
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Glob. Womens Health , 17 March 2022
Sec. Women's Mental Health
Volume 3 - 2022 | https://doi.org/10.3389/fgwh.2022.834040
This article is part of the Research Topic Innovations in women’s body image: What does the future hold? View all 8 articles
 Juliana Fernandes Filgueiras Meireles1*
Juliana Fernandes Filgueiras Meireles1* Clara Mockdece Neves1
Clara Mockdece Neves1 Ana Carolina Soares Amaral2
Ana Carolina Soares Amaral2 Fabiane Frota da Rocha Morgado3
Fabiane Frota da Rocha Morgado3 Maria Elisa Caputo Ferreira1
Maria Elisa Caputo Ferreira1Background: During pregnancy and the postpartum period, women experience tremendous biopsychosocial changes in a short period of time. Poor body appreciation, depressive symptoms, and low self-esteem during the perinatal period may cause negative consequences for both the mother and the infant's physiological and psychological health. The aim of this study was to analyze the differences in body appreciation, depressive symptoms, and self-esteem between the three gestational trimesters and the postpartum period.
Methods: Participants (N = 1,423 pregnant and postpartum Brazilian women), aged between 18 and 42 years old (M = 29.22; SD = ±5.72), answered questionnaires on body appreciation, depressive symptoms, and self-esteem. BMI was self-reported. Descriptive and nonparametric covariance analysis were performed, comparing women who were in the first, second, and third trimesters and the postpartum period.
Results: Body appreciation was significantly higher among women in the third trimester compared to those in the first and second trimester. However, it was lower for women in all three gestational trimesters than for those in the postpartum. There was no difference in self-esteem during pregnancy, but it was significantly lower in the postpartum group. Similarly, depressive symptoms did not vary through pregnant groups but it was significantly higher in the postpartum group.
Conclusions: The results showed that the postpartum period can be a difficult experience for women. They presented poor body appreciation and lower self-esteem and higher depressive symptoms compared to the pregnancy period. Therefore, it is necessary for public health policies to support women in this period, preserving their mental health and making this experience more positive.
During pregnancy and the postpartum period, women experience several biopsychosocial changes in a short period of time (1–4). The gestational period is divided into first, second, and third trimesters. In the first trimester (weeks 1–12), the woman begins to gain weight, and mood swings may occur, such as moments of depression and agitation (5). The second trimester (weeks 13–25) is characterized by the onset of fetal movements and the belly becomes more visible (5). This trimester is also considered the most emotionally stable (6). In the third trimester (from week 26 onwards), there is a greater increase in maternal weight (5, 7) and this is the period of greatest apprehension for most women due to proximity to delivery (6). Up to 6 months after delivery, women deal with the complex recovery of the body from changes that occurred during pregnancy and childbirth (5), and they are susceptible to psychological vulnerability (3, 8).
Mental health disorders affect many women during pregnancy and the postpartum period (3, 8, 9). Low self-esteem, depressive symptoms, and low levels of body appreciation during pregnancy and postpartum can have negative consequences for the well-being of the woman, her partner, and her family, and for the birth and development of the child (10). In particular, ~30–70% of women who have given birth have had lower self-esteem after delivery (11). Low self-esteem causes a series of social and psychological problems, such as degraded marital relationships, depression, bulimia, lower mother-fetus attachment, and early termination of breastfeeding (1, 11, 12). Associated with this low self-esteem, about 20% of women may develop depression during pregnancy (13), and in the postpartum period (9), which may be related to malnutrition, alcohol use and smoking, suicidal behaviors, and postpartum depression, as well as risk factors for pre-eclampsia, premature labor, and low birth weight (2, 14, 15).
