
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Environ. Sci. , 16 November 2023
Sec. Toxicology, Pollution and the Environment
Volume 11 - 2023 | https://doi.org/10.3389/fenvs.2023.1296606
This article is part of the Research Topic Recent Research Advances on Heavy Metals, Microplastics, Persistent Organic Pollutants, and Solid Waste in Aquatic and Terrestrial Ecosystems View all 11 articles
 Govindasamy Kadirvel*
Govindasamy Kadirvel* Jasmine Diengdoh
Jasmine Diengdoh Sourabh Deori
Sourabh Deori Raju Kumar Dewry
Raju Kumar Dewry Sayed Nabil Abedin
Sayed Nabil Abedin Prabha Moirangthem
Prabha MoirangthemObjective: Reproductive toxicology is a field that deals with the effects of heavy metals on various aspects of reproduction, including sperm count, motility, viability, spermatogenesis, follicular atresia, hormonal imbalance, and oocyte maturation, among others. The present study was carried out to examine the effects of heavy metals, viz., arsenic (As), lead (Pb), and fluoride (F), on boar sperm quality parameters in vitro.
Materials and Methods: Forty (40) ejaculates from six (6) boars, averaging eight ejaculates per boar, were collected with the gloved hand technique using a dummy sow. Six (6) different concentrations were selected for the in vitro study: 5, 10, 25, 50, 100, and 200 µM for As and Pb, and 5, 10, 25, 50, 100, and 200 mM for F. The ejaculates were co-incubated with heavy metals at these different concentrations and assessed after different incubation periods (0, 0.5, and 1 h) for sperm functional attributes, viz., sperm progressive motility, viability and membrane integrity, and sperm mitochondrial membrane potential (MMP). The combined effects of heavy metals on sperm functional attributes were also evaluated at different doses (5, 10, 25, 50, 100, and 200 μM/μM for As–Pb; 5, 10, 25, 50, 100, and 200 μM/mM for As–F; and 5, 10, 25, 50, 100, and 200 μM/mM for Pb–F).
Results: The present study revealed a highly significant (p <0.001) decrease in sperm progressive motility, viable sperm, membrane integrity, and sperm MMP in samples treated with heavy metals under different incubation periods; furthermore, the longer the incubation time, the greater the toxicity. There was also a significant (p <0.05) decrease in sperm motility, membrane integrity, and MMP in the samples treated with combined heavy metals (As–Pb, As–F, and Pb–F), as compared to the control, after different incubation periods. A significant (p <0.05) reduction in sperm quality attributes was recorded even at the lowest concentrations in the case of heavy metal combinations.
Conclusion: It can be concluded that As, Pb, and F are toxic to boar spermatozoa in vitro, causing reductions in sperm functional attributes in a dose- and time-dependent manner.
Heavy metals alter several reproductive functions in both males and females, causing infertility; the outcomes include a decrease in sperm count, motility, viability, and spermatogenesis; hormonal imbalance; follicular atresia; and delay in oocyte maturation, and these effects form an important aspect of reproductive toxicology. Heavy metals are regarded as one of the oldest environmental issues across the globe, and are toxic even at the micro level (Carvalho et al., 2011). The main sources of heavy metals in the environment are either natural or man-made, and these sources contribute to exposure to human and animal health hazards. Anthropogenic activities such as rapid industrialization, overcrowding, and environmental manipulation can release heavy metals into the environment, in turn infiltrating the food chain (Maartens et al., 2015). Exposure to heavy metals produces either acute or chronic poisoning cases; their accumulation in different organs of an individual has the potential to harm particular organ systems or possibly the entire organism (Kumar and Singh, 2015). Gastrointestinal and kidney dysfunction, vascular damage, birth defects, skin lesions, nervous system disorders, immune system dysfunction, and cancer are a few examples of such harm, and simultaneous exposure to two or more metals may have cumulative effects, each potentiating the toxicity of the other (Gazwi et al., 2020; Balali-Mood et al., 2021). The amounts of components that accumulate in body organs is determined by exposure interval, the amount swallowed, animals’ production and reproduction periods, age and breed, the method of consumption, and the interplay between necessary and harmful elements, which determines the toxicity of the element in the animal’s biological systems (Mendiola et al., 2011). During grazing or feeding, fodder contaminated with toxic metals or toxic compounds enters the animal’s body through the respiratory and digestive systems or through dermal contact and affects physiological functions (Alam and Shilpa, 2020). Among the heavy metals, arsenic (As), lead (Pb), and fluoride (F) are among those that most significantly endanger human and animal health even at low levels of exposure. Arsenic is one of the most toxic substances that organisms can be exposed to through food and drinking water; it produces toxicity in livestock, humans, poultry, and aquatic animals due to its use in herbicides, rodenticides, and fungicides, and is particularly harmful to the male reproductive system (Knazicka et al., 2012; Shankar et al., 2014). It has been reported that protein responses are dysregulated in the male reproductive organs in poultry and animals as a result of arsenic toxicity, in turn lowering the sperm count per ejaculate, reducing sperm motility and viability, and causing abnormal sperm morphology (Zhao et al., 2017; Renu et al., 2018; Verma et al., 2018). Lead is widely used in acid battery plant refineries, smelters, the fuel combustion industry, printing presses, and automobile exhausts, where tetraethyl Pb acts as an anti-knocking agent; this results in exposure of humans and animals to lead, and its toxicity in the male reproductive system is manifested by Pb deposition in the testes, epididymis, vas deferens, seminal vesicles, and seminal ejaculate, leading to negative effects on sperm count and motility (Chowdhury, 2009); a decrease in sperm quality is also seen in mice (Li et al., 2018). Finally, the third heavy metal, fluoride, usually exists widely in the environment as an inorganic or organic compound; due to its greater reactivity toward the reproductive system, it causes decreased sperm count and abnormal sperm ratios, disrupted spermatogenesis, and a significant decrease in testosterone levels (Nickson et al., 2005). The toxicity of heavy metals has been reported in laboratory animals, but no studies have documented the in vitro effect of heavy metals on boar spermatozoa, either separately or in combination. Therefore, the present study was designed to investigate the in vitro toxic effects of As, Pb, and F separately and in combination, at different concentrations and with different incubation periods, on sperm functional attributes in a boar model.
