- 1Yaya Gulale Woreda Health Office, North Shoa, Oromia, Ethiopia
- 2School of Nursing and Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 3Department of Population and Family Health, Institute of Health, Faculty of Health Sciences, Jimma University, Jimma, Ethiopia
- 4Department of Public Health and Emergency Management, Kellam Wallaga Zonal Health Office, Dembi Dolo, Oromia, Ethiopia
- 5School of Public Health, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 6Department of Midwifery, College of Health Sciences, Salale University, Fitche, Ethiopia
Introduction: Preconception care is an important preventive intervention for adverse pregnancy outcomes. It is recognized as a strategy to optimize women's health and pregnancy outcomes in Western countries. However, preconception care is underutilized in sub-Saharan Africa, like Ethiopia, where maternal mortality is high. Evidence is scarce in the study area about the prevalence and factors associated with preconception care utilization. Therefore this study aimed to assess the proportion of preconception care utilization and associated factors among pregnant mothers in Fiche town, central Ethiopia, 2021.
Method: A community-based cross-sectional study was done from May 10 to June 25, 2021. A systematic random sample technique was used to choose 393 pregnant women for the study. A structured, pre-tested, interviewer-administered questionnaire was used to collect data. The data were entered into Epi Data version 3.1 and then exported into SPSS version 25 for analysis. A Bivariable and multivariable logistic regression analysis was used to check for the association. Odds ratio along with 95% was used to describe the association. Finally, a significant association was declared at a p-value less than 0.05.
Results: 388 respondents participated in this study, making the response rate 98.7%. Of total study participants only 84 (21.6%; 95% CI, 18, 25.8) utilized preconception care. The study found that diploma or higher level of education (AOR = 3.47, 95% CI: 1.27, 9.53), psychological and financial support from a partner (AOR = 3.86, 95% CI: 2.1, 7.10), joint discussion and plan with a partner (AOR = 3.32, 95% CI: 1.55, 7.13), history of chronic disease (AOR = 3.47, 95% CI: 1.67, 7.25), and good knowledge about preconception care (AOR = 2.42, 95% CI: 1.34, 4.38) were significantly associated with preconception care utilization.
Conclusions: Overall, less than a quarter of the pregnant mothers utilized preconception care, indicating that awareness is very low. Pregnant mothers who have a higher educational level, have good communication and support from their partners, have chronic health problems, and have good knowledge about preconception care were more likely to utilize the service. Preconception care is a better opportunity to intervene and maintain the mother in the continuum of care.
1. Introduction
Preconception care (PCC) is the provision of biomedical, behavioral, and social health interventions to women and couples before conception to enhance their health and improve pregnancy outcomes (1–3). PCC is an important preventive health care intervention before conception for a couple (4, 5). It is also cost-effective in preventing adverse pregnancy outcomes, especially for those with chronic medical disorder (6–8).
Globally, 303,000 mothers die each year from maternal causes, with one in every 180 at risk; developing regions account for 99% of maternal deaths (9). About 66% of the global maternal mortality ratio (MMR) accounts for sub-Saharan Africa alone (10). In developing countries, maternal and neonatal mortality continues to be a serious public health problem (11, 12). To ensure and enhance maternal health and reduce MMR, preconception care is essential (11, 13).
Globally, less than one-third of women of reproductive age discuss their health status and its impact on pregnancy outcomes with a health professional (11, 13, 14). Moreover, the risks to reproductive health are still unacceptably high in many countries (14).
In Western societies, PCC is well recognized as a means of enhancing a healthy pregnancy and its outcome (14). Preconception care is widely recognized as being essential to ensuring the well-being of both women and their offspring (7, 15, 16). However, in most low-income countries, including Ethiopia, maternal health care may not begin until the pregnancy is well established or until more than half of the pregnancy has passed (11, 17).
Preconception care is a strategy for achieving sustainable development goal 3 (SDG 3): reducing maternal mortality to less than 70 per 100,000 live births and newborn mortality to as few as 12 per 1,000 live births by 2030 (18).
A health extension program was in place to address this problem and link the mother and newborn to the continuum of care, especially for those in remote areas (19).
Even though bad pregnancy outcomes, like malformation, are still a public health problem, the Ethiopian government has done its best to increase coverage and access to a continuum of maternity care (20, 21). The majority of policy initiatives have focused on enhancing women's health, increasing child survival, and reducing unfavorable pregnancy outcomes; however, there is an underuse of maternal preconception care (22, 23).
At the time women became aware of their pregnancy and started antenatal care (ANC) in Ethiopia, most of the fetal organs had developed (7, 24). PCC, which is the earliest link between maternal and newborn health, provides a window of opportunity to intervene accordingly and improve this gap (16, 25).
Preconception care is a key entry point to increase other services such as antenatal care, skilled delivery, and postnatal care and reduce adverse pregnancy outcomes (2, 26). Only, little is known and there are few studies on preconception care utilization in the study area. Therefore, this study was done to determine preconception care utilization and associated factors among pregnant women in Fiche Town, central Ethiopia, in 2021.
