
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Glob. Womens Health , 02 December 2022
Sec. Contraception and Family Planning
Volume 3 - 2022 | https://doi.org/10.3389/fgwh.2022.938027
Background: In many low- and middle-income countries (LMIC), men are the key decision-makers and chief providers, often determining women's access to economic resources and maternal health services. Despite the important role of men in maternal healthcare, the involvement of male partners in maternal and child health in LMIC, including Ethiopia, is low.
Objectives: This study aims to assess the extent of male involvement and associated factors in antenatal care (ANC) service utilization in the Bench Sheko zone, Southwest, Ethiopia.
Methods: A community-based, cross-sectional study was conducted in the Bench Sheko zone from February to May 2021. A multistage sampling technique was employed to select study participants. Variables with p-values <0.25 in binary logistic regression were selected as candidates for multiple logistic regression to determine independent factors associated with male involvement adjusting for sociodemographic, health service, personal, environmental, and knowledge-related factors.
Results: A total of 816 men took part in the study, with a 98.2% response rate. The prevalence of male involvement in ANC utilization was 38.2%. In multivariate analyses, residence (urban), age (25–34), education (diploma and above), income (≥2,500 Ethiopian Birr, ETB), and high knowledge of the advantages of ANC were shown to be positively associated with male involvement in ANC utilization.
Conclusion: Male involvement in ANC utilization was low. Considering the importance of male involvement in maternal healthcare, we advocate for policies and strategies that can improve knowledge of the advantages of ANC among men and can enhance their engagement in maternal care. Special attention should be given to younger partners and those partners who live in rural areas.
Male involvement in antenatal care (ANC) utilization can encompass many things including discussing maternal health issues with one's spouse/partner, making a joint decision as a couple about the spacing of a pregnancy, utilization of maternal services, and accompanying one's partner to seek ANC in a health facility (1). In the late 1990s, there was increased recognition of the importance of including men in maternal and newborn health (MNH) programs. Research indicates several mechanisms by which male involvement in MNH can support improved maternal and child health outcomes (2, 3). For example, engaging men in maternal and newborn health can increase care-seeking, improve home care practices, and support more equitable couple communication and decision-making for maternal and newborn health (4).
Male involvement enables men to support their spouses to utilize obstetric services and for the couple to adequately prepare for birth complications. This leads to a reduction in all three phases of obstetric delay: delay in the decision to seek care, delay in reaching care, and delay in receiving care (5). Male partners can play a crucial role in the first and second phases of delay in low- and middle-income countries (LMIC), and thereby positively impact birth outcomes (6,7).
In patriarchal communities in LMIC, men are the key decision-makers and chief providers, often determining women's access to economic resources (5). Women initiate ANC, but men often make decisions about care utilization (8). Male involvement in reproductive health has been promoted as a promising strategy for improving maternal and child health (MCH) as male involvement can play a vital role in ensuring safe pregnancy, delivery, and moral support to women (9, 10). However, more limited attention has been placed on male partners' involvement in maternity care in LMIC (5, 9). A study conducted in the North Gondar zone, Northwest Ethiopia, found that men's level of knowledge about obstetric danger signs, being married, completing college education, escorting their wife to antenatal care, and urban residence were predictors of male involvement in the maternal healthcare system (11).
The tendency to view maternal health as a woman's issue has contributed to a narrow focus that targets mostly women in intervention efforts. Most MCH programs seek to address the health needs of women and children by engaging and educating pregnant women and mothers in care-seeking practices for themselves and their children. This has contributed to men being sidelined as far as reproductive health and MCH matters are concerned (6, 7, 12).
In Ethiopia, the levels of maternal morbidity and mortality are among the highest in the world. According to estimates by World Health Organization (WHO) and UNICEF, the maternal mortality rate (MMR) in 2017 was 401 per 100,000 live births (13), which is more than 40 and 60 times higher than that of Europe and Australia, respectively (10). According to the United Nations' new Sustainable Development Goals (SDGs), all countries should reduce their MMR by at least two-thirds. The average global target is an MMR of less than 70/100,000 live births by 2030. The supplementary national target is that no country should have an MMR greater than 140/100,000 live births (10).
