
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Glob. Womens Health, 08 December 2020
Sec. Maternal Health
Volume 1 - 2020 | https://doi.org/10.3389/fgwh.2020.571055
This article is part of the Research TopicMaternal Health in Conflict SettingsView all 8 articles
Giving birth with a skilled birth attendant at a facility that provides emergency obstetric care services has better outcomes, but many women do not have access to these services in low- and middle-income countries. Individual, household, and societal factors influence women's decisions about place of birth. Factors influencing birthplace preference by type of provider and level of public facility are not well understood. Applying the Andersen Behavioral Model of healthcare services use, we explored the association between characteristics of women and their choice of childbirth location using a multinomial logistic regression, and conducted a scenario analysis to predict changes in the childbirth location by imposing various interventions. Most women gave birth at home (68.1%), while 15.1% gave birth at a public clinic, 12.1% at a public hospital, and 4.7% at a private facility. Women with higher levels of education, from households in the upper two wealth quintiles, and who had any antenatal care were more likely to give birth in public or private facilities than at home. A combination of multisector interventions had the strongest signals from the model for increasing the predicted probability of in-facility childbirths. This study enhances our understanding of factors associated with the use of public facilities and the private sector for childbirth in Afghanistan. Policymakers and healthcare providers should seek to improve equity in the delivery of health services. This study highlights the need for decisionmakers to consider a combination of multisector efforts (e.g., health, education, and social protection), to increase equitable use of maternal healthcare services.
Despite a relative decline of 43.9% in global maternal mortality from 1990 to 2015, more progress is needed to meet the United Nations Sustainable Development Goal (SDG) 3.1—a global maternal mortality ratio (MMR) of fewer than 70 deaths/100,000 live births by 2030 (1). Notably, most deaths and childbirth complications occur in low- and middle-income countries (LMIC) from preventable causes (2, 3). Several interventions have been introduced to reduce maternal mortality, including increasing skilled birth attendants (SBA) for delivery and access to in-facility births (4).
Recommendations pertaining to place of delivery include encouraging low-risk births at home with a SBA to all births in facilities where access to emergency obstetric care is available (5, 6). A third option leaves place of birth to patient and provider preference (5, 6). These preferences may be limited by barriers to accessing facilities as well as individual, household, and societal factors, e.g., needing permission from her husband, inaccessible facilities to accompanying relatives, perceived quality of care, previous experience with provider, cost, transportation, and distance (7–12). Globally, in-facility births ranged from below 40% among the poorest countries to above 90% among middle-income countries (6). Ninety-eight percent of in-facility births were performed by a SBA and 96% of SBA deliveries were in a facility, indicating that, globally, few home births and not all in-facility births were assisted by a SBA (6). This is particularly true for fragile and conflict-affected countries like Afghanistan, among the 11 countries with the lowest in-facility births (<40%); however, <10% of home births were with a SBA (6).
Afghanistan has among the highest maternal death rates in the world, nearly ten times greater than the global MMR (1, 13). While national MMR estimates are debated, regardless of the estimate or data source used, maternal deaths in the country are unacceptably high (14). Despite over 20 years of continuous conflict, significant progress has been made to rebuild the country's health system (15). Between 2003 and 2015, there were increases in the number of births with a SBA (14–51%) and in a facility (13–48%) (15, 16). However, current coverage estimates fall short of the recommended 87% SBA and 81% in-facility births required to achieve SDG 3.1 (1).
Socioeconomic and demographic factors, such as wealth quintile, parity, and education are strong predictors of SBA use in Afghanistan (17–21). Additionally, use of antenatal care (ANC) reduces delays in seeking care for obstetric emergencies (22). Despite an increase in ANC use in Afghanistan, over half of women give birth at home, with only 43% of childbirths in a public facility, and 5% in a private facility (16). Prior studies have shown utilization preferences for health services. For instance, one found that receiving health services in a public or private facility varied by type of service; public facilities were used more for inpatient services and less for outpatient services (23). Public health services in Afghanistan were designed for rapid scale-up through contracting with non-governmental organizations (NGOs) (24). This delivery approach improved the equity of health services provision by reaching the poorest households via NGO implementing partners, where the government lacked capacity to delivery services itself (25). However, as in other LMICs, there is an inequitable use of public compared to private facilities among the poorest and wealthiest households, respectively (23, 26).
Understanding the factors associated with women's place of birth preference is important for decisionmakers to improve planning and administration of maternal health services, such as through health education outreach programs, improved access to emergency obstetric care services, or training of health workers to improve quality of ANC. Unfortunately, factors influencing birthplace preference by type of provider (public vs. private) and level of public facility (clinic vs. hospital) are not well understood in Afghanistan.
We adapted the Andersen Behavioral Model (27) to understand the maternal healthcare utilization context. For this study, this model conceptualizes maternal healthcare use as a function of predisposing (socio-demographic factors), enabling (income and vehicle access), and need (woman's view of her own health or symptoms) factors. Feedback loops show that maternal health status influences predisposing, enabling, and perceived need for services, as well as behaviors (health practices during pregnancy and in-facility childbirth), which subsequently affect maternal health outcomes. Using the Anderson Behavioral Model, we explore the associations between key socio-economic and demographic factors and the likelihood of giving birth in a public clinic, public hospital, private facility, or at home (28).
We used household survey data which was conducted as part of an impact evaluation of a results-based financing (RBF) intervention in nine provinces in Afghanistan (Figure 1) (29, 30). The surveys are repeated cross-sections from 2010, 2013, and 2015. Two questionnaires were used for the household survey: the household questionnaire and the female and child health questionnaire.
The household survey used a multi-stage probability sample of the nine selected provinces purposively selected based on representation by different donors and feasibility of implementing the pilot project. In the first stage, 74 health facilities were randomly selected, stratified and matched by facility type and number of outpatient visits in the previous year. The second stage consisted of randomly selecting 288 villages or clusters in the catchment area of the selected health facilities (two clusters per health facility). Using the household listing conducted prior to the survey, the third stage involved simple random sampling of households in the selected villages. The same villages and health facilities were visited during each year of the survey. However, households may or may not be the same as they were not linked across the datasets. On average, interviews were conducted in 24 households per village, resulting in total household sample sizes of 6,878 in 2010, 6,848 in 2012, and 6,584 in 2015. There was less than a 1% nonresponse rate by households across all 3 years, and <5% missing data across variables.
The household questionnaire collected information from the head of the household on all household members, including name, sex, education, socioeconomic status, and utilization of health services. The female and child health questionnaire collected information from ever-married women age 15–49 or women over 18 years who are primary caretakers of children under 5 years of age; questions included age; literacy; pregnancy-based reproductive history; knowledge and use of family planning methods; access, utilization, and quality of services for antenatal care, delivery, postnatal care, and child health services, including immunization; and, perception and quality of services and trust in healthcare providers.
