- Department of Gynecology and Obstetrics, School of Medicine, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: Oligohydramnios is a pregnancy condition characterized by low volume of amniotic fluid. Based on ultrasound measurement, it is defined as a single maximum vertical pocket of liquor less than 2 cm or summation of four quadrants vertical pockets of liquor measurement less than 5 cm. It is associated with multiple adverse perinatal outcomes (APO) and complicates 0.5%–5% of pregnancies.
Objective: To assess magnitude and associated factors of adverse perinatal outcome among women with oligohydramnios at 3rd trimester at University of Gondar Comprehensive Specialized Hospital, North West Ethiopia
Methods: Institution based cross-sectional study was employed from April 1 to September 30, 2021 in which 264 participants were involved. All women with oligohydramnios at 3rd trimester who meet the inclusion criteria were included. Semi- structured questionnaire was used for data collection after Pre-tested. Collected data was checked for completeness; clarity then coded and entered using Epi data version 4.6.0.2 then exported to STATA version 14.1 for analysis.
Result: The magnitude of APO was 46.6% (95%CI: 40.5–52.7%). Null parity [AOR = 2.2, 95%CI (1.2–4.2)], presence of hypertensive disorders of pregnancy (HDP) [AOR = 4.9, 95%CI (2.0–12.1)] and presence of intrauterine growth restriction (IUGR) [AOR = 8.4, 95%CI (3.5–20.2)] were found to be predictors of APO.
Conclusion: Third trimester oligohydramnios is associated with APO. The presence of HDP, IUGR and being nulliparous were predictors of APO.
Introduction
Amniotic fluid (AF) is necessary for normal development of fetal respiratory, gastrointestinal, urinary tract, and musculoskeletal systems. It is also important for the continued fetal growth in a nonrestricted, sterile and thermally controlled environment (1, 2). AF volume is affected by varies conditions such as postmaturity syndrome; maternal diseases like hypertension, diabetes in pregnancy (especially poorly controlled), autoimmune disorders; maternal medications (prostaglandin synthetase inhibitors); altitude; fetal anomalies (including both immune and nonimmune fetal hydrops); and fetal weight (macrosomic and growth restricted) (1–3).
At third trimester the volume of AF is from fetal urination, lung secretion, fetal swallowing, and intramembranous absorption (4).
Oligohydraminos is usually diagnosed based on ultrasound measurement of amniotic fluid volume and considered when amniotic Fluid Index (AFI) is less than 5 cm or a single deepest pocket of amnionic fluid is below 2 cm (2, 3). Oligohydramnios at third trimester affects 1%–5% of pregnancies (5, 6).
Complications associated with oligohydramnios depend on the gestation at which the diagnosis is made. If the diagnosis of oligohydraminos early in pregnancy, it is often associated with more serious complications such as compression of fetal organs resulting in birth defects, pulmonary hypoplasia and increased risk of miscarriage or stillbirth. Whereas latter in pregnancy, the complications are IUGR, preterm birth, intra uterine fetal demise, intra-partum fetal distress and birth asphyxia. During labor, it can cause cord compression, meconium-stained fluid, abnormal fetal heart rate, operative interventions, and increased risk of cesarean delivery, lower Apgar scores, intensive care unit admission and neonatal death (2, 3, 7–11).
Oligohydraminos associated composite adverse perinatal outcomes varying between 9.7%–38.1% (6, 12). Meconium stained amniotic fluid (MSAF), non-reassuring fetal heart rate pattern (NRFHRP), prematurity, low birth weight, low 5th minute Apgar score, birth asphyxia, IUGR, respiratory distress, early neonatal death and still births are some of the adverse perinatal outcomes associated with oligohydraminos (9, 13–18).
Occurrence of adverse perinatal outcomes in oligohydraminos depends on the extent of oligohydramnios, and the presence of other factors like post term pregnancy, IUGR, presence of hypertensive disorders of pregnancy, gravidity, ANC booking, non-reactive NST, Gestational age at delivery and the cause of oligohydramnios (6, 19–25).
There has been a trend of delivering a fetus if diagnosis of oligohydraminos made at third trimester of pregnancy fearing occurrence of adverse perinatal outcomes. There is also dilemma about the route of delivery especially in set ups where there is no intrapartum electronic fetal heart rate monitoring like Ethiopia where this study was done (12–13, 26–30). There is scarcity of evidences which assess the perinatal outcomes associated with oligohydramnios at third trimester.Thus, this study was aimed to assess the magnitude and associated factors of adverse perinatal outcomes among women with oligohydramnios at third.
