
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Genet. , 20 December 2019
Sec. ELSI in Science and Genetics
Volume 10 - 2019 | https://doi.org/10.3389/fgene.2019.01209
This article is part of the Research Topic Educating Health Professionals in Genomic Medicine: Evidence-Based Strategies and Approaches View all 13 articles
The potential of genomic medicine in improving the quality of healthcare both at population and individual-level is well-recognized globally. However, successful adoption of genetic and genomic evidence into clinical practice depends on training the healthcare workforce and clinical researchers in genomic medicine. Due to limited expertise in the medical genetics and genomics field, widespread uptake largely depends on task-shifting for the implementation of genomic medicine implementation to key healthcare professionals such as nurses. Their knowledge would be developed through courses aimed at professional development. Globally, trainers, and training initiatives in genomic medicine are in early stages of development, but resource limited settings such as the African continent face additional logistical and institutional challenges. The African Genomic Medicine Training (AGMT) Initiative was conceived during a combined conference of the African Society of Human Genetics (AfSHG) and the Human Heredity and Health in Africa Consortium (H3Africa) in 2016, Senegal, in response to the needs for developing knowledge and skills in genomic medicine. AGMT was established to implement a sustainable genomic medicine training initiative primarily for healthcare professionals who are not geneticists but are nurses, doctors, and pharmacists in Africa. This paper reports on the establishment of the AGMT initiative and the strategies developed and piloted by this initiative in designing and implementing an accredited frame-work and community-based blended learning course for nurses across 11 African countries. The global implementation experiences, outcomes and lessons learnt are highlighted. The AGMT initiative strategy takes advantage of existing research consortia and networks to train and create a pool of trainers and has adopted evidence-based approaches to guide curriculum and content development/adaptation. This initiative established the first Africa-wide online blended learning genomic medicine course which forms the basis from which to develop courses for other healthcare professionals and the wider public.
Historically, knowledge translation of genomic knowledge for healthcare in Africa has been challenged by the dearth of genomic data from people of recent African origin (Popejoy and Fullerton, 2016). However, recent initiatives such as the Human, Heredity, and Health in Africa Consortium (H3Africa) (Dandara et al., 2014a; Rotimi et al., 2014), H3ABioNet (Mulder et al., 2016), and MalariaGen (Achidi et al., 2008) aim to build capacity for genomics research in Africa, and are challenging the existing norms (Gurdasani et al., 2015). Cumulating results from genomic projects of human health and disease projects are helping explain African-specific susceptibility and variability in disease severity to conditions such as kidney-related diseases (Cooper et al., 2017) and sickle cell disease (SCD) (Pule et al., 2015). The application of genomics information in optimizing treatment has given rise to development of pharmacogenomics-based dosing of antiretroviral therapy (ART) (Dandara et al., 2014b; Skelton et al., 2014). Large-scale genomic characterization of African populations holds great promise for identification of additional health-linked genetic variants relevant to the understanding of possible genomic drivers of the high burden of infectious diseases and the growing prevalence of noncommunicable diseases in Africa (Wonkam and Mayosi, 2014; Tekola-Ayele and Rotimi, 2015). Therefore, in anticipation of the changing African genomic landscape, there is an urgent need for strategies to translate this genomic knowledge into clinical practice and augment clinical decisions.
Efforts to translate genomics into clinical practice face a number of barriers which include limited resources to sequence and characterize human genomes from African populations. In addition, there is lack of access to next generation technologies and analytical capabilities in Africa and, policies that are silent on genetics and genomics and medical curricula that are not adequate in teaching genetics/genomics concepts, leading to limited appreciation of the utility of genomic knowledge in healthcare (Wonkam et al., 2006; Muzoriana et al., 2017). In addition, African countries lack the critical mass of experts in genetics, genomics, data science, and bioinformatics required to implement country-specific genomic medicine driven healthcare. For example, South Africa is the only African country with a critical mass of skilled genetic counsellors and medical geneticists, key personnel for the implementation of genomic medicine (Abacan et al., 2019).Therefore, cost-effective strategies are urgently required to promote incorporation of genomics research and findings in healthcare in Africa for quality health outcomes. Most of the developed world is moving to adopting genomics in its health care programs, however, Africa is still lagging behind, a trend that will continue to widen existing health disparities between developed and developing countries.
Globally, several introductory genomic medicine courses have been developed and implemented, tailored for specific healthcare workers such as nurses (Nembaware et al., 2016), and other healthcare professionals (https://www.genomicseducation.hee.nhs.uk). However, several of the genomic medicine curricula are characterized by numerous shortcomings, which include limited development of competencies in a systematic manner. Mapping and alignment of curricula and competencies are slowly being integrated into genomics curricula development (Jenkins et al., 2015). Competencies in genomics and genetics for nurses are publicly available online (Jenkins and Calzone, 2007; Kirk et al., 2014), a noteworthy competency resource was developed by the Inter-Society Coordinating Committee for Physician Education in Genomics (ISCC) based on five "Entrustable Professional Activities" EPAs (Korf et al., 2014). Another short-coming of most existing genomic medicine curricula is the limited application of well-established curriculum development frameworks such as the Kern's six step model (Kern and Thomas, 2009). This model is a widely used systematic curriculum development approach which links curricula to healthcare needs and promotes continual curriculum monitoring and evaluation (Khamis et al., 2016). This model has the added advantage of being adaptable to suit the needs of the implementers (Khamis et al., 2016).
