
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Genet., 13 December 2023
Sec. RNA
Volume 14 - 2023 | https://doi.org/10.3389/fgene.2023.1320185
This article is part of the Research TopicReviews in Non-Coding RNA: 2023View all 7 articles
Ovarian cancer is one of the female reproductive system tumors. Chemotherapy is used for advanced ovarian cancer patients; however, drug resistance is a pivotal cause of chemotherapeutic failure. Hence, it is critical to explore the molecular mechanisms of drug resistance of ovarian cancer cells and to ameliorate chemoresistance. Noncoding RNAs (ncRNAs) have been identified to critically participate in drug sensitivity in a variety of human cancers, including ovarian cancer. Among ncRNAs, circRNAs sponge miRNAs and prevent miRNAs from regulation of their target mRNAs. CircRNAs can interact with DNA or proteins to modulate gene expression. In this review, we briefly describe the biological functions of circRNAs in the development and progression of ovarian cancer. Moreover, we discuss the underneath regulatory molecular mechanisms of circRNAs on governing drug resistance in ovarian cancer. Furthermore, we mention the novel strategies to overcome drug resistance via targeting circRNAs in ovarian cancer. Due to that circRNAs play a key role in modulation of drug resistance in ovarian cancer, targeting circRNAs could be a novel approach for attenuation of chemoresistance in ovarian cancer.
Ovarian cancer is one of the malignant tumors, which belongs to the female reproductive system tumors (Giaquinto et al., 2022; Siegel et al., 2023). Ovarian cancer goes undetected in its early stages because its symptoms are vague and similar to other common female reproductive diseases. The symptoms include bloating, pelvic or abdominal pain, and changes in urinary habits. Therefore, ovarian cancer has the high fatality rate (Torre et al., 2018). The most common ovarian cancer is epithelial ovarian cancer, and the other types include stromal tumors and germ cell tumors (Arnaoutoglou et al., 2023). It is unknown regarding the cause of ovarian cancer development; however, several risk factors could contribute to ovarian carcinogenesis, such as a family history of ovarian cancer, age and certain reproductive factors (Ali et al., 2023; Rousseau et al., 2023). The reproductive factors include early onset of menstruation, late menopause and never having been pregnant. The treatment options for ovarian cancer have surgery, radiation therapy and chemotherapy (Konstantinopoulos and Matulonis, 2023; Matsas et al., 2023). Because drug resistance is one important cause of therapeutic failure, it is pivotal to explore the drug resistant mechanisms and to overcome drug resistance in ovarian cancer (Pawlowska et al., 2023).
Genetic mutations have been reported to associate with ovarian cancer progression, such as BRCA1 (breast cancer 1) mutation and BRCA2 (breast cancer 2) mutation (Sanchez-Lorenzo et al., 2022). Moreover, epigenetic regulation has been revealed to participate in the development of ovarian cancer (Wang et al., 2022a; Zhao et al., 2022). It is known that epigenetics refers to heritable changes and do not change DNA sequence. Instead, epigenetic changes include DNA methylation, chromatin remodeling and histone protein modification, which affect gene activity (Portela and Esteller, 2010). Epigenetic alterations often cause abnormal activation or inactivation of key genes, leading to various diseases (Carter and Zhao, 2021; Van Loo et al., 2022). Hypermethylation of promoter regions contributes to the silencing of tumor suppressor genes, while hypomethylation of certain regions in oncogenes confers the activation of oncogenes (Yousefi et al., 2022; Greenberg and Bourc’his, 2019). Chemical modifications of histone proteins affect the DNA accessibility to the transcriptional complex, including phosphorylation, ubiquitination, methylation and acetylation. Abnormal histone modifications lead to the dysregulation of gene expression and cause various diseases. Chromatin remodeling can reposition nucleosomes and regulate the DNA accessibility for transcription (Millan-Zambrano et al., 2022; Shvedunova and Akhtar, 2022).
NcRNAs have been documented to regulate carcinogenesis in a variety of human cancers (Winkle et al., 2021; Liu and Shang, 2022; Zhang et al., 2023a). It is clear that ncRNAs do not code for proteins, but regulate gene expression and cellular functions. NcRNAs include miRNAs (microRNAs), lncRNAs (long noncoding RNAs), snoRNAs (small nucleolar RNAs), piRNAs (piwi-interacting RNAs), rRNAs (ribosomal RNAs), siRNAs (small interfering RNAs) and circRNAs (circular RNAs) (Anastasiadou et al., 2018). In general, miRNAs have around 22 nucleotides in length and bind to the mRNAs of target genes, contributing to their degradation or inhibition of translation (Treiber et al., 2019; Shang et al., 2023). LncRNAs have more than 200 nucleotides and perform diverse functions, such as modulating chromatin structure, regulating gene expression, acting as scaffolds for protein complexes (Liu et al., 2021a; Mattick et al., 2023). CircRNAs are covalently closed RNA molecules, which are highly stable. CircRNAs can sponge miRNAs and sequester miRNAs, which prevent miRNAs from regulation of their target mRNAs. In addition, circRNAs can interact with DNA or proteins to modulate gene expression (Chen, 2020; Kristensen et al., 2022). It has been documented that ncRNAs regulate drug sensitivity in ovarian cancer (Zhang et al., 2021a; Liu et al., 2022a). Understanding the complex interplay between noncoding RNAs and drug resistance in ovarian cancer is critical for developing more effective diagnostic tools and therapeutic strategies.
Drug resistance have obtained much attention to contribute to cancer treatment failure (Freedy and Liau, 2021). Drug resistance refers to the ability of tumor cells to survive in the presence of therapies, such as targeted therapy, chemotherapy and immunotherapy (Pisa and Kapoor, 2020). Drug resistance occurs through various molecular mechanisms and limits the effectiveness of cancer therapies. Inherent resistance might be because of genetic mutations or alterations, which cause the tumor cells less susceptible to drugs. Acquired resistance develops over time after tumor cells adapt to the therapy, leading to therapy failure (Ye et al., 2023). The potential mechanisms of drug resistance include genetic mutations, activation of alternative pathways, efflux pumps, enhanced DNA repair capabilities, tumor microenvironment change (Liu et al., 2022b; Bou Antoun and Chioni, 2023). Epigenetic changes, including ncRNAs, have been reported to affect gene expression and contribute to drug resistance (Jiang et al., 2020; Xie et al., 2022).
Chemotherapy often elicits a good initial benefit; however, some patients with ovarian cancer develop malignant progression due to that tumor cells obtain resistance to chemotherapeutic drugs. Evidence has suggested that circRNAs could play an oncogenic role or exert tumor suppressive functions in ovarian cancer (Zhang et al., 2022a; Ghafouri-Fard et al., 2022; Najafi, 2023). Moreover, circRNAs might be biomarkers for diagnosis and prognosis in ovarian cancer (Qiu et al., 2022). For instance, circRNA1656 was reported to act as a potential biomarker in high grade serous ovarian cancer (Gao et al., 2019a). Plasma circN4BP2L2 was found as a useful biomarker for diagnosis in epithelial ovarian cancer (Ning et al., 2022). Furthermore, circRNAs have been identified to regulate drug resistance in ovarian cancer (Lan et al., 2021). In addition, drug resistance changes the expression of certain circRNAs (Qin et al., 2023a). However, the role and molecular mechanism of circRNAs in ovarian cancer are elusive (Liu et al., 2022c). In this review, we will briefly discuss the role of circRNAs in the development of ovarian cancer. Moreover, we will discuss the function and mechanisms of circRNAs on drug resistance in ovarian cancer. Furthermore, we will describe the strategies to overcome drug resistance via targeting circRNAs in ovarian cancer.
Mounting evidence has revealed that circRNAs critically regulate ovarian cancer development and progression (Yang et al., 2020; Foruzandeh et al., 2021). The circ-ITCH inhibited tumor progression via regulation of miR-145/RASA1 and miR-106a/CDH1 in ovarian cancer (Hu et al., 2018; Lin et al., 2020). CircRNA UBAP2 sponged miR-144, elevated the expression of CHD2, and facilitated tumor progression in ovarian cancer (Sheng et al., 2019). Xu et al. reported that circ-UBAP2 controlled the miR-382-5p/PRPF8 axis and enhanced cell proliferation and inhibited cell apoptosis in ovarian cancer (Xu et al., 2020a). CircPLEKHM3 regulated the expression of miR-9, BRCA1, KLF4, Akt1, DNAJB6 and performed a tumor suppressive function in ovarian cancer (Zhang et al., 2019a). CircWHSC1 sponged miR-145 and miR-1182 and upregulated the expression of MUC1 and hTERT, leading to promotion of tumor progression in ovarian cancer (Zong et al., 2019). CircPUM1 enhanced oncogenesis and progression via interaction with miR-615-5p and miR-6753-5p in ovarian cancer (Guan et al., 2019). Circ_100395 repressed tumor metastasis and proliferation via targeting miR-1228/p53/EMT (epithelial-mesenchymal transition) axis in ovarian cancer (Li et al., 2020a). CircMUC16 interacted with miR-199a and ATG13, and accelerated autophagy in epithelial ovarian cancer (Gan et al., 2020). Circ0004390 sponged miR-198 and elevated the expression of MET and facilitated cell proliferation in ovarian cancer (Xu et al., 2020b). Circ_102958 facilitated tumor progression via modulation of miR-1205 and SH2D3A expression in ovarian cancer (Wang et al., 2020a).
CircRNA FGFR3 triggered EMT by sponging miR-29a-3p and upregulating E2F1 expression in ovarian cancer (Zhou et al., 2020a). CircRNA-9119 regulated the miR-21-5p/PTEN/Akt pathway and attenuated cell viability in ovarian cancer (Gong et al., 2020). Circ_0072995 accelerated the tumor progression via regulating miR-147a and CDK6 expression in epithelial ovarian cancer (Ding et al., 2020). In addition, circKRT7/miR-29a-3p/COL1A1 axis was critically involved in promotion of ovarian cancer cell progression (An et al., 2020). Wang et al. found that circ-0001068 could be a biomarker for ovarian cancer and induce the expression of PD1 expression in T cells (Wang et al., 2020b). CircRNA PVT1 controlled cell invasion and proliferation through targeting FOXM1 expression by sponging miR-149-5p in ovarian cancer (Li et al., 2021). CircRAB11FIP1 induced autophagy flux via regulation of miR-129 and DSC1 in ovarian cancer (Zhang et al., 2021b). Circ-PTK2 (hsa_circ_0008305) targeted miR-639 and FOXC1 expressions and governed the pathogenic processes in ovarian cancer (Wu et al., 2021a).
Circ_0000554 was reported to increase cell invasion and proliferation via sponging miR-567 in ovarian cancer (Wang et al., 2022b). Both circATRNL1 and circZNF608 were found to suppress ovarian cancer progression via sequestering miR-152-5p and regulating encoding protein (Lyu et al., 2022). CircCERS6 was revealed to inhibit tumor development via modulation of miR-630 and RASSF8 in epithelial ovarian cancer (Li et al., 2022a). Wu et al. discovered that circFBXO7/miR-96-5p/MTSS1 axis played a pivotal role in regulation of the Wnt signaling pathway in ovarian cancer (Wu et al., 2022). Circ-BNC2 (hsa_circ_0008732) was uncovered to regulate the miR-223-3p and FBXW7 expressions and retard tumor progression in ovarian cancer (Liu et al., 2022d). Hsa_circ_0001445 was reported to act as a tumor suppressor via regulation of miR-576-5p/SFRP1 axis in ovarian cancer (Wu et al., 2023a). Circ_0015756 can influence the miR-145-5p/PSAT1 axis and lead to enhancement of ovarian cancer progression (Pan et al., 2022a). Extracellular vesicle-packaged circATP2B4 enhanced tumor metastasis via induction of M2 macrophage polarization through interaction with miR-532-3p and regulation of SREBF1 expression in epithelial ovarian cancer (Wang et al., 2023a). Similarly, exosome-transmitted circIFNGR2 influenced tumor metastasis via affecting the miR-378/ST5 axis in ovarian cancer (Chen et al., 2023a). Downregulation of circMFN2 reduced tumor progression and regulated glycolysis via affecting miR-198 and CUL4B pathway in ovarian cancer (Song et al., 2023). Hsa_circ_0001741 adsorbed the miR-188-5p and increased the expression of FOXN2, contributing to inhibition of cell proliferation in ovarian cancer (Wang et al., 2023b). Lastly, circ-PHC3 overexpression stimulated ovarian cancer progression by sponging the miR-497-5p and upregulating SOX9 pathway (Wang et al., 2023c). Altogether, circRNAs participate in ovarian cancer development and progression.
One study explored circRNA expression profiles in 54 ovarian cancer tissues and 54 normal controls, and identified them using circRNA-sequencing based profiles in 4 ovarian tumor specimens and 4 normal ovarian controls. 4388 circRNAs (2556 upregulated, 1832 downregulated) were differentially expressed in the ovarian cancer tissues vs. normal controls. The expression of six circRNAs, including circCELSR1, circEXOC6B, circBNC2, circRHOBTB3, circFAM13B and circN4BP2L2, was associated with clinicopathological characterizations of ovarian cancer. CircEXOC6B and circN4BP2L2 expression could be diagnostic and prognostic biomarkers for ovarian cancer patients (Ning et al., 2018). However, this study did not explore the association between circEXOC6B, circN4BP2L2 and drug resistance in ovarian cancer (Ning et al., 2018). Another study showed that knockdown of circCELSR1 reduced invasion, migration, proliferation and EMT and stimulated apoptosis via binding to miR-598 and upregulation of BRD4 in ovarian cancer cells. Inhibition of miR-598 or overexpression of BRD4 abrogated the function of circCELSR1 in ovarian cancer. Silencing of circCELSR1 decreased tumor metastasis and reduced tumor growth in nude mice (Zeng et al., 2020).