Standard solutions of arsenic (CAS No. 119773; H3AsO4 in HNO3 0.5 mol/L; 1,000 mg/l As Centipur®) and lead (CAS No. 119773; Pb(NO3)2 in HNO3 0.5 mol/L; 1,000 mg/l Pb Centipur®), stabilized in 0.1 mM PBS (phosphate-buffered saline), were purchased from Sigma-Aldrich (St. Louis, MO, United States), and fluoride (CAS No. 7681-49-4) was purchased from HiMedia™ (Thane West, Maharashtra, Pin-400 604, India). The stock solutions of the heavy metals were diluted with distilled water to prepare the working solutions for the experiment with the desired concentration, as per the formula M1V1 = M2V2. Sperm Tyrode’s albumin lactate pyruvate (TALP-100 mM NaCl, 3.1 mM KCl, 25 mM NaHCO3, 0.29 mM NaH2PO4, 21.6 mM C3H5NaO3, 2.0 mM CaCl2, 1.5 mM MgCl2, and 10 mM HEPES) medium was prepared using chemical components purchased from HiMedia™. All other chemicals and reagents were procured from Sigma-Aldrich, unless otherwise stated.
Six superior quality Hampshire crossbred boars (75%) with sexually proven fertility were used for the experiment. A semen sample was collected twice weekly from each boar using the gloved hand technique with a dummy sow. Following the collection of semen, ejaculates were transferred into a Minitube container pre-heated to 37°C in an incubator and transported to the laboratory within 30 min. A total of 40 ejaculates were collected and analyzed immediately for progressive motility. Semen samples with 70% progressive motility or higher were used for further processing and assessment of sperm functional attributes.
In the first experiment, the ejaculated semen sample was aliquoted in a 1.5-mL Eppendorf tube with different concentrations of As (5, 10, 25, 50, 100, and 200 μM), Pb (5, 10, 25, 50, 100, and 200 μM), and F (5, 10, 25, 50, 100, and 200 mM) and co-incubated for 0, 0.5, or 1 h in a CO2 incubator (Thermo Fisher Scientific, United States) with 5% CO2 and 95% humidity at 37°C. A semen sample without the addition of heavy metals was incubated as a control. The in vitro characteristics of sperm (viz., progressive motility, viability and membrane integrity, and MMP) from samples incubated in different concentrations of heavy metals were assessed after each incubation period. Similarly, in the second experiment, semen samples were co-incubated with different combined concentrations of heavy metals, viz., As–Pb (20, 50, 100, and 200 μM/μM), As–F (20, 50, 100, and 200 μM/mM), and Pb–F (20, 50, 100, and 200 μM/mM), and evaluated for sperm functional attributes, namely, progressive motility, viability and membrane integrity, and MMP.
Sperm progressive motility was evaluated by placing 10 µL of sperm suspension on a glass slide and then covering it with a coverslip. Sperm motility was observed under a phase-contrast microscope equipped with a 37°C microscope stage warmer at 400× magnification (Olympus, BX51 FT, Japan). The percentage of spermatozoa with normal, vigorous, and forward linear motion was subjectively assessed to the nearest 5% in different areas of the sample on each slide.
Sperm membrane integrity was assessed using carboxyfluorescein diacetate succinimidyl ester (CFDA) fluorescent dye as per the method described by Kukov et al. (2009), with minor modifications. Briefly, stock solutions of CFDA and propidium iodide (PI) were prepared at a concentration of 1 mg/mL in DMSO (dimethyl sulfoxide) and 1 mg/mL in PBS, respectively. The stock CFDA was added to 250-µL semen aliquots containing different concentrations of As, Pb, and F at a final concentration of 20 µM in an Eppendorf tube and incubated at 37°C for 5 min. Subsequently, 5 µL of PI was added at a final concentration of 15 µM and the solution was incubated for 5 min. After incubation, the tubes were centrifuged at 800 rpm for 5 min, and the supernatant was removed. Then, 200 µL of PBS was added to the sperm pellet in each Eppendorf tube and mixed gently. A drop of 10–15 µL from the stained sperm suspension was placed on a clean, dry glass slide covered with a coverslip, and 200 spermatozoa were observed under a fluorescent microscope (Nikon, Eclipse 80i, Japan). Sperm cells were classified as having an intact plasma membrane (stained with green fluorescence), having a damaged plasma membrane (stained with red fluorescence), or morbid spermatozoa (stained with both green and red fluorescence).
For the assessment of mitochondrial membrane potential, a stock solution of 1.53 mM JC-1 (5,50,6,60-tetrachloro-1,10,3,30-tetraethylbenzimidazolyl carbocyanine iodide) stain was prepared in DMSO. Next, 250 μL of each of the semen aliquots containing different concentrations of As, Pb, and F was stained with 1 µL of the JC-1 stock solution (final concentration of 2 µM) for 30 min at 37°C. Counterstaining of nuclei DNA was performed with 5 µL of the PI stock solution (final concentration of 0.27 mg/mL) and solutions were then incubated for 5 min. At least 200 spermatozoa were counted under a fluorescent microscope at 400× magnification; spermatozoa were observed using FITC and TRITC filters, and the images obtained from the two filters were merged to obtain the final image. When MMP levels are high, the mitochondrial protein JC-1 forms J-aggregates and exhibits orange/red fluorescence, while at a low MMP, it remains in the monomer form and emits green fluorescence (Selvaraju et al., 2008).
All the data obtained were analyzed using SPSS software (version 16.0 for Windows; SPSS Inc., Chicago, IL, United States). Data on various parameters are expressed in the form mean ± SE and analyzed via multivariate analysis of variance (ANOVA), with the specific sperm treatment as the main variable. Post-hoc testing for significant differences was carried out using Tukey’s test; p values <0.05 were considered to represent significance.
After 0 h of incubation, a significant reduction (p <0.05) in sperm motility was recorded at 25 µM As concentration in comparison to the control (Figure 1A). After 0.5 h of incubation, sperm motility at a lower As concentration (5 µM) did not differ significantly (p >0.05) from that of the control. However, a highly significant (p <0.05) decrease was recorded when the concentration was increased to 10 µM, signifying that a lower As concentration became toxic with increasing incubation time. After 1 h of incubation, a significant (p <0.05) reduction in sperm motility in comparison to the control was recorded as the concentration was increased beyond 10 µM. Furthermore, when sperm motility was compared between different incubation periods, a significant decrease was observed (p <0.001) after 0.5 and 1 h of incubation in comparison to 0 h for different As concentrations. Regarding sperm viability, after 0 h of incubation, no significant reduction (p >0.05) was recorded at a 10-μM As concentration in comparison to the control (Figure 1B). However, a highly significant (p <0.05) decrease in sperm viability and membrane integrity was observed with an increase in As concentration to 25 µM and above. After 0.5 h of incubation, even at a lower As concentration (10 µM), a significant (p <0.05) reduction in sperm viability was recorded in comparison to the control; and after 1 h of incubation, a significant (p <0.05) reduction was recorded for a 5-μM As concentration in comparison to the control. In comparisons between the incubation periods, sperm viability and membrane integrity were found to be reduced significantly (p <0.01) between 0 and 0.5 h, and a significant reduction (p <0.05) was also recorded between 0.5 and 1 h. Regarding sperm MMP, after 0 h of incubation, the number of sperm with high MMP was not significantly reduced (p >0.05) at 10 µM (Figure 1C), but a significant reduction (p <0.05) was seen at concentrations from 25 µM. Similar trends were observed after 0.5 and 1 h of incubation, whereby the 5 µM As concentration resulted in significantly (p <0.05) lower numbers of spermatozoa exhibiting high MMP, while in comparisons between the incubation periods, sperm MMP showed a significantly (p <0.001) declining trend with increased time of incubation.
