
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Gastroenterol. , 01 August 2024
Sec. Endoscopy
Volume 3 - 2024 | https://doi.org/10.3389/fgstr.2024.1409290
 Kelly L. Buchanan1
Kelly L. Buchanan1 Robert M. Wilechansky2
Robert M. Wilechansky2 Mythili P. Pathipati2
Mythili P. Pathipati2 Allan M. Goldstein3
Allan M. Goldstein3 Daniel P. Ryan3
Daniel P. Ryan3 Joseph C. Yarze2*
Joseph C. Yarze2*A 21-year-old man presented with severe abdominal pain four days after undergoing upper endoscopy with duodenal biopsies and was found to have an intramural duodenal hematoma. Symptoms progressed after attempts at diet advancement, and repeat imaging showed an enlarging hematoma with duodenal obstruction. The patient was managed with arterial embolization followed by laparoscopic surgical evacuation of the hematoma. This is the first report of an enlarging duodenal hematoma managed by this combination approach. While surgical interventions have previously been reserved for the most severe cases, we review the literature on minimally invasive approaches to manage this rare endoscopic complication.
Intramural duodenal hematoma is a rare complication of upper endoscopy. Information about its occurrence is limited to case reports, and data on incidence rates in adults are lacking. Duodenal hematoma after upper endoscopy is often related to tissue sampling, and the sequelae can be significant; patients may require several weeks of nutritional support due to duodenal obstruction (1–3). Early recognition is key to initiation of conservative management with nasogastric decompression and parenteral nutrition. Surgical decompression is considered in severe cases (4), and recent reports have raised the possibility of minimally invasive approaches to treatment (3, 5).
A 21-year-old man with eosinophilic esophagitis was admitted with acute, severe abdominal pain. The pain initially began in the lower abdomen and progressed to involve the right upper quadrant and epigastrium. He had undergone upper endoscopy at another institution 4 days previously, at which time duodenal biopsies were performed to screen for celiac disease due to chronic upper gastrointestinal symptoms. The EGD was uneventful and there was not any report of excessive bleeding during the procedure. Pathology from these biopsies showed vascular congestion and erosion, negative for increased intraepithelial lymphocytes and negative for eosinophilic infiltration. On admission, his physical exam was notable for right upper quadrant and epigastric tenderness. Bloodwork revealed hypokalemia, and normal blood counts, liver enzymes and serum lipase. A computed tomography (CT) scan showed focal dilation of the second and third portions of the duodenum with luminal narrowing and an intramural duodenal hematoma extending from the second part of the duodenum (D2) to the ligament of Treitz, measuring 4.7 x 3.0 x 3.5 cm (Figure 1). Over the initial 24 hours of hospitalization, the patient developed nausea and bilious emesis with concern for intestinal obstruction. A repeat CT scan showed significant enlargement of the duodenal hematoma, measuring 3.9 x 8.3 x 4.5 cm (Figure 1). A nasogastric tube was placed with copious output. On the third day of hospitalization, due to progressive symptoms, he underwent CT angiography of the abdomen, which demonstrated a punctate focus of arterial phase enhancement consistent with active extravasation (Figure 1). Urgent gastroduodenal arterial embolization was performed. Nasogastric decompression was continued and parenteral feeding was instituted without clinical improvement. On day 7 of hospitalization, given continued lack of improvement with conservative treatment, surgical laparoscopic evacuation of the duodenal hematoma was performed after multidisciplinary discussion. During surgery, a bulging duodenal hematoma was visualized, submucosal blot clot was evacuated, and a drain was placed. Within hours of surgery, nasogastric tube output dropped precipitously, and the nasogastric tube was removed on post-operative day 2. Drain was removed on post-operative day 5. The diet was advanced successfully and the patient was discharged after 13 days of hospitalization.