Data on insecurity incidents by province were obtained from the International NGO Safety Organization (31). We also used spatial data of villages included in the study sample and the country's road network. Spatial data were obtained from several publicly available sources (2012–2013 Afghanistan Information Management Services (AIMS) through the Humanitarian Data Exchange) and the MoPH (32).
The outcome variable was the location of childbirth with four options: public clinic, public hospital, private clinic or hospital, and home. Specifically, public clinics include the primary care clinics providing the Basic Package of Health Services (Comprehensive Health Centers, Basic Health Centers, and Sub Health Centers). Public hospitals include District Hospitals, Provincial Hospitals, and Regional Hospitals. Private clinic or hospital category includes any childbirth delivery in the private sector. Only 2% of home births were attended by a SBA, so Home includes all home births, the majority of which did not have a SBA. Women with an in-facility birth all reported having a SBA. Individual and household-level determinants of health access were chosen based on the Andersen Behavioral Model (Figure 2) (28). The predisposing factors in our model include the woman's age (divided into seven five-year categories), education level (no education, primary, secondary or higher), and gravidity (no previous pregnancies or >1 previous pregnancies). Enabling factors include household wealth status [quintile constructed based on index scores (33)], distance to the nearest main or secondary road (in km) as a proxy for rurality, access to a motor vehicle for transport (yes or no), number of security incidents in the province of residence (continuous), provincial health performance score (continuous), type of nearest public health facility (Hospital, Comprehensive Health Center, Basic Health Center, or Sub-Health Center), and an ANC adequacy index (no ANC, inadequate, and adequate). We calculated the Euclidean distance to the nearest main or secondary road (in km) using the country's road network and geocoded locations of villages included in the study sample in ArcGIS.
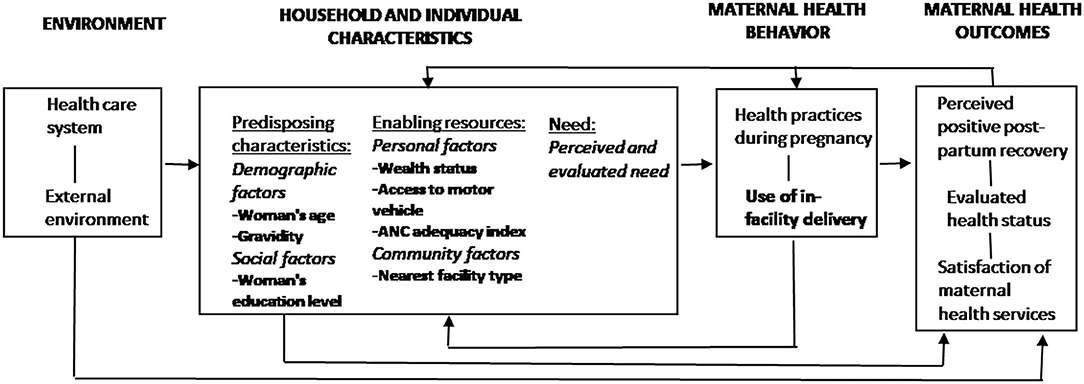
Figure 2. Conceptual model of maternal health care utilization adapted from Andersen's Behavioral Model. Variables included in the analysis are in bold.
Some studies have used ANC as a proxy for need by assuming that women who use ANC are likely to have knowledge of the services or perceive the need due to problems during pregnancy (34, 35). However, receiving ANC is likely to lead to childbirth in certain locations because the woman is better connected to the health care system and not necessarily because she has more need. Thus, ANC adequacy index was included as an enabling factor.
The ANC adequacy index was based on four dimensions of continuity and adequacy: skill of provider (physician, nurse, or midwife), timeliness (care initiated during the first 4 months of pregnancy), sufficiency (at least four ANC visits during the pregnancy), and appropriateness (summary indicator of nine services received: weight check, blood pressure check, urine exam, blood test, nutrition counseling, counseling on signs of pregnancy complications, counseling on where to go when complications occur, iron and folic acid supplementation, and tetanus toxoid 2 vaccine). Studies in LMICs commonly use the receipt of >4 ANC visits due to limited data availability. We modified the Adequacy of Prenatal Care Utilization Index to generate this ANC adequacy index to account for timeliness, content, and process of care based on WHO recommendations as the number of visits alone do not correlate with content and process of care received (36, 37). Use of an ANC index is limited in the LMIC context, however, the need to standardize and better measure effective ANC coverage has been recognized (37, 38). We used a threshold of six services received, relaxing the 80% threshold used in similar studies for “good” or “adequate” ANC that used medical record data (39, 40). ANC was considered adequate if a woman had at least four skilled ANC visits in the first 4 months of pregnancy with at least six of the nine services received. ANC was considered inadequate if a woman had at least one skilled ANC visit after the first 4 months of pregnancy and less than six services received.
Covariates in the model include the province of residence, whether the woman lived in the catchment area of a facility that received the RBF intervention, and year (2010, 2013, 2015).
We accounted for the survey design and weights at each level. A multinomial logistic regression was used to assess the relationship between the characteristics of women and their choice of childbirth location; because giving birth at home has the highest likelihood of maternal-related complications and death and considered undesirable location from a policy perspective, it was selected as the comparison category. We assumed complete case analysis given the low level of missingness across the variables (<5%).
Descriptive statistics were weighted to account for the survey design. Multicollinearity was assessed by obtaining the variance inflation factors (VIF); security incidents and provincial health performance score were both excluded from the final model due to their high levels of correlation with the province variable. Results from the multinomial logistic regression analyses are presented as average marginal effects (AME) with 95% confidence intervals (CI). All statistical analyses were done in Stata 14 (StataCorp).
We used the multinomial logistic model to predict changes in the location of childbirth by altering variables that showed significance in the model as well as our conceptual framework. To provide greater context on the associations identified through the model, we assessed potential policy-relevant variables as single scenarios and a combination of scenarios, but differences were not tested for statistical significance. We assumed full coverage of each scenario in the sample. Based on the model results and our conceptual model, we examined changes in predisposing (education level) and enabling (motor vehicle access, ANC adequacy) factors. We used the method of recycled predictions in which the variables of interest varied across the entire sample, on average, while holding other variables constant (41). The results of individual scenarios and a combination of scenarios are presented as predicted percentages (for interpretability) with 95% confidence intervals (Supplementary Table 1).
Permission to use all datasets for this secondary data analysis was granted by the Ministry of Public Health in Kabul, Afghanistan. We received an exemption from the Institutional Review Board of the authors' institute to conduct this study (#16-3202).
