- 1School of Health Systems and Public Health, University of Pretoria, Pretoria, South Africa
- 2Department of Architecture, University of Pretoria, Pretoria, South Africa
- 3Department of Chemical Engineering, University of Pretoria, Pretoria, South Africa
Background: The interactions between people and places can have a significant impact on the wellbeing of individuals, particularly in warm, arid countries such as South Africa. Coupled to this are the various risks that climate change poses to the development of communities, particularly in informal settlements. Several of these risks include the increasing prevalence of contaminants in water and land, as well as the challenges of managing the effects of climate change.
Objectives: This conceptual analysis aims to highlight the need for a transdisciplinary approach to investigating the interaction between informal urban living spaces, environmental and social determinants of health and further propose a framework that incorporates tools and strategies to improve health and wellbeing.
Discussion: Despite the various advantages of living in an urban environment, many people in informal settlements still lack access to adequate sanitation and water services. This is why it is important that we develop a comprehensive understanding of how these changes can be accommodated in the future. This can be done through the collection of data from the people who live in these communities. A comprehensive understanding of the environmental and social determinants of health, coupled with innovative monitoring systems, would provide a more holistic approach to suggesting a practical strategy for promoting health and wellbeing in communities while working towards developing safe and sustainable health-promoting living spaces.
Conclusion: Currently there is a paucity of information regarding access to water, sanitation and health services, coupled with environmental pollution and poor living conditions causing diseases affecting informal communities, furthermore practical and viable changes to address these concerns are similarly lacking. To ensure that healthier built environments are provided for children and adults, transdisciplinary approaches between researchers and collaboration with, communities within informal settlements and with policymakers to promote health advocacy is essential.
Introduction
The United Nations Sustainable Development Goals (SDGs) have an overarching goal of achieving health and wellbeing for all, through integrated partnerships and trans-disciplinary collaborations (Saxena et al., 2021). Establishing sustainable cities (SDG 11) while ensuring innovation (SDG 9), access to water and sanitation (SDG 6), and an environment free from chemical and other pollutants (SDG 3), all form part of the SDG agenda (World Health Organization, 2018). Given the complexity of environmental and social determinants of health, inter-sectoral collaboration is becoming vital to deal with public health issues (Hussain et al., 2020). With the global rise in non-communicable diseases (IHME, 2018), we often neglect the important connection between health, people and places. In as much as adequately structured housing can offer shelter, physical spaces also have the potential to expose individuals to pollutants, influence diseases of lifestyle and inadvertently contribute to asthma and vulnerability to vector-borne diseases (Arthur et al., 2017). This connection was discussed in detail by Perdue et al. (2003) who explored the legal framework for the pathways to advance the design of the built environment to improve public health. This paper discusses a proposed transdisciplinary approach to analyze the interaction between the environment and users to determine their public health vulnerability–specifically in informal contexts. In this paper, transdisciplinary research is defined as a collaborative effort across multiple fields to define problems and set goals, integrating different disciplines and knowledge systems to address complex socio-environmental issues with cooperative and practical solutions (Kiatkoski et al., 2022).
Human choices can be influenced by the built environment, which consequently adversely affects health and the global climate. The varying density of populations across environments can influence disease transmission dynamics. Infectious diseases are caused by pathogenic microorganisms that can spread among individuals and there are numerous strategies for prevention (Salathé and Jones, 2010). These interventions often range from infectious disease vaccinations to health promotion for living an active lifestyle; including healthy food habits for individuals suffering from chronic diseases (Pinter-Wollman et al., 2018).
The built environment can assist in disease prevention and control by the type of building materials used and the way built formal or informal structures are organized to promote or prevent health risks. In the early 20th century, the hygienist agenda was one of the modernism postulates (Borasi and Zardini, 2012; Schrank and Ekici, 2016). During this period, tuberculosis was a major public health concern and while assuming therapeutic and prevention, modern architecture produced a detailed collection of spatial typologies, including flat roofs, larger windows and patios, which were open to air and were conducive to physical exercise (Campbell, 2012; Colomina, 2015). Environmental factors such as indoor air quality, lighting quality and thermal comfort were regarded as vital in designing approaches (Bluyssen, 2009). Following this modern hygienist ideas for disease prevention, numerous sanitary methods to designing the indoor climatic environment were introduced, coupled with legal regulations that addressed potential adverse health effects associated with building materials (Kjellstrom et al., 2006). Pollutants originating from toxic substances in building materials have been linked to various neurological, cognitive and behavioral disorders and diseases like cancer (Evans, 2003).
It is noteworthy that the selection of building materials and indoor surfaces of living spaces can influence the survival of pathogens (Pinter-Wollman et al., 2018). In diseases such as influenza and tuberculosis, a high population density drives the transmission (Alirol et al., 2011), and recently reports have shown that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (McIntosh, 2022), relies on proximity and physical contact. Thus, the built environment can be adapted to promote healthier behaviors and potentially mitigate the risk of contracting a disease (Perdue et al., 2003).
In informal settlements, unplanned urban expansion, results in concerns regarding the lack of proper sanitation (Pieterse, 2011a). This enables infectious diseases to spread and creates ideal breeding environments for a wide range of disease vectors. However, interventions such as improving housing conditions and destruction of vector habitats, has been shown to be effective in reducing infectious diseases in other peri-urban informal settlements (Alirol et al., 2011).
As we move towards establishing sustainable cities (SDG 11), access to water and sanitation (SDG 6), and an environment free from chemical and other pollutants (SDG 3), are an integral part of attaining health and wellbeing for all in an SDG era (World Health Organization, 2018). In addition, in response to the expected climate change driven water shortages and temperature increases in the Southern African region (Davis et al., 2017), improving the adaptive capacity of communities is vital to achieve tangible adaptation results (SDG13) (O’Brien, 2018). This conceptual analysis aims to highlight the need for a transdisciplinary approach to investigating the interaction between informal urban living spaces, environmental and social determinants of health and further propose a conceptual framework that incorporates tools and strategies to improve health and wellbeing.
Urbanization and social determinants of health
Urban communities are often challenged with air and water pollution and environmental degradation, while rural communities are challenged with issues related to agrochemicals, hygiene and sanitation, (Kuddus et al., 2020). Within a rapidly urbanizing world, Africa is currently urbanizing at the fastest pace globally (United Nations, 2019). Historically urbanization is associated with improved living standards, industrial and economic growth, unfortunately this has not been the case in Southern African urbanization (Tawodzera, 2012). This has resulted in the development of informal urban conditions, often alongside formal urban settlements. Informal settlements are typically defined as unplanned, autonomously built developments with little to no regulatory compliance and often developed with no tenure or landownership (Satterthwaite et al., 2020). Globally about a third of the urban populations resides in informally built urban settlements (Tesha, 2020), notably, 64% of African cities are informal, and many of them represent some form health or wellbeing deficiency due to overcrowding, poor building stock, insecure tenure and no access to water and sanitation (Pieterse, 2011a). In South Africa extent of informality is contested with the latest census results reporting 8.1% of all dwellings being informal, while the Gauteng City Region Observatory reports it 13.4% (Götz et al., 2023). While the reports are showing a downward trend, the prolific development of informal settlements throughout the urban centers in South Africa are difficult to monitor, as these settlements often develop on vulnerable, undevelopable land and hidden from plain sight (Dovey and King, 2011), as a result these communities are typically marginalized and under-represented.
