
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Glob. Womens Health, 01 September 2023
Sec. Maternal Health
Volume 4 - 2023 | https://doi.org/10.3389/fgwh.2023.1131143
 Melaku Hunie Asratie1*
Melaku Hunie Asratie1* Getayeneh Antehunegn Tesema2
Getayeneh Antehunegn Tesema2 Dagmawi Chilot3,4
Dagmawi Chilot3,4 Fantu Mamo Aragaw2
Fantu Mamo Aragaw2 Mehari Woldemariam Merid2
Mehari Woldemariam Merid2 Daniel Gashaneh Belay2,5
Daniel Gashaneh Belay2,5
Introduction: Initiation of family planning in the early post-partum period is a strategic move to reduce maternal, neonatal, and child mortality due to the negative consequences of short interbirth interval and the complications of unintended pregnancy. Antenatal care (ANC) is the noteworthy predictor of scaling up early initiation of post-partum family planning (PPFP) and preventing unintended pregnancy before menses resume. Despite the great role of ANC, information is scant about the effect of content, timing, and the number of ANC visits on the early initiation of PPFP in Ethiopia.
Objective: This study aimed to assess the association of ANC services with the early initiation of PPFP in Ethiopia.
Methods: The study was based on Ethiopian Demographic and Health Survey 2016 data, which was a cross-sectional survey from 18 January 2016 to 27 June 2016. A total weighted sample size of 2,920 post-partum women was included. A multilevel logistic regression model was used because of the hierarchical data, and variables with a p-value of ≤0.2 in the bivariable multilevel analysis were taken to multivariable multilevel analysis. An adjusted odds ratio with a 95% confidence interval (CI) was used to declare both the direction and strength of the association, and variables with a p-value of <0.05 were considered as statistically significant for the outcome variable.
Results: The early initiation of PPFP was 20.4%. Women with at least four ANC visits [adjusted odds ratio (AOR) = 1.31; CI 1.12–2.32], women who started ANC within the first trimester (AOR = 1.25; CI 1.10–2.23), complete routine ANC (AOR = 1.11; CI 1.01–2.03), post-natal care (AOR = 1.45; CI 1.19–1.87), resumption of menses (AOR = 1.67; CI 1.18–1.93), urban residency (AOR = 2.14; CI 1.18–2.51), and high community women’s education (AOR = 1.71; CI 1.51–2.11) were variables significantly associated with the early initiation of PPFP.
Conclusion: The early initiation of PPFP in Ethiopia was very low. Attention needs to be given to the quality of ANC, post-natal care, resumption of menses, residency, and community-level education of women to increase the prevalence of the early initiation of PPFP in Ethiopia. Therefore, the government should design a program targeting the quality of ANC in rural communities, considering women without menses and scaling up the education of women at the community level to the culture of the early initiation of PPFP in order to achieve reduced maternal, neonatal, and child mortality.
Provision of post-partum family planning (PPFP) services is one of the essential components of the maternal continuum of care that can be provided during labor and delivery and at any time of the post-partum period (1, 2). Currently, it is part of comprehensive maternal, neonatal, and child health services (3). In developing countries, PPFP provision is the selected strategy to halt maternal, neonatal, and child mortality (4). It is a means of making the post-partum period a high-impact and cost-effective program for the target group for maternal, neonatal, and child health improvements (5).
In Ethiopia, the majority of maternal and adolescent mortality is due to complications of unplanned and unwanted pregnancy (6, 7). Post-partum women have a high demand for spacing and limiting pregnancies. Approximately 75% of women have an unmet need for preventing pregnancy (6). The unmet need for post-partum contraceptive use is directly associated with unintended pregnancy, especially with the characteristics of short interbirth interval (8, 9). Evidence showed that more than 20% of births in developing countries are with short interbirth intervals (9, 10). A recently published article states that the prevalence of short interbirth intervals in Ethiopia is 46% (11). Developing countries, including Ethiopia, need to give attention to reducing this high magnitude of the short interbirth interval because it is one of the major causes of maternal, neonatal, infant, and child mortality (9–14). Specifically, short interbirth interval due to unmet need is associated with uteroplacental bleeding disorders (placental abruption, placenta previa, and vasa previa) which are the direct causes of maternal mortality (15). Children born within 24 months, especially the 12th and early months of an elder sibling, have a 60% higher risk of dying before celebrating their first birthday as compared to those born after an interval of 3–5 years. Another evidence suggested that children born with intervals of less than 2 years are at a 40% higher risk of dying (16). A study also showed that pregnancies conceived less than 20 months following a prior birth are at higher risk of early neonatal death, prematurity, fetal death, and low birth weight (17). In general, too closely spaced births due to an unmet need for PPFP pose substantial health risks for the mother, fetus, neonate, and child as well (18).
Attention should be given to the timing of initiation of post-partum contraceptives to avert the aforementioned challenges related to short interbirth intervals and the negative consequences of unintended pregnancy (19–22). Different kinds of literature recommend that post-partum contraceptives should be initiated in the early post-partum period (within 6 weeks) as much as possible (23–25). Early initiation of PPFP can avert 75% of maternal mortality, unintended pregnancy by two-thirds, and the risk of abortion by 73% (4). Additional evidence showed that early initiation of a post-partum contraceptive is the supreme intervention for the affirmation of optimal interbirth interval (26). The majority of the post-partum women become fecund before the resumption of the menstrual cycle (27); however, most women do not realize that they are at risk for subsequent pregnancy in this critical period (5). This is one of the hidden challenges in Ethiopia that needs attention to solve by cultivating a culture of the early initiation of PPFP among post-partum period women.
From the clinical experience of different scholars, they recommend that devoting time to counseling post-partum contraceptive use during the antenatal care (ANC) period is the preferred modality to the early initiation of PPFP. However, scant information about the effect of the content, timing, and the number of ANC visits on the early initiation of PPFP (within 6 weeks of post-partum women) in Ethiopia is found. With this paucity of high-quality evidence on the role of the quality of ANC, to improve the prevalence of the early initiation of PPFP, the real risk of short interbirth interval and unintended pregnancy with their negative consequences need great attention for fear of theoretical maternal, neonatal, and child risks. Therefore, this study aimed to assess the effect of content, timing, and the number of ANC visits on the early initiation of PPFP in Ethiopia. Furthermore, the findings of this study could guide program managers or policymakers for the improved prevalence of the early initiation of PPFP with the ultimate goal of reducing maternal, neonatal, and child death.