Materials and methods
Study design, period and setting
Institution based cross-sectional study was employed among pregnant mothers with oligohydramnios at third trimester who were attended at university of Gondar comprehensive specialized hospital from April to September 2021.University of Gondar is one of the pioneer teaching hospitals in North West Ethiopia in previous capital of Ethiopia, Gondar city. The hospital gives service for more than 7 million people in its catchment and has 700 beds of which 177 beds belonged to obstetrics and gynecology services. Its ANC clinic and labor ward provide care for 9,000 and 900 pregnant women monthly respectively.
Study population and inclusion/exclusion criteria
All pregnant women who had oligohydramnios at 3rd trimester and attended maternity unit of university of Gondar comprehensive specialized hospital were included. Whereas women with PROM [N = 15], who cannot communicate, mentally and severely ill, diagnosed IUFD at presentation, with lethal congenital anomaly [N = 3], with unknown or unreliable date or with absence of early milestones to date the pregnancy [N = 22] were excluded.
Sample size determination
The sample size was estimated using single population proportion formula. By considering, 95% confidence level, 5% margin of error, composite adverse perinatal outcome of 38.1% in similar setting (6) and 10% of non-responsive rate the final sample size became 398.
Sampling technique and procedure
A consecutive sampling technique was used to include all women with oligohydramnios at 3rd trimester who meet the inclusion criteria during the study period.
Study variables
After the identification of patients fulfilling the inclusion criteria, baseline data were collected from the patients and clinical variables which cannot be provided by the patient were retrieved from medical records.
Oligohydramnios was considered when AFI ≤ 5 cm or a single deepest pocket of amniotic fluid ≤ 2 cm.
Adverse perinatal outcome was considered if one of the following present Low Apgar score (5th Apgar score < 7), low birth weight, neonatal intensive unit (NICU) admission, perinatal death, MSAF, NRFHR, perinatal asphyxia.
Data collection procedures
Data collection was made by trained medical interns and obstetrics and gynecology residents using Amharic pretested semi-structured questionnaires adapted from similar researches. Written informed consent of participants were obtained after the purpose of the study was clearly explained then Interviewer administered questionnaire.
Data quality assurance
The questionnaire was first developed in English and translated into Amharic language then back to English and consistency was checked. Two-days training was made to the data collectors and 5% questionnaires were pretested on similar setting. The training session covers the overall objective of the study, definition of terms and concepts, approaching of respondents, data collection tools and techniques of interviewing. The collected data was also cross-checked for its completeness, consistency, accuracy, and clarity on a daily basis. Daily supervision of data collectors was carried out throughout data collection period.
Data processing and analaysis
Data was coded and entered using epi data version 4.6.0.2 then exported to STATA version 14.1. Further data clean-up for completeness clarity and recoding was done on STATA before the actual analysis. Descriptive statistics like frequency, percentage, mean, and standard deviation was done to describe the study population in relation to different variables. A chi-square test was done for all variables to check for the assumptions. Stepwise Logistic regression analysis was carried out to identify the independent factors associated with adverse perinatal outcome. Variables having p-value ≤ 0.2 from the bivariable analysis was included for the final multivariable logistic regression and variables having P- value <0.05 was considered to have a significant association with adverse perinatal outcome. An adjusted odds ratio with 95% CI was used as a measure of association.
Ethical considerations
The ethical clearance was obtained from the ethical review committee of the school of medicine, College of medicine and health sciences, on behalf of Institutional Review Board (IRB) of university of Gondar(Dr. Mulugeta Ayalew, Director of school of Medicine, reference number: 643/2021).
Results
Socio-demographic characteristics of the study participants
Two hundred sixty four women participated in the study. Three-fourth of the participants were from the urban setting [N = 198, 75%] and majority were within the age group of 20–34 years [N = 225, 85.29%]. The mean age was 27.36 ± 4.85 years [18–40 years] (Table 1).
