- 1Medical Genetics Center, Maternal and Child Health Hospital of Hubei Province, Wuhan, China
- 2The First Clinical College, Hubei University of Medicine, Shiyan, China
- 3Department of Reproductive Medical Center, Taihe Hospital, Hubei University of Medicine, Shiyan, China
- 4Hubei Key Laboratory of Embryonic Stem Cell Research, School of Basic Medical Sciences, Hubei University of Medicine, Shiyan, China
Objective: This study aims to estimate the maternal age-related risk of Down syndrome in an Asian population.
Methods: We performed a retrospective data analysis including a total of 206,295 pregnant women who presented for second-trimester maternal serum screening for Down syndrome at Hubei Maternal and Child Health Hospital for the years 2008–2017. Cases were assigned to three groups: ≤26 years of age, 27–33 years of age, and ≥34 years of age. The incidence of Down Syndrome was calculated for each age group. The differences between groups were tested using the chi-square (χ2) test.
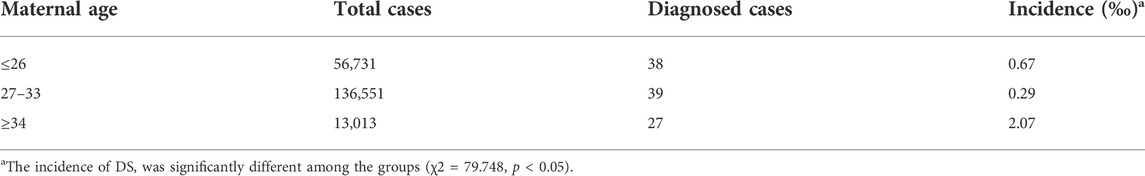
Results: The incidence of Down syndrome in women ≤26 years of age, 27–33 years of age, and ≥34 years of age was 0.67‰, 0.29‰, and 2.07‰ respectively. Statistically significant difference was found between the three age groups (χ2 = 79.748, p < 0.05).
Conclusion: Down syndrome rate was significantly higher in women ≥34 years of age. Younger women (≤26 years of age) had a significantly higher risk for Down’s syndrome, compared to women aged 27–33.
Introduction
Down Syndrome (DS) is the most commonly recognized genetic cause of intellectual disability, which occurs in 3.05 per 10,000 live births in China (Deng et al., 2015; Zhang et al., 2020). Since there is no medical cure for DS, it imposes an enormous financial burden on affected families and the health care system (Chen et al., 2008). The average lifetime economic burden of a new DS case from the family perspective and the societal perspective amounted to US$47,000 and US$55,000, respectively (Luo et al., 2020). People have recognized Down Syndrome, although prenatal screening tests are not mandatory in China, most pregnant women had this test during pregnancy in China.
Advanced maternal age (AMA) is a well-established risk factor for DS and an essential determinant in all prenatal screening strategies (Resta, 2005; Bhaumik et al., 2017; Chen et al., 2020). The association between maternal age distribution and the live birth prevalence of DS has been well documented in American and Europe (McKenzie et al., 2016). However, racial-ethnic differences exist in prenatal diagnostic test use and associated outcomes of AMA (Khoshnood et al., 2000; Khattak et al., 2019). In this study, we estimated the maternal age-related risk of Down syndrome in an Asian population.
Materials and methods
Subjects
We performed a retrospective data analysis including a total of 206,295 pregnant women who presented for second-trimester maternal serum screening for Down syndrome at Hubei Maternal and Child Health Hospital for the years 2008–2017.
Maternal serum screening
For each pregnant woman, 2 ml of maternal peripheral blood was collected and conserved at 4°C after separation of serum. The serum biomarkers, AFP, μE3, and β-HCG were detected by chemiluminescent immunoassay. The TCsoft prenatal screening software was used to calculate the screening risk. Risk = Age-specific Risk*LR (AFP)*LR (β-HCG) *LR (μE3). The initial MOM value was corrected by body weight, race, multiple births, diabetes, and other factors. The cut-off value for DS risk was set at 1:380.
