
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Environ. Sci., 10 April 2023
Sec. Atmosphere and Climate
Volume 11 - 2023 | https://doi.org/10.3389/fenvs.2023.1085103
This article is part of the Research TopicImpact of Climate Change on the Human Living EnvironmentView all 24 articles
Asthma is a chronic respiratory disease resulting from a complex interaction between genetic and environmental factors. Many environmental factors have been associated with incidence or prevalence of asthma although there is still limited knowledge of major environmental causes of asthma in the general population. This study, for the first time, investigated the effects of climatic and geographical variability on asthma hospitalization among an adult population living in Fars province, southwest Iran. During the study period, the home addresses of patients hospitalized with acute asthma from 2016 to 2019 were mapped. The effects of geo-climatic factors including temperature, rainfall, humidity, evaporation, number of rainy and frosty days, slope, and land covers were assessed on adult asthma hospitalization by Geographical Information System (GIS). Data were analyzed using univariate and multivariate binary logistic regression. A total of 349 patients were recruited, including 157 (44.98%) males and 192 (55%) females. The mean age was 57.77 ± 18.84 years, ranging from 19 to 98 years. Asthmatic patients came from a total of 82 points including villages, towns, and cities. In the univariate analysis, urban setting (OR = 13) and Mean Annual Rainy Days (OR = 1.03) were identified as the factors associated with increased asthma hospitalization, while Mean Annual Temperature (MAT) (OR = 0.927), MinMAT (OR = 0.933), MaxMAT (OR = 0.925), Mean Annual Evaporation (MAE) (OR = 0.999), and slope (OR = 0.925) negatively affected asthma hospitalization. Urban setting was considered the only significant factor in multivariate analysis (OR = 11.026). The major risk zones for adulthood acute asthma in southwest Iran were urban settings and areas with higher numbers of rainy days, lower temperatures, and evaporation at lower slopes.
Asthma is a chronic respiratory condition affecting about 300 million people worldwide (Stern et al., 2020). Its prevalence, severity, and mortality vary globally. Environmental and genetic factors, atopic comorbidities, and social determinants influence the disease’s incidence, prevalence, and mortality (Stern et al., 2020).
Meteorological determinants such as temperature, rainfall, or humidity play a prominent role in asthma occurrence. Research is undertaken to evaluate the global association between asthma prevalence and global meteorological variability (Cong et al., 2017; Xing et al., 2018). The impact of climatic factors on the pollen season, associated with the incidence and severity of asthma exacerbation, has been studied, and the relationship with airway infectious diseases and air pollution (D'Amato et al., 2015; Campbell-Lendrum and Prüss-Ustün, 2019). Geographical variation across different areas has also been determined as the main factor for asthma emergencies (Newson et al., 2014; Simunovic et al., 2021).
Different methods are used to evaluate the association between asthma hospitalization and geo-climatic variability. In this way, the Geographical Information System (GIS), a computer system that analyzes and displays geographically referenced information, can be helpful for health scientists to determine the effects of geo-climatic parameters on disease prevalence and occurrence (Aghajani et al., 2017; Ghatee et al., 2020a; Pande et al., 2021; Gautam et al., 2022). In the context of asthma, there are limited GIS-based studies showed a direct association between asthma occurrence and vegetation land cover (Khan et al., 2010), allergens (Keddem et al., 2015), plant pollens (Maya-Manzano et al., 2017), pollution (Gorai et al., 2014) and urban settings (Kanannejad et al., 2022). For acute asthma, remote-sensing and GIS methods help researchers to show nitrogen dioxide (NO2), Normalized Difference Vegetation Index (NDVI), and near-surface air temperature (Ta) as the main determinants of hospital admission due to asthma (Almeida et al., 2017).
In Iran with adult asthma prevalence about 8.9% in 2018 (Fazlollahi et al., 2018), some studies have been performed to investigate the environmental risk factors of asthma (Rabiee et al., 2018; Dastoorpoor et al., 2021; Idani et al., 2021). In some cases, this approach was developed using GIS method, especially in the Tehran and Esfahan provinces (Central of Iran), while there is no GIS-based study in south of Iran (Rashidi et al., 2013; Alizadeh et al., 2016; Khasha et al., 2018; Kaffash-Charandabi et al., 2019; Faraji et al., 2022). Most of these studies were performed to discover the association between air pollution and asthma prevalence, while geo-climatic factors were less under consideration. Only one study in Tehran, the capital of Iran, develop a Mobile GIS-based study based on air pollution and meteorological data to generate predictive algorithms for asthma attack (Khasha et al., 2018).
In this study, for the first time, we evaluated the geo-climatic risk factors of adult asthma hospitalization using GIS method in Fars province, southwest Iran. A better understanding of asthma hospitalization by geo-climatic areas can inform future policy development for managing asthma hospitalization in Fars province.
Fars province is located in the southwest of Iran, between longitude 27°31′N and 31° 42′N and latitude 50° 37′E and 55° 38′E. It covers an area of about 122,608 km2 with a total population of 4.6 million and male to female ratio of 1: 1.03. It comprises 24 counties and 8,191 residential places including small and large villages, with Shiraz as the capital city (Figure 1).