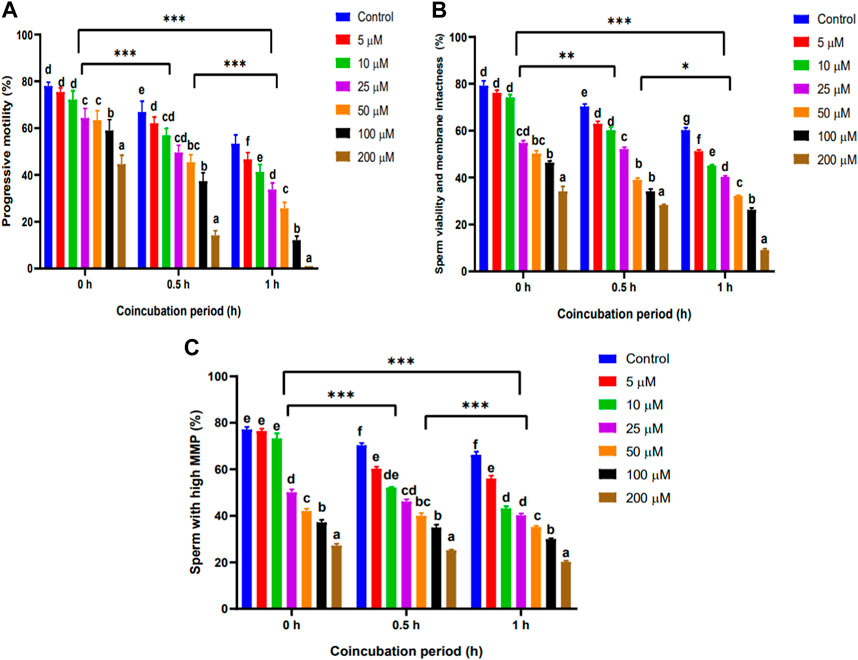
FIGURE 1. Effect of different concentrations of arsenic on sperm functional attributes after different co-incubation periods. (A) Effect of As on sperm progressive motility (%). (B) Effect of As on sperm viability and membrane integrity (%). (C) Effect of As on sperm MMP (%). Different superscripts indicate significant differences in means between the different treatment groups (p <0.05). * p <0.05; ** p <0.01; *** p <0.001 (indicating significant differences under different incubation periods). Abbreviations: As, arsenic; MMP, mitochondrial membrane potential.
After 0 h of incubation, no significant (p >0.05) decline in sperm motility was recorded at 5 µM Pb concentration in comparison to the control (Figure 2A). However, as the concentration was increased beyond 25 µM, a significant (p <0.05) reduction was observed. After 0.5 h of incubation, even 5 µM Pb concentration caused a significant (p <0.05) reduction in sperm motility. Similarly, after a longer incubation period (1 h), a significant (p <0.05) reduction in sperm motility was recorded even at 5 µM Pb concentration. Furthermore, in comparisons between the different incubation periods, it was observed that sperm motility significantly (p <0.001) decreased at 0.5 and 1 h of incubation relative to motility at 0 h for different Pb concentrations. Regarding sperm viability and membrane integrity, no significant (p >0.05) differences in comparison to the control were recorded at 5 µM Pb concentration after 0, 0.5, or 1 h of incubation (Figure 2B). However, there was a significant reduction (p <0.05) after the different incubation periods as the concentration was increased beyond 10 μM Pb. Furthermore, in comparisons between the different incubation periods, it was observed that sperm viability and membrane integrity significantly (p <0.001) decreased after 0.5 and 1 h of incubation relative to measures at 0 h for different Pb concentrations. Regarding sperm MMP, no significant (p >0.05) reduction was seen at 10 µM Pb concentration in comparison to the control at 0 h of incubation (Figure 2C). However, sperm MMP significantly (p <0.05) declined when the concentration was increased to 25 µM and beyond. Similarly, a significantly (p <0.05) declining trend was observed at 10 µM Pb concentration after 0.5 and 1 h of incubation. Furthermore, in comparisons between different incubation periods, it was observed that sperm MMP significantly (p <0.001) decreased at 0.5 and 1 h of incubation relative to MMP at 0 h for different Pb concentrations.
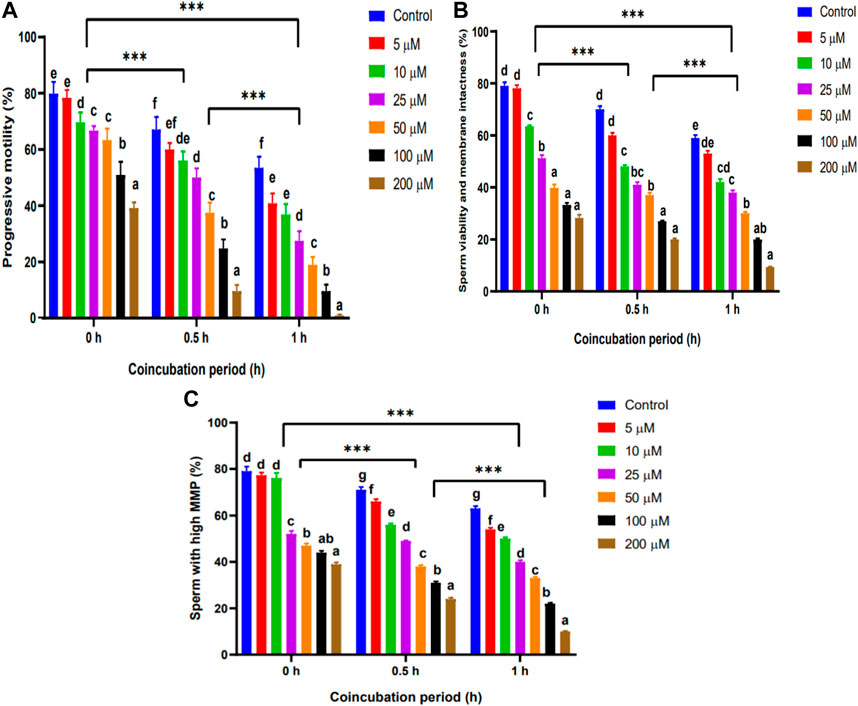
FIGURE 2. Effect of different concentrations of lead on sperm functional attributes after different co-incubation periods. (A) Effect of Pb on sperm progressive motility (%). (B) Effect of Pb on sperm viability and membrane integrity (%). (C) Effect of Pb on sperm MMP (%). Different superscripts indicate significant differences in means between the different treatment groups (p <0.05). ***p <0.001 (indicating significant differences under different incubation periods). Abbreviations: Pb, lead; MMP, mitochondrial membrane potential.
