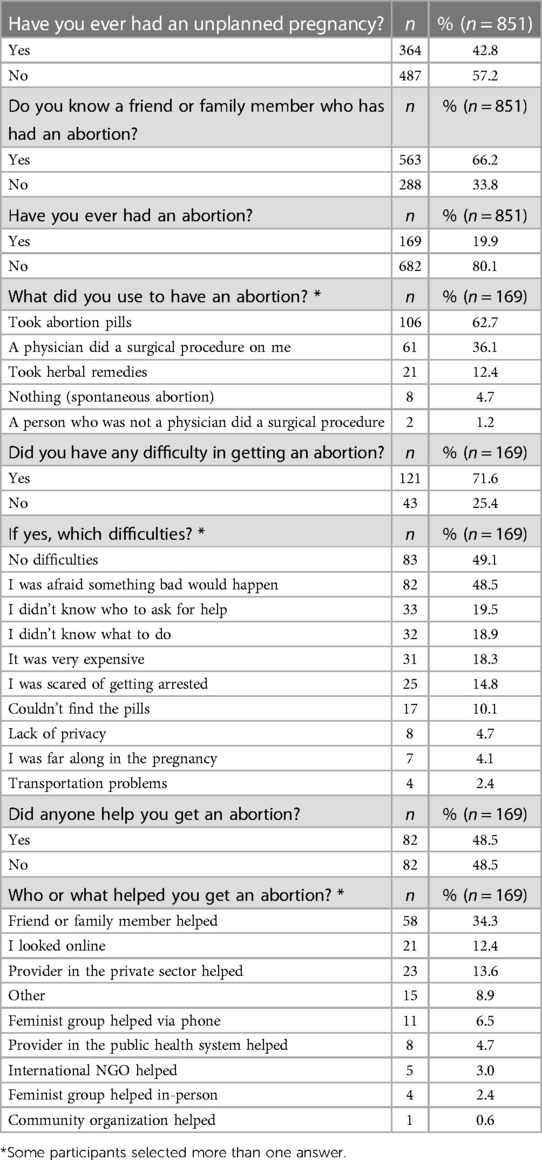
Table 3. Access to abortion among individuals who responded to an online survey conducted in 2020 in Venezuela.
4. Discussion
Results from this online survey of Venezuelan women show that although almost two thirds of respondents used some form of contraception in the two years prior to the survey, almost half of them had problems accessing contraceptive methods in the context of the country's ongoing humanitarian crisis. This finding aligns with existing reports from newspapers and nonprofit organizations (2, 6). A 2019 report published by a coalition of civil society groups reported on scarcity of contraceptives in pharmacies in five cities in Venezuela. They reported that in December of 2018, for example, 75% of the pharmacies queried did not have any contraceptive pills available. The scarcity index was even higher for other methods, including injectables and long-acting reversible methods (11).
We found that the male condom was the most common method used but are unable to tease out whether this was used alone or with other methods. Condoms are easy to access at PLAFAM (for free or subsidized) or from pharmacies. This may make them more easily accessible than other methods. It is interesting to note that the contraceptive implant was one of the most common methods used by our survey respondents, despite it being very difficult to find in Venezuelan pharmacies (11). This is likely because our recruitment strategy targeted social media users who had visited the PLAFAM page. PLAFAM is one of the few organizations that provides free or low cost contraceptive implants in Venezuela (2), and half of our respondents obtained their contraceptive method there. The contraceptive implant is the method most provided at PLAFAM, followed by intrauterine devices.
Another important finding of this study is that despite the near total ban on abortion in Venezuela, a fifth of respondents reported they had an abortion sometime in their life. This is in line with Latin American and the Caribbean regional estimates from the Guttmacher Institute regarding the share of unintended pregnancies that end in abortion, which is approximately 46%. In 2015–2019, there were almost 8 million unintended pregnancies and almost 4 million abortions (12). Banning abortion does not prevent it, but rather increases the proportion of abortions that are unsafe (13). We note that only 14.8% of our respondents who had an abortion reported fear of being arrested as a difficulty in accessing abortion. Thus, there seemed to be relatively little fear of legal prosecution reported by our respondents despite the restrictive legal landscape.
