
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Glob. Womens Health, 17 August 2023
Sec. Maternal Health
Volume 4 - 2023 | https://doi.org/10.3389/fgwh.2023.1131626
This article is part of the Research TopicBirth Experiences and Their Relation to Postnatal Mental Health and Breastfeeding. What Are the Problems? How Can We Improve?View all 5 articles
 Mickiale Hailu1*
Mickiale Hailu1* Aminu Mohammed1
Aminu Mohammed1 Yitagesu Sintayehu1
Yitagesu Sintayehu1 Daniel Tadesse1
Daniel Tadesse1 Legesse Abera1
Legesse Abera1 Neil Abdurashid1
Neil Abdurashid1 Milkiyas Solomon1
Milkiyas Solomon1 Momina Ali1
Momina Ali1 Dawit Mellese1
Dawit Mellese1 Tadesse Weldeamaniel1
Tadesse Weldeamaniel1 Teshale Mengesha1
Teshale Mengesha1 Tekelebirhan Hailemariyam1
Tekelebirhan Hailemariyam1 Sewmehon Amsalu1
Sewmehon Amsalu1 Yesuneh Dejene2
Yesuneh Dejene2 Meklit Girma3
Meklit Girma3
Background: Cultural practices are any experiences or beliefs that are socially shared views and behaviors practiced in a certain society at a certain time. Cultural malpractices are defined as socially shared views and traditionally accepted behaviors experienced in a certain society that harm maternal health. Worldwide, the period of pregnancy, labor, and delivery is embedded with different beliefs, customs, and rituals in different societies that contribute a lot to maternal death. They are responsible for the annual deaths of 303,000 mothers and 2.7 million newborns globally. In developing countries, it accounts for approximately 5%–15% of maternal deaths. In Ethiopia, approximately 18% of infant deaths occur due to cultural malpractice, and 52% of pregnant mothers give birth at home following cultural customs in Dire Dawa city. The objective of this study was to assess cultural malpractices during pregnancy, childbirth, and the postnatal period and its associated factors among women who gave birth once in Dire Dawa City in 2021.
Methods: Community-based mixed study was conducted. A total of 624 study participants were selected through a systematic random sampling technique, and a purposive sampling method was used for qualitative data. The study was conducted in the randomly selected Kebeles of Dire Dawa City, Eastern Ethiopia, from November 1 to December 30, 2021. Data were entered into Epi Data version 4.1 and exported to SPSS version 24 for analysis. Bivariate and multivariate analyses were done, and the degree of association was measured by using the odds ratio with 95% CI and significance was declared at a p-value of <0.05. The qualitative data were analyzed thematically using ATLAS-ti version 7.
Results: The overall prevalence of cultural malpractice during pregnancy, childbirth, and the postnatal period was 74.6% [95% CI: 70.59%, 77.49%]. Women over the age of 35 were two times more likely [AOR 2.61, 95% CI, 1.45–4.72] to commit cultural malpractice than women aged 15–24 and 25–34. Those with no antenatal care (ANC) follow-up were three times more likely to commit cultural malpractice [AOR 3.57, 95% CI, 1.72–7.40], those who were absent from health education were nearly two times more likely to commit cultural malpractice [AOR 1.83, 95%CI, 1.25–2.67], and women whose culture allows harmful traditional practices were nearly two times more likely to commit cultural malpractices than their counterparts [AOR 1.69, 95%CI, 1.29–2.54].
Conclusion: In this study, nearly three-fourths of participants were involved in cultural malpractices. Therefore, strengthening community education and behavioral change messages on the importance of ANC and avoiding unhealthy care during pregnancy, childbirth, postnatal and neonatal periods, especially with pregnancy at old age (age > 35), may help to reduce cultural malpractices.
Cultural practices are any experiences or beliefs that are socially shared views and behaviors practiced in a certain society at a certain time. Cultural malpractices (CMPs) are defined as socially shared views and traditionally accepted behaviors experienced in a certain society that harm maternal health. Worldwide, the period of pregnancy, labor, and delivery is embedded with different beliefs, customs, and rituals in different societies that contribute a lot to maternal death. The majority of the time, those CMPs are largely carried out without the consent of the child/woman (1–4).
Globally, approximately 78 million newborns waited more than 1 h to breastfeed, and two out of five newborns were excluded from colostrum feeding. This figure translates every day to approximately 4,000 infants and young children dying due to colostrum avoidance and the introduction of pre-lacteal feeds, which are part of cultural malpractices. In general, cultural malpractices during pregnancy, delivery, and the postnatal period killed 303,000 mothers and 2.7 million newborns each year (5–7).
The World Medicine Situation report estimates that between 70% and 95% of the population in developing countries and more than 80% of the population in Africa participate in cultural malpractices during pregnancy (8, 9). The World health organization has identified sepsis as the major cause of maternal deaths in sub-Saharan Africa, which accounts for approximately 11% of maternal deaths (10).
Many mothers suffer from infection of the reproductive tract and neonatal sepsis as a result of an unsanitary environment and inadequate care during pregnancy and delivery, with infants improperly delivered by unskilled birth attendants, and/or traditional delivery practices being the leading cause of sepsis and death. The actual incidence of cultural malpractices in developing countries accounts for approximately 5%–15% of maternal deaths (9–11).
The Ethiopian government and other concerned bodies have made some efforts to combat CMPs in different parts of Ethiopia. For example, extensive health education toward the eradication of the identified cultural malpractices was delivered to society via health extension workers, and a regular health education program was provided at health facilities and community levels. In addition to that, the National Constitutional, Criminal and Family laws, Education, Health, Population, and Cultural policies of Ethiopia included articles that directly or indirectly combat CMPs. However, deep-rooted beliefs, customs, rational attitudes, lack of knowledge, and being unaware of the effects of the practices help to maintain these problems (12, 13).