We observed a significant (p <0.05) decline in sperm motility at 10 mM F concentration in comparison to the control after 0 h of incubation (Figure 3A). A similar trend was seen after 0.5 and 1 h of incubation for a lower concentration of F (5 mM). Furthermore, in comparisons between different incubation periods, it was observed that sperm motility significantly (p <0.001) decreased after 0.5 and 1 h of incubation in comparison to motility at 0 h for different F concentrations. Regarding sperm viability and membrane integrity, after 0 h of incubation, a significant (p <0.05) reduction was seen higher concentrations (Figure 3B). After 0.5 h of incubation, a significant (p <0.01) decline was recorded even at lower doses of F (5 mM concentration and beyond). Furthermore, in comparisons between different incubation periods, it was observed that sperm viability significantly (p <0.001) decreased after 0.5 and 1 h of incubation. Regarding sperm MMP, no significant reduction was observed (p >0.05) at 5 mM F concentration after 0 h (Figure 3C). However, as the incubation period was increased to 0.5 h, even 5 mM F caused a significant reduction in sperm MMP.
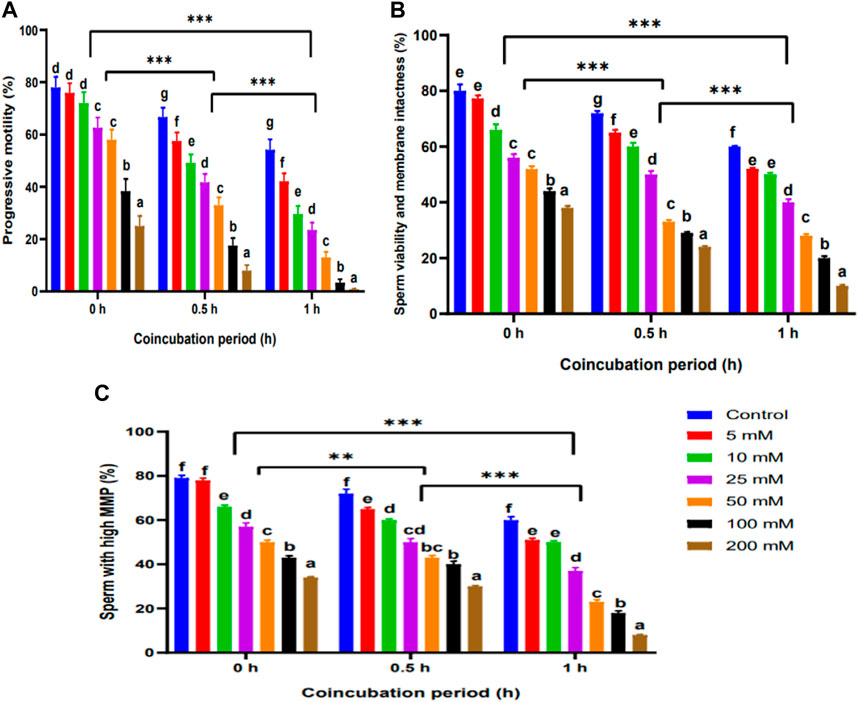
FIGURE 3. Effect of different concentrations of fluoride on sperm functional attributes after different co-incubation periods. (A) Effect of F on sperm progressive motility (%). (B) Effect of F on sperm viability and membrane integrity (%). (C) Effect of F on sperm MMP (%). Different superscripts indicate significant differences in means between the different treatment groups (p <0.05). **p <0.01; ***p <0.001 (indicating significant differences under different incubation periods). Abbreviations: F, fluoride; MMP, mitochondrial membrane potential.
In the experiment examining the As–F combination, even at 0 and 0.5 h of incubation, sperm motility significantly reduced at 5 µM As + 5 mM F in comparison to the control. (Figure 4A). A similar trend was observed for sperm viability (Figure 4B) and sperm MMP (Figure 4C), whereby 5 μM As + 5 mM F caused a significant (p <0.05) reduction in these parameters in comparison to the control. Similarly, in the case of the As–Pb combination, at 0 h, with the lower concentration of 5 μM As + 5 mM Pb, a significant (p < 0.05) reduction in sperm motility was observed (Figure 5A). Similar results were obtained regarding sperm viability (Figure 5B) and sperm MMP (Figure 5C), with a significant (p <0.05) decrease observed after each incubation period when sperm was incubated with a combination of 5 μM As + 5 mM Pb. Overall, a highly significant (p <0.001) decrease in sperm MMP was recorded if sperm was incubated for longer. Similarly, in the case of the Pb + F combination, we observed a significant (p <0.05) decrease in sperm motility even at 5 µM Pb + 5 mM F in comparison to the control after each incubation period (Figure 6A). Furthermore, a highly significant (p <0.001) reduction in sperm motility was recorded after longer periods of incubation. We also observed a significant (p <0.05) decrease in sperm viability after 0 and 1 h of incubation if sperm was incubated with 5 μM Pb + 5 mM F, although this was not the case after 0.5 h (Figure 6B). As the concentration was increased, a significant (p <0.05) decrease in the parameters was observed for all incubation periods (0, 0.5, and 1 h). Similarly, sperm MMP also showed a significantly (p <0.05) declining trend even at the lowest concentration of this heavy metal combination (5 μM Pb + 5 mM F) in comparison to the control (Figure 6C).
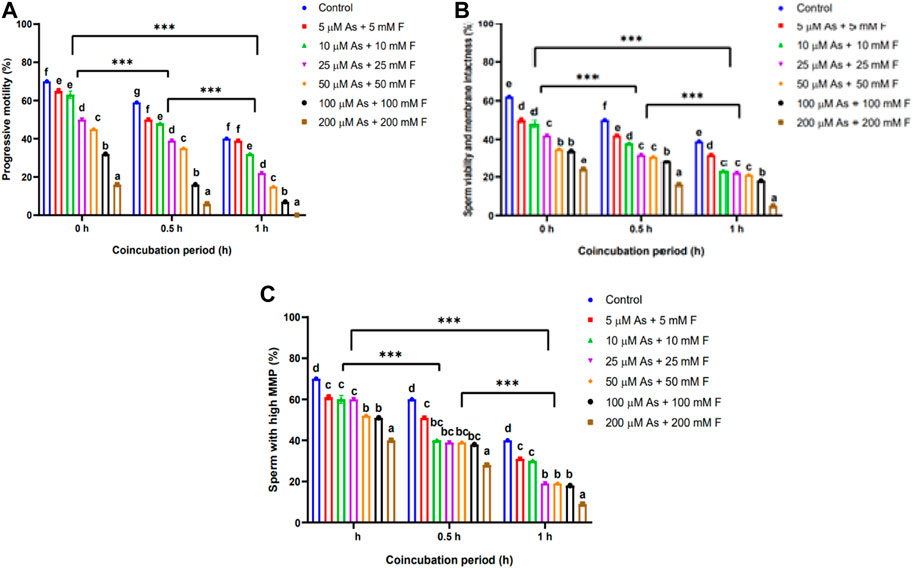
FIGURE 4. Effect of arsenic and fluoride in combination at different concentrations on sperm functional attributes after different co-incubation periods. (A) Combined effect of As–F on sperm progressive motility (%). (B) Combined effect of As–F on sperm viability and membrane integrity (%). (C) Combined effect of As–F on sperm MMP (%). Different superscripts indicate significant differences in means between the different treatment groups (p <0.05). ***p <0.001 (indicating significant differences under different incubation periods). Abbreviations: As, arsenic; F, fluoride; MMP, mitochondrial membrane potential.