A cross-sectional study survey was conducted among reproductive-aged women in Ethiopia from 18 January 2016 to 27 June 2016 by the Ethiopian Central Statistical Agency (ECSA). In the case of our study, we conducted a secondary analysis of the survey using the Ethiopian Demographic and Health Survey (EDHS) 2016. The EDHS 2016 was the fourth survey conducted among nine regional states of the country [Tigray; Afar; Amhara; Oromia; Somali; Benishangul-Gumuz; the Southern Nations, Nationalities, and Peoples’ Region (SNNPR); Gambella; and Harari regions] and two city administrations (Addis Ababa and Dire Dawa). Ethiopia is an eastern African country that is the second-most populous country after Nigeria. At the federal level, divided into nine regions and two city administrations for administrative purposes, those regions are subdivided into zones, zones divided into woredas, and woredas divided into kebeles (the lowest administrative unit). Kebeles is also divided into census enumeration areas (EAs).
The detail of the study area and study design was elaborated from the document of the Central Statistical Agency (CSA) of Ethiopia (28).
All post-partum reproductive-aged women (15–48) who are current contraceptive users in Ethiopia were our source population.
All post-partum period reproductive-aged women (15–48) currently using any contraceptive methods during the data collection period (18 January 2016 to 27 June 2016) in Ethiopia were the study population.
In the EDHS, the survey was conducted with two stages; a stratified cluster sampling technique was used to select participants. In the first stage, 645 EAs were selected by stratifying into 202 urban areas and 443 rural areas. The sampling frame was the 2007 population and housing census using probability proportional to the EA scale. The details of the sampling procedure were elaborated in the EDHS 2016 report from the MEASURE DHS Program website (www.dhsprogram.com). Finally, the weighted values were used for the analysis in order to keep the representativeness of the sampled data. Women's record (IR) EDHS data sets were used. From this data set, we have fixed the study population by considering only PPFP users and non-pregnant women by using variables, and then, after the total sample size of the weighted data set that we have used in our study was 2,920 women who were post-partum, not pregnant, and currently using any kind of contraceptives. The variable month of starting a contraceptive was used to categorize the outcome variable, whether early initiation or late initiation.
Dependent variable: Early initiation of PPFP (yes/no).
Independent variables: All these independent variables were grouped into three major classifications (socio-demographic factors, obstetrical-related factors, and maternal healthcare service-related factors). During the analysis, age of women in a year, age of husband/partner, women's and husband’s level of education, religion, current working status, wealth status, relation to household head, exposure to mass media, parity, number of children under the age of 5 years, history of pregnancy termination, resumption menses, place of delivery, post-partum care, husband/partner desire for children, information about family planning services, number of visits by a health worker in the past 12 months, number of health facility visits in the last 12 months, and distance to health facility were variables moved as individual-level factors, whereas residency, community-level women's education, community-level poverty, and community-level media exposure were variables moved as community-level factors (Table 1).
Early initiation of PPFP: Prevention of unintended and closely spaced pregnancies within 6 weeks following childbirth using modern contraceptives (29).
Components of routine ANC services: This was an independent variable for this study that was measured based on eight essential elements of ANC services: blood pressure measurement, blood sample collection, urine sample collection, weight measurement, tetanus toxoid (TT2+) vaccination, iron folate (90+) supplementation, health education on danger signs and nutrition, and HIV testing. Information on these eight items of ANC content was derived from the response to the question “As part of your antenatal care during this pregnancy, were any of the following done at least once? Was your weight measured? Was your blood pressure measured?”. The answers were recorded as yes or no. It is possible that a single mother may have a urine test or blood test or measurement of weight or blood pressure several times during the same pregnancy. However, as the mother was asked to report any action at least once, the response for any action was recorded as a single action. On the basis of responses, we have created a composite index of ANC content as our second outcome variable, which comprises a simple count of the number of elements of care received. Finally, the outcome variable is dichotomized into incomplete if a woman gets less than eight services = 0 and complete if a woman gets all eight elements = 1 (30, 31).
Post-partum period: It is defined as the time limit from the delivery of the placenta to 12 months of the post-partum period. Therefore, all women within this time period were classified as “post-partum” (32).
The data were first accessed from the website http://www.measuredhs.com/ by online request of permission through a detailed explanation of our research purpose, and the data were extracted and coded, and both descriptive and analytical analyses were done using statistical software STATA version 14. Statistical summaries such as proportion and median were used to present descriptive statistics.
EDHS data were collected by considering clusters as a study unit, and this violates the independent assumptions of a standard logistic regression model. Therefore, multilevel logistic regression analysis was implemented. The first intra-class correlation coefficient (ICC) of the null model was used to detect the presence of variation in the distribution of the outcome variable (early initiation of PPFP) among different clusters, and the magnitude was 22.5%, which entails that there is a significant clustering effect that should be considered during analysis using an advanced statistical model. The median odds ratio (MOR) was also another indicator of the presence of a significant clustering effect with the value of 2.52 (2.35–2.61) in the null model.
Fixed effects (a measure of association) were used to assess the relationship between the outcome variable and the independent variables. Crude odds ratio (COR) with a 95% confidence interval (CI) was used to measure both the direction and strength of the association. Variables with a p-value of ≤0.2 were selected for the analysis in the adjusted model. Finally, in the multilevel analysis, the association between the outcome variables and explanatory variables was judged by using an adjusted odds ratio (AOR) with respect to a CI, and statistical significance was declared at a p-value of <0.05.
Random effects (a measure of variability) were measured by ICC, MOR, proportion change in variance (PCV), and deviance (−2 log-likelihood ratio).
Intra-class correlation coefficient: ICC was the value used to detect the variation in the distribution of outcome variable (early initiation of PPFP) between clusters. In the null model, the ICC was 22.5%, which means, irrespective of other factors such as socio-demographic, obstetrical, and maternal healthcare service-related factors of our study, the cluster determined 22.5% of the variation in the distribution of the outcome variable.
Median odds ratio: MOR was used to quantify the middle odds ratio between the highest and the lowest odds ratios of the clustering effect. It is another way of quantifying cluster-level variance into odds ratio. The MOR in the null model of this study was 2.52 (2.35–2.61) which was significant. It was calculated as follows MOR = exp. [√ (2xVA) × 0.6745], MOR = e0.95√VA where VA = cluster-level variance.