Fars province has three distinct climatic regions with an average temperature of 16.8°C, ranging between 4.7°C and 29.2°C. Its mountainous area has moderately cold winters and mild summers in the north and northwest while the central regions have been identified with relatively rainy mild winters and hot dry summers. The third region located in the south and southeast has cold winters and hot summers. Due to the geo-climatic variation of the province, the region has different land covers from dense forests to bare plains and elevations of 115–3,115 m above sea level (Ghatee et al., 2020b).
This retrospective study collected the medical data of 349 patients hospitalized with acute asthma at the Nemazee hospital of Shiraz, Iran, during 2016–2019. Nemazee is the leading respiratory hospital in Fars province admitting people from all parts of the province with varied socioeconomic statuses. Patients whose spatial information was incomplete or related to provinces other than Fars were excluded from the study. Some patients were contacted randomly to ensure the spatial information of patients. This study was approved by the Ethics Committee of Shiraz University of Medical Sciences (IR.SUMS.MED.REC.1400.297).
The point residence of all patients was extracted from their medical records and recorded on the map based on the latitudes and longitudes of each point. The land cover vector layers and Digital Elevation Model (DEM) raster layer were acquired from the Department of Natural Resources in Fars province. The slope raster map was drawn through the spatial analyst tool, based on DEM, by computing the maximal rate of variation in value between each cell and its adjacent cells. The land cover layer showed spatial data on the different physical characteristics of the surface of the province.
The meteorological and rainfall data including temperature, maximum and minimum temperature, humidity, evaporation, number of rainy and frosty days, sunny hours, and rainfall from 18 synoptic meteorological and 86 rain-gauge stations were acquired from the Fars Province Weather Bureau. The mean values of each data related to the period of study were calculated. The generated variables were including Mean Annual Temperature (MAT), Minimum Mean Annual Temperature (MinMAT), Maximum Mean Annual Temperature (MaxMAT), Mean Annual Evaporation (MAE), Mean Annual Humidity (MAH), Mean Annual Rainfall (MAR), Mean Annual Frosty Days (MAFD), Mean Annual Rainy Days (MARD), and Mean Annual Sunny Hours (MASH). The annual iso-hydral, iso-humid, and frost days’ raster layers were generated using the Kriging interpolation method, and iso-thermal, iso-evaporation, and rainy days’ raster layers using the tension-based Spline interpolation model with a resolution grid of 2 × 2 km.
Geospatial and climatic data were analyzed using Arc GIS version 10.1. The provincial villages and cities’ point shape file layer was extracted with the raster layers. The identity tool was used to compute the geometric intersection of the layer obtained from the extraction of all raster layers with NTR hazard (polyline) and land cover (polygonal) vector layers to develop the final layer in which each point represented the properties of all the overlapped identity features from the above-mentioned raster and vector layers. The attribute of this layer was converted to an excel format for statistical analysis.
Statistical analysis was based on the presence or absence of patient in each point. The effect of geo-climatic factors on acute asthma was assessed after the spatial description of patients in Fars province. In this regard, residential points data including asthma reported and non-reported villages and cities were extracted from final province villages/cities point layer and comparison of environmental and climatic factors was done between asthma reported and non-reported points using univariate and multivariate logistic regression models. The statistical analyses were performed using SPSS version 21.
In this study, 349 patients with acute asthma living in 82 points in Fars province were recruited, including 44.98% (n = 157) males and 55% (n = 192) females; while no hospitalized patient were reported from 8,109 residential places. Their mean age was 57.77 ± 18.84 years, ranging from 19 to 98 years. The mean number of days for hospitalization and duration of hospitalization were 1.77 ± 1.76 and 5.09 ± 13.36, respectively.
Adult cases with acute asthma were recruited from different areas of Fars province with varied climatic and geographical features. The climatic factors including MAT, MinMAT, MaxMAT, MAE, MAH, and MAR of 3 years ranged from 13.53°C to 27.38°C, 6.65°C–18.87°C, 20°C–31.79°C, 1659.5–3,308.2°mm, 31.66%–41.93%, and 133.57–607.58°mm, respectively, among the points with acute asthma in adults (Figures 2, 3). MARD, MAFD, and MASH were 16.77–60.04 days, 0.19–87.01 days, and 2482.51–3,602.52 h for these points, respectively (Figure 4). The range of DEM and slope varied from 349 to 2233 m and 0–28.37°, respectively (Figure 5).
