
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Ecol. Evol. , 27 September 2016
Sec. Conservation and Restoration Ecology
Volume 4 - 2016 | https://doi.org/10.3389/fevo.2016.00112
This article is part of the Research Topic Triage in Conservation View all 11 articles
Conservation triage seems to be at a stalemate between those who accept triage based on utilitarian rationalization, and those that reject it based on a number of ethical principles. We argue that without considered attention to the ethics of conservation triage we risk further polarization in the field of conservation. We draw lessons from the medical sector, where triage is more intuitive and acceptable, and also from disaster planning, to help navigate the challenges that triage entails for conservation science, practice, and policy. We clarify the consequentialist, deontological, and virtue ethical stances that influence the level of acceptance of triage. We emphasize the ethical dimensions of conservation triage in principle and in practice, particularly in the context of stakeholder diversity, a wide range of possible objectives and actions, broader institutions, and significant uncertainties. A focus on a more diverse set of ethics, more considered choice of triage as a conservation tool, open communication of triage objectives, and protocols, greater consideration of risk preferences, and regular review and adaptation of triage protocols is required for conservation triage to become more acceptable among diverse conservation practitioners, institutions, and the general public. Accepting conservation triage as fundamentally an ethical problem would foster more open dialog and constructive debate about the role of conservation triage in a wider system of care.
Triage (derived from the French word, trier, to sort) is essentially the process of making difficult decisions regarding priority under severely constrained resources (financial, knowledge or time; Weinerman et al., 1966; Aacharya et al., 2011). This simplistic definition does not however capture the ethical challenges of triage. In resource-limited contexts, triage decisions “sacrifice” the needs of a few, resource-intensive, critical cases so that resources can be distributed to a greater number of less critical cases, i.e., for “the greater good”. In the biodiversity conservation sector, triage has been interpreted as allowing some critically endangered species to go extinct in order to save others (Jachowski and Kesler, 2009). This interpretation has led conservation triage to be a poignantly controversial issue (Hagerman et al., 2010) with people either promoting triage, accepting the concept but being uncomfortable with its application, or resisting it (Colyvan and Steele, 2011; Hagerman and Satterfield, 2014).
Conservation triage is promoted by those that accept it typically through reference to the rationality of triage as a system for decision-making (Bottrill et al., 2008). The often-inadequate budgets for conservation (Balmford et al., 2003; McCarthy et al., 2012) and the predicted impacts of global change (Rudd, 2011; Hagerman and Satterfield, 2014) suggest that conditions that incite the need to prioritize conservation actions given resource constraints (referred to herein as the triage context) are often unavoidable. From this point of view, triage is seen as a rational (and even inevitable) approach to prioritization under resource scarcity (Bottrill et al., 2009), although taken often with moral discomfort (Hagerman and Satterfield, 2014). Interestingly, the need for prioritization more generally is typically not contested (Hagerman et al., 2010; Hagerman and Satterfield, 2014), unanimously seen as better than decision-making strategies of “no prioritization” or ad hoc prioritization that is not guided by an explicit decision-making system (Martin et al., 2012). Proponents of conservation triage typically cite a utilitarian reasoning for its justification: maximizing benefits given resource constraints, even if this means that some species may be sacrificed in order for resources to be more efficiently distributed.
The position against conservation triage is less singular. On one hand, conservation triage is berated as submission to a “defeatist” ethic, which fails to incentivize for or even recognize opportunities to increase budgets or develop innovative solutions to mitigate extinction (Noss, 1996; Pimm, 2000; Parr et al., 2009). The notion of sacrificing the most critically endangered species is also viewed as a slippery slope to accepting extinction (Pimm, 2000; Hagerman et al., 2010), for example as part of the opportunity costs of development (Noss, 1996; Jachowski and Kesler, 2009). Accepting triage is seen as a contradiction to conserving all biodiversity, which is inherently an ethical consideration for the conservation movement more broadly.
Here, we do not argue the relative merits of conservation triage; these have been discussed in the existing literature (Bottrill et al., 2008). Rather, we argue that the ethical basis of conservation triage have been treated superficially to date. This is epitomized by the suggestion that the inevitability of conservation triage contexts makes triage immune from ethical considerations (Bottrill et al., 2008). While conservation triage contexts may be largely inevitable, decision theory itself does not inform what objective ought to be maximized, for whom, or how (Wilson et al., 2009), and therefore whether prioritization will involve sacrifice of the most critical cases (i.e., triage). The criteria and process under which resources are allocated are clearly ethically laden, and current conservation triage often sits at odds with society preferences (Wilson et al., 2011) and moral ideals (Hagerman et al., 2010; Hagerman and Satterfield, 2014).