Down syndrome diagnosis
Before 2014, pregnant women with a positive screening result were diagnosed with amniocentesis. After 2014, pregnant women with a positive screening result were diagnosed by amniocentesis or screened by non-invasive prenatal screening (NIPS).
Statistical analysis
All cases were assigned to three groups: ≤26 years of age, 27–33 years of age, and ≥34 years of age. The incidence of Down’s Syndrome was calculated for each age group. The differences between groups were tested using the χ2 test. All the analyses were performed by SPSS 16.0 for Windows (SPSS Inc. Chicago, IL, United StatesUnited States). A p value of <0.05 was considered statistically significant.
Results
The incidence of DS by maternal age
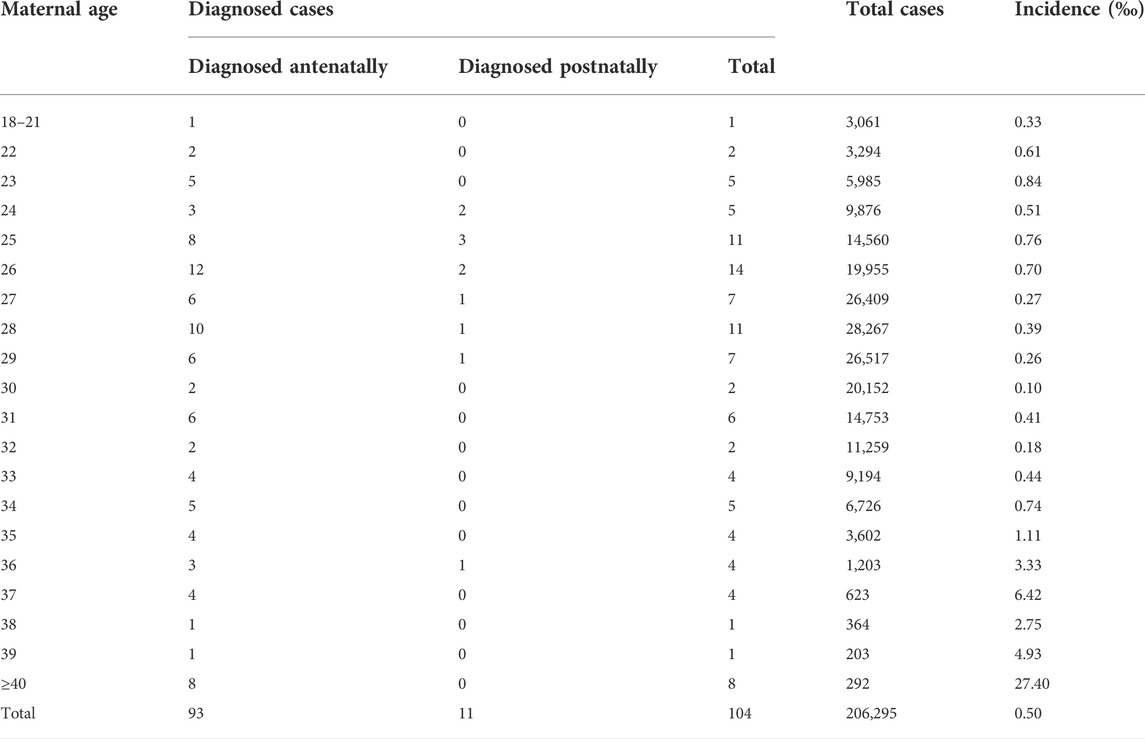
The incidence of DS by maternal age was summarized in Table 1. In a total of 206,295 cases, 13,100 (6.35%) had positive screening tests (DS risk > or = 1:380). 93 (89.4%) fetuses were diagnosed with DS prenatally and 11 (10.6%) fetuses were diagnosed postnatally (these 11 newborns have been genetically confirmed with full/partial trisomy 21 after birth), 78.85% (82/104) of children with Down syndrome are born to women under 35 years of age. (Table 1).