Proportion change in variance: PCV was used to explain the percent of the variation in the early initiation of PPFP detected by the model with the available variables. The PCV of the final model of this study was 6%, which means that 6% of the variability was explained by the model that we fit, whereas the rest 94% of the variability was not explained by the model.
Deviance (−2 log-likelihood): Deviance was used to measure the total variations that come up with both the individual- and community-level factors. It was used to model comparison, and the model with the lowest deviance was taken for the interpretation of the finding, which was model IV.
Since the study was a secondary data analysis of publicly available survey data from the MEASURE DHS Program, ethical approval and participant consent were not necessary for this particular study. We requested the DHS Program, and permission was granted to download and use the data for this study from http://www.dhsprogram.com. The Institutional Review Board approved that procedures for DHS public-use data sets did not in any way allow respondents, households, or sample communities to be identified. No names of individuals or household addresses in the data file were recorded. The geographic identifiers only went down to the regional level (where regions are typically very large geographical areas encompassing several states/provinces). Each EA (primary sampling unit) had a PSU number in the data file, but the PSU numbers did not have any labels to indicate their names or locations.
Among 2,920 post-partum women who were using contraceptives, 1,927 (66%) were within the age group of 20–34 years; 1,898 (65%) had a household head aged 31–59 years; 1,548 (53%) had no formal education; 1,139 (39%) had their husbands achieve primary education; and 2,599 (89%) of their household head’s sex were male. Among all participants, 1,489 (51%) were orthodox; 1,840 (63%) did not have work; 1,489 (51%) were rich; 2,219 (76%) were residing in rural areas; and 2,482 (85%) of them were the wives of the household head. Among all women who participated in this study, 1,956 (67%) and 1,840 (64%) were women with low community education and community media exposure, respectively, whereas 1,781 (61%) of the participants were at high community poverty (Table 2).
Among all participants, 1,956 (67%) had fewer than four ANC visits; 1,635 (56%) started their ANC visits within the first trimester, and 1,752 (60%) did not receive the complete components of routine ANC services. Of all respondents, 2,132 (73%) reported that distance was a significant problem when reaching the nearby health facility; 1,986 (68%) did not have a chance to be visited for fieldwork; and 1,548 (53%) had information about family planning. Among all participants, 2,336 (80%) delivered at a health facility; 2,190 (75%) had post-partum care; and 1,635 (56%) did not visit a health facility within 12 months (Table 3).
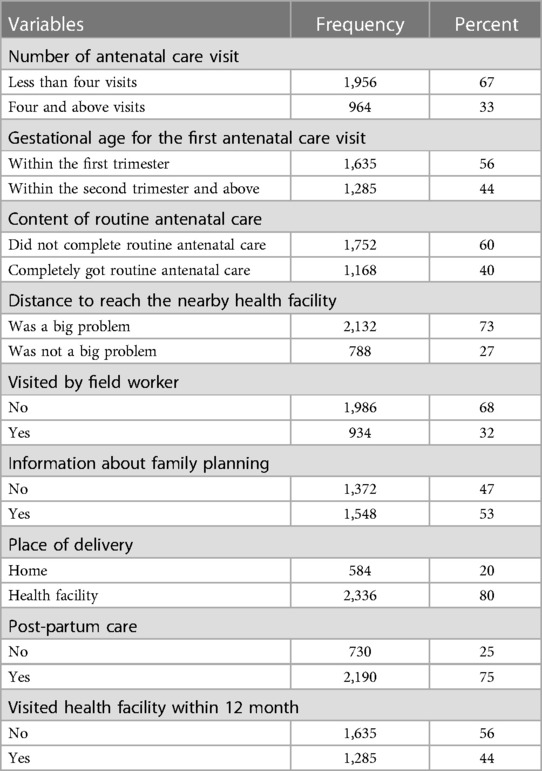
Table 3. Maternal healthcare service-related characteristics of participants in Ethiopia (n = 2,920).
Among the 2,920 participants, 1,285 (44%) were multiparous; 1,680 (58%) had started menstruation, and 1,723 (59%) had a number of children under 5 years old. Of all participants, 2,570 (88%) had no bad obstetric history [stillbirth and abortion (both induced and spontaneous)], and 1,110 (38%) of their husbands wanted more children (Table 4).
The prevalence of the early initiation of PPFP was 20.4%; 95% (19.25–21.7%]) (Figure 1).
A total of three models were fitted to assess the association of variables. In model II, eight individual-level variables and, in model III, two community-level variables were significantly associated with the outcome variable. When we come to model IV, a total of seven variables (number of ANC, gestational age for the first ANC visit, components of routine ANC, post-partum care, resumption of menses, residency, and community women's education) were statistically significant with the early initiation of PPFP.
Women with at least four ANC visits were 1.31 times more likely to initiate PPFP (AOR = 1.31; 95% CI 1.12–2.32) as compared with those with ANC follow-up of less than four. Likewise, women who started ANC within the first trimester were 1.25 times more likely to initiate early PPFP (AOR = 1.25; 95% CI 1.10–2.23) compared with those who had started their ANC visit in the second trimester and above gestational age. Women who had received the full components of routine ANC were 1.11 times more likely to initiate early PPFP (AOR = 1.11; 95% CI 1.01–2.03) compared with those who did not get full components of routine ANC.
The odds of the early initiation of PPFP was 1.45 times higher among women with post-partum care (AOR = 1.45; 95% CI 1.19–1.87) compared with those who had no post-partum care. Women with menses resumption at the time of the survey were 1.67 times more likely to initiate early PPFP (AOR = 1.67; 95% CI 1.18–1.93) as compared with those who never had their menses resumed. The odds of early initiation of PPFP was 2.14 times higher among women who reside in urban areas (AOR = 2.14; 95% CI 1.18–2.51) as compared with those residing in rural areas. The odds of the early initiation of PPFP was 1.71 times higher among women with high community education (AOR = 1.17; 95% CI 1.51–2.11) as compared with those who had low community education (Table 5).