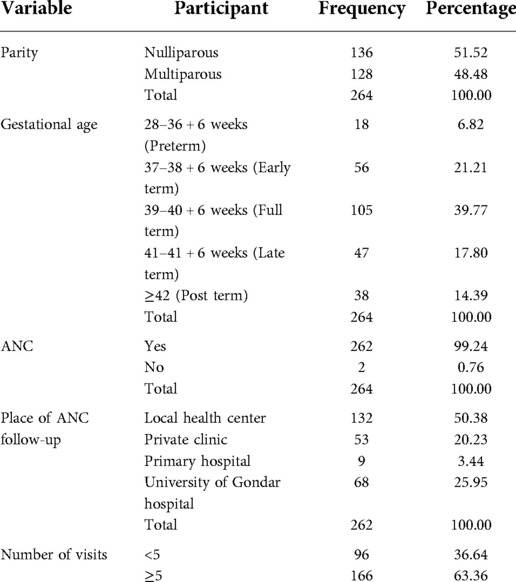
Obstetric characteristics of participants
Nearly half of the study participants were nulliparous (51.5%). At delivery forty percent of participants (39.8%) were full term; 14.4% were post term and 6.8% were preterm. The mean gestational age at diagnosis of oligohydraminos was 40 ± 2 weeks [30 + 4–44 weeks] (Table 2).
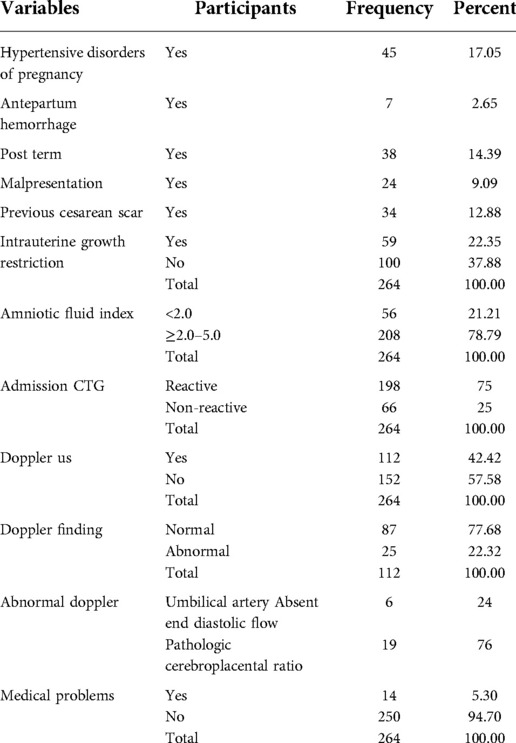
Antepartum obstetric and medical problems
Among participants 62.1% were having antepartum obstetric problems like IUGR (22.4%), HDP (17.1%), post-term (14.4%), and previous cesarean scar (12.9%). Fourteen (5.3%) participants had medical problems such as malaria (five cases), anemia (three cases), HIV/AIDS (three cases), hyperthyroidism (two) and one case with epilepsy. Majority (78.8%) of the participants had amniotic fluid index of 2 cm–5 cm.
At admission three-fourth of the participants had reactive non stress test (NST), and 25% of them had non-reactive NST. Umbilical artery Doppler study was done for 112 participants and 77.7% were normal and 22.3% were abnormal study. Among the abnormal Doppler findings six (24%) were absent end diastolic flow while 76% were abnormal Doppler (Table 3).
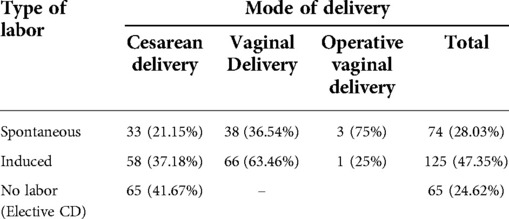
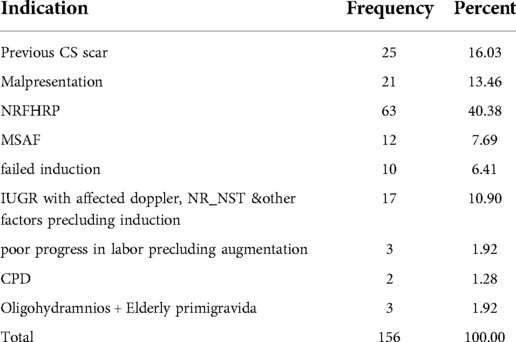
Mode of delivery
Labor started spontaneous in 28.0%, and induced in 47.4% with trans-cervical balloon catheter and oxytocin. Cesarean section (CS) was done for 59.1% of the participants of which 40% had elective CS.There was no cesarean delivery for the mere presence of oligohydraninos alone (Tables 4, 5).