Contrary to the general sentiment, Pieterse (2011a) argues that our current macro-economic developmental models will not be able to replace the existing informal conditions in Africa as envisioned by many, as this form of development is precipitated by increasing inequality, slow economic growth with limited tangible increase in GPD per capita, and a growing infrastructure deficit in most African metropoles. Resultantly, informality can in all probability be accepted as a perpetual condition within Southern African cities (Pieterse, 2019).
A review by Okyere and Kita (2015), highlights the fact that informality does not represent complete negative conditions, as informality presents a high level of adaptive capacity to adjust ones’ environment. Furthermore, Okyere and Kita (2015) highlights the inter-relation of complexity surrounding formal and informal urbanization processes taking place concurrently and argues therefore for an alternative reading of the informal city.
Importantly, informality is vulnerable to major impacts such as climate change which currently, and in future, indiscriminately affect humans and natural systems (IPCC, 2022). While numerous sectors and regions are especially sensitive to the impacts of climate change, cities with their associated higher populations and limited adaptive capacities are increasingly vulnerable climate change driven hazards (Romero-Lankao and Dodman, 2011). Le Roux et al. (2019) profiled several South African communities and identify informal underserviced settlements being particularly sensitive and exposed to externally driven climate change hazards. Le Roux et al. (2019) further notes that the outcome of these service delivery deficits and inadequate living conditions often lead to complex physical and social discord. As noted by Hugo and Plessis (2019) these exposures and sensitivities are not only driven by externally driven hazards, but also further intensified through internal processes of city-making, these include the spatial and material condition of these cities. To understand the exposures and sensitivities of inhabitants in informal settlements, inquiries into the physical context as well as the lived experience of users are needed. This calls for a ground-level understanding of the context and place (Hugo and Plessis, 2019).
To date there is limited research collecting empirical data on public health and the built environment’s interaction in informal settings. This is important as Pieterse (2011a) argues that informality as a developmental driver is set to continue in many African cities. As noted by Osuteye et al. (2017) there are still limited data on the risks and losses associated with informal settlements in the Sub-Saharan context. This is echoed in the work by Pieterse (2011a) arguing that macro analysis processes still ignore the existing lived experiences, access to healthcare and empirical conditions within informal conditions. If we are to capacitate local leverage opportunities and actors within these contexts, then an improved understanding of these informal contexts is needed.
Wellbeing as a complex science and holistic concept
Informal settlements, similar to cities, can be considered as complex adaptive systems (CAS) with specific structure and patterns of use that manifest as social-ecological systems (SES) (Nel et al., 2018). While these spaces may seem unplanned and unstructured, it is important to recognize our own limited understanding of these spaces, and rather consider these as uncharted territories (Dovey, 2015). Resultantly, it is important to acknowledge that informality is a more complex structured organization of place-making and user intent, notably as Okyere and Kita (2015) argue informal settlements are never completely informal, but rather the integration of both formal and informal processes. As cities, particularly informal settlements, are continually changing and shifting considering these as CAS assists researchers and practitioners to understand emergence and self-organization evident in these spaces (Siegenfeld and Bar-Yam, 2020). As these systems are highly complex and difficult to describe, focusing on actors, drivers and their relationships allows one to consider changes, document patterns of place, identify leverage points, and feedback loops (Nel et al., 2018). Ultimately, how these actors and drivers interact affects health outcomes of a community.
To address this complexity, there needs to be acknowledgment of the risks of using a singular reductionist approach, but rather include several disciplines to develop a more complex understanding of users and their environment as tangible and intangible actors and the relationship between them (Siegenfeld and Bar-Yam, 2020). This calls for, a holistic approach aimed at bringing better health to people (Freeman, 2005), however, there has been a paucity regarding how approaches to holistic health promote health and impact public health (Michaelson et al., 2018). While the intention of the UNSDGs is to ensure health and wellbeing for all by following a multi-faceted approach (Lueddeke, 2015), in the context of informal settlements, wellbeing is a complex consideration that addresses both the physical (tangible) factors and the psychological (intangible) aspects, that must be understood both within individual attitudes and along collective (communal) dimensions (Wallace et al., 2021). The built environment, therefore, play a critical role on people’s lives and livelihoods and need to respond to SES to impact health as well as wellbeing. To make such a shift, transdisciplinary approaches are required to understand various actors and their relationships in informal built environments to impact individual’s physical and mental health and their wellbeing (Cassidy, 2021).
Built environment as health determinant
A number of formal and regulatory mechanisms have been developed in the built environment to ensure safer living conditions. Sub-Saharan Africa faces challenges updating outdated building regulations, several rooted in colonial times and ill-suited for local conditions (Walls and Viljoen, 2016). These regulations are often misaligned with the unique local environmental and socio-economic conditions (World Bank, 2023). Efforts to incorporate standards such as the Eurocodes are fraught with complexity and highlight the necessity for more simplified directives tailored to prevalent small-scale constructions (Walls and Viljoen, 2016). The rapid pace of urban development precipitates the emergence of construction on sites susceptible to environmental hazards, notably flooding (Abdrabo et al., 2022). The built environment is shaped by five legal avenues: environmental regulation to cut pollution, zoning laws to segregate land uses, building codes ensuring structure safety, taxation to influence behaviour, and public spending on beneficial projects (Perdue et al., 2003). These mechanisms, varying by location, include local and regional pollution controls, zoning ordinances for land-use and development, building codes for indoor safety, and laws to ensure inclusive infrastructure. While laws provide the framework, effective implementation and enforcement are key to real progress (World Bank, 2023).
Yet informal, auto-constructed settlements do not typically follow these regulatory guides resulting poor living environments hampered with multiple environmental risks (Satterthwaite et al., 2020). With the increase in informal settlements in our urban environments, there is a need for alternative methods to understand and guide the development of these emergent self-directed settlements (Georgiadou and Loggia, 2021). Additionally, there are emerging risks from climate change that can be related to sustainable development, which include challenges to land and water management, the increase in emerging contaminants, adverse effects on human health, degradation of arable land, negative impacts for small-scale subsistence farmers, increasing risk of food insecurity and a major threat to rural livelihoods (Markkanen and Anger-Kraavi, 2019; Morton et al., 2019).
There are several human impacts that threaten the health of South Africa’s freshwater resources. It is essential that we investigate these threats and initiate regulations to protect them, make improvements and maintain existing sanitary infrastructure, and improve the capacity of local, regional and national government to address these issues. This will be especially applicable for poor, informal urban communities, similarly to rural communities, who in numerous cases have limited access to potable water and are reliant on water from contaminated rivers and freshwater impoundments (Dos Santos et al., 2017).
