- 1Department of Cardiology, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, China
- 2The First Clinical College, Zhejiang Chinese Medical University, Hangzhou, China
Background: Previous studies have reported inconsistent results on the causal association between habitual tea consumption and the risk of cardiovascular disease (CVD). This study is aim to determine the association between habitual tea intake and CVD using two-sample Mendelian randomization (MR) analysis.
Methods: The genetically predicted causation between tea consumption and 7 common cardiovascular diseases (atrial fibrillation, hypertension, acute myocardial infarction, coronary atherosclerosis, peripheral vascular disease, angina, and heart failure) was evaluated using MR analysis model. We performed a total of 9 MR analysis methods to analyze the final results. The IVW methods was used as the primary outcome. The other MR analysis method (simple mode, weighted mode, simple median, weighted median, penalized weighted median, MR Egger, and MR-Egger (bootstrap)) were performed as the complement to IVW. Also, the robustness of the MR analysis results was assessed using a leave-one-out analysis.
Results: The IVW analysis methods indicated that there is no causal association between tea consumption and risk of CVD (AF: OR, 0.997, 95% CI, 0.992–1.0001, p = 0.142; hypertension: OR, 0.976, 95% CI, 0.937–1.017, p = 0.242; AMI: OR, 0.996, 95% CI, 0.991–1.000, p = 0.077; CA: OR, 1.001, 95% CI, 0.993–1.009, p = 0.854; PVD: OR, 1.002, 95% CI, 1.000–1.005, p = 0.096; angina: OR, 0.999, 95% CI, 0.993–1.006, p = 0.818; HF: OR, 0.999, 95% CI, 0.996–1.002, p = 0.338). The other MR analysis method and further leave-one-out sensitivity analysis suggested the results were robust.
Conclusion: This MR study indicated that there was no genetically predicted causal association between habitual tea intake and risk of CVD.
Introduction
Cardiovascular disease (CVD) is the leading cause of death worldwide, accounting for one-third of global mortality (Roth et al., 2020). Considering the substantial global burden of CVD, there is a great interest in identifying potential preventative approaches. It has been shown in previous studies that dietary factors may play an important role in the development of CVD (Kim et al., 2019; Shin et al., 2022).
Tea culture is popular all over the world and tea is currently the best-selling beverage worldwide. The causal relationship between habitual tea intake and the risk of CVD is still unclear. On one hand, tea contains phenolic compounds, with anti-oxidant and anti-inflammatory activities, which may contribute to cardiac protection (Manolis et al., 2022). On the other hand, the presence of the substantial amount of caffeine in tea may cause cardiac arrhythmia (Voskoboinik et al., 2019). So far, several studies reported that habitual tea intake may reduce the risk of CVD (Wang et al., 2020; Niu et al., 2021; Chen et al., 2022). However, other observational studies suggested that tea consumption may be associated with a higher risk of CVD (Malasevskaia et al., 2020; Feng et al., 2021; Zheng et al., 2022). In addition, there are also several studies indicated that there is no causation between tea consumption and CVD (Wang et al., 2019; Igho-Osagie et al., 2020). In general, the existing results are contradictory and the genetically predicted causal effect of tea consumption on CVD is still uncertain.
The conflicting results come from previous observational studies are most likely to be attributed to reverse causality and unmeasured confounding. Using genetic variants as instrumental variables (IV), Mendelian randomization (MR) analysis method can eliminate latent confounding factors and reverse causality (Bennett and Holmes, 2017). MR analysis is therefore capable of examining the causal relationship between exposure and outcome in a robust manner. Thus, we conducted a two-sample MR analysis to explore the causation between tea consumption and the risk of CVD in this study.