Incidence of Down syndrome by maternal age groups
All cases were assigned to three groups: ≤26 years of age, 27–33 years of age, and ≥34 years of age. The incidence of DS in women ≤26-years of age, 27–33 years of age, and ≥34 years of age was 0.67‰ (38/56,731), 0.29‰ (39/136,551), and 2.07‰ (27/13,013) respectively (Table 2). Statistically significant difference was found between the three age groups (χ2 = 79.748, p < 0.05) (Table 2). Remarkably, the proportion of pregnant women ≤26-years of age was 27.5% (56,731/206,295) and the incidence of DS in this age group is significantly higher than women 27–33 years of age (Table 2).
Discussion
Down syndrome (DS) can occur at any maternal age but the chance of having a child with DS increases over time. It has been well accepted that women over age 35 at delivery are at higher risk for giving birth to a child with DS. In fact, for a long time, advanced maternal age (AMA) has been considered as a sole indication for genetic amniocentesis for definitive prenatal diagnosis (Bornstein et al., 2009; Stomornjak-Vukadin et al., 2015). In our study, the incidence of DS in women over age 34 was significantly higher than in other age groups (Table 2). These data are consistent with previous research (Howe et al., 2000; Morris et al., 2002). Fortunately, women in this age group are usually well informed about the age-associated risk and treated as if they need the level of care necessary for any high-risk pregnancy. Our data showed all diagnoses in this age group were made prenatally except one (Table 1).
A trend has developed worldwide for women to delay childbearing into their late 30 s or early 40 s. In China, at end of October 2015, the one-child policy was replaced by a universal two-child policy. As a result, the proportion of women with AMA at delivery increased by 85.68%, from 8.52% in 2013 to 15.82% in 2017 in Zhejiang province (Zhang et al., 2020). The results of our study, which analyze a population of pregnant women in Hubei province, showed the proportion of women over age 34 was only 6.3% between 2008 and 2017 suggesting that there are considerable variations in the prevalence of AMA across the county (Table 2). Future studies are required to confirm the trend and understand the demographic differences.
Previous studies conclude there is no association between younger maternal age and the risk of DS. However, we found that women under age 26 (18–26) account for nearly 27% of all pregnant women and are more likely to have babies with DS than women aged 26–34 (χ2-14.858 p < 0.01) (Table 2). This is partly due to the increasing availability of more powerful tests, which significantly increased the overall detection rate. Another explanation could be that young mothers lack all awareness of pregnancy and therefore are more likely to engage in risk behaviors such as smoking, drinking, and using illicit drugs that can induce chromosomal non-disjunction (Czeizel, 1990; Sotonica et al., 2016). They are also more likely to be sleep-deprived, have an imbalanced diet to control body weight. Recent studies have identified some genetic predispositions (just as consanguineous marriage, maternal telomere length, maternal MCM9 polymorphisms, maternal Presenilin-1 and Apolipoprotein E polymorphisms) of women that may cause nondisjunction and Down syndrome birth at younger age (Ray et al., 2016; Bhaumik et al., 2017; Ray et al., 2018; Pal et al., 2021). These are age-independent risk factors. Epidemiological risk factors are not only responsible for DS birth to younger mother. In our study, 18.4% (7/38) of DS in women ≤26 years of age are diagnosed postnatally, compared to 7.7 (3/39) in the women aged 26–34 and 3.7% (1/27) in the woman ≥34 years of age (Tables 1,2). In an early study, it predicts that with continued use of prenatal diagnosis among older women, upward of 80% of DS births will occur to younger mothers (Adams et al., 1981; Antonarakis et al., 2020). Our study shows high occurrence of DS in women younger than 26 years. Therefore, much more attention needs to be given to younger mothers. Maternal serum screening for DS and/or NIPT should be routinely performed to all pregnant women. Healthcare professionals need to help them to understand the importance of this screening test and make informed decisions.
Conclusion
The incidence of DS was significantly higher in women ≥34 years of age. Younger women (≤26 years of age) had a significantly higher risk for DS, compared to women aged 27–33. The strengths that Younger women (≤26 years of age) had a significantly higher risk for DS, compared to women aged 27–33. This could help to increase the awareness in these young mothers to prevent the occurrence in other young mothers. Much more attention needs to be given to younger mothers. Maternal serum screening for DS and/or NIPT should be routinely performed to all pregnant women.