We argue that conservation science, practice, and policy requires a deeper understanding of ethical motivations for and implications of triage, as well as a greater appreciation of the differences between triage in principle and in practice. These advances are required in order to more fully appreciate the benefits and limitations of conservation triage and to effectively communicate these to stakeholders and the general public. To illustrate, we draw on the ethical principles that underpin triage in emergency medicine. The concept of triage is central to emergency medicine, including within hospitals and in field settings, and is rarely questioned by patients, practitioners, or institutions (FitzGerald et al., 2010; Aacharya et al., 2011; Pou, 2013), to the point of being intuitively implemented (FitzGerald et al., 2010). Our aim is to contrast the concept and practice of triage in emergency medicine and conservation in order to discern why it is more accepted in medicine yet polarized in conservation, and to identify areas in conservation triage that may benefit from further research attention.
Acceptance or resistance of triage as a normative concept can essentially be characterized as the realization of fundamentally different ethical principles. Broadly speaking, those in favor of conservation triage take a consequentialist ethical reasoning (the objective of maximizing benefit), and those that resist triage take a deontological or virtue ethical stance (Figure 1; the objective of not wanting to “sacrifice” species). However, it is also possible to oppose conservation triage on consequentialist grounds (e.g., disagreement that resources for conservation are limited), or to oppose the implementation of triage if the triage protocol is controversial (e.g., disagreement of the calculated “benefits” of particular actions). The important difference is in the reasoning behind the arguments, and what this might suggest as a solution to the impasse: for example, the triage protocol might be adjusted to placate stakeholders or the solution might need to address parameters of the problem at larger institutional scales.
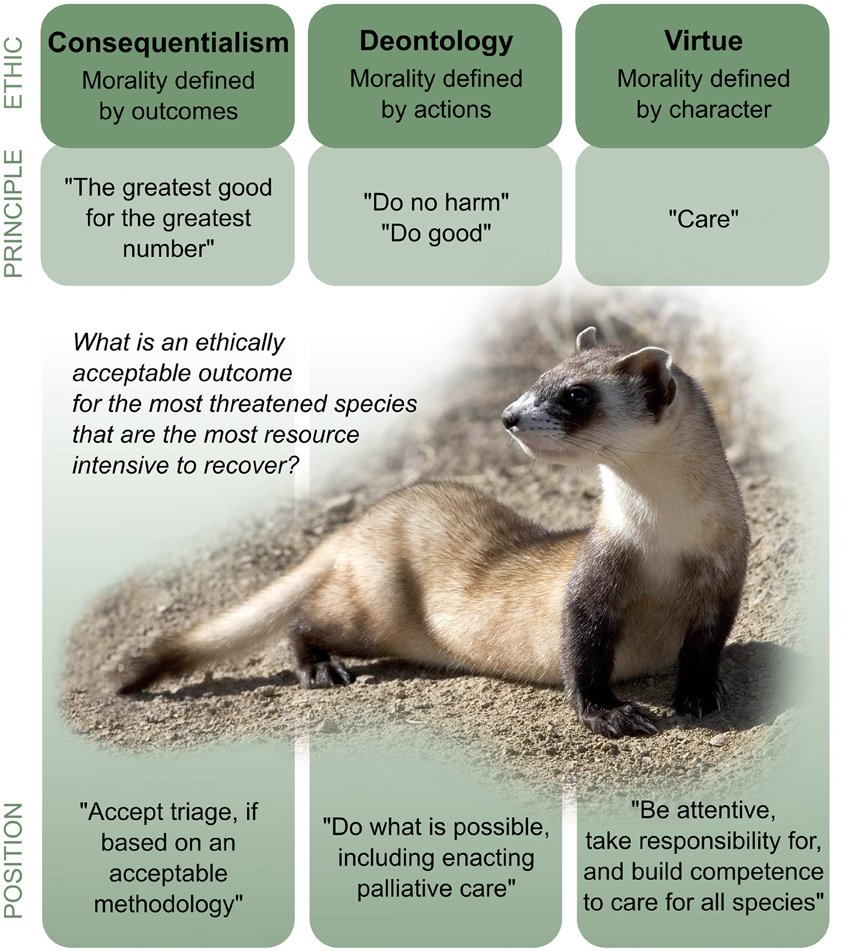
Figure 1. Possible ethical stances in relation to conservation triage. Example principles are given, which may lead to different positions on the triage of critically endangered species, such as the black-footed ferret. Outcomes that may be drawn from these positions are contingent on the context and dependent on subjective interpretations.