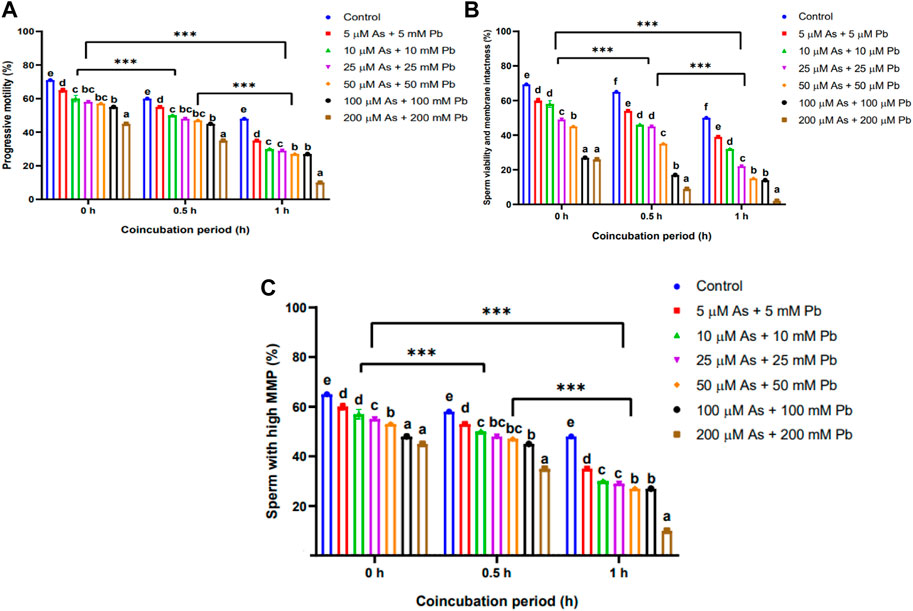
FIGURE 5. Effect of arsenic and lead in combination at different concentrations on sperm functional attributes after different co-incubation periods. (A) Combined effect of As–Pb on sperm progressive motility (%). (B) Combined effect of As–Pb on sperm viability and membrane integrity (%). (C) Combined effect of As–Pb on sperm MMP (%). Different superscripts indicate significant differences in means between the different treatment groups (p <0.05). ***p <0.001 (indicating significant differences under different incubation periods). Abbreviations: As, arsenic; Pb, lead; MMP, mitochondrial membrane potential.
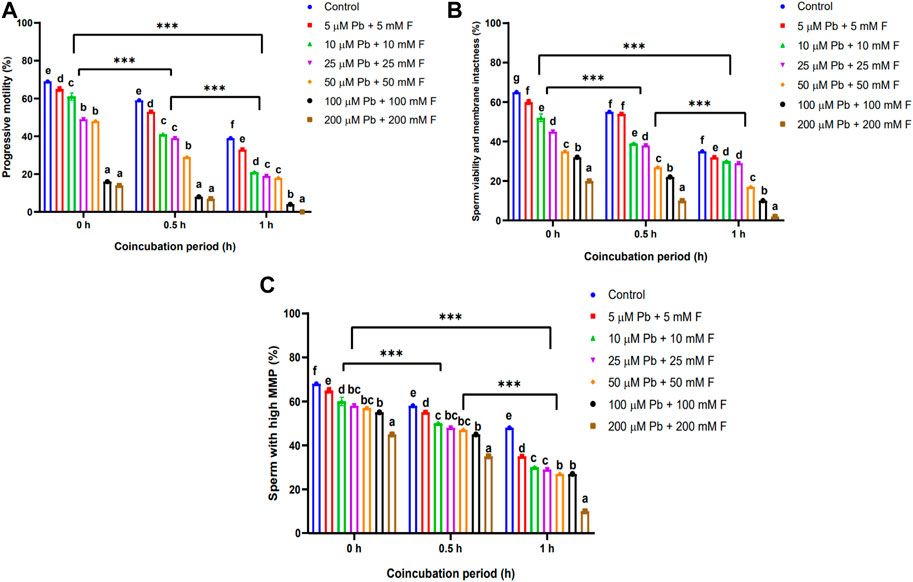
FIGURE 6. Effect of lead and fluoride in combination at different concentrations on sperm functional attributes after different co-incubation periods. (A) Combined effect of Pb–F on sperm progressive motility (%). (B) Combined effect of Pb–F on sperm viability and membrane integrity (%). (C) Combined effect of Pb–F on sperm MMP (%). Different superscripts indicate significant differences in means between the different treatment groups (p <0.05). ***p <0.001 (indicating significant differences under different incubation periods). Abbreviations: Pb, lead; F, fluoride; MMP, mitochondrial membrane potential.
Among all toxic pollutants, humans and animals have been increasingly exposed in particular to heavy metals (particularly As, Pb, and F) due to their industrial uses, biomedical applications, and use in other diagnostic tools in recent years. Toxic metals may have adverse effects on the reproductive system, either directly if they target specific reproductive organs or indirectly when they act on the neuroendocrine system (Pandey and Jain, 2013). The current study focused on the cytotoxic effects of different concentrations of As, Pb, and F, and combinations of these, on sperm functional attributes in vitro. The sperm functional attributes analyzed were observed to deteriorate in a dose- and time-dependent manner under incubation with different concentrations of As, Pb, and F, separately and in combination.
Sperm motility is crucial for male fertility, and lower sperm motility can cause male infertility, as reported in Han Chinese men (Tang et al., 2017). Many recent in vitro studies have shown that As exposure can reduce sperm motility and male fertility (Lima et al., 2018; Zeng et al., 2018). In this study, sperm motility was evidently reduced in a dose-dependent manner when sperm were incubated in different concentrations of As, a finding that is in agreement with previous reports in different laboratory animals (Pant et al., 2004; Zeng et al., 2019). A possible mechanism underlying the decrease in sperm motility might be associated with direct binding of As to sperm (Uckun et al., 2002). A recent study has reported on the partial impairment of spermatogenesis through disorganization of the elongation of spermatids due to As toxicity (Han et al., 2020).
