- 1School of Midwifery, College of Midwifery, Woldia University, Woldia, Ethiopia
- 2School of Public Health, College of Midwifery, Woldia University, Woldia, Ethiopia
Background: A female genital fistula is an abnormal connection between a woman's reproductive tract and her urinary tract or rectum. While numerous studies have aimed to determine the success rate of obstetric fistula closure in different health settings, there remains a significant scarcity of data on closure success rates and incontinence rates for various types of fistulas at the regional and sub-regional levels. The success rate reflects the continent's healthcare setup in regard to the World Health Organization standards. Thus, this study aims to determine the success of surgical closure and the continence rate of obstetric fistula in Africa.
Methods: This systematic review and meta-analysis review includes studies conducted up to February 2023. Search engines like EMBBASE, Medline, Google, PubMed, Google Scholar, African Journals Online, and ScienceDirect databases were utilized to find articles. The Joanna Briggs Institute critical evaluation checklist was used to evaluate the quality of our review, which was conducted in accordance with PRISMA criteria. Heterogeneity was indicated by a p-value for I2 statistics of less than 0.05. Publication bias was assessed using the Egger regression asymmetry test. Data were entered into Microsoft Excel and analyzed using STATA 16.
Result: This review includes 85 studies. A total of 24 countries from East, West, Central, North, and Southern African sub-regions were included. The overall pooled estimated rate of successful obstetric fistula closure is 86.15 (95% CI: 83.88–88.42). Moreover, the pooled estimated rate of successfully closed vesico-vaginal fistulas but with ongoing or residual incontinence (wet) was revealed as 13.41% (95% CI: 11.15–15.68). The pooled estimated rate of successfully closed rectovaginal fistulas and combined VVF and RVF are 91.06% (95% CI: 86.08–96.03) and 62.21% (95% CI: 48.94–75.49), respectively.
Conclusions: The rate of successful obstetric fistula closure in Africa is 86.15, which is higher than the WHO target. However, the surgical closure rate of a combined VVF and RVF is 62.2%, which is significantly lower than the WHO target.
Introduction
A female genital fistula is an abnormal connection between a woman's reproductive tract and her urinary tract or rectum (1). The World Health Organization (WHO) describes vaginal fistulas as the single most cause adverse consequence of neglected childbirth (2). Vaginal fistulas are common in poor countries, mostly in South Asian and Sub-Saharan African nations, where the social norm promotes marriage at a young age, frequently soon after the girl's first period between the ages of 9 and 15. The first pregnancy occurs soon after marriage in many of these situations (3, 4).
Although the global burden of the disease is not exactly known, it is estimated to be 3 million, with 30,000 to 130,000 new cases added each year. Additionally, over 2 million women are living with untreated obstetric fistula in developing countries (5, 6). Fistulas can be categorized, depending on the affected anatomical regions, as rectovaginal fistulas (between the genital tract and the rectum) or vesicovaginal fistulas (between the genital tract and the urinary tract) (7, 8).
Female genital fistulas can occur because of obstetric complications, gynecological procedures, and trauma. Even in expert hands, genital tract injuries are known to occur during gynecological procedures (2, 9). The incidence and the etiology of genital fistulas show geographical variation. In developed countries, 83.2% of fistulas occur following surgery, whereas in low-resourced countries, 95.2% are associated with childbirth when women do not have access to timely emergency obstetric care (10).
The consequences of obstetric fistula are far greater than the visible medical condition. Women with obstetric fistulas have a persistent odor associated with continued urine and/or stool leakage, putting them at risk of health problems and ostracization by their husbands and community, with up to 52% of affected women facing divorce. It is also linked to a higher risk of mental health disorders, with nearly 97% of affected women screening positive for potential mental health disorders. Moreover, obstetric fistula affects economically vulnerable women and garners little attention on the global health stage (11, 12).
With the extensive effects of fistulas on women's health, surgical closure of the fistula is critical to the woman's overall well-being; without it, the likelihood of fistula resolution is almost null, except in the rare cases of early fistula closure by immediate catheterization (13, 14). The WHO established the ideal range of repair outcomes as less than 15% for failed fistula closure and less than 10% for incontinence after successful closure (15). However, there are not many facilities that have the tools and staff that are qualified to conduct fistula closure. Moreover, surgical closure of obstetric fistula does not ensure the patient will have a satisfactory outcome and be able to resume her normal activities; up to 42% of fistula repairs fail, and up to 67% of successful surgical closures result in residual incontinence (16, 17).
Interestingly, the degree of success in obstetric fistula treatment varies depending on the patient (fistula type and location) and health system (staff training, surgical expertise) (18, 19). Although numerous studies have attempted to identify the success rate of fistula repair in African nations, which ranges from 42% in Angola to 97% in Malawi (16, 20); there is a lack of data on the success rate of fistula closure at the continental and sub-region level to indicate the health care setting status. Therefore, this study aims to assess the successful surgical closure rate of obstetric fistula (VVF, RVF, and combined VVF and RVF) in Africa.
Methods
Study design and setting
This systematic review and meta-analysis includes cross-sectional, cohort, and randomized control trial studies conducted in Africa. A comprehensive review and analysis of data from computerized databases was conducted to determine the success rate of fistula closure in Africa.
Search strategy
For this review, relevant articles were searched with different search strategies. Published articles were searched from online databases such as EMBBASE, Medline, Google, PubMed, Google Scholar, African Journals Online, and ScienceDirect databases. In addition, we extended our search by retrieving and extracting potential articles from reference lists of eligible articles. A recommended PRISMA guideline was strictly followed throughout this review. Similarly, the quality of our systematic review and meta-analysis was assessed by the Joanna Briggs Institute critical appraisal checklist (21).
Searching was conducted using Medical Subject Heading (MeSH) terms related to successful fistula closure or repair. MeSH terms enabled us to select related research articles. We conducted the search for terms using Boolean operators “AND” and “OR,” both separately and in combinations. The search terms for the rate of successful fistula closure were ((Fistula) OR (Obstetrics Fistula)) OR (Urinary Fistula)) OR (Vesicovaginal fistula)) OR (Ureterovaginal fistula)) OR (Rectovaginal fistula)) AND (Intervention)) OR (surgical Repair)) OR (surgical Closure)) OR (outcomes)) OR (Successful surgical closure outcomes)) AND (Africa). The search was also made by combining the above search terms with the names of all countries included in Africa. All the search terms are included in the Supplementary material.
Eligibility criteria
Inclusion criteria
There were no restrictions on research design. Cross-sectional, cohort, and randomized control trial studies conducted on the success of fistula closure in Africa were included. Only articles reported in the English language and studies conducted before February 2023 were included. The original articles assessed mainly obstetric fistula closure success rates.
Exclusion criteria
This review does not consider studies focused on fistulas caused by gynecologic surgery or trauma. We excluded articles without full text as they cannot be assessed for their quality. Agreements on the inclusion and exclusion of the articles were held through the participation of all authors.
Quality assessment
The quality of the studies were assessed using the Joana Brigg's Institute (JBI) critical appraisal checklist. The checklists were available online and it was designed separately for cross-sectional, and cohort studies. We used more than one checklist depending on the study design of the published articles. Quality assessment was carried out by all authors. The critical appraisal checklist has eight questions overall; articles with a score of 5 or more out of 8 in the JBI criteria were considered to be of good quality and were included in the review. Any critical appraisal discrepancies among reviewers were resolved through discussion with the third-party reviewer. The table containing the quality appraisal scores is available in the Supplementary material.
Heterogeneity and publication bias
The heterogeneity test of included studies was assessed using the I2 statistics. Heterogeneity was indicated by a P-value for I2 statistics of less than 0.05. The findings of the I2 test were classified as having Low (25%), Moderate (50%), and High (75%) heterogeneity (22). Moreover, the Egger regression asymmetry test was used to evaluate publication bias (23, 24). When the p-value for the Egger test is less than 0.05, publication bias is shown. Additionally, Duval and Tweedie's nonparametric trim and fill analysis using the random effect analysis was conducted to account for publication bias (25).
Outcome Variable
The outcome variable for this review was the rate of successful obstetric fistula closure. This variable has two categories, dichotomized as yes/no. We searched articles that measure and assess this outcome variable.
Data extraction and management
After the data had been screened by title, abstract and reviewing the articles. The data were prepared/extracted in Microsoft excel form, checked and evaluated by all authors. The data extraction format consists of name of first author, title, publication and study year, study country and sub-region, study design, sample size and rate of successful surgical closure of obstetrics fistula types (The extracted data is available in Supplementary file).
Registration and protocol
This review has not previously registered or prepared a protocol. As a result, no adjustments have been made.
Data processing and analysis
The extracted data were exported into Stata version 16 for analysis (meta-analysis). The heterogeneity of included studies was assessed by I2-statics. Publication bias across studies were assessed subjectively by observing the funnel plot and objectively by considering Egger's test estimates at a 5% level of significance. Forest plots were used to estimate the pooled prevalence and effect size of each study. The estimates were presented with a 95% confidence interval. The size of each box indicated the weight of the study, while each crossed line refers to the 95% confidence interval. Subgroup analysis was done by sub-region, which enables the assessment of how successful fistula closure varies across the region of Africa.