Despite the important role of men in maternal health, the involvement of male partners in MCH in LMIC, including Ethiopia, is low. Only 23.1% male partners have physically entered the ANC room with their wives in Addis Ababa (14). Another study from Gondar reported that only 40.1% husbands were involved in HIV counseling and testing during their wife's pregnancy (15). Available studies have explored the perspectives of women, but often not men. Furthermore, previous studies were not comprehensively assessing the role of males in the ANC of their partners. The current study seeks to assess male involvement in ANC and associated factors in the Bench Sheko zone, Southwest Ethiopia.
The study was conducted in the Bench Sheko zone, which is one of the zones of the Ethiopian Southwest region. Mizan Aman is an administrative city, which is located 585 km southwest of the capital, Addis Ababa. The Bench Sheko zone is divided into six woredas and two city administrations namely Semen Bench, Debub Bench, Shay Bench, Gidi Bench, Sheko, Guraferda woredas, Mizan Aman city administration, and Siz city administration. According to the zonal statistics office, the total population of the Bench Sheko zone is 681,549. The Bench Sheko zone has 1 hospital, 26 health centers, and 128 health posts. This community-based cross-sectional study design was conducted from February to May 2021. Male partners of women (whether they were in a formal marriage or informal union) in their reproductive years (18–49) were the source population.
The sample size was computed based on the single population proportion formula, and using the prevalence of male partner's involvement in promoting ANC utilization in Ambo town (59.9%) (16), Z-value of 1.96 at a 95% confidence level, a margin of error of 5%, and 10% nonresponse rate. As we follow multistage sampling, we use design effect two. So the final sample size was 816. Multistage sampling techniques were used to select study participants. Simple random and cluster sampling were used in a step-wise way. Out of six woredas and two city administrations, two woredas (Shay Bench and Guraferda woreda) and one city administration (Mizan Aman city administration) were selected by a simple random sampling technique. Mizan Aman city administration has five kebeles, and among these kebeles, Addis Ketema, Shesheka, and Hibret kebeles were selected with a lottery method. In Guraferda woreda, we select 10 kebeles out of 30 kebeles with simple random sampling and in Shay Bench woreda, 6 of 21 kebeles were selected in the same fashion. Finally, all partners of a woman who has a child whose age was less than 1 year old and lived in the selected kebele were included. A list of women who delivered within 1 year was traced with the help of health extension workers in each kebele.
Male involvement in ANC utilization was defined as the involvement of the male partner in (1) discussions with health professionals on the spouse's delivery location, and (2) whether the husband accompanied the woman at least once during an ANC check-up. If the male partner reported that he had done both of these things, he was classified as “Involved in ANC.” If he missed one of these activities, he was categorized as “Not involved in ANC.”
Level of knowledge about the advantages of ANC: seven questions regarding the definition of ANC, number of visits, the advantage of ANC follow-up, and bad outcomes of not having ANC follow-up were asked. Those participants who scored more than the mean value were considered to have high knowledge about the advantages of ANC utilization. Those participants who scored less than the mean value were considered to have low knowledge about the advantages of ANC utilization.
Attitudes toward ANC utilization: five questions that assess male partners' attitudes toward their female partner's ANC utilization were asked. For example, we asked, “Do you think that ANC follow-up is important for women?” All the respondents with cumulative scores equal to or more than the mean were categorized as having a favorable attitude. Men who answered less than the mean score were considered to have an unfavorable attitude toward the utilization of ANC.
Waiting time: If a partner reported that he had to wait for more than 30 min without talking to a healthcare provider starting from when he arrived at the health facility, we categorized it as a long waiting time. It was assessed by self-report of the husband.
Data were collected using interviewer-administered structured questionnaires that addressed sociodemographic characteristics, personal and environmental factors, and male partners' involvement in the ANC utilization of their spouses/partners, service delivery experience, knowledge about the benefits of ANC, and attitudes of men toward ANC utilization by women. The questionnaire was designed in English, then translated into Amharic, and then back-translated to English by a third person to check for consistency. The interview took place within the households of respondents, and on average, it took about 30 min to complete the interview.