Our findings on sperm membrane integrity corroborated those of earlier reports, whereby exposure to As has been found to cause reduction in sperm membrane integrity in mice (Reddy et al. (2011) and rabbit bucks (Seadawy et al., 2014). Similarly, another study documented a significant reduction in sperm viability when sodium arsenite was fed orally to experimental rats (Momeni and Eskandari, 2012). Exposure to As may induce cell death or apoptosis in the testicular germ cells or somatic Sertoli cells in vitro (Kim et al., 2011). Therefore, it might be possible that apoptosis-related cellular events were more prominent when sperm cells were co-incubated with increased concentrations of As. In this regard, it has also been reported that exposure of cells to As generates reactive oxygen species (ROS), in turn inducing cell death via both caspase-dependent and caspase-independent pathways; this is concomitant with downregulation of p53 and arrest of the cell cycle (Kim et al., 2011). Mitochondria play a crucial role in ATP synthesis and are the major energy producers for sperm motility. In this study, we have reported a significant reduction in sperm MMP upon incubation of sperm with various concentrations of As. Similarly, previous studies have shown that As causes mitochondrial dysfunction, resulting in damage to the structural and functional activity of the spermatozoa (Ulloa-Rodriguez et al., 2017; Keshavarz Bahaghighat et al., 2018; Losano et al., 2018). There are also reports relating As to a rapid decrease in MMP, thus changing the activities of mitochondrial enzymes, resulting in notable changes in morphology and destruction of the internal integrity of the organ, consequently disrupting cell morphology and sperm viability (De Vizcaya-Ruiz et al., 2009). In addition, toxicity caused by sodium arsenite due to generation of oxidative stress and apoptosis of the mitochondria has been reported in rat sperm (Das et al., 2009).
The current study also assessed the possible consequences of Pb exposure with varying concentrations on in vitro sperm functional attributes in boar semen. Pb, as a heavy metal, is widely used in the manufacture of products for daily use, including paints, lead acids, pigments, and varnishes, and human and animal exposure to Pb causes detrimental effects for male reproductive function, including decreased semen quality, thereby causing male infertility (Abadin et al., 2007). We have reported a significant reduction in boar sperm quality in terms of sperm motility, sperm membrane integrity, and sperm MMP after co-incubation with Pb, with effects occurring in a dose- and time-dependent manner. Our findings were congruent with the reports of Li et al. (2018), who reported a significant reduction in sperm quality parameters and DNA integrity in mice on exposure to Pb. The cellular pathways relating to Ca++ control sperm motility and act as an indirect measure for sperm mitochondrial function. Pb, being a divalent metal, can mimic Ca++ entry and its functions, thereby affecting the sperm capacitation process by inhibiting or inducing tyrosine phosphorylation (Kushwaha et al., 2021). The reduction in sperm quality observed in this study may be due to Pb exposure, which is thought to generate ROS in sperm cells, and an increase in ROS can decrease sperm membrane fluidity (Barbier et al., 2010). These findings support our hypothesis regarding the potential toxicity of Pb for sperm function even at micro levels in a dose- and time-dependent manner.
We have also reported a significant reduction in sperm quality attributes after incubation with F, with effects occurring in a dose- and time-dependent manner. Similarly, previous studies have also documented reduced sperm count and increased sperm abnormalities in mice exposed to F-contaminated drinking water (Wei et al., 2016; Sun et al., 2017). Toxic effects of NaF and F on male reproduction have been reported, taking the form of reduced sperm motility, testicular steroidogenesis, increased sperm abnormalities, histological alterations in the testis, and the loss of different stages of spermatozoa and spermatogenesis in the lumen of the seminiferous tubules of the testis (Chaithra et al., 2020). Furthermore, recent studies have documented the finding that F exposure can lead to mitochondrial damage and ROS accumulation, leading to mitochondrial fission/fusion imbalances (Zhou et al., 2020). F toxicity has been found to cause mitochondrial damage by decreasing the mitochondrial membrane potential, which promotes an increase in the production of ROS, and a higher level of ROS results in an increase in abnormal spermatozoa and decreased sperm motility, which in turn affects fertility (Wang et al., 2003). Therefore, we speculate that co-incubation of sperm with F might have resulted in increased ROS generation, which might have interacted with purine and pyrimidine bases to increase the content of messenger RNA, destroying single or double strands of DNA and DNA-dependent proteases, resulting in sperm cell apoptosis.
The combined effects of different concentrations of heavy metals on sperm functional attributes in spermatozoa are poorly documented in human and animal models as of now. In the present study, co-incubation with combinations of different concentrations of As, Pb, and F was found to significantly reduce sperm motility, viability, and MMP in a dose- and time-dependent manner. It was also evident from our findings that combinations of heavy metals were far more toxic, even at the lowest concentration and irrespective of the incubation period, than their individual counterparts, suggesting that heavy metals in combination might act synergistically in mediating the cytotoxic effects on the sperm membrane, thereby damaging sperm fluidity. One previous report on human subjects supports our current findings, whereby heavy metals were found to interact either additively, synergistically, or antagonistically (ATSDR, 1999). The toxicity of heavy metals is dose-dependent, and high-dose exposure leads to severe responses in animals and humans, causing more DNA damage (Gorini et al., 2014). The toxic mechanisms of heavy metals function in similar pathways, usually via ROS generation, enzyme inactivation, and suppression of the antioxidant defense (Balali-Mood et al., 2021). However, some of them cause toxicity in a particular pattern and bind selectively to specific macromolecules. Therefore, more well-designed in vitro investigations should be conducted in order to validate the complicated relationship between these metals and male fertility factors.
The present study is the first of its kind to have demonstrated the cytotoxicity of As, Pb, and F separately and in combination in a dose- and time-dependent manner in terms of boar semen quality in vitro. Moreover, the environment is frequently contaminated with various heavy metals, so it is imperative that in vivo studies on large animal populations are conducted to validate the toxicity of As, Pb, and F, individually and in combination, on sperm functional attributes in a broader sense. The current findings may be of practical significance in the field of livestock and other wild animal species that are frequently exposed to a wide range of environmental contaminants through their food chain.
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding author.
The animal study was approved by the Institutional Animal Ethics Committee of ICAR Research Complex for the NEH Region, Umiam, Meghalaya. The study was conducted in accordance with the local legislation and institutional requirements.
GK: conceptualization, methodology, project administration, writing–original draft, and writing–review and editing. JD: investigation and writing–original draft. SD: conceptualization, methodology, validation, and writing–review and editing. RD: data curation, formal analysis, and writing–original draft. SA: data curation, formal analysis, investigation, writing–original draft, and writing–review and editing. PM: data curation and writing–review and editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The research was funded by the Indian Council of Agricultural Research (ICAR) Complex for the North Eastern Hill Region through an in-house project.