Zhang et al. reported that circCELSR1 (hsa_circ_0063809) conferred paclitaxel (PTX) resistance by influencing the expression of FOXR2 via targeting miR-1252 (Zhang et al., 2020a). Microarray analyses were performed to detect the expression of circCELSR1 in five PTX-sensitive ovarian tissues and five PTX-resistant ovarian cancer tissues. It was found that circCELSR1 was highly expressed in PTX-resistant ovarian cancer tissues. Moreover, qRT-PCR was performed to measure the expression of circCELSR1 in 36 ovarian cancer tissues and adjacent non-tumor tissues (Zhang et al., 2020a). Higher expression of circCELSR1 was displayed in ovarian cancer species. Cell counting kit-8 (CCK-8) data showed that silencing of circCELSR1 promoted PTX-mediated cytotoxicity in ovarian cancer cells. Moreover, suppression of circCELSR1 induced cell apoptosis and led to cell cycle arrest at G0/G1 phase in ovarian cancer cells (Zhang et al., 2020a). In vivo results revealed that inhibition of circCELSR1 suppressed tumor growth of ovarian cancer. Mechanistically, circCELSR1 was revealed to sponge miR-1252 and subsequently inhibit the expression of FOXR2 in ovarian cancer cells. Hence, circCELSR1 promoted PTX resistance via targeting miR-1252/FOXR2 axis in ovarian cancer (Zhang et al., 2020a).
Similarly, Wei et al. found that circCELSR1 expression was increased in PTX-resistant ovarian cancer cells and tumor specimens. Knockdown of circCELSR1 caused inhibition of cell viability, colony formation and promoted cell apoptosis and PTX sensitivity and reduced cell cycle progression in PTX-resistant ovarian cancer cells. Moreover, circCELSR1 sponged miR-149-5p and upregulated SIK2 (salt inducible kinase 2) expression. Suppression of miR-149-5p rescued the effects of circCELSR1 silencing on PTX resistance in PTX-resistant ovarian tumor cells. Meanwhile, upregulation of miR-149-5p blocked PTX resistance via targeting SIK2 in PTX-resistant ovarian cancer cells. In summary, circCELSR1 could target miR-149-5p/SIK2 axis and facilitated PTX resistance in ovarian cancer (Wei et al., 2021a).
ZEB1 (Zinc finger E-box-binding homeobox 1) has been known to trigger the EMT process in human cancer types (Wang et al., 2022c; Park et al., 2022; Perez-Oquendo and Gibbons, 2022). The transcription factor ZEB1 has been reported to be involved in EMT in ovarian cancer (Wei et al., 2021b). Zhang et al. found that circular RNA S-7 mediated EMT progression via sponging miR-641 and elevating ZEB1 and MDM2 in ovarian cancer (Zhang et al., 2020b). Cui et al. reported that ZEB1 promoted cisplatin resistance via inhibition of SLC3A2 expression in ovarian cancer (Cui et al., 2018). LncRNA NEAT1 conferred paclitaxel resistance via regulation of miR-194/ZEB1 axis in ovarian cancer (An et al., 2017). Similarly, inhibition of miR-429 led to drug resistance development via influencing ZEB1 expression in epithelial ovarian cancer (Zou et al., 2017). These findings suggested that ZEB1 was involved in drug resistance of ovarian cancer. One group showed that ZEB1 promoted the transcription of circANKRD17 and caused the progression of ovarian cancer (Cai and Zhang, 2022). Inhibition of ZEB1 reduced cell migration, invasion, EMT and proliferation in ovarian cancer. Silencing of ZEB1 downregulated the expression of circANKRD17, while overexpression of ZEB1 upregulated circANKRD17 expression level in ovarian cancer cells. ZEB1-mediated tumor promotion was due to upregulation of circANKRD17 in ovarian cancer (Cai and Zhang, 2022). Another group reported that circANKRD17 (circ_0007883) contributed to paclitaxel resistance via binding with FUS (fused in sarcoma) to make FOXR2 stability (Liang et al., 2023). The higher expression of circANKRD17 was seen in ovarian cancer tissues and ovarian tumor cell lines, which was associated with PTX sensitivity. In ovarian cancer cells, silencing of circANKRD17 induced apoptosis and decreased cell viability and increased PTX sensitivity. Moreover, circANKRD17 can bind with FUS, one RNA-binding protein, to stabilize FOXR2 (Liang et al., 2023). Therefore, circANKRD17 facilitated PTX resistance in ovarian cancer cells via interaction with FUS and maintenance of FOXR2 stability.
Several studies have revealed that circ_0061140 participated in the development and progression of various types of human cancers. For example, in endometrial carcinoma cells, circ_0061140 promoted tumor progression through impacting miR-149-5p/STAT3 (Liu et al., 2020a). In prostate cancer, circ_0061140 targeted miR-1193 and facilitated tumor malignant development (Wang et al., 2021a). In lung adenocarcinoma, circ_0061140 regulated miR-653 expression and elevated hexokinase 2 levels, leading to promotion of hypoxia-mediated migration, invasion and glycolysis (Wang et al., 2022d). In ovarian cancer, silencing of circ_0061140 abolished FOXM1-induced metastasis and cell proliferation via sponging miR-370 (Chen et al., 2018). One study showed that circ_0061140 conferred tumor malignant development via sponging miR-361-5p and upregulating the RAB1A expression in ovarian cancer cells (Zhang et al., 2022b). Another study reported that circ_0061140 affected miR-761/LETM1 (leucine zipper and EF-hand containing transmembrane protein 1) signaling and led to tumor progression in ovarian cancer (Ma et al., 2023). Moreover, circ_0061140 was found to be highly expressed in PTX-resistant ovarian cancer samples. Inhibition of circ_0061140 improved PTX sensitivity and induced apoptosis as well as suppressed invasion, proliferation and migration in ovarian cancer cells (Zhu et al., 2021). Downregulation of miR-136 restrained circ_0061140 knockdown-mediated PTX sensitivity and antitumor activity in ovarian cancer cells. Strikingly, downregulation of circ_0061140 retarded tumor growth and increased sensitivity to PTX treatment in mice. Furthermore, chromobox 2 (CBX2) was found to be a target of miR-136 in ovarian cancer. To summarize, circ_0061140 sponged miR-136 and elevated the expression of CBX2 in ovarian cancer, leading to PTX resistance and tumor malignant progression (Zhu et al., 2021).
Studies have shown the functions of circ_0025033 on colony formation, migration, invasion and glycolysis metabolism in ovarian cancer cells (Hou and Zhang, 2021). Ovarian cancer tissues and tumor cells have a higher expression of circ_0025033. Depletion of circ_0025033 reduced cell invasion, migration, glycolysis metabolism and colony formation in ovarian cancer cells. Mechanically, circ_0025033 influenced the expression of LSM4 via sponging miR-184 in ovarian cancer cells. Overexpression of LSM4 abolished the circ_0025033 knockdown-mediated inhibitory functions on cell invasion, colony formation, migration and glycolysis metabolism in ovarian cancer (Hou and Zhang, 2021). Another study showed that circ_0025033 was a key modulator in ovarian carcinogenesis. The expression of circ_0025033 was elevated in ovarian cancer tissues. Depletion of circ_0025033 led to suppression of proliferation, angiogenesis, and glutamine metabolism in ovarian cancer cells, and reduced tumor growth in mice. Notably, circ_0025033 promoted ovarian oncogenesis via sponging miR-370-3p and subsequent upregulation of SLC1A5. In parallel, miR-370-3p targeted the expression of SLC1A5 in ovarian cancer cells (Ma et al., 2022).
The involvement of circ_0025033 in regulating PTX resistance via targeting miR-532-3p and FOXM1 has been reported in ovarian cancer. In ovarian cancer tissues and tumor cells, there were high expression of circ_0025033 and FOXM1 and lower expression of miR-532-3p (Huang et al., 2022). After knockdown of circ_0025033 in PTX-resistant ovarian cancer cells, cell invasion and migration were inhibited, and apoptosis was induced. 3-(4, 5-Dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide (MTT) assay data showed that circ_0025033 downregulation induced PTX sensitivity in PTX-resistant ovarian cancer cells. Regarding mechanism, miR-532-3p and FOXM1 were involved in circ_0025033-induced PTX resistance in ovarian cancer (Huang et al., 2022).
CircATL2 (circRNA Atlastin GTPase 2) was found to be highly expressed in PTX-resistant ovarian cancer tissues and ovarian tumor cells. Silencing of circATL2 led to suppression of colony formation and induced cell apoptosis and cell cycle arrest in PTX-resistant ovarian cancer cells (Ying et al., 2022). Deletion of circATL2 attenuated the IC50 of PTX in ovarian cancer cells with PTX resistance. Moreover, in vivo data showed that knockdown of circATL2 restrained cell resistance to PTX in mice. Mechanistic study showed that circATL2 sponged miR-506-3p in PTX-resistant ovarian cancer cells (Ying et al., 2022). Consistently, knockdown of miR-506-3p abrogated the impacts of circATL2 silencing-mediated PTX sensitivity. Furthermore, NFIB acted as a downstream target of miR-506-3p. In addition, upregulation of miR-506-3p reduced cell resistance to PTX in ovarian cancer cells, which can be reversed by elevation of NFIB. In summary, circATL2 facilitated PTX resistance via affecting miR-506-3p/NFIB axis (Ying et al., 2022).
Guo et al. reported that downregulation of circ_0000714 governed RAB17 expression via sponging miR-370-3p and reduced PTX resistance in A2780 ovarian cancer cells. Moreover, RAB17 expression was upregulated in PTX-resistant A2780 ovarian cancer cells (Guo et al., 2020). Silencing of RAB17 enhanced PTX sensitivity, induced cell cycle arrest at G1 phase and attenuated cell proliferation in PTX-resistant A2780 cells. RAB17 activated the CDK6 and RB pathways and performed its biological behaviors. In addition, miR-370-3p was found to target RAB17 expression. Notably, circ_0000714 worked as a miR-370-3p sponge to regulate the expression of RAB17 in ovarian cancer cells. In conclusion, circ_0000714 targeted miR-370-3p/RAB17 axis and activated CDK6/RB signaling pathway, leading to reduction of paclitaxel resistance in ovarian cancer (Guo et al., 2020).
CircRNA SET domain bifurcated histone lysine methyltransferase 1 (circSETDB1) has been reported to regulate ovarian tumorigenesis. The expression level of circSETDB1 was increased in serous ovarian cancer tissues compared with normal fallopian tube tissues. CircSETDB1 expression was elevated in ovarian cancer cells in comparison with normal ovarian epithelial cells (Li and Zhang, 2021). Inhibition of circSETDB1 increased cell apoptosis and reduced cell migration, invasion and growth in serous ovarian cancer. Knockdown of circSETDB1 impaired tumor growth in mice. CircSETDB1 knockdown-induced malignant progression was blocked by inhibition of miR-129-3p. MAP3K3 (mitogen-activated protein kinase kinase kinase 3) was a target of miR-129-3p in serous ovarian cancer cells (Li and Zhang, 2021). Similarly, another group identified the higher expression of circSETDB1 in PTX-resistant ovarian cancer (Huang et al., 2023). Silencing of circSETDB1 exhibited anticancer activity via inhibition of proliferation and cell cycle process and induction of cell apoptosis in PTX-resistant ovarian cancer cells. Moreover, circSETDB1 targeted miR-508-3p and increased the expression of ABCC1 (ATP-binding cassette subfamily C member 1) in ovarian cancer cells. Blockade of miR-508-3p or upregulation of ABCC1 impaired the effects of circSETDB1 depletion on cell resistance to PTX in ovarian cancer. Mouse study also validated that circSETDB1 downregulation promoted cell sensitivity to PTX. In conclusion, circSETDB1 enhanced PTX resistance via inhibition of miR-508-3p and upregulation of ABCC1 expression (Huang et al., 2023).
Wang et al. discovered that serum circSETDB1 could be a potential biomarker for prediction of chemotherapy response and relapse in ovarian cancer. This group measured serum circSETDB1 levels in 18 chemo-resistant patients (platinum-taxane-combined chemotherapy), 42 chemo-sensitive patients and 60 healthy volunteers. In comparison with healthy controls, serum circSETDB1 expression was elevated in serous ovarian cancer patients (Wang t al., 2019a). CircSETDB1 expression level can distinguish ovarian cancer patients from healthy people. Lymph node metastasis, advanced FIGO (international federation of gynecology and obstetrics) stage and survival were correlated with high expression of circSETDB1 in ovarian cancer patients. Ovarian cancer patients with chemoresistance had a higher expression levels of serum circSETDB1, which can distinguish ovarian cancer patients with chemoresistance from those with chemosensitivity (Wang et al., 2019a).
Hsa_circ_0000231 has been revealed to participate in the progression of colorectal cancer cells. The expression of circ_0000231 was elevated in colorectal cancer specimens. Depletion of circ_0000231 alleviated the glycolysis, suppressed invasion, migration and growth via sponging miR-502-5p and upregulating MYO6 in colorectal cancer cells (Liu et al., 2020b). Moreover, a study indicated that sevoflurane, a volatile anesthetic, reduced the process of colorectal cancer via inhibition of circ_0000231 expression and upregulation of miR-622 expression in colorectal cancer cells. Colorectal cancer tissues had an upregulation of circ_0000231 and a downregulation of miR-622. In addition, circ_0000231 can sponge miR-622 and reduce its expression level. Sevoflurane inhibited cell migration, invasion and proliferation and induced apoptosis in colorectal cancer (Wang et al., 2021b). Liu et al. reported that circ_0000231 induced paclitaxel resistance via regulation of miR-140 and RAP1B in ovarian cancer. PTX-resistant ovarian cancer tissues and cells had an upregulation of circ_0000231 and RAP1B and a downregulation of miR-140 level. Silencing of circ_0000231 led to suppression of migration, proliferation, invasion, EMT, and PTX resistance, and induction of apoptosis in PTX-resistant ovarian cancer cells (Liu et al., 2023a). Upregulation of circ_0000231 displayed an opposite effect in PTX-resistant ovarian cancer cells. In vivo data also showed that circ_0000231 downregulation enhanced ovarian cancer cell sensitivity to PTX treatment. Further, miR-140 can be sponged by circ_0000231, and target RAP1B in ovarian cancer. Hence, circ_0000231 is vitally involved in chemoresistance of ovarian cancer (Liu et al., 2023a).