Result
Study selection
This systematic review and meta-analysis includes published studies on the surgical closure of obstetric fistula in Africa. A total of 45,242 records were retrieved through electronic database searching, and 85 articles were included to estimate the pooled rate of successful surgical closure of different types of obstetric fistula (Figure 1).
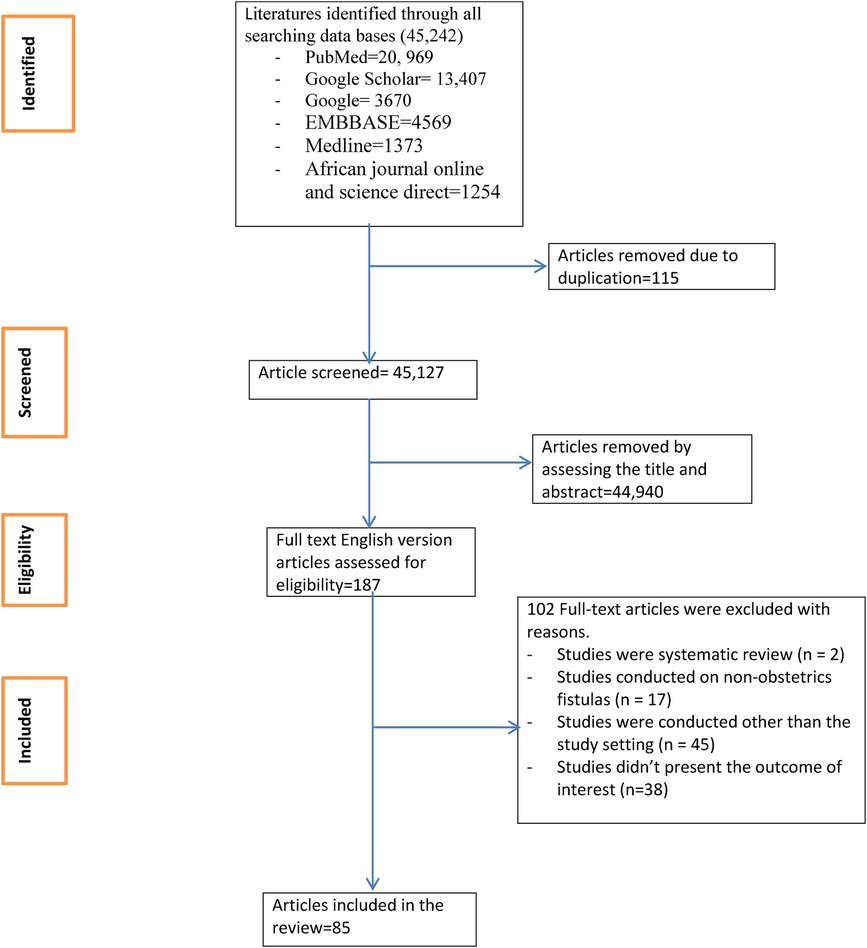
Figure 1. Flow chart of study selection for systematic review and meta-analysis of successful surgical closure of obstetric fistula in Africa.
Characteristics of included studies
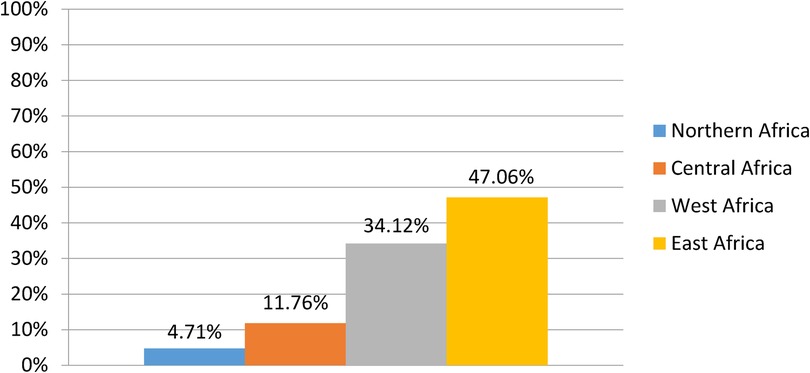
This review includes studies from 24 different African nations. Of the total, 4 (4.71%) were from Northern Africa (26–29), 10 (11.76%) were from Central Africa (13, 16, 30–37), 31 (34.12%) were from West Africa (38–68), and 40 (47.06%) (19, 69–107) were from East Africa (Figure 2). The majority of the included articles were from Sub-Saharan African countries such as Ethiopia, Nigeria, and the Democratic Republic of Congo. Except for a single cross-sectional study from Ethiopia (93), all the included articles were longitudinal and randomized control trial studies.
Rate of successful surgical closure of obstetric fistula in Africa
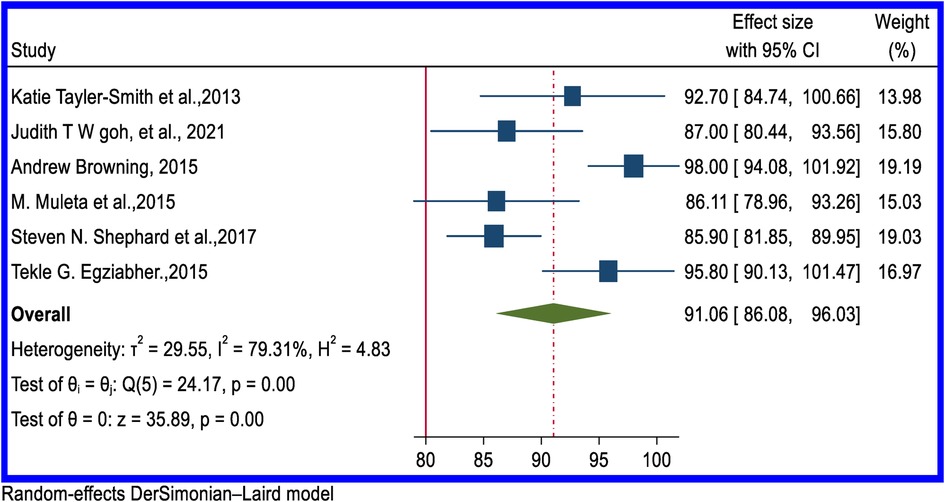
In some articles, for all types of fistulas (VVF, RVF, UVF, VUF, and combined VVF and RVF), successful closure was reported as successful obstetric fistula closure rate. Therefore, the pooled result of successful surgical closure of obstetric fistula uses “obstetric fistula” as a reference for all the different types of fistulas reported. The rate of successful fistula closure varies by country, from 42% in Angola (16) to 98.5 in Nigeria (52). The pooled estimated rate of the overall successful obstetric fistula surgical closure rate in Africa as reported by 23 articles is 86.15% (95% CI: 83.88–88.42) (Figure 3). The studies included in the meta-analysis demonstrated a substantial degree of heterogeneity (I2 = 98.03%; p-value = 0.00001). Egger's regression asymmetry test also revealed significant publication bias, with a p-value of 0.00001. The figure for funnel plot and trim and fill analysis is available in Supplementary Figures S1 and S2, respectively. After adjustment, the overall pooled successful closure rate after the trim and fill analysis was 81.3% (95% CI: 76.34–86.27).
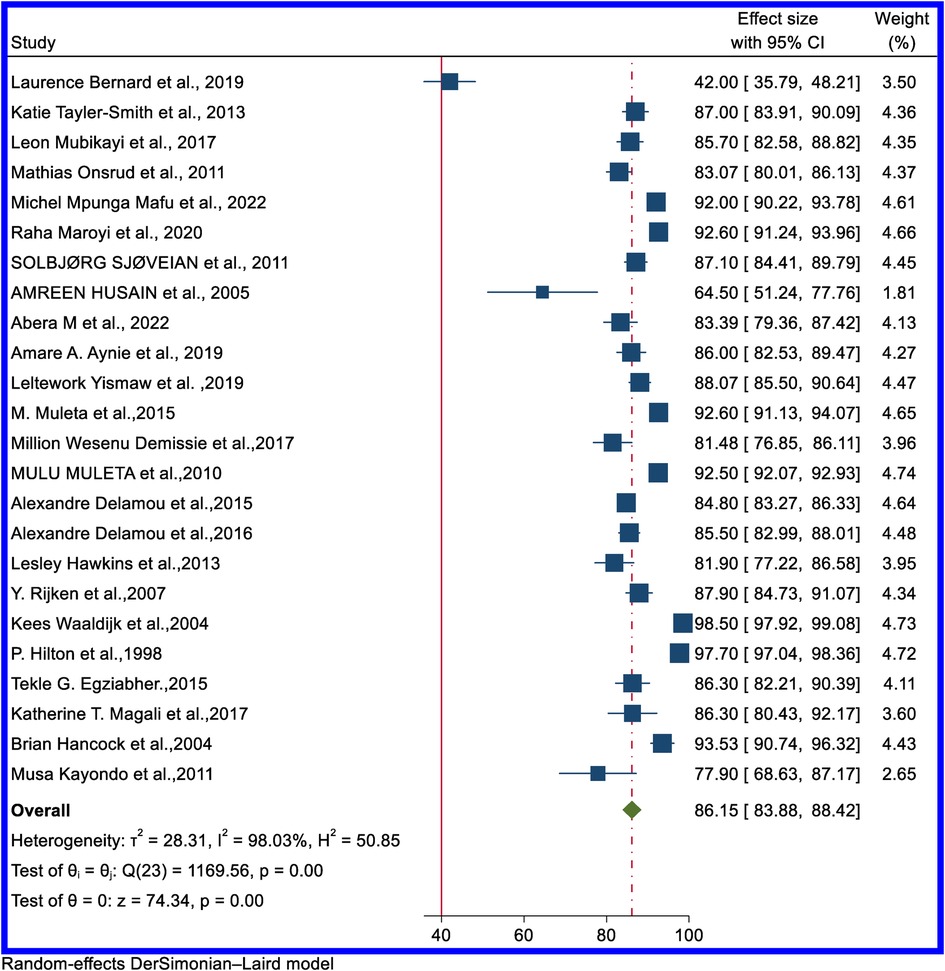
Figure 3. Forest plot of the pooled rate of successful surgical closure of overall obstetrics fistula in Africa.