Methods
Study design and data sources
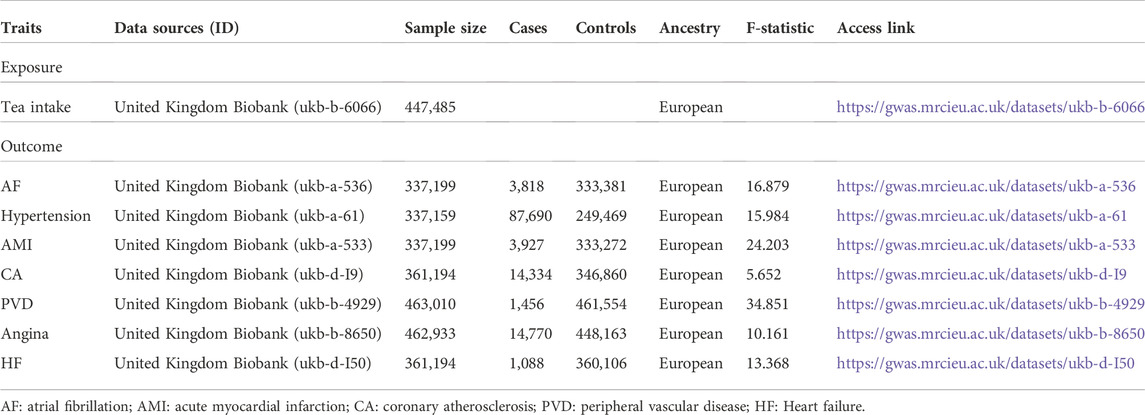
In contrast to one-sample MR analysis, two-sample MR analysis obtains the effect of IV-exposure association and IV-outcome association from two different sample. In other words, one-sample MR analysis is only possible to estimate the relationship between genetic variants and exposure outcomes in one sample. As opposed to one-sample MR, two-sample MR can analyze the association in much larger sample size and therefore obtain statistically higher precision (Lawlor, 2016). Thus, a two-sample MR analysis was conducted in this study to evaluate the causal effect of tea consumption on 7 cardiovascular diseases, including atrial fibrillation (AF), hypertension, acute myocardial infarction (AMI), coronary atherosclerosis (CA), peripheral vascular disease (PVD), angina, and heart failure (HF) (Figure 1). The single nucleotide polymorphisms (SNPs) of both habitual tea consumption and CVD were derived from recently published genome-wide association studies (GWAS). Detailed information about data sources is shown in Table 1. The GWAS meta-analyses data had obtained relevant ethical approval from their ethics committee. In this study, only the summarized data extracted from the GWAS database was used. Therefore, no additional ethics approval is needed for this study.
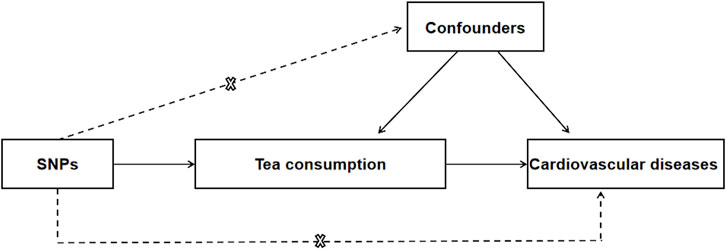
FIGURE 1. Mendelian randomization model of tea consumption and risk of CVD. The design is under the assumption that the genetic variants are associated with tea consumption, but not with confounders, and the genetic variants influence CVD only through tea consumption. CVD, cardiovascular disease; SNP, single nucleotide polymorphism.
Single nucleotide polymorphisms selection
In this Study, genetic variants were selected as IV. IV should meet the following MR assumptions: 1) There was a strong association between exposure and IV. 2) There was no association between IV and any confounders. 3) IV directly impacted the outcomes via exposure instead of other pathways. Tea consumption data was derived from the recently published GWAS analyzing 447,485 individuals of European ancestry of tea consumption based on United Kingdom Biobank. Autosomal biallelic SNPs with p-value <5 × 10–8 and minor frequency >1% were selected as preliminary candidate SNPs (2,672 unique SNPs). Furthermore, the independence of the chosen genetic variants was confirmed through clumping these 2,672 SNPs with linkage disequilibrium (r2 < 0.001 at a 10,000 kb window). Then the association between SNPs and established confounders (such as smoking, lipid traits, obesity, and diabetes) was examined by “PhenoScanner” (http://www.phenoscanner.medschl.cam.ac.uk/). Ultimately, we found 49 independent SNPs related to tea consumption. The SNPs data for CVD were derived from the recently published largest GWAS (https://gwas.mrcieu.ac.uk/) (Nielsen et al., 2018). Detailed information of all SNPs used in this study are presented in Supplementary Table S1–7.