Acceptable triage protocols likely consider multiplicit concepts of distributive justice. Distributive justice is the process of balancing the principles of equality, utility and need, in order to derive equitable distributions (see below), principles which may draw influence from consequentialist, deontological, or virtue ethics. Further, triage systems will differ according to traditions, cultures, social contexts, and religious beliefs (Bodansky, 2009). These varied contexts mean that the situation illustrated by Figure 1, which is predominantly based only on Western philosophical divisions, is in reality much more complex. No ethical reasoning or moral stance based on logical arguments and truths are necessarily “better” or “worse”, or more “right” or “wrong” than others. Even within one triage protocol, triers (the individuals conducting triage) may differ substantially in their classifications (Fernandes et al., 1999; Göransson et al., 2006; FitzGerald et al., 2010). This emphasizes the need for triage systems to reflect and better accommodate possible diverse ethical perspectives.
The principle of equality derives from the deontological principle that each person's life is equal. A focus on equality in triage might be interpreted as allocation on a first-come first-serve basis. This is unlikely to deliver an optimal strategy for the efficient use of scarce resources (it may, for example, result in a greater burden for many). However, the principle of equality can also be interpreted as an equal opportunity to receive care. A central tenet of emergency medicine triage is that no patient is excluded or given preferential treatment, despite how difficult this may be in practice (Ten Have, 2014). In conservation, the principle of equality is contradicted by the fact that species are functional components of ecosystems, that we “use” species every day, and typically we value resources more when they are scarce (Balmford et al., 2011). In developing conservation triage protocols the relative emphasis on equality, utility, and need has to be decided.
The principle of utility confers that we should achieve the greatest good for the greatest number, though there may be many objectives with which to achieve this (for instance maximizing benefit, minimizing harm, or maximizing likelihood of success), and many metrics for which to measure “good”. In medical practice, the benefit metric is somewhat limited as pertaining to human life and happiness, resting on the premise that all humans have an intrinsic value. In conservation the choice of benefit metric is less constrained. The benefit metric may include, for example, measures of extinction or persistence, species richness or phylogenetic diversity, the use or non-use values of species, the contribution of the species to ecosystem processes, functions, and health (Faith, 2009; Probert et al., 2011; Arponen, 2012; Bennett et al., 2015; Redding and Mooers, 2015), and the intrinsic values of nature that are held by some (Justus et al., 2009). The wide selection of available metrics has given rise to controversy, but critical use of metrics has the potential to moderate the ethical implications of triage.
The principle of need entails prioritizing the ones that are worst-off. Focussing on need reflects pity, or a desire for retribution (or guilt) for injury caused (i.e., reparation or restorative justice). In conservation, criteria to define “need” are poorly defined. Is it the most threatened, most urgent, most damaged by humans? Or is it the most “salvageable”? This relates to a general lack of data and knowledge about “symptoms” and what these mean for prognoses in treated and untreated systems. This challenge is different from emergency medicine, as while patients are typically similar and similar symptoms tend to similar prognoses and outcomes, species and ecosystems are more diverse. A population size of 10 may mean a very different prognosis regarding extinction for a long-lived bog turtle than a pygmy rabbit (Shoemaker et al., 2013). A distinction also must be made between the urgency and severity of conditions, as urgent conditions may not necessarily be severe and severe conditions may not necessarily be urgent (Hobbs and Kristjanson, 2003). These knowledge gaps suggest a need to deliberate and consider a wide variety of evidence when developing triage protocols in conservation.
In medicine, a respect for autonomy focuses on the democratic right of the patient to make choices regarding their own care, including informed consent for both evaluation and treatment (Aacharya et al., 2011). This principle is often not given priority, however, given the urgency of emergency situations and the likelihood that patients will lack the capacity to give prior consent. Without dismissing the need for respect for autonomy, emergency medical situations compensate for loss of autonomy though open communication, including information regarding wait times and treatment effects (Aacharya et al., 2011).
In conservation, the principle of respect for autonomy may be extended to considering who the stakeholders are (to ensure recognitional equity) and ensuring their right to participate in decision-making is respected (to achieve procedural equity). Considerations include deliberation on who is qualified to “speak for nature” (O'Neill et al., 2006) and what inherent rights different components of biodiversity ought to have (Sandler, 2014). While the need for recognitional and procedural equity is gaining traction in conservation prioritization (Bennett and Dearden, 2014), these concepts have not featured with respect to triage per-se (Rudd, 2011; Hagerman and Satterfield, 2014). Involving stakeholders to develop prioritization protocols and objectives may increase acceptance of decisions in conservation triage contexts, by forcing participants to recognize the benefits, costs, feasibility, and uncertainty of different actions (Conde et al., 2015).