In sub-regional analysis, West Africa had the highest successful surgical closure rate, at 91.74%; 95% CI: 86.61–96.88), and Central Africa had the lowest, at 84.04% (95% CI: 73.70–88.38). Supplementary Figure S3 contains a forest plot for the sub-regional distribution of the overall successful obstetric fistula surgical closure rate.
Rate of successful surgical closure of VVF in Africa
The successful surgical closure rate of VVF with unknown urinary incontinence status ranged from 63% in Eretria (72) to 100% in Liberia (46) and Nigeria (50). The pooled estimated rate of successful closure of VVF with unknown incontinence status from 55 articles is 86.31% (95% CI: 84.21–88.42) (Figure 4). The funnel plot is available in Supplementary Figure S4.
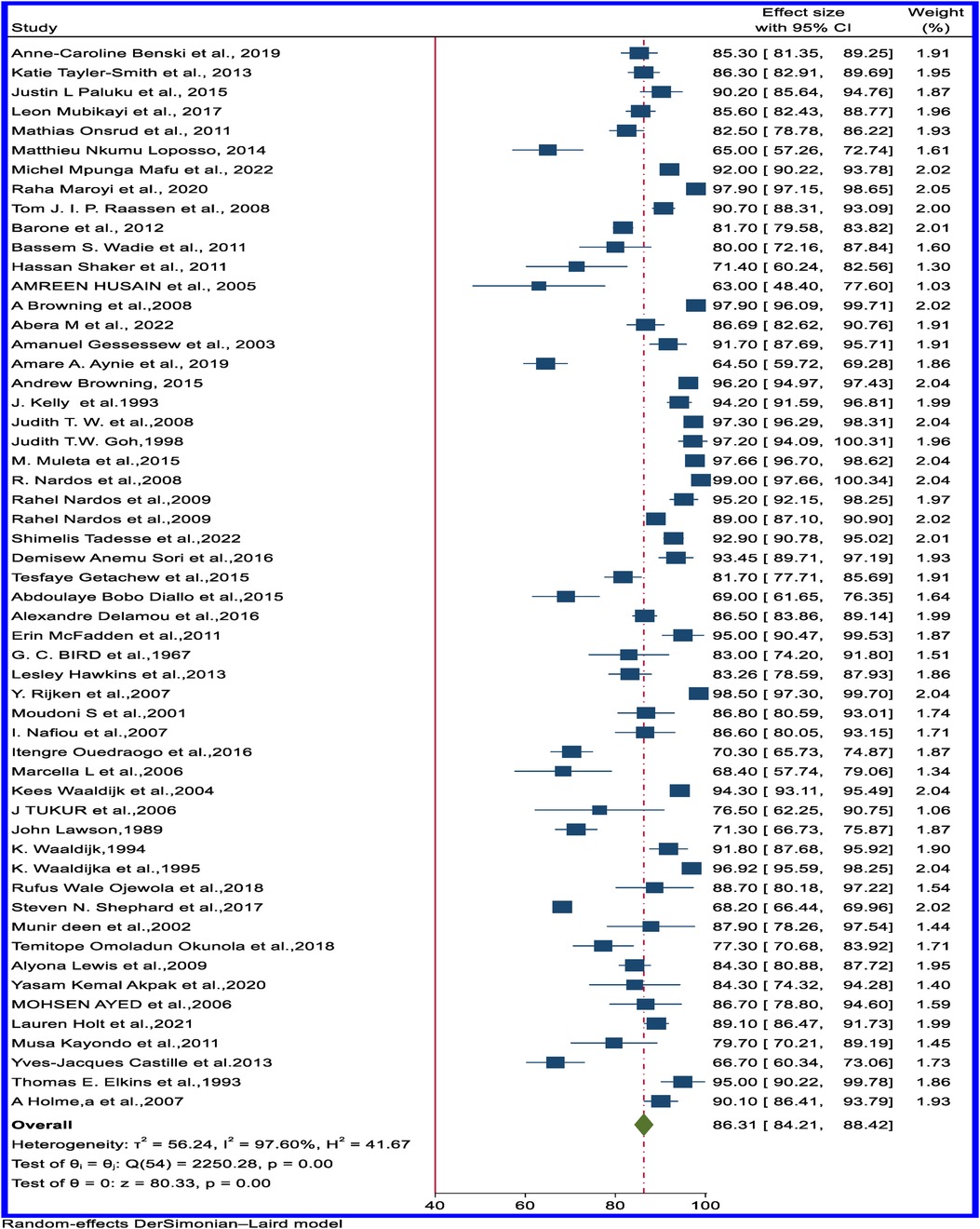
Figure 4. Forest plot of the pooled rate of successful surgical closure of obstetric VVF with unknown status of incontinence in Africa.
In sub-regional analysis, the successful surgical closure rate of VVF with unknown incontinence status was highest, at 90.05% (95%CI: 87.84–92.25), in East Africa and lowest, at 81.60% (95%CI: 75.89–87.31), in West Africa (Table 1). The forest plot of the pooled successful closure rate for VVF with unknown incontinence status based on the sub-regional distribution is available in Supplementary Figure S5.
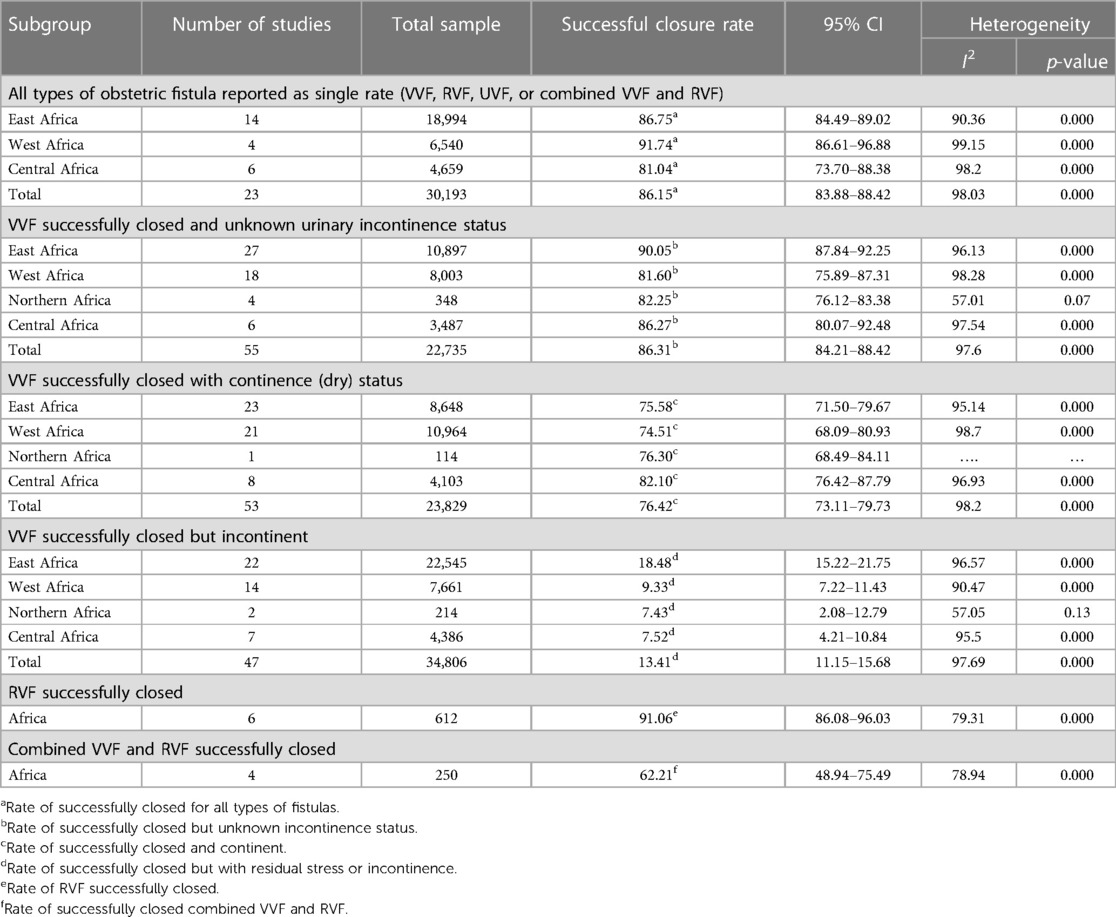
Table 1. Sub-group analysis of the successful surgical closure of obstetric fistula in Africa, 1953-2023.