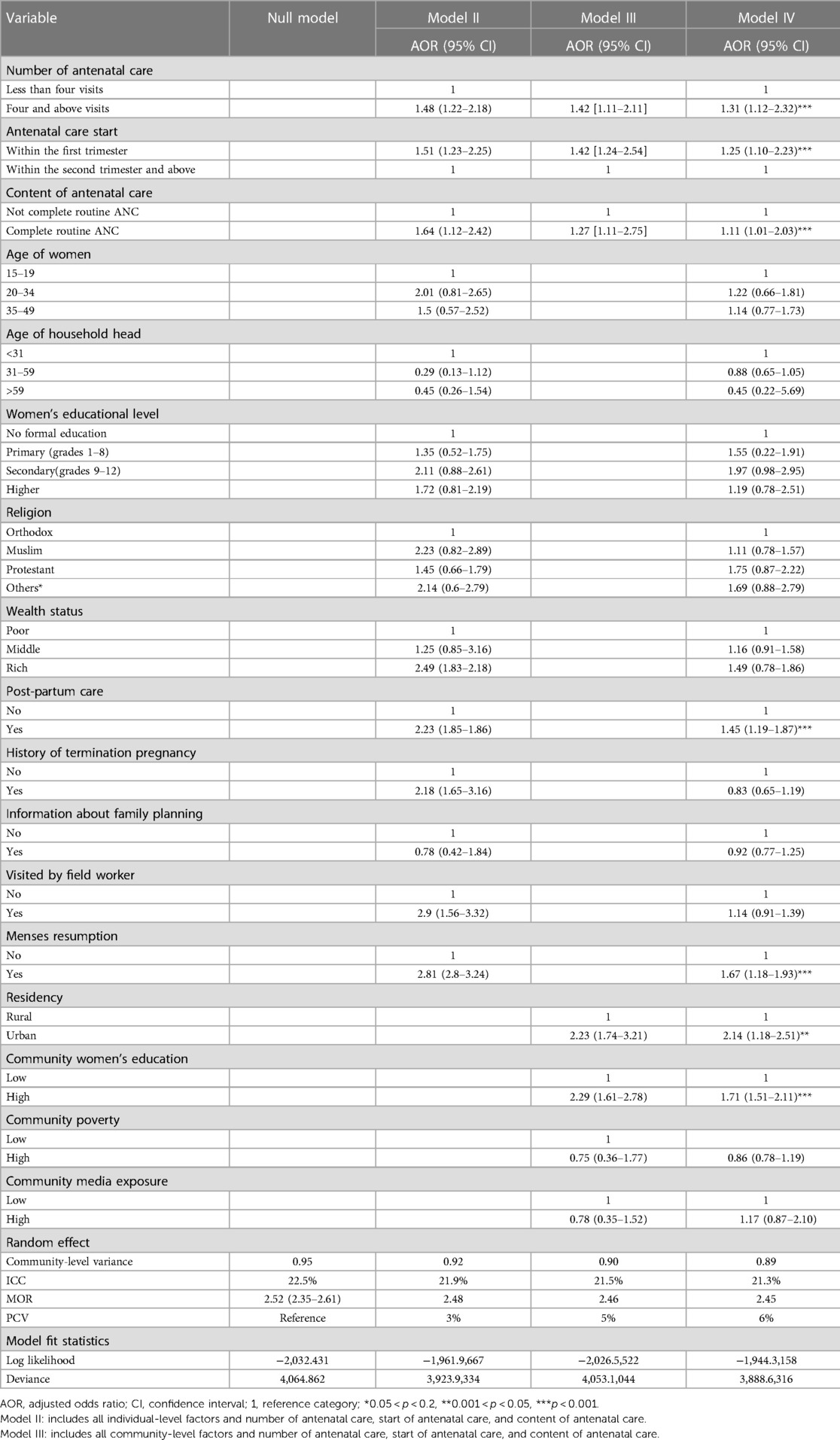
Table 5. Multivariable multilevel logistic regression analysis of factors associated with early initiation of postpartum family planning in Ethiopia (n = 2,920).
Designing, testing, and scaling up effective, affordable, and sustainable health interventions in low-resource countries are critical to address the high unmet need for PPFP (28). The study finds that the magnitude of the early initiation of PPFP is 20.4%. This is lower than that reported in previous studies conducted in Southern Ethiopia (31.7%) (33), Dilla town (Southern Ethiopia) (39.2%) (34), Tanzania (37%) (35), and Uganda (52%) (24). The possible explanation for the low prevalence of the early initiation of PPFP in the current study compared with two studies conducted in Southern Ethiopia could be due to the variation in the composition of the study population. This means that the current study is based on EDHS data which includes a larger proportion of rural communities and women in the rural community less likely to initiate early PPFP. This hypothesis is also supported by the current study as residency is significantly associated with the early initiation of PPFP. The possible explanation for the low prevalence of the current study compared with the previous studies conducted in Tanzania and Uganda could be the difference in socio-demographic factors among the study populations and the difference in the time trend of the data collected.
Regarding the factors associated with the early initiation of PPFP, the number of ANC services, gestational age for the first ANC visit, and content of routine ANC services had a great effect on the early initiation of PPFP. Antenatal care is a noteworthy predictor of subsequent adherence to the maternity continuum of care (health facility delivery, post-natal care, and PPFP use) (36, 37). Evidence shows that the quality of antenatal care is a driving force to achieve the sustainable development goal related to the reduction of maternal, neonatal, and child mortality (38–40). On the other hand, maternal, neonatal, and child mortality are secondary to short interbirth intervals, and the negative consequence of unintended pregnancy is still a problem in Ethiopia which can be alleviated by respecting the quality of maternal healthcare services, especially antenatal care services. The coverage of at least one antenatal care visit in Ethiopia has reached 62% from the EDHS 2016 report (41). This improvement did not result in a significant upswing in maternal, neonatal, and child health. This unresponsive challenge with the existing improved antenatal care service coverage might be solved with an approach to qualified antenatal care services. However, evidence related to the impact of the quality of antenatal care has not been explained well yet. Therefore, this study needs to examine the effect of the quality of antenatal care (number of visits, timing of antenatal care start, and the contents of routine care provided during the antenatal care period) on the early initiation of PPFP.