In addition, the changes that occur in women's bodies during pregnancy and postpartum can have consequences on their body image. Research suggests that body dissatisfaction can worsen at specific periods, such as early pregnancy (16, 17), in the middle (18, 19), at the end (20, 21), or in the postpartum period (3, 22). In these cases, pregnancy and postpartum can intensify or cause a negative relationship with the body (1, 3). Recently, authors reported on the importance of evaluating body dissatisfaction during pregnancy as a predictor of the onset of prenatal depression in Polish women (10). However, the authors pointed out that, in clinical practice, this risk factor should be considered in combination with positive maternal attitudes, not separately (10).
In this sense, previous study found body dissatisfaction in 45% of pregnant women with high BMI and high parity (23). Other studies have also evaluated the association of body image with other psychological variables in pregnant women who asserted that depression, low self-esteem, and higher BMI can trigger negative bodily attitudes in this population (24–26). In addition, current studies showed that more-troubled sociodemographic conditions can be considered as risk factors for negative mental health (9, 27). No family support, unplanned pregnancy, multiparous, single women, having contemplated abortion, low education, and suffering from obesity showed to be alarming conditions for low self-esteem, poor body image, and greater depressive symptoms (9, 27). The occurrence of these issues during this phase of a woman's life can be prolonged and compromise the health of the mother, fetus, and child.
Although body image includes both positive and negative characteristics, much emphasis has been given to the negative aspects of this construct (28). Positive body image can promote and increase engagement in health-related behaviors (29, 30). Furthermore, the authors suggest that a positive body image protects physical health and psychological well-being. Therefore, there is a need to support people in appreciating, respecting, celebrating, and honoring their bodies (31, 32) during all stages of life, including pregnancy and the postpartum period (30).
In women's holistic health care, the assessment of body image during pregnancy and postpartum is recommended so that pregnant women have available assistance while dealing with the typical changes of these periods (1, 17, 33). It is worth emphasizing that promoting positive body image can be a non-pharmacological strategy that offers protection factors against psychological pathologies in pregnancy and the postpartum period. Body image and self-esteem can be important targets for prevention and treatment programs for postpartum depression. In addition, the influence of demographic conditions on body image, depressive symptoms, and self-esteem of pregnant women and postpartum women was already discussed in the literature (9, 11, 20, 23–27). Given these aspects, the aim of this study was to analyze the differences in body appreciation, depressive symptoms, and self-esteem between women in the three gestational trimesters and postpartum period, controlling by some sociodemographic conditions.
The study was approved by the Ethics and Research Committee at the Federal University of Juiz de Fora (registration number 50474115.1.0000.5147). All participants gave informed written consent and were offered no financial compensation.
This investigation presents a cross-sectional delineation and was carried out in different the five regions of Brazil (North, Northeast, Central, Southeast, and South). Data were collected between October 17th 2016 and March 1st 2017.
We recruited a total of 1,861 adult pregnant women regardless of their gestational period, or postpartum women until 6 months after delivery. Women who did not fill out any of the three questionnaires were excluded. Thus, we excluded 438 women that did not answer one or more questionnaires. After missing data exclusion, 1,423 women aged between 18 and 52 years old (M = 29.22 ± 5.72) took part in the study. Among them, 97 (6.8%) were in their first trimester (M = 9.23 ± 2.53 gestational weeks); 449 (31.6%) were in their second trimester (M = 19.96 ± 3.60 gestational weeks), 538 (37.8%) in their third trimester (M = 31.93 ± 3.91 gestational weeks), and 339 (23.8%) were postpartum women (M = 85.45 ± 60.88 days after delivery).
Table 1 presents descriptive analyses of sociodemographic variables for each group. For all four groups, most women were married and had a good relationship with the baby's father, had family support, had planned the pregnancy, and did not think about interrupting the pregnancy.
The researchers contacted many professionals offering services to pregnant and postpartum women (obstetricians, event organizers, and health care institution owners). In obstetric clinics and health institutions, women answered the questionnaires while they were in the waiting room. In the case of events (courses, fairs), a trained team approached women individually in places reserved for rest or food. The participants took ~20 min to complete the questionnaires.