Data availability statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding authors.
Author contributions
SJ and ZJ are responsible for clinical diagnosis and treatment. YS, ZZ are responsible for pathological examination. WB and ZT are responsible for genetic testing and thesis writing.
Funding
This work was supported by Hubei Provincial Health and Family Planning Scientific Research Project [Grant # WJ 2018H0137].
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Adams, M. M., Erickson, J. D., Layde, P. M., and Oakley, G. P. (1981). Down's syndrome. recent trends in the United States. JAMA 246 (7), 758–760. doi:10.1001/jama.246.7.758
Antonarakis, S. E., Skotko, B. G., Rafii, M. S., Strydom, A., Pape, S. E., Bianchi, D. W., et al. (2020). Down syndrome. Nat. Rev. Dis. Prim. 6 (1), 9. doi:10.1038/s41572-019-0143-7
Bhaumik, P., Ghosh, P., Ghosh, S., Feingold, E., Ozbek, U., Sarkar, B., et al. (2017). Combined association of Presenilin-1 and Apolipoprotein E polymorphisms with maternal meiosis II error in Down syndrome births. Genet. Mol. Biol. 40 (3), 577–585. doi:10.1590/1678-4685-GMB-2016-0138
Bornstein, E., Lenchner, E., Donnenfeld, A., Barnhard, Y., Seubert, D., and Divon, M. Y. (2009). Advanced maternal age as a sole indication for genetic amniocentesis; risk-benefit analysis based on a large database reflecting the current common practice. J. Perinat. Med. 37 (2), 99–102. doi:10.1515/JPM.2009.032
Chen, Y., Qian, X., Zhang, J., Li, J., Chu, A., and Schweitzer, S. O. (2008). Preliminary study into the economic burden of down syndrome in China. Birth Defects Res. A Clin. Mol. Teratol. 82 (1), 25–33. doi:10.1002/bdra.20409
Chen, Y., Wang, X., Li, L., Lu, S., and Zhang, Z. (2020). New cut-off values for screening of trisomy 21, 18 and open neural tube defects (ONTD) during the second trimester in pregnant women with advanced maternal age. BMC Pregnancy Childbirth 20 (1), 776. doi:10.1186/s12884-020-03464-z
Czeizel, A. (1990). A case-control analysis of the teratogenic effects of co-trimoxazole. Reprod. Toxicol. 4 (4), 305–313. doi:10.1016/0890-6238(90)90042-t
Deng, C., Yi, L., Mu, Y., Zhu, J., Qin, Y., Fan, X., et al. (2015). Recent trends in the birth prevalence of down syndrome in China: Impact of prenatal diagnosis and subsequent terminations. Prenat. Diagn. 35 (4), 311–318. doi:10.1002/pd.4516
Howe, D. T., Gornall, R., Wellesley, D., Boyle, T., and Barber, J. (2000). Six year survey of screening for Down's syndrome by maternal age and mid-trimester ultrasound scans. BMJ 320 (7235), 606–610. doi:10.1136/bmj.320.7235.606
Khattak, M. T., Supriyanto, E., Aman, M. N., and Al-Ashwal, R. H. (2019). Predicting Down syndrome and neural tube defects using basic risk factors. Med. Biol. Eng. Comput. 57 (7), 1417–1424. doi:10.1007/s11517-019-01969-0
Khoshnood, B., Pryde, P., Wall, S., Singh, J., Mittendorf, R., and Lee, K. S. (2000). Ethnic differences in the impact of advanced maternal age on birth prevalence of down syndrome. Am. J. Public Health 90 (11), 1778–1781. doi:10.2105/ajph.90.11.1778
Luo, W., He, B., Han, D., Yuan, L., Chen, X., Pang, L., et al. (2020). A retrospective analysis of different contingent screening models for fetal down syndrome in southwestern China. Sci. Rep. 10 (1), 9457. doi:10.1038/s41598-020-66320-2
