- 1Department of Psychology, Government General Degree College, Singur, Hooghly, India
- 2Department of Psychology, University of Calcutta, Kolkata, India
Introduction: The differential effect of the Covid-19 pandemic on the mental health of the population around the globe is well documented. Social isolation, loss of job, financial crisis, and fear of infection due to the pandemic have widely affected people across countries, and the sexual and gender minority (SGM) group is no exception. However, the additional stressors like stigma, discrimination, rejection, non-acceptance, and violence associated with diverse sexual orientation complicated the situation for the SGM group in the context of the Covid-19 pandemic.
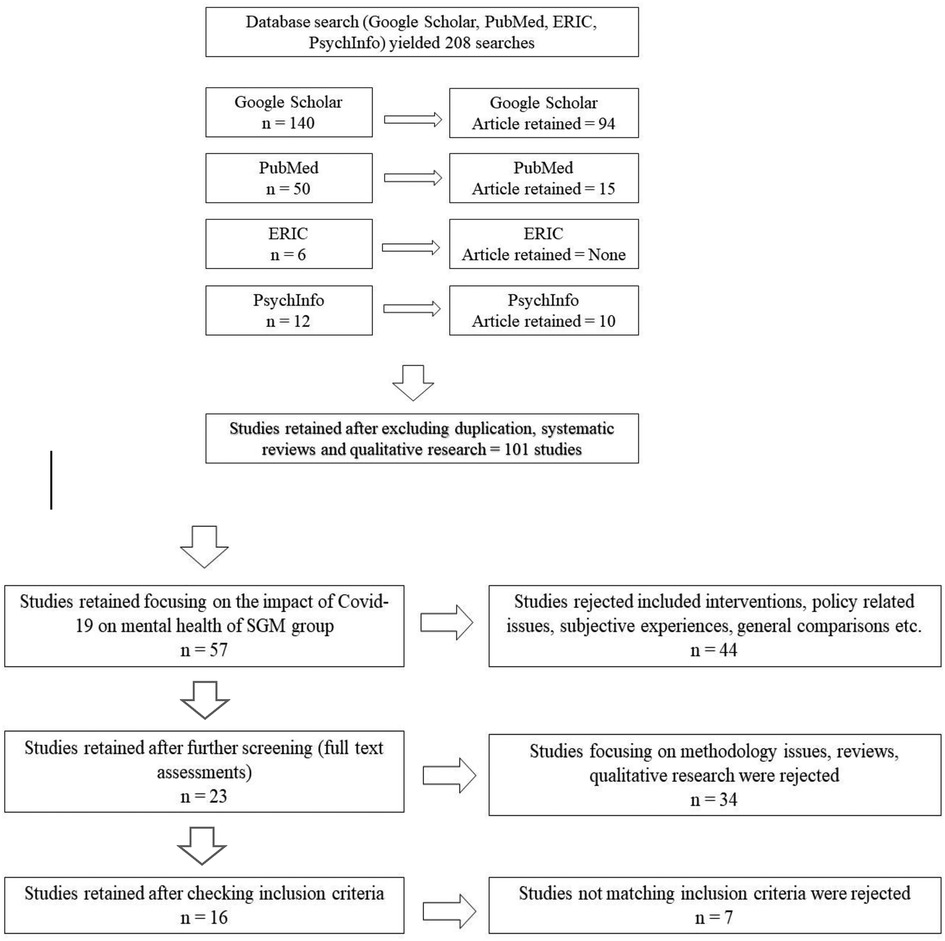
Method: The present study conducted a systematic review of research (n = 16) investigating the impact of Covid-19 stress on the psychological health of SGM individuals. The review had two objectives: (a) to explore the effect of the stress associated with the pandemic on the psychological health of the SGM individuals; and (b) to identify potential stressors associated with the Covid-19 pandemic affecting the mental health of SGM individuals. Studies were selected following a PRISMA protocol and several inclusion criteria.
Results: The review provided new insights into the mental health issues of the SGM individual in the Covid-19 context. The outcome of the review focused on five aspects: (a) depression and anxiety symptoms related to Covid-19 symptoms; (b) perceived social support and Covid-19 stress; (c) family support and psychological distress related to Covid-19; (d) Covid-19 stress and disordered eating, and (e) problem drinking and substance abuse associated with Covid-19 stress.
Discussion: The present review indicated a negative association between Covid-19 stress and psychological distress among sexual and gender minority individuals. The findings have important implications for psychologists and social workers working with this population and policymakers around the globe.
Introduction
The incidence of Covid-19 in the past couple of years caused immense damage to the physical and mental health of people around the globe (1–4). With subsequent waves of the mutant version of the virus, millions of people suffered, and thousands were dead (5–8). The existence of co-morbid physical conditions like cardiac problems, diabetes, cancer, etc. proved to be fatal in most cases. In this mayhem, the marginalized communities suffered significantly under such circumstances, with lessened healthcare delivery and limited social security (9). The lesbian, gay, bisexual, transgender, and queer (LGBTQ) community is one of those marginalized groups that suffered immensely.
To reduce the spread of infection, every government imposed lockdowns, social distancing, quarantine, and banned travel around the world (10, 11). Although the Covid virus affected people around the globe in a similar way, the outcomes were felt differently across some sections of the society, specifically for the SGM population, the reason being a profound level of social discrimination faced by these individuals across different cultures and societies (10). Moreover, studies reported that many of them have co-morbid conditions of HIV, Cancer, and other forms of physical conditions, which increased their difficulties instead (12, 13). Lockdown and quarantine situations also inhibited them from going to their workplace, which in certain cases, serves as an escape for them, especially in low-income countries of Asia and Africa (10, 14). Hence, the overall situation during the pandemic undoubtedly put them at a higher risk of physical and psychological turmoil.
Risk factors for depression, anxiety, and suicidality among SGM youths
Recent researches suggests that loneliness, anxiety, fear of contraction, and limited access to healthcare facilities due to the Covid-19 pandemic might have worsened psychological health with heightened symptoms of depression, anxiety, self-harm, and suicidal ideation among minority groups (1–4, 15). For sexual minority groups, the situation was more compound because of their pre-existing psychological vulnerabilities associated with social inequalities and discrimination (5–8). Research indicates that the Covid-19 pandemic also resulted in changes in the life circumstances of sexual minority groups. For instance, Conron (16) reported that several SGM young adults in the US had to return to their parental house due to the financial crisis, loss of jobs, and complete lockdown of university campuses due to the pandemic. This imposed additional pressure on them as many of them preferred avoiding their families due to non-acceptance by the family members Across the world, the socially disadvantaged SGM group faced unemployment, food insecurity, social discrimination, and severe financial crisis during the Covid-19 pandemic (17). All this resulted in heightened psychological vulnerabilities and declined subjective well-being among these young adults (5, 8, 18). Pre-existing mental health conditions such as depression, anxiety, and addiction problems, further aggravated the situation for them as they were forced to stay at home with very limited social interactions and rejection from family members (9, 19).