Women provided demographic information such as age, education level, marital status, relationship with the baby's father, family support, gestation planning, and initial desire to have an abortion. Pregnant women also reported their gestational age in weeks and postpartum women provided the delivery date. Participants self-reported their weight and height data, which we used to calculate their Body Mass Index (BMI) and to classify these participants as low weight, eutrophic, overweight, and obese.
We used the Body Appreciation Scale (BAS) (34) to assess body appreciation. The 13-item scale is a self-report instrument with 5 Likert response options. In our study, we found a high internal consistency (α = 0.903) for this measure (35, 36).
We applied the Rosenberg Self-Esteem Scale (RSS) (37) to evaluate the participant's self-esteem. This scale is composed of 10 items that use a four-point Likert scale. The scale demonstrated good internal consistency (α = 0.863) when used in this study (35, 36).
We used the Beck Depression Inventory (BDI) (38) to verify the presence of depressive symptoms through 21 items. BDI reliability was considered adequate (0.866) (35, 36).
We conducted this analysis in Statistical Package for the Social Sciences (SPSS) version 28.0, and in all cases the level of significance adopted was p < 0.05. Mean, standard deviation, median, minimum, and maximum were calculated for each variable in the study. Also, we analyzed absolute and relative frequencies for the category variables. We evaluated the scales' internal consistency through Cronbach's alpha. This was followed by the Kolmogorov Smirnov normality test, and inspection of asymmetry and kurtosis of the scores obtained. Based on previous literature, more troubled sociodemographic backgrounds can be more harmful to psychological vulnerability during the perinatal period (9, 11, 20, 23–27). Preliminary analysis was performed to test this hypothesis carrying out Mann–Whitney test and Kruskal–Wallis test in order to verify the existence of any difference between the groups for each outcome (BAS, RSS, and BDI). We run a non-parametric Quade test (ANCOVA), adjusting the effect of the variables that showed difference in the preliminary analysis on each outcome, between the four groups (first, second, third trimester, and postpartum). For all the comparative analyses, the size of the effect was determined by Cohen's d (39). We considered small, medium, and large effect sizes values lower than 0.5, between 0.5 and 0.79, or ≥0.8, respectively (39, 40).
Table 2 shows the results regarding differences in the outcomes compared for nutritional status, educational level, marital status, parity, relationship with the baby's father, family support, gestational planning, and initial desire to have an abortion.
Based on the preliminary analysis, we used as covariate in the main analysis only the variables that demonstrated an influence on the outcomes. Then, BMI, parity, gestational planning, and initial desire to have an abortion were used as covariates for body appreciation and depressive symptoms. BMI, family support, gestational planning, and initial desire to have an abortion were used as covariates for self-esteem.
We found significant statistical differences for body appreciation, depressive symptoms, and anxiety (Table 3). Women in their first trimester had lower body appreciation than women who were currently in their third trimester (p = 0.010). Pregnant women on their second trimester had lower body appreciation than those on third (p = 0.027). In addition, women during the postpartum period presented lower body appreciation when compared to those on their first (p = 0.045), second (p = 0.0001), and third (p = 0.0001) trimesters. Self-esteem was similar between groups of pregnancy trimesters, but it was significantly lower in the postpartum period group when compared to pregnant women in the different gestational trimesters (p = 0.012; p = 0.0001; p = 0.0001). Similarly, depressive symptoms did not vary through pregnant groups, but it was significantly higher in the postpartum period group (p = 0.036; p = 0.0001; p = 0.0001).