Of 9,705 women in the study sample, 15.1% gave birth at a public clinic, 12.1% at a public hospital, 4.7% at a private facility, and 68.1% at home. Over half the women were between 20 and 29 years of age, and fewer than 10.0% received any formal education (Table 1). Among women who delivered at home, about 40.0% were from households in the lowest two wealth quintiles. Women who delivered at a facility, however, were overwhelmingly from households in the highest two wealth quintiles (45.0% of women at a public clinic, 60.0% at a public hospital, 70.0% at a private facility). Women who went to a public hospital or private clinic lived on average <10 km from the nearest main or secondary road; women who went to a public clinic or gave birth at home lived at least 20 km away. Among women who gave birth at home, about 47.0% did not receive ANC. On the other hand, about 75.0% of women who delivered in either a public clinic or hospital received inadequate ANC; only 10.0% received adequate ANC. Fewer women received adequate ANC (8.7%) among those who gave birth at a private facility.
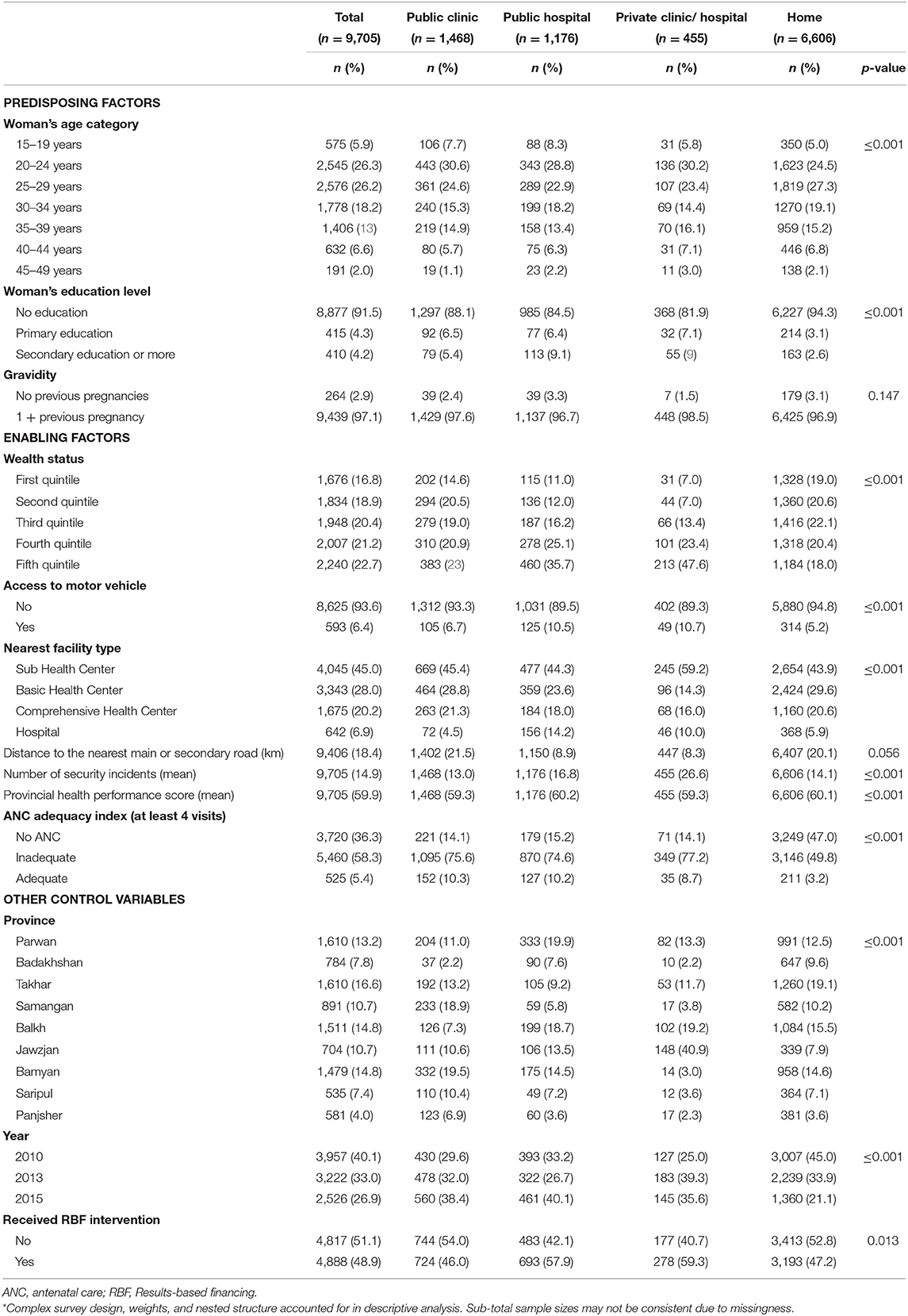
Table 1. Characteristics of women included in study sample by delivery location used for most recent birth within the last 2 years, accounting for complex survey design* (n = 9,705).
Table 2 presents the results from the multivariate multinomial logistic regression with home births as the base outcome. Education was significantly associated with a woman giving birth at a public clinic, public hospital, or a private facility compared to at home. Women with primary education had a 4.3% point increase in the predicted probability of childbirth at a public clinic [95% CI (0.0, 8.5)]. The average marginal effects of primary and secondary education were a 4.5 and 6.7% point increase in the predicted probability of childbirth at a public hospital [95% CI (1.3, 7.7); (2.9, 10.5)]. Women with secondary education had a 4.0% point increase in the predicted probability of childbirth at a private facility compared to home [95% CI (1.4, 6.5)]. Wealth status was significantly associated with a woman giving birth at a public clinic or private facility compared to home. Being in the second, fourth, and fifth quintiles compared to the first quintile was associated with a 4.1, 3.3, and 4.7% point increase in the predicted probability of childbirth at a public clinic, respectively [95% CI (1.5, 6.7); (0.2, 6.4); (1.1, 8.3)]. Being in the fifth wealth quintile compared to the first quintile was associated 3.6% point increase in the predicted probability of childbirth at a private facility [95% CI (1.0, 6.2)]. ANC adequacy index was significantly associated with a woman giving birth at any facility option compared to home. Receipt of inadequate ANC compared to no ANC was associated with a 13.5, 8.5, and 3.0% point increase in the predicted probability of childbirth at a public clinic, public hospital, or private facility, respectively [95% CI (11.3, 15.7); (6.7, 10.4); (1.9, 4.0)]. Larger associations were found between in-facility births and the receipt of adequate ANC compared to no ANC {22.6, 12.9, and 3.8% point increase in the predicted probability of childbirth at a public clinic, public hospital, or private facility, respectively [95% CI (17.4, 27.8); (9.3, 16.6); (1.4,6.3)]}.