The authors thankfully acknowledge the Director, ICAR Research Complex for the North Eastern Hill Region, for granting necessary permissions and providing the facilities to carry out the work.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abadin, H., Ashizawa, A., Stevens, Y., Llados, F., Diamond, G., SageQuinones, G., et al. (2007). Toxicological profile for lead. Atlanta (GA): Agency for Toxic Substances and Disease Registry US. Chemical and Physical Information.
Alam, M. S., and Silpa, M. V. (2020). “Indo Australian workshop transfer of mitigastion technologies for heat stress in farm animals 5–7 February 2020,” in Impacts of heavy metal feed contaminants in cattle farming, Bangalore, India, 147–152. (accessed on 1 September 2021).
ATSDR (1999). “Toxicological profile for mercury [update],” in Agency for toxic substances and disease registry (Atlanta, GA, USA: US Department of Health and Human Services. Public Health Service).
Balali-Mood, M., Naseri, K., Tahergorabi, Z., Khazdair, M. R., and Sadeghi, M. (2021). Toxic mechanisms of five heavy metals: mercury, lead, chromium, cadmium, and arsenic. Front. Pharmacol. 12, 643972. doi:10.3389/fphar.2021.643972
Barbier, O., Arreola-Mendoza, L., and Del Razo, L. M. (2010). Molecular mechanisms of fluoride toxicity. Chem. Biol. Interact. 188, 319–333. doi:10.1016/j.cbi.2010.07.011
Carvalho, C. M., Zhang, F., and Lupski, J. R. (2011). Structural variation of the human genome mechanisms, assays, and role in male infertility. Syst. Biol. Reprod. Med. 57 (1-2), 3–16. doi:10.3109/19396368.2010.527427
Chaithra, B., Sarjan, H. N., and Shivabasavaiah, E. (2020). A comparative analysis of fluoride-contaminated groundwater and sodium fluoride-induced reproductive toxicity and its reversibility in male rats. Biol. Trace Elem. Res. 197, 507–521. doi:10.1007/s12011-019-01994-y
Chowdhury, A. R. (2009). Recent advances in heavy metals induced effect on male reproductive function-A retrospective. Al Ameen J. Med. Sci. 2 (2), 37–42.
Das, J., Ghosh, J., Manna, P., Sinha, M., and Parames, S. C. (2009). Taurine protects rat testes against NaAsO(2)-induced oxidative stress and apoptosis via mitochondrial dependent and independent pathways. Toxicol. Lett. 187, 201–210. doi:10.1016/j.toxlet.2009.03.001
De Vizcaya-Ruiz, A., Barbier, O., Ruiz-Ramos, R., and Cebrian, M. E. (2009). Biomarkers of oxidative stress and damage in human populations exposed to arsenic. Mutat. Res. 674, 85–92. doi:10.1016/j.mrgentox.2008.09.020
Gazwi, H. S. S., Yassien, E. E., and Hassan, H. M. (2020). Mitigation of lead neurotoxicity by the ethanolic extract of Laurus leaf in rats. Ecotoxicol. Environ. Safe. 192, 110297. doi:10.1016/j.ecoenv.2020.110297
Gorini, F., Muratori, F., and Morales, M. A. (2014). The role of heavy metal pollution in neurobehavioral disorders: a focus on autism. Rev. J. Autism Dev. Disord. 1 (4), 354–372. doi:10.1007/s40489-014-0028-3
Han, Y., Liang, C., Manthari, R. K., Yu, Y., Gao, Y., Liu, Y., et al. (2020). Arsenic influences spermatogenesis by disorganizing the elongation of spermatids in adult male mice. Chemosphere 238, 124650. doi:10.1016/j.chemosphere.2019.124650
Keshavarz-Bahaghighat, H., Sepand, M. R., Ghahremani, M. H., Aghsami, M., Sanadgol, N., Omidi, A., et al. (2018). Acetyl-L-carnitine attenuates arsenic-induced oxidative stress and hippocampal mitochondrial dysfunction. Biol. Trace Elem. Res. 184, 422–435. doi:10.1007/s12011-017-1210-0
Kim, Y. J., Chung, J. Y., Lee, S. G., Kim, J. Y., Park, J. E., Kim, W. R., et al. (2011). Arsenic trioxide-induced apoptosis in TM4 Sertoli cells: the potential involvement of p21 expression and p53 phosphorylation. Toxicology 285, 142–151. doi:10.1016/j.tox.2011.04.013
Knazicka, Z., Tvrda, E., Bardos, L., and Lukac, N. (2012). Dose- and time-dependent effect of copper ions on the viability of bull spermatozoa in different media. J. Environ. Sci. Health 47, 1294–1300. doi:10.1080/10934529.2012.672135
Kukov, A., Daskalova, D., Ivanova-Kicheva, M., Stefanov, R., and Neicheva, A. (2009). Immunocytochemical localization of separated seminal plasma proteins on the ram's sperm plasma membrane during in vitro preservation at 4ºC. Biotechnol. Anim. Husb. 25, 925–934. doi:10.2164/jandrol.04172
Kumar, N., and Singh, A. K. (2015). Trends of male factor infertility, an important cause of infertility: a review of literature. J. Hum. Reprod. Sci. 8, 191–196. doi:10.4103/0974-1208.170370
Kushwaha, B., Beniwal, R., Mohanty, A., Singh, A. K., Yadav, R. K., and Garg, S. K. (2021). Effect of heavy metals on tyrosine kinases signaling during sperm capacitation. Infertil. Assisted Reproduction 157. doi:10.5772/intechopen.99261
Li, C., Zhao, K., Zhang, H., Liu, L., Xiong, F., Wang, K., et al. (2018). Lead exposure reduces sperm quality and DNA integrity in mice. Environ. Toxicol. 33, 594–602. doi:10.1002/tox.22545
Lima, G. D. A., Sertorio, M. N., Souza, A. C. F., Menezes, T. P., Mouro, V. G. S., Gonçalves, N. M., et al. (2018). Fertility in male rats: disentangling adverse effects of arsenic compounds. Reprod. Toxicol. 78, 130–140. doi:10.1016/j.reprotox.2018.04.015
Losano, J. D. A., Angrimani, D. S. R., Ferreira Leite, R., Simoes da Silva, B. D. C., Barnabe, V. H., and Nichi, M. (2018). Spermatic mitochondria: role in oxidative homeostasis, sperm function and possible tools for their assessment. Zygote 26, 251–260. doi:10.1017/S0967199418000242
Maartens, P. J., Aboua, Y. G., and du Plessis, S. S. (2015). “Role of environmental factors and gonadotoxin exposure in unexplained male infertility,” in Unexplained infertility: pathophysiology, evaluation and treatment. Editors G. L. Schattman, S. C. Esteves, and A. Agarwal (New York: Springer), 121–138. Ch.12.