In our study, abortion pills were the most common method used for abortion (106, 62.7%). We did not ask about specific pill regimens used, but we assume that most individuals used misoprostol alone. Mifepristone is not registered in Venezuela, though it can sometimes be obtained through international organizations. For the third of respondents who had abortions performed by a physician, we are unable to delineate whether these were legal abortions under the exception to save the life of the woman or clandestine induced abortion procedures. Some may have been provision of post-abortion care after incomplete abortions induced with medications. In any case, it is interesting to note that physicians are involved in a large proportion of the abortions reported by our respondents.
Our findings add to the current state of knowledge about abortion in Venezuela, which comes primarily from reports of abortion hotlines run by feminist accompaniment groups. A 2019 report published by Faldas-R, a group that runs an abortion support hotline, called abortion a “daily occurrence” in Venezuela, supporting our finding of abortion being relatively common (14). This group reported a 40% increase in calls to their hotline from 2018 to 2019, suggesting that the incidence of abortion may be increasing with the worsening economic crisis. The authors of a qualitative study that examined abortion hotlines in five countries describe one hotline in Venezuela, which received approximately 450 calls per month (15). While these collectives serve an important role in helping women access safe abortion, less than ten percent of our respondents who had an abortion sought the help of a women's group, either in-person or via phone. Most went to friends, family members, and private physicians – thus suggesting that abortion is even more common than the estimates based on hotline calls.
Our study has several limitations. First, it is a survey study and as such it is subject to response bias. Because the survey was hosted on social media, only those who knew how to use technology and had access to data could respond. This explains why younger women and university graduates were over-represented among our respondents. Further, we used PLAFAM's social media pages to promote the survey, and PLAFAM is the only entity in Venezuela that has been able to provide reliable and affordable access to contraceptive methods in recent years. Hence our high prevalence of contraceptive use is likely a biased view that is only representative of PLAFAM's clientele and not of the Venezuelan population as a whole. That said, most of our respondents experienced fuel shortages, lack of access to the Internet, clean water, medicines, and transportation, among other challenges – thus demonstrating that they were not insulated by privilege. Social desirability bias is another risk inherent to any survey that covers sensitive topics related to sexual and reproductive health – it is possible that respondents under-reported abortions, for example (16). However, the anonymity of our survey may have reduced this bias.
Our study also has several strengths. First, our survey was designed and pilot-tested with input from multiple stakeholders in Venezuela and around the world. Second, it utilizes a novel strategy, harnessing the power of social media to reach a wide range of women who would not otherwise be engaged in research. It is important to note that the study was conducted in July of 2020, at the height of the COVID-19 pandemic. Social media allowed us to reach a relatively large number of respondents remotely without putting their health at risk. Finally, this is the only study to our knowledge that quantitatively describes women's access to abortion and contraception in the country's humanitarian context, providing a snapshot of the two-year period from July 2018 to July 2020. Overall, our findings represent a new contribution to the scientific literature. Future research should continue to investigate the impact on women's reproductive and sexual health of the evolving Venezuelan political and economic context.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Allendale Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BS participated in survey design, conducted data analysis, and wrote the first draft of the manuscript. RG had the idea for the research, participated in survey design, and edited the manuscript. GL, GT, NZ, GC, and SM-S participated in survey design and data collection efforts. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by a grant by Grand Challenges Canada's OPTions Iniatiative.
Acknowledgments
We wish to acknowledge the contributions and efforts of: PLAFAM, a Venezuelan sexual and reproductive health organization that is a partner of Fòs Feminista, Antonella Lavelanet at the World Health Organization Department of Sexual and Reproductive Health Research, and The Game, an Ecuadorian-based social media and marketing company that supported our social media survey strategy. The Game was not involved in the study design, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. The Lancet. The collapse of the Venezuelan health system. Lancet (London, England). (2018) 391:1331. doi: 10.1016/S0140-6736(16)00277-4
2. Turkewitz J, Herrera I. Venezuelan women lose access to contraception, and control of their lives. New York Times (2021). Available from: https://www.nytimes.com/2021/02/20/world/americas/venezuela-birth-control-women.html (Accessed February 1, 2023).
3. UNHCR. Coordination in Complex Emergencies (2001). Available at: https://www.unhcr.org/en-us/partners/partners/3ba88e7c6/coordination-complex-emergencies.html (Accessed February 20, 2023).