Statistical analysis
This study was performed using a total of 9 MR analysis methods: inverse-variance weighted approach (IVW) (fixed-effect and random-effect model) (Bowden et al., 2016), MR-Egger regression approach (General model and bootstrap model) (Bowden et al., 2015), weighted median estimator analyses (simple median, weighted median, and Penalised weighted median) (Bowden et al., 2016), and mode based-estimator analyses (weighted mode based-estimator analyses and simple mode based-estimator analyses) (Hartwig et al., 2017). IVW was the primary method to analyze the results because it can provide robust causal estimate even when heterogeneity exists. Due to the requirement that all instrumental variables should meet the MR assumptions in the IVW method, the other methods were used as the complement to IVW. The MR-Egger regression could detect and adjust the pleiotropy, and obtain a causal effect assessment and determine whether directional horizontal pleiotropy is responsible for the results. The weighted median estimator could provide consistent causal assess when more than half of the instrumental variables are valid. The mode based-estimator method can reduce the bias and therefore are less biased than other methods but were less precise. Furthermore, we used IVW methods with MR Egger intercept (Burgess and Thompson, 2017) and Cochran’s Q statistics to assess the pleiotropy and heterogeneity of individual SNPs. As long as the intercept did not significantly differ from 0 (p > 0.05), pleiotropic effects were considered absent. The value of Cochrane’s Q was used to evaluate the heterogeneity. When the p-value was <0.05, the IVW method with multiplicative random-effects model was applied as the primary outcome; otherwise, the IVW method with fixed-effects model was used as the primary outcome. In this study, the F-statistic was applied to assess the strength of the IV–exposure association. F-statistics was calculated as (N-k-1)/k*R2/(1-R2). R2: the cumulative explained variance of selected SNPs on exposure; k: the number of selected SNPs; N: the sample size. In the case of F > 10, the association between IV and exposure was considered strong enough. Moreover, a leave-one-out analysis was conducted to assess the robustness of MR analysis results through any outlier SNP. Referring to the previous study (Zhang et al., 2021), the causal relationship was deemed significant if three conditions were met: 1) The p-value of IVW <0.05.2) There is no difference in the direction of estimates by the IVW, MR-Egger, and weighted median methods. 3) The p-value of MR-Egger intercept test was more than 0.05. We used the ‘TwoSampleMR’ R package for all MR analyses involved in this study. All Statistical analyses were performed by R version 3.4.2 (R Foundation for Statistical Computing, Vienna, Austria), and a two-tailed p-value < 0.05 was statistically significant.
Results
Detailed descriptions of all genetic datasets used in this study are presented in Table 1. As shown in Table 1, the majority F statistics for genetic instruments are greater than 10, therefore, there is less likelihood of weak instrumental bias in this study. As presented in Figure 2 and Supplementary Figure S1, a total of 9 MR methods were performed to analyze the final results. The IVW methods as the primary outcome indicated that there is no causal association between tea consumption and risk of CVD (AF: OR, 0.997, 95% CI, 0.992–1.0001, p = 0.142; hypertension: OR, 0.976, 95% CI, 0.937–1.017, p = 0.242; AMI: OR, 0.996, 95% CI, 0.991–1.000, p = 0.077; CA: OR, 1.001, 95% CI, 0.993–1.009, p = 0.854; PVD: OR, 1.002, 95% CI, 1.000–1.005, p = 0.096; angina: OR, 0.999, 95% CI, 0.993–1.006, p = 0.818; HF: OR, 0.999, 95% CI, 0.996–1.002, p = 0.338), as shown in Figure 2. The other MR analysis method (simple mode, weighted mode, simple median, weighted median, penalized weighted median, MR Egger) were performed as the complement to IVW, confirming the robustness of the IVW analysis results (Figure 2 and Supplementary Figure S1). As summarized in Supplementary Table S8, the pleiotropy and heterogeneity of individual SNPs were examined by IVW methods, MR Egger intercept, and Cochran’s Q statistics. The results of the leave-one-out sensitivity analysis indicated that the association between tea consumption and CVD risk was not substantially driven by any individual SNP (Figure 3). The funnel plot result showed that there was no evidence of obvious heterogeneity across the estimates (Figure 4).