It has been reported that circTNPO3 regulates tumorigenesis in various cancer types. CircTNPO3 inhibited tumor metastasis via decoying IGF2BP3 protein and regulating the expression of Snail and Myc in gastric cancer (Yu et al., 2021). CircTNPO3 suppressed tumor metastasis via interaction with IGF2BP3 and destabilization of SERPINH1 mRNA in clear cell renal cell carcinoma (Pan et al., 2022b). CircTNPO3 enhanced tumor progression via upregulation of STRN expression by decoying miR-199b-5p in hepatocellular carcinoma (Liu and Liu, 2023). CircTNPO3 expression was increased in ovarian cancer tissues and associated with PTX resistance. Downregulation of circTNPO3 increased PTX sensitivity by induction of PTX-mediated apoptosis. CircTNPO3 could decoy miR-1299 and upregulate NEK2 (NIMA-related kinase 2) in ovarian cancer. Hence, circTNPO3 promoted PTX resistance in ovarian cancer (Xia et al., 2020).
CircNRIP1 was reported to work as a miR-149-5p sponge to target the Akt and mTOR pathways, leading to promoting gastric cancer progression (Zhang et al., 2019b). CircNRIP1 affected the miR-186-5p and MYH9 expressions and enhanced tumor progression and tumor glycolysis in gastric cancer (Liu et al., 2020c). CircNRIP1 sponged miR-629-3p and influenced the PTP4A1 and ERK1/2 pathways, resulting in promotion of cell invasion and migration in cervical cancer (Li et al., 2020b). Inhibition of circNRIP1 reduced the paclitaxel resistance via targeting the miR-211-5p and HOXC8 (homeobox C8) in ovarian cancer (Li et al., 2020c).
CircEXOC6B was observed to repress tumor metastasis via promotion of interaction with RBMS1 (RNA binding motif single strand interacting protein 1) and HuR (human antigen R) in prostate cancer (Zhang et al., 2023b). CircEXOC6B repressed invasion and migration of prostate cancer cells in vitro and in vivo. CircEXOC6B can bind with RBMS1 and HuR and elevate AKAP12 (A-kinase anchoring protein 12) expression levels, leading to inhibition of tumor metastasis in prostate cancer (Zhang et al., 2023b). In colorectal cancer, circEXOC6B can bind to an mTORC1 activator, RRAGB, reduced tumor progression via antagonization of HIF1A/RRAGB/mTORC1 loop. CircEXOC6B promoted the 5-fluorouracil sensitivity of colorectal cancer cells (Li et al., 2022b). CircEXOC6B decreased tumor progression via sponging miR-421 and inhibiting RUS1 expression in ovarian cancer (Wang et al., 2020c). Inhibition of circEXOC6B facilitated cell invasion and proliferation in ovarian cancer A2780 cells. Overexpression of circEXOC6B displayed an opposite function in ovarian cancer SKOV3 cells via induction of apoptosis and reduction of proliferation and invasion. Further, miR-421 was sponged by circEXOC6B, and RUS1 was a target of miR-421 in ovarian cancer cells (Wang et al., 2020c). The low expression of circEXOC6B was correlated with LNM and younger age in ovarian cancer patients. The high level of circEXOC6B was linked to a better overall survival in ovarian cancer patients (Ning et al., 2018). Zheng et al. reported that circEXOC6B expression levels were downregulated in ovarian cancer specimens, which were correlated with malignant clinical features in ovarian cancer patients. CircEXOC6B reduced PTX resistance and motility and growth in ovarian cancer via targeting miR-376c-3p. FOXO3 (forkhead box O3) was a potential target of miR-376c-3p in ovarian cancer cells. Hence, CircEXOC6B accelerated cell sensitivity to PTX via decoying miR-376c-3p and upregulating FOXO3 in ovarian cancer (Zheng et al., 2022). CircSLC39A8 reduced paclitaxel resistance via modulation of BMF expression by interacting with miR-185-5p in ovarian cancer (Liu et al., 2023b).
CircLPAR3 was highly expressed in esophageal cancer (ESCC) tissues and cells (Shi et al., 2020; Cheng et al., 2022). ESCC patients with high expression of circLPAR3 had advanced clinical stage and lymph node metastasis. Moreover, circLPAR3 sponged miR-198 and upregulated the expression of MET gene, leading to activation of RAS/MAPK and PI3K/AKT signaling pathways. Furthermore, circLPAR3 enhanced invasion, metastasis and migration in ESCC cells and in mice (Shi et al., 2020). Similarly, another group reported that circLPAR3 downregulation inhibited Warburg effect, metastasis and proliferation and increased cell apoptosis in ESCC cells. Downregulation of circLPAR3 impaired xenograft tumor growth in mice and impeded Warburg effect. CircLPAR3 elevated the expression of LDHA via sponging miR-873-5p in ESCC cells (Cheng et al., 2022). Two studies showed that circLPAR3 expression was higher in oral squamous cell carcinoma (OSCC) samples and cells. Knockdown of circLPAR3 caused suppression of proliferation, stemness and metastasis, and induction of cell apoptosis (Fu et al., 2022a; Su et al., 2022). Mechanistically, circLPAR3 absorbed miR-643 to upregulate the expression of HMGB2. Downregulation of circLPAR3 retarded OSCC oncogenesis in mice (Fu et al., 2022a). Su et al. found that depletion of circLPAR3 reduced glycolysis and repressed tumor progression via suppression of miR-144-3p and promotion of LPCAT1 in OSCC. OSCC patients with higher expression of circLPAR3 displayed a shorter survival (Su et al., 2022).
Chen et al. found that circLPAR3 upregulated the expression of JPT1 via sponging miR-513b-5p, which enhanced glycolytic activation and inhibited radiosensitivity in prostate cancer (Chen et al., 2023b). Liu et al. reported that circLPAR3 increased the cisplatin resistance in ovarian cancer. The expression of circLPAR3 was elevated in cisplatin-resistant ovarian cancer tissues and cells. Downregulation of circLPAR3 led to promotion of cisplatin sensitivity in ovarian cancer cells. Moreover, circLPAR3 interacted with miR-634 and sponged its expression. PDK1 was found to be a target of miR-634 in ovarian cancer. Overexpression of PDK1 inverted the function of miR-634 on cisplatin sensitivity of ovarian cancer. Inhibition of miR-634 rescued circLPAR3 downregulation-mediated cisplatin sensitivity in ovarian cancer. Thereafter, circLPAR3 facilitated cisplatin resistance of ovarian cancer cells (Liu et al., 2022e).
Accumulating evidence has suggested that circITGB6 was involved in cisplatin sensitivity in ovarian cancer. Using circRNA deep sequencing, one group found that circITGB6 expression was upregulated in tumor specimens and serums from ovarian cancer patients, who had cisplatin resistance. The expression of circITGB6 was associated with worse prognosis in ovarian cancer patients (Li et al., 2022c). Upregulation of circITGB6 increased an M2 macrophage-mediated cisplatin resistance in vitro and in vivo. Mechanistically, circITGB6 was found to bind with IGF2BP2 and FGF9 mRNA to build a ternary complex, including circITGB6, IGF2BP2, and FGF9, in the cytoplasm, contributing to stabilization of FGF9 mRNA and induction of polarization of TAMs to M2 phenotype. Consistently, an antisense oligonucleotide to inhibit circITGB6 expression abrogated the circITGB6-participated cisplatin resistance in ovarian cancer. To sum up, circITGB6 accelerated cisplatin resistance of ovarian cancer cells (Li et al., 2022c).
The expression of circPBX3 was reported to be increased in ovarian tumor samples and cisplatin-resistant ovarian cancer cells. Increased circPBX3 induced apoptosis and promoted colony formation and elevated cisplatin resistance in ovarian cancer cells. Upregulation of circPBX3 increased tumor xenografts growth in mice. Downregulation of circPBX3 inhibited apoptosis and reduced colony formation and cisplatin resistance in ovarian cancer cells. Notably, circPBX3 can bind with IGF2BP2 and elevate the stability of ATP7A at mRNA levels, thereby contributing to upregulation of ATP7A protein in ovarian cancer. The function of circPBX3 upregulation on cisplatin resistance was abolished by downregulation of ATP7A in ovarian cancer cells. In conclude, circPBX3 accelerated cisplatin resistance in ovarian cancer (Fu et al., 2022b).
It has been reported that circSnx12 regulated ferroptosis via sponging miR-224-5p during heart failure (Zheng et al., 2021). Higher expression of circSnx12 was reported in ovarian cancer cells and tumor tissues with cisplatin resistance. Inhibition of circSnx12 caused cell sensitive to cisplatin treatment in cisplatin-resistant ovarian cancer cells via activation of ferroptosis. This phenotype was impaired by suppression of miR-194-5p in cisplatin-resistant ovarian cancer cells. Mechanistical experiments showed that circSnx12 sponged miR-194-5p and subsequently upregulated SLC7A11 in ovarian cancer cells. In conclusion, circSnx12 repressed ferroptosis via targeting miR-194-5p/SLC7A11 axis and conferred cisplatin resistance (Qin et al., 2023b).
It has been reported that exosomal circ_PIP5K1A (phosphatidylinositol-4-phosphate 5-kinase type 1 alpha) was highly expressed in NSCLC tumor samples, serum samples and tumor cells (Shao et al., 2021). Moreover, suppression of exosomal circ_PIP5K1A reduced proliferation, invasiveness and migrative abilities in NSCLC cells. Inhibition of circ_PIP5K1A induced apoptosis and cisplatin sensitivity and inhibited tumor growth in mice. Furthermore, circ_PIP5K1A sponged the miR-101 and upregulated the expression of ABCC1 in NSCLC cells (Shao et al., 2021). Suppression of miR-101 reversed the functions of circ_PIP5K1A knockdown on reduction of tumor progression and induction of cisplatin sensitivity. In addition, circ_PIP5K1A promoted NSCLC progression and cisplatin resistance via sponging miR-101 and targeting ABCC1 (Shao et al., 2021). Similarly, another group reported that circ_PIP5K1A increased cisplatin resistance and tumor progression via regulation of miR-493-5p/ROCK1 axis in NSCLC (Feng et al., 2021). DDP-resistant cells and tumor tissues displayed the higher expression of circ_PIP5K1A in NSCLC. Depletion of circ_PIP5K1A decreased cisplatin resistance and cell motility as well as proliferation in DDP-resistant NSCLC cells (Feng et al., 2021). Silencing of circ_PIP5K1A overcame cisplatin resistance via sponging miR-942-5p and targeting NFIB expression in ovarian cancer. The expression of circ_PIP5K1A was elevated in DDP-resistant ovarian cancer cells and tissues. Silencing of circ_PIP5K1A constrained cell invasion, migration and cell growth and increased cisplatin sensitivity in DDP-resistant ovarian cancer cells (Sheng and Wang, 2023). Hence, circ-PIP5K1A promotes cell resistance to cisplatin in ovarian cancer.
Several studies have revealed the role of circ_0026123 in ovarian cancer progression and drug resistance. For example, one study showed that circ_0026123 expression was upregulated in ovarian cancer cell lines and tissues. Silencing of circ_0026123 reduced migration and proliferation of ovarian cancer cells. Moreover, downregulation of circ_0026123 reduced the expression of CSC markers. Mechanistically, circ_0026123 sponged miR-124-3p and upregulated the expression of EZH2 (enhancer of zeste homolog 2) (Yang et al., 2021). The other study showed that circ_0026123 increased cisplatin resistance and tumor progression of ovarian cancer. The expression of circ_0026123 was increased in DDP-resistant ovarian cancer tissues and cancer cells. Downregulation of circ_0026123 increased cisplatin sensitivity in DDP-resistant ovarian cancer cells. Moreover, downregulation of circ_0026123 suppressed cell migration, angiogenesis, invasion and proliferation in DDP-resistant ovarian cancer cells. Further, circ_0026123 sequestered miR-543 and upregulated RAB1A in ovarian cancer cells. Overexpression of RAB1A or knockdown of miR-543 reversed the functions of circ_0026123 knockdown on cisplatin sensitivity and tumor behaviors in DDP-resistant ovarian cancer cells (Wei et al., 2022). Therefore, circ_0026123 elevated the expression of RAB1A via sponging miR-543, leading to promotion of oncogenesis and cisplatin resistance in ovarian cancer.
It has been reported that circ_0063804 was involved in cisplatin resistance in ovarian cancer cells. In 108 ovarian cancer patients, circ_0063804 expression was elevated, which was associated with poor prognosis (You et al., 2022). Moreover, circ_0063804 promoted cell proliferation, inhibited cell apoptosis and increased cisplatin resistance in ovarian cancer cells. Notably, circ_0063804 can sponge miR-1276 and the expression of miR-1276 was reduced in ovarian cancer patients. CLU was found to be a target of miR-1276 and was increased in ovarian cancer patients (You et al., 2022). Strikingly, circ_0063804 exacerbated cisplatin resistance and enhanced tumor malignant behaviors via promotion of CLU expression by sponging miR-1276. Furthermore, depletion of circ_0063804 retarded tumor growth, reduced cisplatin resistance in mice (You et al., 2022). In conclusion, circ_0063804 enhances cisplatin resistance in ovarian cancer via targeting miR-1276/CLU axis.
Several reports showed that circ_0007841 plays a key role in tumorigenesis, including multiple myeloma, NSCLC and ovarian cancer (Wang et al., 2020d; Huang et al., 2021; Long et al., 2022; Guo et al., 2023). Long et al. reported that circ_0007841 took part in tumor progression via regulation of miR-199a-5p/SphK2 axis (Long et al., 2022). Gao et al. found circ_0007841 as a new potential biomarker and drug resistance in multiple myeloma (Gao et al., 2019b). Song et al. reported that circ_0007841 promoted chemotherapy resistance via upregulation of ABCG2 in multiple myeloma (Song et al., 2020). Moreover, one group reported that circ_0007841 promoted tumor malignant progression via targeting miR-338-3p and BRD4 in multiple myeloma (Wang et al., 2020e). Another group found that downregulation of circ_0007841 reduced the development of multiple myeloma and BTZ resistance via inhibition of miR-129-5p and upregulation of JAG1 (Wang et al., 2020d). Huang et al. reported that circ_0007841 accelerated tumorigenesis via facilitating the expression of MEX3C by inhibition of miR-151-3p activity in ovarian cancer cells (Huang et al., 2021). Upregulation of circ_0007841 was observed in ovarian cancer patients, which was associated with poor prognosis. Downregulation of circ_0007841 repressed invasion, migration and cell growth in ovarian cancer. Moreover, circ_0007841 elevated the expression of MEX3C by sponging miR-151-3p (Huang et al., 2021). Downregulation of circ_0007841 led to promotion of cisplatin sensitivity via inhibition of NFIB expression by sponging miR-532-5p in ovarian cancer (Gao and Huang, 2023).