In Ethiopia, more than half of pregnant mothers give birth at home and follow the cultural birth customs. Approximately 18% of infant deaths occur due to cultural malpractices during the postnatal period. According to the Ethiopian Ministry of Women, Children, and Youth Affairs report, there are various forms of CMPs against women and children, which are widely practiced in Ethiopia. But the types and prevalence of those practices vary among regions, cultural settings, and religious values. So routine assessment and investigation of CMPs are mandatory (12–14).
As seen in other parts of Ethiopia, in Dire Dawa town and around, there may be different cultural practices that are practiced during pregnancy and childbirth, but there is no data that clearly indicates the types and prevalence of cultural malpractice and their influencing factors; however, it is known that 52% of pregnant mothers give birth at home following cultural customs (15). Even though few studies have been conducted regarding cultural malpractices during pregnancy, labor, and the postpartum period, some factors like family, social, and health system factors have not been assessed yet. So, the purpose of this study was to assess the magnitude of cultural malpractices during pregnancy, childbirth, and postpartum and its associated factors among women who gave birth once in Dire Dawa city administration.
Dire Dawa town is one of the federal city administrations in Ethiopia, which is located at a distance of 515 kilometers from Addis Ababa (the capital city) to the east. The city administration has 9 urban and 38 rural kebeles (the smallest administrative division and sometimes also called tabia or tabiya. They are at the neighborhood level and are the primary contact for most citizens living in Ethiopia). The Ethnic groups in the region include the Oromo (46%), Somali (24%), Amhara (20%), Gurage (15,543, 4.5%), and other groups (5.5%). The total fertility rate and urban unemployment rate of the city are 3.4 children per woman and 25.3%, respectively. The literacy rate for women is 50.8% and 78.6% for men.
There are 2 government hospitals, 5 private hospitals, 15 health centers, and 33 health posts. The current metro area population is 426,129, of which 49.8% of them are men and 50.2% are women. The total number of women in the reproductive age group (15–49 years) is 506,637, which accounts for 15.4% of the total population (16). A community-based quantitative cross-sectional study complemented by a qualitative study was conducted from November 1 to December 30, 2021.
The source populations were all women who had at least one history of delivery in Dire Dawa city administration, and the study populations were systematically selected women who had experienced at least one history of delivery at the selected kebeles in Dire Dawa city administration during the study period. The study included women aged 18 to 49 who had given birth at least once in the previous 5 years and had stayed in the kebele for more than 6 months. Women who were in the immediate postpartum period and women who had chronic medical illnesses were excluded from the study.
The sample size for the quantitative part was calculated by using the single population proportion formula with the assumption of n = sample size required for the study, Zα/2 = 1.96, which is the standardized normal distribution curve value for the 95% CI, p = 0.383 (9), and d = 0.04, which is the degree of freedom or margin of error.
A total of 20 individual participants (5 Key informants (KIs) and 15 In-depth interviews (IDI) were planned to be involved in this study, but the final sample size was determined by data saturation.
The Dire Dawa City administration has 9 urban and 38 rural kebeles. Using the random sampling method, five kebeles were selected. Then, based on the total number of women aged 18 to 49 who had given birth at least once in the previous 5 years in each selected kebeles, the sample size was proportionally allocated to each selected kebeles. Individual participants in each kebele were selected using a systematic random sampling technique by considering their house number as a sampling frame. The desired sampling interval was calculated using the two-month delivery reports of each health facility in each kebele (977/624 = 2). The first participant was selected by lottery. The subsequent units were selected at fixed intervals with a skip interval of k = 2.
First, the questionnaires were adopted from previous studies and were prepared in Afan Oromo, Somali, and Amharic versions. A total of five midwives with BSc were recruited for the community-based data collection, and face masks were given to the women during the process of data collection.
Qualitative data was collected through in-depth interviews and key informant interviews using semi-structured questions. A total of two midwives with BSc who have experience in qualitative data collection were recruited for data collection. A purposive sampling technique was used for the qualitative study. Women who have experienced cultural malpractices were selected for IDI. The KIs for this study were religious and community leaders. The principal investigator was moderating IDI and KI interviews and was assisted by an experienced notetaker. After the notetaker and the interviewer introduce themselves, the participants were informed about the purpose of the study and the confidentiality of the data, and probing questions were forwarded to the participants. All interviews were tape-recorded and transcribed in full text.
Cultural malpractices during pregnancy, childbirth, and the postnatal period: Involvement in one or more cultural practices during pregnancy, labor, and postpartum that the Ethiopian Ministry of Women, Children, and Youth Affairs classifies as harmful cultural malpractice (14).
For quantitative data collection, before the actual data collection, data collectors obtained two-day training about the aim of the study and the content of the instrument. A pretest was done in Dire Dawa city administration (non-selected kebeles) on 5% of the sample size. For qualitative data collection, open-ended questions were used to avoid acquiescence bias, and proper training was given to the data collector regarding how to take keynotes and record using a tape recorder. For consistency and possible modification, a pre-test was done on one key note, and in-depth interviews were conducted in Dire Dawa city administration (non-selected kebeles). The recorded data was transcribed by experts. The key informant and in-depth interviews were conducted in a silent place.