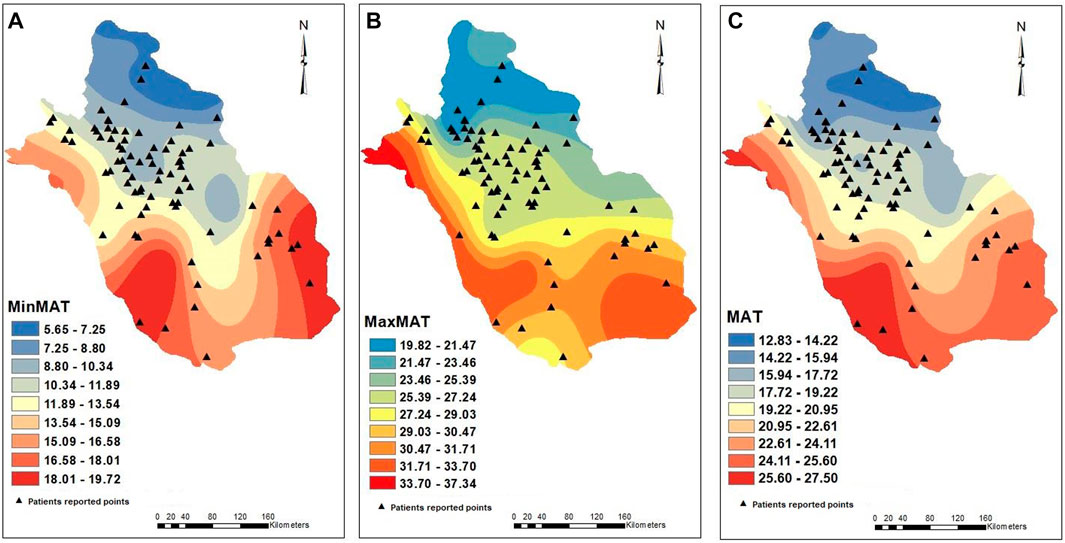
FIGURE 2. Isothermal raster models. Points with acute adult asthma (triangle symbol) located in areas with varied range of MinMAT (A), MaxMAT (B), and MAT (C).
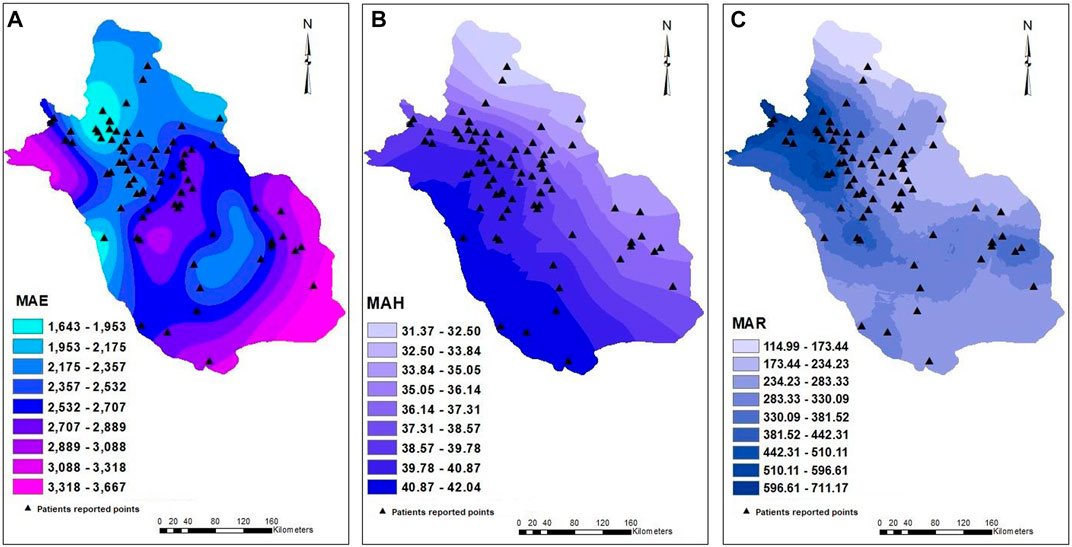
FIGURE 3. Points with acute adult asthma (triangle symbol) located in areas with varied range of MAE (A), MAH (B), and MAR (C).
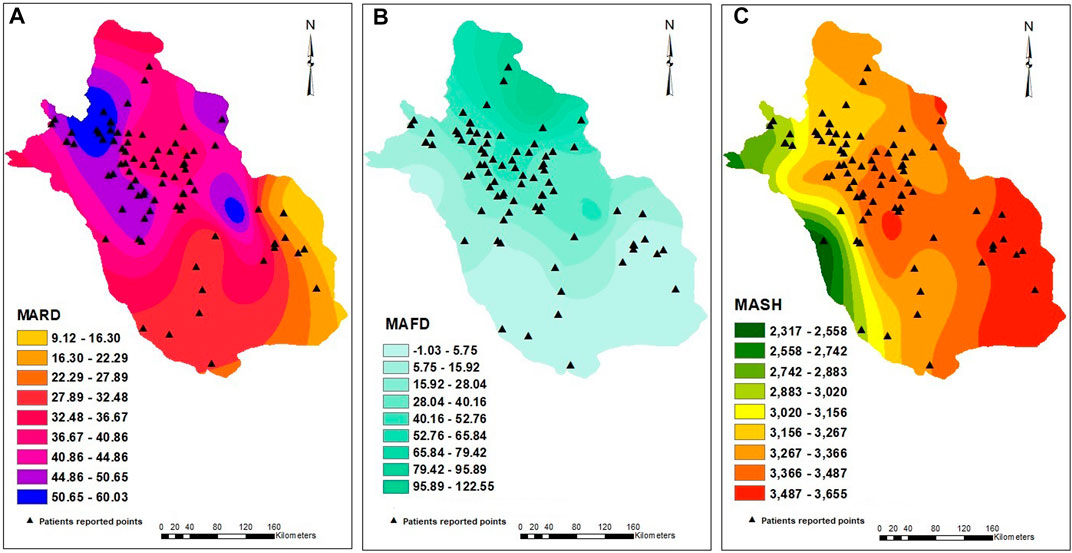
FIGURE 4. Points with acute adult asthma (triangle symbol) located in areas with varied range of MARD (A), MAFD (B), and MASH (C).