Another line of studies pointed out that alcohol use, substance abuse, and drug dependence among SGM young adults is a common practice (20, 21), even before Covid-19. As noted by Bourdieu (22), subtle differences in “cultural and normative markers” (23) like body language, gestures, accent, etc. can interact with demographic identities like gender, race, and ethnicity to produce hierarchical judgments potentially enough to cause discrimination in the society. Contributing factors to the higher incidence of drug dependence and substance abuse among SGM youths have often been attributed to such hierarchical power structures creating and causing inequalities in employment, health care, living conditions, and other social aspects (24–27). Several pieces of research across the globe reported a higher incidence of substance abuse among SGM youths during Covid-19, leading to poorer mental health and self-harm tendencies. For instance, Slemon et al. (27) compared SGM youths with non-SGM youths in a Canadian population. The study found that in comparison to the non-SGM group, the SGM respondents had experienced a higher impact of Covid-19 and substance abuse, which included poorer psychological health, deteriorated coping, self-harm behaviors, suicidal thoughts, and greater dependence on drugs and substance abuse to survive. Similar findings were reported by Salerno et al. (8) in a US population. The researchers found that almost one-third of the SGM respondents had an increased level of substance abuse since the commencement of Covid-19. This increased abuse along with alcohol problems, and drug dependence contributed to ill-psychological health and complicated the situation among SGM youths.
Higher psychological distress among SGM youths and adolescents has been reported by several researchers. Risk factors for increased suicidality among this minority group result from symptoms of depression, hopelessness, substance abuse, psychiatric distress, and recent incidences of suicide by another family member or a friend (28–30). During the pandemic, an elevated level of loneliness was reported in SGM adolescents and young adults (31, 32). Herrmann et al. (33) compared the loneliness and depressive symptoms among transgender and cisgender individuals across the first and second waves of Covid-19 in a German population. The researchers noted a higher level of loneliness among transgenders in comparison to the cisgender respondents. Moreover, it was found that loneliness mediated the symptoms of depression among the SGM respondents. Jacmin-Park et al. (34) found that the buffering effect of perceived loss of social support due to discrimination during the pandemic on depressive symptoms was four times higher among the transgender group than the cisgender respondents. Gonzales et al. (15) found more frequent symptoms of psychological distress and symptoms of anxiety and depression among 60% of American college-going SGM youths. As per the Sexual Minority Stress Model (35), group solidarity and social support are important protective factors for the SGM group against psychological distress associated with stigma and discrimination (34–37).
Mental health issues among the SGM group associated with the Covid-19 pandemic are a crucial concern, although under-explored. Several studies have been conducted to explore the issue in the past couple of years. The present study intends to present a systematic review of the incidences of psychological distress as reported among SGM youths, especially symptoms of depression and anxiety, associated with the isolation and discrimination faced during the Covid-19 pandemic across the world. The review has the following objectives: (a) To explore the impact of Covid-19 stress on the psychological health of the sexual minority group, and (b) To identify the stressors associated with the Covid-19 pandemic that impacts the mental health well-being of the sexual minority individuals. This review will help integrate and understand the overall effect of the Covid-19 pandemic on the psychological health of the SGM youths.
Method
Search method
The review followed the format of the PRISMA (Preferred Reporting Items for Systematic Reviews) framework. The selection process is illustrated in Figure 1 which depicts the selection process following the inclusion criteria for the review. Chiefly, studies were selected from online databases namely, Google Scholar, PubMed, Eric, and PsychInfo. The keywords used for the search were “Sexual Minority”, “LGBTQ” “Transgender”, “Mental Health”, “Covid-19”, “Pandemic”, and also “Depression” and “Anxiety”, jointly and also in isolation. The review was done during the second week of September 2022. The initial search generated thousands of research out of which 140 searches were relevant in Google Scholar, 50 searches were relevant in PubMed, ERIC yielded six related searches, and PsychInfo yielded 12 searches. Relevance was judged based on the keywords used for the search. For instance, a combination of “Mental Health”, “Covid-19”, “Pandemic”, “Depression” and “Anxiety” keywords yielded hundreds of studies addressing populations other than sexual minority groups. Again, a search with the keyword “Sexual Minority”, and “LGBTQ” yielded research addressing different issues related to this population. Hence only those studies addressing the impact of the “Covid-19” “pandemic” on the “Mental Health” of the “Sexual Minority”/“LGBTQ”/“Transgender” population were included in the current review, yielding a total of 208 studies.
Figure 1 shows the PRISMA framework used for the search process. out of the relevant 208 searches yielded by the database search, 101 studies were retrieved (excluding the duplication).
In the next stage, the 101 studies were reviewed and 57 studies were selected focusing on the impact of Covid-19 on the mental health of the SGM group. The 44 studies rejected in this stage were focusing on intervention, policy-related issues, subjective descriptions of experiences, systematic reviews, general comparisons, and others. This review process was mostly done by analyzing the study abstracts and occasionally looking into the full paper as required. In the next stage, out of the 57 studies, 23 studies were selected after rejecting other studies focusing on methodology issues, comparisons, qualitative research, etc. Studies focusing on subjective descriptions, methodological issues, and systematic reviews were excluded since most of those addressed issues beyond the purview of the current study. Qualitative researches were also excluded because comparing results across quantitative reports using questionnaires with qualitative reports based on interviews is complicated and might invite unnecessary methodological complications.
Subsequently, the 23 studies (full papers) were thoroughly reviewed and finally, 16 studies were selected following the inclusion criteria: (a) Study subjects belonging to Sexual and Gender Minority groups; (b) Subjects are adults; (c) Subjects experiencing symptoms of depression and anxiety; (d) Study reported quantitative assessment (using questionnaires instead of semi-structured interviews); (e) Sample characteristics clearly mentioned; (f) Study objectives focusing on the impact of Covid-19 on the psychological health of SGM group; (g) Details of testing materials discussed clearly;(h) Statistical analysis reported and discussed elaborately; (i) Results indicate a significant impact of the pandemic on the psychological health of SGM group. These 16 studies were independently reviewed by the two authors on these inclusion criteria and then included in the review. All the studies fulfilled the inclusion criteria set for the review and are therefore considered for the present review.
Quality assessment
All the 16 studies were quality assessed using the Joanna Briggs Institute (JBI) checklist for analytical cross-sectional studies (38). The checklist consists of eight criteria assessing the quality of the studies included (related to methodological issues). The studies were rated on the checklist by both authors independently. All the studies were found to be meeting the standards of quality assessment.