The existing publicly available genomic medicine curricula require tailoring of competencies and content for the African context due to the continent's diverse cultures, disease burdens, and healthcare facilities and resources. In addition, reported challenges from an informal online survey in training genetics and genomics highlight lack of expertise, and lack of resources and funds (https://training.h3abionet.org/AGMC_2016/outputs/). To address the highlighted training needs and establish a foundation for genomic medicine in the region, the African Genomic Medicine Training Initiative (AGMT) was initiated to pool expertise and resources from across Africa to develop a training program for African healthcare professionals, which could be further tailored across the diverse countries. The goals of the AGMT initiative are to:
● establish a comprehensive, adaptable and coordinated genomic medicine curriculum and training plan for Africa;
● develop distributed model/flagship training programs based on the curricula;
● establish genomic medicine critical quality indicators to assess competency levels of healthcare professionals in Africa; and
● establish a monitoring and evaluation system to capture the rate of adoption of the curriculum once developed and to track trainees
This article focuses only on the curriculum development objective of the AGMT and outlines the steps taken in the development and implementation of the genomic medicine curriculum, firstly targeted at nurses in Africa. The article demonstrates how the AGMT initiative adapted the Kern's six-step model for the development of a medical curriculum. In addition, the Kern's six-step model was modified to incorporate a competency mapping approach developed by the International Society of Computational Bioinformatics (ISCB) (Mulder et al., 2018). Formal medical educational programs have aims and goals that are often not clearly articulated and, in some instances, poorly understood by key constituents inside and outside of the formal education system (Kern and Thomas, 2009). Using a model/framework to develop the curriculum helps clarify aims and objectives around which the curriculum is structured (Kern and Thomas, 2009). The curriculum becomes the official documentation that includes the goals of teaching and learning; the instructional methods and materials as well as the assessment. The curriculum reflects the envisaged aspirations of society as well as the curriculum that is ultimately implemented. This helps the newly trained medical educators meet the needs of their students, patients, and other key stakeholders. The use of a framework to guide the development of genomic medicine training for Africa also presents an opportunity to implement formal evaluations and studies to share lessons and to learn from.
A workshop aimed at establishing AGMT initiative was conducted during a combined conference of the African Society for Human Genetics and H3Africa Consortium in Senegal, May 2016, and was attended by over 80 participants. The workshop was used to plan and initiate the Kern's six-step approach for designing medical education curricula, which guided development of the AGMT nurse curriculum. Steps included conducting a general needs assessment, followed by specific needs of targeted learners, defining goals and objectives, determining the educational strategies, planning the implementation, and developing an evaluation plan (Kern and Thomas, 2009). The specific needs of targeted learners and defining goals and objectives of the training was guided by the competency mapping strategy from the ISCB (Mulder et al., 2018). Key results from each step are outlined below:
During the AGMT establishment workshop, general needs for new approaches which promote community-based genomic medicine training in Africa were solicited and deliberated by the members present. Data and information generated from this workshop provided the foundation of a survey which was conducted online and advertised through various mailing lists. The survey was conducted to solicit gaps and needs in genomic medicine training from a broad representation of 33 stakeholders and from 19 African countries (https://training.h3abionet.org/AGMC_2016/wp-content/uploads/2017/01/TrainingSurveyAfrica-Upload.pdf). In addition, monthly planning meetings were held to refine the training strategy, develop the curriculum and map competencies, and plan and implement the pilot.