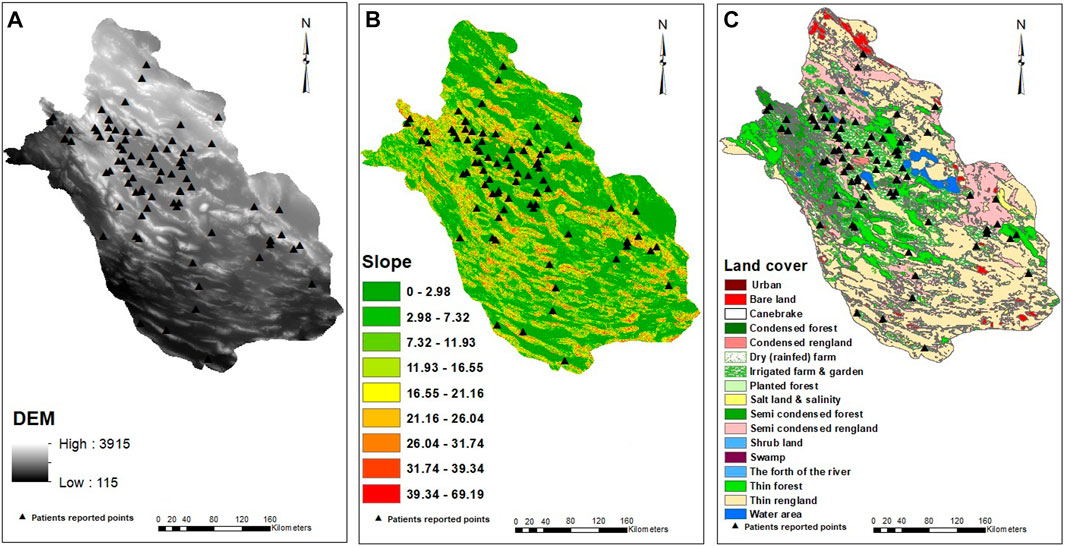
FIGURE 5. Patient distributions (triangle symbol) among areas with varied elevation (A), slope (B), and land covers (C).
The analysis showed MAT, MinMAT, MaxMAT, MAE, and MARD as significant climatic factors related to acute asthma occurrence. MARD was a factor (p = 0.025, OR = 1.030, CI = 1.004–1.058) increasing the probability of acute asthma by 3%/day, whilst there was a decreasing trend for MaxMAT (p = 0.008, OR = 0.925, CI = 0.873–0.980), MAT (p = 0.014, OR = 0.927, CI = 0.873–0.985), MinMAT (p = 0.035, OR = 0.933, CI = 0.875–0.995), and MAE (p = 0.013, OR = 0.999, CI = 0.999–1.000). Other climatic factors were not significant (Table 1). Max-MAT, MAT, MinMAT, and MAE decreased the probability of acute asthma occurrence by 0.075%, 0.073%, 0.067%, and 0.001%, respectively.
Urban setting was a significant variable, increasing the odds of acute asthma by 13 folds (p = 0.000, OR = 13, CI = 4.951–34.471) (Table 2). Other land covers were not associated with acute asthma.
Each degree increase in slope significantly reduced acute asthma by 7.5% (p = 0.008, OR = 0.925, CI = 0.873–0.979).
Multivariate binary logistic regression analysis was performed to reveal the concomitant effects of significant variables detected by univariate analysis. Urban setting (p = 0.000, OR = 11.026, CI = 3.808–31.928) was the only significant factor detected by multivariate analysis while other variables lost their significance (Table 3).
Asthma is a complex disease with multiple environmental factors suggested to contribute to etiology. Geographical analyses can shed light on the determinants of asthma. For the first time, this study was performed to investigate the geo-climatic risk factors of adult asthma hospitalization in Fars province, southwest Iran. We found that asthma hospitalization was affected mainly by significant climatic and environmental variables, including MAE, MaxMAT, MinMAT, MAT, MARD, slope, and urban settings.
MARD was a significant factor related to acute asthma in adults in the current study. The rainy days create humid and wet conditions resulting in homes being damp. Such conditions favor the growth of allergens like dust mites, mold, and fungi. Evidence supports that exposure to such indoor allergens is causally related to asthma incidence (Ghosh et al., 2018; Campo et al., 2019). Home dampness and molds are essential elements influenced by humidity levels and are associated with asthma symptoms (Williamson et al., 1997; Cox-Ganser, 2015). In addition, on rainy days, people prefer to stay at home, increasing exposure to these allergens. Similar to our study, Akpinar-Elci. et al. showed an increase in asthma visits during rainy months, while an inverse relationship was found by Wen-Chao Ho et al. (Ho et al., 2007; Akpinar-Elci et al., 2015). They explained that rainy days might interact with particulate matter (PM10), creating a washout effect (Ho et al., 2007; Akpinar-Elci et al., 2015).