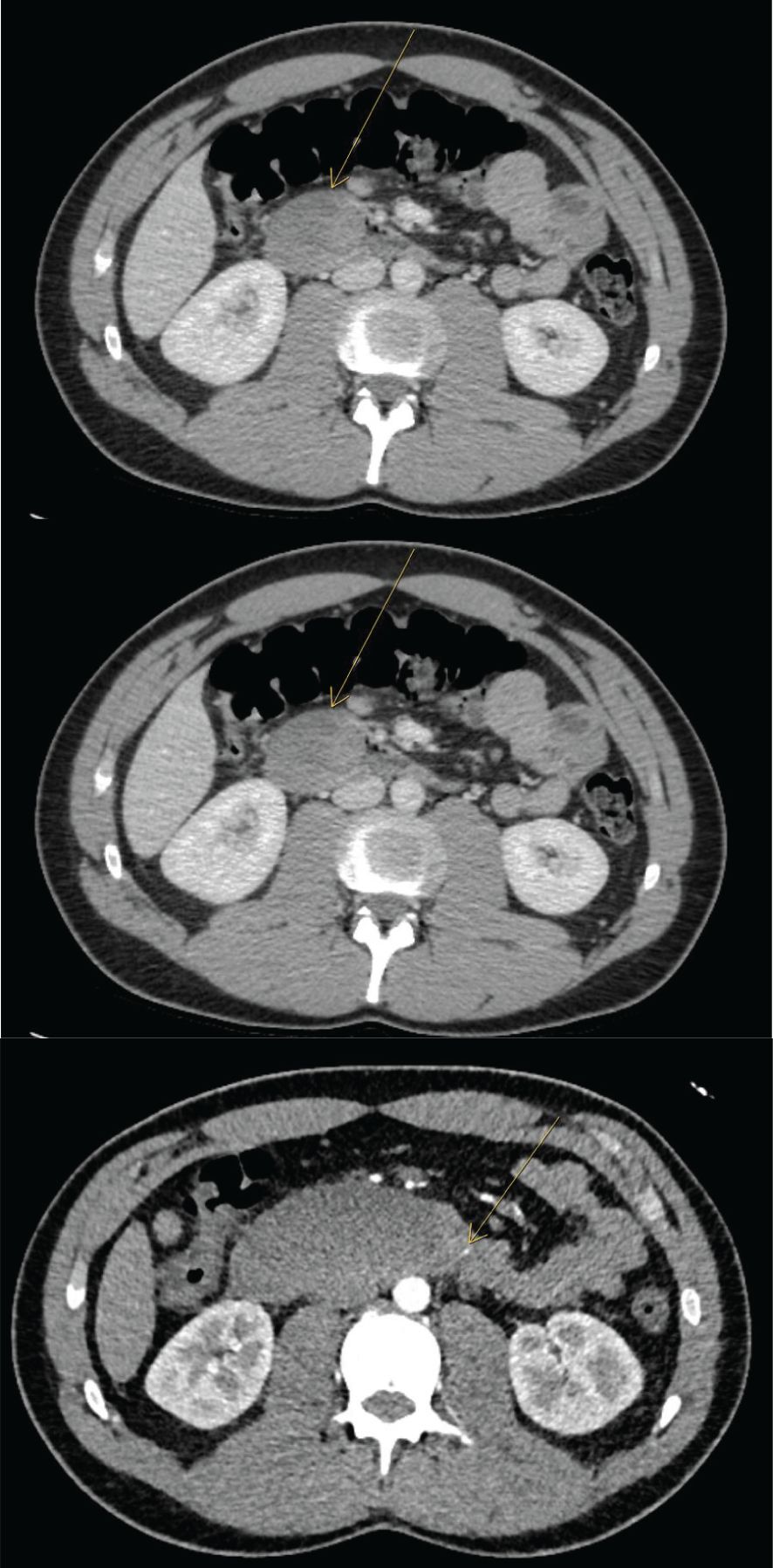
Figure 1 Progressive CT A/P images at day 1 and day 3 with expansion of duodenal hematoma and CT angio at day 5 with area of active extravasation.
Intramural duodenal hematoma is an exceedingly rare complication after endoscopic biopsy. Duodenal hematoma is more commonly caused by blunt abdominal trauma, particularly in children due to their thinner abdominal walls. In the post-endoscopy population, research to date has focused on its incidence in pediatric populations. In a single-center retrospective study of 26,905 pediatric patients, intramural duodenal hematoma after endoscopy had an incidence of approximately 1 in 2000 (1). Similar numbers in children have been reported at other institutions (2). The incidence rate of duodenal hematoma in adults has not been established, and may be even more rare. The first case report of duodenal hematoma after routine endoscopic biopsy in an adult was reported in 1989 (6), and since then, there have been only 10 additional reports (Table 1). Additional cases of duodenal hematoma have been reported after other endoscopic procedures [e.g. endoscopic retrograde cholangiopancreatography (7), ulcer therapy (8)], as well as in cases of blunt abdominal trauma, duodenal ulcers, and pancreatitis (9).