With the current burden of disease, deteriorating state of aquatic pollution and the fragile social, political and financial conditions, vulnerable communities with poor living conditions and housing are most at risk (IHME, 2018; Watts et al., 2018). In addition to being under-serviced, these communities are also often under resourced to provide adequate shelter for themselves. As South Africa is already experiencing above global average temperature increases (Fitchett, 2021), these climatic changes coupled with inadequate urban and built conditions are likely to increase the heat stress of these already vulnerable communities (Bek et al., 2018), resulting in increased mortality and morbidity in vulnerable communities (Kovats and Hajat, 2008; Tan et al., 2010). In addition to heat stress, increased temperatures may lead to increases in cardiovascular and cerebrovascular risks as well as increase exposure to EDC associated with choice of building materials. The associated risks and how communities respond to these impacts, require investigation.
Social determinants of health interface
The social determinants of health (SDH) are acknowledged as indicators of health and wellbeing. The World Health Organization (WHO) has defined SDH as circumstances in which individuals are born, grow, work, live, and age, and encompasses a broader group of factors and structures which shape and individual’s daily life conditions. These factors and structures span development agendas, social policies and norms, and economic and political systems (Andermann and Collaboration, 2016). The established the Commission on SDH in 1998 and recommended interventions and policies related to structural determinants (education and welfare), individual social status (ethnicity, gender, social cohesion), and intermediary factors (lifestyle, living and working situations) (World Health Organization, 2011). The SDH that are relevant to communicable and non-communicable disease alike and they are mostly responsible for health inequities. Major determinants of health include, poverty, housing conditions, gender inequities, unemployment, environmental conditions, access to health services and determinants associated with migration and urbanization (Scott et al., 2017). In addition, SDH also relate to factors including education, access to healthcare, employment, socioeconomics, physical environment and social support structures. To reduce the gap in health and healthcare inequities, it has become vital to address the SDH (Scott et al., 2017).
Access to healthcare as a determinant of health
Healthcare services (primary, secondary, tertiary care) are also considered as SDH. Inequities linked to access to healthcare pertaining to certain population groups include 1) the absence of healthcare providers who are culturally sensitive; 2) language or communication barriers; 3) area of origin of an individual 4) duration of stay in the area; and 5) healthcare services expectation prior and post migration (Hannah and Lê, 2012). People who live in informal settlements may find themselves having difficulty in accessing healthcare services. For woman, their socio-demographic and cultural shape their access to healthcare services. A study conducted in an informal settlement in Tshwane, South Africa, explored the experiences of healthcare providers and clients regarding the provision of reproductive health services including the prevention of HIV and AIDS. The findings show that females residing in informal settlements were aware that the PHC setting was unable provide adequate reproductive healthcare and was unable to meet their requirements (Mataboge et al., 2016).
High healthcare costs and income loss can be detrimental to poor individuals, who may not be able to return to their former economic situation quickly about repeated bouts of illness. Thus, it has become apparent that there should be investments in health, which is acknowledged to be an important means of economic development. Furthermore, in developing countries, and for the poorer residents, these investments will be essential to reduce poverty and improve their quality of life. Ensuring that individuals have adequate access to healthcare contributes to sustainable development by increasing education, labor and investment outputs. Although health is considered a basic right, it is essential that poorer individuals, especially in informal settlements benefit from supportive economic policies and health-focused sustainable development agendas that are geared to reduce the double burden of poverty and poor health (Murray, 2006). These environments pose a potential health threat to the urban poor; with poor sanitation contributing to the spread of infections, and a higher incidence of conditions such as asthma (Weimann and Oni, 2019). These environmental determinants of health have the potential to increase infectious and non-communicable conditions (NCDs), increasing the burden on an already stressed health system (Budreviciute et al., 2020).
Environmental determinants of health
Synthetic, chemically treated and often processed material are frequently used in the built environment which has the potential to adversely affect health. These potentially harmful chemicals may leach into the ambient air and are undetectable. Informal settlements are typically representing poor housing quality with limited services and infrastructure, extreme occupant and building densities, and limited adaptive capacity due to the poor economic status of the inhabitants, this leaves these communities vulnerable to climate change driven impacts (Pieterse, 2011b). However, there have been limited reports of associations between weather, climate and health in these populations, which places constrains on disaster risk mitigation, planning and reduction (Scovronick et al., 2015).
Vectors
Different risk factors in the urban environment may include inadequate housing, which contributes to increases in rodent and vector diseases. The spread of these vectors can be intricately linked to poor water supply, and inadequate sanitation and waste management processes, which create an enabling environment for vectors to thrive and infectious diseases to spread (Himsworth et al., 2013). In informal settlements, residents often live in close proximity and in high density, which creates the potential for hotspots that enable infectious diseases, such as respiratory viruses to spread easily. Knowledge sharing is vital to ensure that correct information about infectious disease prevention and control are essential in urban informal settlements, as these can be tools to aid the residents be resilient to infectious diseases outbreaks and could reduce some of the burden on the healthcare system. Additionally, local healthcare facilities can benefit from these tools and improve testing and treatment of often late or misdiagnosed infectious diseases, due to limited knowledge and inadequate health literacy (Dodson et al., 2015).
Emerging or re-emerging infectious diseases
Urbanization has the potential to contribute to the emergence or re-emergence of infectious diseases. This can be due to ecosystem degradation, agriculture intensification, and increased opportunities for the human-animal interactions, particularly, domestic reservoir species, such as rodents (Hassell et al., 2017). With high population density, poor housing and sanitation infrastructure, informal urban settlements have been associated with increased risks of contracting infectious diseases (Neiderud, 2015). However, it should be noted that not all urban, and informal urban settles are similar, thus there may be a wide range of risk factors to consider within the region or area. (Boyce et al., 2019). One example would be environmental risks. These are exposures which will be categorical in nature and would indicate household access to adequate sanitation or water, while other factors may vary across the population, such as outdoor air pollution.
Water and sanitation
While the inadequate infrastructure in the urban informal settlements can be a potential barrier to improving living conditions, there exists the opportunity for initiating interventions targeted at providing safe and clean water, with improved sanitation facilities, that can vastly improve health and wellbeing. Health and wellbeing strategies which encompass accessibility to basic services (energy, water and sanitation) for the poor, especially residents in informal settlements, is of local and global concern and forms part of the United Nations Sustainable Development Goals (SDGs) (Morton et al., 2019). There are two specific SDG goals and associated targets aimed at improving access to basic services. More specifically SDG 6 aims to ensure equitable and universal access to water and sanitation, while SDG 7 aims to address access to affordable, reliable and sustainable energy for all individuals (Fourie, 2018). As previously noted, informal settlements are severely lacking in terms of SDG6 and SDG 7, and this decreases a community’s ability to be resilient to climate-sensitive health risks. This is evident as a recent study found that residents in South African informal settlements had low satisfaction levels regarding sanitation provision, waste management and supply of electricity (Mutyambizi et al., 2020).