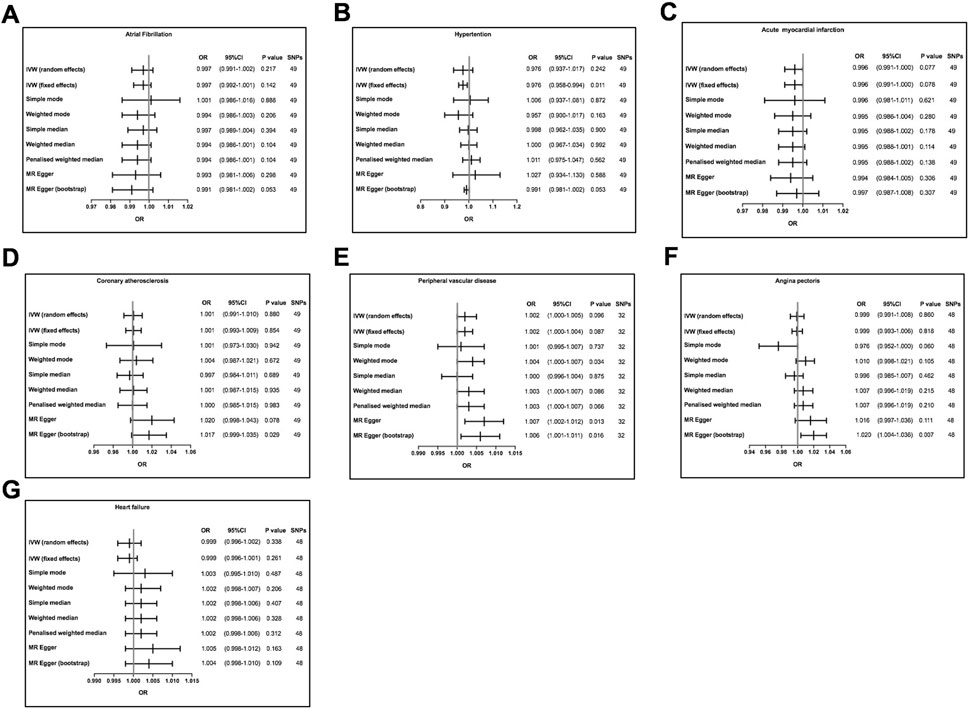
FIGURE 2. Mendelian randomization assessment of the association between tea consumption and the risk of CVD. (A) atrial fibrillation; (B) hypertension; (C) acute myocardial infarction; (D) coronary atherosclerosis; (E) peripheral vascular disease; (F) angina; (G) heart failure. The slope of the straight line indicates the magnitude of the causal association. SNPs, single nucleotide polymorphisms; OR, odds ratio; CI, confidence interval.