A negative association between high temperature and asthma hospitalization was detected in our study. These results are consistent with some research in the field of asthma. A study by Son JY et al. in eight major cities in Korea found a significant association between asthma hospitalization and low temperature (Son et al., 2014). Similar results for childhood asthma were reported by Guo et al. in Shanghai (Guo et al., 2012). An increase in respiratory bacterial and viral infections associated with infiltration of inflammatory factors and mucus secretion has often followed a cold temperature, which may explain the effect of low temperature on asthma exacerbation (Li et al., 2011). However, some studies have demonstrated increased asthma hospitalization in high temperatures (Lin et al., 2009; Yamazaki et al., 2013). These different patterns of association between temperature and asthma geographically may be related to the effects of temperature on some asthma risk factors that differ in prevalence and seasonality by region (Buckley and Richardson, 2012). The impact of temperature on asthma exacerbation may also be related to differences in the levels of exposure, public health interventions, health and social care services, and susceptibility of subpopulations (Michelozzi et al., 2006; Anderson and Bell, 2011).
Evaporation was another significant factor negatively affecting asthma occurrence in this study. To our knowledge, this was the first evaluation of this factor in the literature. The rate of water evaporation depends on climatic factors such as temperature, solar radiation, wind, and relative humidity. Sunny, hot, dry, and windy conditions produce higher evaporation rates. This is consistent with our data that showed low acute asthma incidence in warm and low humidity conditions associated with increased evaporation. However, we failed to find a statistically significant value for humidity.
The urban setting was the most critical factor affecting asthma in this study. Previous asthma studies reported that urban lifestyle could affect individual health through industrial emissions, occupation, and daily use of products (Khan et al., 2010). Global urbanization is associated with increased environmental pollution caused by the combustion of fossil fuels, biomass, emissions from agriculture, and windborne mineral dust and organic matter. Higher PM2.5 and PM10 levels are associated with increased use of asthma medication, GP consultations, and hospitalization by activating cytokine pathways and inflammation in the airway (Nel et al., 1998; Nel, 2005; Brandt et al., 2015; Clifford et al., 2017). In addition to air pollution, the socioeconomic difference between urban and rural environments could affect the quality and access to healthcare and, finally asthma hospitalization. Urban locations generally tend to have a prototype environment that predisposes individuals to asthma, but it can be decreased if socioeconomic issues are addressed. Similar to our results, Solé et al. (2007) reported higher asthma prevalence among adolescents living in urban areas compared to the rural ones in Brazil. We previously found increased asthma hospitalization occurrences in urban regions of Fars province compared with rural areas (Kanannejad et al., 2022). The farming environment of rural areas is one explanation for lower asthma prevalence in such places (Strachan, 1989). Consumption of unpasteurized cow milk, exposure to farm animals, and fodder in rural areas may have a protective effect on asthma (Pechlivanis and von Mutius, 2020). Increased exposure to farm animals results in higher microbial exposures through which the protective effect might be mediated. Also, the consumption of unpasteurized milk can modulate cytokine production patterns toward the Th-1 (T helper-1) response, which could be responsible for the observed protective effect. One study reported that increased endotoxin exposure at birth was associated with a lower risk of allergic sensitization and eczema (Simpson et al., 2006). On the other hand, some studies have shown higher asthma occurrences in rural areas due to low-quality healthcare services, lower socioeconomic statuses, and cultural barriers to access to medicine compared with urban ones (Pesek et al., 2010; Roy et al., 2010).
The slope was another significant environmental factor affecting acute asthma occurrence in Fars province, where more asthma hospitalization was detected in areas with a lower pitch. Our previous study on childhood populations showed the powerful effect of slope on asthma hospitalization (Kanannejad et al., 2022). It may be related to higher population density in regions with a downward slope that usually is connected with increased air pollutants, nanoparticles, and transmissible infectious viral agents (Bröms et al., 2009). This study is the first of its kind which reflects slope effect on adult asthma, worldwide.
There are some limitations in this study. Poor adherence to prescribed medication is a cause of asthma exacerbation, which was not considered in this study. Therefore, the applied models do not predict factors responsible for individual-level hospitalization. In addition, daily mean concentrations of air pollutants as another leading cause of asthma attacks should be considered in future studies.
This retrospective study disclosed that major risk zones for acute asthma include urban settings and areas with higher numbers of rainy days, lower temperatures, and evaporation at lower slopes. GIS and spatial analysis techniques allow healthcare policy to understand the spatial distribution of asthma risk factors and develop surveillance strategies to protect asthmatic patients from the effects of risk factors.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by Ethic Committee of Shiraz University of Medical Sciences (IR.SUMS.MED.REC.1400.297).