2. Method
2.1. Design, period and setting
A community-based, cross-sectional study was conducted from 10 May to 25 June, 2021, in Fiche Town, central Ethiopia. Fiche is a town located in the central part of Ethiopia, about 120 kilometers (km) from Addis Ababa. It is in the northern Shoa Zone of the Oromia region and has four kebele (lowest administrative unit in Ethiopia). The district has a total population of 104,345 people, according to the 2021 report obtained from the town health office, with 54,981 men and 49,364 women. Women in reproductive age groups in the town were 17,129. Data obtained from the health bureau of the Fiche town administration at the time of the study indicated the presence of about 936 pregnant women in the study area.
2.2. Source and study population
All pregnant women who lived in Fiche town for 6 months and above.
2.3. Sample size and sampling procedure
The single population proportion formula was used to calculate sample size with the following assumptions: Z /2 = 1.96, 95% confidence level, p = 18.2% of women use preconception care from a previous study conducted in northern Ethiopia (27), margin of error (d) = 4%, non-response rate = 10%. Finally, 393 people were chosen as the final sample size.
Data from the Fiche town health bureau, with the support of the health extension, was used to identify the number of pregnant women. Individual study participants were chosen using a systematic random sampling technique with k values of 2 (936/393 = 2.38). The first household to be included in the study was selected by the lottery method. If more than one pregnant mother was found in a single household, the lottery method was used to select study participants.
2.4. Variables of the study
Maternal utilization of preconception care is the study's dependent variable. Socio-demographic characteristics, obstetric and gynecologic characteristics, awareness and knowledge of preconception care, partner-related factors, and health system-related aspects are all independent variables.
2.5. Operational definitions
Preconception care is a comprehensive set of interventions that should be given to reproductive-age women before pregnancy to promote a healthy pregnancy and its outcome (28).
Preconception care utilization: Women will be considered to have used PCC if they received at least one of the following components of preconception care before pregnancy: counseling, disease screening and treatment, folic acid, vaccines, changing their diet, cessation of alcohol drinking, cessation of smoking, or creating a healthy environment (advice, treatment, and lifestyle modification) (26).
Knowledge of women about PCC: Eight knowledge questions were used to measure preconception care knowledge. Those who responded correctly 50% or above to preconception care knowledge questions were considered to have good knowledge, while those who scored less than 50% of correct responses were considered to have poor knowledge (29).
History of adverse pregnancy outcome: Previous pregnancy that ended in any of the following: preterm, low birth weight, abortion, stillbirth/intrauterine fetal death, birth defect (30).
2.6. Data collection instrument
A face-to-face interview was used to collect data using a pre-tested structured questionnaire. The tool consists of different parts that were developed from reviewing different literature and modified according to the local context (21, 31–33). Four bachelor's degree-holding nurses were used as data collectors and supervised by two MSC-holding nurses. During the data collection, regular supportive supervision and discussions with data collectors and supervisors were done. Onsite checking and review of the completed questionnaire were done by the principal investigator.
2.7. Data management and quality
Data collectors were trained for two days so that they became familiar with the aims of the study, its contents, sampling procedure, interviewing technique, data collection tools, and the issue of confidentiality. The questionnaire was first prepared in English and then translated to Afan Oromo and Amaharic by experts, then translated back to English by another person to ensure its consistency and accuracy. A pretest was carried out on 5% of the total sample size in one kebele, Sheraro town, which was placed outside of the main study area before the actual data collection. Following the pre-test, questionnaire modifications were made to improve the instrument's validity and reliability.
2.8. Data analysis
The editing, coding, and sorting of the collected questionnaire were done manually daily to check for completeness. After being checked for completeness, the data were entered into Epi-data Manager version 3.1 and then exported to SPSS version 25 for analysis. Descriptive statistics were done and the information was presented using tables, figures, and text.
There was no multicollinearity among the independent variables included in the model, and the maximum variance inflation factor was 1.058. The models' fitness was checked using the Hosmer and Lemeshow goodness of fit test. The internal validity of the tools was tested using Cronbach's alpha coefficient (0.76), which is good. Logistic regression was applied to analyze the association between dependent and independent variables. Bivariate analysis was employed to select candidate variables for multivariable analysis. Multivariable analysis was performed on variables with a p-value of less than or equal to 0.2. Multivariable analysis was carried out to assess the association between dependent and independent variables, and variables that have a p-value of less than 0.05 were identified as predictors. Adjusted odds ratios along with 95% confidence intervals were calculated for each of the independent variables in logistic regression to declare a significant association.