The principle of non-maleficence (“do no harm”) and beneficence (“do or promote good”) focuses attention in emergency medicine triage on providing care, rather than only considering efficient use of resources (Aacharya et al., 2011). In the broader system of health care these principles also enact the need for preventative medicine to reduce the need for symptomatic care, and palliative care for cases with an imminent inevitability of death (Hobbs and Kristjanson, 2003; Pou, 2013). Here, it becomes evident of the small, but important role that triage systems play in a wider system of medical healthcare (Figure 2): triage systems themselves typically aim to facilitate the initiation of further assessment and treatment, but do not typically concern resources for that further care (FitzGerald et al., 2010).
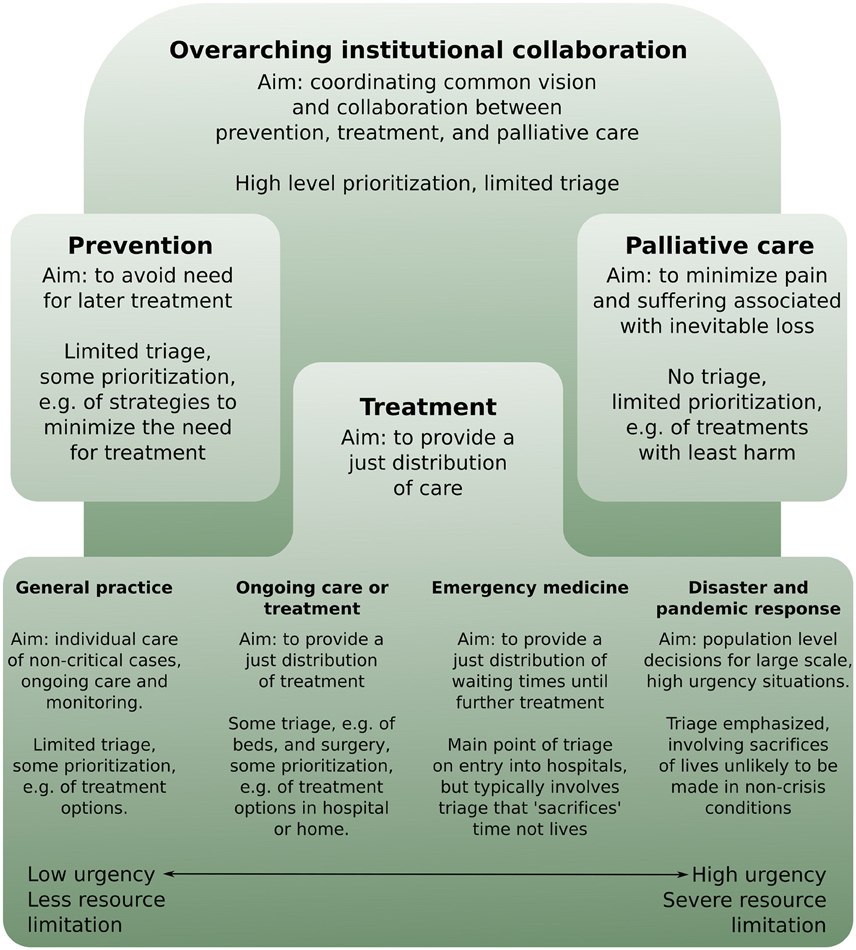
Figure 2. Triage decisions (here defined as prioritization that may involve sacrifice of some critical but resource intensive cases so these resources can be allocated to “the greater good”) can be understood as just one element in a wider system of care. Here we illustrate how triage decisions in medicine are typically concentrated in disaster and pandemic responses, and, albeit with different aims, in emergency medicine, but play a much less emphasized role in other sectors of the wider system of care.
Applications of conservation triage have typically been more ambitious. However, if the medical model is to be followed, triage should be seen as just one element in the conservation toolbox, to be enacted at specific times, within specific contexts, and with a carefully defined objective. This will require different types of care in conservation to be clarified, including what might constitute “preventative” and “palliative care”, and when these different categories of care should be enacted (Hobbs and Kristjanson, 2003). For example, preventative care in conservation could relate to habitat improvements and controlling threatening processes, while palliative care could relate to taking remaining individuals from a species into captive breeding or storing seed or genetic material when species become functionally extinct (Sandler, 2014; Conde et al., 2015). Many species and ecosystems are now perceived to be reliant on conservation actions in perpetuity (Wiens et al., 2012). “Chronic” conditions such as these are typically are not dealt with in an emergency medicine triage situation; instead institutional strategies are aimed at reducing crowding in emergency rooms, and limiting the need for triage in the first case (Aacharya et al., 2011).
Situating conservation triage within a wider system of care would also necessitate greater coordination and collaboration among individuals and institutions working toward a “common vision” that encompasses a range of ethical stances (Sexton et al., 2010). We envisage that like in medicine, a coordinated system of care would help, for example, “top-down” policy makers and on-ground practitioners to understand the scope and role of their duties within a larger context of care. For instance, it may clarify urgent and resource-limited contexts where triage is a pragmatic process, from contexts where other systems of prioritization that need not involve the sacrifice of the most critical cases. The latter may include exploring how budgets or other resources may be expanded, or enacting novel interventions (Pimm, 2000; Parr et al., 2009; Cundill et al., 2012).