The quantitative part was entered after the data collection into Epi Data version 4.1, and the data was exported to SPSS version 24 for analysis. First descriptive analysis was done, and then, bivariate analysis was done. In multivariate logistic regression analysis, a variable with a p-value <0.2 in bivariate logistic regression analysis was entered, and the point degree of association was declared at a p-value of 0.05. An odds ratio with a 95% confidence interval was used to measure the degree of association between those significant independent variables and cultural malpractices practiced during pregnancy, childbirth, and the postnatal period. The dependent variable was classified as a dummy variable. The model fit was checked by the Hosmer and Lemeshow Test, which is the most reliable test of model fit available in SPSS. Hence, the chi-square value for the Hosmer-Lemeshow test is 4.024 with a significance level of 0.74. This value is greater than 0.05, therefore indicating the goodness of model fit. A Multicollinearity test was also done to assess how much the variance of an estimated regression coefficient increases if the predictors are correlated. All values of the variance inflation factor were less than two (a maximum of 1.309 and a minimum value of 1.073). All values of the tolerance test were also above 0.2 (a maximum of 0.954 and a minimum value of 0.764). These values show that there was no problem with multicollinearity in this study. The results are presented in the form of narrations, tables, and graphs.
The data was analyzed thematically using computer-assisted qualitative data analysis software ATLAS-ti version 7. The transcribed data was entered into the software, and similar ideas were organized together to create codes. Then, themes were derived from the codes in the transcribed data and translated into an English version by language experts. Their inductive meaning was extracted using the verbatim of the participants. Then, the final report was developed using the narrative analysis method.
A total of 624 women who had experienced at least one history of delivery found in the selected kebeles of Dire Dawa city were included in the study, and the response rate was 100%.
Regarding the socio-demographic characteristics of the respondents, 305 (48.9%) were in the age group of 25–34. The majority of them were from urban areas (471 or 75.5%) and married (527 or 98.7%) by residence and marital status, respectively. Out of the 624 participants, the majority of them (314 or 50.3%) had completed secondary education and above, followed by primary education (187 or 30%). Concerning the average monthly income, the majority of the participants (457 or 73.2%) had less than 1,500 Ethiopian Birr (Table 1).

Table 1. A socio-demographic characteristic of respondents to assess the prevalence of cultural malpractice during pregnancy, childbirth, and the postnatal period among women who gave birth once in Dire Dawa city in 2021 (N = 624).
Concerning the obstetrical characteristics of study participants, 525 (84.1%) of the participants were not pregnant during the study period, and 519 (83.2%) of the participants had received antenatal care follow-up (ANC) during the last pregnancy. Among those who had received ANC follow-up during the last pregnancy, 388 (62.2%) of the participants had attended three to four ANC visits. Regarding the post-natal care and place of delivery of study participants during the last pregnancy, 433 (70%) of the participants had post-natal care follow-up (PNC) and 528 (84.6%) of the participants gave birth in a health facility (Table 2).
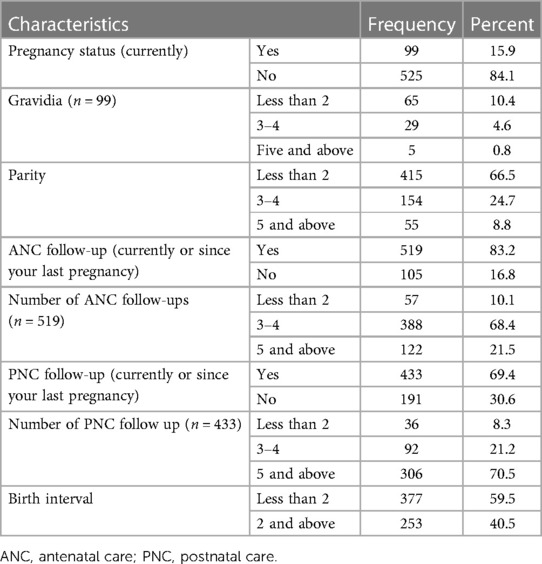
Table 2. Obstetrics characteristics of respondents to assess the prevalence of cultural malpractice during pregnancy, childbirth, and the postnatal period among women who gave birth once in Dire Dawa city in 2021 (N = 624).
Out of the 624 respondents, 74.4% [95% CI: 70.59%, 77.49%] of the pregnant women were involved in cultural malpractices during their pregnancy, childbirth, and the postnatal period (Figure 1).
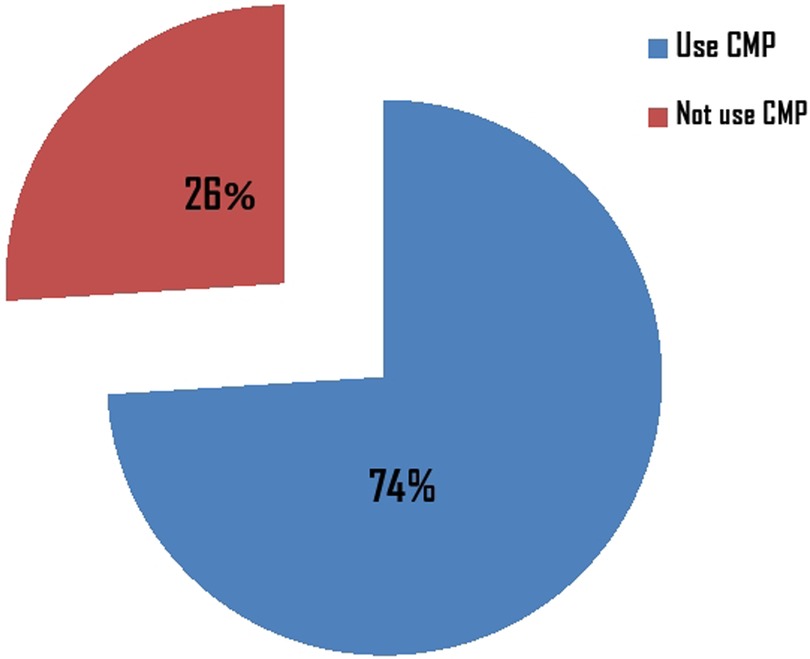
Figure 1. The overall prevalence of cultural malpractices during pregnancy, childbirth, and the postnatal period among women who gave birth once in Dire Dawa city in 2021 (N = 624). *CMP, cultural malpractice.