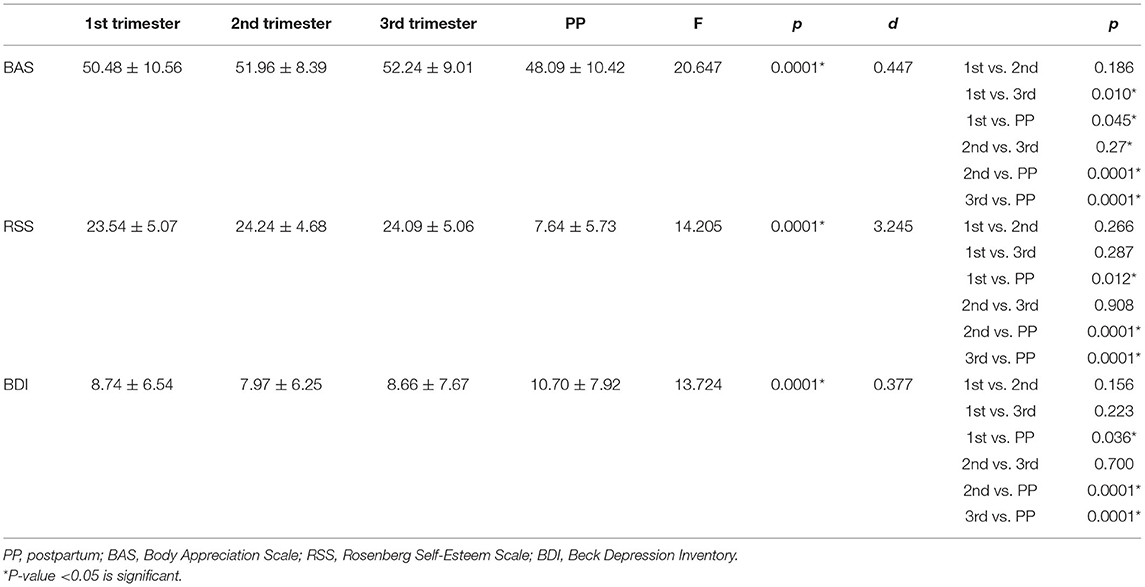
Table 3. Covariance analyses of body appreciation, depression symptoms, and self-esteem between the perinatal period adjusting covariates for each variable.
The goal of this study was to compare the differences in body appreciation, self-esteem, and depressive symptoms between women in the three gestational trimesters and in the postpartum period. The results showed significant differences for all the analyzed variables, demonstrating that the gestational period and the postpartum period have an impact on women's mental health. It is relevant to investigate body image from a positive perspective (29, 30, 32), seeking to prevent mental health disturbance in this population (41, 42).
Body appreciation was lower in pregnant women in their first trimester when compared to those on their third trimester. Furthermore, those on their second trimester had lower body appreciation than those on third. During the first gestational weeks, women may show less appreciation for their pregnant body as there is a feeling of weight gain without visibly appearing to be pregnant (2, 18). As the gestational trimesters progress, it is possible to accept and appreciate the increase in body dimensions. During these phases, mothers tend to prioritize their own health and baby's health, going beyond aesthetic concerns (1, 4). Pregnancy can be a reason for them to appreciate the functionality of their bodies, discouraging objectification (43). Furthermore, it seems that during pregnancy, the woman has a social allowance for the body to move away from the socially established standard of beauty, contributing to greater bodily acceptance (1, 2, 4).
However, our results showed lower body appreciation in the postpartum period group when compared to the three gestational trimesters groups, demonstrating that women had a less positive body image at this stage. Clark et al. (18) explained that there are no more excuses for larger body dimensions after the delivery. The fact that mothers feel fat can also be explained by the unrealistic expectations they have about the speed and ease with which the body will return to its pre-pregnancy shape (18, 44). In the same sense, previous studies found that mothers' body satisfaction decreased after delivery (25, 45). Thus, it is important not only to educate women about the expected weight and body changes in the postpartum period, but also to promote a positive body image, self-acceptance, and self-esteem after the delivery.
Findings for self-esteem and depressive symptoms were similar. These variables remained stable with no significant differences between the three gestational trimesters groups. Similarly, in a Brazilian longitudinal investigation, Meireles et al. (7) pointed out that self-esteem and depressive symptoms remained constant throughout pregnancy. Conversely, Chan et al. (25) found variations in the emotional state during pregnancy, with the third trimester showing more positive levels. Although the previous literature does not present a consensus regarding the variability of the pregnant woman's mental state, the fact is that the assessment of the mother's psychological aspects in the first trimester of pregnancy is extremely relevant since a troubled condition can persist throughout the pregnancy (11).