Triage in practice needs to account for uncertainty and the limits of knowledge, of both the trier and the triage protocol (Parr et al., 2009). Medicine has a greater history of being evidence-based (Ahmad et al., 2014), and as human patients are more alike than differing species, such evidence is more readily transferred between patients. This means there is a higher level of certainty in regard to what different “symptoms” may mean for both diagnosis and prognosis in medicine, compared to conservation. This higher level of uncertainty means risk profiles ought to be more emphasized in conservation prioritization (Auerbach et al., 2015). Large uncertainties may indicate a greater role for deontological, rule-based ethical systems, rather than relying solely on a consequentialism perspective. Triage assessment protocols also need to be updated regularly as conditions change, values shift and new knowledge and technology arises (Aacharya et al., 2011).
To achieve optimal delivery of care and to maximize patient safety, triage processes in emergency medicine seek to minimize under-triage (to reduce preventable morbidity and mortality) while keeping over-triage low (to enhance efficiency; Uleberg et al., 2007; Lehmann et al., 2009; Xiang et al., 2014; Shawhan et al., 2015). The temptation to over-triage is often exaggerated when long wait times may result in increased harm (Aacharya et al., 2011), if there is emotional involvement or high possibility of litigation (Pou, 2013), or if there is institutional or financial incentive to do so (FitzGerald et al., 2010). The conservation sector must also be cognizant about such conditions that may lead to incorrect or undesirable triage decisions. This necessitates being critical of the data and information available, seeking baseline information and supporting the evaluation of actions that are implemented (Miteva et al., 2012).
The basic premise of triage in emergency medicine is that we should preserve and protect as many human lives as possible by assigning priority to patients with an immediate need for life-sustaining treatment. The scale of the conservation problem could however be more accurately reflected by triage decisions faced in disaster or pandemic contexts. Pandemic and disaster triage are characterized by sudden onset and overwhelming resource scarcity, and with larger scales and longer timeframes than in emergency medicine contexts. A feature that conservation shares with disaster triage is a shift in focus from management of individuals to populations (Aacharya et al., 2011; O'Mathúna et al., 2014; Ten Have, 2014).
Disaster triage conditions typically require more “hard” decisions to be made, that is, decisions that demand consideration of sacrifice of human life for “the greater good”. Sacrifices that could be avoidable, and would, under normal circumstances, not be made (O'Mathúna et al., 2014). In reality, these challenging triage decisions mean that efforts in disaster contexts are often far from being optimally or equitably distributed (Ten Have, 2014). The field of disaster ethics is in its infancy (Thompson et al., 2006; O'Mathúna et al., 2014, but early efforts have looked toward preparedness, including special protocols, for example, stating that the decision not to treat cases considered “beyond emergency care” cannot be considered a failure to come to aid (World Medical Association, 2006), giving legitimacy to the utilitarian aspects of triage. Such protocols need to be set, agreed on, and clearly communicated prior to a disaster context in order to be effective, and even still they can be challenging to implement on an individual level (Pou, 2013; O'Mathúna et al., 2014). Biodiversity conservation has often been compared to a “crisis”, although some individual cases are clearly more urgent and severe than others. Clearly recognizing instances of high magnitude, urgency and severity as “special” cases may increase acceptability of triage as a prioritization option, provided triage is not over-emphasized in other sectors of care or other less critical conservation contexts.
Emergency medicine triage and triage in the biodiversity conservation sector are notionally similar in that they relate to prioritization, but differ in terms of aims (e.g., allocation of wait times, vs. treatment), entities (e.g., individuals vs. groups), resource availability, including knowledge of prognoses with and without treatment, and institutional contexts. Medical and conservation triage are however unified by a wide variation in cultural and social contexts, and because the burden in both systems are increasing, as are the expectations of society.
We suggest conservation can learn much from emergency medicine triage. Emergency medicine triage has a much stronger emphasis on a wider variety of ethical principles than do common examples of conservation triage. Systems for conservation triage need to reflect more diverse ethical considerations to ensure it is more critically and effectively utilized. Conservation triage has to date been based on the principle of maximum utility, but needs to widen the scope of its ethical principles to include consideration of other concepts of distributional justice such as need. Importantly, triage contexts in conservation need not force the sacrifice of the most critically endangered species or ecosystems, as the outcome of any prioritization will depend on the proximal and distal objectives of the prioritization itself and the trade-offs that are acceptable (Conde et al., 2015).