Women with at least four or more ANC visits were 1.31 times more likely to early initiate PPFP as compared with those who had antenatal care visits of less than four. This finding was supported by different studies (34, 42–47). The possible explanation could be that women with a greater number of antenatal care visits have greater contact with healthcare providers. This can be important to get the full service of antenatal care including counseling about birth spacing and early initiation of PPFP service. In addition, it is obvious that family planning use-related counseling is recommended after the third trimester or more at the fourth visit (37, 47). Therefore, those women with four and more antenatal care visits might have better information about PPFP use, and they might initiate early within 6 weeks of the post-partum period compared with those with less than four antenatal care visits.
Women who started ANC within the first trimester were 1.25 times more likely to initiate early PPFP as compared with women's first antenatal care visit starting within the second trimester and above. This finding was supported by studies conducted in Cambodia and Tanzania (46, 48). The possible explanation for this could be that women who start antenatal care at an early gestational age have a higher chance to contact healthcare providers and they could get PPFP counseling services from this intern, who helps them initiate PPFP early. The other possible explanation which is supported by evidence is that women who start antenatal care at an early gestational age are mostly free from the cultural influence from the community to attend the maternity continuum of care (49). Reduced exposure to misleading rumors about post-partum contraceptives might encourage women to initiate use of contraceptives earlier as compared to women influenced solely by cultural beliefs.
Lastly, women who completely took routine antenatal care services were 1.11 times more likely to initiate early PPFP compared with those who did not get full components of routine antenatal care services. Components of routine antenatal care services are the crux part of antenatal care, which is provided for all pregnant women irrespective of their risk/complication status (50, 51). Therefore, those services directly measure both the commitment of the healthcare provider assigned for antenatal care provision and women's engagement across the maternity continuum of care (52). Women who are committed to attending the full components of routine antenatal care services might be more likely to engage in the subsequent elements of the maternity continuum of care including the early initiation of PPFP compared with those women who did not receive the full components of routine antenatal care (53).
Four additional variables (post-partum care, resumption of menses, residency, and community women's education) statistically significant with the outcome variable early initiation of PPFP were identified. Women with post-partum care were 1.45 times more likely to initiate PPFP as compared with those who had no post-partum care. This finding was supported by different studies conducted in Ethiopia and Kenya (33, 54, 55). The possible explanation could be that post-partum care is one of the elements of the maternity continuum of care and routinely recommends PPFP use (56). Therefore, those women with post-partum care have greater information about the timing of post-partum contraceptive use, and they might initiate PPFP early compared with women without post-partum care.
In this study, the odds of early initiation of PPFP was 1.67 higher in women whose menses had resumed. This finding was supported by the study conducted in western Ethiopia as women with menses resumption of 2.6 times a higher time (within 6 weeks of the post-partum period) initiate PPFP compared with those who have menses yet not resumed (33). Another study conducted in Ethiopia showed that resumption of menses is significantly associated with the early initiation of PPFP (34). The possible explanation could be due to menses, which is alarming because of the occurrence of pregnancy whenever there is sexual intercourse in the post-partum period (57). Evidence showed that the majority of post-partum period women depended on their menses resumption to initiate PPFP and they were not informed about the occurrence of pregnancy with the absence of menses (58, 59). This was one of the challenges in Ethiopia for the huge number of unintended pregnancies due to post-partum contraceptives not used (60–62).
The odds of early initiation of PPFP were 2.14 times higher among women residing in urban areas compared with their counterparts. This finding was supported by different studies as residence was significantly associated with PPFP use (63, 64). The possible explanation could be that those women who reside in urban areas are nearest to media exposure and most media has a positive impact on awareness creation about family planning use (65). On the other hand, urban areas are known for a large proportion of educated participants (66), and education is one factor for the early initiation of PPFP in Ethiopia as proven by the current study.
Women with a high level of community education were 1.71 times more likely to initiate PPFP early compared with their counterparts. This finding was supported by evidence conducted in southern Ethiopia as women with high-level educational status were 1.5 times more likely to initiate PPFP early (34). The possible explanation could be that education is the driving force to be engaged on the continuum of maternity care including PPFP use in Ethiopia (67, 68). Educated women are familiar with the methods of contraceptives that are suitable for the post-partum period, and they might initiate PPFP early. The other possible explanation would be that educated women might be informed that pregnancy can occur before post-partum menses resumption and they might use contraceptives in the early post-partum period due to fear of unintended pregnancy.
This study used nationally representative data, which were collected with standardized and validated data collection tools.
This study used an advanced model that accounts for the correlated nature of the EDHS data in the determination of estimates.
The cross-sectional nature of the survey does not show the temporal or causal relationship between independent variables and the outcome variables.
The EDHS data were based on post-partum period women with the last birth at the different time periods, and it might cause recall bias on the content of antenatal care services and timing of the initiation of PPFP.
The initiation of PPFP within 6 weeks of post-partum period included women who had initiated even within 2 months. This might increase the prevalence of the outcome variable.
This study demonstrated that early initiation of PPFP was low. Women with at least four ANC visits, first antenatal care visit within the first trimester, the full content of routine antenatal care services, having post-partum care, resumed menses, urban residency, and high community education were positively associated with early initiation of PPFP. The Demographic and Health Survey should revise the way of reaching out to the timing of PPFP initiation in weeks rather than in months.
The original contributions presented in the study are included in the article, and further inquiries can be directed to the corresponding author.
Ethical review and approval were not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
MA: initiated the idea of research and conceptualization, developed the proposal, performed the analysis, and wrote the manuscript. GT, DC, FA, MM, and DB: carried out the analysis, reviewed the manuscript, and corrected it. Finally, all the authors have approved the manuscript, by preparing it for submission. All authors contributed to the article and approved the submitted version.