Results
Study characteristics
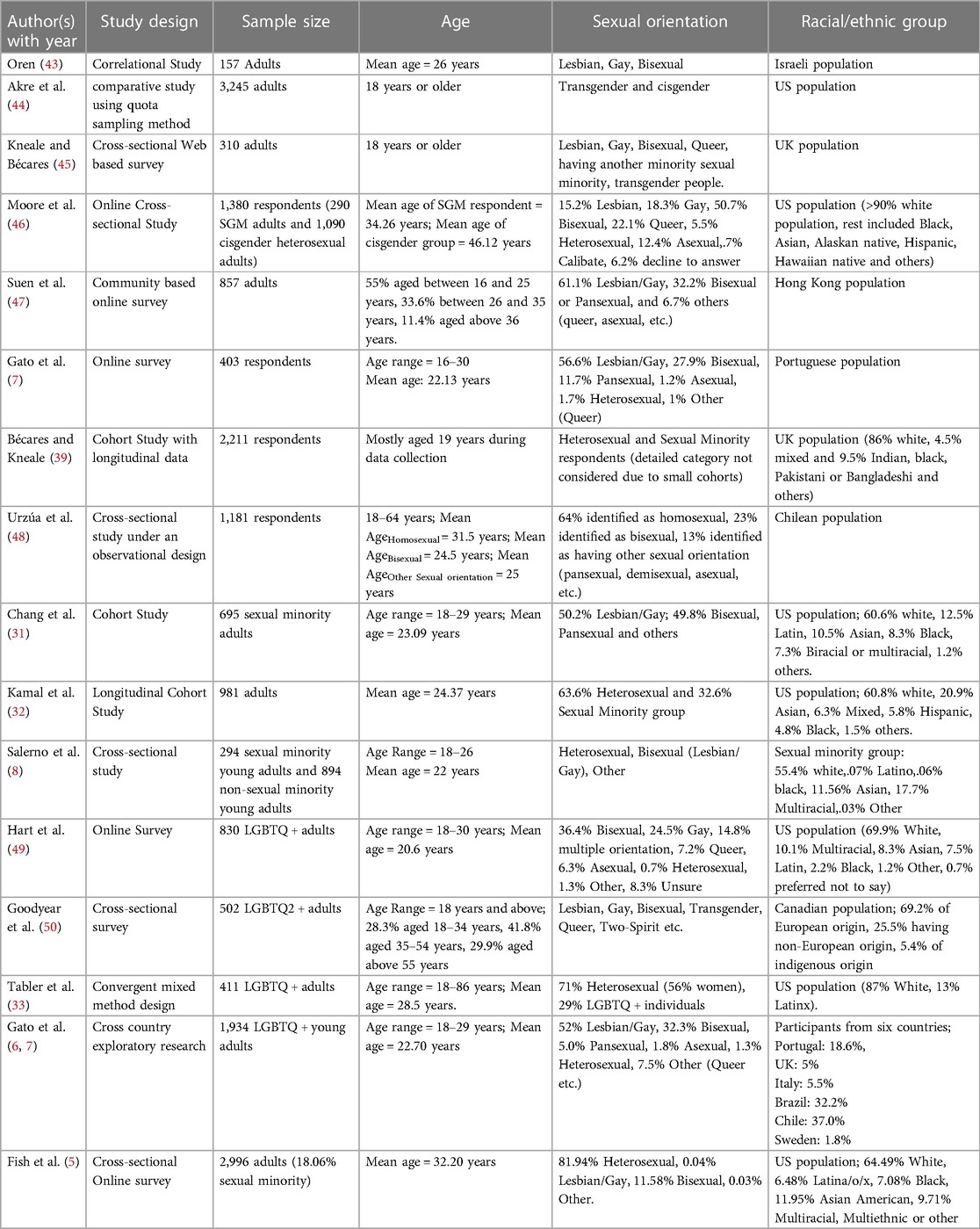
The studies selected for the review, mostly followed online or web-based cross-sectional survey method, comparing the different sexual minority groups with cisgender heterosexual groups, except three studies that followed a Cohort design/ Longitudinal Cohort study (39–41). For instance, Kamal et al. (41) considered the data collected during Wave 1 of the Covid-19 pandemic through a US-based longitudinal cohort study (CARES: Covid-19 Adult Resilience Experiences Study) for the investigation. Similarly, Chang et al. (40) collected data in three cohorts in 2020, January–March (n = 99), July–September (n = 390), and September–November (n = 305). The second and third cohorts were finally considered for the investigation. On the other hand, the study by Bécares and Kneale (39) was a typical longitudinal cohort research that was a part of the Millennium Cohort Study done among UK infants born between 2000 and 2002. The present research included participants who had responded in the 6th and 7th data collection sweeps and during the 1st wave of the Covid-19 pandemic. Hence, this study provided a comparative view of the mental health of the SGM group during the pre-pandemic phase and the 1st wave of the pandemic. Apart from these three studies, one other study (42) followed a mixed method design, where a quantitative assessment was mixed with a qualitative approach and hence aided in providing a more comprehensive and rich understanding of SGM mental health issues during Covid-19 pandemic. Additionally, the study by Gato et al. (6, 7) did a cross-country exploration among LGBTQ+ individuals from six different nations. This study, therefore, provides a more in-depth insight into the prevalence of psychological distress among the SGM group across different nations. It is important to note that all the studies followed a web-based survey method, considering the physical restrictions imposed during the pandemic. Table 1 provides a comparative view of the study characteristics and demographics of the study participants of all sixteen studies included in the review.
Sample characteristics
Out of the 16 studies, seven studies presented a comparative account across heterosexual and SGM respondents (5, 8, 39, 32, 33, 44, 46), while three more studies included heterosexual respondents although in very small percentages (6, 7, 49). The rest of the studies included only the SGM group for the investigation. Participants of all the studies were adults with mostly young age groups included in the research. Additionally, the studies considered for the review include participants from across a wide range of race/ethnic groups. Eight studies were conducted on the US population (5, 8, 31–33, 44, 46, 49), although the US population included in the studies was a heterogenous mix of Asian American, Latin American, African American, and multiracial origins along with White Americans. Two studies were conducted among the UK population (39, 45), also a heterogeneous group of white individuals, mixed racial groups, and Asian individuals. The rest of the studies included participants representing several different countries like Israel (43), Hong Kong (47), Portugal (7), Chile (48), and Canada (50). Gato et al. (6, 7) included participants from six different countries namely, Portugal, the UK, Italy, Brazil, Chile, and Sweden. Hence, the study results are representative of the mental health scenario of the SGM group across a wide geographical region.
Study measures
All the studies included in the review assessed the psychological distress related to Covid-19 and the associated symptoms of depression and anxiety among SGM individuals. While the measures for assessing depression and anxiety were all standardized instruments (for instance, 8-item Patient Health Questionnaire (PHQ-8), Kroenke, et al. (51) and 7-item Generalized Anxiety Disorder scale (GAD-7) (52); Depression Anxiety Stress Scales (DASS-21), Lovibond and Lovibond (53), most studies used customized questions to assess the Covid-19 related stress (for instance (31, 43, 46, 47, 50). The chief reason cited for this practice was a lack of a standardized scale for measuring stress related to Covid-19 among SGM individuals, although Tabler et al. (33) used the Pandemic Stress Scale developed by Taylor et al. (54).
Apart from anxiety, depression, and psychological distress, several studies also measured perceived social support (39, 32–43, 46). The most commonly used measure was the modified Medical Outcomes Study Social Support Survey (8-items) (55), although Kamal et al. (32) and Oren (43) used the 12-item Multidimensional Scale of Perceived Social Support (57) for measuring the same. Some of the studies also studied variables like Loneliness, Rumination, and Quality of relationships in addition to the stress and psychological symptoms related to Covid-19. Additionally, Hart et al. (49) and Tabler et al. (33) measured eating disorder symptoms as well using the Eating Disorder Examination-Questionnaire (58) and Eating Disorder Examination—Questionnaire Short (EDE-QS) (12 items) (59, 60) respectively. Akre et al. (44) and Goodyear et al. (50) measured problem drinking using the Patient-Reported Outcomes Measurement Information System (PROMIS) and substance use through a set of semi-structured questions. Table 2 presents a detailed account of the measures used in the studies.
Study outcomes
Almost all the studies highlighted the significance of the impact of Covid-19 related stress on the psychological health of minority individuals. It can be noted that the studies identified potential Covid-19 stressors that contribute to an increased level of psychological distress among SGM individuals.