Documenting disease dynamics in informal settings
The current urban informal settings are stimulating conversations in field of public health to reconsider the complex health dynamics in cities. Coupled with the increase density of poor and vulnerable individuals, these complex health dynamics pose an imperative community health challenge. Urban informal settlements pose everyday health risks and have considerable increasing negative impacts on the health and wellbeing. Residents in these informal settlements face daily health risks associated with overcrowded homes, inadequate sanitation and limited to no access to clean water (Zerbo et al., 2020). While adhering to the principles of disease prevention and control, disease dynamics in informal settlements pose a challenge. Care should be taken to ensure preventative measures are inclusive of individuals facing health risks within today’s informal urban environments (Weimann and Oni, 2019). The health and wellbeing of individuals living in informal settlements has been highlighted in the SDG agenda. Several countries are striving to address operational and transitional determinants of inadequate healthcare provision and basic services in informal settings. When viewed through the “determinants of health” lens, multi-level interventions are needed so that issues of inequity and unequal distribution of health services to the urban poor are redressed (David et al., 2007).
Exposure to infectious diseases, coupled with limited access to clean water, proper sanitation and over-crowding leads to physical and intellectual growth impedance, posing a major public health threat. Factors including migration, density, adequate water and sanitation can enable pathogen transmission and amend vector dynamics. Consequently, social factors, such socioeconomic status, which drives health inequality influences infectious disease epidemiology in urban areas and needs to be addressed in any sustainable development approaches (Alirol et al., 2011). Recently, the mandatory practices of social distancing and proper hand washing etiquette in these urban informal settlements has been debated, as it has become implausible to adhere to these regulations with overcrowding, limited to no access to basic services, such as water and waste removal (Teare et al., 2020). There needs to be a comprehensive discussion regarding feasible practices in these resource constrained environments as we move towards establishing inclusivity in health and wellbeing strategies.
Built environment-health nexus
The built environment is a significant contributor to public health and climate change. In urban settings, environmental and human health can be affected by access to transportation services, use of land and infrastructure. Thus, the built environment and public health fields collaborate to design cities that are sustainable, inclusive and promote positive health outcomes, which align to SDG 11. Collaboration will address factors such as energy consumption, optimizing human health and sustainable material selection, which will reduce unintended exposures. The importance of these factors is addressed in detail by Rider (2020). Additionally, the external environment is categorized into three sectors: built environment (spaces where one lives, works, and play), natural environment (spanning air, water and land), and social (including socio-demographic, economic, and political factors) (Juarez et al., 2020). Information on environmental interaction with public health spaces is a valuable resource that can be used to design and implement community disease control initiative by local health officials (NRCIM, 2013). The need for accurate climatic and environmental data capturing within these living spaces is evident and would add significant value to a ground-level community engagement program. This would enable a direct coupling between a person’s sense of wellbeing and their living environment and surroundings. Thermal comfort levels can also provide insight into the effect of construction methods and materials within these living spaces (Adunola and Ajibola, 2016).
A low-key climatic and environmental monitoring system is required for autonomous and unobtrusive data capturing within the indoor living environment of the inhabitants within these informal settlements (Williams et al., 2019). The development of such a monitoring system will provide the involved members with a better understanding of the living environments and challenges faced by communities who live in these settlements and may enhance further community engagement and activities. Local development of a low-key climatic and environmental monitoring system also introduces opportunities for engineering students to participate in product development, as evidenced in similar, albeit large scale, smart environmental monitoring and assessment technologies (Trevathan and Johnstone, 2018). Small-scale product development and entrepreneurial activities are crucial to upskilling and empowering of young engineers, introduces the possibility of small business opportunities, and create transdisciplinary studies that can involve training of students from other disciplines.
Summary
The Public Health - Built Environment Nexus offers a comprehensive understanding of the intricate interplay between factors that shape the health and wellbeing of individuals and communities. This conceptual framework (Figure 1), with inter and intra linkages, provides a holistic approach to addressing health challenges and aligns closely with the United Nations’ Sustainable Development Goals (SDGs).
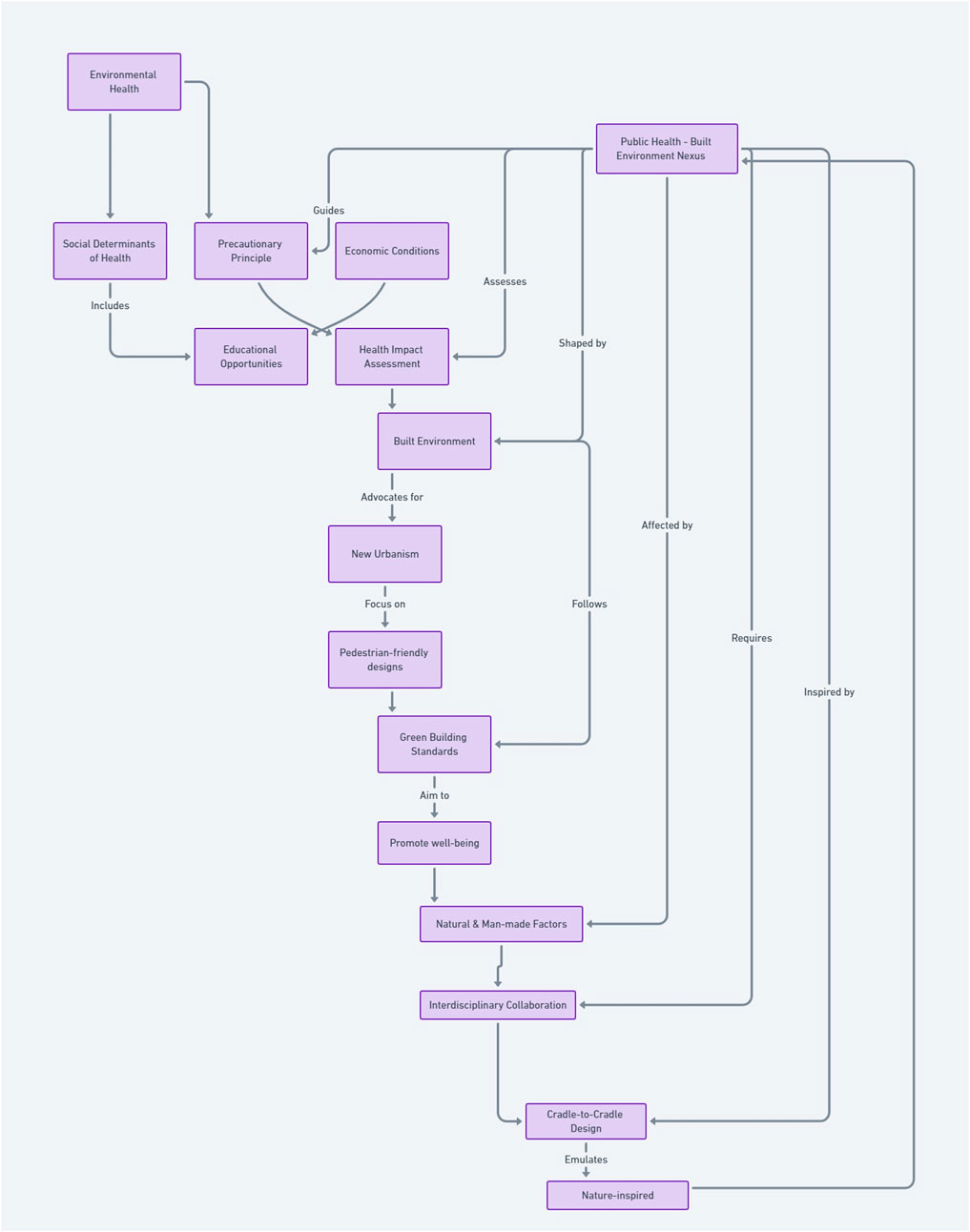
FIGURE 1. Conceptualizing the inter and intra linkages between the Public Health and Built Environment Nexus.