Rate of successful surgical closure of VVF based on incontinence/continence outcome
Successful surgeries resulting in continence (dry) ranged from 45% in Ethiopia (79) to 100% in Nigeria (50). The pooled estimated rate of VVF successfully closed and dry from 53 articles was 76.07% (95% CI: 72.68–79.46) (Figure 5). Supplementary Figures S6 and S7 contain the funnel plot figures for VVF successfully closed and dry and VVF successfully closed but with stress or residual incontinence (wet). Sub-regional analysis showed relatively comparable results across the regions (Table 1).
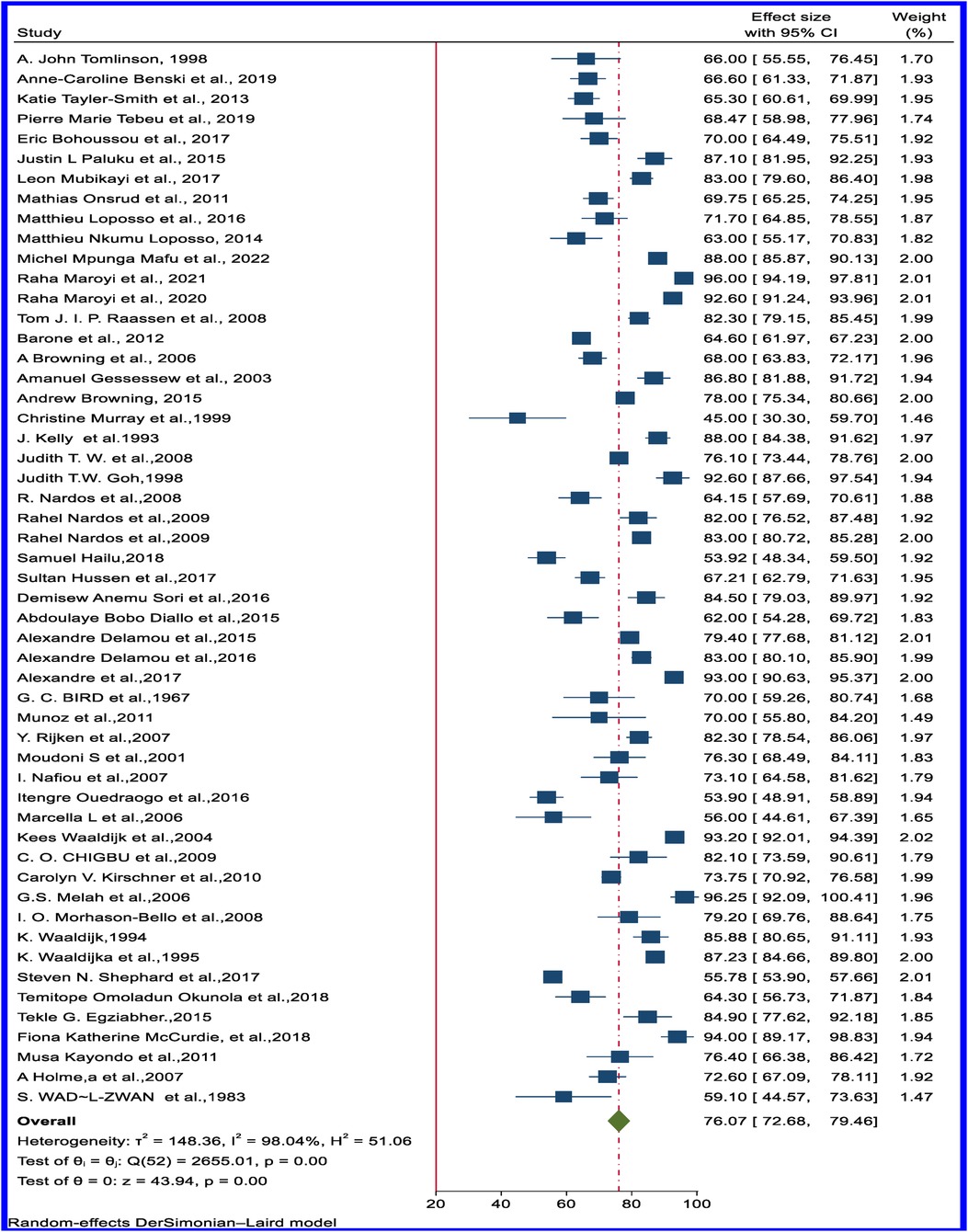
Figure 5. Forest plot of the pooled rate of successfully closed and continent (dry) obstetrics VVF in Africa.
Moreover, the pooled estimated rate of VVFs that are closed but have stress or residual incontinence (wet) from 45 articles revealed 13.41% (95% CI: 11.15–15.68) (Figure 6). Sub-regional analysis results show a large variation across the regions: the highest residual stress or incontinence despite successful closure was observed in East Africa, at 18.48% (95% CI: 15.22–21.75), and the lowest was observed in Northern Africa, at 7.43% (95% CI: 2.08−12.79) (Table 1). Supplementary Figures S8 and S9 show the forest plot of the pooled rate of VVF successfully closed and dry and VVF successfully closed but wet based on the sub-regional distribution.
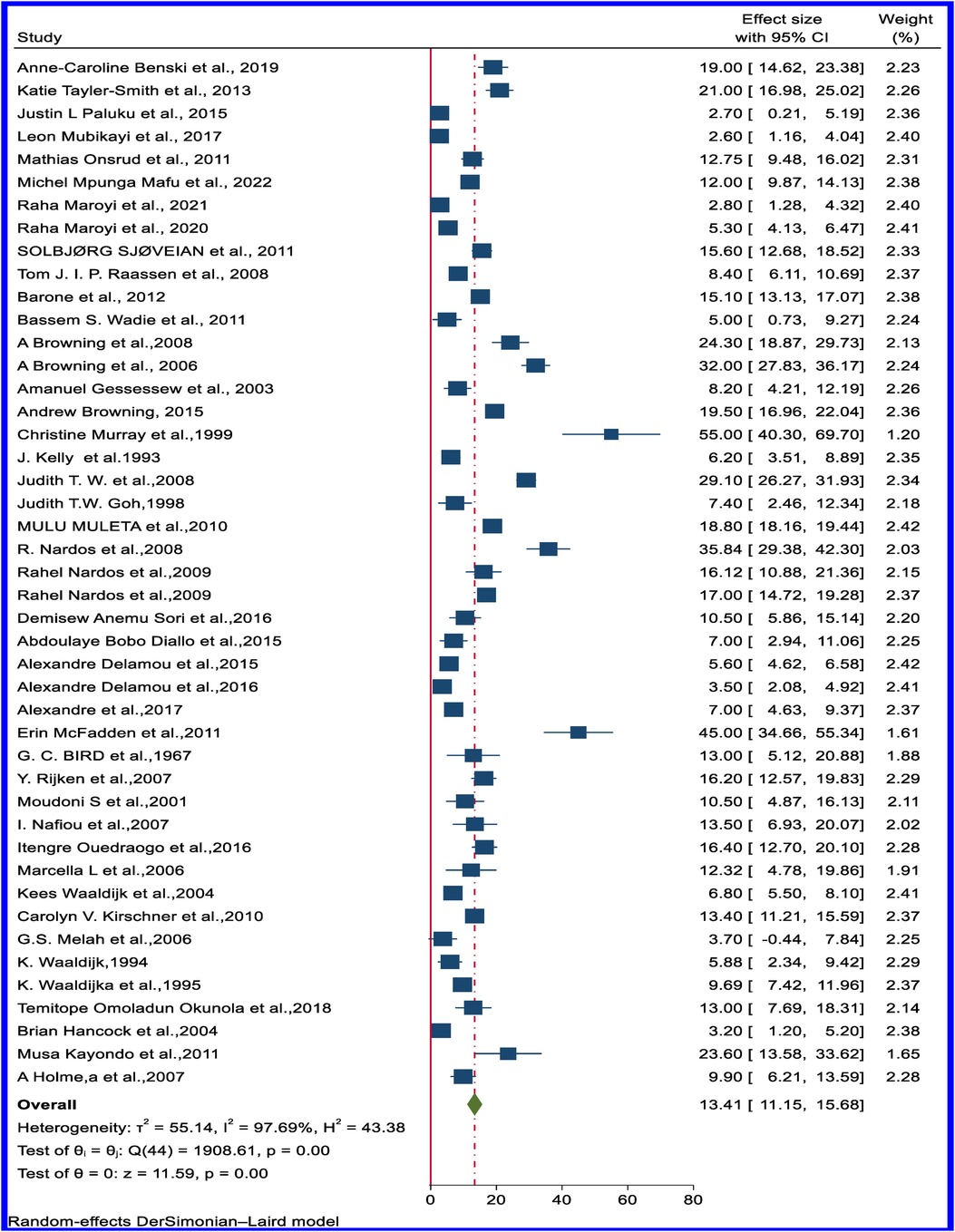
Figure 6. Forest plot of the pooled rate of successfully closed but incontinent (wet) of obstetric VVF in Africa.