Our deepest gratitude goes to the MEASURE DHS Program for the permission of access and for the use of the 2016 EDHS data.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Tran NT, Seuc A, Tshikaya B, Mutuale M, Landoulsi S, Kini B, et al. Effectiveness of post-partum family planning interventions on contraceptive use and method mix at 1 year after childbirth in Kinshasa, DR Congo (yam daabo): a single-blind, cluster-randomised controlled trial. Lancet Glob Health. (2020) 8(3):e399–410. doi: 10.1016/S2214-109X(19)30546-7
2. Blazer C, Prata N. Postpartum family planning: current evidence on successful interventions. Open Access J Contracept. (2016) 7:53. doi: 10.2147/OAJC.S98817
3. Pfitzer A, Mackenzie D, Blanchard H, Hyjazi Y, Kumar S, Lisanework Kassa S, et al. A facility birth can be the time to start family planning: postpartum intrauterine device experiences from six countries. Int J Gynaecol Obstet. (2015) 130:S54–61. doi: 10.1016/j.ijgo.2015.03.008
4. Cleland J, Shah IH, Daniele M. Interventions to improve postpartum family planning in low-and middle-income countries: program implications and research priorities. Stud Fam Plann. (2015) 46(4):423–41. doi: 10.1111/j.1728-4465.2015.00041.x
5. Tran NT, Gaffield ME, Seuc A, Landoulsi S, Yamaego WME, Cuzin-Kihl A, et al. Effectiveness of a package of postpartum family planning interventions on the uptake of contraceptive methods until twelve months postpartum in Burkina Faso and the democratic Republic of Congo: the YAM DAABO study protocol. BMC Health Serv Res. (2018) 18(1):1–12. doi: 10.1186/s12913-017-2770-6
6. Cleland J, Shah IH, Benova L. A fresh look at the level of unmet need for family planning in the postpartum period, its causes and program implications. Int Perspect Sexual Reprod Health. (2015) 41(3):155–62. doi: 10.1363/intsexrephea.41.3.155
7. Huber D, Curtis C, Irani L, Pappa S, Arrington L. Postabortion care: 20 years of strong evidence on emergency treatment, family planning, and other programming components. Glob Health Sci Pract. (2016) 4(3):481–94. doi: 10.9745/GHSP-D-16-00052
8. DeGraff DS, de Silva V. A new perspective on the definition and measurement of unmet need for contraception. Int Fam Plan Perspect. (1996):140–7. doi: 10.2307/2950811
9. Gebrehiwot SW, Abera G, Tesfay K, Tilahun W. Short birth interval and associated factors among women of child bearing age in northern Ethiopia, 2016. BMC Women’s Health. (2019) 19(1):1–9. doi: 10.1186/s12905-019-0776-4
10. Shifti DM, Chojenta C, Holliday EG, Loxton D. Individual and community level determinants of short birth interval in Ethiopia: a multilevel analysis. PLoS One. (2020) 15(1):e0227798. doi: 10.1371/journal.pone.0227798
11. Aychiluhm SB, Tadesse AW, Mare KU, Abdu M, Ketema A. A multilevel analysis of short birth interval and its determinants among reproductive age women in developing regions of Ethiopia. PLoS One. (2020) 15(8):e0237602. doi: 10.1371/journal.pone.0237602
12. Dadi AF. A systematic review and meta-analysis of the effect of short birth interval on infant mortality in Ethiopia. PLoS one. (2015) 10(5):e0126759. 10.137126001079
13. Mekonnen Y, Tensou B, Telake DS, Degefie T, Bekele A. Neonatal mortality in Ethiopia: trends and determinants. BMC Public Health. (2013) 13(1):1–14. doi: 10.1186/1471-2458-13-483
14. Shifti DM, Chojenta C, Holliday E, Loxton D. Effects of short birth interval on neonatal, infant and under-five child mortality in Ethiopia: a nationally representative observational study using inverse probability of treatment weighting. BMJ Open. (2021) 11(8):e047892. doi: 10.1136/bmjopen-2020-047892
15. Conde-Agudelo A, Rosas-Bermúdez A, Kafury-Goeta AC. Effects of birth spacing on maternal health: a systematic review. Am J Obstet Gynecol. (2007) 196(4):297–308. doi: 10.1016/j.ajog.2006.05.055
16. Rutstein SO. Further evidence of the effects of preceding birth intervals on neonatal, infant, and under-five-years mortality and nutritional status in developing countries: evidence from the demographic and health surveys: Macro International Incorporated (2008).
17. Lawn JE, Blencowe H, Oza S, You D, Lee AC, Waiswa P, et al. Every newborn: progress, priorities, and potential beyond survival. Lancet. (2014) 384(9938):189–205. doi: 10.1016/S0140-6736(14)60496-7
18. Abraha TH, Teferra AS, Gelagay AA. Postpartum modern contraceptive use in northern Ethiopia: prevalence and associated factors. Epidemiol Health. (2017) 39. doi: 10.4178/epih.e2017012
19. McDougal L, Atmavilas Y, Hay K, Silverman JG, Tarigopula UK, Raj A. Making the continuum of care work for mothers and infants: does gender equity matter? Findings from a quasi-experimental study in bihar, India. PLoS One. (2017) 12(2):e0171002. doi: 10.1371/journal.pone.0171002
20. Roy N, Adhikary P, Kabra R, Kiarie J, Mburu G, Dhabhai N, et al. Postpartum contraceptive practices among urban and peri-urban women in north India: a mixed-methods cohort study protocol. BMC Pregnancy Childbirth. (2021) 21(1):1–8. doi: 10.1186/s12884-020-03485-8
21. Erfina E, Widyawati W, McKenna L, Reisenhofer S, Ismail D. Exploring Indonesian adolescent women’s healthcare needs as they transition to motherhood: a qualitative study. Women Birth. (2019) 32(6):e544–e51. doi: 10.1016/j.wombi.2019.02.007
22. Dwomoh D. Geospatial analysis of determinants of neonatal mortality in Ghana. BMC Public Health. (2021) 21(1):1–18. doi: 10.1186/s12889-021-10473-w
23. Brunson MR, Klein DA, Olsen CH, Weir LF, Roberts TA. Postpartum contraception: initiation and effectiveness in a large universal healthcare system. Am J Obstet Gynecol. (2017) 217(1):55. e1-e9. doi: 10.1016/j.ajog.2017.02.036
24. Atukunda EC, Mugyenyi GR, Obua C, Atuhumuza EB, Lukyamuzi EJ, Kaida A, et al. Provision of family planning vouchers and early initiation of postpartum contraceptive use among women living with HIV in southwestern Uganda: a randomized controlled trial. PLoS Med. (2019) 16(6):e1002832. doi: 10.1371/journal.pmed.1002832
25. Taub RL, Jensen JT. Advances in contraception: new options for postpartum women. Expert Opin Pharmacother. (2017) 18(7):677–88. doi: 10.1080/14656566.2017.1316370
26. Sridhar A, Salcedo J. Optimizing maternal and neonatal outcomes with postpartum contraception: impact on breastfeeding and birth spacing. Matern Health Neonatol Perinatol. (2017) 3(1):1–10. doi: 10.1186/s40748-016-0040-y
27. Borda MR, Winfrey W, McKaig C. Return to sexual activity and modern family planning use in the extended postpartum period: an analysis of findings from seventeen countries. Afr J Reprod Health. (2010) 14(4).21812200
28. Demographic CE. Health survey-2011. Central statistical agency Addis Ababa. Maryland, USA: Ethiopia ICF International Calverton (2016).
