- Department of Nursing Management and Education, School of Nursing and Public Health, The University of Dodoma, Dodoma, Tanzania
Background: Breast cancer is a global disease affecting an enormous number of women worldwide and a primary cause of cancer-related deaths in women. In Tanzania, women's breast cancer is the second-ranked among all types of cancers, with an incidence of 15.9%. Despite the Breast Self Examination (BSE) being one of the secondary prevention of breast cancer and an important measure for early diagnosis of breast cancer, little is known whether women could practice routine BSE.
Objectives: The study aims to Assess breast self-examination (BSE) knowledge, attitude, and practice among female undergraduates at the University of Dodoma.
Methodology: An institutionally-based analytical cross-sectional study will be carried out in the Dodoma region of Tanzania through a validated questionnaire. The study will involve 384 female undergraduate students aged 18 years. The data will be entered and analyzed in the Statistical Package for Social Sciences (SPSS) Version 25. Descriptive analysis (frequencies and percentages) and inferential statistics [Cross-tabulation, Chi-square (χ2), and Regression analysis] will be used.
Conclusion: The practice of BSE among women remains unsatisfactory, which is highly linked to the lack of BSE knowledge. The deficit knowledge is on how to perform BSE, the benefit of BSE, and the interval of doing BSE. Most of the women seem to possess a positive attitude towards BSE.
Introduction
Breast cancer is a global disease affecting an enormous number of women worldwide and a primary cause of cancer-related deaths in women (1). According to World Health Organization (WHO), 2.3 million women worldwide were diagnosed with breast cancer in 2020, among them 685,000 died (2). In developing countries, the prevalence of breast cancer is increasing due to unhealthy lifestyles like smoking, physical inactivity, calorie-dense food consumption, changes in childbearing and breastfeeding, and exogenous hormonal intake (3).
Breast cancer mortality is secondary to late diagnosis, causing poor outcomes of management and eventually death (4). Regular BSE is among the options to prevent breast cancer deaths (5). BSE is the secondary prevention of breast cancer (6). BSE is a cheap and affordable secondary prevention of breast cancer among third-world countries that aids in the detection of tumors and abnormalities predisposing to malignant tumors compared to Mammography (4).
In Ethiopia, BSE prevalence is as low as 15.2% (7). In India, 57.5% of nursing students were aware of BSE, only 5.3% performed BSE and among them, 6.6% knew the correct BSE testing procedure (8). It is reported that 44% of girls had inadequate knowledge of BSE and 54% had unfavourable attitudes (9). In another study it is indicated that 66.3% of participants had poor knowledge about breast self-examination, however, 95.3% had favourable attitudes.
BSE which aims to detect breast abnormalities involves five steps; ① examining breasts in a mirror while placing hands on hips and maintaining a straight back ② raising arms to check for the same changes in the breasts ③ looking for breast fluid warning signs while looking in the mirror ④ examine for breast lumps while lying down using the right hand to feel left breast while the left hand behind the head and vice versa and ⑤ examining breasts while sitting or standing using firm smooth touch with fingers like step three (10). The reported factors influencing BSE involve the family history of breast cancer, knowledge of BSE, self-efficacy in performing BSE, and information sharing from a health professional and media (11).
In Tanzania, women's breast cancer is the second-ranked among all types of cancers, with an incidence of 15.9%, and newly diagnosed cases of 3,992 women out of 29,883,105 population (12). More than 80% of breast cancer patients receive their diagnosis at stage III or IV (13). Between 2006 and 2013, there were twice as many new instances of cancer overall, and by 2030, the number of new cases and fatal cases of breast cancer is predicted to increase by 80% and 50%, respectively (13). Despite the BSE is one of the secondary prevention of breast cancer and an important measure for early diagnosis of breast cancer, little is known about regular Breast self-examination. More documentation focuses on the general population, with little documentation of BSE practice among University students. The study aims to assess young adult women's knowledge, attitude, and practice regarding breast self-examination. The study has three specific objectives (I) To assess knowledge of self-breast examination among female undergraduates at Dodoma University (II) To examine female undergraduates’ attitudes towards self-breast examination at the University of Dodoma and (III) To determine BSE practice among female undergraduate's students at the University of Dodoma.
Methodology
Study area
The study will be carried out in the Dodoma region of Tanzania because it is a rapidly developing region with people from various cultural backgrounds. Tanzania has a total population of 61,741,120, with females (31,687,990) and males (30,053,130). Meanwhile, Dodoma Region is the capital city of Tanzania, found in the central zone of Tanzania, with 41,310 km2 and a total population of 3,085,625 people, female (1,572,865) and male (1,512,760) (14).