Numerous studies have shown that circ_0067934 acts as a cancer driver in various types of human cancers (Zhou et al., 2020b; Al-Hawary et al., 2023; Yu et al., 2023). For example, circ_0067934 expression was increased in ESCC (esophageal squamous cell carcinoma) and enhanced cell proliferation (Xia et al., 2016). Circ_0067934 regulated the miR-1324/FZD5/Wnt/β-catenin pathway in hepatocellular carcinoma, which facilitated tumor metastasis and tumor growth (Zhu et al., 2018). Inhibition of circ_0067934 reduced cell invasion, proliferation and migration via regulation of miR-1182 and KLF8 and upregulation of Wnt/β-catenin in NSCLC cells. Circ_0067934 expression was associated with unfavorable prognosis in patients with NSCLC (Wang and Li, 2018; Zou et al., 2018; Zhao et al., 2020). Upregulation of circ_0067934 enhanced cervical cancer progression through targeting miR-545 and EIF3C (Hu et al., 2019). Similarly, overexpression of circ_0067934 facilitated tumor progression via regulation of CXCR1 expression by sponging miR-1304 and associated with poor prognosis in thyroid carcinoma (Wang et al., 2019b; Zhang et al., 2019c). Circ_0067934 reduced tumor cell ferroptosis via modulating miR-545-3p/SLC7A11 pathway and promoted tumor progression via miR-1301-3p/HMGB1 in thyroid cancer (Wang et al., 2021c; Dong et al., 2022). In glioblastoma, overexpression of circ_0067934 conferred tumor progression via activation of PI3K/AKT pathway (Xin et al., 2019). In gastric cancer, downregulation of circ_0067934 contributed to tumor progression via interacting with miR-4705 and regulating BMPR1B expression as well as targeting miR-1301-3p/KIF23 axis (He et al., 2019; Xu et al., 2022). In bladder cancer, circ_0067934 elevated cell invasion, proliferation and migration via inhibition of miR-1304 expression and upregulation of Myc expression (Liu et al., 2020d). In laryngeal squamous, circ_0067934 accelerated tumor progression via interacting with miR-1324 and associated with poor prognosis (Chu, 2020). In breast cancer, circ_0067934 increased the expression of Mcl-1 and performed an oncogenic role in breast tumorigenesis (Wang et al., 2019c). Circ_0067934 was linked to lymph node metastasis and advanced tumor stage. Circ_0067934 facilitated cisplatin resistance via reduction of JNK phosphorylation by targeting miR-545-3p/PPA1 axis in ovarian cancer (Yin et al., 2022).
Circ_0010467 increased cisplatin resistance via regulation of miR-637, LIF (leukemia inhibitory factor) and STAT3 pathways in ovarian cancer cells, which was induced by AUF1 (Wu et al., 2023b). Circ_0010467 was highly expressed in cisplatin-resistant ovarian cancer cells and tumor tissues as well as serum exosomes, which was linked to poor prognosis of patients with ovarian cancer. Inhibition of circ_0010467 increased cisplatin sensitivity by inhibition of cell proliferation in ovarian cancer (Wu et al., 2023b). Several studies have showed that circFoxp1 promoted tumor progression in gallbladder cancer (Wang et al., 2019d), hepatocellular carcinoma (Wang et al., 2020f), lung cancer (Li et al., 2020d), colon cancer (Luo et al., 2020), renal cell carcinoma (Fang et al., 2021), and osteosarcoma (Zhang et al., 2021c). CircFoxp1 overexpression contributed to cisplatin resistance and cell proliferation in epithelial ovarian cancer. Knockdown of circFoxp1 led to cisplatin sensitivity in ovarian cancer cells and in mice (Luo and Gui, 2020). Exosomal circFoxp1 expression was upregulated in DDP-resistant ovarian cancer patients, which was correlated with IFGO (International Federation of Gynecology and Obstetrics) stage, tumor metastasis and tumor size as well as survival. CircFoxp1 regulated cisplatin resistance in part due to regulation of miR-150-3p and miR-22 in ovarian cancer cells. Moreover, circFoxp1 could regulate the expression of FMNL3 (formin like 3) and CEBPG (CCAAT enhancer binding protein gamma) in ovarian cancer (Luo and Gui, 2020). Hsa_circ_0000585 was reported to increase cisplatin resistance via regulating autophagy in epithelial ovarian cancer (Du et al., 2023).
Circ_0078607 has been reported to control tumorigenesis and regulate proliferation and migration in human cancers. Downregulation of circ_0078607 blocked the gastric cancer development and induced the inactivation of the ERK1/2 and Akt pathways via targeting the miR-188-3p and RAP1B (Bian et al., 2021). Circ_0078607 has been found to repress tumor progression via modulating the miR-518a-5p and Fas signaling pathway in ovarian cancer (Zhang et al., 2020c). Moreover, circ_0078607 expression was lower in high-grade serous ovarian cancer and associated with poor prognosis (Zhang et al., 2021d). Furthermore, circ_0078607 was reported to inhibit tumor progression via governing the miR-32-5p and SIK1 pathways in ovarian cancer (Jin and Wang, 2022). Circ_0078607 enhanced cisplatin sensitivity in ovarian cancer cells by regulation of miR-196b-5p and GAS7 (growth arrest-specific 7) expressions (Dai et al., 2023). Circ_0078607 expression was lower in DDP-resistant ovarian cancer cells. Upregulation of circ_0078607 suppressed cisplatin resistance, enhanced apoptosis and repressed cell proliferation in DDP-resistant cells. In term of mechanism, circ_0078607 sequestered miR-196b-5p and elevated the expression of GAS7 (Dai et al., 2023). Therefore, circ_0078607 attenuated cisplatin resistance in ovarian cancer. CircRNA Cdr1as has been reported to inhibit ovarian cancer progression via sponging miR-135b-5p (Chen et al., 2019). CircRNA Cdr1as suppressed cisplatin resistance via sponging miR-1270 and upregulating SCA1 in ovarian cancer (Zhao et al., 2019). Moreover, circRNA Cdr1as inhibited miR-1299 expression and reduced cisplatin-based chemoresistance in ovarian cancer (Wu et al., 2021b).
Hsa_circ_0006404 and hsa_circ_0000735 have been found to regulate docetaxel (DTX) resistance in ovarian cancer. Hsa_circ_0006404 was remarkably inhibited in DTX-treated ovarian cancer SKOC3-R cells. Circ_0006404 was observed to sponge the miR-346 in ovarian cancer cells. Moreover, miR-346 was observed to inhibit the expression of DKK3 and regulate the p-GP expression in ovarian cancer cells (Chen and Tai, 2022). In addition, Circ_0000735 was found to be increased in DTX-treated ovarian cancer cells. Circ_0000735 can inhibit the expression of miR-526b and elevate the expression of DKK4, leading to regulation of the p-GP expression in ovarian cancer (Chen and Tai, 2022). Hence, overexpression of circRNA_0006404 and inhibition of circRNA_0000735 might be a potential strategy to suppress the expression of p-GP, contributing to better benefit of docetaxel treatment in ovarian cancer.
One study showed that circNRIP1 (circRNA nuclear receptor-interacting protein 1) maintained hypoxia-mediated 5-fluorouracil resistance via sponging miR-138-5p and regulating HIF-1alpha-dependent glucose metabolism in gastric cancer (Xu et al., 2020c). Another study revealed that circNRIP1 governed the miR-515-5p/IL-25 axis to regulate cisplatin and 5-fluorouracil resistance in nasopharyngeal carcinoma (Lin et al., 2021). Downregulation of circNRIP1 sensitized cells to 5-fluorouracil treatment via affecting miR-532-3p in colorectal cancer (Liu et al., 2021b). It is unclear whether circNRIP1 regulates the 5-fluorouracil resistance in ovarian cancer.
In conclusion, circRNAs play an important role in regulation of paclitaxel resistance (Table 1; Figure 1), cisplatin resistance (Table 2; Figure 2), docetaxel and 5-fluorouracil resistance (Table 3) mainly via sponging miRNAs in ovarian cancer. It is pivotal to mention that there is an interaction between circRNAs and drug resistance in ovarian cancer. Some circRNAs regulate drug resistance in ovarian cancer, while drug resistance changes the expression of certain circRNAs (Qin et al., 2023a). Moreover, circRNAs could be potential biomarkers for prediction of drug resistance in ovarian cancer. Because of critical role of circRNAs in governing drug sensitivity, targeting these circRNAs could be useful for overcoming drug resistance in ovarian cancer.
To fully understand the mechanism of drug resistance in ovarian cancer, several issues should be mentioned. A majority of circRNAs promote drug resistance in ovarian cancer, including cisplatin, paclitaxel and docetaxel (Figure 3). A few circRNAs increase drug sensitivity in ovarian cancer. Besides circRNAs, miRNAs and lncRNAs are critically involved in modulation of drug resistance in ovarian cancer. Three chemotherapeutic drugs, cisplatin, docetaxel and paclitaxel, were reported to be regulated by circRNAs in ovarian cancer. It is interesting to explore whether resistance to other chemotherapeutic agents, such as gemcitabine, oxaliplatin, carboplatin, is regulated by circRNAs in ovarian cancer. It is important to note that besides noncoding RNAs, protein post-translational modifications regulate drug resistance in human cancers, including ovarian cancer. The E3 ubiquitin ligases regulated tumor progression and immunotherapy resistance in human cancer (Hou et al., 2023). Hence, targeting the E3 ubiquitin ligases might be helpful for overcoming drug resistance in ovarian cancer.
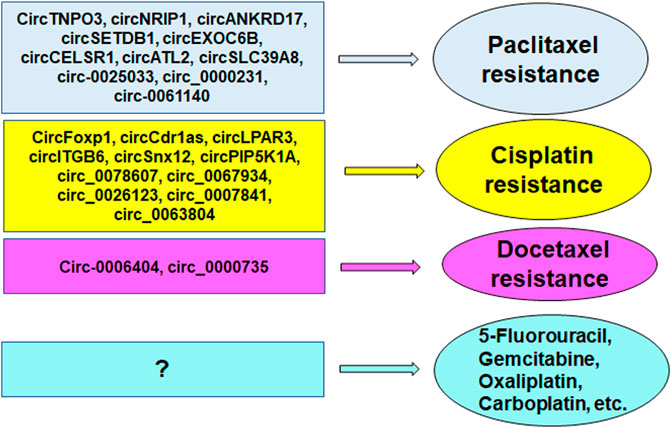
FIGURE 3. CircRNAs regulate drug resistance in ovarian cancer, including cisplatin, paclitaxel and docetaxel.
Several compounds have shown to regulate the expression of circRNAs in human cancers. Curcumin, an active component of turmeric, increased the expression of circ-PLEKHM3 in ovarian cancer, and targeted miR-320a/SMG1 axis (Sun and Fang, 2021). Moreover, curcumin has been reported to be a therapeutic agent in cancer therapy via affecting circRNAs (Si et al., 2023). It is necessary to determine whether curcumin could enhance drug sensitivity via targeting circRNAs in ovarian cancer. In addition, it is unclear whether there is the feedback regulation between circRNAs and drug resistance in ovarian cancer. It is elusive whether circRNAs interact with other factors involved in drug sensitivity to modify chemoresistance. Cancer stem cells play an essential role in inducing drug resistance. It is required to determine whether circRNAs control drug resistance via targeting ovarian cancer stem cells. Importantly, the application of circRNAs for prediction and treatment in clinic remain inadequate and challenging. In summary, in-depth exploration into the mechanisms of drug resistance in ovarian cancer is essential to development novel drugs and treatment strategies by targeting ncRNAs that can overcome drug resistance.