Mendiola, J., Moreno, J. M., Roca, M., Vergara-Juarez, N., Martinez-Garcia, M. J., Garcia-Sanchez, A., et al. (2011). Relationships between heavy metal concentrations in three different body fluids and male reproductive parameters: a pilot study. Environ. Health Perspect. 10, 6–7. doi:10.1186/1476-069X-10-6
Momeni, H. R., and Eskandari, N. (2012). Effect of vitamin E on sperm parameters and DNA integrity in sodium arsenite-treated rats. Iran. J. Reprod. Med. 10, 249–256.
Nickson, R. T., McArthur, J., Shrestha, J. M., Kyaw-Myint, B., and Lowry, T. (2005). Arsenic and other drinking water quality issues, Muzaffargarh District, Pakistan. Appl. Geochem. 20, 55–68. doi:10.1016/j.apgeochem.2004.06.004
Pandey, G., and Jain, G. C. (2013). A Review on toxic effects of aluminium exposure on male reproductive system and probable mechanisms of toxicity. Int. J. Toxicol. Appl. Pharmacol. 3, 48–57.
Pant, N., Murthy, R. C., and Srivastava, S. P. (2004). Male reproductive toxicity of sodium arsenite in mice. Hum. Exp. Toxicol. 23 (8), 399–403. doi:10.1191/0960327104ht467oa
Reddy, M. V. B., Sudheer, S. D., Sasikala, P., Reddy, P. S., Reddy, S. H., and Karthik, A. (2011). Effect of transplacental and lactational exposure to arsenic on male reproduction in mice. J. Reprod. Infertil. 2, 41–45.
Renu, K., Madhyastha, H., Madhyastha, R., Maruyama, M., Vinayagam, S., and Gopalakrishnan, A. V. (2018). Review on molecular and biochemical insights of arsenic-mediated male reproductive toxicity. Life Sci. 212, 37–58. doi:10.1016/j.lfs.2018.09.045
Seadawy, I. E. E., Walid, S., El-Nattat, M. M., El-Tohamy, H. A., and El-Rahman, A. (2014). The influence of curcumin and ascorbic acid on libido and semen characteristics of arsenic-exposed rabbit bucks. World Appl. Sci. J. 32, 1789–1794.
Selvaraju, S., Ravindra, J. P., Ghosh, J., Gupta, P. S. P., and Suresh, K. P. (2008). Evaluation of sperm functional attributes in relation to in vitro sperm zona pellucida binding ability and cleavage rate in assessing frozen thawed buffalo (Bubalus bubalis) semen quality. Anim. Reprod. Sci. 106, 311–321. doi:10.1016/j.anireprosci.2007.05.005
Shankar, S., Shanker, U., and Shikha, (2014). Arsenic contamination of groundwater: a review of sources, prevalence, health risks, and strategies for mitigation. Sci. World J. 2014, 1–18. doi:10.1155/2014/304524
Sun, Z., Xue, X., Zhang, Y., Niu, R., and Wang, J. (2017). Effect of sodium fluoride on the sperm mitochondrial DNA in mice. Biochem. Biophys. Res. Commun. 492, 295–299. doi:10.1016/j.bbrc.2017.08.129
Tang, S., Wang, X., Li, W., Yang, X., Li, Z., Liu, W., et al. (2017). Biallelic mutations in CFAP43 and CFAP44 cause male infertility with multiple morphological abnormalities of the sperm flagella. Am. J. Hum. Genet. 100, 854–864. doi:10.1016/j.ajhg.2017.04.012
Uckun, F. M., Liu, X. P., and D’Cruz, O. J. (2002). Human sperm immobilizing activity of aminophenyl arsenic acid and its N-substituted quinazoline, pyrimidine, and purine derivatives: protective effect of glutathione. Reprod. Toxicol. 16, 57–64. doi:10.1016/S0890-6238(01)00195-2
Ulloa-Rodriguez, P., Figueroa, E., Diaz, R., Lee-Estevez, M., Short, S., and Farias, J. G. (2017). Mitochondria in teleost spermatozoa. Mitochondrion 34, 49–55. doi:10.1016/j.mito.2017.01.001
Verma, R., Vijayalakshmy, K., and Chaudhiry, V. (2018). Detrimental impacts of metals on animal reproduction: a review. J. Ento. Zool. Stud. 6 (6), 27–30.
Wang, X., Sharma, R., Gupta, A., George, V., Thomas, A. J., Falcone, T., et al. (2003). Alterations in mitochondria membrane potential and oxidative stress in infertile men: a prospective observational study. Fertil. Steril. 80, 844–850. doi:10.1016/S0015-0282(03)00983-X
Wei, R., Luo, G., Sun, Z., Wang, S., and Wang, J. (2016). Chronic fluoride exposure-induced testicular toxicity is associated with inflammatory response in mice. Chemosphere 153, 419–425. doi:10.1016/j.chemosphere.2016.03.045
Zeng, Q., Yi, H., Huang, L., An, Q., and Wang, H. (2018). Reduced testosterone and Ddx3y expression caused by long -term exposure to arsenic and its effect on spermatogenesis in mice. Environ. Toxicol. Pharmacol. 63, 84–91. doi:10.1016/j.etap.2018.08.012
Zeng, Q., Yi, H., Huang, L., An, Q., and Wang, H. (2019). Long -term arsenite exposure induces testicular toxicity by redox imbalance, G2/M cell arrest and apoptosis in mice. Toxicology 411, 122–132. doi:10.1016/j.tox.2018.09.010
Zhao, P., Guo, Y., Zhang, W., Chai, H., Xing, H., and Xing, M. (2017). Neurotoxicity induced by arsenic in Gallus Gallus: regulation of oxidative stress and heat shock protein response. Chemosphere 166, 238–245. doi:10.1016/j.chemosphere.2016.09.060
Keywords: cytotoxicity, arsenic, lead, fluoride, sperm attributes, boar semen, heavy metals
Citation: Kadirvel G, Diengdoh J, Deori S, Dewry RK, Abedin SN and Moirangthem P (2023) Cytotoxic effects of heavy metals on functional attributes of boar sperm: an in vitro study. Front. Environ. Sci. 11:1296606. doi: 10.3389/fenvs.2023.1296606
Received: 18 September 2023; Accepted: 23 October 2023;
Published: 16 November 2023.
Edited by:
Zhenming Zhang, Guizhou University, ChinaReviewed by:
Wen-Jun Shi, South China Normal University, ChinaCopyright © 2023 Kadirvel, Diengdoh, Deori, Dewry, Abedin and Moirangthem. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Govindasamy Kadirvel, dmVsdmV0LjIwMDdAcmVkaWZmbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.