Interlinkages
Environmental Health emphasizes the significance of both natural and man-made elements that impact health. It advocates for proactive measures such as the Precautionary Principle and Health Impact Assessment (HIA) (Green et al., 2021). The emphasis on proactive health measures and understanding environmental impacts aligns with SDG 3 (Good Health and Wellbeing) and SDG 13 (Climate Action). The Social Determinants of Health underscores the broader societal structures, from economic conditions to educational opportunities, which influence health outcomes. Addressing these determinants is crucial for achieving SDG 1 (No Poverty), SDG 4 (Quality Education), and SDG 10 (Reduced Inequality). Principles of Green Building Standards (Agbajor and Mewomo, 2022) New Urbanism (Trudeau, 2013) are central to the built environment, encompassing our physical surroundings and infrastructures, plays a pivotal role in shaping health behaviors and outcomes. These principles resonate with SDG 11 (Sustainable Cities and Communities) and SDG 12 (Responsible Consumption and Production). Engineering brings in innovative philosophies like Cradle-to-Cradle Design (Toxopeus et al., 2015) and Biomimicry (Jamei and Vrcelj, 2021), emphasizing regenerative and efficient designs inspired by nature. Such sustainable engineering solutions contribute to SDG 9 (Industry, Innovation, and Infrastructure) and SDG 12 (Responsible Consumption and Production).
Intra-linkages
Within each of these primary factors, there are intricate connections. For instance, within Environmental Health, the relationship between natural and man-made factors and their subsequent impact on health is evident. The Precautionary Principle (Rechnitzer, 2022), which suggests taking preventive action in the face of uncertainty, is closely tied to the Health Impact Assessment, a tool used to evaluate the potential health effects of a project or policy. Similarly, within the Social Determinants of Health, economic conditions directly influence educational opportunities. A thriving economy can lead to better funding for schools and more educational opportunities for residents, which in turn can lead to better health outcomes. In the Built Environment, the principles of New Urbanism, which promote pedestrian-friendly and environmentally sustainable urban designs, are intricately linked with Green Building Standards. Both aim to create environments that are conducive to health and sustainability. Lastly, within Engineering, the Cradle-to-Cradle Design philosophy, which emphasizes creating products that can be fully recycled or upcycled, is intrinsically linked to Biomimicry, where designs are inspired by nature’s time-tested patterns and strategies.
Recommendations
The Public Health - Built Environment Nexus framework, with its intricate inter and intra linkages, provides a roadmap for understanding and addressing the multifaceted challenges related to health and sustainability. By aligning this framework with the SDGs, we can work towards a more holistic, integrated, and sustainable approach to public health and urban development.
The recommended roles and responsibilities for each disciple are: Public Health: Evaluate health outcomes in informal settlements, conduct Health Impact Assessments (HIA) for new projects, uphold the Precautionary Principle to avoid health risks, tackle Social Determinants of Health such as economic and educational disparities, and tailor public health initiatives to the unique needs of these communities. Built Environment: Design safe, affordable, and health-promoting housing; incorporate New Urbanism for walkable, mixed-use communities; adopt Green Building Standards for environmental sustainability; partner with engineers to create flexible housing designs for the evolving needs of informal settlements. Engineering: Employ Cradle-to-Cradle Design for sustainable material use; leverage Biomimicry for efficient, nature-inspired solutions; construct essential public health infrastructure like water and waste systems; innovate in providing affordable, sustainable energy for informal settlements.
To address these transdisciplinary challenges, the recommended community engagement activities are: Public Health: Undertake community health assessments, empower local health workers for credibility, provide culturally appropriate health education, and collaborate with community leaders on health initiatives. Built Environment: Co-create housing with residents to ensure cultural appropriateness, hold educational workshops on sustainable living, involve the community in building and upkeep to ensure long-term sustainability, and solicit feedback on designs to ensure they meet community needs. Engineering: Consult the community on infrastructure needs, employ local workers for construction projects to enhance skills and provide jobs, conduct training for infrastructure maintenance, and partner with local businesses to create maintainable, community-based solutions.
Author contributions
SP: Conceptualization, Funding acquisition, Investigation, Methodology, Visualization, Writing–original draft, Writing–review and editing. JH: Conceptualization, Visualization, Writing–original draft, Writing–review and editing. PS: Conceptualization, Visualization, Writing–original draft, Writing–review and editing. JS: Conceptualization, Visualization, Writing–original draft, Writing–review and editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The authors thank the University of Pretoria Research Development Program (RDP2054) and the United Nations Children’s Fund One Health for Change (UNICEF-OHC) for funding.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abdrabo, K. I., Kantosh, S. A., Saber, M., Sumi, T., Elleithy, D., Habiba, O. M., et al. (2022). “The role of urban planning and landscape tools concerning flash flood risk reduction within arid and semiarid regions,” in Wadi flash floods: challenges and advanced approaches for disaster risk reduction. Editors T. Sumi, S. A. Kantoush, and M. Saber (Singapore: Springer Singapore), 238–316.