Data were entered into Epi data version 4.4 and exported to Statistical Package for Social Science (SPSS) version 23 for analysis. Data exploration was conducted to examine different characteristics of the data. After data cleaning, descriptive statistics such as frequencies, proportions, and percentages were used to assess the categorical variables, while measures of central tendency and dispersion were used to summarize continuous data.
Bivariate logistic regression was carried out to select candidate variables for multivariate logistic regression analysis with a p-value <0.25. Candidate variables were entered into a multivariable logistic regression model using a backward method to identify the statistically significant factors for male involvement by controlling possible confounders. The degree of association between dependent and independent variables was assessed using odds ratios and a p-value < 0.05.
The dependent variable was the male partner's involvement in ANC utilization resulting in a child who is less than 1 year old. The independent variables were sociodemographic variables (age, marital status, educational level, ethnicity, religion, occupation, and wealth status), obstetric and related factors (previous history of ANC visit with his partner, parity, and family size), cultural factors, health service-related factors (cost, waiting time, distance from home to health facility, quality of service, and affordability and accessibility of services), knowledge, and attitudes about ANC.
Data collectors were trained on how to collect and handle data. Questionnaires were pretested on 5% of the sample in the Keffa zone before formal data collection began. After data collection, each questionnaire was given a unique code by the principal investigators. Double entry of data was used to decrease errors and 5% of the entered data were rechecked by comparing the entered data with the actual questionnaire. Any errors identified at this time were corrected. The principal investigator reviewed the completed questionnaires at the end of data collection every day for completeness, consistency, and to take corrective measures.
Ethical clearance was obtained from Mizan Tepi University’s Ethical Review Committee. Written consent was obtained from the study subjects, and the right of the respondents to withdraw or not to participate was respected. The anonymity and confidentiality of the data provided were strictly maintained. Participants were assured that their participation was voluntary.
A total of 816 men took part in the study, with a 98.2% response rate. About two-thirds (65.5%) of the respondents were aged 25–34 years. The mean age of respondents was 29.3 (SD ± 3.68) years. Most of the respondents (70.7%) lived in rural areas, and 41.2% completed primary level education. Almost half (46.6%) of study participants were involved in private sector work and 38.6% of respondents were Protestants. The majority of respondents (77.8%) were married (Table 1).
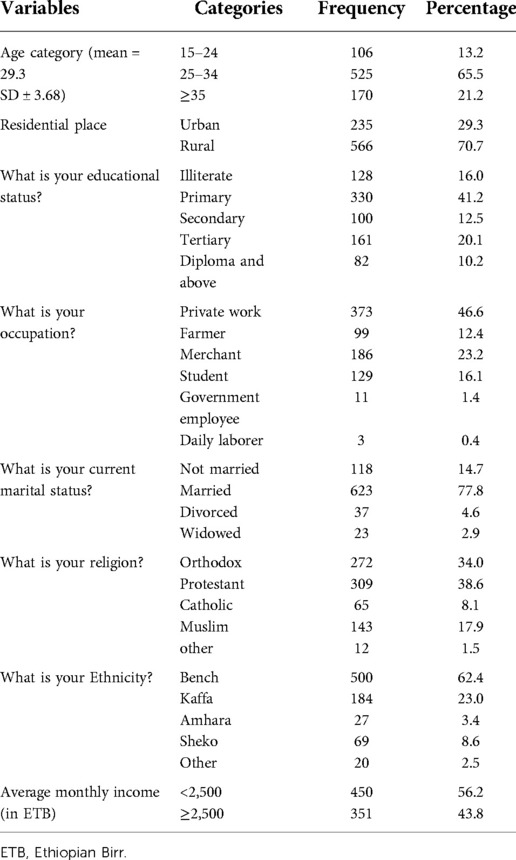
Table 1. Sociodemographic characteristics of male partners of women within the reproductive age group (18–49 years) in the Bench Sheko zone, Southwest region, Ethiopia, 2021.