Rate of successful surgical closure of rectovaginal fistula and combined RVF and VVF
In all reviewed articles, the success rate for surgical closure of RVF was above 80%, and in five studies, it was 100%. Six studies provided a pooled estimated rate of the successful closure of RVF of 91.06% (95% CI: 86.08–96.03) (Figure 7). From five articles, the overall successful closure rate of combined VVF and RVF was 62.21% (95% CI: 48.94–75.49) (Figure 8). Supplementary Figures S10 and S11 contain the funnel plot figures for the successful closure of RVF and combined VVF and RVF, respectively.
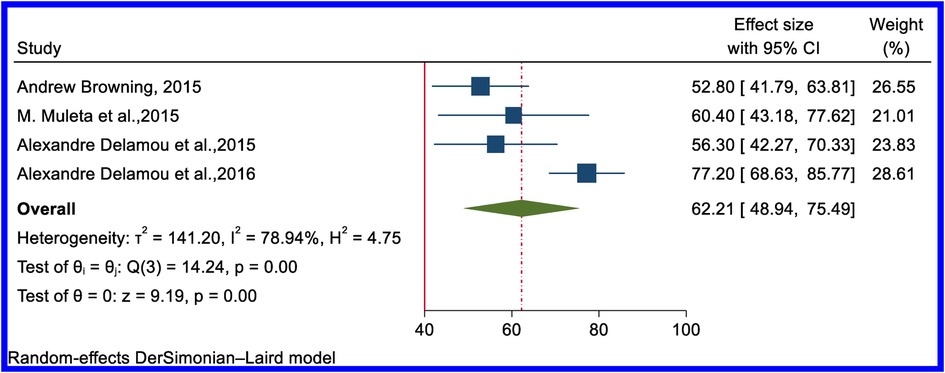
Figure 8. Forest plot of the pooled rate of successful surgical closure of obstetric combined RVF and VVF in Africa.
Discussion
Obstetric fistula is still a public health concern in Africa. However, the public and medical community remain largely unaware of this problem (6). Obstetric fistula closure rate reports across healthcare settings of African countries are varied. Therefore, this systematic review and meta-analysis were conducted to estimate the pooled successful surgical closure rate for different types of obstetric fistulas in Africa.
Our results show that the pooled estimated rate of successful closure of VVF with unknown incontinence status is 86.31% (95% CI: 84.21–88.42). The pooled estimated rate of successfully closed VVF and continent (dry) is 76.07% (95% CI: 72.68–79.46). The pooled estimated rate of successfully closed VVF but with ongoing or residual incontinence (wet) is 13.41% (95% CI: 11.15–15.68). Despite the high rate of successful closure, a significant number of women are faced with ongoing or residual incontinence. This might be because a large number of women live with a fistula for several years before seeking medical assistance, and this might affect the successful surgical closure of obstetric fistulas in the region (69).
In line with the Nepal finding (88%), this review reported a successful surgical closure rate of VVF of 86.31% (95% CI: 84.21–88.42). The sub-regional result also showed a lower successful closure rate than Nepal's finding, except in the East African region, which had a higher success rate (90.05%). A systematic review conducted in both developed and underdeveloped countries showed the rate of successful surgical reconstruction in developed countries was >90% (10, 108). The high success rate was due to the different types of fistulas, as in these countries, small iatrogenic fistulas are more common, which are much easier to cure. Yet, a relatively comparable result was found in underdeveloped countries (10).
This review reveals that the Northern Africa sub-region has a lower success rate (82.25%) than the WHO recommendation, whereas, the East, West, and Central African sub-regions have success rates comparable to or higher than the recommendation. This might be because the studies conducted in Northern Africa were from 1983 to 2011 and had small sample sizes.
The transvaginal route of surgical closure is preferred as it has low morbidity, higher success rates, and minimal complications. Nevertheless, transabdominal VVF closure in correctly chosen individuals yields satisfactory treatment outcomes (109, 110). Moreover, to increase the success rate of closure using a combined abdominovaginal approach with the use of a generous rotational bladder flap for closure of a complex vesicovaginal fistula is vital. Additionally, due to the excellent exposure and healthy, well-vascularized tissue, giant vesicovaginal fistulas have a high success rate on the first attempt (111). Thus, fistula surgeons must consider the best method of closure for complicated fistulas as the first attempt is vital for the success of surgical fistula closure. Moreover, for women who initially present with incontinence, physiotherapy, pelvic floor training, and abdominal wall control are crucial steps to take before surgery (66). Although there isn't enough evidence to support it, encouraged to continue exercise improvement were noted in residual stress incontinence (112).
According to our review, combined VVF and RVF have a lower surgical closure rate than other types of fistulas. Because a combined fistula is indicative of more severe and extensive injuries and more scarring, patients are more likely to have a circumferential VVF, which has worse outcomes. A trial investigation also demonstrated that the use of fibrin glue as an interposition layer during the complex VVF vaginal anatomical closure appears as an alternative to the use of Martius flap interposition (113). Fibrin glue is a valuable resource that can improve the outcome of the closure of VVFs and decrease the time and complexity of the procedure (114). Lastly, difficult and complicated fistulas, experienced surgeons, the establishment of separate fistula surgery units, and appropriate care and expertise are important factors in achieving the desired results (115).
As a limitation, the literature included in this review has a lack of consistency in assessment methods used to investigate obstetric fistula closure and continence rate. In addition, differences in the study population and setting among the included studies might influence the results of this review. Furthermore, the scope of this review was restricted to English-language literature on obstetric fistula. Future review studies that explain factors affecting the successful surgical closure of obstetric fistulas are vital.
Conclusions and recommendations
Though there is a high rate of successful obstetric fistula closure in Africa, significant numbers of women face residual or ongoing incontinence. Furthermore, the successful surgical closure rate of combined VVF and RVF was found to be considerably below the WHO recommendation.
In Africa, a comprehensive package of fistula care using a dedicated fistula facility or a mobile surgical outreach program might address the problem. Additionally, increased access to timely, quality fistula treatment and comprehensive post-operative care for women with fistulas in Africa is vital to achieving high success rates and lower residual incontinence. Furthermore, wide-scale network-based treatment of fistulas has improved awareness, reduced stigma, increased access to surgery, strengthened the fistula workforce, and facilitated post-operative follow-up and reintegration support for women. This integrated approach is an effective and replicable model for building capacity to deliver comprehensive fistula care services in countries where the burden of fistula is high and success rates are low (116). In such cases, women with fistulas might have access to early treatment and repeat trials for failed surgical closure. Repeat trials have the potential to achieve successful surgical closure (69, 102) and might, therefore, help improve the overall rate of satisfactory surgical closure of obstetric fistula in Africa.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
HK, MA, AA, EM, TH, and LT conducted the search and data extraction. Additionally, HK, LT, and MA wrote the first draft of the manuscript. Lastly, LT and HK conducted the statistical analyses and data interpretation and wrote the final draft. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2023.1188809/full#supplementary-material
The supplementary material consists of separate figures showing funnel plots of publication bias tests among the studies conducted on successful surgical closure of overall obstetric fistula, VVF, RVF, VVF successfully closed and incontinent (wet), VVF successfully closed but continent (dry) obstetric VVF, and combined VVF and RVF obstetric fistula. Additionally, figures showing forest plots of the pooled rate of successful surgical closure of obstetric fistulas based on sub-regional distribution for all types of fistulas are presented in the supplementary material. Furthermore, trim and fill analysis of studies conducted on successful surgical closure of overall obstetric fistula is available in the supplementary material.
Abbreviations
CI, Confidence interval; RVF, Recto-vaginal fistula; UVF, Uretero-vaginal fistula; VVF, Vesico-vaginal fistula; VUF, Vesico-uterine fistula, WHO, World Health Organization.
References
1. Sayegh AS, Medina LG, Sotelo R. Vesicovaginal fistula: Minimally invasive surgery (MIS) approaches. In: Urinary fistula. Cham: Springer International Publishing (2023). p. 125–38.
3. Roush KM. Social implications of obstetric fistula: an integrative review. J Midwifery Women’s Health. (2009) 54(2):e21–33. doi: 10.1016/j.jmwh.2008.09.005
4. Baker Z, Bellows B, Bach R, Warren C. Barriers to obstetric fistula treatment in low-income countries: a systematic review. Trop Med Int Health. (2017) 22(8):938–59. doi: 10.1111/tmi.12893
6. Wall LL. Obstetric vesicovaginal fistula as an international public-health problem. Lancet. (2006) 368(9542):1201–9. doi: 10.1016/S0140-6736(06)69476-2
8. Goh J, Krause HG. Classification of female genital tract fistulas. In: Drew LB, Ruder B, Schwartz DA, editors. A Multidisciplinary Approach to Obstetric Fistula in Africa. Global Maternal and Child Health. Cham: Springer (2022). p. 227–37.
9. Børseth KF, Acharya G, Kiserud T, Trovik J. Incidence of gynecological fistula and its surgical treatment: a national registry-based study. Acta Obstet Gynecol Scand. (2019) 98(9):1120–6. doi: 10.1111/aogs.13611
10. Hillary CJ, Osman NI, Hilton P, Chapple CR. The aetiology, treatment, and outcome of urogenital fistulae managed in well-and low-resourced countries: a systematic review. Eur Urol. (2016) 70(3):478–92. doi: 10.1016/j.eururo.2016.02.015
11. Baba SB. Birth and sorrow: the psycho-social and medical consequences of obstetric fistula. Int J Medical Sociol Anthropol. (2014) 2(2):055–65.