29. Harrison MS, Goldenberg RL. Immediate postpartum use of long-acting reversible contraceptives in low-and middle-income countries. Matern Health Neonatol Perinatol. (2017) 3(1):24. doi: 10.1186/s40748-017-0063-z
30. Islam MM, Masud MS. Determinants of frequency and contents of antenatal care visits in Bangladesh: assessing the extent of compliance with the WHO recommendations. PLoS One. (2018) 13(9):e0204752. doi: 10.1371/journal.pone.0204752
31. Haile D, Habte A, Bogale B. Determinants of frequency and content of antenatal care in postnatal mothers in Arba Minch Zuria District, SNNPR, Ethiopia, 2019. Int J Women’s Health. (2020) 12:953. doi: 10.2147/IJWH.S261705
32. Cunningham FG, Leveno KJ, Bloom SL, Spong CY, Dashe JS. Williams obstetrics, 24e. NY, USA: Mcgraw-hill New York (2014).
33. Dona A, Abera M, Alemu T, Hawaria D. Timely initiation of postpartum contraceptive utilization and associated factors among women of child bearing age in aroressa district, southern Ethiopia: a community based cross-sectional study. BMC Public Health. (2018) 18(1):1–9. doi: 10.1186/s12889-018-5981-9
34. Abate ZG, Obsie GW. Early postpartum modern family planning utilization and associ-ated factors in dilla town, southern Ethiopia; 2019. J Womens Health Gyn. (2021) 8:1–9. doi: 10.17303/jwhg.2021.8.102
35. Rwabilimbo MM, Elewonibi BR, Yussuf MH, Robert M, Msuya SE, Mahande MJ. Initiation of postpartum modern contraceptive methods: evidence from Tanzania demographic and health survey. PLoS One. (2021) 16(3):e0249017. doi: 10.1371/journal.pone.0249017
36. Lori JR, Chuey M, Munro-Kramer ML, Ofosu-Darkwah H, Adanu RM. Increasing postpartum family planning uptake through group antenatal care: a longitudinal prospective cohort design. Reprod Health. (2018) 15(1):1–8. doi: 10.1186/s12978-017-0439-6
37. Puri MC, Moroni M, Pearson E, Pradhan E, Shah IH. Investigating the quality of family planning counselling as part of routine antenatal care and its effect on intended postpartum contraceptive method choice among women in Nepal. BMC Women’s Health. (2020) 20(1):1–11. doi: 10.1186/s12905-019-0871-6
38. Kuhnt J, Vollmer S. Antenatal care services and its implications for vital and health outcomes of children: evidence from 193 surveys in 69 low-income and middle-income countries. BMJ Open. (2017) 7(11):e017122. doi: 10.1136/bmjopen-2017-017122
39. Koblinsky M, Moyer CA, Calvert C, Campbell J, Campbell OM, Feigl AB, et al. Quality maternity care for every woman, everywhere: a call to action. Lancet. (2016) 388(10057):2307–20. doi: 10.1016/S0140-6736(16)31333-2
40. Oladapo O, Tunçalp Ö, Bonet M, Lawrie T, Portela A, Downe S, et al. WHO Model of intrapartum care for a positive childbirth experience: transforming care of women and babies for improved health and wellbeing. BJOG. (2018) 125(8):918. doi: 10.1111/1471-0528.15237
41. Csa I. Central statistical agency (CSA)[Ethiopia] and ICF. Ethiopia demographic and health survey, Addis Ababa, Ethiopia and Calverton, Maryland, USA. (2016).
42. Singh K, Story WT, Moran AC. Assessing the continuum of care pathway for maternal health in south Asia and sub-Saharan Africa. Matern Child Health J. (2016) 20(2):281–9. doi: 10.1007/s10995-015-1827-6
43. Adjiwanou V, LeGrand T. Does antenatal care matter in the use of skilled birth attendance in rural Africa: a multi-country analysis. Soc Sci Med. (2013) 86:26–34. doi: 10.1016/j.socscimed.2013.02.047
44. Amare NS, Araya BM, Asaye MM. Dropout from maternity continuum of care and associated factors among women in Debre Markos town, northwest Ethiopia. BioRxiv. (2019):620120.