ZK and SA: Development or design of methodology. MG: Analyzing data, and revising the manuscript. ZK: Writing and editing the manuscript. YS: Data gathering and writing the manuscript. SS: Revising the manuscript.
This study was extracted from the fellowship thesis written by Yousef Shokri and financially supported by Shiraz University of Medical Sciences (Grant no. 23943).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fenvs.2023.1085103/full#supplementary-material
Aghajani, J., Farnia, P., and Velayati, A. (2017). Impact of geographical information system on public health sciences. Biomed. Biotechnol. Res. J. (BBRJ) 1 (2), 94–100. doi:10.4103/bbrj.bbrj_34_17
Akpinar-Elci, M., Martin, F. E., Behr, J. G., and Diaz, R. (2015). Saharan dust, climate variability, and asthma in Grenada, the Caribbean. Int. J. biometeorology 59 (11), 1667–1671. doi:10.1007/s00484-015-0973-2
Alizadeh, M., Ghasemi Hashtroodi, L., Chavoshzadeh, Z., and Rezaei, N. (2016). Effect of air pollution in frequency of hospitalizations in asthmatic children. Acta medica Iran. 54 (8), 542–546.
R. Almeida, A. C. Teodoro, H. Gonçalves, A. Freitas, A. Sa-Sousa, and C Jácome. Editors (2017). Forecasting asthma hospital admissions from remotely sensed environmental data (GISTAM).
Anderson, G. B., and Bell, M. L. (2011). Heat waves in the United States: Mortality risk during heat waves and effect modification by heat wave characteristics in 43 U.S. Communities. Environ. health Perspect. 119 (2), 210–218. doi:10.1289/ehp.1002313
Brandt, E. B., Biagini Myers, J. M., Acciani, T. H., Ryan, P. H., Sivaprasad, U., Ruff, B., et al. (2015). Exposure to allergen and diesel exhaust particles potentiates secondary allergen-specific memory responses, promoting asthma susceptibility. J. allergy Clin. Immunol. 136 (2), 295–303.e7. doi:10.1016/j.jaci.2014.11.043
Bröms, K., Norbäck, D., Eriksson, M., Sundelin, C., and Svärdsudd, K. (2009). Effect of degree of urbanisation on age and sex-specific asthma prevalence in Swedish preschool children. BMC public health 9, 303. doi:10.1186/1471-2458-9-303
Buckley, J. P., and Richardson, D. B. (2012). Seasonal modification of the association between temperature and adult emergency department visits for asthma: A case-crossover study. Environ. health a Glob. access Sci. source 11, 55. doi:10.1186/1476-069x-11-55
Campbell-Lendrum, D., and Prüss-Ustün, A. (2019). Climate change, air pollution and noncommunicable diseases. Bull. World Health Organ 97 (2), 160–161. doi:10.2471/blt.18.224295
Campo, P., Eguiluz-Gracia, I., Plaza-Serón, M. C., Salas, M., Jose Rodriguez, M., Perez-Sanchez, N., et al. (2019). Bronchial asthma triggered by house dust mites in patients with local allergic rhinitis. Allergy 74 (8), 1502–1510. doi:10.1111/all.13775
Clifford, R. L., Jones, M. J., MacIsaac, J. L., McEwen, L. M., Goodman, S. J., Mostafavi, S., et al. (2017). Inhalation of diesel exhaust and allergen alters human bronchial epithelium DNA methylation. J. allergy Clin. Immunol. 139 (1), 112–121. doi:10.1016/j.jaci.2016.03.046
Cong, X., Xu, X., Zhang, Y., Wang, Q., Xu, L., and Huo, X. (2017). Temperature drop and the risk of asthma: A systematic review and meta-analysis. Environ. Sci. Pollut. Res. Int. 24 (28), 22535–22546. doi:10.1007/s11356-017-9914-4
Cox-Ganser, J. M. (2015). Indoor dampness and mould health effects - ongoing questions on microbial exposures and allergic versus nonallergic mechanisms. Clin. Exp. allergy J. Br. Soc. Allergy Clin. Immunol. 45 (10), 1478–1482. doi:10.1111/cea.12601
D'Amato, G., Holgate, S. T., Pawankar, R., Ledford, D. K., Cecchi, L., Al-Ahmad, M., et al. (2015). Meteorological conditions, climate change, new emerging factors, and asthma and related allergic disorders. A statement of the World Allergy Organization. World Allergy Organ J. 8 (1), 25. doi:10.1186/s40413-015-0073-0