McKenzie, K., Milton, M., Smith, G., and Ouellette-Kuntz, H. (2016). Systematic review of the prevalence and incidence of intellectual disabilities: current trends and issues. Curr. Dev. Disord. Rep. 3 (2), 104–115. doi:10.1007/s40474-016-0085-7
Morris, J. K., Mutton, D. E., and Alberman, E. (2002). Revised estimates of the maternal age specific live birth prevalence of Down's syndrome. J. Med. Screen. 9 (1), 2–6. doi:10.1136/jms.9.1.2
Pal, U., Halder, P., Ray, A., Sarkar, S., Datta, S., Ghosh, P., et al. (2021). The etiology of Down syndrome: Maternal MCM9 polymorphisms increase risk of reduced recombination and nondisjunction of chromosome 21 during meiosis I within oocyte. PLoS Genet. 17 (3), e1009462. doi:10.1371/journal.pgen.1009462
Ray, A., Hong, C. S., Feingold, E., Ghosh, P., Ghosh, P., Bhaumik, P., et al. (2016). Maternal telomere length and risk of Down syndrome: Epidemiological impact of smokeless chewing tobacco and oral contraceptive on segregation of chromosome 21. Public health genomics 19 (1), 11–18. doi:10.1159/000439245
Ray, A., Oliver, T. R., Halder, P., Pal, U., Sarkar, S., Dutta, S., et al. (2018). Risk of Down syndrome birth: Consanguineous marriage is associated with maternal meiosis-II nondisjunction at younger age and without any detectable recombination error. Am. J. Med. Genet. A 176 (11), 2342–2349. doi:10.1002/ajmg.a.40511
Resta, R. G. (2005). Changing demographics of advanced maternal age (AMA) and the impact on the predicted incidence of Down syndrome in the United States: Implications for prenatal screening and genetic counseling. Am. J. Med. Genet. A 133A (1), 31–36. doi:10.1002/ajmg.a.30553
Sotonica, M., Mackic-Djurovic, M., Hasic, S., Kiseljakovic, E., Jadric, R., and Ibrulj, S. (2016). Association of parental age and the type of down syndrome on the territory of Bosnia and Herzegovina. Med. Arch. 70 (2), 88–91. doi:10.5455/medarh.2016.70.88-91
Stomornjak-Vukadin, M., Kurtovic-Basic, I., Mehinovic, L., and Konjhodzic, R. (2015). Combined use of cytogenetic and molecular methods in prenatal diagnostics of chromosomal abnormalities. Acta Inf. Med. 23 (2), 68–72. doi:10.5455/aim.2015.23.68-72
Zhang, X., Chen, L., Wang, X., Wang, X., Jia, M., Ni, S., et al. (2020). Changes in maternal age and prevalence of congenital anomalies during the enactment of China's universal two-child policy (2013-2017) in Zhejiang Province, China: An observational study. PLoS Med. 17 (2), e1003047. doi:10.1371/journal.pmed.1003047
Keywords: down syndrome, maternal serum screening, advanced maternal age (AMA), Asian population, Hubei China
Citation: Song Y, Jieping S, Tianshu Z, Zhijun Z, Jingxuan Z and Bo W (2022) Incidence of Down Syndrome by maternal age in Chinese population. Front. Genet. 13:980627. doi: 10.3389/fgene.2022.980627
Received: 28 June 2022; Accepted: 02 August 2022;
Published: 25 August 2022.
Edited by:
Sujay Ghosh, University of Calcutta, IndiaReviewed by:
Hala El-Bassyouni, National Research Centre (Egypt), EgyptEmilia Severin, Carol Davila University of Medicine and Pharmacy, Romania
Copyright © 2022 Song, Jieping, Tianshu, Zhijun, Jingxuan and Bo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhang Zhijun, emhhbmd6aGlqdW5AdGFpaGVob3NwaXRhbC5jb20=; Zhang Jingxuan, NDIyNzI5NTk0QHFxLmNvbQ==; Wang Bo, d2FuZ2JvMTAwNUAxNjMuY29t
 Yi Song1
Yi Song1 Zhou Tianshu
Zhou Tianshu Zhang Jingxuan
Zhang Jingxuan Wang Bo
Wang Bo