Study design
An institutionally based analytical cross-sectional study will be conducted to examine female undergraduate students' knowledge, attitude, and practice regarding BSE.
Study population
The population of this study is female undergraduate students studying at the two Universities located in Dodoma. Most of these students are young (18–22) and are directly from high schools.
Inclusion criteria and exclusion criteria
Female undergraduate students studying at the Universities and aged 18 years and above years will be recruited into the study. Those who are unwilling to participate will be excluded from the study.
Sample size calculation
Sample size calculation will be obtained using Kish Leslie's formula (15) as presented below.
Whereby, n = Desired sample size, Z = confidence level at 95% (standard value of 1.96), P = estimated proportion of the respondents with a positive response towards BSE arbitrary proportion of 50%, and d = margin of error at 5% (standard value of 0.05).
Therefore, the total sample size of the study will be 384 participants.
Sampling technique
This study will utilize a stratified random sampling to conduct the study in two Universities. Simple random sampling at the Universities will be applied in selecting participants from each stratum (campus) thus respondents in each stratum will have an equal chance of being selected. The proportionate sampling will be applied to determine number of required samples at each stratum.
Data collection procedure and data collection tools
The data will be collected from 30th May to June 2023 by a principal investigator and one research assistant, through a validated questionnaire. The research assistant will be trained on how to use the tool and how to collect data. The questionnaire about sociodemographics and knowledge of BSE is adopted from the previous study by Sayi (16), while the questionnaire to assess attitude and BSE practice is adopted from (17). The complete questionnaire has four sections; Section A: Sociodemographic characteristics, Section B: Knowledge level of breast self-examination, Section C: Attitude towards breast self-examination, and Section D: Breast self-examination practice. Refer to Appendix 1.
Validity and reliability
The questionnaires adopted from the previous studies will be shared with experts to rank the effectiveness of tools and seek their comments for improvements. The pilot study will be conducted to pretest the tool, using 30% of actual sample size. If Cronbach's Alpa is 0.7 and above, the tools will be considered reliable. If Cronbach's Alpa is below 0.7, the Principle Component Analysis (PCA) will be utilized for factor analysis to modify weak variables.
Data analysis plan
The data will be entered and analyzed in the Statistical Package for Social Sciences (SPSS) Version 25. Descriptive analysis (frequencies and percentages) will be used to analyze the participants’ sociodemographic characteristics, BSE knowledge, attitudes towards BSE, and BSE practices. Meanwhile, the inferential statistics will be used to compute the associations of variables through Cross-tabulation, Chi-square (χ2), and Regression analysis. The significant difference will be set at P = 0.05.
Ethics approval and consent to participate
Ethical approval will be obtained from the University of Dodoma Institutional Research Review Committee (UDOM-IRREC). The introduction letter will be provided by the School of Nursing and Public Health of UDOM. The permission letter to conduct the study at the University of Dodoma will be provided by the council director of the Dodoma Municipality and the ward executive officer (WEO). The participants' confidentiality will be maintained by avoiding using participants' actual names and well-keeping filled questionnaires out of non-research team members. Each participant will complete the written informed consent before participating in the study. Participants will be free to participate and withdraw from the study at any time they feel to do so. The participants will be informed that there will be no compensation for their time.
Discussion
Knowledge of breast self-examination
The vast majority of previous studies demonstrate that there is a lack of knowledge on how to perform a thorough BSE. The research conducted in Bangladesh conducted among university students shows the overall mean score of total knowledge was 15 (SD = 3) out of 43, with an overall correct rate of 34% (18). Even though the majority of young women are aware of breast cancer, their knowledge of performing a self-breast check is still quite limited. A quasi-experimental carried out in Bangladesh reported low baseline awareness and knowledge of BSE (19). The campaigns about BSE should aim to promote knowledge and not awareness. The ongoing campaigns does not help women to understand deeper about BSE that's why women end up with awareness and inadequate knowledge. Despite the available studies on knowledge of BSE among University students, there is limited documentation concerning BSE knowledge among University students undertaking health related programs.
Attitude on breast self-examination
An institutional-based cross-sectional study conducted among young adults attending family planning services revealed that 224 (53.2%) women believed that it would be simple to perform BSE, 293 (69.6%) women mentioned that BSE was not a sexual activity initiation, 179 (42.5%) women reported that it was inappropriate to touch their breasts, 73.9% women said that BSE is important for preventing breast cancer and 59.4% women want BSE because it does not result in a positive cancer test (20). The systematic scoping review that included 21 studies revealed that the majority of senior high school students in Nigeria (82.6%) and female nurses in Ghana and Ethiopia (59.2%) had positive attitudes toward BSE (21). Since the attitude is promising, more efforts need to focus on coverage to ensure everyone is educated on BSE. The coverage can be through media health education.