Perinatal outcome
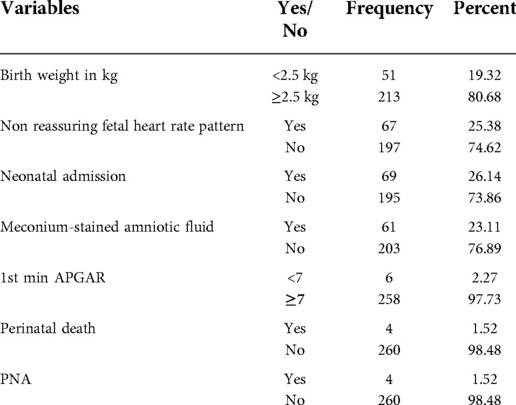
The rate of adverse perinatal outcome was 46.6% [95%CI, 40.5–52.7%]. The frequency of adverse outcomes were low birth weight (19.3%), non-reassuring fetal heart rate pattern (25.4%), neonatal admission (26.1%), Meconium-stained amniotic fluid (23.1%), low 1st minute APGAR (2.3%), perinatal asphyxia (1.5%) and 4 perinatal deaths. Among the perinatal deaths, one was intrapartam death; the three were early neonatal deaths. Sixty-nine neonates were admitted to NICU with diagnosis of RDS [N = 25, 36.23%], MAS [N = 18, 26.08%], neonatal sepsis [N = 23, 33.33%] (Table 6).
Factors associated with adverse perinatal outcome
Adverse perinatal outcomes were increased by two-fold in nulliparous compared to multiparous [AOR = 2.2, 95%CI: 1.2–4.2]. Mothers whose pregnancy complicated with IUGR had eight-fold increase risk of adverse perinatal outcomes compared to mothers with no IUGR [AOR = 8.4, 95%CI: 3.5–20.1]. Similarly in women with hypertensive disorders of pregnancy the odds of experiencing adverse perinatal outcome were found to be increased by nearly five-fold as compared to women with no hypertensive disorders of pregnancy [AOR = 4.933, 95%CI: 2.015–12.077] (Table 6, 7).
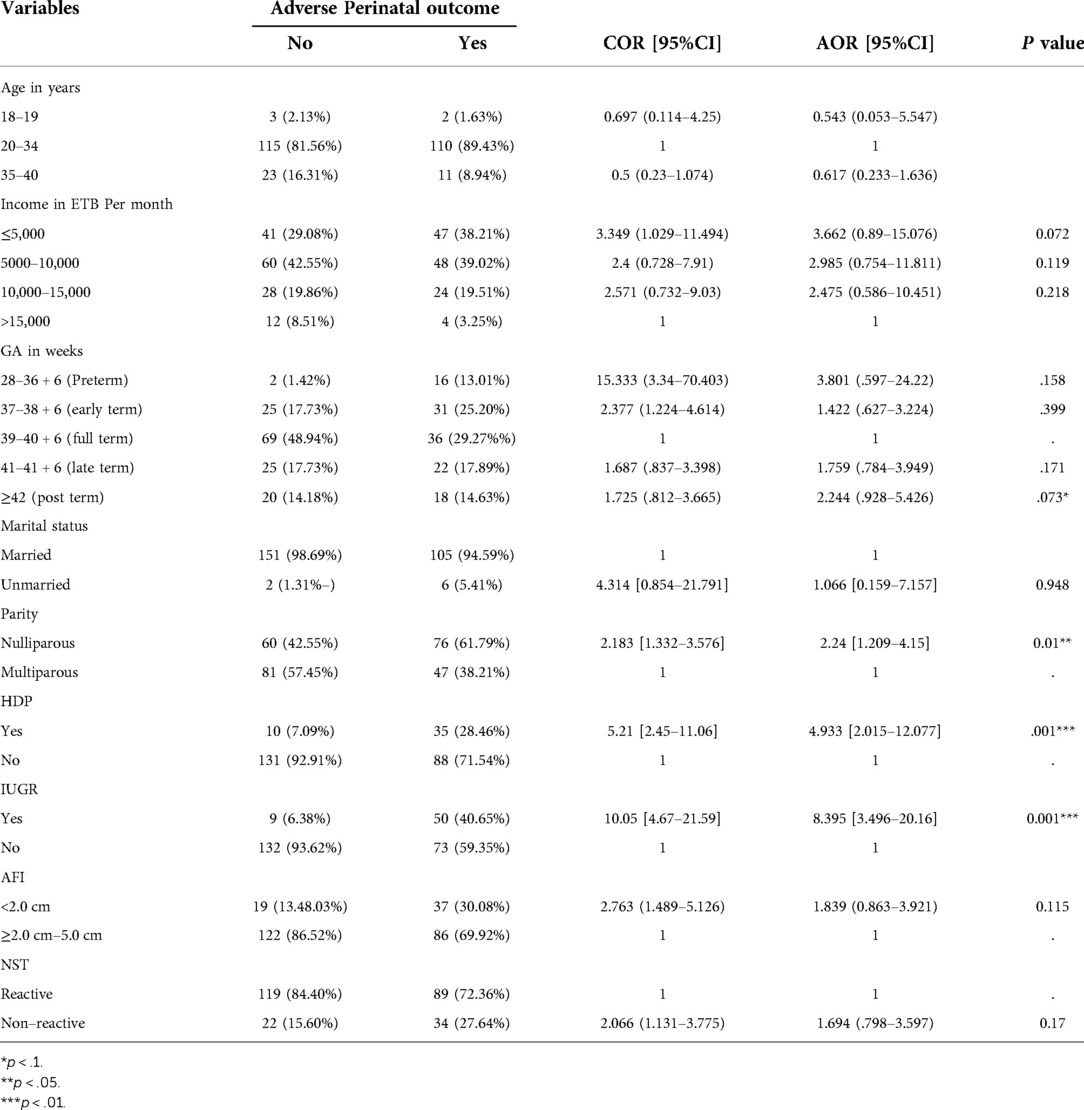
Table 7. Bivariate and multivariable analysis of factors associated with adverse perinatal outcome, 2021.
Discussion
In this study 264 study participants were involved and majority were in the age group of 20–34 years [N = 225, 85.3%] with mean age being 27.4 ± 4.9 years [18–40 years] which is similar with study done in Mekele, Ethiopia(85.3% vs. 89.4%) (6). This shows that most of the oligohydraminos were among women whose age group is said to be favorable for better pregnancy outcomes. The gestational age was full term for 40% of participants, and the mean gestational age was 40 ± 2 weeks [30 + 4 – 44 weeks] which showed most of the deliveries were in gestational age group assumed to have at lower risk to develop adverse perinatal outcomes. Slightly more than half (51.0%) of the participants were nulliparous, this might show most of the participants were at increased risk for developing nulliparous related obstetric problems and labor abnormalities.