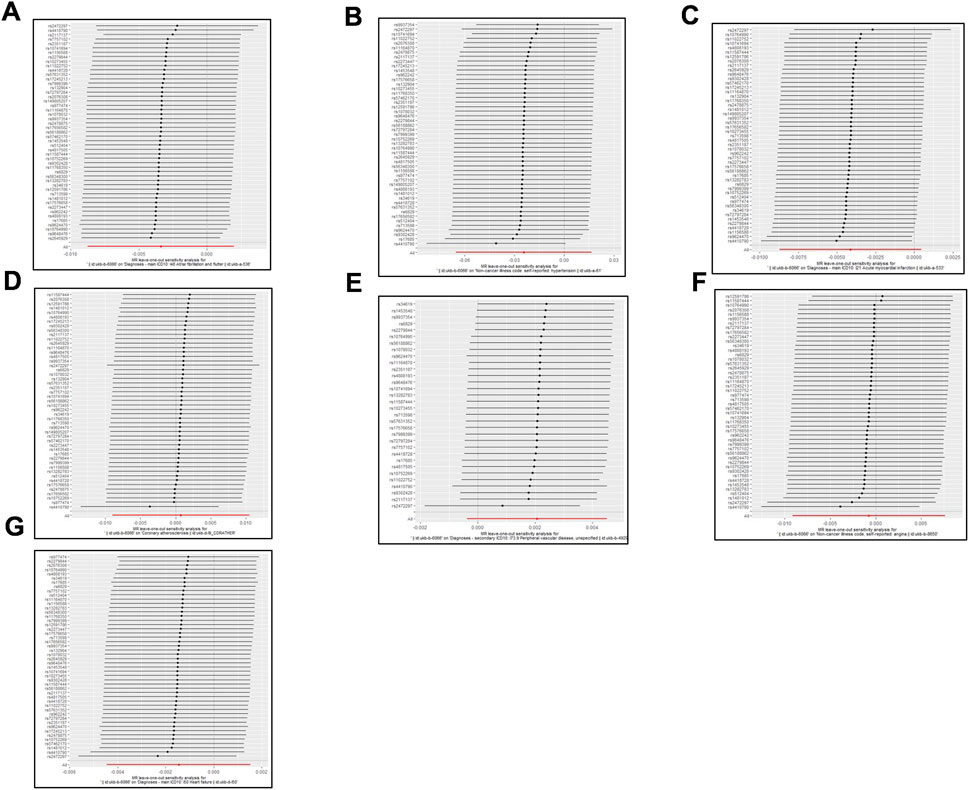
FIGURE 3. MR leave-one-out sensitivity analysis for tea consumption on CVD. (A) atrial fibrillation; (B) hypertension; (C) acute myocardial infarction; (D) coronary atherosclerosis; (E) peripheral vascular disease; (F) angina; (G) heart failure. Circles indicate MR estimates for tea consumption on CVD using inverse-variance weighted fixed-effect method if each SNP was omitted in turn. The bars indicate the CI.
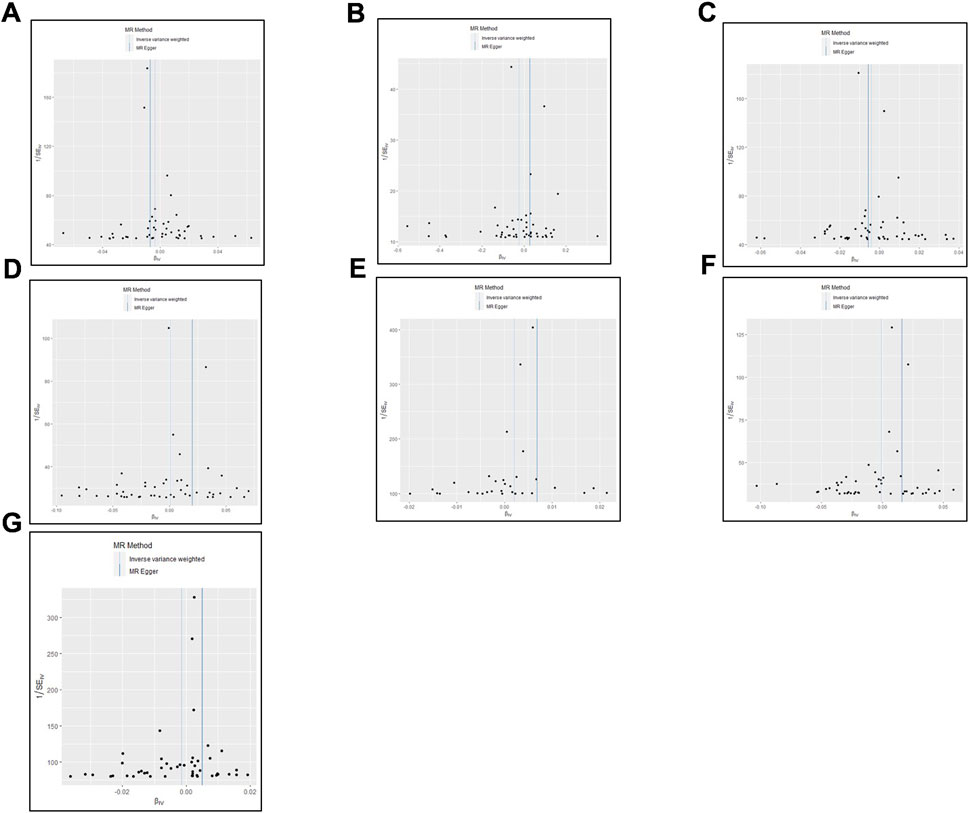
FIGURE 4. The estimation of heterogeneity using Funnel plot. (A) atrial fibrillation; (B) hypertension; (C) acute myocardial infarction; (D) coronary atherosclerosis; (E) peripheral vascular disease; (F) angina; (G) heart failure.
Discussion
In this study, we used up to 9 MR analysis methods to estimate the association between tea consumption and risk of CVD in a large sample size. Our data showed that there is no relationship between tea consumption and the risk of 7 common cardiovascular diseases, including atrial fibrillation, hypertension, acute myocardial infarction, coronary atherosclerosis, peripheral vascular disease, angina, and heart failure.
Due to the popularity of habitual tea intake and the high morbidity of CVD around the world, it is of great significance to clarify the role of tea consumption on CVD. However, previous studies exhibited inconsistent results. There are several possible reasons. First, reverse causality and residual confounding cannot be excluded from previous observational studies. For example, the effect of other anti-oxidative ingredients in food, which have been shown to be associated with the risk of CVD, has not been adjusted in these studies (Rodrigo et al., 2013; Yuan and Larsson, 2019). In addition, compared with people who work during the day, individuals who work night shifts may prefer habitual tea intake because tea drinking may help them improve their attention and work better during the night. Nevertheless, this reverse day/night lifestyle is also a potential confounding of cardiac arrhythmia. Second, the