JZ: Data curation, Formal Analysis, Investigation, Methodology, Resources, Writing–original draft. ZL: Data curation, Formal Analysis, Investigation, Methodology, Software, Writing–original draft. CL: Formal Analysis, Investigation, Project administration, Resources, Writing–original draft. DW: Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Writing–original draft. LY: Data curation, Investigation, Methodology, Software, Writing–original draft. XX: Conceptualization, Funding acquisition, Investigation, Project administration, Supervision, Validation, Visualization, Writing–review and editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by China’s national key research and development program (Grant Number: 2022YFC3600304).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Al-Hawary, S. I. S., Asghar, W., Amin, A., Mustafa, Y. F., Hjazi, A., Almulla, A. F., et al. (2023). Circ_0067934 as a novel therapeutic target in cancer: from mechanistic to clinical perspectives. Pathol. Res. Pract. 245, 154469. doi:10.1016/j.prp.2023.154469
Ali, A. T., Al-Ani, O., and Al-Ani, F. (2023). Epidemiology and risk factors for ovarian cancer. Prz. Menopauzalny 22 (2), 93–104. doi:10.5114/pm.2023.128661
An, J., Lv, W., and Zhang, Y. (2017). LncRNA NEAT1 contributes to paclitaxel resistance of ovarian cancer cells by regulating ZEB1 expression via miR-194. Onco Targets Ther. 10, 5377–5390. doi:10.2147/OTT.S147586
An, Q., Liu, T., Wang, M. Y., Yang, Y. J., Zhang, Z. D., Lin, Z. J., et al. (2020). circKRT7-miR-29a-3p-COL1A1 Axis promotes ovarian cancer cell progression. Onco Targets Ther. 13, 8963–8976. doi:10.2147/OTT.S259033
Anastasiadou, E., Jacob, L. S., and Slack, F. J. (2018). Non-coding RNA networks in cancer. Nat. Rev. Cancer 18 (1), 5–18. doi:10.1038/nrc.2017.99
Arnaoutoglou, C., Dampala, K., Anthoulakis, C., Papanikolaou, E. G., Tentas, I., Dragoutsos, G., et al. (2023). Epithelial ovarian cancer: a five year review. Med. Kaunas. 59 (7), 1183. doi:10.3390/medicina59071183
Bian, W., Liu, Z., Chu, Y., and Xing, X. (2021). Silencing of circ_0078607 prevents development of gastric cancer and inactivates the ERK1/2/AKT pathway through the miR-188-3p/RAP1B axis. Anticancer Drugs 32 (9), 909–918. doi:10.1097/CAD.0000000000001083
Bou Antoun, N., and Chioni, A. M. (2023). Dysregulated signalling pathways driving anticancer drug resistance. Int. J. Mol. Sci. 24 (15), 12222. doi:10.3390/ijms241512222
Cai, W., and Zhang, Q. (2022). The transcription factor ZEB1 mediates the progression of epithelial ovarian cancer by promoting the transcription of CircANKRD17. J. Biochem. Mol. Toxicol. 36 (8), e23086. doi:10.1002/jbt.23086
Carter, B., and Zhao, K. (2021). The epigenetic basis of cellular heterogeneity. Nat. Rev. Genet. 22 (4), 235–250. doi:10.1038/s41576-020-00300-0
Chen, H., Mao, M., Jiang, J., Zhu, D., and Li, P. (2019). Circular RNA CDR1as acts as a sponge of miR-135b-5p to suppress ovarian cancer progression. Onco Targets Ther. 12, 3869–3879. doi:10.2147/OTT.S207938
Chen, L. L. (2020). The expanding regulatory mechanisms and cellular functions of circular RNAs. Nat. Rev. Mol. Cell Biol. 21 (8), 475–490. doi:10.1038/s41580-020-0243-y
Chen, Q., Zhang, J., He, Y., and Wang, Y. (2018). hsa_circ_0061140 knockdown reverses FOXM1-mediated cell growth and metastasis in ovarian cancer through miR-370 sponge activity. Mol. Ther. Nucleic Acids 13, 55–63. doi:10.1016/j.omtn.2018.08.010
Chen, X., Ren, X., Zhou, Y., and Bian, R. (2023a). Exosome-transmitted circIFNGR2 modulates ovarian cancer metastasis via miR-378/ST5 Axis. Mol. Cell Biol. 43 (1), 22–42. doi:10.1080/10985549.2022.2160605
Chen, Y. Y., Luo, L. P., and Deng, K. C. (2023b). Circular RNA LPAR3 targets JPT1 via microRNA-513b-5p to facilitate glycolytic activation but repress prostate cancer radiosensitivity. Acta Biochim. Pol. 70 (1), 153–162. doi:10.18388/abp.2020_6379
Chen, Y. Y., and Tai, Y. C. (2022). Hsa_circ_0006404 and hsa_circ_0000735 regulated ovarian cancer response to docetaxel treatment via regulating p-GP expression. Biochem. Genet. 60 (1), 395–414. doi:10.1007/s10528-021-10080-9
Cheng, Y., Ma, Z., Liu, S., Yang, X., and Li, S. (2022). CircLPAR3 knockdown suppresses esophageal squamous cell carcinoma cell oncogenic phenotypes and Warburg effect through miR-873-5p/LDHA axis. Hum. Exp. Toxicol. 41, 9603271221143695, 9603271221143695. doi:10.1177/09603271221143695
Chu, Y. L. (2020). Circ_0067934 correlates with poor prognosis and promotes laryngeal squamous cell cancer progression by sponging miR-1324. Eur. Rev. Med. Pharmacol. Sci. 24 (8), 4320–4327. doi:10.26355/eurrev_202004_21013
Cui, Y., Qin, L., Tian, D., Wang, T., Fan, L., Zhang, P., et al. (2018). ZEB1 promotes chemoresistance to cisplatin in ovarian cancer cells by suppressing SLC3A2. Chemotherapy 63 (5), 262–271. doi:10.1159/000493864
Dai, C., Dai, S. Y., Gao, Y., Yan, T., Zhou, Q. Y., Liu, S. J., et al. (2023). Circ_0078607 increases platinum drug sensitivity via miR-196b-5p/GAS7 axis in ovarian cancer. Epigenetics 18 (1), 2175565. doi:10.1080/15592294.2023.2175565
Ding, J., Wang, Q., Guo, N., Wang, H., Chen, H., Ni, G., et al. (2020). CircRNA circ_0072995 promotes the progression of epithelial ovarian cancer by modulating miR-147a/CDK6 axis. Aging (Albany NY) 12 (17), 17209–17223. doi:10.18632/aging.103668
Dong, L. P., Chen, L. Y., Bai, B., Qi, X. F., Liu, J. N., and Qin, S. (2022). circ_0067934 promotes the progression of papillary thyroid carcinoma cells through miR-1301-3p/HMGB1 axis. Neoplasma 69 (1), 1–15. doi:10.4149/neo_2021_210608N771
Du, P., Xu, X., and Wang, Y. (2023). Hsa_circ_0000585 promotes chemoresistance to cis-platin in epithelial cells of ovarian cancer by modulating autophagy. Biochem. Biophys. Res. Commun. 678, 186–192. doi:10.1016/j.bbrc.2023.08.048
Fang, L., Ye, T., and An, Y. (2021). Circular RNA FOXP1 induced by ZNF263 upregulates U2AF2 expression to accelerate renal cell carcinoma tumorigenesis and Warburg effect through sponging miR-423-5p. J. Immunol. Res. 2021, 8050993, 8050993. doi:10.1155/2021/8050993
Feng, N., Guo, Z., Wu, X., Tian, Y., Li, Y., Geng, Y., et al. (2021). Circ_PIP5K1A regulates cisplatin resistance and malignant progression in non-small cell lung cancer cells and xenograft murine model via depending on miR-493-5p/ROCK1 axis. Respir. Res. 22 (1), 248. doi:10.1186/s12931-021-01840-7
Foruzandeh, Z., Zeinali-Sehrig, F., Nejati, K., Rahmanpour, D., Pashazadeh, F., Seif, F., et al. (2021). CircRNAs as potent biomarkers in ovarian cancer: a systematic scoping review. Cell Mol. Biol. Lett. 26 (1), 41. doi:10.1186/s11658-021-00284-7
Freedy, A. M., and Liau, B. B. (2021). Discovering new biology with drug-resistance alleles. Nat. Chem. Biol. 17 (12), 1219–1229. doi:10.1038/s41589-021-00865-9
Fu, L., Zhang, D., Yi, N., Cao, Y., Wei, Y., Wang, W., et al. (2022b). Circular RNA circPBX3 promotes cisplatin resistance of ovarian cancer cells via interacting with IGF2BP2 to stabilize ATP7A mRNA expression. Hum. Cell 35 (5), 1560–1576. doi:10.1007/s13577-022-00748-8
Fu, Y., Qiu, C., Yang, Y., Lu, J., and Qi, Y. (2022a). CircLPAR3 acts as an oncogene in oral squamous cell carcinoma through regulating the miR-643/HMGB2 network. Biochem. Genet. 60 (3), 882–898. doi:10.1007/s10528-021-10134-y
Gan, X., Zhu, H., Jiang, X., Obiegbusi, S. C., Yong, M., Long, X., et al. (2020). CircMUC16 promotes autophagy of epithelial ovarian cancer via interaction with ATG13 and miR-199a. Mol. Cancer 19 (1), 45. doi:10.1186/s12943-020-01163-z
Gao, M., Li, C., Xiao, H., Dong, H., Jiang, S., Fu, Y., et al. (2019b). hsa_circ_0007841: a novel potential biomarker and drug resistance for multiple myeloma. Front. Oncol. 9, 1261. doi:10.3389/fonc.2019.01261
Gao, Y., and Huang, Y. (2023). Circ_0007841 knockdown confers cisplatin sensitivity to ovarian cancer cells by down-regulation of NFIB expression in a miR-532-5p-dependent manner. J. Chemother. 35 (2), 117–130. doi:10.1080/1120009X.2022.2056995
Gao, Y., Zhang, C., Liu, Y., and Wang, M. (2019a). Circular RNA profiling reveals circRNA1656 as a novel biomarker in high grade serous ovarian cancer. Biosci. Trends 13 (2), 204–211. doi:10.5582/bst.2019.01021
Ghafouri-Fard, S., Khoshbakht, T., Hussen, B. M., Taheri, M., and Samsami, M. (2022). Emerging role of circular RNAs in the pathogenesis of ovarian cancer. Cancer Cell Int. 22 (1), 172. doi:10.1186/s12935-022-02602-1
Giaquinto, A. N., Broaddus, R. R., Jemal, A., and Siegel, R. L. (2022). The changing landscape of gynecologic cancer mortality in the United States. Obstet. Gynecol. 139 (3), 440–442. doi:10.1097/AOG.0000000000004676
Gong, J., Xu, X., Zhang, X., and Zhou, Y. (2020). Circular RNA-9119 suppresses in ovarian cancer cell viability via targeting the microRNA-21-5p-PTEN-Akt pathway. Aging (Albany NY) 12 (14), 14314–14328. doi:10.18632/aging.103470
Greenberg, M. V. C., and Bourc’his, D. (2019). The diverse roles of DNA methylation in mammalian development and disease. Nat. Rev. Mol. Cell Biol. 20 (10), 590–607. doi:10.1038/s41580-019-0159-6
Guan, X., Zong, Z. H., Liu, Y., Chen, S., Wang, L. L., and Zhao, Y. (2019). circPUM1 promotes tumorigenesis and progression of ovarian cancer by sponging miR-615-5p and miR-6753-5p. Mol. Ther. Nucleic Acids 18, 882–892. doi:10.1016/j.omtn.2019.09.032
Guo, M., Li, S., Zhao, X., Yuan, Y., Zhang, B., and Guan, Y. (2020). Knockdown of circular RNA Hsa_circ_0000714 can regulate RAB17 by sponging miR-370-3p to reduce paclitaxel resistance of ovarian cancer through CDK6/RB pathway. Onco Targets Ther. 13, 13211–13224. doi:10.2147/OTT.S285153
Guo, Y., Feng, X., Wang, Z., Zhang, R., Zheng, K., Xu, J., et al. (2023). The quantification of circular RNA 0007841 during induction therapy helps estimate the response and survival benefits to bortezomib-based regimen in multiple myeloma. Ir. J. Med. Sci. doi:10.1007/s11845-023-03410-w
He, S. N., Guan, S. H., Wu, M. Y., Li, W., Xu, M. D., and Tao, M. (2019). Down-regulated hsa_circ_0067934 facilitated the progression of gastric cancer by sponging hsa-mir-4705 to downgrade the expression of BMPR1B. Transl. Cancer Res. 8 (8), 2691–2703. doi:10.21037/tcr.2019.10.32
Hou, B., Chen, T., Zhang, H., Li, J., Wang, P., and Shang, G. (2023). The E3 ubiquitin ligases regulate PD-1/PD-L1 protein levels in tumor microenvironment to improve immunotherapy. Front. Immunol. 14, 1123244. doi:10.3389/fimmu.2023.1123244
Hou, W., and Zhang, Y. (2021). Circ_0025033 promotes the progression of ovarian cancer by activating the expression of LSM4 via targeting miR-184. Pathol. Res. Pract. 217, 153275. doi:10.1016/j.prp.2020.153275
Hu, C., Wang, Y., Li, A., Zhang, J., Xue, F., and Zhu, L. (2019). Overexpressed circ_0067934 acts as an oncogene to facilitate cervical cancer progression via the miR-545/EIF3C axis. J. Cell Physiol. 234 (6), 9225–9232. doi:10.1002/jcp.27601
Hu, J., Wang, L., Chen, J., Gao, H., Zhao, W., Huang, Y., et al. (2018). The circular RNA circ-ITCH suppresses ovarian carcinoma progression through targeting miR-145/RASA1 signaling. Biochem. Biophys. Res. Commun. 505 (1), 222–228. doi:10.1016/j.bbrc.2018.09.060
Huang, C., Qin, L., Chen, S., and Huang, Q. (2023). CircSETDB1 contributes to paclitaxel resistance of ovarian cancer cells by sponging miR-508-3p and regulating ABCC1 expression. Anticancer Drugs 34 (3), 395–404. doi:10.1097/CAD.0000000000001465