Depression and anxiety symptoms related to COVID-19 stress
Increased levels of anxiety and depression were found to be associated with the perceived stress related to the Covid-19 pandemic. Most of the researchers reported such elevated symptoms during the first wave of the pandemic and also during the subsequent waves. Severe symptoms of depression and anxiety were also found to be associated with Covid-19 related physical symptoms (46), psychological distress (c), loneliness (5, 39), and poor quality of life (5). Kamal et al. (32) additionally, reported symptoms of post-traumatic stress disorder associated with higher levels of depression among SGM youths.
Most commonly such experience of psychological distress was attributed to stressors like perceived social support (39, 32–43, 46), family-related issues (8), social discriminations (32) and non-affirmation of one's identity (43).
Perceived social support and COVID-19 stress
In connection to the issue of social support, Meyer (35) proposed the Minority Stress Model in association with lesbian, gay, and bisexual (LGB) health. As per the minority stress model, stressors can be distal or proximal. Distal stressors are characterized by the actual experiences of discrimination, prejudices, harassment, and even violence, while the proximal stressors include the occurrence of internalized homophobia, the need for acceptance by others, and the suppression of one's own sexual identity (43). Several researchers have provided evidence for the fact that such minority distal and proximal stressors lead to elevated levels of psychological distress, a relationship mediated by the development of pathological cognitive processes, and conflictual social and interpersonal relationships (43, 81). In contrast, perceived social support works as a buffer against the negative effects of minority stressors and therefore can be considered an important resource in protecting SGM mental health (35, 43, 82).
Tabler et al. (33) noted that social support plays an important role as a potential protective safeguard against the elevated risks of disordered eating symptoms associated with Covid-19 stress. These findings were further validated by the work of Bécares and Kneale (39) who noted a significantly poorer level of perceived social support associated with lower levels of self-rated health and poor psychological health among the SGM respondents. Moore et al. (46), in a comparison study among SGM and non-SGM adults, noted significantly lower perception (p < .001) of emotional support, tangible support, affectionate support, and positive social interaction support among the SGM respondents in comparison to their non-SGM counterparts. The study also reported significantly heightened symptoms of depression and anxiety among the SGM adults in comparison to the non-SGM respondents. Such findings, therefore, suggest that lack of perceived social support acted as a potential stressor for the SGM individuals under the impact of the Covid-19 pandemic.
Family support and psychological distress related to COVID-19
There is no dearth of studies reporting a lack of family support among sexual minority groups (32, 83, 84). Kamal et al. (32) found that SGM respondents experienced a significantly decreased level of family support (p < .001) in comparison to the non-SGM respondents, and this in turn is associated with significantly increased levels of depression (p = .003), post-traumatic stress disorder symptoms (p = .013), higher levels of worries related to Covid-19 pandemic (p < .001) and grief related to the pandemic (p = .032) among the sexual minority individuals than among the non-SGM individuals. Moreover, the mandate of staying at home due to quarantine had a more debilitating effect on the mental health of the minority group (85, 86). Gato et al. (7) noted that individuals staying at home might be experiencing elevated risks of depression and anxiety, provided the fact that the associated home climate is hostile and non-affirming of the sexual identity of the individuals. Hence, staying at home although, provided a sense of security to most individuals during the pandemic, for the SGM group the response was different, owing to the associated discrimination and parental rejections. These findings were also confirmed by Salerno et al. (8). The researchers noted that sexual minority youths who went back to their parental house during the post-onset of the pandemic experienced significantly higher levels of psychological distress and decreased well-being in comparison to the others who were already staying before, the reasons being the same.
COVID-19 stress and disordered eating
Covid-19 stress is often associated with weight stigmatizing in social media messaging (87), which in turn can contribute to increased perceptions of weight gain and disordered eating behavior (88, 89). Disordered eating behavior among sexual minority groups is a common problem and is often associated with negative experiences of stigma and discrimination (90–92). Such problem behavior is considered a coping mechanism for minority individuals in the face of minority stress (33).
The current review also found that Covid-19 stress among SGM individuals is associated with elevated risks of disordered eating behavior and increased perception of weight gain among them (33). Hart et al. (49) noted that most of their study participants reported an increase in the urge and frequency of engaging in disordered eating behavior. Moreover, they found an association between disordered eating behavior and increased levels of psychological stress due to Covid-19 and the quality of relationships at home and non-acceptance of one's sexual identity by family members. Tabler et al. (33) noted that nearly one out of three participants presented clinically significant symptoms of disordered eating.
Problem drinking and substance abuse associated with COVID-19 stress
Sexual and gender minority individuals are at an increased level of abusing substances and alcohol in comparison to non-SGM individuals even before the onset of the pandemic (16, 93–95). More often, negative experiences of psycho-social stresses contribute to heavy alcohol consumption and other substance abuse among SGM individuals, which in turn leads to elevated risks of psychological distress (96, 97).
In the present review, Goodyear et al. (50) reported increased alcohol use among 24.5% of the study participants and increased cannabis use among 18.5% of the respondents due to the pandemic stress. furthermore, they reported that higher levels of alcohol consumption were associated with poor coping skills, and lower levels of self-rated psychological health, while increased use of cannabis was associated with suicidal thoughts. Along the same line, Fish et al. (5) reported that in comparison to heterosexual men, gay men, and bisexual men experienced a significant decrease in psychological health, quality of life, higher levels of stress, feelings of loneliness, and alcohol consumption. Lesbian individuals also reported significantly higher levels of alcohol consumption in their study.
Discussion
The present review had two objectives; first, to explore the impact of Covid-19 stress on the psychological health of the sexual minority group, and, second, to identify the stressors associated with the Covid-19 pandemic. For the same, 16 studies were selected following the PRISMA framework from among an initial pool of 208 studies. The studies were all selected strategically following nine different inclusion criteria. A detailed review of the studies helped fulfill the two objectives of the current study.
All sixteen studies reported an elevated risk of depression and anxiety symptoms among sexual minority individuals. The heightened symptoms of depression and anxiety were also found to be associated with loneliness (5, 39), symptoms of post-traumatic stress disorder, worries related to the Covid-19 severity and related grief (32), poor quality of relationships (49), suicidal thoughts (50), substance use and alcohol abuse (5, 50), and disordered eating behavior (33, 49). Higher levels of depression and anxiety are more often experienced by non-working, European SGM youths, who are more susceptible to feeling uncomfortable, isolated, and emotionally impacted by the pandemic (6, 7) and among transgender or gender-diverse women who are full-time students (31). Urzúa et al. (59) studied the differential impact of Covid-19 stress among the different subgroups of SGM individuals as well. Their findings suggested a higher occurrence of depressive symptoms among bisexual and lesbian women in comparison to bisexual and gay men.
In most cases, the incidences of worsened psychological health and problem behavior were found to be associated with lower levels of perceived social support, discrimination, hostile family climate, and non-affirming of one's sexual identity (5–7, 32–43, 46). Such findings are in line with other similar studies reporting the role of psychosocial factors in mediating the worsened psychological health among SGM individuals (9, 16, 17).
A second objective of the review was to identify the stressors associated with the pandemic. The present review identified two potential stressors, strong enough to produce a debilitating impact on the mental health of the sexual and gender minority population. First, the present review noted the importance of perceived social support as a buffer against the ill effects of the minority stressors like stigma, discrimination, violence, non-acceptance, and rejection (39, 33, 46). Lower levels of perceived social support (emotional, tangible, affectionate, and positive social interactions) are associated with poor psychological health of SGM individuals. This finding is particularly important since this validates the hypothesis of “Social Support as a buffer against stress” in the Covid-19 context. Second, the review identified the importance of family support in mediating psychological well-being among SGM individuals. The findings revealed that decreased level of family support is associated with increased symptoms of depression, anxiety, post-traumatic stress disorder, and higher levels of worries and grief related to the Covid-19 pandemic (32). Moreover, similar effects on mental health resulted from a hostile family environment and non-acceptance of one's own sexual identity by the family (7, 8). Hence, a lack of family support can be considered a potential stressor in the Covid-19 context.