data from previous studies were obtained based on self-reported tea intake. There may exist a misclassification of habitual tea intake. Therefore, the measurement of long-term tea consumption in observational studies may be inaccurate (Liu et al., 2016). Last, in real-world settings, habitual tea-drinking populations are not randomly distributed. It has been influenced to a certain extent by the popularity of tea culture in different areas. It also has a close relationship with age and gender. All of these factors may influence the results of previous observational studies.
The greatest advantage of this study is the two-sample MR study design. MR is a genetic epidemiology design, which can conquer unmeasured confounding and make more robust causal inferences. Thus MR is a particularly powerful approach to access whether an exposure factor has a causation with the development of one disease. In our study, the association between tea consumption and CVD was fully estimated using a total of 9 MR methods in a large sample size. Our work contributes new evidence that there is no relationship between habitual tea intake and risk of CVD. To some extent, our work may helpful in further understanding the effects of habitual tea intake on cardiovascular disease and may useful in guiding the dietary management of patients with CVD.
Of note, there are several inevitable limitations. First, the data in this study was obtained from a European database. Thus the finding might not be applicable in other ethnic groups. Second, the effect of tea type and the amount of intake cannot be evaluated because there was no corresponding information in the database. Third, considering the exposure and outcomes were derived from United Kingdom biobank population, there may be a degree of sample overlap. We do not have a good way to evaluate the overlapping sample size in our study. Population overlapping would increase the possibility of false positives. However, our results are negative. Therefore, population overlapping is unlikely to affect our conclusion.