Adunola, A. O., and Ajibola, K. (2016). Factors significant to thermal comfort within residential neighborhoods of Ibadan metropolis and preferences in adult residents’ use of spaces. SAGE Open 6, 215824401562494. doi:10.1177/2158244015624949
Agbajor, F. D., and Mewomo, M. C. (2022). Green building research in South Africa: a scoping review and future roadmaps. Energy Built Environ. 5 (2), 316–335. doi:10.1016/j.enbenv.2022.11.001
Alirol, E., Getaz, L., Stoll, B., Chappuis, F., and Loutan, L. (2011). Urbanisation and infectious diseases in a globalised world. Lancet Infect. Dis. 11, 131–141. doi:10.1016/s1473-3099(10)70223-1
Andermann, A., and Collaboration, C. (2016). Taking action on the social determinants of health in clinical practice: a framework for health professionals. Can. Med. Assoc. J. 188, E474–E483. doi:10.1503/cmaj.160177
Arthur, R. F., Gurley, E. S., Salje, H., Bloomfield, L. S. P., and Jones, J. H. (2017). Contact structure, mobility, environmental impact and behaviour: the importance of social forces to infectious disease dynamics and disease ecology. Philosophical Transactional R. Soc. B 372, 20160454. doi:10.1098/rstb.2016.0454
Bek, M. A., Azmy, N., and Elkafrawy, S. (2018). The effect of unplanned growth of urban areas on heat island phenomena. Ain Shams Eng. J. 9, 3169–3177. doi:10.1016/j.asej.2017.11.001
Bluyssen, P. M. (2009). The indoor environment handbook: how to make buildings healthy and comfortable. London, United Kingdom: Routledge, 320. doi:10.4324/9781849774611
Borasi, G., and Zardini, M. (2012). “Demedicalize architecture,” in Imperfect health: the medicalization of architecture. Editors G. Borasi, and M. Zardini (Montreal, Canada: Canadian Centre for Architecture), 15–37.
Boyce, M. R., Katz, R., and Standley, C. J. (2019). Risk factors for infectious diseases in urban environments of sub-Saharan Africa: a systematic review and critical appraisal of evidence. Trop. Med. Infect. Dis. 4 (4), 123. doi:10.3390/tropicalmed4040123
Budreviciute, A., Damiati, S., Sabir, D. K., Onder, K., Schuller-Goetzburg, P., Plakys, G., et al. (2020). Management and prevention strategies for non-communicable diseases (NCDs) and their risk factors. Front. Public Health 8, 574111. doi:10.3389/fpubh.2020.574111
Campbell, M. (2012). “Strange bedfellows: modernism and tuberculosis,” in Imperfect health: the medicalization of architecture. Editors G. Borasi, and M. Zardini (Montreal, Canada: Canadian Centre for Architecture), 133–151.
Cassidy, K. (2021). Evolving the built environment for health and wellbeing: prioritizing people’s needs at the start of every infrastructure project. Available at: https://www.wsp.com/en-ZA/insights/evolving-the-built-environment-for-health-and-wellbeing (Accessed February 15, 2022).
Colomina, B. (2015). X-ray architecture: the tuberculosis effect. Harv. Des. Mag. 40, 70–91. Avaialble at: https://www.harvarddesignmagazine.org/issues/well-well-well/.
David, A. M., Mercado, S. P., Becker, D., Edmundo, K., and Mugisha, F. (2007). The prevention and control of HIV/AIDS, TB and vector-borne diseases in informal settlements: challenges, opportunities and insights. J. Urban Health 84, 65–74. doi:10.1007/s11524-007-9183-5
Davis, C., Engelbrecht, F., Tadross, M., Wolski, P., and van Garderen, E. A. (2017). “Future climate change over southern Africa,” in Understanding the social and environmental implications of global change. Editors J. Mambo, and K. Faccer (South Africa: African Sun Media), 13–23.
Dodson, S., Good, S., and Or, H. (2015). Health literacy toolkit for low and middle-income countries: a series of information sheets to empower communities and strengthen health systems. New Delhi: Regional Office for South-East Asia: World Health Organization. Avaialble at: https://www.who.int/publications/i/item/9789290224754.
Dos Santos, S., Adams, E. A., Neville, G., Wada, Y., de Sherbinin, A., Mullin Bernhardt, E., et al. (2017). Urban growth and water access in sub-Saharan Africa: progress, challenges, and emerging research directions. Sci. Total Environ. 607-608, 497–508. doi:10.1016/j.scitotenv.2017.06.157
Dovey, K. (2015). Sustainable informal settlements? Procedia Soc. Behav. Sci. 179, 5–13. doi:10.1016/j.sbspro.2015.02.406
Dovey, K., and King, R. (2011). Forms of informality: morphology and visibility of informal settlements. Built Environ. 37 (1), 11–29. doi:10.2148/benv.37.1.11
Evans, G. W. (2003). The built environment and mental health. J. Urban Health 80, 536–555. doi:10.1093/jurban/jtg063
Fitchett, J. (2021). Climate change has already hit southern Africa. Here's how we know. Avaialble at: https://theconversation.com/climate-change-has-already-hit-southern-africa-heres-how-we-know-169062 (Accessed February 12, 2022).
Fourie, W. (2018). Aligning South Africa’s national development plan with the 2030 agenda’s sustainable development goals: guidelines from the policy coherence for development movement. Sustain. Dev. 26, 765–771. doi:10.1002/sd.1745
Freeman, J. (2005). Towards a definition of holism. Br. J. General Pract. 55, 154–155. Avaialble at: https://bjgp.org/content/55/511/154.
Georgiadou, M. C., and Loggia, C. (2021). “African cities and collaborative futures,” in Beyond self-help: learning from communities in informal settlements in Durban (South Africa: Manchester University Press), 209. doi:10.7765/9781526155351.00010
Götz, G., Ballard, R., Hassen, E. K., Hamann, C., Mahamuza, P., Maree, G., et al. (2023). “Statistical surprises: key results from census 2022 for Gauteng,” in GCRO rapid research paper (Johannesburg: Gauteng City-Region Observatory). doi:10.36634/PTPX7414
Green, L., Ashton, K., Bellis, M. A., Clemens, T., and Douglas, M. (2021). 'Health in all policies'-a key driver for health and well-being in a post-COVID-19 pandemic world. Int. J. Environ. Res. Public Health 18 (18), 9468. doi:10.3390/ijerph18189468
Hannah, C. T., and Lê, Q. (2012). Factors affecting access to healthcare services by intermarried Filipino women in rural Tasmania: a qualitative study. Rural. Remote Health 12, 2118–2119. doi:10.22605/RRH2118
Hassell, J. M., Begon, M., Ward, M. J., and Fèvre, E. M. (2017). Urbanization and disease emergence: dynamics at the wildlife-livestock-human interface. Trends Ecol. Evol. 32, 55–67. doi:10.1016/j.tree.2016.09.012
Himsworth, C. G., Parsons, K. L., Jardine, C., and Patrick, D. M. (2013). Rats, cities, people, and pathogens: a systematic review and narrative synthesis of literature regarding the ecology of rat-associated zoonoses in urban centers. Vector Borne Zoonotic Dis. 13, 349–359. doi:10.1089/vbz.2012.1195
Hugo, J., and Plessis, C. (2019). A quantitative analysis of interstitial spaces to improve climate change resilience in southern African cities. Clim. Dev. 12, 591–599. doi:10.1080/17565529.2019.1664379
Hussain, S., Javadi, D., Andrey, J., Ghaffar, A., and Labonté, R. (2020). Health intersectoralism in the Sustainable Development Goal era: from theory to practice. Glob. Health 16, 15. doi:10.1186/s12992-020-0543-1
Institute for Health Metrics and Evaluation (2018). Findings from the global burden of disease study 2017. Seattle, WA: Institute for Health Metrics and Evaluation. Avaialble at: https://www.healthdata.org/sites/default/files/files/policy_report/2019/GBD_2017.