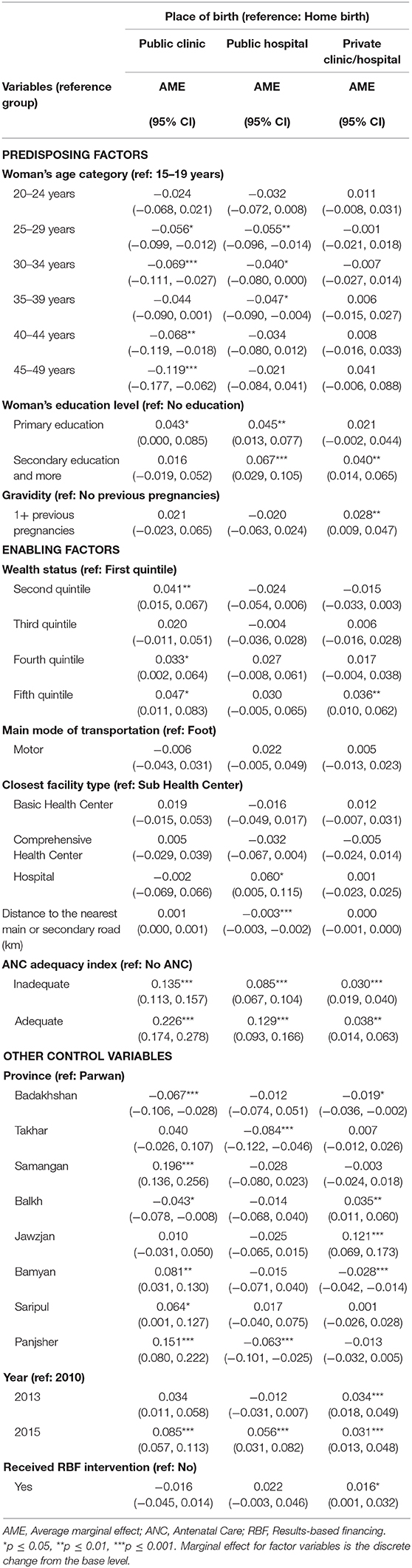
Table 2. Multinomial regression analysis of women's characteristics and childbirth location for most recent birth within the last 2 years (n = 8,921).
Figures 3, 4 present the results of the various scenarios of target variables and their predicted changes on utilization patterns of in-facility births at public clinics, public hospitals, private facilities, and home, assuming all individuals reach the full potential of the target variables. Overall, adequate ANC as a single variable yielded the largest changes in decreased home childbirth (from 66.3 to 44.4%). However, a combination of variables was the most effective in decreasing home childbirths. Increased access to secondary education and adequate ANC was associated with a decrease in home births from 66.3 to 32.2%, with 29.7% at public clinics, 26.8% at public hospitals, and 11.2% at private facilities. The addition of a motor vehicle to this combination predicted further decreased home births (to 30.0%). Increased access to primary education, adequate ANC, and motor vehicle decreased home births to 31.2% with 32.4% at public clinics, 27.0% at public hospitals, and 9.4% at private facilities. Despite assessing the full coverage of the combined scenarios, about 30.0% of women were predicted to still give birth at home.
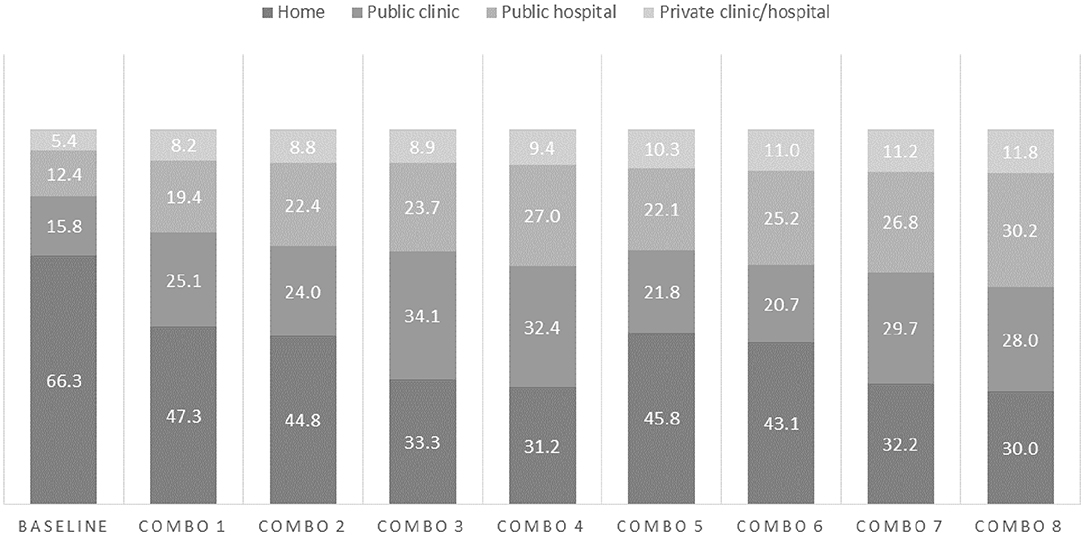
Figure 4. Predicted percentages of childbirth location given a combination of scenarios*. *Combo 1: Primary education + at least inadequate ANC; Combo2: Primary education + at least inadequate ANC + motor vehicle; Combo 3: Primary education + adequate ANC; Combo 4: Primary education + adequate ANC + motor vehicle; Combo 5: Secondary education + at least inadequate ANC; Combo 6: Secondary education + at least inadequate ANC + motor vehicle; Combo 7: Secondary education + adequate ANC; Combo 8: Secondary education + adequate ANC + motor vehicle.
Using the Andersen Behavioral Model, the findings show that women with higher levels of education, greater household wealth, and having any ANC were more likely to give birth in public or private facilities than at home. The scenario analysis found that a combination of variables, particularly access to secondary education, adequate ANC, and motor vehicle for care, would have the largest change on the predicted decrease of home births and increase of in-facility births, particularly at public clinics and hospitals. These results are consistent with the literature and highlight the need for decisionmakers to consider a combination of multisector efforts (e.g., health, education, and social protection), to increase equitable use of maternal health services.
We found that primary and secondary education increased a woman's predicted probability of giving birth at a higher-level facility. Maternal education has been found to be a key determinant of maternal health utilization (42, 43). Women with higher levels of education often know when to seek care, understand benefits of preventive care, and are more empowered to actually seek care (44). Education can serve as a tool to enhance a woman's confidence and ability to make decisions for herself and seek out higher quality care (45, 46). However, within the context of strongly patriarchal societies, studies have shown the value of engaging husbands and other household decision makers, such as mothers-in-law, in educational sessions for improving maternal and child health (10, 43, 47). The ability of a woman to seek maternal health care is correlated with her household decision-making status and level of her husband's education, occupation, and support (48–50). Further, a woman's ability to obtain secondary education has been a consistent predictor of maternal health service utilization (51, 52). These factors should not be overlooked when designing programs to either jointly engage husbands and mothers-in-law or to recognize their role as a precondition to successful maternal health education interventions, as well as education for young girls.