Labor was spontaneous in 28.0% and induced in 47.4% of the participants. Of all participants 59.1% delivered by cesarean and 39.4% were vaginal. This shows that the presence of oligohydramnios is a major risk for having cesarean delivery. However, it is lower than previous studies with CD rate varied 69.9–80.3%, and vaginal delivery varied [19.7–30.1% (5, 6)].
In this study the rate of adverse perinatal outcome was 46.6%. Compared to similar study done in Israel the rate of composite adverse outcome was found to be higher [9.7%]. (12). This can be explained by the difference in obstetric profile of study participants as the study in Israel included only cases with isolated oligohydramnios at term. This difference might also be explained by the study in Israel uses fetal PH assessment as an adverse outcome and this may reduce cases of NRFHR pattern while in our study we have no PH assessment and may increase cases of NRFHRP.
This finding was also higher than similar study done in Ethiopia [38.1%] (6). This can be explained by the high number of cases with other obstetric problems HDP [17.05 vs. 6.2%], IUGR [22.35 vs. 11.72%] in this study. This may also be explained by the high number of NRFHR cases in our study which can be detected with CTG monitoring.
The rate of individual adverse outcomes also found to be higher than previous study done in Ethiopia, NICU admission rate [26.14 vs. 15.4%], NRFHRP [25.38 vs. 15.8%], MSAF [23.11 vs. 9.2%] while LBW almost similar [19.32 vs. 19.8%]. This can be explained by better detection of fetal heart rate abnormalities with CTG and better antepartum fetal evaluation with maternal fetal medicine fellows (31).