From this multiapproach general needs assessment, several gaps were identified which included: limited and not up-to-date curriculum content, lack of expertise in training in genomic medicine relevant fields such as genomics and genetics; and lack of training resources at the various institutes and limited funding. To address these challenges and gaps, the strategy included short courses, which may be developed further into diploma level content, graduate and postgraduate programs for healthcare and research professionals. Training would also target patients, especially those who plan on being advocates in the genetics and genomics fields. Public engagement activities could also be implemented to align with the training developed for healthcare professionals and patients. Figure 1 illustrates some of the key trainees AGMT could target in the near future. In addition to healthcare workers, it is important to engage/train patients and the general public in genomic medicine. A website (https://training.h3abionet.org/AGMC_2016/) and mailing list were created to facilitate seamless communication. This was made possible through support from the H3Africa Consortium's H3ABioNet, a pan-African bioinformatics network which focuses on genomics capacity development (http://h3abionet.org).
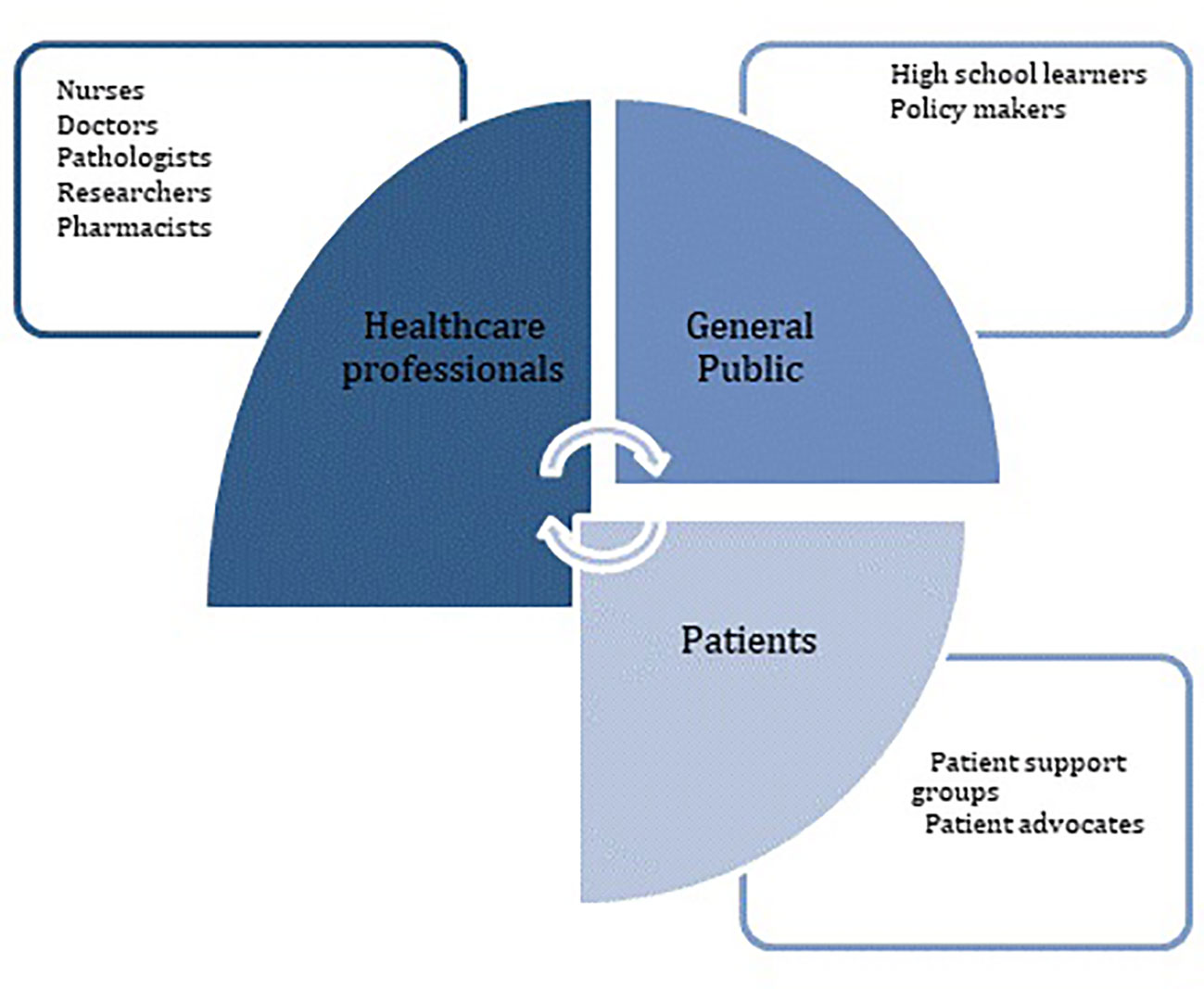
Figure 1 Illustration of key target trainees in genomic medicine for AGMT in the near future. Healthcare workers, patients, and the general public.
This step aims to embed the specific training needs of targeted learners and identify specific stakeholders for the curriculum development, implementation, and evaluation. AGMT engaged with the nurse professors/lecturers, recent graduates, and the Global Research Nurses forum to identify specific needs of the nursing community. An article was published on the Global Health Nurses portal (https://globalresearchnurses.tghn.org/articles/preparing-genomic-medicine-nurse-training-africa/) which summarized existing nurse training and highlighted the role of nurses in Africa. In a similar fashion to the ISCB strategy developed for a Bioinformatics curriculum, four nurse personas were created to make explicit the nurses' current roles and their training needs and targeted outcomes in genomic medicine (Table 1). Nurses at different professional levels developed the initial personas and their roles based on the common nurse specializations in Africa. We had a professor in nursing who has worked and trained nurses from several different African countries. The team agreed to work with four personas as they were a convenient number that was perceived to be sufficient to capture common nurse roles in different contexts across the continent. Although the effectiveness of the four personas in informing the curriculum might need to be probed the future, it is believed that convenient sampling used, that is small in scale and purposively selected on the basis of crucial criteria, was deemed appropriate by the team and allowed us to focus on our purpose (Punch, 2005). Based on roles of nurses highlighted by the nurse personas and feedback from nurses it became clear that the course needed to emphasize practical application of content into students' current settings and roles using problem-based learning with clinical case studies relevant to Africa. This strategy was critical to highlight the relevance of the course to current clinical practice and increase uptake. In addition, skills in genetic counseling, community engagement, ethical conduct in research, inclusion of genetics and genomics in patient care, and development of health promotion material which included relevant genetics/genomic material were also found to be required. There was also a need to address stigmas and misconceptions of genetics and genomics commonly found in African communities.
In general, the course aims to support improved genetics and genomics knowledge, attitudes and skills for: research nurses in the biomedical field or those aspiring to be research nurses; specialist nurses working in the genomics/genetics field and general nurse practitioners in their day to day duties, or recent graduates. The overall objectives for the nurse personas were to develop and implement a plan of care for patients that incorporates genetic and genomics knowledge and is sensitive to individual and cultural preferences, practices and norms by offering basic genetic counseling to patients and families, and conducting genomics research that is ethical and appropriate to the nurses' context.
Competencies were adapted from the ISCC competency portal (https://genomicseducation.net/competency) to suit the needs of the African continent and these were mapped to the nurse personas in one face to face workshop, Google documents, and several online meetings. The mapping of ISCC to the AGMT nurse competencies were not retained due to numerous rounds of editing. The AGMT competency mapping team was split into three groups to review the personas and map competencies. Two personas were reviewed by two groups only instead of three. Consensus was agreed during monthly meetings, after face to face discussions and via Google docs. Once the targeted competencies had been established, the Bloom's taxonomy was used to determine the most appropriate level for a specific nurse by several competency mapping teams (see Table 2) for each persona. The final recommended competency to target is indicated in the last column in Table 2 and was arrived upon after the three competency mapping teams (each team's competency level mapping is colour coded in Table 2) had reached a consensus.