We also found a lower self-esteem and higher depressive symptoms in the postpartum group when compared to the gestational trimesters. These findings reinforce that this phase can be the most troublesome for the mental health of the mother. Previous studies have pointed out that the postpartum period involves low self-esteem and high depressive symptoms (9, 11, 46, 47). Furthermore, the theoretical model tested by Lee and Park (46) demonstrated that self-esteem and antepartum depressive symptoms are predictors of postpartum depression. Thus, if identified early, the woman can receive adequate support and avoid negative consequences in the postpartum period and during the baby's development (46, 48).
We must also acknowledge a few limitations of this study. The first limitation consisted in the collection of self-reported weight and height. It is possible that this information was under or overestimated by the participants. The anthropometric data measured are more reliable. However, researchers indicate the use of self-report measures to provide data on nutritional status in investigations with a large sample size (49). In addition, previous studies with pregnant and postpartum women also used self-reported anthropometric data (21, 42, 50). Second, the smaller sample size of first-trimester pregnant women is considered a limitation, considering the number of participants included in the other groups. It should be noted that there is greater difficulty in accessing this group of women as some of them discover the pregnancy late or even prefer not to expose the pregnancy. This is a common feature in comparative studies in this population (1, 17, 18). However, this study included 97 pregnant women in the first trimester. Finally, the cross-sectional design does not allow causal inferences and does not provide an assessment of the changes experienced by each of these women throughout pregnancy and the postpartum period. Despite these limitations, this study filled a gap in the literature because it examines positive body image, self-esteem, and depression symptoms of pregnant and postpartum women, which may contribute to the development and improvement of prevention strategies and gestational follow-up.
We conclude that the postpartum period can be a difficult experience for women. After delivery, women showed low body acceptance, low self-esteem, and higher depressive symptoms compared to the gestational period. We recommend future studies that investigate the factors that can impact on body appreciation, self-esteem, and depressive symptoms, such as: race, ethnicity, breastfeeding during postpartum period, and type of delivery. We also indicate the need of longitudinal investigations that include the periods before, during, and after pregnancy.
Pregnancy and postpartum can be stressful events for women due to biopsychosocial changes. Multidisciplinary health teams play an important role in providing care to women. It is known that the obstetric examination is irreplaceable and extremely important for the physical health of the mother and baby. These teams should also be aware that some women may not cope with the rapid physical changes that are necessarily associated with pregnancy and the postpartum period, and that assistance at this time might be needed to promote a positive experience.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ethics and Research Committee at the Federal University of Juiz de Fora. The patients/participants provided their written informed consent to participate in this study.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
This research was funded by the Universidade Federal Rural do Rio de Janeiro.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors would like to thank all participants without whom there would be no study.
1. Meireles JFF, Neves CM, Carvalho PHB, Ferreira MEC. Body dissatisfaction among pregnant women: an integrative review of the literature. Cien Saude Colet. (2015) 20:2091–103. doi: 10.1590/1413-81232015207.05502014
2. Skouteris H. Pregnancy: physical and body image changes. In: Cash T, editor. Encyclopedia of Body Image and Human Appearance. San Diego, CA: Academic Press (2012). p. 664–8.
3. Walker LO, Gao J, Xie B. Postpartum psychosocial and behavioral health: a systematic review of self-administered scales validated for postpartum women in the United States. Women Health Issues. (2015) 25:586–600. doi: 10.1016/j.whi.2015.05.006
4. Watson B, Fuller-Tyszkiewicz M, Broadbent J, Skouteris H. The meaning of body image experiences during the perinatal period: a systematic review of the qualitative literature. Body Image. (2015) 14:102–13. doi: 10.1016/j.bodyim.2015.04.005
5. Cunningham FG, Leveno KJ, Bloom SL, Dashe JS, Hoffman BL, Casey BM, et al. Williams Obstetrics, 25th Edn. New York, NY: McGraw Hill (2021).