In this study, 318 (51.1%) participants reported that they undertook some form of harmful cultural practices during the perinatal period. Regarding food taboos, 50 (8%) of the participants had consumed food taboos (Figure 2). On the other hand, 287 (46%) had drunk telba during their pregnancy, and approximately 30 (4.8%) of them had practiced abdominal massage (Table 3).
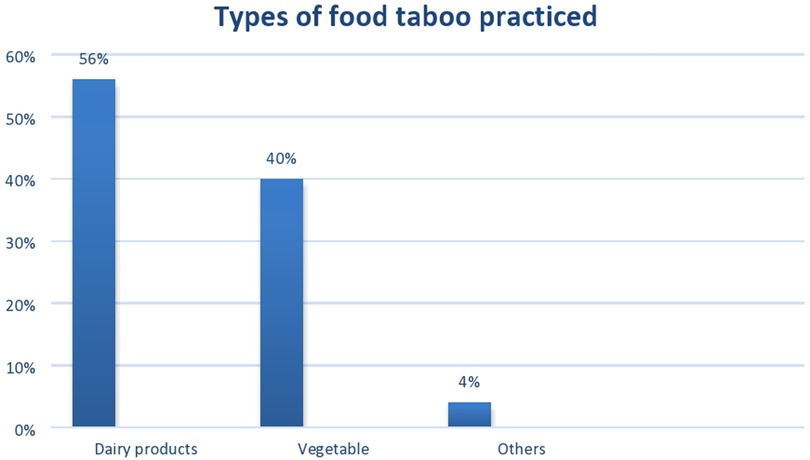
Figure 2. Types of food taboos practiced by women who gave birth once during the pregnancy period in dire dawa city in 2021 (N = 624).
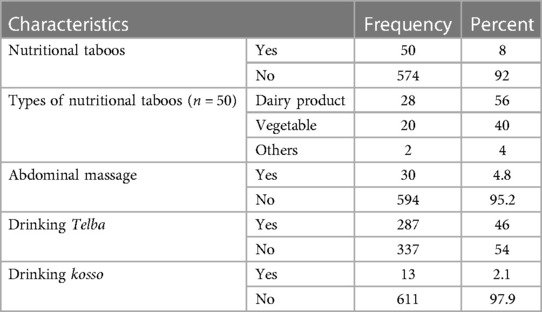
Table 3. Cultural malpractices during the pregnancy period among women who gave birth once in Dire Dawa city in 2021 (N = 624).
In terms of birthplace, 96 (15.4%) of the participants had home delivery. Regarding umbilical cord care, 63 (65.6%) respondents used an unclean blade to cut the umbilical cord, and 89 (92.7%) of them used unclean thread to tie the umbilical cord. On the other hand, 44 (45.8%) of the mothers wash their babies before 24 h and 23 (23.9%) of the respondents wash their babies after 24 h (Table 4).
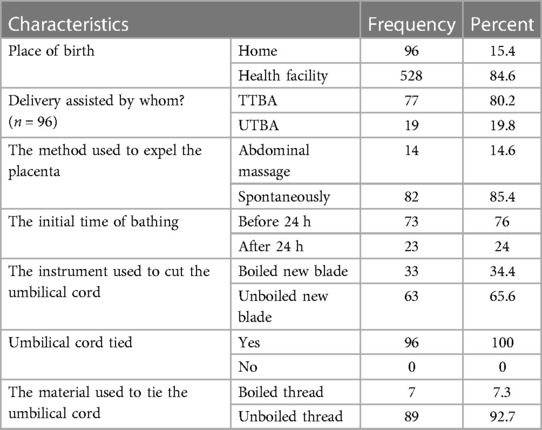
Table 4. Cultural malpractices during childbirth among women who gave birth once in Dire Dawa city in 2021 (N = 624).
In this study, 259 (41.5%) had been involved in cultural malpractices during their postnatal period. Among these, 131 (21%) of them had applied traditional medicine to the neonate's umbilicus, 89 (67.9%) of the participants applied butter, and 40 (30.5%) of them applied vaseline or zeyit to the neonates’ umbilicus during the postnatal period (Table 5).
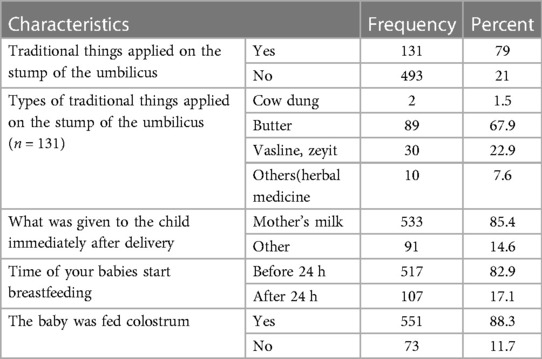
Table 5. Cultural malpractices during the postnatal period among women who gave birth once in Dire Dawa city in 2021 (N = 624).