The majority of men (78.4%) said that they decided on health-seeking behaviors together with their female partners. More than half (55.8%) of respondents have nearby health institutions (within 5 km radius) in their kebele, whereas 67.9% of respondents took more than 30 min to reach a health center (Table 2).
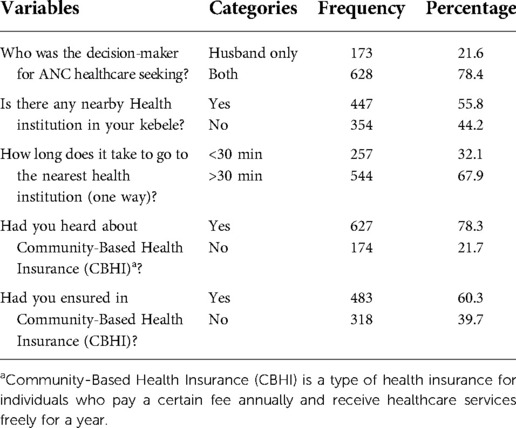
Table 2. Personal and environmental factors of male partners of women in their reproductive years (18–49 years) in the Bench Sheko zone, Southwest region, Ethiopia, 2021.
About half (51.5%) of men did not attend ANC with their female partners because they were not comfortable going with their partners. A similar percentage of respondents (51.9%) thought that ANC is a women's affair (Figure 1).
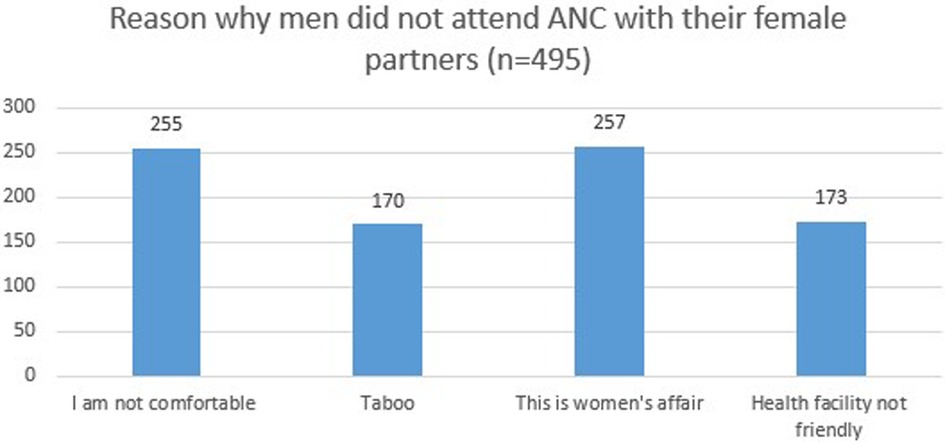
Figure 1. Reason why men did not attend ANC with their female partners in the Bench Sheko zone, Southwest region, Ethiopia, 2021. ANC, antenatal care.
Participants could select more than one reason for not attending ANC with their female partner. Therefore, percentages do not sum to 100.
The prevalence of male involvement in antenatal care service utilization was 38.2%. About 44.6% of the respondents said they experienced a long wait time (characterized as waiting for more than 30 min without having contact with a healthcare provider) when they came with their female partner for ANC, and 42.8% of respondents said that healthcare professionals were not cooperative during a visit with their female partners (Table 3).
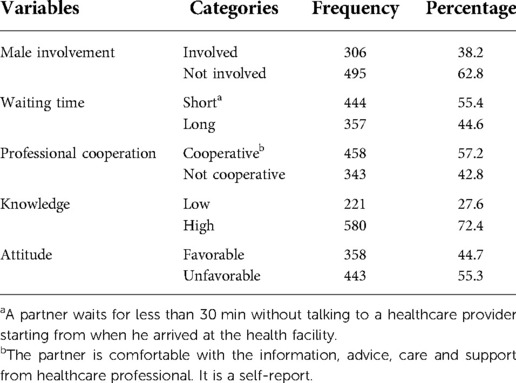
Table 3. Prevalence of male involvement, service delivery experience, knowledge, and attitudes of male partners of women with reproductive age group (15–49 years) in the Bench Sheko zone, Southwest region, Ethiopia, 2021.