Clear identification and communication of triage protocols and objectives, and situating triage within a broader system of care are key components of effective and ethical triage systems. While triage in emergency medicine is commonly evoked to justify/promote acceptance of conservation triage, for conservation there are likely better analogies from pandemic or disaster triage, where more “hard” decisions that involve sacrifice for the “greater good” are typically made—but still with unease and controversy. However, all conservation contexts need not be characterized as crises: a single conservation triage process would be better characterized as an important, but small component of a larger system of care and be driven by a wider and more diverse ethical perspective than has been previously been referred to.
We do not argue for or against triage as a concept, but rather conclude that to cast triage systems as “just” decision-making is simplistic. To expect one triage protocol will satisfy all stakeholders is naïve. Triage, like any prioritization or environmental decision, is associated with poignant environmental, economic, social, and ethical trade-offs. Triage systems may ultimately seek to deliver more good than harm from each triage decision that is made, but the premise of triage in medicine is to give ethical, rather than merely efficient, care. There is thus a need to reframe the notion of conservation triage from being predominantly about “rational” and “efficient” use of resources to considering the ethics of triage decisions when they are enacted.
KW and EL designed the paper, drafted and revised the paper, and approved the final version of the manuscript before submission.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We appreciate the comments received on earlier versions of this manuscript from E. Meijaard, D. Biggs, G. FitzGerald, S. Hagerman, B. Traill, H. Possingham and I. Lunt. KW and EL acknowledge funding from the Australian Research Council (http://www.arc.gov.au/), Future Fellowship (FT100100413), Centre of Excellence (CE110001014), and Discovery (DP150101300) programs.
Aacharya, R. P., Gastmans, C., and Denier, Y. (2011). Emergency department triage: an ethical analysis. BMC Emerg. Med. 11:16. doi: 10.1186/1471-227X-11-16
Ahmad, A., Mahmud, M. S., and O'Mathúna, P. D. (2014). “Evidence and Healthcare Needs During Disasters,” in Disaster Bioethics: Normative Issues When Nothing is Normal: Normative Issues When Nothing is Normal, eds. P. D. O'Mathúna, B. Gordijn, and M. Clarke (Dordrecht: Springer Netherlands), 95–106.
Arponen, A. (2012). Prioritizing species for conservation planning. Biod. Cons. 21, 875–893. doi: 10.1007/s10531-012-0242-1
Auerbach, N. A., Wilson, K. A., Tulloch, A. I., Rhodes, J. R., Hanson, J. O., and Possingham, H. P. (2015). Effects of threat management interactions on conservation priorities. Conserv. Biol. 29, 1626–1635. doi: 10.1111/cobi.12551
Balmford, A., Fisher, B., Green, R. E., Naidoo, R., Strassburg, B., Turner, R. K., et al. (2011). Bringing ecosystem services into the real world: an operational framework for assessing the economic consequences of losing wild nature. Environ. Res. Econ. 48, 161–175. doi: 10.1007/s10640-010-9413-2
Balmford, A., Gaston, K. J., Blyth, S., James, A., and Kapos, V. (2003). Global variation in terrestrial conservation costs, conservation benefits, and unmet conservation needs. Proc. Nat. Acad. Sci. U.S.A. 100, 1046–1050. doi: 10.1073/pnas.0236945100
Bennett, J. R., Maloney, R., and Possingham, H. P. (2015). Biodiversity gains from efficient use of private sponsorship for flagship species conservation. Proc. Biol. Sci. 282:20142693. doi: 10.1098/rspb.2014.2693
Bennett, N. J., and Dearden, P. (2014). From measuring outcomes to providing inputs: governance, management, and local development for more effective marine protected areas. Mar. Pol. 50, 96–110. doi: 10.1016/j.marpol.2014.05.005
Bodansky, D. M. S. (2009). Ethical dilemmas in triage: a perspective from the Jewish philosophical tradition. Ethics Med. 25, 49–56.
Bottrill, M. C., Joseph, L. N., Carwardine, J., Bode, M., Cook, C., Game, E. T., et al. (2008). Is conservation triage just smart decision making? Trends Ecol. Evol. 23, 649–654. doi: 10.1016/j.tree.2008.07.007
Bottrill, M. C., Joseph, L. N., Carwardine, J., Bode, M., Cook, C. N., Game, E. T., et al. (2009). Finite conservation funds mean triage is unavoidable. Trends Ecol. Evol. 24, 183–184. doi: 10.1016/j.tree.2008.11.007
Colyvan, M., and Steele, K. (2011). “Environmental ethics and decision theory: fellow travellers or bitter enemies,” in Philosophy of Ecology, eds D. M. Gabbay, B. Brown, P. Thagard, K. De Laplante, K. Peacock, and J. Woods (Amsterdam: Elsevier), 285–299.