Dastoorpoor, M., Khodadadi, N., Madadizadeh, F., Shahidizadeh, E., Shoushtari, M. H., Raji, H., et al. (2021). Risk factors for current wheeze among school children (6-7 and 13-14 years old) in Khuzestan, Iran. Public health Pract. 2, 100172. doi:10.1016/j.puhip.2021.100172
Faraji, M., Mohammadi, A., Najmi, M., Fallahnezhad, M., Sabetkish, N., Kazemnejad, A., et al. (2022). Exposure to road noise and asthma prevalence in adults. Environ. Sci. Pollut. Res. Int. 29 (16), 23512–23519. doi:10.1007/s11356-021-17531-1
Fazlollahi, M. R., Najmi, M., Fallahnezhad, M., Sabetkish, N., Kazemnejad, A., Bidad, K., et al. (2018). The prevalence of asthma in Iranian adults: The first national survey and the most recent updates. Clin. Respir. J. 12 (5), 1872–1881. doi:10.1111/crj.12750
Gautam, V. K., Pande, C. B., Kothari, M., Singh, P. K., and Agrawal, A. J. (2023). Exploration of groundwater potential zones mapping for hard rock region in the Jakham river basin using geospatial techniques and aquifer parameters. Adv. Space Res. 71 (6), 2892–2908. doi:10.1016/j.asr.2022.11.022
Ghatee, M. A., Nikaein, K., Taylor, W. R., Karamian, M., Alidadi, H., Kanannejad, Z., et al. (2020). Environmental, climatic and host population risk factors of human cystic echinococcosis in southwest of Iran. BMC public health 20 (1), 1611. doi:10.1186/s12889-020-09638-w
Ghatee, M. A., Taylor, W. R., and Karamian, M. (2020). The geographical distribution of cutaneous leishmaniasis causative agents in Iran and its neighboring countries, A review. Front. public health 8, 11. doi:10.3389/fpubh.2020.00011
Ghosh, A., Dutta, S., Podder, S., Mondal, P., Laha, A., Saha, N. C., et al. (2018). Sensitivity to house dust mites allergens with atopic asthma and its relationship with CD14 C(-159T) polymorphism in patients of West Bengal, India. J. Med. entomology 55 (1), 14–19. doi:10.1093/jme/tjx178
Gorai, A. K., Tuluri, F., and Tchounwou, P. B. (2014). A GIS based approach for assessing the association between air pollution and asthma in New York State, USA. Int. J. Environ. Res. public health 11 (5), 4845–4869. doi:10.3390/ijerph110504845
Guo, Y., Jiang, F., Peng, L., Zhang, J., Geng, F., Xu, J., et al. (2012). The association between cold spells and pediatric outpatient visits for asthma in Shanghai, China. PloS one 7 (7), e42232. doi:10.1371/journal.pone.0042232
Ho, W. C., Hartley, W. R., Myers, L., Lin, M. H., Lin, Y. S., Lien, C. H., et al. (2007). Air pollution, weather, and associated risk factors related to asthma prevalence and attack rate. Environ. Res. 104 (3), 402–409. doi:10.1016/j.envres.2007.01.007
Idani, E., Dastoorpoor, M., Goudarzi, G., Haddadzadeh Shoushtari, M., and Raji, H. (2021). Three consecutive episodes of thunderstorm asthma in ahvaz, Iran: The possible role of conocarpus pollen. Tanaffos 20 (3), 261–267.
Kaffash-Charandabi, N., Alesheikh, A. A., and Sharif, M. (2019). A ubiquitous asthma monitoring framework based on ambient air pollutants and individuals' contexts. Environ. Sci. Pollut. Res. Int. 26 (8), 7525–7539. doi:10.1007/s11356-019-04185-3
Kanannejad, Z., Shomali, M., Esmaeilzadeh, H., Nabavizadeh, H., Nikaein, K., Ghahramani, Z., et al. (2022). Geoclimatic risk factors for childhood asthma hospitalization in southwest of Iran. Pediatr. Pulmonol. 57 (9), 2023–2031. doi:10.1002/ppul.25971
Keddem, S., Barg, F. K., Glanz, K., Jackson, T., Green, S., and George, M. (2015). Mapping the urban asthma experience: Using qualitative GIS to understand contextual factors affecting asthma control. Soc. Sci. Med. 140, 9–17. doi:10.1016/j.socscimed.2015.06.039
Khan, I. A., Arsalan, M. H., Siddiqui, M. F., Zeeshan, S., and Shaukat, S. S. (2010). Spatial association of asthma and vegetation in karachi: A gis perspective. Pak J. Bot. 42 (5), 3547–3554.