Five variables, namely, residence (urban), age (25–34), education (diploma and above), income (≥2,500 Ethiopian Birr, ETB), and high knowledge of the advantages of ANC, were independently associated with male involvement in ANC in multivariable logistic regression models. Male partners who lived in urban settings had almost five times the odds of male involvement in ANC [adjusted odds ratio (AOR): 4.91, 95% CI: 3.39–7.11] compared to rural residents. The odds of male involvement were two times higher (AOR: 2.17, 95% CI: 1.20–3.92) among men aged 25–34 as compared to 15–24 years. Men who had a diploma or higher-level education had 3.6 times the odds (AOR: 3.66, 95% CI: 1.86–3.7.22) of male involvement in ANC as compared to those who were illiterate. Moreover, men with high knowledge of the advantages of ANC utilization as compared to those with low knowledge of ANC had three times the odds of male involvement in ANC (AOR: 3.12, 95% CI: 1.94–5.01), and men with an average monthly income ≥2,500 ETB had 2.8 times the odds of male involvement in ANC as compared to those with a monthly income below 2,500 ETB (AOR: 2 87, 95% CI: (1.98–4.15) (Table 4).
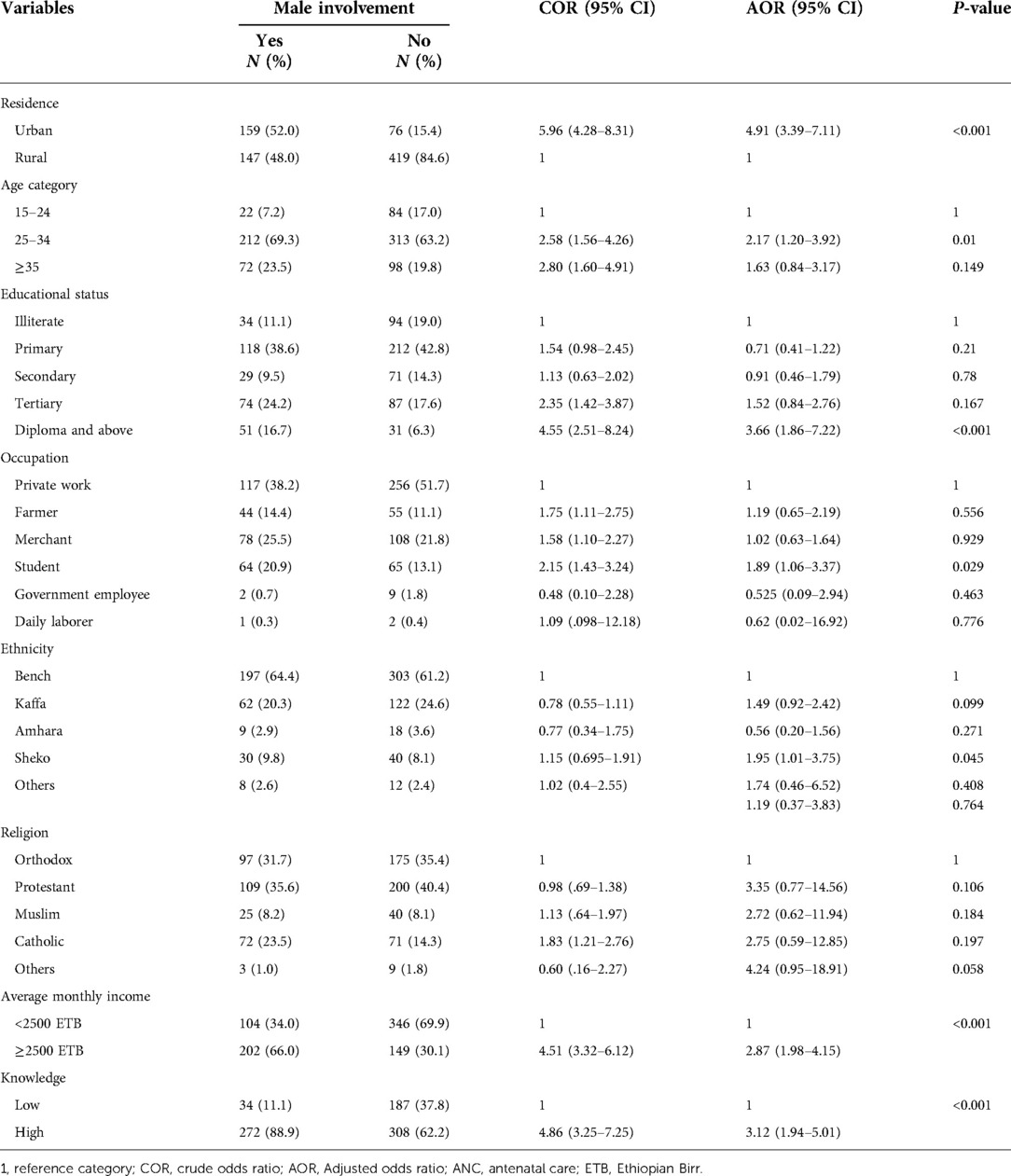
Table 4. Multivariate associations of male involvement in ANC in the Bench Sheko zone, southwest Ethiopia, 2021.
This study assessed the extent of male involvement in the ANC utilization of their female partners and factors associated with their involvement in ANC utilization in the Bench Sheko zone, Ethiopia. The prevalence of male involvement in ANC was 38.2%. The findings are low compared to studies conducted in Addis Ababa (14), Arba Minch (17), and Myanmar (18). A possible explanation for this discrepancy might be that our study area included rural areas, whereas these studies were conducted in urban setting. Male partners who live in urban areas may be more likely to be involved in their spouses’ ANC utilization compared to those living in rural areas. However, our findings were higher compared to studies conducted in Anomabo, Central Region of Ghana (19), and Mekelle, Ethiopia (20), and the variation might be explained due to the different socioeconomic statuses of the regions.