6. Wu H, Sun W, Chen H, Wu Y, Ding W, Liang S, et al. Health-related quality of life in different trimesters during pregnancy. Health Qual Life Outcomes. (2021) 19:1–11. doi: 10.1186/s12955-021-01811-y
7. Meireles JFF, Neves CM, Carvalho PHBd, Ferreira MEC. Body image in pregnant women: a longitudinal study. J Bras Psiquiat. (2016) 65:223–30. doi: 10.1590/0047-2085000000128
8. Liu X, Wang S, Wang G. Prevalence and risk factors of postpartum depression in women: a systematic review and meta-analysis. J Clin Nurs. (2021) 00:1–13. doi: 10.1111/jocn.16121
9. Alshikh Ahmad H, Alkhatib A, Luo J. Prevalence and risk factors of postpartum depression in the Middle East: a systematic review and meta-analysis. BMC Pregnancy Childbirth. (2021) 21:1–12. doi: 10.1186/s12884-021-04016-9
10. Przybyła-Basista H, Kwiecińska E, Ilska M. Body acceptance by pregnant women and their attitudes toward pregnancy and maternity as predictors of prenatal depression. Int J Environ Res Public Health. (2020) 17:9436. doi: 10.3390/ijerph17249436
11. Han J-W, Kim D-J. Longitudinal relationship study of depression and self-esteem in postnatal Korean women using autoregressive cross-lagged modeling. Int J Environ Res Public Health. (2020) 17:3743. doi: 10.3390/ijerph17103743
12. Gillen MM, Markey CH, Rosenbaum DL, Dunaev JL. Breastfeeding, body image, and weight control behavior among postpartum women. Body Image. (2021) 38:201–9. doi: 10.1016/j.bodyim.2021.04.006
13. Pereira PK, Lovisi GM. Prevalence of gestational depression and associated factors. Arch Clin Psychiatry. (2008) 35:144–53. doi: 10.1590/S0101-60832008000400004
14. Sliwerski A, Kossakowska K, Jarecka K, Switalska J, Bielawska-Batorowicz E. The effect of maternal depression on infant attachment: a systematic review. Int J Environ Res Public Health. (2020) 17:2675. doi: 10.3390/ijerph17082675
15. Wilcox M, McGee BA, Ionescu DF, Leonte M, LaCross L, Reps J, et al. Perinatal depressive symptoms often start in the prenatal rather than postpartum period: results from a longitudinal study. Arch Womens Ment Health. (2021) 24:119–31. doi: 10.1007/s00737-020-01017-z
16. Goodwin A, Astbury J, McMeeken J. Body image and psychological well-being in pregnancy. A comparison of exercisers and non-exercisers. Aust N Z J Obstet Gynaecol. (2000) 40:442–7. doi: 10.1111/j.1479-828X.2000.tb01178.x
17. Skouteris H, Carr R, Wertheim EH, Paxton SJ, Duncombe D. A prospective study of factors that lead to body dissatisfaction during pregnancy. Body Image. (2005) 2:347–61. doi: 10.1016/j.bodyim.2005.09.002
18. Clark A, Skouteris H, Wertheim EH, Paxton SJ, Milgrom J. The relationship between depression and body dissatisfaction across pregnancy and the postpartum: a prospective study. J Health Psychol. (2009) 14:27–35. doi: 10.1177/1359105308097940
19. Duncombe D, Wertheim EH, Skouteris H, Paxton SJ, Kelly L. How well do women adapt to changes in their body size and shape across the course of pregnancy? J Health Psychol. (2008) 13:503–15. doi: 10.1177/1359105308088521