3. Results
3.1. Socio-demographic characteristics of pregnant mothers
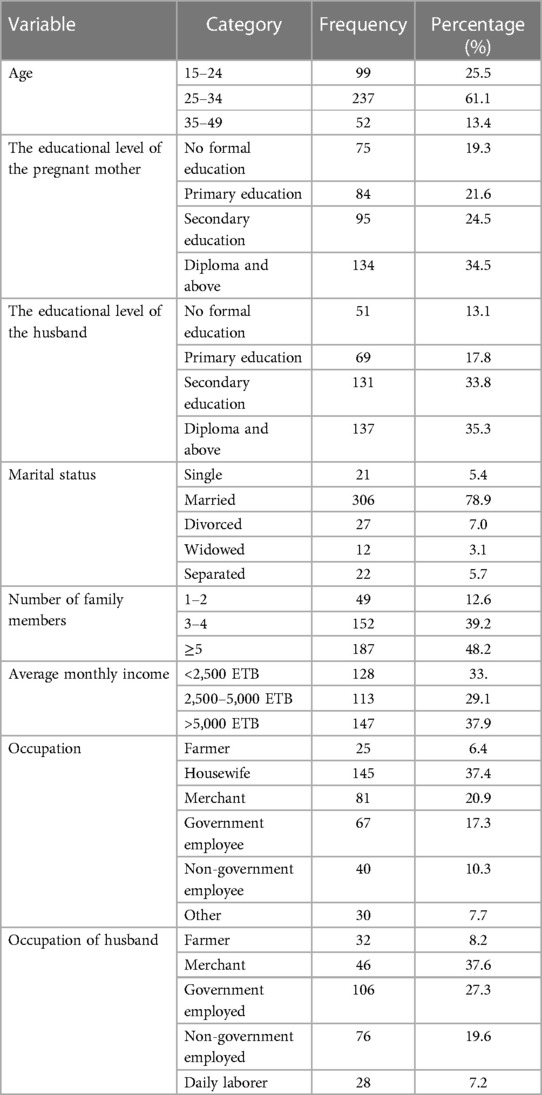
A total of 388 pregnant women were interviewed, making the response rate 98.7%. The study participants' median age was 29 years, with an interquartile range of 24–33 years. More than half of the respondents were between 25 and 34 years old. Approximately half of the study participants (52.1%) have a monthly income of 5,000 ETB (91.68 USD) or less, while 229 (59%) were at the educational level of secondary school or above. The majority of the participants, 306 (78.9%), were married, and 81 (20.9%) of the women were merchants. Nearly half of the participants, 187 (48.2%), have a family size of 5 or above (Table 1).
3.1.1. Obstetric history and reproductive health service-related factors
Almost two-thirds (64.7%) of study participants had 2–4 pregnancies, and 76.5% of study participants received financial and psychological support from a partner. Unplanned pregnancies accounted for 74 pregnancies (19.1%). Ninety-one (23.5%) had had previous miscarriages. We found that 62.4% of study participants had never heard of preconception care (Table 2).
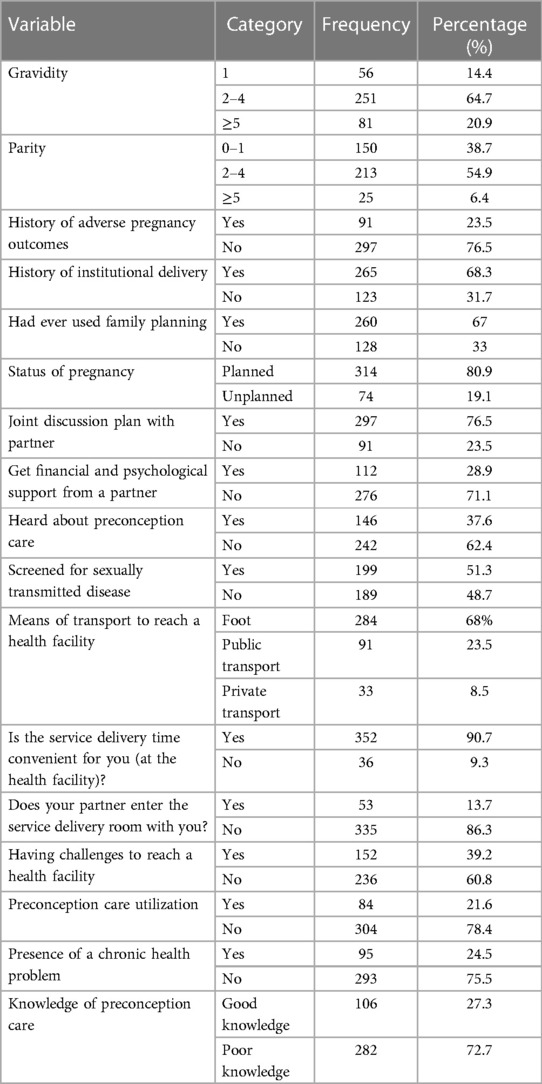
Table 2. Obstetric history and reproductive health service-related factors among pregnant mothers living in Fiche town, 2021.
3.2. Utilization of preconception care
Only 84 (21.6%; 95% CI: 18, 25.8) of the 388 study participants use at least one component of the World Health Organization's preconception care package. Micronutrient supplementation (i.e., iron, folic acid) is the most commonly used component of PCC while optimizing psychological health is the least used (Figure 1).