Men who lived in urban areas had five times greater odds of being involved in the ANC utilization of their female partners. This might be due to individuals who live in urban areas being exposed to media and being close to health facilities. This result was in line with a study done in North Gondar that found urban residence to be positively associated with male involvement in maternal healthcare (11). Men aged 25–34 had two times greater odds of being involved in ANC utilization compared to younger men (15–24 years). This result was in line with a study conducted in northern Nigeria that found that young paternal age was a predictor of low male partner participation in maternity care (21). This result might be due to older partners having previous experience being involved in their female partner's ANC follow-up. This has programming implications. Young male partners may need extra support to be active participants in ANC. This finding suggests that new programs that target younger partners should be established in Ethiopia.
In addition, men with higher educational status and a monthly income of ≥2,500 ETB had four and three times the odds of male involvement in ANC utilization, respectively. This result was supported by studies conducted in Lemmo woreda of southern Ethiopia (22), North Gondar zone (11), Nepal (23), and Kenya (24) that found that those partners with high educational achievement and higher income showed more ANC involvement. Respondents who had high knowledge about ANC utilization had three times greater odds of involvement in the ANC utilization of their female partners. This result was in line with the study conducted in Arba Minch, Ethiopia (14), and Gulu District in Uganda (25), which found that partners’ knowledge about the advantage of ANC utilization showed a positive association with their involvement in their female partners’ ANC utilization.
This study has some limitations. The study used a cross-sectional design, and thus it is not possible to make causal inferences based on the data. Despite the fact, we tried to convince the respondents that the questions were used only for the study purpose; self-reported measures might have introduced social desirability bias. Despite this inherent limitation, the study provides useful information on male partners’ involvement on antenatal care services utilization that will inform health service planners to design strategies to improve maternal health in Ethiopia.