20. Meireles JFF, Neves CM, Carvalho PHB, Ferreira MEC. Body image, eating attitudes, depressive symptoms, self-esteem and anxiety in pregnant women of Juiz de Fora, Minas Gerais, Brazil. Cienc Saude Colet. (2017) 22:437–45. doi: 10.1590/1413-81232017222.23182015
21. Sweeney AC, Fingerhut R. Examining relationships between body dissatisfaction, maladaptive perfectionism, and postpartum depression symptoms. J Obstet Gynecol Neonatal Nurs. (2013) 42:551–61. doi: 10.1111/1552-6909.12236
22. Rallis S, Skouteris H, Wertheim EH, Paxton SJ. Predictors of body image during the first year postpartum: a prospective study. Women Health. (2007) 45:87–104. doi: 10.1300/J013v45n01_06
23. Sui Z, Turnbull D, Dodd J. Effect of body image on gestational weight gain in overweight and obese women. Women Birth. (2013) 26:267–72. doi: 10.1016/j.wombi.2013.07.001
24. Kamysheva E, Skouteris H, Wertheim EH, Paxton SJ, Milgrom J. Examination of a multi-factorial model of body-related experiences during pregnancy: the relationships among physical symptoms, sleep quality, depression, self-esteem, and negative body attitudes. Body Image. (2008) 5:152–63. doi: 10.1016/j.bodyim.2007.12.005
25. Chan CY, Lee AM, Koh YW, Lam SK, Lee CP, Leung KY, et al. Associations of body dissatisfaction with anxiety and depression in the pregnancy and postpartum periods: a longitudinal study. J Affect Disord. (2020) 263:582–92. doi: 10.1016/j.jad.2019.11.032
26. Riquin E, Lamas C, Nicolas I, Dugre Lebigre C, Curt F, Cohen H, et al. A key for perinatal depression early diagnosis: the body dissatisfaction. J Affect Disord. (2019) 245:340–7. doi: 10.1016/j.jad.2018.11.032
27. Meireles JFF, Neves CM, Carvalho PHB, Miranda LB, Carvalho LL, Rossi FGDS, et al. High-risk pregnancy and low-risk pregnancy: association with sociodemographic, anthropometric, obstetric and psychological variables. J Phys Educ Sport. (2021) 21:719–27. doi: 10.7752/jpes.2021.02089
28. Swami V, Barron D. Translation and validation of body image instruments: challenges, good practice guidelines, and reporting recommendations for test adaptation. Body Image. (2019) 31:204–20. doi: 10.1016/j.bodyim.2018.08.014
29. Tylka TL, Wood-Barcalow NL. What is and what is not positive body image? Conceptual foundations and construct definition. Body Image. (2015) 14:118–29. doi: 10.1016/j.bodyim.2015.04.001
30. Webb JB, Wood-Barcalow NL, Tylka TL. Assessing positive body image: contemporary approaches and future directions. Body Image. (2015) 14:130–45. doi: 10.1016/j.bodyim.2015.03.010
31. Avalos L, Tylka TL, Wood-Barcalow N. The Body Appreciation Scale: development and psychometric evaluation. Body Image. (2005) 2:285–97. doi: 10.1016/j.bodyim.2005.06.002
32. Tylka TL. Positive psychology perspectives on body image. In: Cash TF, editor. Encyclopedia of Body Image and Human Appearance. San Diego, CA: Academic Press (2012). p. 657–63.
33. Skouteris H. Body image issues in obstetrics and gynecology. In: Cash TF, Smolak L, editors. Body Image: A Handbook of Science, Practice, and Prevention. New York, NY: The Guilford Press (2011). p. 342–49.