Implications of the study
Although there has not been any dearth of studies reporting the negative impact of the Covid-19 pandemic on the mental health of the sexual and gender minority group, a review of the articles was lacking in this post-Covid period. A review helps gain new insight into an ongoing event or situation. After the onset of Covid-19, there have been several reviews done, focusing on different aspects of the impact of Covid-19 stress (98–101). However, only a handful of reviews focused on the mental health of the sexual and gender minority group (101–103).
Overall, the present review highlighted the importance of studying and considering the mental health outcomes of Covid-19 stress for the sexual and gender minority group. Some of the previously done reviews also underlined the same, although in a different context, for instance, (101) studied the application of psychotherapy for the minority population in the Covid-19 context. However, the present review not only summarized the negative impact of the pandemic stress on the psychological health of the SGM group but also identified the potential stressors and associated outcomes for the minority individuals in the Covid-19 context. This is one of the major strengths of the present review and contributes to the relevance of the study in the present context. Greater effort must be put on the part of clinical psychologists and social workers to mitigate the debilitating impact of the pandemic on the mental health of sexual and gender minority individuals. Moreover, policymakers must consider the unique impact of psychosocial factors on SGM individuals while developing any mental health policy or stating a law applicable to this population.
Another strength of the present review lies in the fact that the review included studies of several different populations, mostly representing the European, British, and US populations. One of the studies also included the population from Hong Kong (47), providing a representation from one of the Asian countries. This is particularly important because this points to the fact that the impact of Covid-19 stress on the psychological health of the SGM group remains indifferent across different cultures, societies, and even continents.
The timing of the review is also of particular importance and has implications. The present review has been done at such a time when most countries have overcome the three waves of the pandemic and the impact of the pandemic on the mental health of people around the globe is more or less explored. All the reviews done previously (during the ongoing first wave or second wave) could only provide a partial, and in certain cases, an incomplete picture of the scenario. The present review is well-timed and provided a well-representation of the situation across different continents, countries, and cultures. Hence, the findings have wider implications for clinical psychologists, social workers, and policymakers around the globe.
Limitations and future research
Like any other research, the present review also has some limitations. First, the present study included SGM individuals mostly belonging to the young adult age group. However, the pandemic has also hugely affected the SGM older adults and individuals with some terminal conditions like HIV infected population. But researches reporting this impact were beyond the purview of the present review, the reason being that such studies are quite less in number and hence do not qualify for a full-fledged review. Future research should consider an elaborate review of such issues in the context of the Covid-19 pandemic. Second, almost all the studies included studied the European, Canadian, American, and British populations. Only one Asian study done on the Hong Kong population could be included. It would have been better if more studies from the Asian continent and African continents could be included in the present review. A major reason for this has been a lack of empirical studies done on the SGM population of Asian or African countries during the pandemic. This can be attributed to the limitations in the healthcare facilities and research infrastructure of these developing societies, in comparison to western societies. Future research should take note of this issue and consider having more research focusing on SGM individuals in developing societies.
Conclusion
The present study reported a systematic review of sixteen studies focusing on the impact of Covid-19 stress on the mental health of the sexual and gender minority population. The review of the studies reported the association between the negative effect of the pandemic stress and higher levels of psychological distress, symptoms of depression, anxiety, loneliness, problem drinking, and disordered eating behavior among minority individuals. Moreover, the study also identified the lack of perceived social support and family support in mediating the inverse relationship between increased Covid-19 stress and decreased psychological health of the sexual and gender minority individuals. Overall, the review provided a detailed understanding and newer insights into the mental health issues of the sexual and gender minority group in the context of the Covid-19 pandemic.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
Both the authors contributed to the development of the idea. The database search and filtering were done by SD. Both SD and TM did the review of the articles for the final selection as per the inclusion criteria. The manuscript was primarily drafted by SD with inputs and suggestions from TM. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Holloway IW, Garner A, Tan D, Ochoa AM, Santos GM, Howell S. Associations between physical distancing and mental health, sexual health and technology use among gay, bisexual and other men who have sex with men during the COVID-19 pandemic. J Homosex. (2021) 68(4):692–708. doi: 10.1080/00918369.2020.1868191
2. Banerjee D, Rai M. Social isolation in COVID-19: the impact of loneliness. Int J Soc Psychiatry. (2020) 66(6):525–7. doi: 10.1177/0020764020922269
3. Sahoo S, Rani S, Parveen S, Pal Singh A, Mehra A, Chakrabarti S, et al. Self-harm and COVID-19 pandemic: an emerging concern—a report of 2 cases from India. Asian J Psychiatr. (2020) 51:102104. doi: 10.1016/j.ajp.2020.102104
4. Sanchez TH, Zlotorzynska M, Rai M, Baral SD. Characterizing the impact of COVID-19 on men who have sex with men across the United States in April, 2020. AIDS Behav. (2020) 24(7):2024–32. doi: 10.1007/s10461-020-02894-2
5. Fish JN, Salerno J, Williams ND, Rinderknecht RG, Drotning KJ, Sayer L, et al. Sexual minority disparities in health and well-being as a consequence of the COVID-19 pandemic differ by sexual identity. LGBT Health. (2021) 8(4):263–72. doi: 10.1089/lgbt.2020.0489
6. Gato J, Barrientos J, Tasker F, Miscioscia M, Cerqueira-Santos E, Malmquist A, et al. Psychosocial effects of the COVID-19 pandemic and mental health among LGBTQ+ young adults: a cross-cultural comparison across six nations. J Homosex. (2021) 68(4):612–30. doi: 10.1080/00918369.2020.1868186
7. Gato J, Leal D, Seabra D. When home is not a safe haven: Effects of the COVID-19 pandemic on LGBTQ adolescents and young adults in Portugal. PSICOLOGIA. (2020) 34(2):89–100.
8. Salerno JP, Doan L, Sayer LC, Drotning KJ, Rinderknecht RG, Fish JN. Changes in mental health and well-being are associated with living arrangements with parents during COVID-19 among sexual minority young persons in the US. Psychol Sex Orientat Gend Divers. (2021). doi: 10.1037/sgd0000520
9. Hall KS, Samari G, Garbers S, Casey SE, Diallo DD, Orcutt M, et al. Centring sexual and reproductive health and justice in the global COVID-19 response. The lancet. (2020) 395(10231):1175–1177.
10. Bhalla R, Agarwal S. Life in a pandemic: intersectional approach exploring experiences of LGBTQ during COVID-19. Int J Spa Wellness. (2021) 4(1):53–68. doi: 10.1080/24721735.2021.1880204
11. European Centre for Disease Prevention and Control-ECDPC. COVID-19 global overview. Covid-19 Situation Dashboard. (2020) Retrieved from https://qap.ecdc.europa.eu/public/extensions/COVID-19/COVID-19.html.