12. Bashah DT, Worku AG, Mengistu MY. Consequences of obstetric fistula in sub Sahara African countries, from patients’ perspective: a systematic review of qualitative studies. BMC Women’s Health. (2018) 18(1):1–12. doi: 10.1186/s12905-018-0605-1
13. Mafu MM, Banze DFK, Aussak BTT, Kolié D, Camara BS, Nembunzu D, et al. Factors associated with surgical repair success of female genital fistula in the democratic Republic of Congo: experiences of the fistula care plus project, 2017–2019. Trop Med Int Health. (2022) 27(9):831–9. doi: 10.1111/tmi.13794
14. Noori IF. Rectovaginal fistulas, outcomes of various surgical repair and predictive factors of healing success. A retrospective cohort study of 40 cases. Int J Surg Open. (2021) 32:100335. doi: 10.1016/j.ijso.2021.100335
15. Lewis G, De Bernis L. Obstetric fistula: guiding principles for clinical management and programme development. World Health Organization (2006).
16. Bernard L, Giles A, Fabiano S, Giles S, Hudgins S, Olson A, et al. Predictors of obstetric fistula repair outcomes in Lubango, Angola. J Obstet Gynaecol Can. (2019) 41(12):1726–33. doi: 10.1016/j.jogc.2019.01.025
17. Nardos R, Jacobson L, Garg B, Wall LL, Emasu A, Ruder B. Characterizing persistent urinary incontinence after successful fistula closure: the Uganda experience. Am J Obstet Gynecol. (2022) 227(1):70.e1–e9. doi: 10.1016/j.ajog.2022.03.008
18. Ryoo S-B, Oh H-K, Ha H-K, Han EC, Kwon Y-H, Song I, et al. Outcomes of surgical treatments for rectovaginal fistula and prognostic factors for successful closure: a single-center tertiary hospital experiences. Ann Surg Treat Res. (2019) 97(3):149–56. doi: 10.4174/astr.2019.97.3.149
19. Kayondo M, Wasswa S, Kabakyenga J, Mukiibi N, Senkungu J, Stenson A, et al. Predictors and outcome of surgical repair of obstetric fistula at a regional referral hospital, Mbarara, western Uganda. BMC Urol. (2011) 11(1):1–9. doi: 10.1186/1471-2490-11-23
20. Bengtson AM, Kopp D, Tang JH, Chipungu E, Moyo M, Wilkinson J. Identifying patients with vesicovaginal fistula at high risk of urinary incontinence after surgery. Obstet Gynecol. (2016) 128(5):945. doi: 10.1097/AOG.0000000000001687
21. Aromataris E, Munn Z. Joanna briggs institute reviewer’s manual. The Joanna Briggs Institute. (2017, 2018).
22. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. (2003) 327(7414):557–60. doi: 10.1136/bmj.327.7414.557
23. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994):1088–101. doi: 10.2307/2533446
24. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. (1997) 315(7109):629–34. doi: 10.1136/bmj.315.7109.629
25. Duval S, Tweedie R. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc. (2000) 95(449):89–98. doi: 10.1080/01621459.2000.10473905
26. Wadie BS, Kamal MM. Repair of vesicovaginal fistula: single-centre experience and analysis of outcome predictors. Arab J Urol. (2011) 9(2):135–8. doi: 10.1016/j.aju.2011.06.005
27. Shaker H, Saafan A, Yassin M, Idrissa A, Mourad MS. Obstetric vesico-vaginal fistula repair: should we trim the fistula edges? A randomized prospective study. Neurourol Urodyn. (2011) 30(3):302–5. doi: 10.1002/nau.20995
28. Ayed M, Atat RE, Hassine LB, Sfaxi M, Chebil M, Zmerli S. Prognostic factors of recurrence after vesicovaginal fistula repair. Int J Urol. (2006) 13(4):345–9. doi: 10.1111/j.1442-2042.2006.01308.x
29. Moudouni S, Nouri M, Koutani A, Attya I, Hachimi M, Lakrissa A. Obstetrical vesico-vaginal fistula. Report of 114 cases. Prog Urol. (2001) 11(1):103–8.11296628
30. Sjøveian S, Vangen S, Mukwege D, Onsrud M. Surgical outcome of obstetric fistula: a retrospective analysis of 595 patients. Acta Obstet Gynecol Scand. (2011) 90(7):753–60. doi: 10.1111/j.1600-0412.2011.01162.x
31. Loposso M, Hakim L, Ndundu J, Lufuma S, Punga A, De Ridder D. Predictors of recurrence and successful treatment following obstetric fistula surgery. Urology. (2016) 97:80–5. doi: 10.1016/j.urology.2016.03.079
32. Paluku JL, Carter TE. Obstetric vesico-vaginal fistulae seen in the northern democratic Republic of Congo: a descriptive study. Afr Health Sci. (2015) 15(4):1104–11. doi: 10.4314/ahs.v15i4.8
33. Loposso MN, Ndundu J, De Win G, Ost D, Punga AM, De Ridder D. Obstetric fistula in a district hospital in DR Congo: fistula still occur despite access to caesarean section. Neurourol Urodyn. (2015) 34(5):434–7. doi: 10.1002/nau.22601
34. Maroyi R, Keyser L, Hosterman L, Notia A, Mukwege D. The mobile surgical outreach program for management of patients with genital fistula in the democratic Republic of Congo. Int J Gynaecol Obstet. (2020) 148:27–32. doi: 10.1002/ijgo.13036
35. Mubikayi L, Matson DO, Lokomba V, Mboloko J, Kamba JP, Tozin R. Determinants of outcomes and prognosis score in obstetric vesico-vaginal fistula repair. Open J Obstet Gynecol. (2017) 7(07):767. doi: 10.4236/ojog.2017.77078
36. Maroyi R, Shahid U, Vangaveti V, Rane A, Mukwege D. Obstetric vesico-vaginal fistulas: midvaginal and juxtacervical fistula repair outcomes in the democratic Republic of Congo. Int J Gynaecol Obstet. (2021) 153(2):294–9. doi: 10.1002/ijgo.13472
37. Onsrud M, Sjøveian S, Mukwege D. Cesarean delivery-related fistulae in the democratic Republic of Congo. Int J Gynaecol Obstet. (2011) 114(1):10–4. doi: 10.1016/j.ijgo.2011.01.018
38. Benski AC, Delavy M, Rochat CH, Viviano M, Catarino R, Elsig V, et al. Prognostic factors and long-term outcomes of obstetric fistula care using the tanguiéta model. Int J Gynaecol Obstet. (2020) 148(3):331–7. doi: 10.1002/ijgo.13071
39. Tebeu Marie P, Ekono M, Noa Ndoua C, Meutchi G, Mawamba Y, Rochat C. Surgical outcome of genito-urinary obstetric fistulas (GUOF) with or without bladder neck involvement: an experience from the university teaching hospital, Yaoundé, Cameroon. Obstet Gynecol Int J. 2019;10(3):223–8. doi: 10.15406/ogij.2019.10.00447
40. Tomlinson AJ, Thornton JG. A randomised controlled trial of antibiotic prophylaxis for vesico-vaginal fistula repair. Br J Obstet Gynaecol. (1998) 105(4):397–9. doi: 10.1111/j.1471-0528.1998.tb10122.x
41. Bohoussou E, Dia JM, Okon G, Djanhan L, Kouamé B, Djanhan Y, et al. Results of the management of urogenital fistulae from community caravans. Open J Obstet Gynecol. (2017) 7(08):858. doi: 10.4236/ojog.2017.78086
42. Diallo AB, Diallo TMO, Bah I, Bah MD, Kanté D, Bah OR, et al. Vesicovaginal fistulas: anatomical clinical and surgical aspects in the Conakry university hospital center. Open J Urol. (2015) 5(12):224. doi: 10.4236/oju.2015.512036
43. Delamou A, Diallo M, Beavogui AH, Delvaux T, Millimono S, Kourouma M, et al. Good clinical outcomes from a 7-year holistic programme of fistula repair in Guinea. Trop Med Int Health. (2015) 20(6):813–9. doi: 10.1111/tmi.12489
44. Delamou A, Delvaux T, Beavogui AH, Toure A, Kolié D, Sidibé S, et al. Factors associated with the failure of obstetric fistula repair in Guinea: implications for practice. Reprod Health. (2016) 13(1):1–9. doi: 10.1186/s12978-016-0248-3
45. Delamou A, Delvaux T, El Ayadi AM, Tripathi V, Camara BS, Beavogui AH, et al. Fistula recurrence, pregnancy, and childbirth following successful closure of female genital fistula in Guinea: a longitudinal study. Lancet Glob Health. (2017) 5(11):e1152–e60. doi: 10.1016/S2214-109X(17)30366-2
46. Munoz O, Bowling CB, Gerten KA, Taryor R, Norman AM, Szychowski JM, et al. Factors influencing post-operative short-term outcomes of vesicovaginal fistula repairs in a community hospital in Liberia. Br J Med Surg Urol. (2011) 4(6):259–65. doi: 10.1016/j.bjmsu.2011.02.001
47. Nafiou I, Idrissa A, Ghaichatou A, Roenneburg M, Wheeless C, Genadry RR. Obstetric vesico-vaginal fistulas at the national hospital of Niamey, Niger. Int J Gynaecol Obstet. (2007) 99:S71–S4. doi: 10.1016/j.ijgo.2007.06.012
48. Roenneburg ML, Genadry R, Wheeless CR Jr. Repair of obstetric vesicovaginal fistulas in Africa. Am J Obstet Gynecol. (2006) 195(6):1748–52. doi: 10.1016/j.ajog.2006.07.031
49. Ouedraogo I, Payne C, Nardos R, Adelman AJ, Wall LL. Obstetric fistula in Niger: 6-month postoperative follow-up of 384 patients from the Danja fistula center. Int Urogynecol J. (2018) 29:345–51. doi: 10.1007/s00192-017-3375-7
50. Umoiyoho AJ, Inyang-Etoh EC, Etukumana EA. Obstetric fistula repair: experience with hospital-based outreach approach in Nigeria. Glob J Health Sci. (2012) 4(5):40. doi: 10.5539/gjhs.v4n5p40
51. Morhason-Bello I, Ojengbede O, Adedokun B, Okunlola M, Oladokun A. Umcomplicated midvaginal vesico-vaginal fistula repair in Ibadan: a comparison of the abdominal and vaginal routes. Ann Ib Postgrad Med. (2008) 6(2):39–43. doi: 10.4314/aipm.v6i2.64051
52. Waaldijk K. The immediate management of fresh obstetric fistulas. Am J Obstet Gynecol. (2004) 191(3):795–9. doi: 10.1016/j.ajog.2004.02.020
53. Waaldijk K. The immediate surgical management of fresh obstetric fistulas with catheter and/or early closure. Int J Gynaecol Obstet. (1994) 45(1):11–6. doi: 10.1016/0020-7292(94)90759-5
54. Melah G, El-Nafaty A, Bukar M. Early versus late closure of vesicovaginal fistulas. Int J Gynaecol Obstet. (2006) 93(3):252–3. doi: 10.1016/j.ijgo.2006.02.017
55. Chigbu C, Nwogu-Ikojo E, Onah H, Iloabachie G. Juxtacervical vesicovaginal fistulae: outcome by route of repair. J Obstet Gynaecol. (2006) 26(8):795–7. doi: 10.1080/01443610600984651
56. Munir-deen AI, Aboyeji AP, Ijaiya ZB. Epidemiology of vesico-vaginal fistula at the university of Ilorin teaching hospital, Ilorin, Nigeria. Trop J Obstet Gynaecol. (2002) 19(2):101–3.