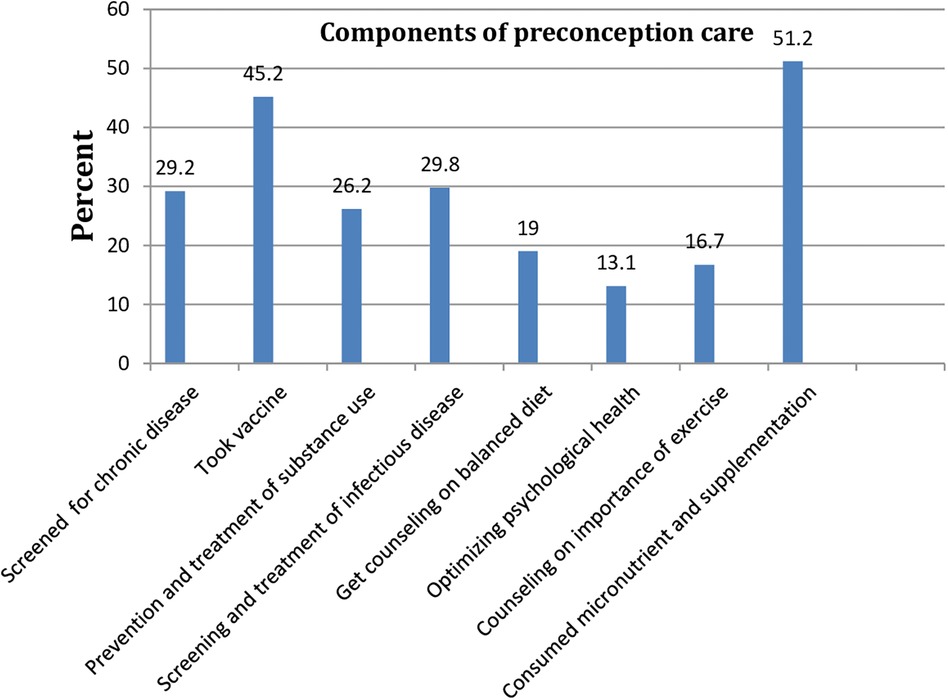
Figure 1. Proportion of World Health Organization components of preconception care utilization among pregnant women found in Fiche town, 2021.
3.3. Factors associated with preconception care
Age, educational status, joint discussion and planning with a partner, getting financial and psychological support from a partner, partner inter ANC rooms, having a chronic health problem, having a bad obstetric history, hearing about preconception care, and having good knowledge about preconception care were associated with preconception care in binary logistic regression. However, in multivariable logistic regression, the educational status of the study participant, joint discussion and planning with the partner, getting financial and psychological support from the partner, having a history of chronic health problems, and knowledge of preconception care were significantly associated with preconception care.
Preconception care use was 3.47 (AOR = 3.47, 95% CI: 1.27, 9.53) times more likely among pregnant women who completed a diploma or a higher level of education. Preconception care utilization was 2.42 (AOR = 2.42; 95% CI: 1.34, 4.38) times more likely among pregnant mothers who had good knowledge (Table 3).
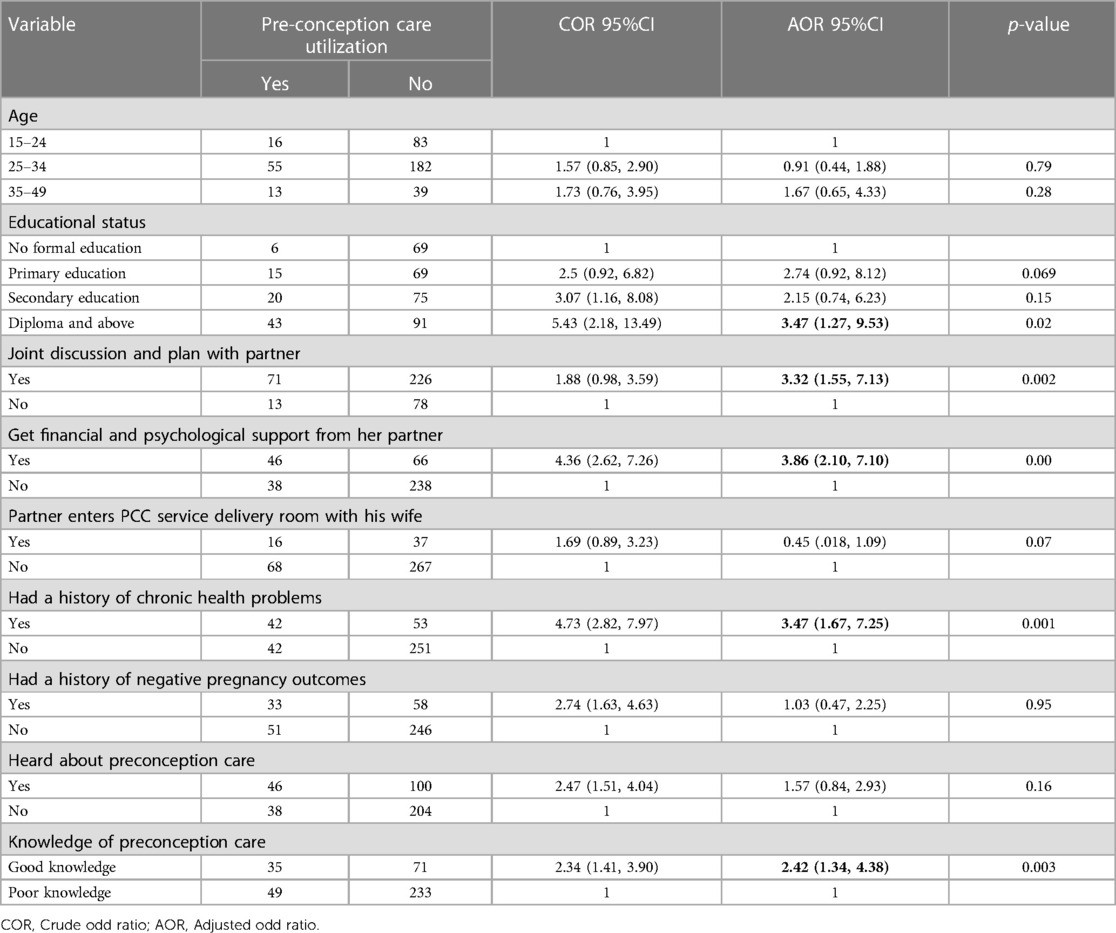
Table 3. A bivariable and multivariable logistic regression model of factors associated with preconception care among pregnant mothers in Fiche town, North Shoa, Ethiopia, in 2021.