34. Swami V, Campana ANNB, Ferreira L, Barrett S, Harris AS, Fernandes MCGC. The Acceptance of Cosmetic Surgery Scale: initial examination of its factor structure and correlates among Brazilian adults. Body Image. (2011) 8:179–85. doi: 10.1016/j.bodyim.2011.01.001
35. Clark LA, Watson D. Constructing validity: new developments in creating objective measuring instruments. Psychol Assess. (2019) 31:1412–27. doi: 10.1037/pas0000626
36. Hair JF, Black WC, Babin BJ, Anderson RE, Tatham RL. Multivariate Data Analysis, 6th Edn. Porto Alegre: Bookman (2009).
37. Dini G, Quaresma M, Ferreira L. Translation into Portuguese, cultural adaptation and validation of the Rosenberg self-esteem scale. Rev Bras Cir Plást. (2004) 19:41–52.
38. Gorenstein C, Andrade LHSG. Validation of a Portuguese version of the Beck Depression Inventory and State-Trait anxiety inventory in Brazilian subjects. Braz J Med Bio Res. (1996) 29:453–7.
39. Cohen J. Statistical power analysis. Curr Dir Psychol Sci. (1992) 1:98–101. doi: 10.1111/1467-8721.ep10768783
41. Fahami F, Amini-Abchuyeh M, Aghaei A. The relationship between psychological well being and body image in pregnant women. Iran J Nurs Midwifery Res. (2018) 23:167. doi: 10.4103/ijnmr.IJNMR_178_16
42. Meireles JFF, Neves CM, Morgado F, Muzik M, Ferreira MEC. Development and psychometric properties of the self-acceptance scales for pregnant and postpartum women. Percept Mot Skills. (2021) 128:258–82. doi: 10.1177/0031512520973518
43. Rubin LR, Steinberg JR. Self-objectification and pregnancy: are body functionality dimensions protective? Sex Roles. (2011) 65:606–18. doi: 10.1007/s11199-011-9955-y
44. Patel P, Lee J, Wheatcroft R, Barnes J, Stein A. Concerns about body shape and weight in the postpartum period and their relation to women's self-identification. J Reproduct Inf Psychol. (2005) 23:347–64. doi: 10.1080/02646830500273657
45. Gjerdingen D, Fontaine P, Crow S, McGovern P, Center B, Miner M. Predictors of mothers' postpartum body dissatisfaction. Women Health. (2009) 49:491–504. doi: 10.1080/03630240903423998
46. Lee EJ, Park JS. Development of a prediction model for postpartum depression: based on the mediation effect of antepartum depression. J Korean Acad Nurs. (2015) 45:211–20. doi: 10.4040/jkan.2015.45.2.211
47. Wardani VA, Lestari KB, Nurbaeti I. Relationship of self-esteem to postpartum depression in postpartum mothers. J Maternity Care Reproduct Health. (2021) 4:62–73. doi: 10.36780/jmcrh.v4i1.164
48. Takács L, Smolík F, Putnam S. Assessing longitudinal pathways between maternal depressive symptoms, parenting self-esteem and infant temperament. PLoS One. (2019) 14:e0220633. doi: 10.1371/journal.pone.0220633
49. Bowman RL, DeLucia JL. Accuracy of self-reported weight: a meta-analysis. Behav Ther. (1992) 23:637–55. doi: 10.1016/S0005-7894(05)80226-6
Keywords: body image, pregnancy, postpartum period, mental health, maternal welfare, cross-sectional study
Citation: Meireles JFF, Neves CM, Amaral ACS, Morgado FFR and Ferreira MEC (2022) Body Appreciation, Depressive Symptoms, and Self-Esteem in Pregnant and Postpartum Brazilian Women. Front. Glob. Womens Health 3:834040. doi: 10.3389/fgwh.2022.834040
Received: 12 December 2021; Accepted: 16 February 2022;
Published: 17 March 2022.
Edited by:
Jayashri Kulkarni, Monash University, AustraliaReviewed by:
Yolanda Contreras-García, University of Concepcion, ChileCopyright © 2022 Meireles, Neves, Amaral, Morgado and Ferreira. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Juliana Fernandes Filgueiras Meireles, ZXVqdWx5OTBAaG90bWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.