45. Osaki K, Hattori T, Kosen S. The role of home-based records in the establishment of a continuum of care for mothers, newborns, and children in Indonesia. Glob Health Action. (2013) 6(1):20429. doi: 10.3402/gha.v6i0.20429
46. Mohan D, LeFevre AE, George A, Mpembeni R, Bazant E, Rusibamayila N, et al. Analysis of dropout across the continuum of maternal health care in Tanzania: findings from a cross-sectional household survey. Health Policy Plan. (2017) 32(6):791–9. doi: 10.1093/heapol/czx005
47. Tafere TE, Afework MF, Yalew AW. Counseling on family planning during ANC service increases the likelihood of postpartum family planning use in Bahir Dar City administration, Northwest Ethiopia: a prospective follow up study. Contracept Reprod Med. (2018) 3(1):1–9. doi: 10.1186/s40834-018-0081-x
48. Sakuma S, Yasuoka J, Phongluxa K, Jimba M. Determinants of continuum of care for maternal, newborn, and child health services in rural Khammouane, Lao PDR. PLoS One. (2019) 14(4). doi: 10.1371/journal.pone.0215635
49. Simkhada B, Teijlingen ERV, Porter M, Simkhada P. Factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. J Adv Nurs. (2008) 61(3):244–60. doi: 10.1111/j.1365-2648.2007.04532.x
50. Osungbade K, Oginni S, Olumide A. Content of antenatal care services in secondary health care facilities in Nigeria: implication for quality of maternal health care. Int J Qual Health Care. (2008) 20(5):346–51. doi: 10.1093/intqhc/mzn026
51. Villar J, Ba'aqeel H, Piaggio G, Lumbiganon P, Belizán JM, Farnot U, et al. WHO Antenatal care randomised trial for the evaluation of a new model of routine antenatal care. Lancet. (2001) 357(9268):1551–64. doi: 10.1016/S0140-6736(00)04722-X
52. Langer A, Villar J, Romero M, Nigenda G, Piaggio G, Kuchaisit C, et al. Are women and providers satisfied with antenatal care? Views on a standard and a simplified, evidence-based model of care in four developing countries. BMC Women’s Health. (2002) 2(1):1–10. doi: 10.1186/1472-6874-2-7
53. Raine R, Cartwright M, Richens Y, Mahamed Z, Smith D. A qualitative study of women’s experiences of communication in antenatal care: identifying areas for action. Matern Child Health J. (2010) 14(4):590–9. doi: 10.1007/s10995-009-0489-7
54. Teka TT, Feyissa TR, Melka AS, Bobo FT. Role of antenatal and postnatal care in contraceptive use during postpartum period in western Ethiopia: a cross sectional study. BMC Res Notes. (2018) 11(1):1–6. doi: 10.1186/s13104-017-3088-5
55. Do M, Hotchkiss D. Relationships between antenatal and postnatal care and post-partum modern contraceptive use: evidence from population surveys in Kenya and Zambia. BMC Health Serv Res. (2013) 13(1):1–14. doi: 10.1186/1472-6963-13-1
56. Taye EB, Mekonen DG, Debele TZ. Prevalence of post partum modern family planning utilization and associated factors among postpartum mothers in Debre Tabor town, North West Ethiopia, 2018. BMC Res Notes. (2019) 12(1):1–7. doi: 10.1186/s13104-018-4038-6
57. Knodel J, Chayovan N. Contraceptive initiation patterns in Thailand. Popul Stud (Camb). (1990) 44(2):257–71. doi: 10.1080/0032472031000144586
58. Huffman SL, Ford K, Allen J, Hubert A, Streble P. Nutrition and fertility in Bangladesh: breastfeeding and post partum amenorrhoea. Popul Stud (Camb). (1987) 41(3):447–62. doi: 10.1080/0032472031000142996
59. Huang Y-M, Merkatz R, Kang J-Z, Roberts K, Hu X-Y, Di Donato F, et al. Postpartum unintended pregnancy and contraception practice among rural-to-urban migrant women in Shanghai. Contraception. (2012) 86(6):731–8. doi: 10.1016/j.contraception.2012.05.007
60. Mohammed F, Musa A, Amano A. Prevalence and determinants of unintended pregnancy among pregnant woman attending ANC at Gelemso General Hospital, Oromiya Region, East Ethiopia: a facility based cross-sectional study. BMC Women’s Health. (2016) 16(1):1–7. doi: 10.1186/s12905-016-0335-1
61. Mehare T, Mekuriaw B, Belayneh Z, Sharew Y. Postpartum contraceptive use and its determinants in Ethiopia: a systematic review and meta-analysis. Int J Reprod Med. (2020) 2020. doi: 10.1155/2020/5174656
62. Dagnew GW, Asresie MB, Fekadu GA, Gelaw YM. Modern contraceptive use and factors associated with use among postpartum women in Ethiopia; further analysis of the 2016 Ethiopia demographic and health survey data. BMC Public Health. (2020) 20:1–9. doi: 10.1186/s12889-020-08802-6
63. Elweshahi HMT, Gewaifel GI, Sadek SSE-D, El-Sharkawy OG. Unmet need for postpartum family planning in Alexandria, Egypt. Alexandria J Med. (2018) 54(2):143–7. doi: 10.1016/j.ajme.2017.03.003
64. Tawiah E. Factors affecting contraceptive use in Ghana. J Biosoc Sci. (1997) 29(2):141–9. doi: 10.1017/S0021932097001417
65. Rutaremwa G, Kabagenyi A, Wandera SO, Jhamba T, Akiror E, Nviiri HL. Predictors of modern contraceptive use during the postpartum period among women in Uganda: a population-based cross sectional study. BMC Public Health. (2015) 15(1):1–9. doi: 10.1186/s12889-015-1611-y
66. Aqeel T, Shabbir A, Basharat H, Bukhari M, Mobin S, Shahid H, et al. Prevalence of self-medication among urban and rural population of Islamabad, Pakistan. Trop J Pharm Res. (2014) 13(4):627–33. doi: 10.4314/tjpr.v13i4.22
67. Asratie MH, Muche AA, Geremew AB. Completion of maternity continuum of care among women in the post-partum period: magnitude and associated factors in the northwest, Ethiopia. PLoS One. (2020) 15(8):e0237980. doi: 10.1371/journal.pone.0237980
68. Muluneh AG, Kassa GM, Alemayehu GA, Merid MW. High dropout rate from maternity continuum of care after antenatal care booking and its associated factors among reproductive age women in Ethiopia, evidence from demographic and health survey 2016. PLoS One. (2020) 15(6):e0234741. doi: 10.1371/journal.pone.0234741
Keywords: early initiation, EDHS, Ethiopia, family planning, post-partum period
Citation: Asratie MH, Tesema GA, Chilot D, Aragaw FM, Merid MW and Belay DG (2023) Socio-demographic and antenatal care-related factors associated with early post-partum family planning use in Ethiopia: evidence from Ethiopian Demographic and Health Survey 2016 data. Front. Glob. Womens Health 4:1131143. doi: 10.3389/fgwh.2023.1131143
Received: 24 December 2022; Accepted: 20 July 2023;
Published: 1 September 2023.
Edited by:
Fatema Khatun, International Centre for Diarrhoeal Disease Research (ICDDR), BangladeshReviewed by:
Zahra Hoodbhoy, Aga Khan University, Pakistan© 2023 Asratie, Tesema, Chilot, Aragaw, Merid and Belay. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Melaku Hunie Asratie bWVsYWtodW5pZTI3QGdtYWlsLmNvbQ==
Abbreviations ANC, antenatal care; AOR, adjusted odds ratio; CI, confidence interval; DHS, Demographic and Health Survey; EDHS, Ethiopian Demographic and Health Survey; EAs, enumeration areas; ICC, intra-class correlation coefficient; MOR, median odds ratio; PCV, proportion change in variance; PHC, population and housing census; PPFP, post-partum family planning.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.