As compared to another previous study done in Ethiopia on similar setting the rate of adverse perinatal outcomes was found to be higher, LBW [19.32 vs. 11.5%], NICU admission [26.14 vs. 10.5%] &MSAF [23.11 vs. 12.88] (5). This can be explained by higher number of isolated oligohydramnios and elective cesarean delivery in the previous study. Alternatively, it may be explained by the previous study was conducted on term pregnancy as compared to ours which includes all 3rd trimester cases.
As compared to similar studies done in India and Texas (United States) the rate of adverse outcomes was found to be lower, LBW [19.32% vs. 26.6%–38.6%], NICU admission [26.14% vs. 24%–40%], NRFHR [25.38% vs. 48%] (3, 17, 32–33).
Parity, presence of hypertensive disorders of pregnancy, presence of intrauterine growth restriction was found to be associated with development of adverse perinatal outcome. This was similar with a study done in Ethiopia and India which reported hypertensive disorders and IUGR as associated factors (6, 34).
The high rate of adverse fetal outcome in nulliparous may be explained by increased risk for other obstetric problems like HDP (53.33% vs. 46.67%) and IUGR (57.63% vs. 42.67%) as compared to multiparous and labor abnormalities with its associated increased fetal risk. This may also be explained compared to previous studies done in Ethiopia in which the presence of these factors leading to elective and emergency cesarean delivery in our study they were allowed to labor unless they have emergency fetal indication.
Strength and limitation of the study
Done on primary data where there is limited evidence on oligohydraminos associated adverse outcomes. However, the fact it is a cross-sectional study, it may not be sufficient enough to identify adverse outcomes and associated factors.
Conclusion
This study found that mothers with oligohydramnios at 3rd trimester are at increased risk of developing adverse perinatal outcome. The presence of HDP, IUGR and nulliparous were found to be predictors of adverse perinatal outcome. However, development of adverse perinatal outcomes was not associated with type of labor and delivery (spontaneous, induced or elective CD).
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by The ethical clearance was obtained from the ethical review committee of the school of medicine, College of medicine and health sciences, on behalf of the Institutional Review Board (IRB) of the University of Gondar (Dr. Mulugeta Ayalew, Director of School of Medicine, reference number: 643/2021). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
MM, WT and ZM participated in the conceptualization, formal analysis, investigation, methodology, supervision, visualization, writing-original draft, writing-review and editing, and approving the final draft. All authors read and approved the manuscript. All authors contributed to the article and approved the submitted version.
Funding
We would like to mention University of Gondar comprehensive specialized teaching hospital for supporting and giving chance to do this study.
Acknowledgments
We would like to extend our gratitude to those involved in the data collection process and University of Gondar Comprehensive Specialized Hospital administrators for permitting access to patients' records.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AF, amniotic fluid; AFI, amniotic fluid index; ANC, antenatal care; CD, cesarean delivery; CI, confidence interval; CM, centimeter; CS, cesarean section; CST, contraction stress test; CTG, cardiotocography; DM, diabetes mellitus; ED, early deceleration; EFM, electronic fetal monitoring; ETB, ethiopian birr; FGR, fetal growth restriction; FHR, fetal heart rate; FHRP, fetal heart rate pattern; GDM, gestational diabetes mellitus; IUFD, Intrauterine fetal death; IUGR, intra uterine growth restriction; KM, kilometer; LD, late deceleration; ML, milliliter; NICU, neonatal intensive care unit; NRFHR, non reassuring fetal heart rate; NST, non stress test; PD, prolonged deceleration; PPH, postpartum hemorrhage; PROM, premature rupture of membranes; SDVP, single deepest vertical pocket; SPSS, statistical package for social science; VD, variable deceleration.
References
1. Lockwood CJ, Moore T, Copel J, Silver RM, Resnik R, Dugoff L, et al. Philadelphia: Elsevier (2015). Creasy & resnik's maternal- fetal medicine, principles and practice. 7th ed.
2. Sherer DM. A review of amniotic fluid dynamics and the enigma of isolated oligohydramnios. Am J Perinatol. (2002) 19(05):253–66. doi: 10.1055/s-2002-33084
3. Casey BM, McIntire DD, Bloom SL, Lucas MJ, Santos R, Twickler DM, et al. Pregnancy outcomes after antepartum diagnosis of oligohydramnios at or beyond 34 weeks’ gestation. Am J Obstet Gynecol. (2000) 182(4):909–12. doi: 10.1016/s0002-9378(00)70345-0
4. Brace RA. Physiology of amniotic fluid volume regulation. Clin Obstet Gynecol. (1997) 40(2):280–9. doi: 10.1097/00003081-199706000-00005
5. Minwuye T. Severe oligohydramnios at term pregnancy and associated factors among pregnant women admitted from June 1, 2015 to June 30, 2017 at gondar university specialized hospital, northwest Ethiopia. Acta Sci Women's Health. (2019) 1:2–7.