Despite the available studies on attitude of BSE among University students, there is limited documentation concerning attitude towards BSE among University students undertaking health related programs.
BSE practice
A study conducted in Northwest Ethiopia in 2021 revealed that 17.4% of students studied had practiced BSE, which is associated with a lack of knowledge (22). Furthermore, the study among women attending family planning in southern Ethiopia revealed that 89 (21.1%) women have ever engaged in BSE, while 192 (57.8%) women have never practiced BSE because they believed they were healthy and others were afraid to be diagnosed with breast cancer (20). Meanwhile, the study in Turkey reported that 50% of students said they had performed BSE, and 33.3% reported having done so regularly. Only 13.3% of people reported performing a BSE routinely every month, compared to 55.5% who said they did it anytime they had the urge (23). Furthermore, 21% of Master's degree students reported practicing BSE (18). Mitigating the poor BSE practices, knowledge and attitude need to be considered factors. Despite the available studies on the practice of BSE among University students, there is limited documentation concerning BSE practice among University students undertaking health-related programs.
Study implications
The finding will assist the policymakers and healthcare stakeholders in identifying issues that need to be addressed to lower breast cancer prevalence and mortality and it will help in the allocation of resources.
Study limitation
Even though mammography is a recommended approach for detection of early stage of cancer, the practice of BSE will be assessed as it is within the capacity of an individual.
Conclusion
The practice of BSE among women remains unsatisfactory, which is highly linked to the lack of BSE knowledge. The deficit knowledge is on how to perform BSE, the benefit of BSE, and the interval of doing BSE. Most of the women seem to possess a positive attitude towards BSE.
Ethics statement
The studies involving humans were approved by University of Dodoma Institutional Research Review Committee (UDOM-IRREC). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
GM developed the draft of the protocol and prepared the manuscript. JM supervised the correctness of information in the protocol, determined the significance of the study, prepared the data collection tools, and revised the prepared manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors acknowledge the University of Dodoma for providing a conducive environment for the study process. We thank the individual contributions of Dr. Saada Seif, Dr. Golden Masika, and Dr. Fabiola Moshi.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Redig AG, McAllisterr SS. Breast cancer as a systemic disease: a view of metastasis. J Intern Med. (2019) 274(2):113–26. doi: 10.1111/joim.12084.Breast (NIH Public Access).
2. Lei S, Zheng R, Zhang S, Wang S, Chen R, Sun K, et al. Global patterns of breast cancer incidence and mortality: a population-based cancer registry data analysis from 2000 to 2020. Cancer Commun. (2021) 41(11):1183–94.
3. Albeshan SM, Brennan PC, Mackey MG, Hossain SZ, Alfuraih AA. Breast cancer epidemiology in gulf cooperation council countries : a regional and international comparison. Clin Breast Cancer. (2018) 18(3):e381–92. doi: 10.1016/j.clbc.2017.07.006
4. Kayan S, Cinar IO. An examination of variables associated with breast cancer early detection behaviors of women. Afr Health Sci. (2022) 22(3):133–44. doi: 10.4314/ahs.v22i3.16
5. Godfrey K, Agatha T, Nankumbi J. Breast cancer knowledge and breast self-examination practices among female university students in Kampala, Uganda: a descriptive study. Oman Med J. (2016) 31(2):129–34.