This step involves planning the content to be taught and the educational methods to be used. Content was mainly adapted from a genomic medicine curriculum developed by Health Education England to upskill United Kingdom's National Health Service healthcare professionals, in readiness for the implementation of genomic approaches through the 100k Genomes project (https://www.genomicseducation.hee.nhs.uk/; https://www.genomicsengland.co.uk/about-genomics-england/the-100000-genomes-project/). Assessments were adapted to align to the specific competencies identified in step 3. Table 3 provides a brief description of the final course modules, full details are available on the AGMT website (https://training.h3abionet.org/AGMC_2016/). The four modules varied in length depending on the number of classes they had. Each class was allocated 1 week with contact sessions which lasted around 2 h. Student centered approaches that encourages integration of prior and current experiences were deemed most suitable to facilitate learning for working adults. By selectively drawing on elements of problem-based and project-based learning this enabled the use of real-life questions, a challenge or problem as educational strategies to facilitate the development of knowledge (Lennon et al., 2019). Therefore, several case studies relevant to African health were sourced from the various working group members and embedded in the course material and class assessments. These types of teaching methods are often used for training of health-care professionals as they get students to engage with self-directed learning and offer opportunities for facilitation by the instructor (Kaufman and Holmes, 1996; Kaufman and Holmes 1998).
Learning activities such as quizzes, online discussions on the University of Cape Town's learning management system Vula (powered by Sakai), preclass exercises, and postclass assignments were developed in alignment with indicative content and competencies for each lesson. In addition, the range of learning activities was structured to enable students to actively engage and apply their knowledge and thus promote student-centered learning and flipped class learning (Goh and Ong, 2019). Furthermore, exercises and assessments were made relevant to the participants' context as it required participants to produce resources such as generate a list of genetics and genomics resources and services available at their institutes to make it easier for them to refer their patients.
Classes were required to submit a collaborative research project at the end of the course. which aimed to promote collaborative development of publishable research and reviews, and the assignments could be submitted to a special collection in a specific journal. However, classes were also free to choose not to publish their work or publish in a separate journal. The initial plan was for the course to run over six months, however the formatting of class projects into manuscripts continued after the course had concluded and this exercise varied across the different classes.
Each classroom is managed by a facilitator who ensures the lectures are played, the class is linked up to the live sessions, and facilitates the interactive activities. We had a brief three-week training for facilitators in three areas; online facilitation; face to face group facilitation; and facilitation of role plays required for genetic counseling. Trainers were asked to develop slides based on the indicative content provided and the aligned competencies and assigned levels. This was a negotiated process.
An electronic advertisement was circulated via several mailing lists to advertise the course, see Figure 2. Almost 30 different sites applied to host a classroom for the course, however 19 classes were chosen based on their meeting the requirements to provide stable internet connectivity, a qualified facilitator in genetics and hardware that could handle hosting webinars. The coordinator advertised the training extensively via social media, the chosen class facilitators were also required to recruit participants in their areas/regions. The course was open to qualified and practising African-based nurses and it ran from April to August in 2017 with a weekly contact session every Wednesday.

Figure 2 Flier circulated widely across various mailing list to attract the first cohort of trainees.
A distributed blended online classroom approach, similar in structure to the Structured Training for African Researchers (STARS) Career development course which was developed through the Association of Commonwealth Universities (https://www.acu.ac.uk/focus-areas/early-careers/structured-training-for-african-researchers/) and was recently adopted and adapted by the H3ABioNet Introduction to Bioinformatics Training course (Gurwitz et al., 2017), was used for the training. For the virtual classroom approach, trainers were required to prerecord their material, which was then loaded onto a learning management system, in this case – Vula (Sakai based). Facilitators of the various classes were then required to download the course material onto local storage devices such as hard drives to avoid relying on internet connectivity during the live weekly contact sessions. The facilitators and learners watched the videos within the physical classrooms distributed across Africa before the 1-h long online contact session with the trainers. The online live sessions were made possible via a webinar platform. During these live sessions, only one connection was allowed from each class via the facilitator. The class could then pose questions via the facilitators. Figure 3 summarizes the distributed classroom approach.