Male involvement in ANC utilization in the study area is low. The type of residence (urban), age (25–34), education (diploma and above), income (≥2,500ETB), and high knowledge of the advantages of ANC were shown to be independently associated with male involvement in ANC utilization. Considering the importance of male involvement in MCH, we recommend advocating for policies and strategies that can improve the knowledge of men on the advantages of ANC and enhance their engagement in maternal care. In addition, interventions to increase male involvement should be carefully designed and implemented to mitigate the potential harmful effects on couple relationship dynamics (4). Special emphasis should be given to rural residents and those individuals with low income. Because the majority of the population in Ethiopia live in rural areas and have low access to media, policymakers should target younger populations in order to maximize male involvement in women's ANC utilization.
Data will be available upon reasonable request from the corresponding author.
Ethical clearance was obtained from Mizan-Tepi University Ethical Review Committee. Written consent was obtained from the study subjects and the right of the respondents to withdraw or not to participate was respected. The anonymity and confidentiality of the data provided were strictly maintained. Participants were assured that their participation was voluntary.
All authors contributed to data analysis, drafting or revising the article, and agree to be accountable for all aspects of the work. All authors contributed to the article and approved the submitted version.
Funding for this research was provided by the Mizan Tepi University, Ethiopia.
Our deepest gratitude goes to Bench Sheko Zone Health Administration and the staff for their kind support during data collection.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ANC, antenatal care; AOR, adjusted odds ratio; CBHI, community-based health insurance; ETB, Ethiopian Birr; LMIC, low- and middle-income countries; MCH, maternal and child health; MMR, maternal mortality rate; SDG, sustainable development goal; SPSS, Statistical Package for Social Science; WHO, World Health Organization.
1. Daniele MA, Ganaba R, Sarrassat S, Cousens S, Rossier C, Drabo S, et al. Involving male partners in maternity care in Burkina Faso: a randomized controlled trial. Bull World Health Organ. (2018) 96(7):450–61. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29962548. doi: 10.2471/BLT.17.206466
2. UNPF. Male involvement in reproductive health, including family planning and sexual health. New York: United Nations Population Fund (1995).
3. Ditekemena J, Koole O, Engmann C, Matendo R, Tshefu A, Ryder R, et al. Determinants of male involvement in maternal and child health services in sub-Saharan Africa: a review. Reprod Health. (2012) 9(1):32. doi: 10.1186/1742-4755-9-32
4. Tokhi M, Comrie-Thomson L, Davis J, Portela A, Chersich M, Luchters S. Involving men to improve maternal and newborn health: a systematic review of the effectiveness of interventions. PLoS One. (2018) 13(1):e0191620. doi: 10.1371/journal.pone.0191620
5. Yargawa J, Leonardi-Bee J. Male involvement and maternal health outcomes: systematic review and meta-analysis. J Epidemiol Community Health. (2015) 69:604–12. doi: 10.1136/jech-2014-204784
6. Redshaw M, Henderson J. Fathers’ engagement in pregnancy and childbirth: evidence from a national survey. BMC Pregnancy Childbirth. (2013) 13(1):70. doi: 10.1186/1471-2393-13-70
7. Story WT, Burgard SA, Lori JR, Taleb F, Ali NA, Hoque DME. Husbands’ involvement in delivery care utilization in rural Bangladesh: a qualitative study. BMC Pregnancy Childbirth. (2012) 12(1):28. doi: 10.1186/1471-2393-12-28
8. Helleve A. Men’s involvement in care and support during pregnancy and childbirth as Partial Fulfilment of An Award of Master of Philosophy in International (2010 May).