4. Discussion
In developing countries, like Ethiopia, where adverse maternal and neonatal outcomes are high, emphasizing preconception care is crucial. This community-based, cross-sectional study identified factors influencing PCC utilization among pregnant mothers in Fiche Town, central Ethiopia.
The findings of our study revealed that 21.6% (95% CI: 18, 25.8) of the respondents utilized preconception care. This finding was in line with studies done in the West Guji Zone (22.3%) (34), Mekelle (18.2%) (27), Hosanna Town (19%) (35), south-east Nigeria (23.4%) (36), and systematic review and meta-analysis in Africa (18.72%) (37).
Our study's findings, on the other hand, were lower than those of Mizan Aman (28.6%) (38), Southern Sri Lanka (27.2%) (39), Los Angeles 29.7 (40), Shanghai, China (42.2%) (41). Disparities in information accessibility, socioeconomic status, and the quality of the healthcare delivery system may all contribute to this variation (42).
This study's findings, however, are higher than those of Adet (9.6%) (26), Debre Birhan town (13.4%) (2), West Shoa zone (14.5%) (29), and Debre Tabor (15.8%) (43). The reason for this variation may be differences in the study population's level of education, culture, study setting, or year of the study. As the year elapses, there may be an increase in awareness and knowledge about the importance of preconception care, which leads to increased service utilization. This study finding is also higher than the systematic review and meta-analysis done by Ayele et al. (16.27%) (44). The possible justification for this may be a single study vs. systematic review and meta-analysis (SRMA). Our study was done at the community level while SRMA was a pooled result of both community and institutional-based studies.
Regarding factors, pregnant mothers who attended education to the level of a diploma or above were 3.47 times more likely to utilize PCC when compared to those who didn’t attend formal education. Studies done in Debre Birhan town (2), Adet (26), and China (45) support this finding. The reason for this may be that pregnant women with higher educational levels have more information and a better understanding of the importance of PCC, which is one of the driving factors for service utilization (34). Additionally, empowering women has a positive impact on maternity service utilization (46, 47).
Discussing and planning with a partner as well as obtaining psychological and financial support from her husband have a significant effect on PCC utilization. This finding was consistent with studies done in Mekelle (27), and Shanghai, China (45). This can be justified as, in developing countries, men are the chief decision-makers; therefore, their psychological and financial support enhances service utilization (31, 20).
The odds of PCC utilization were 3.47 times more likely among pregnant mothers who had a history of chronic health problems. This finding was supported by a study done in Mekelle (27). This may be because those with chronic health problems have followed up with and may have gotten information and advice from health professionals about the effect of their disease on pregnancy (48). They may also be advised on what to do before conception (49–51).
Knowing PCC increases service utilization by 2.42 times. This finding is supported by research conducted in the west Shoa zone (52), Mekelle (27), Mizan Aman (38), and Hosanna town(35). Evidence from Shanghai, China (45), also supports this study. This is an indicator that improving pregnant women's knowledge of the importance of PCC is an entry point for increasing service utilization (53, 54).
5. Strength and limitations
The study was conducted at the community level to address the pregnant mothers who did not visit the health facility. It is also the first study in the study area. However, the study was not without limitations, was cross-sectional, which did not indicate causation, and it was not multicenter. Additionally, there may be social desirability bias as it is interviewer administered.
6. Conclusion
This study indicated that the utilization of preconception care among study participants was found to be low. Reaching a high level of education, having a joint discussion and plan with a partner about pregnancy, getting psychological and financial support from a partner, and having good knowledge about preconception care were among the factors that enhanced service utilization. Having a chronic health problem is also one of the factors that promote service utilization. Involving partners in the maternity care continuum is critical to a positive maternal and neonatal outcome. Preconception is a better opportunity to intervene and maintain the mother in the continuum of care (55).
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethical approval was obtained from the Institutional Health Research Ethics Review Committee (IHRERC) (ref. no. P/S/H/D52) of Jimma University's Institute of Public Health. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
NF is the principal investigator. All authors contributed equally to the work, whether at the conceptual level (NF, AfT, and AK), data acquisition (NF, AdN, AS, and EY), analysis (AbN, AS, KN, and JD), or interpretation (AkT, ML, and FT). They participated equally in drafting, revising, or critically reviewing the work and agreed to be accountable for all aspects of it. All authors contributed to the article and approved the submitted version.