Given the low incidence rate, the mechanism of and risk factors for duodenal hematoma development after endoscopy are poorly characterized. Proposed mechanisms include both macroscopic and microscopic factors. For example, the duodenum may be at increased risk for shear injury given that it is in a fixed retroperitoneal position adjacent to the lumbar spine (6). Further, it has a rich, highly vascularized submucosal plexus which can be prone to bleeding (2, 9). Procedure-related risk factors include method of sedation and positioning, while procedural experience has not been shown to be related to risk (1). Clinical risk factors for duodenal hematoma include coagulopathy, prior solid organ transplant, prior bone marrow transplant, and anticoagulation (1, 2, 6). Our patient had no known risk factors.
The natural history of duodenal hematoma has been established through case reports. Patients typically present within the first 72 hours following endoscopy (1); in this case, the patient presented at approximately 96 hours. Growth of the hematoma in this location can occlude the duodenal lumen causing proximal intestinal obstruction, resulting in vomiting. Compression and obstruction of the ampulla of Vater can lead to pancreatitis, and if left untreated, biliary obstruction may occur. In order to avoid these complications, we felt that surgical management would provide the most definitive solution given that surgical management has been the mainstay of treatment thus far. There are rare reports of more serious complications such as extraluminal rupture and hemoperitoneum (4).
The standard of care for duodenal hematoma after endoscopic biopsy is conservative management; of the 11 case reports in adults, 7 were managed conservatively with nasogastric decompression and parenteral nutrition (Table 1) (6, 10–14). In these patients, 3–4 weeks of parenteral nutrition was often required before clinical improvement. The other 4 patients received intervention: surgical evacuation (10), endoscopic dilation (3), or ultrasound-guided drainage (15). AXIOS stent is a possibility for management as well (16).
Here, we report the first case of a patient managed with arterial embolization to limit hematoma expansion followed by surgical evacuation to treat persistent duodenal obstruction. While conservative and surgical management have been the mainstays of treatment to date, advances in endoscopic and interventional radiology techniques have expanded treatment options. On review of duodenal hematoma reports across the spectrum of age and causes, 7 prior cases have been managed with minimally invasive techniques, including image-guided drainage (3, 15, 17, 18), endoscopic incision and drainage (7, 8), and endoscopy with dilation (3, 5). Arterial embolization represents a new approach for active bleeding (Table 2).
In this case, we attempted conservative manage at first but the patient’s symptoms became worse each day. He initially did not have obstructive symptoms and developed these the course of his admission and was having difficulty tolerating tube feeds with an NG tube. Ultimately multiple options were presented to the patient, but given the rapid expansion of his hematoma and ongoing severe symptoms, we felt that surgical intervention would provide the most definitive and expeditious improvement which was in line with the patient’s preferences as well.
In conclusion, we describe an unusual case of duodenal hematoma in a 21-year-old man occurring after routine endoscopic duodenal biopsies. The patient had no clear risk factors, he presented more than 72 hours after endoscopy, and the hematoma enlarged by more than three-fold in the first 24-hours of hospital observation. Given rapid progression of the hematoma and persistent duodenal obstruction, the patient was managed with a combination of arterial embolization which successfully prevented further expansion of the hematoma, and subsequent laparoscopic hematoma evacuation. Further study and use of minimally invasive approaches for duodenal hematoma management could help reduce potential complications and time to recovery.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
KB: Writing – original draft, Writing – review & editing. RW: Writing – review & editing. MP: Writing – review & editing. AG: Writing – review & editing. DR: Writing – review & editing. JY: Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Sahn B, Anupindi SA, Dadhania NJ, Kelsen JR, Nance ML, Mamula P. Duodenal hematoma following EGD: Comparison with blunt abdominal trauma-induced duodenal hematoma. J Pediatr Gastroenterol Nutr. (2015) 60:69–74. doi: 10.1097/MPG.0000000000000564