Similar to other studies (11, 23, 45), we found that the poorest women were more likely to deliver at home and wealthier women were more likely to deliver in the private sector. We also found that women in the second poorest wealth quintile were more likely to use a public clinic for childbirth compared to the poorest women. Public clinics, which deliver the BPHS, have been found to be more equitable than other facility types (public hospitals or private facilities) in Afghanistan (23, 25). However, the poorest women may still face barriers to accessing the lowest levels of the health system for maternal healthcare. Although public clinics should be free of charge, patients often make informal payments for services and must bear the additional costs for such things as transportation and food, likely unaffordable for the poorest women (10, 20). High out-of-pocket payments by households remains a major barrier to accessing healthcare in Afghanistan (53). Households reported spending on transportation for healthcare services as the second highest expense following medicines and supplies (54). Policies are needed to address financial barriers to accessing maternal healthcare services, particularly for transportation, such as through vouchers, cash transfers, or community transport options to cover the cost and availability of transportation to a health facility.
Use of ANC was positively associated with giving birth at any of the facility types. Receiving adequate ANC had almost twice the effect as inadequate ANC in the likelihood of childbirth at a public clinic. The timing and number of ANC visits have been associated with a woman's preference on where to give birth (55, 56). Inadequate services during ANC can influence a woman's decision to seek additional care during pregnancy or childbirth. ANC visits are the best opportunity to support women in birth preparedness and to understand signs of pregnancy complications and how to seek emergency obstetric care when needed. Birth preparedness has been positively associated with in-facility births and as a means to reduce maternal and newborn deaths (57–59). Implementation of birth plans during ANC visits should be considered as a strategy to improve the uptake of maternal health services, including the number and content of ANC visits, skilled attendant at birth, and post-natal care. However, observed associations between ANC use and in-facility delivery may be suspect of resulting from confounding factors such as availability of and access to services, knowledge of pregnancy risks, and attitudes toward health services (60).
Although motor vehicle access was not significant in the model, it is commonly cited as a barrier to accessing facilities in qualitative studies and in other studies. Adding this variable to the scenario analysis achieved the highest predicted increase of in-facility births. Where resources are limited and increasing the number of facilities infeasible, countries like Afghanistan may consider different modes of transport to influence access to needed health care [such as conditional cash transfer for transportation (61, 62)], particularly in rural areas with diverse terrain (63–65).
Increasing in-facility births requires ensuring quality of care and availability of services, personnel, and medicines. With increased demand for services, particularly in the public sector, decision makers should ensure continuity of maternal healthcare services from pregnancy to post-partum and increase the availability and quality of emergency obstetric care in public facilities. In-facility births alone may not decrease mortality (66) without ensuring sufficient quality of care (67, 68). In a five-country study in sub-Saharan Africa, the quality of basic maternal healthcare functions was substantially lower in primary care compared to secondary level facilities (67). There is a perception that private health facilities have better quality care, and evidence has shown that women who can afford to, prefer to bypass their nearest public clinic for a higher level clinic or hospital (20, 69). Equitable access to quality maternity healthcare should be considered, particularly as poorer women tend to utilize services at public clinics. Further, interventions targeting women who continue to deliver at home should increase access to birth planning support, knowledge of pregnancy complications and obstetric dangers signs, and access to SBAs.
We found that the combination of secondary education, adequate ANC, and motor vehicle in the scenario analysis had the strongest signals from the model for increasing the predicted probability of in-facility childbirths. The scenario analysis does not show causality between the multisector inputs and improved maternal health care utilization; however, it highlights the importance of multisector efforts to contribute to substantial changes in maternal healthcare utilization. Further, it highlights the need for health research to better measure and assess multisector factors on healthcare use and health-related outcomes. The SDGs comprise of 17 goals to spur action among countries to improve health, education, economic growth, and tackle climate change. SDG 4 specifically focuses on universal access to primary and secondary education which would help decrease maternal mortality as stated in SDG 3. Global efforts to build coherent policies through the SDGs need to similarly bridge interactions across sectors in countries for greater human development impacts (70). Achieving the SDGs requires multisectoral interventions that address poverty, food insecurity and malnutrition, universal health coverage, quality universal education, and environmental protection (71). Investments across the relevant sectors with policy interactions may not only decrease preventable deaths but also “ensure health and well-being, and expand enabling environments” (72). Multisector interventions should be studied to better understand their linkages to improving maternal health outcomes.
We note several limitations of this study. First, we were unable to identify or account for women with high-risk pregnancies. Failing to control for pregnancy risk may introduce confounding as it is likely to be on the causal pathway. Second, our study includes nine provinces in Afghanistan, thus limiting generalizability, particularly the southern provinces which are geographically and ethnically different from the central and northern regions and have greater insecurity. Studies have shown that maternal healthcare utilization and outcomes, as well as coverage of health facilities are poorer in the southern region (15, 16, 33, 73). Third, our sample was limited to women who delivered in the past 2 years so not all births were captured. However, this shortened recall period may reduce recall bias. Fourth, the situation in Afghanistan is volatile and the security levels change rapidly in the country. We were unable to control for district-level security incidents, and it is unclear how specific villages and households are affected. Yet, evidence has shown that conflict affects access and use of health services (74). Fifth, we did not account for clustering at the village level. The multinomial model would enhance the efficiency and is likely to reduce the standard errors of coefficients by dividing the total variance into variance at the group level and that at the individual level. Although our model did not account for the variation at the village level, with a lower efficiency of detecting potentially meaningful variables predicting the use of maternal services, the coefficients remained unbiased. Sixth, we did not have the full spectrum of women's preferences for place of childbirth usually determined by a discrete choice experiment, which was beyond the scope of this study. Finally, we did not have specific quality measures of care or perceptions of care that a woman received at her place of childbirth. Perception of quality and satisfaction of care may influence a woman's decision to seek care at a specific facility and should be accounted for in future studies.
This study enhances our understanding of factors associated with the use of public facilities and the private sector for childbirth in Afghanistan. Policymakers and healthcare providers should seek to improve equity in the delivery of health services, particularly for necessary emergency obstetric care. Strengthened collaborations between health and other sectors, such as increased access to education for girls, may address critical leverage points in improving maternal health outcomes and overall well-being. Further, there is a need to address the financial barriers to transportation to reach health facilities in a timely manner. Additional research is needed to investigate health system factors that are amenable to change such as health service quality to provide a more complete understanding of individual, health systems, and community level factors that influence a woman's place of childbirth.
The data analyzed in this study is subject to the following licenses/restrictions: Raw data were generated at the Silk Route Training and Research Organization and owned by the Afghanistan Ministry of Public Health. Derived data supporting the findings of this study are available from the corresponding author (CK) on request, with permission from the Afghanistan Ministry of Public Health. Several of the spatial datasets that support the findings of this study are openly available in the Humanitarian Data Exchange at data.humdata.org. Requests to access these datasets should be directed to Christine Kim, christine_kim@alumni.unc.edu;data.humdata.org.