Funding
Jimma University's Faculty of Health Sciences contributed to the study's funding in part. However, they are not involved in the study's planning, data gathering, analysis, or interpretation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Chibwae A, Kapesa A, Jahanpour O, Seni J, Basinda N, Kadelya E, et al. Attendance of male partners to different reproductive health services in Shinyanga District, North western Tanzania. Tanzan J Health Res. (2018) 20(2). doi: 10.4314/thrb.v20i2.9
2. Demisse TL, Aliyu SA, Kitila SB, Tafesse TT, Gelaw KA, Zerihun MS. Utilization of preconception care and associated factors among reproductive age group women in Debre Birhan town, North Shewa, Ethiopia. Reprod Health. (2019) 16(1):1–10. doi: 10.1186/s12978-019-0758-x
3. Jack BW, Culpepper L. Preconception care: risk reduction and health promotion in preparation for pregnancy. JAMA. (1990) 264(9):1147–9. doi: 10.1001/jama.1990.03450090083032
4. Hillemeier MM, Weisman CS, Chase GA, Dyer AM, Shaffer ML. Women’s preconceptional health and use of health services: implications for preconception care. Health Serv Res. (2008) 43(1p1):54–75. doi: 10.1111/j.1475-6773.2007.00741.x
5. Shannon GD, Alberg C, Nacul L, Pashayan N. Preconception healthcare delivery at a population level: construction of public health models of preconception care. Matern Child Health J. (2014) 18:1512–31. doi: 10.1007/s10995-013-1393-8
6. Mittal P, Dandekar A, Hessler D. Use of a modified reproductive life plan to improve awareness of preconception health in women with chronic disease. Perm J. (2014) 18(2):28–32. doi: 10.7812/TPP/13-146
7. Organization WH. Meeting to develop a global consensus on preconception care to reduce maternal and childhood mortality and morbidity: World Health Organization Headquarters, Geneva, 6–7 February 2012: meeting report. (2013).
8. Tieu J, Middleton P, Crowther CA, Shepherd E. Preconception care for diabetic women for improving maternal and infant health. Cochrane Database Syst Rev. (2017) (8). doi: 10.1002/14651858.CD007776.pub3
9. Organization WH. Trends in maternal mortality: 1990–2015: estimates from WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: World Health Organization. (2015). Available at: https://reliefweb.int/report/world/trends-maternal-mortality-1990-2015-estimates-who-unicef-unfpa-world-bank-group-and?gclid=Cj0KCQjw7aqkBhDPARIsAKGa0oJyNpv7L4Txqnd86j5XVL_nguinkMOAtRDO1G7xp4o3zyrJ4VAPwsgaAvJGEALw_wcB
10. Organization WH. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. (2019).
11. Berglund A, Lindmark G. Preconception health and care (PHC)—a strategy for improved maternal and child health. Upsala J Med Sci. (2016) 121(4):216–21. doi: 10.1080/03009734.2016.1191564
12. Dean SV, Mason EM, Howson CP, Lassi ZS, Imam AM, Bhutta ZA. Born too soon: care before and between pregnancy to prevent preterm births: from evidence to action. Reprod Health. (2013) 10(1):1–16. doi: 10.1186/1742-4755-10-1
13. Johnson K, Posner SF, Biermann J, Cordero JF, Atrash HK, Parker CS, et al. Recommendations to improve preconception health and Health Care—United States: report of the CDC/ATSDR preconception care work group and the select panel on preconception care. MMWR Recomm Rep. (2006) 55(6):1-CE-4.
14. World Health Organization. Pre-conception care: maximizing the gains for maternal and child health. Policy brief. (2013).
15. Dean SV, Lassi ZS, Imam AM, Bhutta ZA. Preconception care: closing the gap in the continuum of care to accelerate improvements in maternal, newborn and child health. Reprod Health. (2014) 11(3):1–8. doi: 10.1186/1742-4755-11-S3-S1
16. Bailey C, Walker R, Hill B, Hills Ap, Venn A, Skouteris H. Preconception health and wellbeing interventions in the workplace: A systematic review. Research Square [preprint]. (2019) Available at: https://doi.org/10.21203/rs.2.12690/v1
17. Bishwajit G, Tang S, Yaya S, Ide S, Fu H, Wang M, et al. Factors associated with male involvement in reproductive care in Bangladesh. BMC Public Health. (2017) 17(1):1–8. doi: 10.1186/s12889-016-3915-y
18. United Nations Ethiopia. Good Health and Well-being. Available at: https://ethiopia.un.org/en/sdgs/3
19. Karim AM, Admassu K, Schellenberg J, Alemu H, Getachew N, Ameha A, et al. Effect of Ethiopia’s health extension program on maternal and newborn health care practices in 101 rural districts: a dose-response study. PLoS One. (2013) 8(6):e65160. doi: 10.1371/journal.pone.0065160
20. Abrha MW, Asresu TT, Weldearegay HG. Husband support rises women’s awareness of preconception care in Northern Ethiopia. Sci World J. (2020) 2020:1–7. doi: 10.1155/2020/3415795
21. Falade-Fatila O, Adebayo AM. Male partners’ involvement in pregnancy related care among married men in Ibadan, Nigeria. Reprod Health. (2020) 17(1):1–12. doi: 10.1186/s12978-020-0850-2
22. Masaba BB, Mmusi-Phetoe RM. Barriers to and opportunities for male partner involvement in antenatal care in efforts to eliminate mother-to-child transmission of human immunodeficiency virus in Kenya: systematic review. Open Nurs J. (2020) 14(1):232–9. doi: 10.2174/1874434602014010232
23. Young CT, Urquia ML, Ray JG. Preconception care in low-and middle-income countries: new opportunities and a new metric. PLoS Med. (2013) 10(9):e1001507. doi: 10.1371/journal.pmed.1001507
24. Hailegebreal S, Gilano G, Seboka BT, Ahmed MH, Simegn AE, Tesfa GA, et al. Prevalence and associated factors of caesarian section in Ethiopia: a multilevel analysis of the 2019 Ethiopia Mini Demographic Health Survey. BMC Pregnancy Childbirth. (2021) 21(1):1–9. doi: 10.1186/s12884-021-04266-7