International Panel on Climate Change (2022). Global warming of 1.5°C: IPCC special report on impacts of global warming of 1.5°C above pre-industrial levels in context of strengthening response to climate change, sustainable development, and efforts to eradicate poverty. Cambridge: Cambridge University Press. doi:10.1017/9781009157940
Jamei, E., and Vrcelj, Z. (2021). Biomimicry and the built environment, learning from nature’s solutions. Appl. Sci. 11, 7514. doi:10.3390/app11167514
Juarez, P. D., Hood, D. B., Song, M. A., and Ramesh, A. (2020). Use of an exposome approach to understand the effects of exposures from the natural, built, and social environments on cardio-vascular disease onset, progression, and outcomes. Front. Public Health 8, 379. doi:10.3389/fpubh.2020.00379
Kiatkoski, K. M., Douglas, M. M., Pannell, D., Setterfield, S. A., Hill, R., Laborde, S., et al. (2022). When to use transdisciplinary approaches for environmental research. Front. Environ. Sci. 10, 840569. doi:10.3389/fenvs.2022.840569
Kjellstrom, T., Lodh, M., McMichael, T., Ranmuthugala, G., Shrestha, R., and Kingsland, S. (2006). “Air and water pollution: burden and strategies for control,” in Disease control priorities in developing countries (Washington (DC), USA: Oxford University Press). Avaialble at: https://www.ncbi.nlm.nih.gov/books/NBK11728/.
Kovats, R. S., and Hajat, S. (2008). Heat stress and public health: a critical review. Annu. Rev. Public Health 29, 41–55. doi:10.1146/annurev.publhealth.29.020907.090843
Kuddus, M. A., Tynan, E., and McBryde, E. (2020). Urbanization: a problem for the rich and the poor? Public Health Rev. 41, 1. doi:10.1186/s40985-019-0116-0
Le Roux, A., Le Mans, G., Huyssteen, E., and van Niekerk, W. (2019). “Profiling the vulnerabilities and risks of South African settlements,” in Understanding the social and environmental implications of global change. Editors J. Mambo, and K. Faccer (Stellenbosch: African Sun Media), 26–35. Avaialble at: http://hdl.handle.net/10204/10025.
Lueddeke, G. (2015). Survival: one health, one planet, one future. South East. Eur. J. Public Health 2 (1), 1–18. doi:10.56801/seejph.vi.157
Markkanen, S., and Anger-Kraavi, A. (2019). Social impacts of climate change mitigation policies and their implications for inequality. Clim. Policy 19, 827–844. doi:10.1080/14693062.2019.1596873
Mataboge, M. L. S., Beukes, S., and Nolte, A. G. W. (2016). The experiences of clients and healthcare providers regarding the provision of reproductive health services including the prevention of hiv and aids in an informal settlement in Tshwane. Health S. Afr. 21, 67–76. doi:10.1016/j.hsag.2015.05.002
McIntosh, K. (2022). Covid-19: epidemiology, virology, and prevention. Avaialble at: https://www.uptodate.com/contents/covid-19-epidemiology-virology-and-prevention (Accessed August 15, 2023).
Michaelson, V., Pickett, W., and Davison, C. (2018). The history and promise of holism in health promotion. Health Promot. Int. 34, 824–832. doi:10.1093/heapro/day039
Morton, S., Pencheon, D., and Bickler, G. (2019). The Sustainable Development Goals provide an important framework for addressing dangerous climate change and achieving wider public health benefits. Public Health 174, 65–68. doi:10.1016/j.puhe.2019.05.018
Mutyambizi, C., Mokhele, T., Ndinda, C., and Hongoro, C. (2020). Access to and satisfaction with basic services in informal settlements: results from a baseline assessment survey. Int. J. Environ. Res. Public Health 17 (12), 4400. doi:10.3390/ijerph17124400
Neiderud, C. J. (2015). How urbanization affects the epidemiology of emerging infectious diseases. Infect. Ecol. Epidemiol. 5, 27060. doi:10.3402/iee.v5.27060
Nel, D., du Plessis, C., and Landman, K. (2018). Planning for dynamic cities: introducing a framework to understand urban change from a complex adaptive systems approach. Int. Plan. Stud. 23 (3), 250–263. doi:10.1080/13563475.2018.1439370
NRCIM (2013) Physical and social environmental In: health in international perspective: shorter lives, poorer health. Editors S. H. Woolf, and L. Aron (Washington (DC): National Research Council and Institute of Medicine, National Academies Press), 192–206. doi:10.17226/13497
O’Brien, K. (2018). Is the 1.5°c target possible? Exploring the three spheres of transformation. Curr. Opin. Environ. Sustain. 31, 153–160. doi:10.1016/j.cosust.2018.04.010
Okyere, S., and Kita, M. (2015). Rethinking urban informality and informal settlements growth in urban Africa: a literature discussion. J. Sustain. Dev. Afr. 17, 101–124. Avaialble at: https://jsd-africa.com/Jsda/Vol17No6-Fall15B/article17-06.html.
Osuteye, E., Johnson, C., and Brown, D. (2017). The data gap: an analysis of data availability on disaster losses in sub-Saharan African cities. Int. J. Disaster Risk Reduct. 26, 24–33. doi:10.1016/j.ijdrr.2017.09.026
Perdue, W. C., Stone, L. A., and Gostin, O. (2003). The built environment and its relationship to the public's health: the legal framework. Am. J. Public Health 93, 1390–1394. doi:10.2105/ajph.93.9.1390
Pieterse, E. (2011a). Grasping the unknowable: coming to grips with African urbanisms. Soc. Dyn. 37, 5–23. doi:10.1080/02533952.2011.569994
Pieterse, E. (2019). “Debunking the myths about African urbanism,” in To build a city in Africa. Editors R. Keeton, and M. Provoost (Rotterdam: nai010 Publishers), 48–56. Avaialble at: https://www.nai010.com/en/publicaties/to-build-a-city-in-africa/139474.