Huang, H., Yan, L., Zhong, J., Hong, L., Zhang, N., and Luo, X. (2022). Circ_0025033 deficiency suppresses paclitaxel resistance and malignant development of paclitaxel-resistant ovarian cancer cells by modulating the miR-532-3p/FOXM1 network. Immunopharmacol. Immunotoxicol. 44 (2), 275–286. doi:10.1080/08923973.2022.2038194
Huang, K., Liu, D., and Su, C. (2021). Circ_0007841 accelerates ovarian cancer development through facilitating MEX3C expression by restraining miR-151-3p activity. Aging (Albany NY) 13 (8), 12058–12066. doi:10.18632/aging.202911
Jiang, W., Xia, J., Xie, S., Zou, R., Pan, S., Wang, Z. W., et al. (2020). Long non-coding RNAs as a determinant of cancer drug resistance: towards the overcoming of chemoresistance via modulation of lncRNAs. Drug Resist Updat 50, 100683. doi:10.1016/j.drup.2020.100683
Jin, Y., and Wang, H. (2022). Circ_0078607 inhibits the progression of ovarian cancer via regulating the miR-32-5p/SIK1 network. J. Ovarian Res. 15 (1), 3. doi:10.1186/s13048-021-00931-9
Konstantinopoulos, P. A., and Matulonis, U. A. (2023). Clinical and translational advances in ovarian cancer therapy. Nat. Cancer 4 (9), 1239–1257. doi:10.1038/s43018-023-00617-9
Kristensen, L. S., Jakobsen, T., Hager, H., and Kjems, J. (2022). The emerging roles of circRNAs in cancer and oncology. Nat. Rev. Clin. Oncol. 19 (3), 188–206. doi:10.1038/s41571-021-00585-y
Lan, H., Yuan, J., Zeng, D., Liu, C., Guo, X., Yong, J., et al. (2021). The emerging role of non-coding RNAs in drug resistance of ovarian cancer. Front. Genet. 12, 693259. doi:10.3389/fgene.2021.693259
Li, B., and Zhang, L. (2021). CircSETDB1 knockdown inhibits the malignant progression of serous ovarian cancer through miR-129-3p-dependent regulation of MAP3K3. J. Ovarian Res. 14 (1), 160. doi:10.1186/s13048-021-00875-0
Li, H., Luo, F., Jiang, X., Zhang, W., Xiang, T., Pan, Q., et al. (2022c). CircITGB6 promotes ovarian cancer cisplatin resistance by resetting tumor-associated macrophage polarization toward the M2 phenotype. J. Immunother. Cancer 10 (3), e004029. doi:10.1136/jitc-2021-004029
Li, M., Cai, J., Han, X., and Ren, Y. (2020c). Downregulation of circNRIP1 suppresses the paclitaxel resistance of ovarian cancer via regulating the miR-211-5p/HOXC8 Axis. Cancer Manag. Res. 12, 9159–9171. doi:10.2147/CMAR.S268872
Li, M., Chi, C., Zhou, L., Chen, Y., and Tang, X. (2021). Circular PVT1 regulates cell proliferation and invasion via miR-149-5p/FOXM1 axis in ovarian cancer. J. Cancer 12 (2), 611–621. doi:10.7150/jca.52234
Li, O., Kang, J., Zhang, J. J., Wang, J., Hu, L. W., Li, L., et al. (2020d). Circle RNA FOXP1 promotes cell proliferation in lung cancer by regulating miR-185-5p/Wnt1 signaling pathway. Eur. Rev. Med. Pharmacol. Sci. 24 (12), 6767–6778. doi:10.26355/eurrev_202006_21665
Li, X., Jiang, X., Lu, J., Lin, Y., Jiang, L., Li, Y., et al. (2022a). CircCERS6 suppresses the development of epithelial ovarian cancer through mediating miR-630/RASSF8. Biochem. Genet. 60 (6), 2611–2629. doi:10.1007/s10528-022-10227-2
Li, X., Lin, S., Mo, Z., Jiang, J., Tang, H., Wu, C., et al. (2020a). CircRNA_100395 inhibits cell proliferation and metastasis in ovarian cancer via regulating miR-1228/p53/epithelial-mesenchymal transition (EMT) axis. J. Cancer 11 (3), 599–609. doi:10.7150/jca.35041
Li, X., Ma, N., Zhang, Y., Wei, H., Zhang, H., Pang, X., et al. (2020b). Circular RNA circNRIP1 promotes migration and invasion in cervical cancer by sponging miR-629-3p and regulating the PTP4A1/ERK1/2 pathway. Cell Death Dis. 11 (5), 399. doi:10.1038/s41419-020-2607-9
Li, X., Wang, J., Lin, W., Yuan, Q., Lu, Y., Wang, H., et al. (2022b). circEXOC6B interacting with RRAGB, an mTORC1 activator, inhibits the progression of colorectal cancer by antagonizing the HIF1A-RRAGB-mTORC1 positive feedback loop. Mol. Cancer 21 (1), 135. doi:10.1186/s12943-022-01600-1
Liang, Y. X., Zhang, L. L., and Yang, L. (2023). circANKRD17(has_circ_0007883) confers paclitaxel resistance of ovarian cancer via interacting with FUS to stabilize FOXR2. Mol. Cell Biochem. 478 (4), 835–850. doi:10.1007/s11010-022-04548-4
Lin, C., Xu, X., Yang, Q., Liang, L., and Qiao, S. (2020). Circular RNA ITCH suppresses proliferation, invasion, and glycolysis of ovarian cancer cells by up-regulating CDH1 via sponging miR-106a. Cancer Cell Int. 20, 336. doi:10.1186/s12935-020-01420-7
Lin, J., Qin, H., Han, Y., Li, X., Zhao, Y., and Zhai, G. (2021). CircNRIP1 modulates the miR-515-5p/IL-25 Axis to control 5-fu and cisplatin resistance in nasopharyngeal carcinoma. Drug Des. Devel Ther. 15, 323–330. doi:10.2147/DDDT.S292180
Liu, F., Li, R., Zhang, R., He, M., and Zhang, Y. (2021b). Knockdown of circNRIP1 sensitizes colorectal cancer to 5-FU via sponging miR-532-3p. Oncol. Rep. 46 (4), 218. doi:10.3892/or.2021.8169
Liu, J., and Liu, B. (2023). CircTNPO3 promotes hepatocellular carcinoma progression by sponging miR-199b-5p and regulating STRN expression. Kaohsiung J. Med. Sci. 39 (3), 221–233. doi:10.1002/kjm2.12631
Liu, J., and Shang, G. (2022). The roles of noncoding RNAs in the development of osteosarcoma stem cells and potential therapeutic targets. Front. Cell Dev. Biol. 10, 773038. doi:10.3389/fcell.2022.773038
Liu, J., Wang, H., Xiao, S., Zhang, S., Qi, Y., and Wang, M. (2023a). Circ_0000231 promotes paclitaxel resistance in ovarian cancer by regulating miR-140/RAP1B. Am. J. Cancer Res. 13 (3), 872–885.
Liu, M., Cao, S., Guo, Z., Wu, Z., Meng, J., Wu, Y., et al. (2022c). Roles and mechanisms of CircRNAs in ovarian cancer. Front. Cell Dev. Biol. 10, 1044897. doi:10.3389/fcell.2022.1044897
Liu, M., Zhang, H., Li, Y., and Wang, S. (2022a). Noncoding RNAs interplay in ovarian cancer therapy and drug resistance. Cancer Biother Radiopharm. 37 (3), 186–198. doi:10.1089/cbr.2021.0339
Liu, Q., Zhou, Q., and Zhong, P. (2020d). circ_0067934 increases bladder cancer cell proliferation, migration and invasion through suppressing miR-1304 expression and increasing Myc expression levels. Exp. Ther. Med. 19 (6), 3751–3759. doi:10.3892/etm.2020.8648
Liu, S. J., Dang, H. X., Lim, D. A., Feng, F. Y., and Maher, C. A. (2021a). Long noncoding RNAs in cancer metastasis. Nat. Rev. Cancer 21 (7), 446–460. doi:10.1038/s41568-021-00353-1
Liu, T., Yuan, L., and Zou, X. (2022d). Circular RNA circ-BNC2 (hsa_circ_0008732) inhibits the progression of ovarian cancer through microRNA-223-3p/FBXW7 axis. J. Ovarian Res. 15 (1), 95. doi:10.1186/s13048-022-01025-w
Liu, X., Yin, Z., Wu, Y., Zhan, Q., Huang, H., and Fan, J. (2022e). Circular RNA lysophosphatidic acid receptor 3 (circ-LPAR3) enhances the cisplatin resistance of ovarian cancer. Bioengineered 13 (2), 3739–3750. doi:10.1080/21655979.2022.2029109
Liu, Y., Chang, Y., and Cai, Y. (2020a). Hsa_circ_0061140 promotes endometrial carcinoma progression via regulating miR-149-5p/STAT3. Gene 745, 144625. doi:10.1016/j.gene.2020.144625
Liu, Y., Jiang, Y., Xu, L., Qu, C., Zhang, L., Xiao, X., et al. (2020c). circ-NRIP1 promotes glycolysis and tumor progression by regulating miR-186-5p/MYH9 Axis in gastric cancer. Cancer Manag. Res. 12, 5945–5956. doi:10.2147/CMAR.S245941
Liu, Y., Li, H., Ye, X., Ji, A., Fu, X., Wu, H., et al. (2020b). Hsa_circ_0000231 knockdown inhibits the glycolysis and progression of colorectal cancer cells by regulating miR-502-5p/MYO6 axis. World J. Surg. Oncol. 18 (1), 255. doi:10.1186/s12957-020-02033-0
Liu, Y., Shen, Z., Wei, X., Gu, L., Zheng, M., Zhang, Y., et al. (2023b). CircSLC39A8 attenuates paclitaxel resistance in ovarian cancer by regulating the miR-185-5p/BMF axis. Transl. Oncol. 36, 101746. doi:10.1016/j.tranon.2023.101746
Liu, Z., Zou, H., Dang, Q., Xu, H., Liu, L., Zhang, Y., et al. (2022b). Biological and pharmacological roles of m(6)A modifications in cancer drug resistance. Mol. Cancer 21 (1), 220. doi:10.1186/s12943-022-01680-z
Long, F., Li, Z., Wei, Z., and Xie, Y. (2022). Circular RNA circ_0007841 participates in progression of nonsmall cell lung cancer via miR-199a-5p/SphK2 axis. Anticancer Drugs 33 (10), 1035–1046. doi:10.1097/CAD.0000000000001348
Luo, Y., and Gui, R. (2020). Circulating exosomal circFoxp1 confers cisplatin resistance in epithelial ovarian cancer cells. J. Gynecol. Oncol. 31 (5), e75. doi:10.3802/jgo.2020.31.e75
Luo, Y., Liu, F., Ma, J., Fu, Y., and Gui, R. (2020). A novel epigenetic regulation of circFoxp1 on Foxp1 in colon cancer cells. Cell Death Dis. 11 (9), 782. doi:10.1038/s41419-020-03007-6
Lyu, M., Li, X., Shen, Y., Lu, J., Zhang, L., Zhong, S., et al. (2022). CircATRNL1 and circZNF608 inhibit ovarian cancer by sequestering miR-152-5p and encoding protein. Front. Genet. 13, 784089. doi:10.3389/fgene.2022.784089
Ma, H., Qu, S., Zhai, Y., and Yang, X. (2022). circ_0025033 promotes ovarian cancer development via regulating the hsa_miR-370-3p/SLC1A5 axis. Cell Mol. Biol. Lett. 27 (1), 94. doi:10.1186/s11658-022-00364-2
Ma, L., Liu, W., and Li, M. (2023). Circ_0061140 contributes to ovarian cancer progression by targeting miR-761/LETM1 signaling. Biochem. Genet. 61 (2), 628–650. doi:10.1007/s10528-022-10277-6
Matsas, A., Stefanoudakis, D., Troupis, T., Kontzoglou, K., Eleftheriades, M., Christopoulos, P., et al. (2023). Tumor markers and their diagnostic significance in ovarian cancer. Life (Basel) 13 (8), 1689. doi:10.3390/life13081689
Mattick, J. S., Amaral, P. P., Carninci, P., Carpenter, S., Chang, H. Y., Chen, L. L., et al. (2023). Long non-coding RNAs: definitions, functions, challenges and recommendations. Nat. Rev. Mol. Cell Biol. 24 (6), 430–447. doi:10.1038/s41580-022-00566-8
Millan-Zambrano, G., Burton, A., Bannister, A. J., and Schneider, R. (2022). Histone post-translational modifications - cause and consequence of genome function. Nat. Rev. Genet. 23 (9), 563–580. doi:10.1038/s41576-022-00468-7
Najafi, S. (2023). The emerging roles and potential applications of circular RNAs in ovarian cancer: a comprehensive review. J. Cancer Res. Clin. Oncol. 149 (5), 2211–2234. doi:10.1007/s00432-022-04328-z
Ning, L., Lang, J., and Wu, L. (2022). Plasma circN4BP2L2 is a promising novel diagnostic biomarker for epithelial ovarian cancer. BMC Cancer 22 (1), 6. doi:10.1186/s12885-021-09073-z
Ning, L., Long, B., Zhang, W., Yu, M., Wang, S., Cao, D., et al. (2018). Circular RNA profiling reveals circEXOC6B and circN4BP2L2 as novel prognostic biomarkers in epithelial ovarian cancer. Int. J. Oncol. 53 (6), 2637–2646. doi:10.3892/ijo.2018.4566
Pan, X., Huang, B., Ma, Q., Ren, J., Liu, Y., Wang, C., et al. (2022b). Circular RNA circ-TNPO3 inhibits clear cell renal cell carcinoma metastasis by binding to IGF2BP2 and destabilizing SERPINH1 mRNA. Clin. Transl. Med. 12 (7), e994. doi:10.1002/ctm2.994
Pan, Y., Huang, Q., Peng, X., Yu, S., and Liu, N. (2022a). Circ_0015756 promotes ovarian cancer progression via the miR-145-5p/PSAT1 axis. Reprod. Biol. 22 (4), 100702. doi:10.1016/j.repbio.2022.100702
Park, M. K., Lee, H., and Lee, C. H. (2022). Post-translational modification of ZEB family members in cancer progression. Int. J. Mol. Sci. 23 (23), 15127. doi:10.3390/ijms232315127
Pawlowska, A., Rekowska, A., Kurylo, W., Panczyszyn, A., Kotarski, J., and Wertel, I. (2023). Current understanding on why ovarian cancer is resistant to immune checkpoint inhibitors. Int. J. Mol. Sci. 24 (13), 10859. doi:10.3390/ijms241310859
Perez-Oquendo, M., and Gibbons, D. L. (2022). Regulation of ZEB1 function and molecular associations in tumor progression and metastasis. Cancers (Basel) 14 (8), 1864. doi:10.3390/cancers14081864
Pisa, R., and Kapoor, T. M. (2020). Chemical strategies to overcome resistance against targeted anticancer therapeutics. Nat. Chem. Biol. 16 (8), 817–825. doi:10.1038/s41589-020-0596-8