Conde, D. A., Colchero, F., Güneralp, B., Gusset, M., Skolnik, B., Parr, M., et al. (2015). Opportunities and costs for preventing vertebrate extinctions. Curr. Biol. 25, R219–R221. doi: 10.1016/j.cub.2015.01.048
Cundill, G., Cumming, G. S., Biggs, D., and Fabricius, C. (2012). Soft systems thinking and social learning for adaptive management. Conserv. Biol. 26, 13–20. doi: 10.1111/j.1523-1739.2011.01755.x
Faith, D. P. (2009). Phylogenetic triage, efficiency and risk aversion. Trends Ecol. Evol. 24, 182; author reply 183–184. doi: 10.1016/j.tree.2009.01.002
Fernandes, C. M. B., Wuerz, R., Clark, S., and Djurdjev, O. (1999). How reliable is emergency department triage? Ann. Emerg. Med. 34, 141–147. doi: 10.1016/S0196-0644(99)70248-9
FitzGerald, G., Jelinek, G. A., Scott, D., and Gerdtz, M. F. (2010). Emergency department triage revisited. Emerg. Med. J. 27, 86–92. doi: 10.1136/emj.2009.077081
Göransson, K. E., Ehrenberg, A., Marklund, B., and Ehnfors, M. (2006). Emergency department triage: is there a link between nurses' personal characteristics and accuracy in triage decisions? Accid. Emerg. Nurs. 14, 83–88. doi: 10.1016/j.aaen.2005.12.001
Hagerman, S., Dowlatabadi, H., Satterfield, T., and McDaniels, T. (2010). Expert views on biodiversity conservation in an era of climate change. Glob. Environ. Change 20, 192–207. doi: 10.1016/j.gloenvcha.2009.10.005
Hagerman, S., and Satterfield, T. (2014). Agreed but not preferred: expert views on taboo options for biodiversity conservation, given climate change. Ecol. Appl. 24, 548–559. doi: 10.1890/13-0400.1
Hobbs, R. J., and Kristjanson, L. J. (2003). Triage: how do we prioritize health care for landscapes? Ecol. Man. Rest. 4, S39–S45. doi: 10.1046/j.1442-8903.4.s.5.x
Jachowski, D. S., and Kesler, D. C. (2009). Allowing extinction: should we let species go? Trends Ecol. Evol. 24, 180; author reply 183–184. doi: 10.1016/j.tree.2008.11.006
Justus, J., Colyvan, M., Regan, H., and Maguire, L. (2009). Buying into conservation: intrinsic versus instrumental value. Trends Ecol. Evol. 24, 197–191. doi: 10.1016/j.tree.2008.11.011
Lehmann, R., Brounts, L., Lesperance, K., Eckert, M., Casey, L., Beekley, A., et al. (2009). A simplified set of trauma triage criteria to safely reduce overtriage: a prospective study. Arch. Surg. 144, 853–858. doi: 10.1001/archsurg.2009.153
Martin, T. G., Nally, S., Burbidge, A. A., Arnall, S., Garnett, S. T., Hayward, M. W., et al. (2012). Acting fast helps avoid extinction. Conserv. Lett. 5, 274–280. doi: 10.1111/j.1755-263X.2012.00239.x
McCarthy, D. P., Donald, P. F., Scharlemann, J. P., Buchanan, G. M., Balmford, A., Green, J. M., et al. (2012). Financial costs of meeting global biodiversity conservation targets: current spending and unmet needs. Science 338, 946–949. doi: 10.1126/science.1229803
Miteva, D. A., Pattanayak, S. K., and Ferraro, P. J. (2012). Evaluation of biodiversity policy instruments: what works and what doesn't? Oxf. Rev. Econ. Policy 28, 69–92. doi: 10.1093/oxrep/grs009
Noss, R. F. (1996). Conservation or convenience? Conserv. Biol. 10, 921–922. doi: 10.1046/j.1523-1739.1996.10040921.x
O'Neill, J., Haila, Y., and Dyke, C. (2006). “Who speaks for nature?” in How Nature Speaks, eds Y. Haila, C. Dyke (Durham, CL; London: Duke University Press), 261–278.
O'Mathúna, D.N.P., Gordijn, B., and Clarke, M. (2014). “Disaster bioethics: an introduction,” in Disaster bioethics: normative issues when nothing is normal, eds. D.N.P. O'Mathúna, B. Gordijn & M. Clarke. (Dordrecht: Springer Science+Business Media), 3–12.