Permission to use all datasets for this secondary data analysis was granted by the Ministry of Public Health in Kabul, Afghanistan. We received an exemption from the Institutional Review Board of the authors' institute to conduct this study (#16-3202).
CK contributed to study conception and design, analyzed data, and drafted the manuscript. DE, KN, AS, and WZ contributed to critical review and manuscript revision. All authors contributed to the article and approved the submitted version.
DE was employed by the company Paraxel International.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We thank the Silk Route Training and Research Organization and the Afghanistan Ministry of Public Health for their support and sharing data for this study.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2020.571055/full#supplementary-material
Abbreviations: ANC, Antenatal Care; BPHS, Basic Package of Health Services; LMIC, Low and middle-income country; MMR, Maternal mortality ratio; NGO, Non-governmental organization; RBF, Results based Financing; SBA, Skilled Birth Attendance; SDG, Sustainable Development Goals; VIF, Variance Inflation Factors.
1. Kassebaum NJ, Barber RM, Dandona L, Hay SI, Larson HJ, Lim SS, et al. Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. (2016) 388:1775–812. doi: 10.1016/S0140-6736(16)31470-2
2. Alkema L, Chou D, Hogan D, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet. (2016) 38:462–74. doi: 10.1016/S0140-6736(15)00838-7
3. Bank TW. Trends in Maternal Mortality: 1990 to 2013 Estimates by WHO, UNICEF, UNFPA. The World Bank and the United Nations Population Division, Geneva (2016). p. 1–7.
4. Campbell OM, and Graham WJ. Strategies for reducing maternal mortality: getting on with what works. Lancet. (2006) 368:1284–99. doi: 10.1016/S0140-6736(06)69381-1
5. Mahdi SS, and Habib O. A study on preference and practices of women regarding place of delivery. East Mediterr Heal J. (2010) 16:874–8. doi: 10.26719/2010.16.8.874
6. Joseph G, Da Silva ICM, Wehrmeister FC, Barros AJD, and Victora CG. Inequalities in the coverage of place of delivery and skilled birth attendance: analyses of cross-sectional surveys in 80 low and middle-income countries. Reprod Health. (2016) 13:1–13. doi: 10.1186/s12978-016-0192-2
7. Kruk ME, Paczkowski M, Mbaruku G, De Pinho H, and Galea S. Women's preferences for place of delivery in rural Tanzania: a population-based discrete choice experiment. Am J Public Health. (2009) 99:1666–72. doi: 10.2105/AJPH.2008.146209
8. Wild K, Barclay L, Kelly P, and Martins N. Birth choices in Timor-Leste : a framework for understanding the use of maternal health services in low resource settings. Soc Sci Med. (2010) 71:2038–45. doi: 10.1016/j.socscimed.2010.09.012
9. Newbrander W, Natiq K, Shahim S, Hamid N, and Skena NB. Barriers to appropriate care for mothers and infants during the perinatal period in rural Afghanistan: a qualitative assessment. Glob Public Health. (2014) 9:93–109. doi: 10.1080/17441692.2013.827735
10. Higgins-Steele A, Burke J, Foshanji AI, Farewar F, Naziri M, Seddiqi S, et al. Barriers associated with care-seeking for institutional delivery among rural women in three provinces in Afghanistan. BMC Pregn Childb. (2018) 18:1–9. doi: 10.1186/s12884-018-1890-2
11. Thakur B, Kar S, Pathak M, and Thakur N. Public-private share in maternal health care services utilization in India: a multinomial logistic regression analysis from three consecutive survey data. Clin Epidemiol Glob Heal. (2019) 7:22–8. doi: 10.1016/j.cegh.2017.12.003
12. Yorlets RR, Iverson KR, Leslie HH, Gage AD, Roder-Dewan S, Nsona H, et al. Latent class analysis of the social determinants of health-seeking behaviour for delivery among pregnant women in Malawi. BMJ Glob Heal. (2019) 4:1–10. doi: 10.1136/bmjgh-2018-000930
13. Bartlett L, LeFevre A, Zimmerman L, Saeedzai SA, Torkamani S, Zabih W, et al. Progress and inequities in maternal mortality in Afghanistan. (RAMOS-II): a retrospective observational study. Lancet Glob Heal. (2017) 5:e545–55. doi: 10.1016/S2214-109X(17)30139-0
14. Alba S, Sondorp E, Kleipool E, Yadav RS, Rahim AS, Juszkiewicz KT, et al. Estimating maternal mortality : what have we learned from 16 years of surveys in Afghanistan? BMJ Glob Heal. (2020) 5:e002126. doi: 10.1136/bmjgh-2019-002126
15. Akseer N, Bhatti Z, Rizvi A, Salehi AS, Mashal T, and Bhutta ZA. Coverage and inequalities in maternal and child health interventions in Afghanistan. BMC Public Health. (2016) 16:797. doi: 10.1186/s12889-016-3406-1
16. Ministry of Public Health [Afghanistan] and Central Statistics Organization [Afghanistan]. Afghanistan Demographic and Health Survey 2015. (2017). Available online at: https://dhsprogram.com/pubs/pdf/FR323/FR323.pdf (accessed November 25, 2020).
17. Mayhew M, Hansen PM, Peters DH, Edward A, Singh LP, Dwivedi V, et al. Determinants of skilled birth attendant utilization in Afghanistan: a cross-sectional study. Am J Public Health. (2008) 98:1849–56. doi: 10.2105/AJPH.2007.123471
18. Shooshtari S, Samadi SA, Zarei K, Naghipur S, Martin T, and Lee M. Facilitating and impeding factors for knowledge translation in intellectual and developmental disabilities: results from a consultation workshop in Iran. J Policy Pract Intellect Disabil. (2014) 11:210–6. doi: 10.1111/jppi.12084
19. Shahram MS, Hamajima N, and Reyer JA. Factors affecting maternal healthcare utilization in Afghanistan: secondary analysis of Afghanistan Health Survey 2012. Nagoya J Med Sci. (2015) 77:595–607.