Conclusion
This MR study suggested that there is no causal relationship between habitual tea intake and risk of CVD.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
JC and DC conceived and designed the research; JC, DC, and YW collected the data and conducted the research; JC analyzed and interpreted the data; DC and JC wrote the initial paper; CJ revised the paper; CJ approved the final version to be submitted. DC had primary responsibility for the final content. All authors read and approved the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgene.2022.989772/full#supplementary-material
References
Bennett, D. A., and Holmes, M. V. (2017). Mendelian randomisation in cardiovascular research: An introduction for clinicians. Heart 103 (18), 1400–1407. doi:10.1136/heartjnl-2016-310605
Bowden, J., Davey Smith, G., and Burgess, S. (2015). Mendelian randomization with invalid instruments: Effect estimation and bias detection through egger regression. Int. J. Epidemiol. 44 (2), 512–525. doi:10.1093/ije/dyv080
Bowden, J., Davey Smith, G., Haycock, P. C., and Burgess, S. (2016). Consistent estimation in mendelian randomization with some invalid instruments using a weighted median estimator. Genet. Epidemiol. 40 (4), 304–314. doi:10.1002/gepi.21965
Burgess, S., and Thompson, S. G. (2017). Interpreting findings from Mendelian randomization using the MR-Egger method. Eur. J. Epidemiol. 32 (5), 377–389. doi:10.1007/s10654-017-0255-x
Chen, Y., Zhang, Y., Yang, H., Ma, Y., Zhou, L., Lin, J., et al. (2022). Association of coffee and tea consumption with cardiovascular disease, chronic respiratory disease, and their comorbidity. Mol. Nutr. Food Res., e2200419. doi:10.1002/mnfr.202200419
Feng, C., Cao, Y., Su, Y., Cai, H., Shu, X. O., Zheng, W., et al. (2021). Association between tea consumption and hypertension risk among middle-aged and older Chinese adults. J. Nutr. 151 (12), 3773–3780. doi:10.1093/jn/nxab293
Hartwig, F. P., Davey Smith, G., and Bowden, J. (2017). Robust inference in summary data Mendelian randomization via the zero modal pleiotropy assumption. Int. J. Epidemiol. 46 (6), 1985–1998. doi:10.1093/ije/dyx102
Igho-Osagie, E., Cara, K., Wang, D., Yao, Q., Penkert, L. P., Cassidy, A., et al. (2020). Short-term tea consumption is not associated with a reduction in blood lipids or pressure: A systematic review and meta-analysis of randomized controlled trials. J. Nutr. 150 (12), 3269–3279. doi:10.1093/jn/nxaa295
Kim, Y., Je, Y., and Giovannucci, E. (2019). Coffee consumption and all-cause and cause-specific mortality: A meta-analysis by potential modifiers. Eur. J. Epidemiol. 34 (8), 731–752. doi:10.1007/s10654-019-00524-3
Lawlor, D. A. (2016). Commentary: Two-sample mendelian randomization: Opportunities and challenges. Int. J. Epidemiol. 45 (3), 908–915. doi:10.1093/ije/dyw127
Liu, D., Yan, J., Wang, Y., Wang, Z., Xie, Z., Ma, Y., et al. (2016). Low-dose green tea intake reduces incidence of atrial fibrillation in a Chinese population. Oncotarget 7 (51), 85592–85602. doi:10.18632/oncotarget.12243
Malasevskaia, I., Al-Awadhi, A. A., and Mohammed, L. (2020). Tea in the morning and khat afternoon: Health threats due to khat chewing. Cureus 12 (12), e12363. doi:10.7759/cureus.12363
Manolis, A. A., Manolis, T. A., Apostolopoulos, E. J., Melita, H., and Manolis, A. S. (2022). The cardiovascular benefits of caffeinated beverages: Real or surreal? "Metron ariston - all in moderation. Curr. Med. Chem. 29 (13), 2235–2260. doi:10.2174/0929867328666210708091709