Regarding the health system and social-related characteristics, 173 (27.7%) of the participants responded that the maternal and child health service was not accessible, and 377 (60.4%) of the participants reported the absence of home-to-home education. Regarding the culture of the participants, 259 (41.5%) of the participants reported that their culture permits those harmful traditional practices (Table 6).
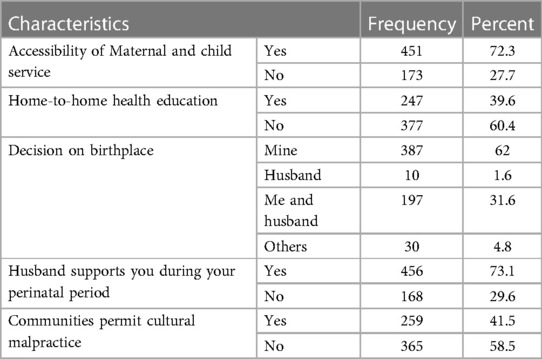
Table 6. Health system and social-related characteristics of respondents to assess the prevalence of cultural malpractices during pregnancy, childbirth, and the postnatal period among women who gave birth once in Dire Dawa city in 2021 (N = 624).
In this study, the age of study participants was significantly associated with cultural malpractices during the perinatal period. The odds of cultural malpractices during the perinatal period were two [AOR 2.61, 95%CI, 1.45–4.72] times higher in women ages 35 and above than in women within the age categories of 15–24 and 25–34.
This study also revealed that ANC follow-up was significantly associated with cultural malpractices during the perinatal period. Participants who had not attended ANC follow-up during the last pregnancy were three [AOR 3.57, 95%CI, 1.72–7.40] times more likely to commit cultural malpractices during the perinatal period than their counterparts.
Home-to-home education was another factor that was significantly associated with cultural malpractices during the perinatal period in the study area. Women who did not have home-to-home education were almost two [AOR 1.83, 95%CI, 1.25–2.67] times more likely to commit cultural malpractices than their counterparts.
Lastly, community culture was significantly associated with cultural malpractices during the perinatal period in the study area. Women whose culture (community) permits or allows harmful traditional practices were almost two [AOR 1.69, 95%CI, 1.29–2.54] times more likely to perform cultural malpractices than their counterparts (Table 7).

Table 7. Results of bivariate and multivariate analyses for assessment of cultural malpractice during pregnancy, childbirth, and the postnatal period and its associated factors among women who gave birth once in Dire Dawa city in 2021 (N = 624).
A total of 14 participants participated in 11 in-depth interviews and three key informant interviews. The in-depth interview participants comprised 11 women who had histories of giving birth, and the key informant interviews included community and religious leaders. The participants represented a wide age range (19–55 years); most did not attend formal education, and participants were enrolled in farming and were housewives.
From the qualitative analysis of data, four major themes were derived. Participants were interviewed and socio-demographic characteristics, experience of cultural malpractices, types and reasons for cultural malpractices, and availability of health education were discussed. While the themes were reported as being discrete, there was considerable overlap among them. Furthermore, participants' responses to interview questions often addressed more than one theme. In those cases, the interview data were described where they appear to fit most logically.
The period of labor and delivery is embedded with different beliefs, customs, and rituals in different societies that contribute a lot to maternal death. Major cultural malpractices during pregnancy, childbirth, and the postnatal period stated by participants were drinking telba, prohibiting food, using different herbs, and avoiding colostrum. The experience stated by two participants can be read as:
“During my last period of my pregnancy, my grandmother and my husband advised me to take telba because they told me that it facilitate labor and make my labor easily and short. I have also observed many pregnant mothers in our area while they take telba. I took it starting 7 month up to my labor started”. [sic] (A 32-year-old in-depth interview participant woman).
“In the past three my pregnancies, I have not take meat and egg. Because in our culture meat and egg are not advisable because they may make the baby big and may make my labor difficult”.[sic] (A 37-year-old in-depth interview participant woman).
Participants describe that cultural beliefs and practices can markedly influence a woman's pregnancy and childbirth experiences and may shape her mothering behavior. In addition, dietary intake before and during pregnancy and through lactation is often influenced by cultural beliefs and practices. The majority of the study participants held the view that the existence of traditional practices and beliefs about food held as taboos are inherent in the community. They stated that the reasons for their practice of cultural malpractices are from cultural influences. Plenty of cultural malpractices directly or indirectly have an impact on the health of the mother and her baby like pre-lacteal feeding, avoidance of colostrum, and restriction of certain food types. One of the participants states her experiences as follows:
“… Our community strongly believes in culture. Sometimes it may be difficult to be out of the culture of the community. If you fail to do the cultural practice you may have many influences from your friends, families, sometimes you may be discriminated from the society”. [sic] (A 47-year-old Key informant interview participant).
One of the focus of the study is maternal education and women's empowerment. Participants reveal that there is not much home-to-home health education even at health centers during ANC and PNC. The participants state their experience as follows:
“….Majority of the time, the health extension comes here for vaccination or registration or for other issue. They does not provide any health education; sometimes they may cone after long period of time. Personally, I believe that the government should provide periodic and regular education on the risks and complications of those harmful cultural practices”. [sic] (A 51-year-old in-depth interview participant woman).
“……In the past 4 of my pregnancy, I have been attended ANC and PNC follow-up. During my ANC follow-up, the ANC room were much crowed and the health professionals are also very busy. They take same sample and do some measurement around my abdomen. Sometimes they may give me some medication. This is a routine experience; they don’t have any time to provide education regarding the CMP”. [sic] (A 45-year-old in-depth interview participant woman).