4. Fund for Peace. Fragile states index annual report 2021. Washington, D.C.: Fund for Peace (2021).
5. Doocy S, Ververs M-T, Spiegel P, Beyrer C. The food security and nutrition crisis in Venezuela. Soc Sci Med. (2019) 226:63–8. doi: 10.1016/j.socscimed.2019.02.007
6. Luigi-Bravo G, Gill RK. Safe abortion within the Venezuelan complex humanitarian emergency: understanding context as key to identifying the potential for digital self-care tools in expanding access. Sex Reprod Heal Matters. (2021) 29:2067104. doi: 10.1080/26410397.2022.2067104
7. Global Abortion Policies Database. Country Profile: Venezuela 2017. https://abortion-policies.srhr.org/ [Accessed February 1, 2023].
8. Turkewitz J, Herrera I. Childbirth in Venezuela, where women’s deaths are a state secret. New York Times (2020). https://www.nytimes.com/2020/04/10/world/americas/venezuela-pregnancy-birth-death.html [Accessed February 1, 2023].
9. Gobierno Bolivariano de Venezuela. Boletín Epidemiológico (2016). https://www.ovsalud.org/wp-content/uploads/Boletin-Epidemiologico-2016.pdf [Accessed July 1, 2023].
10. Mujeres al Limite. Derechos de las mujeres de cara al agravamiento de la emergencia humanitaria en Venezuela. Caracas. (2019) https://www.academia.edu/40709441/MUJERES_AL_L%C3%8DMITE_2019_DERECHOS_DE_LAS_MUJERES_DE_CARA_AL_AGRAVAMIENTO_DE_LA_EMERGENCIA_HUMANITARIA_COMPLEJA_EN_VENEZUELA [Accessed February 1, 2023].
11. Equivalencias en Acción. ĺndice de escasez de métodos anticonceptivos en farmacias de cinco ciudades de Venezuela. (2019). https://avesawordpress.files.wordpress.com/2019/02/indice-escasez-ma.-enero-2019.pdf [Accessed February 1, 2023].
12. Guttmacher Institute. Unintended Pregnancy and Abortion in Latin America and the Caribbean (2022). [factsheet]. https://www.guttmacher.org/fact-sheet/unintended-pregnancy-and-abortion-latin-america-and-caribbean. [Accessed February 1, 2023].
13. Ganatra B, Gerdts C, Rossier C, Johnson BR, Tunçalp Ö, Assifi A, et al. Global, regional, and subregional classification of abortions by safety, 2010–14: estimates from a Bayesian hierarchical model. Lancet. (2017) 390(10110):P2372–81. doi: 10.1016/S0140-6736(17)31794-4
14. Faldas R. El aborto desde la escucha: informe de atencion de la linea aborto: información segura. (2019). https://clacaidigital.info/handle/123456789/1328 [Accessed February 1, 2023].
15. Drovetta RI. Safe abortion information hotlines: an effective strategy for increasing women’s access to safe abortions in Latin America. Reprod Health Matters. (2015) 23:47–57. doi: 10.1016/j.rhm.2015.06.004
Keywords: abortion, contraception, Venezuela, survey, social media, humanitarian crisis, sexual and reproductive health, digital health post-abortion care
Citation: Stifani BM, Luigi G, Tam G, Zamberlin N, Carino G, Medina-Salas S, Fetters T and Gill R (2023) Contraception and abortion in times of crisis: results from an online survey of Venezuelan women. Front. Glob. Womens Health 4:1189706. doi: 10.3389/fgwh.2023.1189706
Received: 19 March 2023; Accepted: 21 August 2023;
Published: 18 September 2023.
Edited by:
Catherine Todd, Independent Researcher, Lusaka, ZambiaReviewed by:
Deborah L. Billings, University of South Carolina, United StatesHeather Vahdat, Male Contraceptive Initiative, United States
© 2023 Stifani, Luigi, Tam, Zamberlin, Carino, Medina-Salas, Fetters and Gill. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bianca M. Stifani YmlhbmNhLnN0aWZhbmlAZ21haWwuY29t Roopan Gill cmdpbGxAdml0YWxhZ2xvYmFsLm9yZw==
 Bianca M. Stifani
Bianca M. Stifani Genesis Luigi2
Genesis Luigi2 Giselle Carino
Giselle Carino Tamara Fetters
Tamara Fetters