Nielsen, J. B., Thorolfsdottir, R. B., Fritsche, L. G., Zhou, W., Skov, M. W., Graham, S. E., et al. (2018). Biobank-driven genomic discovery yields new insight into atrial fibrillation biology. Nat. Genet. 50 (9), 1234–1239. doi:10.1038/s41588-018-0171-3
Niu, X. G., Cai, C., Liu, F. C., Li, J. X., Huang, K. Y., Yang, X. L., et al. (2021). Associations of tea consumption with blood pressure progression and hypertension incidence. J. Geriatr. Cardiol. 18 (8), 645–653. doi:10.11909/j.issn.1671-5411.2021.08.004
Rodrigo, R., Korantzopoulos, P., Cereceda, M., Asenjo, R., Zamorano, J., Villalabeitia, E., et al. (2013). A randomized controlled trial to prevent post-operative atrial fibrillation by antioxidant reinforcement. J. Am. Coll. Cardiol. 62 (16), 1457–1465. doi:10.1016/j.jacc.2013.07.014
Roth, G. A., Mensah, G. A., Johnson, C. O., Addolorato, G., Ammirati, E., Baddour, L. M., et al. (2020). Global burden of cardiovascular diseases and risk factors, 1990-2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 76 (25), 2982–3021. doi:10.1016/j.jacc.2020.11.010
Shin, S., Lee, J. E., Loftfield, E., Shu, X. O., Abe, S. K., Rahman, M. S., et al. (2022). Coffee and tea consumption and mortality from all causes, cardiovascular disease and cancer: A pooled analysis of prospective studies from the asia cohort consortium. Int. J. Epidemiol. 51 (2), 626–640. doi:10.1093/ije/dyab161
Voskoboinik, A., Koh, Y., and Kistler, P. M. (2019). Cardiovascular effects of caffeinated beverages. Trends cardiovasc. Med. 29 (6), 345–350. doi:10.1016/j.tcm.2018.09.019
Wang, D., Karvonen-Gutierrez, C. A., Jackson, E. A., Elliott, M. R., Appelhans, B. M., Barinas-Mitchell, E., et al. (2019). Prospective associations between beverage intake during the midlife and subclinical carotid atherosclerosis: The Study of Women's Health across the Nation. PLoS One 14 (7), e0219301. doi:10.1371/journal.pone.0219301
Wang, X., Liu, F., Li, J., Yang, X., Chen, J., Cao, J., et al. (2020). Tea consumption and the risk of atherosclerotic cardiovascular disease and all-cause mortality: The China-PAR project. Eur. J. Prev. Cardiol. 27 (18), 1956–1963. doi:10.1177/2047487319894685
Yuan, S., and Larsson, S. C. (2019). No association between coffee consumption and risk of atrial fibrillation: A mendelian randomization study. Nutr. Metab. Cardiovasc. Dis. 29 (11), 1185–1188. doi:10.1016/j.numecd.2019.07.015
Zhang, Y., Liu, Z., Choudhury, T., Cornelis, M. C., and Liu, W. (2021). Habitual coffee intake and risk for nonalcoholic fatty liver disease: A two-sample mendelian randomization study. Eur. J. Nutr. 60 (4), 1761–1767. doi:10.1007/s00394-020-02369-z
Keywords: tea consumption, causal association, Mendelian randomization (MR), SNPs (single nucleotide polymorphisms), atrial fibrillation
Citation: Cai D, Chen J, Wu Y and Jiang C (2022) No causal association between tea consumption and 7 cardiovascular disorders: A two-sample Mendelian randomization study. Front. Genet. 13:989772. doi: 10.3389/fgene.2022.989772
Received: 08 July 2022; Accepted: 18 November 2022;
Published: 30 November 2022.
Edited by:
Youxin Wang, Capital Medical University, ChinaCopyright © 2022 Cai, Chen, Wu and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jun Chen, MjE4MTgzNTRAemp1LmVkdS5jbg==; Chenyang Jiang, Y3lqaWFuZ0B6anUuZWR1LmNu
†These authors have contributed equally to this work
 Dongsheng Cai
Dongsheng Cai Jun Chen
Jun Chen Yuteng Wu2
Yuteng Wu2