20. Tappis H, Koblinsky M, Doocy S, Warren N, and Peters DH. Bypassing primary care facilities for childbirth: findings from a multilevel analysis of skilled birth attendance determinants in Afghanistan. J Midwifery Womens Health (2016) 61:185–95. doi: 10.1111/jmwh.12359
21. Mumtaz S, Bahk J, and Khang YH. Current status and determinants of maternal healthcare utilization in Afghanistan: analysis from Afghanistan demographic and health survey 2015. PLoS ONE. (2019) 14:1–14. doi: 10.1371/journal.pone.0217827
22. Hirose A, Borchert M, Niksear H, Alkozai AS, Cox J, Gardiner J, et al. Difficulties leaving home: a cross-sectional study of delays in seeking emergency obstetric care in Herat, Afghanistan. Soc Sci Med. (2011) 73:1003–13. doi: 10.1016/j.socscimed.2011.07.011
23. Kim C, Saeed KMA, Salehi AS, and Zeng W. An equity analysis of utilization of health services in Afghanistan using a national household survey. BMC Public Health. (2016) 16:1226. doi: 10.1186/s12889-016-3894-z
24. Salehi AS, Saljuqi ATK, Akseer N, Rao K, and Coe K. Factors influencing performance by contracted non-state providers implementing a basic package of health services in Afghanistan. Int J Equity Health. (2018) 17:1–16. doi: 10.1186/s12939-018-0847-4
25. Alonge O, Gupta S, Engineer C, Salehi AS, and Peters DH. Assessing the pro-poor effect of different contracting schemes for health services on health facilities in rural Afghanistan. Health Policy Plan. (2015) 30:1229–42. doi: 10.1093/heapol/czu127
26. Ergler CR, Sakdapolrak P, Bohle HG, and Kearns RA. Entitlements to health care: why is there a preference for private facilities among poorer residents of Chennai, India? Soc Sci Med. (2011) 72:327–37. doi: 10.1016/j.socscimed.2010.09.042
27. Babitsch B, Gohl D, von Lengerke T, and Von Lengerke T. Re-revisiting Andersen's behavioral model of health services use: a systematic review of studies from 1998–2011. GMS Psycho Soc. (2012) 9:1–15. doi: 10.3205/psm000089
28. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. (1995) 36:1–10. doi: 10.2307/2137284
29. Ministry of Public Health (Afghanistan) Royal Tropical Institute of Amsterdam (KIT) and Silk Route Training and Research Organization (SRTRO). An Impact Evaluation of the Results-based Financing Intervention in Afghanistan. Final Report 2015 (2015).
30. Engineer CY, Dale E, Agarwal A, Agarwal A, Alonge O, Edward A, et al. Effectiveness of a pay-for-performance intervention to improve maternal and child health services in Afghanistan: a cluster-randomized trial. Int J Epidemiol. (2016) 45:451–9. doi: 10.1093/ije/dyv362
31. INSO. International NGO Safety Organization. (2011). Available online at: https://www.ngosafety.org/keydata-dashboard/ (accessed October 28, 2020).
32. OCHA. The Humanitarian Data Exchange v1.32.2. (2019). Available online at: https://data.humdata.org/search?q=afghanistan&ext_search_source=main-nav&page=1 (accessed July 28, 2019).
34. Mubyazi G. Knowledge and perceptions of antenatal services need and delivery and reasons for seeking such services among women in Tanzania: implications for utilization and coverage of intermittent presumptive treatment of malaria in pregnancy in two districts. Rwanda J. (2015) 2:65. doi: 10.4314/rjhs.v2i1.9F
35. Nisar YB, Aurangzeb B, Dibley MJ, and Alam A. Qualitative exploration of facilitating factors and barriers to use of antenatal care services by pregnant women in urban and rural settings in Pakistan. BMC Pregn Childb. (2016) 16:1–9. doi: 10.1186/s12884-016-0829-8
36. Kotelchuck M. An evaluation of the kessner adequacy of prenatal care index and a proposed adequacy of prenatal care utilization index. Am J Public Health. (1994) 84:1414–20. doi: 10.2105/AJPH.84.9.1414
37. Hodgins S, and Agostino D. The quality – coverage gap in antenatal care : toward better measurement of effective coverage. Glob Heal. (2014) 2:173–81. doi: 10.9745/GHSP-D-13-00176
38. Morón-Duarte LS, Ramirez Varela A, Segura O, and Freitas da Silveira M. Quality assessment indicators in antenatal care worldwide: a systematic review. Int J Qual Heal Care. (2018) 31:497–505. doi: 10.1093/intqhc/mzy206
39. Majrooh MA, Hasnain S, Akram J, Siddiqui A, and Memon ZA. Coverage and quality of antenatal care provided at primary health care facilities in the “Punjab” province of “Pakistan.” PLoS ONE. (2014) 9:e113390. doi: 10.1371/journal.pone.0113390
40. Yeoh PL, Hornetz K, Shauki NIA, and Dahlui M. Assessing the extent of adherence to the recommended antenatal care content in Malaysia: Room for improvement. PLoS ONE. (2015) 10:1–15. doi: 10.1371/journal.pone.0135301
41. Fagerland MW, and Hosmer DW. A generalized Hosmer–Lemeshow goodness-of-fit test for multinomial logistic regression models. Stata J. (2012) 12:447–53. doi: 10.1177/1536867X1201200307
42. Adam IF. The influence of maternal health education on the place of delivery in conflict settings of Darfur, Sudan. Confl Health. (2015) 9:1–9. doi: 10.1186/s13031-015-0057-2
43. Gopalan SS, Das A, and Howard N. Maternal and neonatal service usage and determinants in fragile and conflict-affected situations: a systematic review of Asia and the Middle-East. BMC Womens Health. (2017) 17:1–12. doi: 10.1186/s12905-017-0379-x
44. Celik Y, and Hotchkiss DR. The socio-economic determinants of maternal health care utilization in Turkey. Soc Sci Med. (2000) 50:1797–806. doi: 10.1016/S0277-9536(99)00418-9
45. Rutaremwa G, Wandera SO, Jhamba T, Akiror E, and Kiconco A. Determinants of maternal health services utilization in Uganda. BMC Health Serv Res. (2015) 15:1–8. doi: 10.1186/s12913-015-0943-8
46. Cohen J, Golub G, Kruk ME, and McConnell M. Do active patients seek higher quality prenatal care?: A panel data analysis from Nairobi, Kenya. Prev. Med. (2016) 92, 74–81. doi: 10.1016/j.ypmed.2016.09.014
47. Mahato PK, van Teijlingen E, Simkhada P, Sheppard ZA, and Silwal RC. Factors related to choice of place of birth in a district in Nepal. Sex Reprod Healthc. (2017) 13:91–6. doi: 10.1016/j.srhc.2017.07.002
48. Lewis S, Lee A, and Simkhada P. The role of husbands in maternal health and safe childbirth in rural Nepal: a qualitative study. BMC Pregn Childb. (2015) 15:1–10. doi: 10.1186/s12884-015-0599-8
49. Adjiwanou V, Bougma M, and LeGrand T. The effect of partners' education on women's reproductive and maternal health in developing countries. Soc Sci Med. (2018) 197:104–15. doi: 10.1016/j.socscimed.2017.11.054
50. Rahman AE, Perkins J, Islam S, Siddique AB, Moinuddin M, Anwar MR, et al. Knowledge and involvement of husbands in maternal and newborn health in rural Bangladesh. BMC Pregn Childb. (2018) 18:1–12. doi: 10.1186/s12884-018-1882-2
51. Raghupathy S. Education and the use of maternal health care in Thailand. Soc Sci Med. (1996) 43:459–71. doi: 10.1016/0277-9536(95)00411-4
52. Ikeako LC, Onah HE, and Iloabachie GC. Influence of formal maternal education on the use of maternity services in Enugu, Nigeria. J Obstet Gynaecol. (2006) 26:30–4. doi: 10.1080/01443610500364004
53. Frost A, Wilkinson M, Boyle P, Patel P, and Sullivan R. An assessment of the barriers to accessing the Basic Package of Health Services. (BPHS) in Afghanistan: was the BPHS a success? Global Health. (2016) 12:71. doi: 10.1186/s12992-016-0212-6
54. National Statistics and Information Authority (NSIA) Ministry of Public Health (MoPH) and Royal Tropical Institute [Amsterdam]. Afghanistan Health Survey 2018. Kabul (2019). Available online at: https://www.kit.nl/wp-content/uploads/2019/07/AHS-2018-report-FINAL-15-4-2019.pdf (accessed November 25, 2020).