12. Wood SM, Salas-Humara C, Dowshen NL. Human immunodeficiency virus, other sexually transmitted infections, and sexual and reproductive health in lesbian, gay, bisexual, transgender youth. Pediatr Clin North Am. (2016) 63:1027–55. doi: 10.1016/j.pcl.2016.07.006
13. Tomar A, Spadine MN, Graves-Boswell T, Wigfall LT. COVID-19 among LGBTQ + individuals living with HIV/AIDS: psycho-social challenges and care options. AIMS Public Health. (2021) 8(2):303. doi: 10.3934/publichealth.2021023
14. Banerjee D, Nair VS. “The untold side of COVID-19”: struggle and perspectives of the sexual minorities. J Psychosexual Health. (2020) 2(2):113–20. doi: 10.1177/2631831820939017
15. Beima-Sofie K, Ortblad KF, Swanson F, Graham SM, Stekler JD, Simoni JM. “Keep It Going if You Can”: HIV service provision for priority populations during the COVID-19 pandemic in Seattle, WA. AIDS and Behavior. (2020) 24:2760–3.32385679
16. Conron KJ, O’Neill K, Sears B. COVID-19 and students in higher education: A 2021 study of the impact of the COVID-19 pandemic on the educational experiences of LGBTQ and non-LGBTQ U.S. adults aged 18–40. California: The Williams Institute, UCLA (2021).
17. Salerno JP, Devadas J, Pease M, Nketia B, Fish JN. Sexual and gender minority stress amid the COVID-19 pandemic: implications for LGBTQ young persons’ mental health and well-being. Public Health Rep. (2020a) 135(6):721–7. doi: 10.1177/0033354920954511
18. Gonzales G, Loret de Mola E, Gavulic KA, McKay T, Purcell C. Mental health needs among lesbian, gay, bisexual, and transgender college students during the COVID-19 pandemic. J Adolesc Health. (2020) 67(5):645–8. doi: 10.1016/j.jadohealth.2020.08.006
19. Fish JN, McInroy LB, Paceley MS, Williams ND, Henderson S, Levine DS, et al. I'm kinda stuck at home with unsupportive parents right now: LGBTQ youths’ experiences with COVID-19 and the importance of online support. Journal of Adolescent Health. (2020) https://doi.org/10.1016/j.jadohealth.2020.06.002
20. Boyd CJ, Veliz PT, McCabe SE. Severity of DSM-5 cannabis use disorders in a nationally representative sample of sexual minorities. Subst Abus. (2020) 41:191–5. doi: 10.1080/08897077.2019.1621242
21. Krueger EA, Fish JN, Upchurch DM. Sexual orientation disparities in substance use: investigating social stress mechanisms in a national sample. Am J Prev Med. (2020) 58(1):59–68. doi: 10.1016/j.amepre.2019.08.034
23. Bourgois P, Holmes SM, Sue K, Quesada J. Structural vulnerability: Operationalizing the concept to address health disparities in clinical care. Acad. Med. (2017) 92:299–30727415443
24. Hatzenbuehler ML, McLaughlin KA, Slopen N. Sexual orientation disparities in cardiovascular biomarkers among young adults. Am J Prev Med. (2013) 44(6):612–21. doi: 10.1016/j.amepre.2013.01.027
25. Valdiserri RO, Holtgrave DR, Poteat TC, Beyrer C. Unraveling health disparities among sexual and gender minorities: a commentary on the persistent impact of stigma. J Homosex. (2019) 66(5):571–89. doi: 10.1080/00918369.2017.1422944
26. Kibrik EL, Cohen N, Stolowicz-Melman D, Levy A, Boruchovitz-Zamir R, Diamond GM. Measuring adult children’s perceptions of their parents’ acceptance and rejection of their sexual orientation: initial development of the parental acceptance and rejection of sexual orientation scale (PARSOS). J Homosex. (2018) 66(11):1513–34. doi: 10.1080/00918369.2018.1503460
27. Slemon A, Richardson C, Goodyear T, Salway T, Gadermann A, Oliffe JL, et al. Widening mental health and substance use inequities among sexual and gender minority populations: findings from a repeated cross-sectional monitoring survey during the COVID-19 pandemic in Canada. Psychiatry Res. (2022) 307:114327. doi: 10.1016/j.psychres.2021.114327
28. Bochicchio LA, Drabble LA, Riggle EDB, Munroe C, Wootton AR, Hughes TL, Understanding Alcohol and Marijuana Use among Sexual Minority Women during the COVID-19 Pandemic: A Descriptive Phenomenological Study. J. Homosex. (2021) 68:631–646.33439793
29. Bertolote JM, Fleischmann A. Suicide and psychiatric diagnosis: a worldwide perspective. World Psychiatry. (2002) 1(3):181.16946849
30. Russell ST, Joyner K. Adolescent sexual orientation and suicide risk: evidence from a national study. Am J Public Health. (2001) 91(8):1276–81. doi: 10.2105/AJPH.91.8.1276
31. Fish JN, McInroy LB, Paceley MS, Williams ND, Henderson S, Levine DS, Edsall RN. I'm kinda stuck at home with unsupportive parents right now: LGBTQ youths' experiences with COVID-19 and the importance of online support. Journal of Adolescent Health. (2020) https://doi.org/10.1016/j.jadohealth.2020.06.002.
32. Salerno JP, Devadas J, Pease M, Nketia B, Fish JN. Sexual and gender minority stress amid the COVID-19 pandemic: Implications for LGBTQ young persons’ mental health and well-being. Public Health Reports. (2020) 135(6):721–727. https://doi.org/10.1177/003335492095451133026972
33. Herrmann WJ, Oeser P, Buspavanich P, Lech S, Berger M, Gellert P. Loneliness and depressive symptoms differ by sexual orientation and gender identity during physical distancing measures in response to COVID?19 pandemic in Germany. Applied Psychology: Health and Well-Being. (2023).35666060
34. Jacmin-Park S, Rossi M, Dumont L, Lupien SJ, Juster RP. Mental health and social support of sexual and gender diverse people from Québec, Canada during the COVID-19 crisis. LGBT Health. (2022) 9(3):151–60. doi: 10.1089/lgbt.2021.0255
35. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. (2003) 129:674–97. doi: 10.1037/0033-2909.129.5.674
36. Testa RJ, Habarth J, Peta J, Balsam K, Bockting W. Development of the gender minority stress and resilience measure. Psychol Sex Orientat Gend Divers. (2015) 2(1):65. doi: 10.1037/sgd0000081
37. Frost DM, Meyer IH, Schwartz S. Social support networks among diverse sexual minority populations. Am J Orthopsychiatry. (2016) 86(1):91. doi: 10.1037/ort0000117
38. Joanna Briggs Institute. Critical appraisal tools. (2020). Available at: https://joannabriggs.org/criticalappraisal-tools (Accessed September 10, 2022).