Parr, M. J., Bennun, L., Boucher, T., Brooks, T., Chutas, C. A., Dinerstein, E., et al. (2009). Why we should aim for zero extinction. Trends Ecol. Evol. 24, 181; author reply 183–184. doi: 10.1016/j.tree.2009.01.001
Pimm, S. L. (2000). Conservation: against triage. Science 289, 2289–2289. doi: 10.1126/science.289.5488.2289
Pou, A. M. (2013). Ethical and legal challenges in disaster medicine. Sthn. Med. J. 106, 27–30. doi: 10.1097/SMJ.0b013e31827ca40c
Probert, W. J. M., Drechsler, M., Baxter, P. W. J., and Possingham, H. P. (2011). Resource allocation in two species systems: is it worth acknowledging species interactions? Ecol. Mod. 222, 1781–1789. doi: 10.1016/j.ecolmodel.2011.02.026
Redding, D. W., and Mooers, A. O. (2015). Ranking mammal species for conservation and the loss of both phylogenetic and trait diversity. PLoS ONE 10:e0141435. doi: 10.1371/journal.pone.0141435
Rudd, M. A. (2011). Scientists' opinions on the global status and management of biological diversity. Conserv. Biol. 25, 1165–1175. doi: 10.1111/j.1523-1739.2011.01772.x
Sandler, R. (2014). The ethics of reviving long extinct species. Conserv. Biol. 28, 354–360. doi: 10.1111/cobi.12198
Sexton, J. P., Schwartz, M. W., and Winterhalder, B. (2010). Incorporating sociocultural adaptive capacity in conservation hotspot assessments. Div. Dist. 16, 439–450. doi: 10.1111/j.1472-4642.2010.00656.x
Shawhan, R. R., McVay, D. P., Casey, L., Spears, T., Steele, S. R., and Martin, M. J. (2015). A simplified trauma triage system safely reduces overtriage and improves provider satisfaction: a prospective study. Amer. J. Surg. 209, 856–863. doi: 10.1016/j.amjsurg.2015.01.008
Shoemaker, K. T., Breisch, A. R., Jaycox, J. W., and Gibbs, J. P. (2013). Reexamining the minimum viable population concept for long-lived species. Conserv. Biol. 27, 542–551. doi: 10.1111/cobi.12028
Ten Have, H. (2014). “Macro-triage in disaster planning,” in Disaster Bioethics: Normative Issues When Nothing is Normal: Normative Issues When Nothing is Normal, eds P. D. O'Mathúna, B. Gordijn, and M. Clarke (Dordrecht: Springer Netherlands), 13–32.
Thompson, A. K., Faith, K., Gibson, J. L., and Upshur, R. E. G. (2006). Pandemic influenza preparedness: an ethical framework to guide decision-making. BMC Med. Ethics 7:12. doi: 10.1186/1472-6939-7-12
Uleberg, O., Vinjevoll, O. P., Eriksson, U., Aadahl, P., and Skogvoll, E. (2007). Overtriage in trauma - what are the causes? Acta Anaesthesiol. Scand. 51, 1178–1183. doi: 10.1111/j.1399-6576.2007.01414.x
Weinerman, E. R., Ratner, R. S., Robbins, A., and Lavenhar, M. A. (1966). Yale studies in ambulatory medical care. V. Determinants of use of hospital emergency services. Amer. J. Pub. Health Nat. Health 56, 1037–1056. doi: 10.2105/AJPH.56.7.1037
Wiens, J. A., Goble, D. D., and Scott, M. (2012). Time to accept conservation triage. Nature 488, 281. doi: 10.1038/488281c
Wilson, H. B., Joseph, L. N., Moore, A. L., and Possingham, H. P. (2011). When should we save the most endangered species? Ecol. Lett. 14, 886–890. doi: 10.1111/j.1461-0248.2011.01652.x
Wilson, K. A., Carwardine, J., and Possingham, H. P. (2009). Setting conservation priorities. Ann. NYAS 1162, 237–264. doi: 10.1111/j.1749-6632.2009.04149.x
World Medical Association (2006). Statement on medical ethics in the event of disasters. Available online at: http://www.wma.net/en/30publications/10policies/d7/index.html (Accessed April 12, 2016).
Keywords: biodiversity, decision-making, equality, equity, optimization, prioritization, socially acceptable, utilitarianism
Citation: Wilson KA and Law EA (2016) Ethics of Conservation Triage. Front. Ecol. Evol. 4:112. doi: 10.3389/fevo.2016.00112
Received: 19 April 2016; Accepted: 12 September 2016;
Published: 27 September 2016.
Edited by:
Matt W. Hayward, Bangor University, UKReviewed by:
Bilal Butt, University of Michigan, USACopyright © 2016 Wilson and Law. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kerrie A. Wilson, ay53aWxzb24yQHVxLmVkdS5hdQ==
Elizabeth A. Law, ZS5sYXdAdXEuZWR1LmF1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.