The result of the study revealed that the prevalence of cultural malpractices during pregnancy, childbirth, and the postnatal period was 74% [95% CI: 70.59%, 77.49%]. This finding was comparable with studies done in Southern Ethiopia (71.4%) (17), North Karnataka, India (74.5%) (18), Zambia (74.9%) (11), and Cross River State, Nigeria (77.4%) (19). However, the result of this finding was lower than studies done in African women and the Diasporas (79.9%) (8), Turkey (84.5%) (2), Aksum (87.8%) (12), and KwaZulu-Natal, South Africa (79%) (20). It was also higher than studies done in Meshenti (50.9%) (13), Gozamen district (31.2%) (21), and Mizan Aman (35.5%) (7). These findings may differ due to differences in method, study settings, socio-demographic characteristics of study participants, and the availability and accessibility of health service infrastructures.
In this study, women aged 35 and above were more likely to be involved in cultural malpractices during the perinatal period than women aged 15–24 and 25–34. This finding was similar to studies conducted in Mizan aman (7), Gozamen district (21), Southern Ethiopia (17), Nepal (22), Turkey (23), and Nigeria (19). The reason could be that elderly mothers have accepted it as a cultural practice from the past generation.
This study also revealed that participants who had not attended ANC follow-up during their last pregnancy were more likely to be involved in cultural malpractices during the perinatal period than their counterparts. This finding is in agreement with studies conducted in Southern Ethiopia (17), North West Ethiopia (24), Gozamen district (22), Western Region of Ghana (25), Awi zone (26), and Aksum (27). The possible justification for this could be that women who have visited a health facility for an ANC service will have an awareness of the risks and complications of CMP. However, this result was inconsistent with a study done in Turkey (24). This variation might be due to a difference in the availability and accessibility of the health service infrastructure.
Home-to-home health education was another factor that was significantly associated with cultural malpractices during the perinatal period in the study area. Women who did not have home-to-home education were more engaged in cultural malpractices during the perinatal period than their counterparts. This finding was also supported by the qualitative results.
“……In the past 4 of my pregnancy, I have been attended ANC and PNC follow-up. During my ANC follow-up, the ANC room were much crowed and the health professionals are also very busy. They take same sample and do some measurement around my abdomen. Sometimes they may give me some medication. This is a routine experience; they don’t have any time to provide education regarding the CMP”. [sic] (A 45-year-old in-depth interview participant woman).
“…..The majority of the time, the health extension comes here for vaccination or registration or for other issues. They do not provide any health education. Sometimes they may return after a long period of time. Personally, I believe that the government should provide periodic and regular education on the risks and complications of those harmful cultural practices”. [sic] (a 51-year-old in-depth interview participant woman).
This finding was consistent with studies conducted in Southern Ethiopia (17), Mizan Aman (7), Raya Kobo (28), the UNICEF report (29), Asia (30), and the United Kingdom (31). The possible reason could be due to the fact that health education is an empowerment tool that not only makes knowledge and information about CMP available but also provides enlightenment as to what courses of action can be taken against CMP. However, this result was inconsistent with a study done in South Africa (21). This variation could be attributed to differences in the study participants' healthcare systems and socio-demographic characteristics.
Lastly, women whose culture (community) permits or allows harmful traditional practices were more engaged in cultural malpractices during the perinatal period than their counterparts.
This finding was also supported by the qualitative results.
“… Our community strongly believes in culture. It can be difficult to be outside of the community's culture at times. If you do not participate in the cultural practice, your friends and family may influence you, and you may face discrimination from society”. [sic] (A 47-year-old key informant interviewed participants).
This finding was supported by West Gijam (32), Shey Bench (33), Mizan Aman (7), Asia (30), Mbombela City (34), Northern Ghana (35), and Zambia (11). The plausible reason could be that pregnant mothers may be exposed to harmful cultural malpractices because culture has such close attachments to the day-to-day life of a certain society. However, this result was inconsistent with a study done in Australia (2). This demarcation may be attributed to the difference in the socio-economic status of study participants.
As there are few studies conducted on CMPs, this study might have an implication for further research on CMPs and related topics because it can be used as baseline data. It might also have an implication for maternal and child healthcare; by identifying the gaps, it helps to improve quality of care and reduce maternal and child mortality and morbidity.
Despite the fact that well-trained data collectors have been assigned, recall bias may be a concern among mothers with a child less than 12 months before the study to remember what happened to that child's feeding. This was minimized by probing the respondents about the event. Due to the cross-sectional nature of this study, establishing a true cause-and-effect relationship between harmful cultural practices and associated factors would be impossible.
In this study, nearly three-fourths of the study participants were involved in cultural malpractices during the perinatal period. Generally, these findings were almost all higher than other recent studies conducted in Ethiopia so far. Being older than 35, ANC follow-up, home-to-home health education, and the culture of the community were significantly associated with cultural malpractices during the perinatal period.
The Federal Ministry of Health might come up with policies that strengthen community education and behavioral change messages to minimize unhealthy care during pregnancy, childbirth, and the postnatal and neonatal periods, especially with pregnancy at old age (age > 35). Health facilities should provide health education programs that target addressing the major reasons that push mothers to participate in such harmful traditional practices and to increase their maternal and child health (MCH) service utilization, especially ANC. Primary healthcare workers should take an active role in the importance of MCH services during the ANC and PNC follow-ups. Lastly, we would like to recommend that other researchers conduct other study designs for better results.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethical clearance was obtained from the Institutional Review Board of Dire Dawa University. An official letter from the Research and Academic Directorate office of Dire Dawa University was submitted to the Dire Dawa Health Bureau. The selected kebeles were then given a letter of permission from the Dire Dawa Health Bureau. Voluntary informed written consent was obtained from the study participant’s right after the objectives of the study were explained to the study participants and confidentiality of the study participants was assured throughout the study period. Participants were informed that they have the right to terminate the discussion (interview) or they can’t answer any questions they didn’t want to answer.