55. Sharma SR, Poudyal AK, Devkota BM, and Singh S. Factors associated with place of delivery in rural Nepal. BMC Public Health. (2014) 14:306. doi: 10.1186/1471-2458-14-306
56. Tebekaw Y, James Mashalla Y, and Thupayagale-Tshweneagae G. Factors influencing women's preferences for places to give birth in Addis Ababa, Ethiopia. Obstet Gynecol Int. (2015) 2015:1–7. doi: 10.1155/2015/439748
57. Magoma M, Requejo J, Campbell O, Cousens S, Merialdi M, and Filippi V. The effectiveness of birth plans in increasing use of skilled care at delivery and postnatal care in rural Tanzania: a cluster randomised trial. Trop Med Int Heal. (2013) 18:435–43. doi: 10.1111/tmi.12069
58. Nawal D, and Goli S. Birth preparedness and its effect on place of delivery and post-natal check-ups in Nepal. PLoS ONE. (2013) 8:e60957. doi: 10.1371/journal.pone.0060957
59. Wilcox ML, Krupp K, Niranjankumar B, Srinivas V, Jaykrishna P, Arun A, et al. Birth preparedness and place of birth in rural Mysore, India: a prospective cohort study. Midwifery. (2016) 34:245–52. doi: 10.1016/j.midw.2015.11.001
60. Gabrysch S, and Campbell O. Still too far to walk : Literature review of the determinants of delivery service use. BMC Pregn Childb. (2009) 18:1–18. doi: 10.1186/1471-2393-9-34
61. Lin A, and Salehi AS. Stimulating demand: effects of a conditional cash transfer programme on increasing maternal and child health-service utilisation in Afghanistan, a quasi-experimental study. Lancet. (2013) 381:S84. doi: 10.1016/S0140-6736(13)61338-0
62. Edmond KM, Foshanji AI, Naziri M, Higgins-Steele A, Burke JM, Strobel N, et al. Conditional cash transfers to improve use of health facilities by mothers and newborns in conflict affected countries, a prospective population based intervention study from Afghanistan. BMC Pregn Childb. (2019) 19:1–18. doi: 10.1186/s12884-019-2327-2
63. dos Anjos Luis A, and Cabral P. Geographic accessibility to primary healthcare centers in Mozambique. Int J Equity Health. (2016) 15:173. doi: 10.1186/s12939-016-0455-0
64. Chen YN, Schmitz MM, Serbanescu F, Dynes MM, Maro G, and Kramer MR. Geographic access modeling of emergency obstetric and neonatal care in Kigoma Region, Tanzania: Transportation Schemes and Programmatic Implications. Glob Heal Sci Pract. (2017) 5:430–45. doi: 10.9745/GHSP-D-17-00110
65. Kim C, Tappis H, McDaniel P, Soroush MS, Fried B, Weinberger M, et al. National and subnational estimates of coverage and travel time to emergency obstetric care in Afghanistan: modeling of spatial accessibility. Heal Place. (2020) 66:102452. doi: 10.1016/j.healthplace.2020.102452
66. Gabrysch S, Nesbitt RC, Schoeps A, Hurt L, Soremekun S, Edmond K, et al. Does facility birth reduce maternal and perinatal mortality in Brong Ahafo, Ghana? A secondary analysis using data on 119 244 pregnancies from two cluster-randomised controlled trials. Lancet Glob Heal. (2019)7:e1074–87. doi: 10.1016/S2214-109X(19)30165-2
67. Kruk ME, Leslie HH, Verguet S, Mbaruku GM, Adanu RMK, and Langer A. Quality of basic maternal care functions in health facilities of five African countries: an analysis of national health system surveys. Lancet Glob Heal. (2016) 4:e845–55. doi: 10.1016/S2214-109X(16)30180-2
68. Fink G, and Cohen J. Delivering quality: safe childbirth requires more than facilities. Lancet Glob Heal. (2019) 7:e990–1. doi: 10.1016/S2214-109X(19)30193-7
69. Altai Consulting. Private Secotr Healthcare Provision in Afghanistan. Kabul: Altai Consulting (2019).
70. Nilsson M, Chisholm E, Griggs D, Howden-Chapman P, McCollum D, Messerli P, et al. Mapping interactions between the sustainable development goals: lessons learned and ways forward. Sustain Sci. (2018) 13:1489–503. doi: 10.1007/s11625-018-0604-z
71. Tangcharoensathien V, Mills A, and Palu T. Accelerating health equity: the key role of universal health coverage in the sustainable development goals. BMC Med. (2015) 13:1–5. doi: 10.1186/s12916-015-0342-3
72. Brizuela V, and Tunçalp Ö. Global initiatives in maternal and newborn health. Obstet Med. (2017) 10:21–5. doi: 10.1177/1753495X16684987
73. Mirzazada S, Padhani ZA, Jabeen S, Fatima M, Rizvi A, Ansari U, et al. Impact of conflict on maternal and child health service delivery: a country case study of Afghanistan. Confl Health. (2020) 14:1–13. doi: 10.1186/s13031-020-00285-x
Keywords: maternal health care utilization, place of childbirth, Afghanistan, health equity, healthcare access
Citation: Kim C, Erim D, Natiq K, Salehi AS and Zeng W (2020) Combination of Interventions Needed to Improve Maternal Healthcare Utilization: A Multinomial Analysis of the Inequity in Place of Childbirth in Afghanistan. Front. Glob. Womens Health 1:571055. doi: 10.3389/fgwh.2020.571055
Received: 09 June 2020; Accepted: 19 November 2020;
Published: 08 December 2020.
Edited by:
Tabassum Firoz, Yale New Haven Health System, United StatesReviewed by:
Maisam Najafizada, Memorial University of Newfoundland, CanadaCopyright © 2020 Kim, Erim, Natiq, Salehi and Zeng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christine Kim, Y2hyaXN0aW5lX2tpbUBhbHVtbmkudW5jLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.