6. Kolak A, Kami M, Sygit K, Budny A. Primary and secondary prevention of breast cancer. Ann Agric Environ Med. (2018) 24(4):549–53. doi: 10.26444/aaem/75943
7. Dagne AH, Ayele AD, Assefa EM. Assessment of breast self- examination practice and associated factors among female workers in Debre Tabor Town public health facilities, North West Ethiopia, 2018 : cross- sectional study. PLoS One. (2019) 14(8):e0221356. doi: 10.1371/journal.pone.0221356
8. Kale Kalpana M, Aswar Nandkeshav R. A study of awareness about breast cancer and breast self-examination in nursing students. Sch J Appl Med Sci. (2020) 6691:2018–23. doi: 10.36347/sjams.2020.v08i09.009
9. Asmare K, Birhanu Y, Wako Z. Knowledge, attitude, practice towards breast self-examination and associated factors among women in Gondar town, Northwest Ethiopia, 2021: a community-based study. BMC Women’s Health. (2022) 22(1):1–14. doi: 10.1186/s12905-022-01764-4
10. Ramadas K, Basu P, Mathew BS, Muwonge R, Venugopal M, Prakasan AM, et al. Effectiveness of triennial screening with clinical breast examination: 14-years follow-up outcomes of randomized clinical trial in Trivandrum, India. Cancer. (2023) 129(2):272–82. doi: 10.1002/cncr.34526
11. Ymele F. Knowledge, attitude and practice of breast self-examination amongst women in two communities of Cameroon. Open J Obstet Gynecol. (2021) 11(6):773–93. doi: 10.4236/ojog.2021.116072
12. Turashvili G, McKinney SE, Goktepe O, Leung SC, Huntsman DG, Gelmon KA, et al. P-cadherin expression as a prognostic biomarker in a 3992 case tissue microarray series of breast cancer. Mod Pathol. [Internet]. (2011) 24(1):64–81. Available from: http://dx.doi.org/10.1038/modpathol.2010.189
13. Rweyemamu LP, Gültaşlar BK, Akan G, Dharsee N, Namkinga LA, Lyantagaye SL, et al. Breast cancer in East Africa: prevalence and spectrum of germline SNV/indel and CNVs in BRCA1 and BRCA2 genes among breast cancer patients in Tanzania. Cancer Med. (2023) 12(3):3395–409.
14. Rugeiyamu R, Ackim J. The Tanzania housing and population census 2022 : a Panacea for local service delivery and development drawbacks. Local Adm J. (2022) 15(1):1–13.
15. Kish L. Survey Sampling. Chichester: John Wiley & Sons, Inc (1965). doi: 10.1002/bimj.19680100122
16. Sayi E. Knowledge, Attitude and Practice of Breast Self- Examination Among Female Students in Institutions of Higher Learning: A Case of Mount Kenya University by. Nairobi: University of Nairobi (2018). p. 1–88.
17. Mengie T, Yifru A, Fikre A, Niguse W, Demsie D, Ekubay M. Assessment of knowledge, attitude and practice regarding breast self-examination among female students in Debre Birhan University, North Shewa Ethiopia. Am J Clin Exp Med. (2020) 8(3):48–54. doi: 10.11648/j.ajcem.20200803.13
18. Sarker R, Id SI, Moonajilin MS, Rahman M, Gesesew HA, Ward PR. Knowledge of breast cancer and breast self-examination practices and its barriers among university female students in Bangladesh: findings from a cross-sectional study. PLoS One. (2022) 17(6):e0270417. doi: 10.1371/journal.pone.0270417
19. Sarker R, Islam S, Moonajilin MS, Rahman M. Effectiveness of educational intervention on breast cancer knowledge and breast self- examination among female university students in Bangladesh : a pre-post quasi-experimental study. BMC Cancer. (2022) 22:1–7. doi: 10.1186/s12885-022-09311-y
20. Israel E, Awoke N, Yakob T, Aynalem A, Talto A. Determinants of breast self - examination practice among women attending pastoralist health facilities, southern Ethiopia : a cross—sectional study. BMC Women’s Health. (2023) 23:1–9. doi: 10.1186/s12905-023-02158-w
21. Udoh RH, Tahiru M, Ansu-mensah M, Bawontuo V, Danquah FI, Kuupiel D. Women’s knowledge, attitude, and practice of breast self- examination in Sub-Saharan Africa : a scoping review. Arch Pub Health. (2020) 78:1–10. doi: 10.1186/s13690-020-00452-9
22. Self-examination, B., Study, S., & Knowledge, B. C. Knowledge and Practice on Breast Self-Examination and Associated Factors among Summer Class Social Science Undergraduate Female Students in the University of Gondar, Northwest Ethiopia (2021).