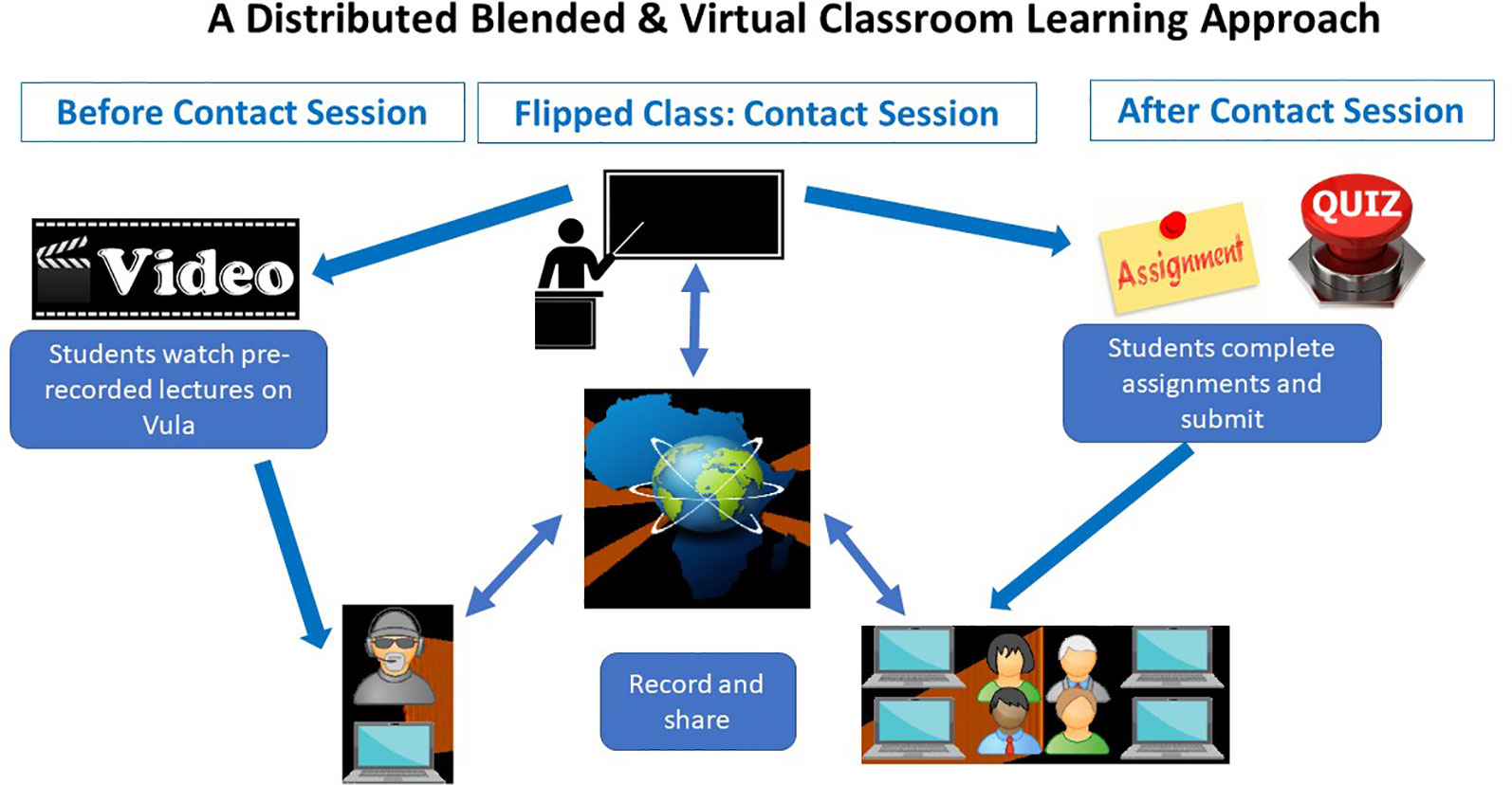
Figure 3 A summary of how the training is conducted using the distributed virtual classroom and blended learning approach. At least 7 days before the face to face sessions, participants can download videos from Vula and watch before class and do preclass exercises. During class (face to face sessions), participants engage with learning material (videos, lectures, etc) during face to face classrooms predownloaded by a facilitator. The class can then connect with the trainer virtually for a question and answer session. Participants also submit a quiz and rate the class. After class participants submit an assignment.
All facilitators were encouraged to obtain accreditation from relevant bodies across Africa for continued professional development points (CPD). While the initial plan was to obtain accreditation from all affiliated universities for this course as a short course, this was not feasible and therefore the short course accreditation was only obtained from the University of Cape Town. During the first implementation of the project, facilitators were also tasked with marking the qualitative and face to face assessments such as role plays.
Two types of assessments were designed for the participants, namely summative and formative analysis (Taras, 2005). Formative assessments included the prelesson exercises which were posted on the Vula discussion forum for all to comment, assess, and give feedback. These prelesson exercises aimed to facilitate the students to acquire key skills or understand concepts that the lesson was targeting to address as required for flipped classes (Riddell et al., 2017). Facilitators also used these preclass exercises to gauge general understanding of the concepts by the participants. In addition, feedback forms were sent to participants after each lesson for the participants to rate content, trainers, and logistics. Classes were also required to submit their research proposals for review by the coordinator and the AGMT working group after lessons on research proposal development. AGMT working group members volunteered to assist/review class proposals that aligned with their own research interests. The summative assessment included the participants completing a knowledge, attitude, perceptions, and practices survey during registration to gauge knowledge at baseline. The same survey was administered at the end of the course and will be administered again 24 months after completion of the course. The summative assessment also included assignments and quizzes given to participants after each lesson. Once the research proposals had been approved by the AGMT working group members, as part of the summative assessment each class was required to write a research report which made up 30% of the students' final marks.
In addition to the participant focused assessments, the overall course's implementation process was also evaluated in order to:
● Understand factors influencing motivation of nurses to sign up for a genomic medicine training course.
● Investigate implementation fidelity, challenges and successes experienced by the facilitators (as described in Step 5).
● Monitor attendance registers and statistics for access to the Vula platform.
The data collection surveys were adapted from literature and used to collect data for each of the assessment strategies highlighted above (McCann et al., 2007; Muzoriana et al., 2017). The participant's assessment strategy and overall implementation evaluation of the project was submitted for review by the Ethics Approval Committee University of Cape Town, Faculty of Health Sciences Ethics Review board.
To facilitate a rapid and informed adoption of genomic medicine into routine clinical care in Africa, Continuous Professional Development (CPD) training and formal higher education for healthcare professionals requires radical transformation suitable for low resource settings. Lack of or inappropriate training could delay the translation of the emerging information from several capacity building efforts in genomics and genetics into quality healthcare (Wonkam and Mayosi, 2014; Weitzel et al., 2016). However, instead of being deterred by the challenges and gaps rampant in Africa, the AGMT course was created to pool resources and expertise across the continent and beyond to provide training for healthcare professionals in genomic medicine which would not have been possible through a single institute or initiative.
While a more thorough evaluation of this program is currently ongoing, preliminary results suggest that this is a feasible model. During the first iteration of the course, 368 applications were received, and 225 participants enrolled into the course from 19 Classrooms in 11 Countries. 35% of the participants completed the course and obtained a certificate of completion of the short course from the University of Cape Town. A special collection was set up by the AGMT to which classes submitted their class projects as manuscripts in this peer-reviewed journal http://gheg-journal.co.uk/2018/05/advancing-genomic-medicine-globally/. So far, one, one class published their class project the special collection. The second iteration of the course is still ongoing.