2. Guzman C, Bousvaros A, Buonomo C, Nurko S. Intraduodenal hematoma complicating intestinal biopsy: Case reports and review of the literature. Am J Gastroenterol. (1998) 93:2547–50. doi: 10.1111/j.1572-0241.1998.00716.x
3. Samra M, Al-Mouradi T, Berkelhammer C. Gastric Outlet Obstruction due to Intramural Duodenal Hematoma after Endoscopic Biopsy: Possible Therapeutic Role of Endoscopic Dilation. Case Rep Gastroenterol. (2018) 12:692–8. doi: 10.1159/000494967
4. Elmoghazy W, Noaman I, Mahfouz AE, Elaffandi A, Khalaf H. Surgical management of complicated intramural duodenal hematoma: A case report and review of the literature. Int J Surg Case Rep. (2015) 17:103–5. doi: 10.1016/j.ijscr.2015.10.028
5. Alharbi FM, Abo Amer ZA, Hamamesh KH, Algubaisi SN. Endoscopic dilatation as a new technique in managing pediatric duodenal hematoma. Saudi Med J. (2020) 41:874–7. doi: 10.15537/smj.2020.8.25128
6. Zinelis SA, Hershenson LM, Ennis MF, Boller M, Ismail-Beigi F. Intramural duodenal hematoma following upper gastrointestinal endoscopic biopsy. Dig Dis Sci. (1989) 34:289–91. doi: 10.1007/BF01536064
7. Pan YM, Wang TT, Wu J, Hu B. Endoscopic drainage for duodenal hematoma following endoscopic retrograde cholangiopancreatography: A case report. World J Gastroenterol. (2013) 19:2118–21. doi: 10.3748/wjg.v19.i13.2118
8. Kwon CIL, Ko KH, Kim HY, Kim Y, Hong SP, Hwang SG, et al. Bowel obstruction caused by an intramural duodenal hematoma: A case report of endoscopic incision and drainage. J Korean Med Sci. (2009) 24:179–83. doi: 10.3346/jkms.2009.24.1.179
9. Niehues SM, Denecke T, Bassir C, Hamm B, Haas M. Intramural duodenal hematoma: clinical course and imaging findings. Acta Radiol Open. (2019) 8:205846011983625. doi: 10.1177/2058460119836256
10. Lipson SA, Perr HA, Koerper MA, Ostroff JW, Snyder JD, Goldstein RB. Intramural duodenal hematoma after endoscopic biopsy in leukemic patients. Gastrointest Endosc. (1996) 44:620–3. doi: 10.1016/S0016-5107(96)70024-X
11. Sgouros SN, Karamanolis G, Papdopoulou E, Papageorgiou G, Stefanides G, Nastos H, et al. Postbiopsy intramural hematoma of the duodenum in an adult with Noonan’s syndrome. J Gastroenterol Hepatol. (2004) 19:1217–9. doi: 10.1111/j.1400-1746.2004.02931.x
12. Hoenisch K, Prommegger R, Schwaighofer H, Freund M, Schocke M, Vogel W, et al. Intramural duodenal hematoma after upper gastrointestinal endoscopy. Wiener Medizinische Wochenschrift. (2011) 161:441–4. doi: 10.1007/s10354-011-0029-0
13. Worynski A, Zimmerman M, Herrmann RP, Forbes GM. Intramural duodenal haematoma following endoscopic biopsy in a bone marrow transplant patient. Aust N Z J Med. (1998) 28:843–4. doi: 10.1111/j.1445-5994.1998.tb01572.x
14. Chen YY, Su WW, Soon MS, Yen HH. Gastrointestinal: Intramural hematoma of the duodenum. J Gastroenterol Hepatol. (2006) 21:1071. doi: 10.1111/j.1440-1746.2006.04522.x
15. Lloyd GM, Sutton CD, Marshall LJ, Jameson JS. Case of duodenal haematoma treated with ultrasound guided drainage. ANZ J Surg. (2004) 74:500–1. doi: 10.1111/j.1445-1433.2004.03045.x
16. Ramai D, Facciorusso A, Deluca M, Barakat M, Adler D. Adverse events associated with AXIOS stents: Insights from the manufacturer and user facility device experience database. Endosc Ultrasound. (2022) 11:231–6. doi: 10.4103/EUS-D-21-00096
17. Aizawa K, Tokuyama H, Yonezawa T, Doi M, Matsuzono Y, Matumoto M, et al. A case of traumatic intramural hematoma of the duodenum effectively treated with ultrasonically guided aspiration drainage and endoscopic balloon catheter dilatation. Gastroenterol Jpn. (1991) 26:218–23. doi: 10.1007/BF02811084
Keywords: duodenal hematoma, surgical evacuation, laparoscopic, endoscopic complications, arterial embolization
Citation: Buchanan KL, Wilechansky RM, Pathipati MP, Goldstein AM, Ryan DP and Yarze JC (2024) Duodenal hematoma following endoscopic duodenal biopsy in an adult requiring arterial embolization and surgical evacuation: a case report and review of the literature. Front. Gastroenterol. 3:1409290. doi: 10.3389/fgstr.2024.1409290
Received: 29 March 2024; Accepted: 16 July 2024;
Published: 01 August 2024.
Edited by:
Maddalena Zippi, Sandro Pertini Hospital, ItalyReviewed by:
Muhammad Hashim Hayat, Vanderbilt University Medical Center, United StatesCopyright © 2024 Buchanan, Wilechansky, Pathipati, Goldstein, Ryan and Yarze. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joseph C. Yarze, anlhcnplQG1naC5oYXJ2YXJkLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.