6. Teka H, Gidey H, Gebreezgabher T, Yemane A, Ebuy H, Berhe Y, et al. Determinants of maternal and neonatal outcomes of oligohydramnios after 37+0 weeks of gestation in mekelle public hospitals, northern Ethiopia. Mekelle: Research square (2020).
7. Demasio K, Kuba K. Strip of the month: term oligohydramnios and prolonged decelerations. NeoReviews. (2018) 19(10):e620–e32. doi: 10.1542/neo.19-10-e620
8. Chauhan N, Namdeo P, Modi J. Evidence based management of oligohydramnios. Bhopal: Medwin Publishers (2018).
9. Chate P, Khatri M, Hariharan C. Pregnancy outcome after diagnosis of oligohydramnios at term. Int J Reprod Contracept Obstet Gynecol. (2013) 10(1):23–6. doi: 10.5455/2320-1770.ijrcog20130204
10. Hamed A, Mohamed G. Pregnancy outcome among patients with oligohydramnios and suggested plan of action. IOSR J Nurs Health Sci (IOSR-JNHS). (2015) 4(5):65–75. doi: 10.9790/1959-04536575
11. Shenker L, Reed KL, Anderson CF, Borjon NA. Significance of oligohydramnios complicating pregnancy. Am J Obstet Gynecol. (1991) 164(6):1597–600. doi: 10.1016/0002-9378(91)91442-Y
12. Ashwal E, Hiersch L, Melamed N, Aviram A, Wiznitzer A, Yogev Y. The association between isolated oligohydramnios at term and pregnancy outcome. Arch Gynecol Obstet. (2014) 290(5):875–81. doi: 10.1007/s00404-014-3292-7
13. Hou L, Wang X, Hellerstein S, Zou L, Ruan Y, Zhang W. Delivery mode and perinatal outcomes after diagnosis of oligohydramnios at term in China. J Matern Fetal Neonatal Med. (2020) 33(14):2408–14. doi: 10.1080/14767058.2018.1553944
14. Figueroa L, McClure EM, Swanson J, Nathan R, Garces AL, Moore JL, et al. Oligohydramnios: a prospective study of fetal, neonatal and maternal outcomes in low-middle income countries. Reprod Health. (2020) 17(1):19. doi: 10.1186/s12978-020-0854-y
15. Nazlima N, Fatima B. Oligohydramnios at third trimester and perinatal outcome. Bangladesh J Medical Sci. (2012) 11(1):33–6. doi: 10.3329/bjms.v11i1.9820
16. Alchalabi HA, Obeidat BR, Jallad MF, Khader YS. Induction of labor and perinatal outcome: the impact of the amniotic fluid index. Eur J Obstet Gynecol Reprod Biol. (2006) 129(2):124–7. doi: 10.1016/j.ejogrb.2005.10.039
17. Hasegawa J, Matsuoka R, Ichizuka K, Kotani M, Ohmori A, Nakamura M, et al. Intrapartum fetal heart rate pattern in oligohydramnios. Fetal Diagn Ther. (2008) 24(3):267–70. doi: 10.1159/000151674
18. Tiparse A, Kalathiya B, Bajaj P. Ultrasound evaluation of pregnancies with oligohydramnios in third trimester and their feto-maternal outcome at tertiary care hospital. J Res Med Sci. (2017) 5(8):3292–8. doi: 10.18203/2320-6012.ijrms20173099
19. Elsandabesee D, Majumdar S, Sinha S. Obstetricians’ attitudes towards “isolated” oligohydramnios at term. J Obstet Gynaecol. (2007) 27(6):574–6. doi: 10.1080/01443610701469669
20. Rossi AC, Prefumo F. Perinatal outcomes of isolated oligohydramnios at term and post-term pregnancy: a systematic review of literature with meta-analysis. Eur J Obstet Gynecol Reprod Biol. (2013) 169(2):149–54. doi: 10.1016/j.ejogrb.2013.03.011
21. Tuladhar A, editor. Perinatal outcome of term pregnancies with borderline amniotic fluid index at Nepal medical college and teaching hospital. Kathmandu: Nepal Med Coll J (2016).