Nurses are frontline workers in most healthcare facilities in Africa and have access to in-depth knowledge of the patients, families, and communities (Prows et al., 2005). There has been an ongoing debate on whether genetic counselling should only be done by professionally trained genetic counselors or if nurses can receive extra training to enable them to provide basic genetic counseling as a component of their current role (Barr et al., 2018). Based on recent review of 10 articles, Barr et al. (2018) confirmed that nurses already provide genetic counseling, as highlighted by the nurse personas development in this study. However, the provision of genetic counseling by nurses is not standardized. There are calls for formal recognition of the nurses' counseling role and the provision of training to support this task. Because of the lack of genetic counselors on the continent (Abacan et al., 2019) and limited resources to train and employ genetic counselors widely in addition to low job creation for genetic counselors low (Kromberg et al., 2013), providing training in genomics and genetics to nurses who can provide basic genetic counseling seems like a feasible strategy to increase the availability of genetic counseling in Africa.
The importance of establishing a set of core competencies to guide the development of skills, knowledge and attitudes required to deliver safe and effective healthcare is well established (Korf et al., 2014). Competencies in genomics and genetics for nurses have been developed and are publicly available online. However, the alignment of existing curricula to such competencies remains limited or is probably reported poorly. The slow rate of curricula modifications in Europe and America has been largely attributed to lack of implementing personnel and difficulties in operationalization of long and complicated competency lists (Jenkins and Calzone, 2007). Noteworthy, is that developing continents including Africa have been largely underrepresented in such competency development initiatives or curricula development initiatives (Jenkins and Calzone, 2007; Korf et al., 2014). This may be partly due to outdated and static curricula which make the alignment with competencies very difficult because it cannot respond appropriately to societal challenges and needs (Gonzalo et al., 2017).
The draft curriculum and competency map provided from this work are likely to promote increased adoption and adaptation of the genomic medicine training into existing nursing curricula across nurse training colleges and centers across Africa. The embedding of online/distance learning modules into formal university/college training has been demonstrated for various massive online open courses (MOOCs). Although MOOCS were originally developed as stand-alone training to be accessed by university students outside of regular curriculum (Swinnerton et al., 2017), when embedded in university medical curriculum, participants have reported high satisfaction on MOOC sourced-course material (Aboshady et al., 2015). Guidelines would need to be developed to facilitate the inclusion of the AGMT modules into existing university curriculum as done by de Jong et al. (de Jong et al., 2019) for the MOOCs.
Another immediate goal of AGMT is to design training for other healthcare workers such as doctors, pharmacists, clinical scientists, patients, and the general public (e.g., patient support groups). The pilot training program and experiences of the process provides a foundation for the group to develop a toolkit for designing and implementing training for other healthcare workers and possibly offering tailored modules across different professions to reflect the multidisciplinary approach in healthcare systems. Unlike other continents/countries such as Europe (Paneque et al., 2016), Australia (McEwen et al., 2013), and Canada (Ferrier et al., 2013) where bodies have been established to standardize the genetic counseling competencies, where genetic counselors and genetic nurses can register/be certified, most countries in Africa do not yet have certification or registration systems or guidelines to advise on training and practice standards for genomic medicine. The AGMT initiative provides a unique opportunity to be a springboard for development by partnering with existing professional bodies, and by extending training activities to other healthcare professionals.
To our knowledge, this is the first large-scale community-based training initiative for genomic medicine that has been conducted across Africa. This study highlights the importance of societies and consortia in developing a rigorous training program and a pool of trainers and resources for emerging areas such as genomic medicine.
All datasets generated for this study are included in the article/supplementary material.
Approval was not required according to the study format and local legislation. The paper reports on the implementation of a training program and does not contain personal information.
VN and NM developed the first manuscript draft. AGMT members who edited or contributed to the manuscript are listed in alphabetical order in the Appendix. Their role in the project is noted in the first column. Members of the planning team (Kuda Majada, Minnet Cotzee, Faisal Fadlelmola, Pedro Fernandes, Samar Kamal Kassim, Cordelia Leisegang, Ebony Madden, Alice Matimba, Oyekanmi Nash, Michael Pepper, Fouzia Radouani, Raj Ramesar, Michelle Skelton) were responsible for the course development and organization.
NM is supported by the National Human Genome Research Institute (NHGRI) and the Office of The Director (OD), the National Institutes of Health under award numbers U41HG006941 and U24HG006941. VN is supported by NIH/NHLBI U24HL135600. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We thank Dr Maria Giovanni for reviewing the article and Jennifer Troyer for helping with strategy.