25. Yohannes Z, Tenaw Z, Astatkie A, Siyoum M, Bekele G, Taye K, et al. Levels and correlates of knowledge and attitude on preconception care at public hospitals in Wolayita Zone South Ethiopia. BioRxiv. (2019) 1:586636. doi: 10.1101/586636
26. Goshu Y, Liyeh T, Ayele AS. Preconception care utilization and its associated factors among pregnant women in Adet, North-Western Ethiopia (Implication of Reproductive Health). J Women’s Health Care. (2018) 7(445):2167-0420. doi: 10.4172/2167-0420.1000445
27. Asresu TT, Hailu D, Girmay B, Abrha MW, Weldearegay HG. Mothers’ utilization and associated factors in preconception care in northern Ethiopia: a community based cross sectional study. BMC Pregnancy Childbirth. (2019) 19(1):1–7. doi: 10.1186/s12884-019-2478-1
28. World Health Organization. Preconception care [Internet]. WHO Regional Office for South-East Asia. (2014). Available at: https://apps.who.int/iris/handle/10665/205637
29. Fekene DB, Woldeyes BS, Erena MM, Demisse GA. Knowledge, uptake of preconception care and associated factors among reproductive age group women in West Shewa zone, Ethiopia, 2018. BMC Womens Health. (2020) 20:1–8. doi: 10.1186/s12905-020-00900-2
30. Kebede AS, Muche AA, Alene AG. Factors associated with adverse pregnancy outcome in Debre Tabor town, Northwest Ethiopia: a case control study. BMC Res Notes. (2018) 11(1):1–6. doi: 10.1186/s13104-017-3088-5
31. Yargawa J, Leonardi-Bee J. Male involvement and maternal health outcomes: systematic review and meta-analysis. J Epidemiol Community Health. (2015) 69(6):604–12. doi: 10.1136/jech-2014-204784
32. Fitrianingsih J, Stang C, Amiruddin R. Prevention model on pregnancy complication as early warning programs through self care approach. Ann Romanian Soc Cell Biol. (2021) 25(6):12226–40.
33. Hibbert EJ, Chalasani S, Kozan P, Myszka R, Park KE, Black KI. Preconception care and contraceptive use among Australian women with diabetes mellitus. Aust J Gen Pract. (2018) 47(12):877–83. doi: 10.31128/AJGP-03-18-4529
34. Amaje E, Fikrie A, Utura T. Utilization of preconception care and its associated factors among pregnant women of West Guji Zone, Oromia, Ethiopia, 2021: a community-based cross-sectional study. Health Serv Res Manag Epidemiol. (2022) 9:23333928221088720. doi: 10.1177/23333928221088720
35. Wegene MA, Gejo NG, Bedecha DY, Kerbo AA, Hagisso SN, Damtew SA. Utilization of preconception care and associated factors in Hosanna Town, Southern Ethiopia. PLoS One. (2022) 17(1):e0261895. doi: 10.1371/journal.pone.0261895
36. Odira CC, Chiejina EN, Okafor CN, Ibekwe AM. Preconception care utilization among childbearing women in South-East Nigeria. Midwifery. (2020) 4(6):1–13. doi: 10.52589/AJHNM-5MRKM80J
37. Tekalign T, Lemma T, Silesh M, Lake EA, Teshome M, Yitna T, et al. Mothers’ utilization and associated factors of preconception care in Africa, a systematic review and meta-analysis. PLoS One. (2021) 16(7):e0254935. doi: 10.1371/journal.pone.0254935
38. Setegn Alie M, Alemu T, Alemayehu D, Negesse Y, Gebremariam A. Preconception care utilization and associated factors among reproductive age women in Mizan-Aman town, Bench Sheko zone, Southwest Ethiopia, 2020. A content analysis. PLoS One. (2022) 17(8):e0273297. doi: 10.1371/journal.pone.0273297
39. Patabendige M, Goonewardene I. Preconception care received by women attending antenatal clinics at a Teaching Hospital in Southern Sri Lanka. Sri Lanka J Obstet Gynaecol. (2013) 35(1):3–9. doi: 10.4038/sljog.v35i1.5996
40. Batra P, Higgins C, Chao SM. Previous adverse infant outcomes as predictors of preconception care use: an analysis of the 2010 and 2012 Los Angeles mommy and baby (LAMB) surveys. Matern Child Health J. (2016) 20(6):1170–7. doi: 10.1007/s10995-015-1904-x
41. Du L, La X, Zhu L, Jiang H, Xu B, Chen A, et al. Utilization of preconception care and its impacts on health behavior changes among expectant couples in Shanghai, China. BMC Pregnancy Childbirth. (2021) 21(1):1–8. doi: 10.1186/s12884-020-03485-8
42. Celik Y, Hotchkiss DR. The socio-economic determinants of maternal health care utilization in Turkey. Soc Sci Med. (2000) 50(12):1797–806. doi: 10.1016/S0277-9536(99)00418-9
43. Ayele AD, Ayenew NT, Kassa BG, Teffera AG, Mihretie GN, Yehuala ED, et al. Preconception care utilization and its associated factors among women in debre tabor town Northwest Ethiopia: community based cross-sectional study. SAGE Open. (2022) 12(2):21582440221097392. doi: 10.1177/21582440221097392
44. Ayele AD, Belay HG, Kassa BG, Worke MD. Knowledge and utilisation of preconception care and associated factors among women in Ethiopia: systematic review and meta-analysis. Reprod Health. (2021) 18(1):1–15. doi: 10.1186/s12978-021-01132-9
45. Ding Y, Li XT, Xie F, Yang YL. Survey on the implementation of preconception care in S hanghai, C hina. Paediatr Perinat Epidemiol. (2015) 29(6):492–500. doi: 10.1111/ppe.12218
46. Ahmed S, Creanga AA, Gillespie DG, Tsui AO. Economic status, education and empowerment: implications for maternal health service utilization in developing countries. PLoS One. (2010) 5(6):e11190. doi: 10.1371/journal.pone.0011190
47. Tekelab T, Chojenta C, Smith R, Loxton D. Factors affecting utilization of antenatal care in Ethiopia: a systematic review and meta-analysis. PLoS One. (2019) 14(4):e0214848. doi: 10.1371/journal.pone.0214848
48. Metasebia G. (2020) Utilization of preconception care and associated factors among HIV positive women attending art clinics in north Shoa Zone governmental hospitals, 2020 [dissertation]. Debre Berhan: Debre Berhan University.