22. Biradar K, Shamanewadi A. Maternal and perinatal outcome in oligohydramnios: study from a tertiary care hospital, bangalore, Karnataka, India. Int J Reprod Contracept Obstet Gynecol. (2016) 5:2291–4. doi: 10.18203/2320-1770.ijrcog20162113
23. Hoskins IA, Frieden FJ, Young BK. Variable decelerations in reactive nonstress tests with decreased amniotic fluid index predict fetal compromise. Am J Obstet Gynecol. (1991) 165(4):1094–8. doi: 10.1016/0002-9378(91)90478-A
24. Rizvi S, Farooq S, Farooq M. A study of oligohydramnios at term on maternal and fetal outcome. Int J Adv Res. (2017) 5(10):652–5. doi: 10.21474/IJAR01/5571
25. Chauhan R, Sahni S, Dubey A. A study on fetal outcome in patients with oligohydramnios. Int J Reprod Contracept Obstet Gynecol. (2019) 8(2):665. doi: 10.18203/2320-1770.ijrcog20190302
26. Jagatia K, Singh N, Patel S. Maternal and fetal outcome in oligohydramnios: a study of 100 cases. Int J Med Sci Public Health. (2013) 2(3):724–7. doi: 10.5455/ijmsph.2013.070520132
27. Jagatia K, Singh N, Patel S. Maternal and fetal outcome in oligohydramnios- study of 100 cases. Int J Med Sci Public Health. (2013) 2(3):724–27. doi: 10.5455/ijmsph.2013.070520132
28. Shrem G, Nagawkar SS, Hallak M, Walfisch A. Isolated oligohydramnios at term as an indication for labor induction: a systematic review and meta-analysis. Fetal Diagn Ther. (2016) 40(3):161–73. doi: 10.1159/000445948
29. Bangal VB, Giri PA, Sali BM. Incidence of oligohydramnios during pregnancy and its effects on maternal and perinatal outcome. J Pharm Biomed Sci (JPBMS). (2011) 12(5):1–4.
30. Chiniwar MA, Joe Kaushik M, Menasinkai SB. Maternal and fetal outcome in oligohydramnios after 34 weeks of gestation. Int J Reprod Contracept Obstet Gynecol. (2015) 7(11):4604–8. doi: 10.18203/2320-1770.ijrcog20184515
31. Destegül E, Akkaya H, Büke B, Gürer G. Evaluation of cerebroplacental ratio as a new tool to predict adverse perinatal outcomes in patients with isolated oligohydramnios. J Surg Med. (2020) 4(12):1169–72. doi: 10.28982/josam.829499
32. Chiniwar MA, Menasinkai SB. Maternal and fetal outcome in oligohydramnios after 34 weeks of gestation. Int J Reprod Contracept Obstet Gynecol. (2018) 7(11):4604–9.
33. Jakatia K, Singh N, Patel S. Maternal and fetal outcomes in oligohydromnios: a study of 100 cases. Int J Med Sci Public Health. (2013) 2(3):724–7.
Keywords: oligohydramnios, adverse perinatal outcome, gondar, Ethiopia, oligohydraminos, adverse perinaqtal outcome
Citation: Molla M, Mengistu Z, Tsehaye W and Sisay G (2023) Magnitude and associated factors of adverse perinatal outcomes among women with oligohydramnios at 3rd trimester at University of Gondar comprehensive specialized hospital, North West Ethiopia. Front. Glob. Womens Health 3:958617. doi: 10.3389/fgwh.2022.958617
Received: 31 May 2022; Accepted: 29 November 2022;
Published: 30 January 2023.
Edited by:
Wessel Ganzevoort, Academic Medical Center, NetherlandsReviewed by:
Mustafa Kaplanoglu, Cukurova University, TurkeyTanbir Najrana, Brown University, United States
© 2023 Molla, Mengistu, Tsehaye and Sisay. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zelalem Mengistu ZW11c2hlMTBAeWFob28uY29t
Specialty Section: This article was submitted to Maternal Health, a section of the journal Frontiers in Global Women's Health
 Mezigebu Molla
Mezigebu Molla Zelalem Mengistu
Zelalem Mengistu Winta Tsehaye
Winta Tsehaye