Abacan, M., Alsubaie, L., Barlow-Stewart, K., Caanen, B., Cordier, C., Courtney, E., et al. (2019). The global state of the genetic counseling profession. Eur. J. Hum. Genet. 27, 183–197. doi: 10.1038/s41431-018-0252-x
Aboshady, O. A., Radwan, A. E., Eltaweel, A. R., Azzam, A., Aboelnaga, A. A., Hashem, H. A., et al. (2015). Perception and use of massive open online courses among medical students in a developing country: multicentre cross-sectional study. BMJ Open 5, e006804. doi: 10.1136/bmjopen-2014-006804
Achidi, E. A., Agbenyega, T., Allen, S., Amodu, O., Bojang, K., Conway, D., et al. (2008). A global network for investigating the genomic epidemiology of malaria. Nature 456, 732–737. doi: 10.1038/nature07632
Barr, J. A., Tsai, L. P., Welch, A., Faradz, S. M. H., Lane-Krebs, K., Howie, V., et al. (2018). Current practice for genetic counselling by nurses: an integrative review. Int. J. Nurs. Pract. 24, e12629. doi: 10.1111/ijn.12629
Cooper, A., Ilboudo, H., Alibu, V. P., Ravel, S., Enyaru, J., Weir, W., et al. (2017). APOL1 renal risk variants have contrasting resistance and susceptibility associations with African trypanosomiasis. eLife 6, e2546. doi: 10.7554/eLife.25461
Dandara, C., Huzair, F., Borda-Rodriguez, A., Chirikure, S., Okpechi, I., Warnich, L., et al. (2014a). H3Africa and the African life sciences ecosystem: building sustainable innovation. Omi. A J. Integr. Biol. 18, 733–739. doi: 10.1089/omi.2014.0145
Dandara, C., Swart, M., Mpeta, B., Wonkam, A., Masimirembwa, C. (2014b). Cytochrome P450 pharmacogenetics in African populations: implications for public health. Expert Opin. Drug Metab. Toxicol. 10, 769–785. doi: 10.1517/17425255.2014.894020
de Jong, P. G. M., Pickering, J. D., Hendriks, R. A., Swinnerton, B. J., Goshtasbpour, F., Reinders, M. E. J., et al. (2019). Twelve tips for integrating massive open online course content into classroom teaching. Med. Teach. 1–5. doi: 10.1080/0142159X.2019.1571569
Ferrier, R. A., Connolly-Wilson, M., Fitzpatrick, J., Grewal, S., Robb, L., Rutberg, J., et al. (2013). The establishment of core competencies for canadian genetic counsellors: validation of practice based competencies. J. Genet. Couns. 22, 690–706. doi: 10.1007/s10897-013-9651-x
Goh, C. F., Ong, E. T. (2019). Flipped classroom as an effective approach in enhancing student learning of a pharmacy course with a historically low student pass rate. Curr. Pharm. Teach. Learn. 11, 621–629. doi: 10.1016/j.cptl.2019.02.025
Gonzalo, J. D., Haidet, P., Papp, K. K., Wolpaw, D. R., Moser, E., Wittenstein, R. D., et al. (2017). Educating for the 21st-century health care system. Acad. Med. 92, 35–39. doi: 10.1097/ACM.0000000000000951
Gurdasani, D., Carstensen, T., Tekola-Ayele, F., Pagani, L., Tachmazidou, I., Hatzikotoulas, K., et al. (2015). The African Genome Variation Project shapes medical genetics in Africa. Nature 517, 327–332. doi: 10.1038/nature13997
Gurwitz, K. T., Aron, S., Panji, S., Maslamoney, S., Fernandes, P. L., Judge, D. P., et al. (2017). Designing a course model for distance-based online bioinformatics training in Africa: the H3ABioNet experience. PloS Comput. Biol. 13, e1005715. doi: 10.1371/journal.pcbi.1005715
Jenkins, J., Calzone, K. A. (2007). Establishing the essential nursing competencies for genetics and genomics. J. Nurs. Scholarsh. an Off. Publ. Sigma Theta Tau Int. Honor Soc Nurs. 39, 10–16. doi. 10.1111/j.1547-5069.2007.00137.x
Jenkins, J., Calzone, K. A., Caskey, S., Culp, S., Weiner, M., Badzek, L. (2015). Methods of genomic competency integration in practice. J. Nurs. Scholarsh. an Off. Publ. Sigma Theta Tau Int. Honor Soc Nurs. 47, 200–210. doi: 10.1111/jnu.12131
Kaufman, D. M., Holmes, D. B. (1996). Tutoring in problem-based learning: perceptions of teachers and students. Med. Educ. 30, 371–377. doi. 10.1111/j.1365-2923.1996.tb00850.x
Kaufman, D. M., Holmes, D. B. (1998). The relationship of tutors’ content expertise to interventions and perceptions in a PBL medical curriculum. Med. Educ. 32, 255–261. doi. 10.1046/j.1365-2923.1998.00158.x
Kern, D. E., Thomas, PA, H. M. (2009). Curriculum Development for Medical Education: A Six-Step Approach Baltimore, MD: The John’s hopkins University Press.
Khamis, N. N., Satava, R. M., Alnassar, S. A., Kern, D. E. (2016). A stepwise model for simulation-based curriculum development for clinical skills, a modification of the six-step approach. Surg. Endosc. 30, 279–287. doi: 10.1007/s00464-015-4206-x
Kirk, M., Tonkin, E., Skirton, H. (2014). An iterative consensus-building approach to revising a genetics/genomics competency framework for nurse education in the UK. J. Adv. Nurs. 70, 405–420. doi: 10.1111/jan.12207
Korf, B. R., Berry, A. B., Limson, M., Marian, A. J., Murray, M. F., O’Rourke, P. P., et al. (2014). Framework for development of physician competencies in genomic medicine: report of the Competencies Working Group of the Inter-Society Coordinating Committee for Physician Education in Genomics. Genet. Med. 16, 804–809. doi: 10.1038/gim.2014.35
Kromberg, J. G. R., Wessels, T.-M., Krause, A. (2013). Roles of genetic counselors in South Africa. J. Genet. Couns. 22, 753–761. doi: 10.1007/s10897-013-9606-2
Lennon, O., Phelan, D., Wallace, D., King, J., Barrett, T. (2019). The more you did, the more it made sense: problem-based learning to improve early evidence-based practice in an undergraduate physiotherapy professional programme. Physiother. Res. Int. 24, e1774. doi: 10.1002/pri.1774
McCann, S., MacAuley, D., Barnett, Y., Bunting, B., Bradley, A., Jeffers, L., et al. (2007). Cancer genetics: consultants? Perceptions of their roles, confidence and satisfaction with knowledge. J. Eval. Clin. Pract. 13, 276–286. doi: 10.1111/j.1365-2753.2006.00695.x
McEwen, A. R., Young, M. A., Wake, S. A. (2013). Genetic counseling training and certification in Australasia. J. Genet. Couns. 22, 875–884. doi: 10.1007/s10897-012-9567-x
Mulder, N. J., Adebiyi, E., Alami, R., Benkahla, A., Brandful, J., Doumbia, S., et al. (2016). H3ABioNet, a sustainable pan-African bioinformatics network for human heredity and health in Africa. Genome Res. 26, 271–277. doi: 10.1101/gr.196295.115
Mulder, N., Schwartz, R., Brazas, M. D., Brooksbank, C., Gaeta, B., Morgan, S. L., et al. (2018). The development and application of bioinformatics core competencies to improve bioinformatics training and education. PloS Comput. Biol. 14, e1005772. doi: 10.1371/journal.pcbi.1005772
Muzoriana, N., Gavi, S., Nembaware, V., Dhoro, M., Matimba, A. (2017). Knowledge, attitude, and perceptions of pharmacists and pharmacy students towards pharmacogenomics in zimbabwe. Pharm. (Basel Switzerland) 5, 36. doi: 10.3390/pharmacy5030036
Nembaware, V., Mulder, N., Ramesar, R. (2016). Article: preparing for genomic medicine nurse training in africa - global research nurses. Glob. Res. Nurses Netw.https://globalresearchnurses.tghn.org/articles/preparing-genomic-medicine-nurse-training-africa/. Available at: [Accessed October 24, 2016].