9. Lowe M. Social and cultural barriers to husbands’ involvement in maternal health in rural Gambia. Pan Afr Med J. (2017) 27:255. doi: 10.11604/pamj.2017.27.255.11378
11. Mersha AG. Male involvement in the maternal health care system: implication towards decreasing the high burden of maternal mortality. BMC Pregnancy Childbirth. (2018) 18(1):493. doi: 10.1186/s12884-018-2139-9
12. Black RE, Laxminarayan R, Temmerman M, Walker N. Reproductive, maternal, newborn, and child health. Disease control priorities. 3rd ed., Vol. 2. Washington, DC: World Bank (2016). doi: 10.1596/978-1-4648-0348-2
14. Mohammed BH, Johnston JM, Vackova D, Hassen SM, Yi H. The role of the male partner in the utilization of maternal health care services in Ethiopia: a community-based couple study. BMC Pregnancy Childbirth. (2019) 19(1):28. doi: 10.1186/s12884-019-2176-z
15. Zenebe A, Gebeyehu A, Derseh L, Ahmed KY. Male partner's involvement in HIV counselling and testing and associated factors among partners of pregnant women in Gondar Town, Northwest Ethiopia. J Pregnancy. (2016) 2016:3073908. Available from: https://www.ncbi.nlm.nih.gov/pubmed/27555968. doi: 10.1155/2016/3073908
16. Demisse Dereje B. Involvement of male in antenatal care, birth preparedness and complication readiness and associated factors in Ambo Town, Ethiopia. J Health Med Nurs. (2016) 27(1).
17. Kejela G, Mira G, Gaga B, Muktar A, Ololo B, Bezabehe S. The role of male involvement in family planning utilization and associated factors in Arba Minch Town, Gamo Gofa Zone, Ethiopia. Eur J Prev Med. (2017) 5(4):39–44. doi: 10.11648/j.ejpm.20170504.11
18. Wai KM, Shibanuma A, Oo NN, Fillman TJ, Saw YM, Jimba M. Are husbands involving in their spouses’ utilization of maternal care services?: a cross-sectional study in Yangon, Myanmar. PLoS One. (2015) 10(12):e0144135. doi: 10.1371/journal.pone.0144135
19. Craymah JP, Oppong RK, Tuoyire DA. Male involvement in maternal health care at Anomabo, Central Region, Ghana. Int J Reprod Med. (2017) 2017:2929013. doi: 10.1155/2017/2929013
20. Haile F, Brhan Y. Male partner involvements in PMTCT: a cross-sectional study, Mekelle, Northern Ethiopia. BMC Pregnancy Childbirth. (2014) 14(1):65. doi: 10.1186/1471-2393-14-65
21. Iliyasu Z, Abubakar IS, Galadanci HS, Aliyu MH. Birth preparedness, complication readiness and fathers’ participation in maternity care in a northern Nigerian community. Afr J Reprod Health. (2010) 14(1):21–32. PMID: 20695136
22. Katiso NA, Adinew YM. Male partners’ involvement in institutional delivery in rural Ethiopia: community based survey. J Women Health Care. (2015) 4(3):3–6. doi: 10.4172/2167-0420.1000239
23. Bhatta DN. Involvement of males in antenatal care, birth preparedness, exclusive breastfeeding, and immunizations for children in Kathmandu. Nepal. BMC Pregnancy Childbirth. (2013) 13(1):14. doi: 10.1186/1471-2393-13-14
24. Cheptum J, Omoni G, Mirie W. Role of men in birth preparedness: a qualitative study of women attending antenatal clinics in Migori County, Kenya. J Midwifery Reprod Health. (2019) 7(1):1513–20. doi: 10.22038/jmrh.2018.25789.1281
Keywords: male involvement, antenatal care, Bench Sheko, Ethiopia, southwest Ethiopia
Citation: Mekonen M, Shifera N, Bogale B and Assefa A (2022) Extent of male involvement and associated factors in antenatal care service utilization in Bench Sheko zone, Southwest Ethiopia: A community-based cross-sectional study. Front. Glob. Womens Health 3:938027. doi: 10.3389/fgwh.2022.938027
Received: 6 May 2022; Accepted: 7 November 2022;
Published: 2 December 2022.
Edited by:
Sarah A. Gutin, University of California, United StatesReviewed by:
Theresa Hoke, Family Health International 360, United States© 2022 Mekonen, Shifera, Bogale and Assefa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mengistu Ayenew Mekonen bWVuZ2lzdHVheWVuZXdAZ21haWwuY29t Ashenafi Assefa YXNoZWFzaHUyMUBnbWFpbC5jb20=
Specialty Section: This article was submitted to Contraception and Family Planning, a section of the journal Frontiers in Global Women's Health
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.