39. Bécares L, Kneale D. Inequalities in mental health, self-rated health, and social support among sexual minority young adults during the COVID-19 pandemic: analyses from the UK millennium cohort study. Soc Psychiatry Psychiatr Epidemiol. (2022) 57:1–8. doi: 10.1007/s00127-022-02291-1
40. Chang CJ, Feinstein BA, Chu BC, Selby EA. The negative impact of COVID-19 on sexual minority young adults: demographic differences and prospective associations with depression. Psychol Sex Orientat Gend Divers. (2021) 8(2):220. doi: 10.1037/sgd0000494
41. Kamal K, Li JJ, Hahm HC, Liu CH. Psychiatric impacts of the COVID-19 global pandemic on US sexual and gender minority young adults. Psychiatry Res. (2021) 299:113855. doi: 10.1016/j.psychres.2021.113855
42. Tabler J, Schmitz RM, Charak R, Dickinson E. Perceived weight gain and eating disorder symptoms among LGBTQ + adults during the COVID-19 pandemic: a convergent mixed-method study. J Eat Disord. (2021) 9(1):1–11. doi: 10.1186/s40337-021-00470-0
43. Oren L. COVID-19 stress, minority stress, and mental health among LGB Israeli individuals. Psychol Trauma. (2022). doi: 10.1037/tra0001232
44. Akré ER, Anderson A, Stojanovski K, Chung KW, VanKim NA, Chae DH. Depression, anxiety, and alcohol use among LGBTQ+ people during the COVID-19 pandemic. Am J Public Health. (2021) 111(9):1610–9. doi: 10.2105/AJPH.2021.306394
45. Kneale D, Bécares L. Discrimination as a predictor of poor mental health among LGBTQ+ people during the COVID-19 pandemic: cross-sectional analysis of the online Queerantine study. BMJ Open. (2021) 11(6):e049405. doi: 10.1136/bmjopen-2021-049405
46. Moore SE, Wierenga KL, Prince DM, Gillani B, Mintz LJ. Disproportionate impact of the COVID-19 pandemic on perceived social support, mental health and somatic symptoms in sexual and gender minority populations. J Homosex. (2021) 68(4):577–91. doi: 10.1080/00918369.2020.1868184
47. Suen YT, Chan RC, Wong EMY. Effects of general and sexual minority-specific COVID-19-related stressors on the mental health of lesbian, gay, and bisexual people in Hong Kong. Psychiatry Res. (2020) 292:113365. doi: 10.1016/j.psychres.2020.113365
48. Urzúa A, Barrientos J, Guzmán-González M, Ulloa F. Mental health in the Chilean LGBT population in times of COVID-19. Salud Ment. (2022) 45(4):169–75. doi: 10.17711/SM.0185-3325.2022.023
49. Hart EA, Rubin A, Kline KM, Fox KR. Disordered eating across COVID-19 in LGBTQ+ young adults. Eat Behav. (2022) 44:101581. doi: 10.1016/j.eatbeh.2021.101581
50. Goodyear T, Slemon A, Richardson C, Gadermann A, Salway T, Dhari S, et al. Increases in alcohol and cannabis use associated with deteriorating mental health among LGBTQ2+ adults in the context of COVID-19: a repeated cross-sectional study in Canada, 2020–2021. Int J Environ Res Public Health. (2021) 18(22):12155. doi: 10.3390/ijerph182212155
51. Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. (2009) 114(1–3):163–73. doi: 10.1016/j.jad.2008.06.026
52. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166(10):1092–7. doi: 10.1001/archinte.166.10.1092
53. Taylor S, Landry CA, Paluszek MM, Fergus TA, McKay D, Asmundson GJ. Development and initial validation of the COVID stress scales. J Anxiety Disord. (2020) 72:102232. doi: 10.1016/j.janxdis.2020.102232
54. Moser A, Stuck AE, Silliman RA, Ganz PA, Clough-Gorr KM. The eight-item modified medical outcomes study social support survey: psychometric evaluation showed excellent performance. J Clin Epidemiol. (2012) 65(10):1107–16. doi: 10.1016/j.jclinepi.2012.04.007
55. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther. (1995) 33(3):335–43. doi: 10.1016/0005-7967(94)00075-U
56. Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. (1990) 55(3–4):610–7. doi: 10.1207/s15327752jpa5503%264_17
57. Fairburn CG, Beglin SJ. Eating disorder examination questionnaire. Cognitive behavior therapy and eating disorders, Volume 309. Guilford Press (2008). p. 313.
58. Gideon N, Hawkes N, Mond J, Saunders R, Tchanturia K, Serpell L. Development and psychometric validation of the EDE-QS, a 12 item short form of the eating disorder examination questionnaire (EDE-Q). PLoS ONE. (2016) 11(5):e0152744. doi: 10.1371/journal.pone.0152744
59. Prnjak K, Mitchison D, Griffiths S, Mond J, Gideon N, Serpell L, et al. Further development of the 12-item EDE-QS: identifying a cut-off for screening purposes. BMC Psychiatry. (2020) 20(1):1–7. doi: 10.1186/s12888-020-02565-5
60. Mohr JJ, Kendra MS. Revision and extension of a multidimensional measure of sexual minority identity: the lesbian, gay, and bisexual identity scale. J Couns Psychol. (2011) 58(2):234–45. doi: 10.1037/a0022858
61. Christensen KS, Toft T, Frostholm L, Ørnbøl E, Fink P, Olesen F. Screening for common mental disorders: who will benefit? Results from a randomised clinical trial. Fam Pract. (2005) 22(4):428–34. doi: 10.1093/fampra/cmi032
62. Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D, et al. Item banks for measuring emotional distress from the patient-reported outcomes measurement information system (PROMIS®): depression, anxiety, and anger. Assessment. (2011) 18(3):263–83. doi: 10.1177/1073191111411667
63. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behavior. (1983) 24:385–96. doi: 10.2307/2136404
64. Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D. Am J Prev Med. (1994) 10(2):77–84. doi: 10.1016/S0749-3797(18)30622-6
65. Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. (1991) 32(6):705–14. doi: 10.1016/0277-9536(91)90150-B
66. Treynor W, Gonzalez R, Nolen-Hoeksema S. Rumination reconsidered: a psychometric analysis. Cognit Ther Res. (2003) 27(3):247–59. doi: 10.1023/A:1023910315561
67. Pais-Ribeiro J, Honrado A, Leal I. Contribuição para o estudo da adaptação portuguesa das Escalas de Depressão Ansiedade Stress de Lovibond e Lovibond [Contribution to the adaptation study of the lovibond and lovibond depression, anxiety, stress scales to the Portuguese population]. Psychologica. (2004a) 36:235–46. http://hdl.handle.net/10400.12/1058
68. Cutrona CE, Russell DW. The provisions of social relationships and adaptation to stress. Adv Pers Relationsh. (1987) 1(1):37–67.
69. Henry JD, Crawford JR. The short-form version of the depression anxiety stress scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. (2005) 44(2):227–39. doi: 10.1348/014466505X29657
70. Daza P, Novy DM, Stanley MA, Averill P. The depression anxiety stress scale-21: Spanish translation and validation with a Hispanic sample. J Psychopathol Behav Assess. (2002) 24(3):195–205. doi: 10.1023/A:1016014818163
71. Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand S-LT, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. (2002) 32:959–76. doi: 10.1017/S0033291702006074
73. Ladouceur CD. COVID-19 adolescent symptom & psychological experience questionnaire. Unpublished Manuscript (2020).
74. Pierce GR, Pierce GR, Sarason IG, Sarason BR, Solky-Butzel JA, Nagle LC. Assessing the quality of personal relationships. J Soc Pers Relat. (1997) 14(3):339–56. doi: 10.1177/0265407597143004
75. Haynos AF, Fruzzetti AE. Initial evaluation of a single-item screener to assess problematic dietary restriction. Eat Weight Disord. (2015) 20(3):405–13. doi: 10.1007/s40519-014-0161-0
76. Sinclair VG, Wallston KA. The development and psychometric evaluation of the brief resilient coping scale. Assessment. (2004) 11(1):94–101. doi: 10.1177/1073191103258144
77. Centers for Disease Control and Prevention: United States COVID-19 Cases and Deaths by State. (2021). Available at: www.cdc.gov/coronavirus/2019-ncov/cases-updates/us-cases-deaths.html (Accessed September 24, 2022).