Paneque, M., Moldovan, R., Cordier, C., Serra-Juhé, C., Feroce, I., Lambert, D., et al. (2016). Development of a registration system for genetic counsellors and nurses in health-care services in Europe. Eur. J. Hum. Genet. 24, 312–314. doi: 10.1038/ejhg.2015.234
Popejoy, A. B., Fullerton, S. M. (2016). Genomics is failing on diversity. Nature 538, 161–164. doi: 10.1038/538161a
Prows, C. A., Glass, M., Nicol, M. J., Skirton, H., Williams, J. (2005). Genomics in nursing education. J. Nurs. Scholarsh. 37, 196–202. doi. 10.1111/j.1547-5069.2005.00035.x
Pule, G. D., Ngo Bitoungui, V. J., Chetcha Chemegni, B., Kengne, A. P., Antonarakis, S., Wonkam, A. (2015). Association between variants at bcl11a erythroid-specific enhancer and fetal hemoglobin levels among sickle cell disease patients in cameroon: implications for future therapeutic interventions. OMICS 19, 627–631. doi: 10.1089/omi.2015.0124
Riddell, J., Jhun, P., Fung, C.-C., Comes, J., Sawtelle, S., Tabatabai, R., et al. (2017). Does the flipped classroom improve learning in graduate medical education?. J. Grad. Med. Educ. 9, 491–496. doi: 10.4300/JGME-D-16-00817.1
Rotimi, C., Abayomi, A., Abimiku, A., Adabayeri, V. M., Adebamowo, C., Adebiyi, E., et al. (2014). Research capacity. Enabling the genomic revolution in Africa. Science 344, 1346–1348. doi: 10.1126/science.1251546
Skelton, M. M., Kampira, E. E., Wonkam, A. A., Mhandire, K. K., Kumwenda, J. J., Duri, K. K., et al. (2014). Frequency variation among sub-Saharan populations in virus restriction gene, BST-2 proximal promoter polymorphisms: implications for HIV-1 prevalence differences among African countries. OMICS 18, 461–471. doi: 10.1089/omi.2013.0127
Swinnerton, B. J., Morris, N. P., Hotchkiss, S., Pickering, J. D. (2017). The integration of an anatomy massive open online course (MOOC) into a medical anatomy curriculum. Anat. Sci. Educ. 10, 53–67. doi: 10.1002/ase.1625
Taras, M. (2005). Assessment - Summative and Formative - Some Theoratical reflections. Br. J. Educ. Stud. 53:4, 466–478. doi: 10.1111/j.1467-8527.2005.00307.x
Tekola-Ayele, F., Rotimi, C. N. (2015). Translational genomics in low- and middle-income countries: opportunities and challenges. Public Health Genomics 18, 242–247. doi: 10.1159/000433518
Weitzel, K. W., Alexander, M., Bernhardt, B. A., Calman, N., Carey, D. J., Cavallari, L. H., et al. (2016). The IGNITE network: a model for genomic medicine implementation and research. BMC Med. Genomics 9, 1. doi: 10.1186/s12920-015-0162-5
Wonkam, A., Mayosi, B. M. (2014). Genomic medicine in Africa: promise, problems and prospects. Genome Med. 6, 11. doi: 10.1186/gm528
Wonkam, A., Njamnshi, A. K., Angwafo, F. F. (2006). Knowledge and attitudes concerning medical genetics amongst physicians and medical students in Cameroon (sub-Saharan Africa). Genet. Med. 8, 331–338. doi: 10.109701.gim.0000223542.97262.21
Keywords: genomic medicine, Africa, precision medicine, training, nurses, competencies, Kern's six step model
Citation: Nembaware V, African Genomic Medicine Training Initiative and Mulder N (2019) The African Genomic Medicine Training Initiative (AGMT): Showcasing a Community and Framework Driven Genomic Medicine Training for Nurses in Africa. Front. Genet. 10:1209. doi: 10.3389/fgene.2019.01209
Received: 07 August 2019; Accepted: 01 November 2019;
Published: 20 December 2019.
Edited by:
Sylvia Ann Metcalfe, Murdoch Childrens Research Institute (MCRI), AustraliaReviewed by:
Christine Patch, Genomics England, United KingdomCopyright © 2019 Nembaware, African Genomic Medicine Training Initiative and Mulder. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nicola Mulder, bmljb2xhLm11bGRlckB1Y3QuYWMuemE=; Victoria Nembaware, dm5lbWJhd2FyZUBnbWFpbC5jb20=
†Full list of contributing members is available in Appendix
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.