57. Kirschner CV, Yost KJ, Du H, Karshima JA, Arrowsmith SD, Wall LL. Obstetric fistula: the ECWA evangel VVF center surgical experience from Jos, Nigeria. Int Urogynecol J. (2010) 21:1525–33. doi: 10.1007/s00192-010-1231-0
58. Ojewola W, Tijani K, Jeje E, Ogunjimi M. Transabdominal repair of vesicovaginal fistulae: a 10-year tertiary care hospital experience in Nigeria. (2018).
59. Hilton P, Ward A. Epidemiological and surgical aspects of urogenital fistulae: a review of 25 years’ experience in southeast Nigeria. Int Urogynecol J. (1998) 9:189–94. doi: 10.1007/BF01901602
60. Waaldijk K. Surgical classification of obstetric fistulas. Int J Gynaecol Obstet. (1995) 49(2):161–3. doi: 10.1016/0020-7292(95)02350-L
61. Okunola TO, Yakubu E, Daniyan B, Ekwedigwe K, Eliboh M, Sunday-Adeoye I. Profile and outcome of patients with recurrent urogenital fistula in a fistula centre in Nigeria. Int Urogynecol J. (2019) 30:197–201. doi: 10.1007/s00192-018-3738-8
62. Arrowsmith SD. Genitourinary reconstruction in obstetric fistulas. J Urol. (1994) 152(2):403–6. doi: 10.1016/S0022-5347(17)32749-0
63. Tukur J, Jido T, Uzoho C. The contribution of Gishiri cut to vesicovaginal fistula in Birnin Kudu, northern Nigeria. Afr J Urol. (2006) 12(3):121–5.
64. Lawson J. Tropical obstetrics and gynaecology. 3. Vesico-vaginal fistula—a tropical disease. Trans R Soc Trop Med Hyg. (1989) 83(4):454–6. doi: 10.1016/0035-9203(89)90244-7
65. Lewis A, Kaufman MR, Wolter CE, Phillips SE, Maggi D, Condry L, et al. Genitourinary fistula experience in Sierra Leone: review of 505 cases. J Urol. (2009) 181(4):1725–31. doi: 10.1016/j.juro.2008.11.106
66. Castille Y-J, Avocetien C, Zaongo D, Colas J-M, Peabody JO, Rochat C-H. Impact of a program of physiotherapy and health education on the outcome of obstetric fistula surgery. Int J Gynaecol Obstet. (2014) 124(1):77–80. doi: 10.1016/j.ijgo.2013.06.032
67. Elkins TE. Surgery for the obstetric vesicovaginal fistula: a review of 100 operations in 82 patients. Am J Obstet Gynecol. (1994) 170(4):1108–20. doi: 10.1016/S0002-9378(94)70105-9
68. Shephard SN, Lengmang SJ, Anzaku SA, Mamven OV, Kirschner CV. Effect of HIV infection on outcomes after surgical repair of genital fistula. Int J Gynaecol Obstet. (2017) 138(3):293–8. doi: 10.1002/ijgo.12233
69. Tayler-Smith K, Zachariah R, Manzi M, van den Boogaard W, Vandeborne A, Bishinga A, et al. Obstetric fistula in Burundi: a comprehensive approach to managing women with this neglected disease. BMC Pregnancy Childbirth. (2013) 13(1):1–8. doi: 10.1186/1471-2393-13-164
70. Raassen TJ, Verdaasdonk EG, Vierhout ME. Prospective results after first-time surgery for obstetric fistulas in east African women. Int Urogynecol J. (2008) 19:73–9. doi: 10.1007/s00192-007-0389-6
71. Barone MA, Frajzyngier V, Ruminjo J, Asiimwe F, Barry TH, Bello A, et al. Determinants of postoperative outcomes of female genital fistula repair surgery. Obstet Gynecol. (2012) 120(3):524. doi: 10.1097/AOG.0b013e31826579e8
72. Husain A, Johnson K, Glowacki CA, Osias J, Wheeless CR Jr, Asrat K, et al. Surgical management of complex obstetric fistula in Eritrea. J Women’s Health. 2005;14(9):839–44. doi: 10.1089/jwh.2005.14.839
73. Browning A. Risk factors for developing residual urinary incontinence after obstetric fistula repair. BJOG. (2006) 113(4):482–5. doi: 10.1111/j.1471-0528.2006.00875.x
74. Browning A, Menber B. Women with obstetric fistula in Ethiopia: a 6-month follow up after surgical treatment. BJOG. (2008) 115(12):1564–9. doi: 10.1111/j.1471-0528.2008.01900.x
75. Gessessew A, Mesfin M. Genitourinary and rectovaginal fistulae in Adigrat zonal hospital, Tigray, north Ethiopia. Ethiop Med J. (2003) 41(2):123–30.15227971
76. Holt L, Potluri T, Tanner JP, Duffy S, Wasingya L, Greene K. Risk factors for early and late failures following repair of urogenital fistulas. Int Urogynecol J. (2021):1–10.
77. Aynie AA, Yihunie AG, Munae AM. Magnitude of repair failure and associated factors among women undergone obstetric fistula repair in Bahir Dar Hamlin Fistula Center, Amhara Region, Northwest Ethiopia. (2019).
78. Browning A, Whiteside S. Characteristics, management, and outcomes of repair of rectovaginal fistula among 1,100 consecutive cases of female genital tract fistula in Ethiopia. Int J Gynaecol Obstet. (2015) 131(1):70–3. doi: 10.1016/j.ijgo.2015.05.012
79. Murray C, Goh JT, Fynes M, Carey MP. Urinary and faecal incontinence following delayed primary repair of obstetric genital fistula. BJOG. (2002) 109(7):828–32. doi: 10.1111/j.1471-0528.2002.00124.x
80. Kelly J, Kwast B. Epidemiologic study of vesicovaginal fistulas in Ethiopia. Int Urogynecol J. (1993) 4:278–81. doi: 10.1007/BF00372737
81. Goh JT. Genital tract fistula repair on 116 women. Aust N Z J Obstet Gynaecol. (1998) 38(2):158–61. doi: 10.1111/j.1479-828X.1998.tb02991.x
82. Goh JT, Browning A, Berhan B, Chang A. Predicting the risk of failure of closure of obstetric fistula and residual urinary incontinence using a classification system. Int Urogynecol J. (2008) 19:1659–62. doi: 10.1007/s00192-008-0693-9
83. Yismaw L, Alemu K, Addis A, Alene M. Time to recovery from obstetric fistula and determinants in Gondar university teaching and referral hospital, northwest Ethiopia. BMC women’s Health. (2019) 19(1):1–8. doi: 10.1186/s12905-018-0700-3
84. Muleta M. Obstetric fistulae: a retrospective study of 1210 cases at the Addis Ababa Fistula hospital. J Obstet Gynaecol. (1997) 17(1):68–70. doi: 10.1080/01443619750114194
85. Demissie MW. Determinants and heterogeneity of time-to-recovery from obstetric fistula patients; comparison of acceleration failure time and parametric shared frailty models. Int J Stat Probab. (2017) 7(1):99. doi: 10.5539/ijsp.v7n1p99
86. Muleta M, Rasmussen S, Kiserud T. Obstetric fistula in 14,928 Ethiopian women. Acta Obstet Gynecol Scand. (2010) 89(7):945–51. doi: 10.3109/00016341003801698
87. Nardos R, Browning A, Member B. Duration of bladder catheterization after surgery for obstetric fistula. Int J Gynaecol Obstet. (2008) 103(1):30–2. doi: 10.1016/j.ijgo.2008.05.021
88. Nardos R, Browning A, Chen CCG. Risk factors that predict failure after vaginal repair of obstetric vesicovaginal fistulae. Am J Obstet Gynecol. (2009) 200(5):578.e1–e4. doi: 10.1016/j.ajog.2008.12.008
89. Hailu S. Predictors of time to recovery from a surgical repair of obstetric fistula at Mekelle Hamlin Fistula Center, Tigray, Ethiopia. J Pregnancy Child Heal. (2018) 5(01):1–8.