Portela, A., and Esteller, M. (2010). Epigenetic modifications and human disease. Nat. Biotechnol. 28 (10), 1057–1068. doi:10.1038/nbt.1685
Qin, K., Zhang, F., Wang, H., Wang, N., Qiu, H., Jia, X., et al. (2023b). circRNA circSnx12 confers Cisplatin chemoresistance to ovarian cancer by inhibiting ferroptosis through a miR-194-5p/SLC7A11 axis. BMB Rep. 56 (2), 184–189. doi:10.5483/BMBRep.2022-0175
Qin, M., Zhang, C., and Li, Y. (2023a). Circular RNAs in gynecologic cancers: mechanisms and implications for chemotherapy resistance. Front. Pharmacol. 14, 1194719. doi:10.3389/fphar.2023.1194719
Qiu, Y., Chen, Y., Agbede, O., Eshaghi, E., and Peng, C. (2022). Circular RNAs in epithelial ovarian cancer: from biomarkers to therapeutic targets. Cancers (Basel) 14 (22), 5711. doi:10.3390/cancers14225711
Rousseau, F., Ranchon, F., Bardin, C., Bakrin, N., Lavoue, V., Bengrine-Lefevre, L., et al. (2023). Ovarian cancer in the older patient: where are we now? What to do next? Ther. Adv. Med. Oncol. 15 (17588359231192397), 17588359231192397. doi:10.1177/17588359231192397
Sanchez-Lorenzo, L., Salas-Benito, D., Villamayor, J., Patino-Garcia, A., and Gonzalez-Martin, A. (2022). The BRCA gene in epithelial ovarian cancer. Cancers (Basel) 14 (5), 1235. doi:10.3390/cancers14051235
Shang, R., Lee, S., Senavirathne, G., and Lai, E. C. (2023). microRNAs in action: biogenesis, function and regulation. Nat. Rev. Genet. 24, 816–833. doi:10.1038/s41576-023-00611-y
Shao, N., Song, L., and Sun, X. (2021). Exosomal circ_PIP5K1A regulates the progression of non-small cell lung cancer and cisplatin sensitivity by miR-101/ABCC1 axis. Mol. Cell Biochem. 476 (6), 2253–2267. doi:10.1007/s11010-021-04083-8
Sheng, H., and Wang, X. (2023). Knockdown of circ-PIP5K1A overcomes resistance to cisplatin in ovarian cancer by miR-942-5p/NFIB axis. Anticancer Drugs 34 (2), 214–226. doi:10.1097/CAD.0000000000001406
Sheng, M., Wei, N., Yang, H. Y., Yan, M., Zhao, Q. X., and Jing, L. J. (2019). CircRNA UBAP2 promotes the progression of ovarian cancer by sponging microRNA-144. Eur. Rev. Med. Pharmacol. Sci. 23 (17), 7283–7294. doi:10.26355/eurrev_201909_18833
Shi, Y., Fang, N., Li, Y., Guo, Z., Jiang, W., He, Y., et al. (2020). Circular RNA LPAR3 sponges microRNA-198 to facilitate esophageal cancer migration, invasion, and metastasis. Cancer Sci. 111 (8), 2824–2836. doi:10.1111/cas.14511
Shvedunova, M., and Akhtar, A. (2022). Modulation of cellular processes by histone and non-histone protein acetylation. Nat. Rev. Mol. Cell Biol. 23 (5), 329–349. doi:10.1038/s41580-021-00441-y
Si, L., Zhang, L., Xing, S., Fang, P., Tian, X., Liu, X., et al. (2023). Curcumin as a therapeutic agent in cancer therapy: focusing on its modulatory effects on circular RNAs. Phytother. Res. 37 (7), 3121–3134. doi:10.1002/ptr.7863
Siegel, R. L., Miller, K. D., Wagle, N. S., and Jemal, A. (2023). Cancer statistics, 2023. CA Cancer J. Clin. 73 (1), 17–48. doi:10.3322/caac.21763
Song, R., Chai, T., Liu, J., Chu, A., Sun, C., and Liu, Z. (2023). Knockdown of circMFN2 inhibits cell progression and glycolysis by miR-198/CUL4B pathway in ovarian cancer. J. Biochem. Mol. Toxicol. 37 (8), e23383. doi:10.1002/jbt.23383
Song, Y., Hu, N., Song, X., and Yang, J. (2020). Hsa_Circ_0007841 enhances multiple myeloma chemotherapy resistance through upregulating ABCG2. Technol. Cancer Res. Treat. 19, 1533033820928371. 1533033820928371. doi:10.1177/1533033820928371
Su, Z., Pan, C., Xie, H., Ning, Y., Li, S., and Xiao, H. (2022). Downregulation of circLPAR3 inhibits tumor progression and glycolysis by liberating miR-144-3p and upregulating LPCAT1 in oral squamous cell carcinoma. Laryngoscope Investig. Otolaryngol. 7 (2), 425–436. doi:10.1002/lio2.771
Sun, S., and Fang, H. (2021). Curcumin inhibits ovarian cancer progression by regulating circ-PLEKHM3/miR-320a/SMG1 axis. J. Ovarian Res. 14 (1), 158. doi:10.1186/s13048-021-00916-8
Torre, L. A., Trabert, B., DeSantis, C. E., Miller, K. D., Samimi, G., Runowicz, C. D., et al. (2018). Ovarian cancer statistics. CA Cancer J. Clin. 68 (4), 284–296. doi:10.3322/caac.21456
Treiber, T., Treiber, N., and Meister, G. (2019). Regulation of microRNA biogenesis and its crosstalk with other cellular pathways. Nat. Rev. Mol. Cell Biol. 20 (1), 5–20. doi:10.1038/s41580-018-0059-1
Van Loo, K. M. J., Carvill, G. L., Becker, A. J., Conboy, K., Goldman, A. M., Kobow, K., et al. (2022). Epigenetic genes and epilepsy - emerging mechanisms and clinical applications. Nat. Rev. Neurol. 18 (9), 530–543. doi:10.1038/s41582-022-00693-y
Wang, F., Niu, Y., Chen, K., Yuan, X., Qin, Y., Zheng, F., et al. (2023a). Extracellular vesicle-packaged circATP2B4 mediates M2 macrophage polarization via miR-532-3p/SREBF1 Axis to promote epithelial ovarian cancer metastasis. Cancer Immunol. Res. 11 (2), 199–216. doi:10.1158/2326-6066.CIR-22-0410
Wang, G., Zhang, H., and Li, P. (2020a). Upregulation of hsa_circRNA_102958 indicates poor prognosis and promotes ovarian cancer progression through miR-1205/SH2D3A Axis. Cancer Manag. Res. 12, 4045–4053. doi:10.2147/CMAR.S248560
Wang, H., Lan, S., Wang, L., Zhao, J., Jia, X., Xu, J., et al. (2023c). Expression of circ-PHC3 enhances ovarian cancer progression via regulation of the miR-497-5p/SOX9 pathway. J. Ovarian Res. 16 (1), 142. doi:10.1186/s13048-023-01170-w
Wang, H., Liang, C., Lin, J., Dong, Y., Wang, Y., and Xia, L. (2023b). Hsa_circ_0001741 suppresses ovarian cancer cell proliferations through adsorption of miR-188-5p and promotion of FOXN2 expression. Mol. Biotechnol. doi:10.1007/s12033-023-00773-4
Wang, H., Yan, X., Zhang, H., and Zhan, X. (2019b). CircRNA circ_0067934 overexpression correlates with poor prognosis and promotes thyroid carcinoma progression. Med. Sci. Monit. 25, 1342–1349. doi:10.12659/MSM.913463
Wang, H., Zhang, X., Qiao, L., and Wang, H. (2022b). CircRNA circ_0000554 promotes ovarian cancer invasion and proliferation by regulating miR-567. Environ. Sci. Pollut. Res. Int. 29 (13), 19072–19080. doi:10.1007/s11356-021-13710-2
Wang, H. H., Ma, J. N., and Zhan, X. R. (2021c). Circular RNA Circ_0067934 attenuates ferroptosis of thyroid cancer cells by miR-545-3p/slc7a11 signaling. Front. Endocrinol. (Lausanne) 12, 670031. doi:10.3389/fendo.2021.670031
Wang, J., and Li, H. (2018). CircRNA circ_0067934 silencing inhibits the proliferation, migration and invasion of NSCLC cells and correlates with unfavorable prognosis in NSCLC. Eur. Rev. Med. Pharmacol. Sci. 22 (10), 3053–3060. doi:10.26355/eurrev_201805_15063
Wang, J., Li, S., Zhang, G., and Han, H. (2021b). Sevoflurane inhibits malignant progression of colorectal cancer via hsa_circ_0000231-mediated miR-622. J. Biol. Res. Thessal. 28 (1), 14. doi:10.1186/s40709-021-00145-6
Wang, J. M., Li, X. J., and Wang, J. (2019c). Circular RNA circ_0067934 functions as an oncogene in breast cancer by targeting Mcl-1. Eur. Rev. Med. Pharmacol. Sci. 23 (21), 9499–9505. doi:10.26355/eurrev_201911_19444
Wang, K., Fan, Y., Sun, J., Zhao, L., Yu, Y., and Li, G. (2021a). Circ_0061140 stimulates the malignant development of prostate cancer by targeting miR-1193. Transl. Androl. Urol. 10 (5), 1928–1938. doi:10.21037/tau-20-1477
Wang, S., Zhang, H., Xia, L., and Lan, F. (2022d). Circular RNA circ_0061140 accelerates hypoxia-induced glycolysis, migration, and invasion in lung adenocarcinoma through the microRNA-653/hexokinase 2 (HK2) axis. Bioengineered 13 (3), 7156–7166. doi:10.1080/21655979.2021.2000743
Wang, S., Zhang, Y., Cai, Q., Ma, M., Jin, L. Y., Weng, M., et al. (2019d). Circular RNA FOXP1 promotes tumor progression and Warburg effect in gallbladder cancer by regulating PKLR expression. Mol. Cancer 18 (1), 145. doi:10.1186/s12943-019-1078-z
Wang, W., Li, Y., Li, X., Liu, B., Han, S., Li, X., et al. (2020f). Circular RNA circ-FOXP1 induced by SOX9 promotes hepatocellular carcinoma progression via sponging miR-875-3p and miR-421. Biomed. Pharmacother. 121, 109517. doi:10.1016/j.biopha.2019.109517
Wang, W., Liu, W., Chen, Q., Yuan, Y., and Wang, P. (2022c). Targeting CSC-related transcription factors by E3 ubiquitin ligases for cancer therapy. Semin. Cancer Biol. 87, 84–97. doi:10.1016/j.semcancer.2022.11.002
Wang, W., Wang, J., Zhang, X., and Liu, G. (2019a). Serum circSETDB1 is a promising biomarker for predicting response to platinum-taxane-combined chemotherapy and relapse in high-grade serous ovarian cancer. Onco Targets Ther. 12, 7451–7457. doi:10.2147/OTT.S220700
Wang, X., Yao, Y., and Jin, M. (2020b). Circ-0001068 is a novel biomarker for ovarian cancer and inducer of PD1 expression in T cells. Aging (Albany NY) 12 (19), 19095–19106. doi:10.18632/aging.103706
Wang, Y., Huang, Z., Li, B., Liu, L., and Huang, C. (2022a). The emerging roles and therapeutic implications of epigenetic modifications in ovarian cancer. Front. Endocrinol. (Lausanne) 13, 863541. doi:10.3389/fendo.2022.863541
Wang, Y., Lin, Q., Song, C., Ma, R., and Li, X. (2020d). Depletion of circ_0007841 inhibits multiple myeloma development and BTZ resistance via miR-129-5p/JAG1 axis. Cell Cycle 19 (23), 3289–3302. doi:10.1080/15384101.2020.1839701
Wang, Y., Lin, Q., Song, C., Ma, R., and Li, X. (2020e). Circ_0007841 promotes the progression of multiple myeloma through targeting miR-338-3p/BRD4 signaling cascade. Cancer Cell Int. 20, 383. doi:10.1186/s12935-020-01475-6
Wang, Z., Zhang, W., Fang, J., Xie, P., Miao, M., and Yang, H. (2020c). Circular RNA circEXOC6B inhibits the progression of ovarian cancer by sponging miR-421 and regulating RUS1 expression. Onco Targets Ther. 13, 8233–8243. doi:10.2147/OTT.S243040
Wei, L., He, W., Zhao, H., and Zhao, P. (2022). Circ_0026123 promotes cisplatin resistance and progression of ovarian cancer by upregulating RAB1A through sequestering miR-543. Anticancer Drugs 33 (10), 1069–1080. doi:10.1097/CAD.0000000000001373
Wei, L., He, Y., Bi, S., Li, X., Zhang, J., and Zhang, S. (2021b). miRNA-199b-3p suppresses growth and progression of ovarian cancer via the CHK1/E-cadherin/EMT signaling pathway by targeting ZEB1. Oncol. Rep. 45 (2), 569–581. doi:10.3892/or.2020.7895
Wei, S., Qi, L., and Wang, L. (2021a). Overexpression of circ_CELSR1 facilitates paclitaxel resistance of ovarian cancer by regulating miR-149-5p/SIK2 axis. Anticancer Drugs 32 (5), 496–507. doi:10.1097/CAD.0000000000001058
Winkle, M., El-Daly, S. M., Fabbri, M., and Calin, G. A. (2021). Noncoding RNA therapeutics - challenges and potential solutions. Nat. Rev. Drug Discov. 20 (8), 629–651. doi:10.1038/s41573-021-00219-z
Wu, H., Zhao, X., Wang, J., Jiang, X., Cheng, Y., He, Y., et al. (2021b). Circular RNA CDR1as alleviates cisplatin-based chemoresistance by suppressing MiR-1299 in ovarian cancer. Front. Genet. 12, 815448. doi:10.3389/fgene.2021.815448
Wu, M., Qiu, Q., Zhou, Q., Li, J., Yang, J., Zheng, C., et al. (2022). circFBXO7/miR-96-5p/MTSS1 axis is an important regulator in the Wnt signaling pathway in ovarian cancer. Mol. Cancer 21 (1), 137. doi:10.1186/s12943-022-01611-y
Wu, S. G., Zhou, P., Chen, J. X., Lei, J., Hua, L., Dong, Y., et al. (2021a). circ-PTK2 (hsa_circ_0008305) regulates the pathogenic processes of ovarian cancer via miR-639 and FOXC1 regulatory cascade. Cancer Cell Int. 21 (1), 277. doi:10.1186/s12935-021-01985-x
Wu, Y., Xu, M., Feng, Z., Wu, H., Wu, J., Ha, X., et al. (2023b). AUF1-induced circular RNA hsa_circ_0010467 promotes platinum resistance of ovarian cancer through miR-637/LIF/STAT3 axis. Cell Mol. Life Sci. 80 (9), 256. doi:10.1007/s00018-023-04906-5