Pinter-Wollman, N., Jelić, A., and Wells, N. M. (2018). The impact of the built environment on health behaviours and disease transmission in social systems. Philosophical Trans. R. Soc. Lond. B Biol. Sci. 373, 20170245. doi:10.1098/rstb.2017.0245
Rechnitzer, T. (2022). Unifying 'the' precautionary principle? Justification and reflective equilibrium. Philosophia 50, 2645–2661. doi:10.1007/s11406-022-00582-0
Rider, T. R. (2020). Climate and health in cities: a challenge for the built environment. N. C. Med J. 81, 331–337. doi:10.18043/ncm.81.5.331
Romero-Lankao, P., and Dodman, D. (2011). Cities in transition: transforming urban centers from hotbeds of GHG emissions and vulnerability to seedbeds of sustainability and resilience. Curr. Opin. Environ. Sustain. 3, 113–120. doi:10.1016/j.cosust.2011.02.002
Salathé, M., and Jones, J. H. (2010). Dynamics and control of diseases in networks with community structure. PLoS Comput. Biol. 6, e1000736. doi:10.1371/journal.pcbi.1000736
Satterthwaite, D., Archer, D., Colenbrander, S., Dodman, D., Hardoy, J., Mitlin, D., et al. (2020). Building resilience to climate change in informal settlements. One Earth 2, 143–156. doi:10.1016/j.oneear.2020.02.002
Saxena, A., Ramaswamy, M., Beale, J., Marciniuk, D., and Smith, P. (2021). Striving for the united nations (UN) sustainable development goals (SDGs): what will it take? Discov. Sustain. 2, 20. doi:10.1007/s43621-021-00029-8
Schrank, S., and Ekici, D. (2016). Healing spaces, modern architecture, and the body. Oxford, UK: Routledge, 244. doi:10.4324/9781315586298
Scott, V., Schaay, N., Schneider, H., and Sanders, D. (2017). Addressing social determinants of health in South Africa: the Journey Continues. South Afr. Health Rev. 1, 77–87. doi:10.10520/EJC-c80ea0402
Scovronick, N., Lloyd, S. J., and Kovats, R. S. (2015). Climate and health in informal urban settlements. Environ. Urbanization 27, 657–678. doi:10.1177/0956247815596502
Siegenfeld, A. F., and Bar-Yam, Y. (2020). An introduction to complex systems science and its applications. Complexity 2020, 1–16. doi:10.1155/2020/6105872
Tan, J., Zheng, Y., Tang, X., Guo, C., Li, L., Song, G., et al. (2010). The urban heat island and its impact on heat waves and human health in Shanghai. Int. J. Biometeorology 54, 75–84. doi:10.1007/s00484-009-0256-x
Tawodzera, G. (2012). “Urban household vulnerability to food security and climate change. Experiences from urban areas of Zimbabwe,” in Climate change, assets and food security in southern African cities. Editors B. Frayne, C. Moser, and G. Ziervogel (Oxon: Earthscan), 57–74. doi:10.4324/9780203144084
Teare, J., Mathee, A., Naicker, N., Swanepoel, C., Kapwata, T., Balakrishna, Y., et al. (2020). Dwelling characteristics influence indoor temperature and may pose health threats in LMICs. Ann. Glob. Health 86, 91. doi:10.5334/aogh.2938
Tesha, D. (2020). Households livelihood coping strategies in the urban informal settlements the case of mlalakuwa, dar-Es-salaam Tanzania. Int. J. Soc. Sci. Humanit. Invent. 7 (7), 6046–6075. doi:10.18535/ijsshi/v7i07.05
Toxopeus, M. E., de Koeijer, B. L. A., and Meij, AGGH (2015). Cradle to Cradle: effective vision vs. Efficient practice? Procedia CIRP 29, 384–389. doi:10.1016/j.procir.2015.02.068
Trevathan, J., and Johnstone, R. (2018). Smart environmental monitoring and assessment technologies (SEMAT)-a new paradigm for low-cost, remote aquatic environmental monitoring. Sensors 18 (7), 2248. doi:10.3390/s18072248
Trudeau, D. (2013). New urbanism as sustainable development? Geogr. Compass 7 (6), 435–448. doi:10.1111/gec3.12042
United Nations (2019). World urbanization prospects. (The 2018 Revision). New York: United Nations Department of Economic and Social Affairs. Avaialble at: https://esa.un.org/unpd/wup/.
Wallace, K. J., Jago, M., Pannell, D. J., and Kiatkoski, M. (2021). Wellbeing, values, and planning in environmental management. J. Environ. Manag. 277, 111447. doi:10.1016/j.jenvman.2020.111447
Walls, R. S., and Viljoen, C. (2016). A comparison of technical and practical aspects of Eurocode 3-1-1 and SANS 10162-1 hot-rolled steelwork design codes. J. South Afr. Institution Civ. Eng. 58, 16–25. doi:10.17159/2309-8775/2016/v58n1a2
Watts, N., Amann, M., Arnell, N., Ayeb-Karlsson, S., Belesova, K., Berry, H., et al. (2018). The 2018 report of the lancet countdown on health and climate change: shaping the health of nations for centuries to come. Lancet 392, 2479–2514. doi:10.1016/S0140-6736(18)32594-7
Weimann, A., and Oni, T. (2019). A systematised review of the health impact of urban informal settlements and implications for upgrading interventions in South Africa, a rapidly urbanising middle-income country. Int. J. Environ. Res. Public Health 16 (19), 3608. doi:10.3390/ijerph16193608
Williams, D. S., Máñez Costa, M., Sutherland, C., Celliers, L., and Scheffran, J. (2019). Vulnerability of informal settlements in the context of rapid urbanization and climate change. Environ. Urbanization 31, 157–176. doi:10.1177/0956247818819694
World Bank (2023). Building regulations in sub-saharan Africa: a status of the building regulatory environment. Washington, DC: International Bank for Reconstruction and Development. Avaialble at: https://www.gfdrr.org/en/publication/building-regulations-sub-saharan-africa.
World Health Organization (2011). Rio political declaration on social determinants of health. Geneva: World Health Organization. Avaialble at: https://www.who.int/publications/i/item/rio-political-declaration-on-social-determinants-of-health.
World Health Organization (2018). World health statistics 2018: monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization. Avaialble at: https://www.who.int/publications/i/item/9789240074323.
Keywords: public health, built environment, engineering, conceptual analysis, South Africa, urban
Citation: Patrick SM, Hugo J, Sonnendecker P and Shirinde J (2024) A conceptual analysis of the public health-architecture nexus within rapidly developing informal urban contexts. Front. Environ. Sci. 12:1285352. doi: 10.3389/fenvs.2024.1285352
Received: 29 August 2023; Accepted: 03 January 2024;
Published: 15 January 2024.
Edited by:
Haoran Yang, East China Normal University, ChinaReviewed by:
Paul Chelule, Sefako Makgatho Health Sciences University, South AfricaShah Md Atiqul Haq, Shahjalal University of Science and Technology, Bangladesh
Adele Houghton, Biositu, LLC, United States
Copyright © 2024 Patrick, Hugo, Sonnendecker and Shirinde. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sean M. Patrick, c2Vhbi5wYXRyaWNrQHVwLmFjLnph
 Sean M. Patrick
Sean M. Patrick Jan Hugo
Jan Hugo Paul Sonnendecker
Paul Sonnendecker Joyce Shirinde
Joyce Shirinde