All authors contributed significantly to the work reported, whether in the conception, study design, execution, data acquisition, analysis, and interpretation, or in all of these areas: participating in drafting, revising, or critically reviewing the article; giving final approval of the version to be published; agreeing on the journal to which the article was submitted; and agreeing to be accountable for all aspects of the work. All authors contributed to the article and approved the submitted version.
This work has been funded by Dire Dawa University for data collection purposes. The Dire Dawa University College of Medicine and Health Sciences was involved in the project through monitoring and evaluation of the work from the beginning to the result submission. However, this organization was not involved in the design, analysis, critical review of its intellectual content, or manuscript preparation, and its budget did not include publication.
We are very grateful to Dire Dawa University for the financial support for this study and to the College of Medicine and Health for its monitoring. We thank all study participants for their willingness to respond to our questionnaire.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Melesse MF, Bitewa YB, Dessie KN, Wondim DB, Bereka TM. Cultural malpractices during labor/delivery and associated factors among women who had at least one history of delivery in selected zones of Amhara region, north west Ethiopia. BMC Pregnancy Childbirth. (2021) 21:504. doi: 10.1186/s12884-021-03971-7
2. Frese M. Cultural practices, norms, and values. J Cross Cultural Psychol. (2015) 46:1–2. doi: 10.1177/0022022115600267
3. Sychareun V. Cultural beliefs and traditional rituals about child birth practices in Lao PDR. Kuala Lumpur: The Asian-Pacific Resource & Research Centre for Women (ARROW) (2009).
4. Chand SB. Cultural beliefs and traditional rituals about child birth practice in rural, Nepal. MOJ Public Health. (2016) 5(1):196–8. doi: 10.15406/mojph.2016.04.00106
5. Zenebe K, Alem H, Merga A, Abate G, Taha H, Melese M, et al. Prevalence of cultural malpractice and associated factors among women attending MCH clinic at debretabor governmental health institutions south Gondar, Amhara region, north west Ethiopia. Gynecol Obstet. (2015) 6(4):371. doi: 10.4172/2161-0932.1000371
6. Turner C, Pol S, Suon K, Neou L, Day N, Parker M, et al. Beliefs and practices during pregnancy, post-partum and in the first days of an infant's life in rural Cambodia. BMC Pregnancy Childbirth. (2017) 17:116. doi: 10.1186/s12884-017-1305-9
7. Muluken A. Determinants of early days of newborn feeding malpractice among mothers of children less than one year of age in Mizan-Aman town, southwestern Ethiopia. Pediatric Health Med Ther Dovepress. (2020) 12:79–89. doi: 10.2147/PHMT.S297828
8. Zewdneh S, Tinashe D, Caroline A. The use of traditional medicine in maternity care among African women in Africa and the diaspora: a systematic review. BMC Complement Altern Med. (2017) 17:382. doi: 10.1186/s12906-017-1886-x
9. Tadesse N, Andualem H. Cultural malpractices during pregnancy, child birth and postnatal period among women of child bearing age in Limmu Genet town, southwest Ethiopia. Sci J Public Health. (2015) 3(5):752–6. doi: 10.11648/j.sjph.20150305.32
10. Say L, Chou D, Gemmill A, Tunçalp O, Moller A, Daniels J, et al. Global causes of maternal death: A WHO systematic analysis. Special programme of research, development and research training in human reproduction (HRP), department of reproductive health and research. Geneva, Switzerland: World Health Organization (2014). 10.1016/
11. Namakau C, Langalibalele H, Mabuza P. Cultural and health beliefs of pregnant women in Zambia regarding pregnancy and child birth. Curationis. (2015) 38(1):1–3. doi: 10.4102/curationis.v38i1.1232
12. Kahsu G, Atsede F, Gerezgiher B. Magnitude and reasons for harmful traditional practices among children less than 5 years of age in Axum town, north Ethiopia, 2013. Int J Pediatr. (2014) 2014:169795. doi: 10.1155/2014/169795
13. AdaneT HG, Etsubdink D. The prevalence of traditional malpractice during pregnancy, child birth, and postnatal period among women of childbearing age in Meshenti town, Hindawi. Int J Reprod Med. (2018) 2018:3–7. doi: 10.1155/2018/5945060
14. Federal Democratic Republic of Ethiopia Ministry of Women, Children and Youth Affairs (MoWCYA). National strategy and action plan on harmful traditional practices (HTPs) against women and children. Adis Abeba, Ethiopia: The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education (2013).