23. Koc G, Gulen-Savas H, Ergol S, Yildirim-Cetinkaya M, Aydin N. Female university students’ knowledge and practice of breast self-examination in Turkey. Niger J Clin Pract. (2019) 22(3):410–5. doi: 10.4103/njcp.njcp_341_18
Appendix
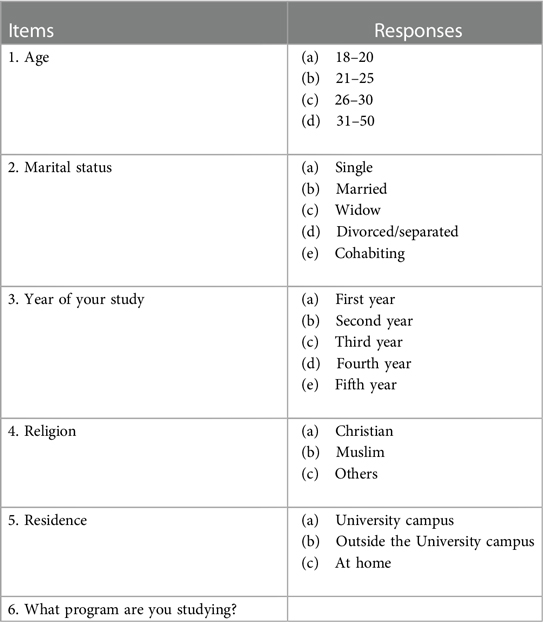
Section A: Sociodemographic characteristics
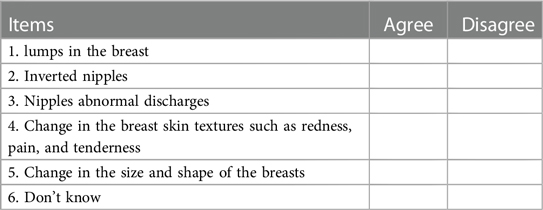
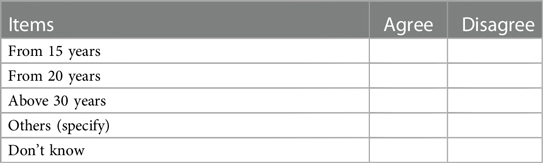
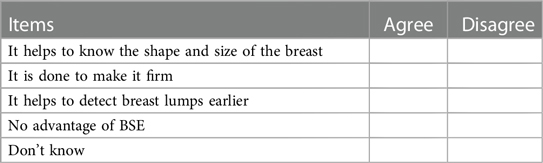
Section B: knowledge level of breast self-examination
1. What kind of things do you look for during self-examination yourself?
2. At what age should breast self-examination be practiced?
3. What are the advantages of breast self-examination?
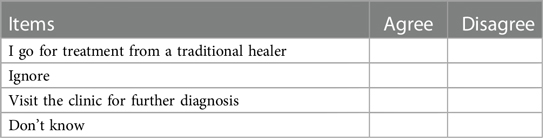
4. If you notice a lump in your breast, what is the most likely thing you would do?
5. How often do you do the procedure of BSE?
Section C: attitude towards breast self-examination.1. Is breast self-examination time-consuming?
(a) Yes […]
(b) No […]
2. Is breast self examination expensive?
(a) Yes […]
(b) No […]
3. Is it difficult to perfume breast self-examination?
(a) Yes […]
(b) No […]
4. Is breast self-examination embarrassing and unpleasant?
(a) Yes […]
(b) No […]
Section D: breast self-examination practice
1. Have you ever performed breast self-examination?
(a) Yes […]
(b) No […]
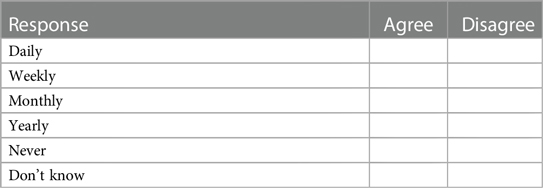
2. How often do you perform breast self-examination?
(a) Everyday […]
(b) Weakly […]
(c) Monthly […]
(d) Yearly […]
(e) At random […]
3. What is the appropriate time to perform breast self-examination?
(a) Before menstruation […]
(b) During menstruation […]
(c) Some days after menstruation […]
(d) No particular time […]
4. How do you perform breast self-examination?
(a) In front of the mirror […]
(b) While showering […]
(c) Lay down on the Bed […]
Keywords: breast self-examination, knowledge, attitude, breast cancer, secondary prevention
Citation: Masawa G and Mboineki JF (2024) Assessing breast self-examination knowledge, attitude and practice as a secondary prevention of breast cancer among female undergraduates at the University of Dodoma: a protocol of analytical cross-sectional study. Front. Epidemiol. 4:1227856. doi: 10.3389/fepid.2024.1227856
Received: 23 May 2023; Accepted: 12 April 2024;
Published: 30 May 2024.
Edited by:
Segun Fatumo, University of London, United KingdomReviewed by:
Su Yon Jung, University of California, Los Angeles, United StatesAllan Kalungi, Makerere University, Uganda
© 2024 Masawa and Mboineki. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joanes Faustine Mboineki, 624639045@qq.com
 Glory Masawa
Glory Masawa Joanes Faustine Mboineki
Joanes Faustine Mboineki