49. Willhoite MB, Bennert HW Jr, Palomaki GE, Zaremba MM, Herman WH, Williams JR, et al. The impact of preconception counseling on pregnancy outcomes: the experience of the Maine Diabetes in Pregnancy Program. Diabetes Care. (1993) 16(2):450–5. doi: 10.2337/diacare.16.2.450
50. Chuang CH, Velott DL, Weisman CS. Exploring knowledge and attitudes related to pregnancy and preconception health in women with chronic medical conditions. Matern Child Health J. (2010) 14:713–9. doi: 10.1007/s10995-009-0518-6
51. Dunlop AL, Jack BW, Bottalico JN, Lu MC, James A, Shellhaas CS, et al. The clinical content of preconception care: women with chronic medical conditions. Am J Obstet Gynecol. (2008) 199(6):S310–27. doi: 10.1016/j.ajog.2008.08.031
52. Gezahegn A. (2016) Assessment Knowledge and Experience of Preconception Care among Pregnant Mothers Attending Antenatal Care in West Shoa Zone Public Health Centers, 2016. [master's thesis]. Addis Ababa: Addis Ababa University.
53. Mousa O, Alfadhel R, Almubarak H. Assessing the level of awareness and utilization of preconception care among Saudi women in Al Ahsa, Saudi Arabia. Nur Primary Care. (2021) 5(6):1–6. doi: 10.33425/2639-9474.1200
54. Gamshe E, Demissie D. Perinatal factors affecting knowledge and utilization of preconception care among pregnant women in Addis Ababa: A cross-sectional study. MJH (2022) 1(1):2790–1378.
55. Tollman SM, Bastian H, Doll R, Hirsch LJ, Guess HA. What are the effects of the fifth revision of the declaration of Helsinki? Fair partnerships support ethical researchGains and losses for rights of consumer and research participantsResearch will be impededSome clauses will hinder development of new drugs and vaccines. Br Med J. (2001) 323(7326):1417–23. doi: 10.1136/bmj.323.7326.1417
Keywords: preconception, care, utilization, pregnant, Fiche, Ethiopia
Citation: Fetena N, Negash A, Kebede A, Sertsu A, Nega A, Nigussie K, Lami M, Yadeta E, Dereje J, Tamire A, Tolessa F and Tadele A (2023) Utilization of preconception care and associated factors among pregnant mothers in Fiche Town, Central Ethiopia: a community-based cross-sectional study 2021. Front. Glob. Womens Health 4:1159693. doi: 10.3389/fgwh.2023.1159693
Received: 2 May 2023; Accepted: 16 August 2023;
Published: 18 September 2023.
Edited by:
Lorena Binfa, University of Chile, ChileReviewed by:
Macarena Martínez Órdenes, University of Chile, ChileAudra Gollenberg, Shenandoah University, United States
© 2023 Fetena, Negash, Kebede, Sertsu, Nega, Nigussie, Lami, Yadeta, Dereje, Tamire, Tolessa and Tadele. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abraham Negash aGFybWVlMTIxQGdtYWlsLmNvbQ==
Abbreviations ANC, Antenatal Care; PCC, Preconception Care; WHO, World Health Organization; SDG, Sustainable Development Goal.
†ORCID Abraham Negash orcid.org/0000-0001-9406-1979
 Negash Fetena1
Negash Fetena1 Abraham Negash
Abraham Negash Addisu Sertsu
Addisu Sertsu Addisu Nega
Addisu Nega Kabtamu Nigussie
Kabtamu Nigussie Magarsa Lami
Magarsa Lami Elias Yadeta
Elias Yadeta Jerman Dereje
Jerman Dereje Aklilu Tamire
Aklilu Tamire Fikadu Tolessa
Fikadu Tolessa