Wu, Y., Zhou, J., Li, Y., Shi, X., Shen, F., Chen, M., et al. (2023a). Hsa_circ_0001445 works as a cancer suppressor via miR-576-5p/SFRP1 axis regulation in ovarian cancer. Cancer Med. 12 (5), 5736–5750. doi:10.1002/cam4.5317
Xia, B., Zhao, Z., Wu, Y., Wang, Y., Zhao, Y., and Wang, J. (2020). Circular RNA circTNPO3 regulates paclitaxel resistance of ovarian cancer cells by miR-1299/NEK2 signaling pathway. Mol. Ther. Nucleic Acids 21, 780–791. doi:10.1016/j.omtn.2020.06.002
Xia, W., Qiu, M., Chen, R., Wang, S., Leng, X., Wang, J., et al. (2016). Circular RNA has_circ_0067934 is upregulated in esophageal squamous cell carcinoma and promoted proliferation. Sci. Rep. 6, 35576. doi:10.1038/srep35576
Xie, W., Chu, M., Song, G., Zuo, Z., Han, Z., Chen, C., et al. (2022). Emerging roles of long noncoding RNAs in chemoresistance of pancreatic cancer. Semin. Cancer Biol. 83, 303–318. doi:10.1016/j.semcancer.2020.11.004
Xin, J., Zhang, X. Y., Sun, D. K., Tian, L. Q., and Xu, P. (2019). Up-regulated circular RNA hsa_circ_0067934 contributes to glioblastoma progression through activating PI3K-AKT pathway. Eur. Rev. Med. Pharmacol. Sci. 23 (8), 3447–3454. doi:10.26355/eurrev_201904_17709
Xu, F., Ni, M., Li, J., Cheng, J., Zhao, H., Zhao, J., et al. (2020b). Circ0004390 promotes cell proliferation through sponging miR-198 in ovarian cancer. Biochem. Biophys. Res. Commun. 526 (1), 14–20. doi:10.1016/j.bbrc.2020.03.024
Xu, G., Li, M., Wu, J., Qin, C., Tao, Y., and He, H. (2020c). Circular RNA circNRIP1 sponges microRNA-138-5p to maintain hypoxia-induced resistance to 5-fluorouracil through HIF-1α-Dependent glucose metabolism in gastric carcinoma. Cancer Manag. Res. 12, 2789–2802. doi:10.2147/CMAR.S246272
Xu, J., Sang, N., Zhao, J., He, W., Zhang, N., and Li, X. (2022). Knockdown of circ_0067934 inhibits gastric cancer cell proliferation, migration and invasion via the miR-1301-3p/KIF23 axis. Mol. Med. Rep. 25 (6), 202. doi:10.3892/mmr.2022.12718
Xu, Q., Deng, B., Li, M., Chen, Y., and Zhuan, L. (2020a). circRNA-UBAP2 promotes the proliferation and inhibits apoptosis of ovarian cancer though miR-382-5p/PRPF8 axis. J. Ovarian Res. 13 (1), 81. doi:10.1186/s13048-020-00685-w
Yang, X., Mei, J., Wang, H., Gu, D., Ding, J., and Liu, C. (2020). The emerging roles of circular RNAs in ovarian cancer. Cancer Cell Int. 20, 265. doi:10.1186/s12935-020-01367-9
Yang, X., Wang, J., Li, H., Sun, Y., and Tong, X. (2021). Downregulation of hsa_circ_0026123 suppresses ovarian cancer cell metastasis and proliferation through the miR-124-3p/EZH2 signaling pathway. Int. J. Mol. Med. 47 (2), 668–676. doi:10.3892/ijmm.2020.4804
Ye, J., Wu, J., and Liu, B. (2023). Therapeutic strategies of dual-target small molecules to overcome drug resistance in cancer therapy. Biochim. Biophys. Acta Rev. Cancer 1878 (3), 188866. doi:10.1016/j.bbcan.2023.188866
Yin, Y., Li, J., Rong, J., Zhang, B., Wang, X., and Han, H. (2022). Circ_0067934 reduces JNK phosphorylation through a microRNA-545-3p/PPA1 axis to enhance tumorigenesis and cisplatin resistance in ovarian cancer. Immunopharmacol. Immunotoxicol. 44 (2), 261–274. doi:10.1080/08923973.2022.2038193
Ying, H., Zhao, R., Yu, Q., Zhang, K., and Deng, Q. (2022). CircATL2 enhances paclitaxel resistance of ovarian cancer via impacting miR-506-3p/NFIB axis. Drug Dev. Res. 83 (2), 512–524. doi:10.1002/ddr.21882
You, J., Han, Y., Qiao, H., Han, Y., Lu, X., Lu, Y., et al. (2022). Hsa_circ_0063804 enhances ovarian cancer cells proliferation and resistance to cisplatin by targeting miR-1276/CLU axis. Aging (Albany NY) 14 (11), 4699–4713. doi:10.18632/aging.203474
Yousefi, P. D., Suderman, M., Langdon, R., Whitehurst, O., Davey Smith, G., and Relton, C. L. (2022). DNA methylation-based predictors of health: applications and statistical considerations. Nat. Rev. Genet. 23 (6), 369–383. doi:10.1038/s41576-022-00465-w
Yu, L., Zheng, J., Yu, J., Zhang, Y., and Hu, H. (2023). Circ_0067934: a circular RNA with roles in human cancer. Hum. Cell 36, 1865–1876. doi:10.1007/s13577-023-00962-y
Yu, T., Ran, L., Zhao, H., Yin, P., Li, W., Lin, J., et al. (2021). Circular RNA circ-TNPO3 suppresses metastasis of GC by acting as a protein decoy for IGF2BP3 to regulate the expression of MYC and SNAIL. Mol. Ther. Nucleic Acids 26, 649–664. doi:10.1016/j.omtn.2021.08.029
Zeng, X. Y., Yuan, J., Wang, C., Zeng, D., Yong, J. H., Jiang, X. Y., et al. (2020). circCELSR1 facilitates ovarian cancer proliferation and metastasis by sponging miR-598 to activate BRD4 signals. Mol. Med. 26 (1), 70. doi:10.1186/s10020-020-00194-y
Zhang, C., Wang, S., Chao, F., Jia, G., Ye, X., Han, D., et al. (2023b). The short inverted repeats-induced circEXOC6B inhibits prostate cancer metastasis by enhancing the binding of RBMS1 and HuR. Mol. Ther. 31 (6), 1705–1721. doi:10.1016/j.ymthe.2022.08.006
Zhang, F., Xu, Y., Ye, W., Jiang, J., and Wu, C. (2020b). Circular RNA S-7 promotes ovarian cancer EMT via sponging miR-641 to up-regulate ZEB1 and MDM2. Biosci. Rep. 40 (7), BSR20200825. doi:10.1042/BSR20200825
Zhang, H., Ma, X. P., Li, X., and Deng, F. S. (2019c). Circular RNA circ_0067934 exhaustion expedites cell apoptosis and represses cell proliferation, migration and invasion in thyroid cancer via sponging miR-1304 and regulating CXCR1 expression. Eur. Rev. Med. Pharmacol. Sci. 23 (24), 10851–10866. doi:10.26355/eurrev_201912_19789
Zhang, H., Yu, Z., Wu, B., and Sun, F. (2021c). Circular RNA circFOXP1 promotes angiogenesis by regulating microRNA -127-5p/CDKN2AIP signaling pathway in osteosarcoma. Bioengineered 12 (2), 9991–9999. doi:10.1080/21655979.2021.1989258
Zhang, J., Wang, C., Jia, C., Zhang, Y., Qing, X., Zhang, Y., et al. (2022a). The role of circular RNAs in the physiology and pathology of the mammalian ovary. Int. J. Mol. Sci. 23 (23), 15204. doi:10.3390/ijms232315204
Zhang, L., Zhou, Q., Qiu, Q., Hou, L., Wu, M., Li, J., et al. (2019a). CircPLEKHM3 acts as a tumor suppressor through regulation of the miR-9/BRCA1/DNAJB6/KLF4/AKT1 axis in ovarian cancer. Mol. Cancer 18 (1), 144. doi:10.1186/s12943-019-1080-5
Zhang, N., Jin, Y., Hu, Q., Cheng, S., Wang, C., Yang, Z., et al. (2020c). Circular RNA hsa_circ_0078607 suppresses ovarian cancer progression by regulating miR-518a-5p/Fas signaling pathway. J. Ovarian Res. 13 (1), 64. doi:10.1186/s13048-020-00664-1
Zhang, N., Yang, Z., Jin, Y., Cheng, S., Yang, J., and Wang, Y. (2021d). Low expression of circular RNA hsa_circ_0078607 predicts poor prognosis in high-grade serous ovarian cancer. Cancer Manag. Res. 13, 2877–2883. doi:10.2147/CMAR.S300738
Zhang, S., Cheng, J., Quan, C., Wen, H., Feng, Z., Hu, Q., et al. (2020a). circCELSR1 (hsa_circ_0063809) contributes to paclitaxel resistance of ovarian cancer cells by regulating FOXR2 expression via miR-1252. Mol. Ther. Nucleic Acids 19, 718–730. doi:10.1016/j.omtn.2019.12.005
Zhang, X., Liu, Q., Zhang, J., Song, C., Han, Z., Wang, J., et al. (2023a). The emerging role of lncRNAs in osteoarthritis development and potential therapy. Front. Genet. 14, 1273933, 1273933. doi:10.3389/fgene.2023.1273933
Zhang, X., Wang, S., Wang, H., Cao, J., Huang, X., Chen, Z., et al. (2019b). Circular RNA circNRIP1 acts as a microRNA-149-5p sponge to promote gastric cancer progression via the AKT1/mTOR pathway. Mol. Cancer 18 (1), 20. doi:10.1186/s12943-018-0935-5
Zhang, Y., Di, Q., Chen, J., Chang, M., Ma, Y., and Yu, J. (2022b). Circ_0061140 contributes to the malignant progression in ovarian cancer cells by mediating the RAB1A level through sponging miR-361-5p. Biochem. Genet. 60 (6), 1946–1962. doi:10.1007/s10528-022-10200-z
Zhang, Y., Wei, Y. J., Zhang, Y. F., Liu, H. W., and Zhang, Y. F. (2021a). Emerging functions and clinical applications of exosomal ncRNAs in ovarian cancer. Front. Oncol. 11, 765458. doi:10.3389/fonc.2021.765458
Zhang, Z., Zhu, H., and Hu, J. (2021b). CircRAB11FIP1 promoted autophagy flux of ovarian cancer through DSC1 and miR-129. Cell Death Dis. 12 (2), 219. doi:10.1038/s41419-021-03486-1
Zhao, L., Guo, H., Chen, X., Zhang, W., He, Q., Ding, L., et al. (2022). Tackling drug resistance in ovarian cancer with epigenetic targeted drugs. Eur. J. Pharmacol. 927, 175071, 175071. doi:10.1016/j.ejphar.2022.175071
Zhao, M., Ma, W., and Ma, C. (2020). Circ_0067934 promotes non-small cell lung cancer development by regulating miR-1182/KLF8 axis and activating Wnt/beta-catenin pathway. Biomed. Pharmacother., 129, 110461. doi:10.1016/j.biopha.2020.110461
Zhao, Z., Ji, M., Wang, Q., He, N., and Li, Y. (2019). Circular RNA Cdr1as upregulates SCAI to suppress cisplatin resistance in ovarian cancer via miR-1270 suppression. Mol. Ther. Nucleic Acids 18, 24–33. doi:10.1016/j.omtn.2019.07.012
Zheng, H., Shi, L., Tong, C., Liu, Y., and Hou, M. (2021). circSnx12 is involved in ferroptosis during heart failure by targeting miR-224-5p. Front. Cardiovasc Med. 8, 656093. doi:10.3389/fcvm.2021.656093
Zheng, Y., Li, Z., Yang, S., Wang, Y., and Luan, Z. (2022). CircEXOC6B suppresses the proliferation and motility and sensitizes ovarian cancer cells to paclitaxel through miR-376c-3p/FOXO3 Axis. Cancer Biother Radiopharm. 37 (9), 802–814. doi:10.1089/cbr.2020.3739
Zhou, C., Li, R., and Mi, W. (2020b). circ_0067934: a potential biomarker and therapeutic target for hepatocellular carcinoma. Ann. Clin. Lab. Sci. 50 (6), 734–738.
Zhou, J., Dong, Z. N., Qiu, B. Q., Hu, M., Liang, X. Q., Dai, X., et al. (2020a). CircRNA FGFR3 induces epithelial-mesenchymal transition of ovarian cancer by regulating miR-29a-3p/E2F1 axis. Aging (Albany NY) 12 (14), 14080–14091. doi:10.18632/aging.103388
Zhu, J., Luo, J. E., Chen, Y., and Wu, Q. (2021). Circ_0061140 knockdown inhibits tumorigenesis and improves PTX sensitivity by regulating miR-136/CBX2 axis in ovarian cancer. J. Ovarian Res. 14 (1), 136. doi:10.1186/s13048-021-00888-9
Zhu, Q., Lu, G., Luo, Z., Gui, F., Wu, J., Zhang, D., et al. (2018). CircRNA circ_0067934 promotes tumor growth and metastasis in hepatocellular carcinoma through regulation of miR-1324/FZD5/Wnt/β-catenin axis. Biochem. Biophys. Res. Commun. 497 (2), 626–632. doi:10.1016/j.bbrc.2018.02.119
Zong, Z. H., Du, Y. P., Guan, X., Chen, S., and Zhao, Y. (2019). CircWHSC1 promotes ovarian cancer progression by regulating MUC1 and hTERT through sponging miR-145 and miR-1182. J. Exp. Clin. Cancer Res. 38 (1), 437. doi:10.1186/s13046-019-1437-z
Zou, J., Liu, L., Wang, Q., Yin, F., Yang, Z., Zhang, W., et al. (2017). Downregulation of miR-429 contributes to the development of drug resistance in epithelial ovarian cancer by targeting ZEB1. Am. J. Transl. Res. 9 (3), 1357–1368.
Zou, Q., Wang, T., Li, B., Li, G., Zhang, L., Wang, B., et al. (2018). Overexpression of circ-0067934 is associated with increased cellular proliferation and the prognosis of non-small cell lung cancer. Oncol. Lett. 16 (5), 5551–5556. doi:10.3892/ol.2018.9357
Keywords: chemotherapy, circRNA, drug, miRNA, ovarian cancer, resistance
Citation: Zhan J, Li Z, Lin C, Wang D, Yu L and Xiao X (2023) The role of circRNAs in regulation of drug resistance in ovarian cancer. Front. Genet. 14:1320185. doi: 10.3389/fgene.2023.1320185
Received: 11 October 2023; Accepted: 04 December 2023;
Published: 13 December 2023.
Edited by:
Bodhisattwa Banerjee, University of Vermont, United StatesReviewed by:
Mehak Gupta, Vertex Pharmaceuticals, United StatesCopyright © 2023 Zhan, Li, Lin, Wang, Yu and Xiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xue Xiao, eGlhb3h1ZTE5ODExNDU0QDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.