78. Kessler RC, Ormel J, Demler O, Stang PE. Comorbid mental disorders account for the role impairment of commonly occurring chronic physical disorders: results from the national comorbidity survey. J Occup Environ Med. (2003):1257–66. doi: 10.1097/01.jom.0000100000.70011.bb
79. Russell D, Peplau LA, Cutrona CE. The revised UCLA loneliness scale: concurrent and discriminant validity evidence. J Pers Soc Psychol. (1980) 39(3):472. doi: 10.1037/0022-3514.39.3.472
80. Mason TB, Lewis RJ, Winstead BA, Derlega VJ. External and internalized heterosexism among sexual minority women: the moderating roles of social constraints and collective self-esteem. Psychol Sex Orientat Gend Divers. (2015) 2(3):313–20. doi: 10.1037/sgd0000115
81. Ryan C, Russell ST, Huebner D, Diaz R, Sanchez J. Family acceptance in adolescence and the health of LGBT young adults. J Child Adolesc Psychiatr Nurs. (2010) 23(4):205–13. doi: 10.1111/j.1744-6171.2010.00246.x
82. Baams L, De Luca SM, Brownson C. Use of mental health services among college students by sexual orientation. LGBT Health. (2018) 5(7):421–30. doi: 10.1089/lgbt.2017.0225
83. Hatzenbuehler ML, Nolen-Hoeksema S, Dovidio J. How does stigma “get under the skin”?: The mediating role of emotion regulation. Psychol. Sci. (2009) 20:1282–1289.19765237
84. Holmes A. Marching with pride? Debates on uniformed police participating in Vancouver’s LGBTQ pride parade. J Homosex. (2021) 68(8):1320–52. doi: 10.1080/00918369.2019.1696107
85. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395I(10227):912–20. doi: 10.1016/S0140-6736(20)30460-8
86. Pearl RL. Weight stigma and the “quarantine-15.”. Obesity. (2020) 28(7):1180–1. doi: 10.1002/oby.22850
87. Puhl RM, Lessard LM, Larson N, Eisenberg ME, Neumark-Stzainer D. Weight stigma as a predictor of distress and maladaptive eating behaviors during COVID-19: longitudinal fndings from the EAT study. Annals Behav Med. (2020) 54(10):738–46. doi: 10.1093/abm/kaaa077
88. Watson RJ, Adjei J, Saewyc E, Homma Y, Goodenow C. Trends and disparities in disordered eating among heterosexual and sexual minority adolescents. Int J Eat Disord. (2017) 50(1):22–31. doi: 10.1002/eat.22576
89. Mensinger JL, Granche JL, Cox SA, Henretty JR. Sexual and gender minority individuals report higher rates of abuse and more severe eating disorder symptoms than cisgender heterosexual individuals at admission to eating disorder treatment. Int J Eat Disord. (2020) 53(4):541–54. doi: 10.1002/eat.23257
90. Watson RJ, Veale JF, Saewyc EM. Disordered eating behaviors among transgender youth: probability profles from risk and protective factors. Int J Eat Disord. (2017) 50(5):515–22. doi: 10.1002/eat.22627
91. Greenwood GL, Gruskin EP. LGBT Tobacco and alcohol disparities. In: Meyer IH, Northridge ME, editors. The health of sexual minorities. Boston, MA, United States: Springer (2007). p. 566–83.
92. McCabe SE, Hughes TL, Bostwick WB, West BT, Boyd CJ. Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction. (2009) 104:1333–45. doi: 10.1111/j.1360-0443.2009.02596.x
93. Roxburgh A, Lea T, de Wit J, Degenhardt L. Sexual identity and prevalence of alcohol and other drug use among Australians in the general population. Int J Drug Policy. (2016) 28:76–82. doi: 10.1016/j.drugpo.2015.11.005
94. Canadian Centre on Substance Use and Addiction. COVID-19, alcohol cannabis use. Ottawa, ON, Canada: Canadian Centre on Substance Use and Addiction (2020). p. 1–5.
95. Pacek LR, Martins SS, Crum RM. The bidirectional relationships between alcohol, cannabis, co-occurring alcohol and cannabis use disorders with major depressive disorder: results from a national sample. J Affect Disord. (2013) 148:188–95. doi: 10.1016/j.jad.2012.11.059
96. Gibson B, Schneider J, Talamonti D, Forshaw M. The impact of inequality on mental health outcomes during the COVID-19 pandemic: a systematic review. Can Psychol. (2021) 62(1):101. doi: 10.1037/cap0000272
97. Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. (2020) 89:531–42. doi: 10.1016/j.bbi.2020.05.048
98. Elharake JA, Akbar F, Malik AA, Gilliam W, Omer SB. Mental health impact of COVID-19 among children and college students: a systematic review. Child Psychiatry Hum Dev. (2022):1–13. 10.1007/s10578-021-01297-135013847
99. Garg I, Hanif H, Javed N, Abbas R, Mirza S, Javaid MA, et al. COVID-19 vaccine hesitancy in the LGBTQ+ population: a systematic review. Infect Dis Rep. (2021) 13(4):872–87. doi: 10.3390/idr13040079
100. McGowan VJ, Lowther HJ, Meads C. Life under COVID-19 for LGBT+ people in the UK: systematic review of UK research on the impact of COVID-19 on sexual and gender minority populations. BMJ Open. (2021) 11(7):e050092. doi: 10.1136/bmjopen-2021-050092
101. Bochicchio LA, Drabble LA, Riggle ED, Munroe C, Wootton AR, Hughes TL. Understanding alcohol and marijuana use among sexual minority women during the COVID-19 pandemic: a descriptive phenomenological study. J Homosex. (2021) 68(4):631–46. doi: 10.1080/00918369.2020.1868187
102. Bochicchio L, Reeder K, Ivanoff A, Pope H, Stefancic A. Psychotherapeutic interventions for LGBTQ+ youth: a systematic review. J LGBT Youth. (2022) 19(2):152–79. doi: 10.1080/19361653.2020.1766393
Keywords: Sexual and gender minority (LGBTQ) populations issues, LGBTQ+, depression, anxiety, COVID-19 pandemic, stress
Citation: Datta S and Mukherjee T (2023) Impact of COVID-19 stress on the psychological health of sexual & gender minority individuals: A systematic review. Front. Glob. Womens Health 4:1132768. doi: 10.3389/fgwh.2023.1132768
Received: 27 December 2022; Accepted: 28 February 2023;
Published: 29 March 2023.
Edited by:
Maureen Edwards, Montgomery College, United StatesReviewed by:
Kelly Melekis, University of Vermont, United StatesSwapnajeet Sahoo, Post Graduate Institute of Medical Education and Research (PGIMER), India
© 2023 Datta and Mukherjee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sumona Datta c3Vtb25hZGF0dGEucHN5Y2hAZ21haWwuY29t
Specialty Section: This article was submitted to Women’s Mental Health, a section of the journal Frontiers in Global Women’s Health
 Sumona Datta
Sumona Datta Tilottama Mukherjee
Tilottama Mukherjee