16. Dire Dawa administration regional health bureau: Six months report (DDHB, months report [unpublished], (2017).
17. AbebeH BG, Mulat BS. Harmful cultural practices duringperinatal period and associated factors among women of childbearing age in southern Ethiopia. PLoS One. (2021) 16(7):e0254095. doi: 10.1371/journal.pone.0254095
18. Nethra N, Rekha U. A study on traditional beliefs and practices in newborn care among mothers in a tertiary health care centre in Vijayapura, north Karnataka. Int J Community Med Public Health. (2018) 5(3):1035–40. doi: 10.18203/2394-6040.ijcmph20180757
19. Ukweh I, Kechukwu N, Ukweh O, Odeyemi K, Ekanem A. Influence of cultural and traditional beliefs on maternal and child health practices in rural and urban communities in Cross River state, Nigeria. Ann Med Res Pract. (2019) 1(4):6–10. doi: 10.25259/ANMRP_4_2019
20. Mmbulaheni R, Helene W, Nontuthuko R. The use of African traditional medicines amongst zulu women during childbearing in northern KwaZulu-Natal African. J Reprod Health. (2022) 26(1):69–72. doi: 10.29063/ajrh2022/v26i1.7
21. Ambaw YL, Yirdaw BW, Biwota MA, Mekuryaw AM, Taye BT. Antenatal care follow-up decreases the likelihood of cultural malpractice during childbirth and postpartum among women who gave birth in the last one-yearin Gozamen district, Ethiopia. Arch Public Health. (2022) 80:53. doi: 10.1186/s13690-022-00814-5
22. Prativa D, Mangala S, Dharanidhar B, Santosh P. Factors affecting the place of delivery among mothers residing in Jhorahat VDC, Morang, Nepal. IJCBNM. (2018) 6(1):4–7.
23. Sultan A, Sengul Yaman E. The European journal of contraception and reproductive health care. Potential Harm Traditional Pract Dur Pregnancy Postpartum. (2008) 13(3):282–8. doi: 10.1080/13625180802049427
24. Misganaw F, Berhim J. Cultural malpractices during labor/delivery and associated factors among women who had at least one history of delivery in selected zones of Amhara region, north west Ethiopia. BMC Pregnancy Childbirth. (2021) 21:504. doi: 10.1186/s12884-021-03971-7
25. Patience O, Helen H, Augustine A. Food prohibitions and other traditional practices in pregnancy: a qualitative study in western Region of Ghana. Adv Reprod Sci. (2015) 3:41–9. http://www.scirp.org/journal/arsci doi: 10.4236/arsci.2015.33005
26. Melesse MF, Bitew YB, Dessie KN, Wondim DB, Bereka TM. Impact of cultural practices during labor and delivery on maternal and child health service utilization and associated factors in Awi, east and west Gojjam zones, Amhara Region, north west Ethiopia. BMC Pregnancy Childbirth. (2021) 1:7–20. doi: 10.21203/rs.3.rs-255071/v1
27. Weldesamuel GT, Atalay HT, Zemichael TM, Gebre HG, Abrha DG, Amare AK, et al. Colostrum avoidance and associated factors among mothers having children less than 2 years of age in Aksum town, tigray, Ethiopia. BMC Res Notes. (2017) 11:601. doi: 10.1186/s13104-018-3712-z
28. Misgan L, Melake D, Firehiwot M, Demewoz H. Factors associated with colostrum avoidance among mothers of children aged less than 24 months in Raya Kobo district, north-eastern Ethiopia. J Trop Pediatr. (2015) 0:1–7. doi: 10.1093/tropej/fmv039
29. USAID. Harmful traditional practices in urban settings a review of the evidence on prevalence and effective interventions (2017).
30. Mellissa W, Nina K, Esther L. Traditional beliefs and practices in pregnancy, childbirth and postpartum: a review of the evidence from Asian countries. Midwifery. (2018) 56:158–70. doi: 10.1016/j.midw.2017.10.019
31. Kusqaum A. What steps must we take to eliminate harmful traditional practices? UK: Honour Abuse Research Matrix (HARM) University of Central Lancashire (2020).
32. Yeshalem M, Getu D, Tefera B. Dietary practices and associated factors among pregnant women in west Gojjam zone, northwest Ethiopia. BMC Pregnancy and Childbirth. (2020) 3:6–10. doi: 10.1186/s12884-019-2702-z
33. Nahom S, Melkamsew T. Traditional practices during pregnancy and childbirth among mothers in Shey Bench district, south west Ethiopia. SAGE Open Med. (2022)10:1–8. doi: 10.1177/20503121221098139
34. Lucia D. Influence of cultural and religious practices on the management of pregnancy at Mbombela municipality, South Africa: an explorative study. Open Nurs J. (2021) 15:132–3. doi: 10.2174/1874434602115010130
Keywords: cultural malpractice, pregnancy, child birth, postnatal, women’s
Citation: Hailu M, Mohammed A, Sintayehu Y, Tadesse D, Abera L, Abdurashid N, Solomon M, Ali M, Mellese D, Weldeamaniel T, Mengesha T, Hailemariyam T, Amsalu S, Dejene Y and Girma M (2023) Cultural malpractice during pregnancy, childbirth, and the postnatal period and its associated factors among women who gave birth once in Dire Dawa city administration, Eastern Ethiopia, in 2021. Front. Glob. Womens Health 4:1131626. doi: 10.3389/fgwh.2023.1131626
Received: 25 December 2022; Accepted: 31 July 2023;
Published: 17 August 2023.
Edited by:
Diane Sanford, Saint Louis University, United StatesReviewed by:
Berenger Kabore, Clinical Research Unit of Nanoro (CRUN), Burkina Faso© 2023 Hailu, Mohammed, Sintayehu, Tadesse, Abera, Abdurashid, Solomon, Ali, Mellese, Weldeamaniel, Mengesha, Hailemariyam, Amsalu, Dejene and Girma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mickiale Hailu bWljaGlhbGUxNDkzQGdtYWlsLmNvbQ==
Abbreviations AOR, adjusted odds ratio; ANC, antenatal care; CMP, cultural malpractice; COR, crudes odds ratio; IDI, in-depth interview; KI, key informant; MCH, maternal and child health; PNC, postnatal care; WHO, world health organization.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.