90. Tadesse S, Ejigu N, Edosa D, Ashegu T, Dulla D. Obstetric fistula repair failure and its associated factors among women underwent repair in Yirgalem Hamlin Fistula Center, Sidama regional state, southern Ethiopia, 2021: a retrospective cross sectional study. BMC Women’s Health. (2022) 22(1):1–11. doi: 10.1186/s12905-022-01866-z
91. Hussen S, Melese E. Time-to-recovery from obstetric fistula and associated factors: the case of Harar Hamlin Fistula Center. Ethiop J Health Dev. (2017) 31(2):85–96.
92. Ambese TY, Gebre H, Berhe A, Fisseha G, Gufue ZH, Hailu NA, et al. Effect of vaginal scarring on the recovery of surgical repair of obstetric fistula in northern Ethiopia. Int J Gynaecol Obstet. (2023) 160(3):915–25. doi: 10.1002/ijgo.14425
93. Sori DA, Azale AW, Gemeda DH. Characteristics and repair outcome of patients with vesicovaginal fistula managed in Jimma University Teaching Hospital, Ethiopia. BMC Urol. (2016) 16:1–6. doi: 10.1186/s12894-016-0120-3
94. Getachew T, Taye A, Jabessa S. Survival analysis of time to recovery from obstetric fistula: a case study at Yirgalem Hamlin Fistula Hospital, Ethiopia. J Biom Biostat. (2015) 6(3):1. doi: 10.4172/2155-6180.1000242
95. McFadden E, Taleski SJ, Bocking A, Spitzer RF, Mabeya H. Retrospective review of predisposing factors and surgical outcomes in obstetric fistula patients at a single teaching hospital in western Kenya. J Obstet Gynaecol Can. (2011) 33(1):30–5. doi: 10.1016/S1701-2163(16)34769-7
96. Hawkins L, Spitzer RF, Christoffersen-Deb A, Leah J, Mabeya H. Characteristics and surgical success of patients presenting for repair of obstetric fistula in western Kenya. Int J Gynaecol Obstet. (2013) 120(2):178–82. doi: 10.1016/j.ijgo.2012.08.014
97. Bird G. Osbtetric vesico-vaginal and allied fistulae: a report on 70 cases. BJOG. (1967) 74(5):749–52. doi: 10.1111/j.1471-0528.1967.tb03791.x
98. Rijken Y, Chilopora G. Urogenital and recto-vaginal fistulas in southern Malawi: a report on 407 patients. Int J Gynaecol Obstet. (2007) 99:S85–S9. doi: 10.1016/j.ijgo.2007.06.015
99. Egziabher TG, Eugene N, Ben K, Fredrick K. Obstetric fistula management and predictors of successful closure among women attending a public tertiary hospital in Rwanda: a retrospective review of records. BMC Res Notes. (2015) 8(1):1–7. doi: 10.1186/s13104-015-1771-y
100. Akpak YK, Yenidede I, Kilicci C. Evaluation of etiology, characteristics, and treatment of patients with vesicovaginal fistula observed in rural Africa. J Gynecol Obstet Hum Reprod. (2021) 50(6):101879. doi: 10.1016/j.jogoh.2020.101879
101. Magali KT, Seni J, Massinde AN, Gumodoka B, Rumanyika RN. Short-term complications and associated factors among women undergoing obstetric fistula repair at Bugando Medical Centre, Mwanza, Tanzania. Ethiop Med J. (2017) 55(2).
102. Hancock B, Collie M. Vesico-vaginal fistula surgery in Uganda. East Cent Afr J Surg. (2004) 9(2):32–7.
103. McCurdie FK, Moffatt J, Jones K. Vesicovaginal fistula in Uganda. J Obstet Gynaecol. (2018) 38(6):822–7. doi: 10.1080/01443615.2017.1407301
104. Holme A, Breen M, MacArthur C. Obstetric fistulae: a study of women managed at the Monze Mission Hospital, Zambia. BJOG. (2007) 114(8):1010–7. doi: 10.1111/j.1471-0528.2007.01353.x
105. Wadhawan S, Wacha D. A review of urinary fistulae in a university teaching hospital. Int J Gynaecol Obstet. (1983) 21(5):381–5. doi: 10.1016/0020-7292(83)90005-X
106. Goh JT, Natukunda H, Singasi I, Kabugho E, Browning A, Krause HG. Surgical repair and follow-up of chronic 4th degree obstetric perineal tear (total perineal defect) in 2 centres in Eastern Africa. Int Urogynecol J. (2021) 32(9):2437–42. doi: 10.1007/s00192-021-04841-8
107. Bihon AM, Meikena HK, Serka S. Survival modeling on the determinants of time to recovery from obstetric fistula: the case of Mekelle Hamlin Fistula Center, Ethiopia. Int J Reprod Med. (2022) 2022. doi: 10.1155/2022/8313575
108. Rajamaheswari N, Bharti A, Seethalakshmi K. Vaginal repair of supratrigonal vesicovaginal fistulae—a 10-year review. Int Urogynecol J. (2012) 23:1675–8. doi: 10.1007/s00192-012-1665-7
109. Singh V, Sinha RJ, Mehrotra S, Sankhwar S, Bhatt S. Repair of vesicovaginal fistula by the transabdominal route: outcome at a north Indian tertiary hospital. Int Urogynecol J. (2012) 23:411–6. doi: 10.1007/s00192-011-1544-7
110. Rajaian S, Pragatheeswarane M, Panda A. Vesicovaginal fistula: review and recent trends. Indian J Urol. (2019) 35(4):250. doi: 10.4103/iju.IJU_147_19
111. Ezzat M, Ezzat MM, Tran VQ, Aboseif SR. Repair of giant vesicovaginal fistulas. J Urol. (2009) 181(3):1184–8. doi: 10.1016/j.juro.2008.10.152
112. Castille Y-J, Avocetien C, Zaongo D, Colas J-M, Peabody JO, Rochat C-H. One-year follow-up of women who participated in a physiotherapy and health education program before and after obstetric fistula surgery. Int J Gynaecol Obstet. (2015) 128(3):264–6. doi: 10.1016/j.ijgo.2014.09.028
113. Safan A, Shaker H, Abdelaal A, Mourad MS, Albaz M. Fibrin glue versus martius flap interpositioning in the repair of complicated obstetric vesicovaginal fistula. A prospective multi-institution randomized trial. Neurourol Urodyn. (2009) 28(5):438–41. doi: 10.1002/nau.20754
114. Spotnitz WD. Commercial fibrin sealants in surgical care. Am J Surg. (2001) 182(2):S8–S14. doi: 10.1016/S0002-9610(01)00771-1
115. Jatoi N, Jatoi NM, Shaikh F, Sirichand P. Key to successful vesico-vaginal Fistula repair-an experience of urogenital fistula surgeries and outcome at gynaecological surgical camp-2005. J Ayub Med Coll Abbottabad. (2008) 20(2):125–7.19385475
Keywords: obstetric fistula, successful surgical closure, continent rate, combined VVF and RVF, Africa
Citation: Kumsa H, Mislu E, Arage MW, Abera A, Hailu T and Tenaw LA (2023) Successful surgical closure and continence rate of obstetric fistula in Africa: systematic review and meta-analysis. Front. Glob. Womens Health 4:1188809. doi: 10.3389/fgwh.2023.1188809
Received: 20 March 2023; Accepted: 13 September 2023;
Published: 3 October 2023.
Edited by:
Getnet Gedefaw, Injibara University, EthiopiaReviewed by:
Liknaw Bewket Zeleke, Debre Markos University, EthiopiaAndrew Browning, Sydney Local Health District, Australia
Adera Debella, Haramaya University, Ethiopia
© 2023 Kumsa, Mislu, Arage, Abera, Hailu and Tenaw. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Henok Kumsa aGVub2trdW1zYUBnbWFpbC5jb20=
 Henok Kumsa
Henok Kumsa Esuyawkal Mislu1
Esuyawkal Mislu1 Mulugeta Wedaje Arage
Mulugeta Wedaje Arage Atitegeb Abera
Atitegeb Abera Tilahun Hailu
Tilahun Hailu