Khasha, R., Sepehri, M. M., Mahdaviani, S. A., and Khatibi, T. (2018). Mobile GIS-based monitoring asthma attacks based on environmental factors. J. Clean. Prod. 179, 417–428. doi:10.1016/j.jclepro.2018.01.046
Li, M., Li, Q., Yang, G., Kolosov, V. P., Perelman, J. M., and Zhou, X. D. (2011). Cold temperature induces mucin hypersecretion from normal human bronchial epithelial cells in vitro through a transient receptor potential melastatin 8 (TRPM8)-mediated mechanism. J. allergy Clin. Immunol. 128 (3), 626–634.e5. doi:10.1016/j.jaci.2011.04.032
Lin, S., Luo, M., Walker, R. J., Liu, X., Hwang, S. A., and Chinery, R. (2009). Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiol. Camb. Mass) 20 (5), 738–746. doi:10.1097/ede.0b013e3181ad5522
Maya-Manzano, J. M., Fernández-Rodríguez, S., Monroy-Colín, A., Silva-Palacios, I., Tormo-Molina, R., and Gonzalo-Garijo, Á. (2017). Allergenic pollen of ornamental plane trees in a Mediterranean environment and urban planning as a prevention tool. Urban For. Urban Green. 27, 352–362. doi:10.1016/j.ufug.2017.09.009
Michelozzi, P., De Sario, M., Accetta, G., de'Donato, F., Kirchmayer, U., D'Ovidio, M., et al. (2006). Temperature and summer mortality: Geographical and temporal variations in four Italian cities. J. Epidemiol. community health 60 (5), 417–423. doi:10.1136/jech.2005.040857
Nel, A. (2005). Air pollution-related illness: Effects of particles. Sci. (New York, NY) 308 (5723), 804–806. doi:10.1126/science.1108752
Nel, A. E., Diaz-Sanchez, D., Ng, D., Hiura, T., and Saxon, A. (1998). Enhancement of allergic inflammation by the interaction between diesel exhaust particles and the immune system. J. allergy Clin. Immunol. 102 (4), 539–554. doi:10.1016/s0091-6749(98)70269-6
Newson, R. B., van Ree, R., Forsberg, B., Janson, C., Lötvall, J., Dahlén, S. E., et al. (2014). Geographical variation in the prevalence of sensitization to common aeroallergens in adults: The GA(2) len survey. Allergy 69 (5), 643–651. doi:10.1111/all.12397
Pande, C. B., Moharir, K. N., and Khadri, S. J. A. W. S. (2021). Assessment of land-use and land-cover changes in Pangari watershed area (MS), India, based on the remote sensing and GIS techniques. Appl. Water Sci. 11 (6), 96–12. doi:10.1007/s13201-021-01425-1
Pechlivanis, S., and von Mutius, E. (2020). Effect of farming on asthma. Acta medica Acad. 49 (2), 144–155. doi:10.5644/ama2006-124.293
Pesek, R. D., Vargas, P. A., Halterman, J. S., Jones, S. M., McCracken, A., and Perry, T. T. (2010). A comparison of asthma prevalence and morbidity between rural and urban schoolchildren in Arkansas. Ann. allergy, asthma & Immunol. official Publ. Am. Coll. Allergy, Asthma, & Immunol. 104 (2), 125–131. doi:10.1016/j.anai.2009.11.038
Rabiee, S., Mousavi, H., and Khafaie, M. A. (2018). Thunderstorm asthma outbreak, a rare phenomenon in southwestsouthwest Iran: Patients' perspectives. Environ. Sci. Pollut. Res. Int. 25 (36), 36158–36162. doi:10.1007/s11356-018-3478-9
Rashidi, M., Ramesht, M. H., Zohary, M., Poursafa, P., Kelishadi, R., Rashidi, Z., et al. (2013). Relation of air pollution with epidemiology of respiratory diseases in isfahan, Iran from 2005 to 2009. J. Res. Med. Sci. official J. Isfahan Univ. Med. Sci. 18 (12), 1074–1079.
Roy, S. R., McGinty, E. E., Hayes, S. C., and Zhang, L. (2010). Regional and racial disparities in asthma hospitalizations in Mississippi. J. allergy Clin. Immunol. 125 (3), 636–642. doi:10.1016/j.jaci.2009.11.046
Simpson, A., John, S. L., Jury, F., Niven, R., Woodcock, A., Ollier, W. E., et al. (2006). Endotoxin exposure, CD14, and allergic disease: An interaction between genes and the environment. Am. J. Respir. Crit. care Med. 174 (4), 386–392. doi:10.1164/rccm.200509-1380oc
Simunovic, M., Boyle, J., Baker, P., Erbas, B., and Davies, J. M. (2021). Spatiotemporal characteristics of asthma emergency department presentations in diverse geographical and climatic regions, Queensland, Australia. Qld. Aust. 33 (4), 623–630. doi:10.1111/1742-6723.13687
Solé, D., Cassol, V. E., Silva, A. R., Teche, S. P., Rizzato, T. M., Bandim, L. C., et al. (2007). Prevalence of symptoms of asthma, rhinitis, and atopic eczema among adolescents living in urban and rural areas in different regions of Brazil. Allergologia Immunopathol. 35 (6), 248–253. doi:10.1157/13112991
Son, J. Y., Bell, M. L., and Lee, J. T. (2014). The impact of heat, cold, and heat waves on hospital admissions in eight cities in Korea. Int. J. biometeorology 58 (9), 1893–1903. doi:10.1007/s00484-014-0791-y
Stern, J., Pier, J., and Litonjua, A. A. (2020). Asthma epidemiology and risk factors. Asthma Epidemiol. risk factors 42 (1), 5–15. doi:10.1007/s00281-020-00785-1
Strachan, D. P. (1989). Hay fever, hygiene, and household size. BMJ Clin. Res. ed) 299 (6710), 1259–1260. doi:10.1136/bmj.299.6710.1259
Williamson, I. J., Martin, C. J., McGill, G., Monie, R. D., and Fennerty, A. G. (1997). Damp housing and asthma: A case-control study. Thorax 52 (3), 229–234. doi:10.1136/thx.52.3.229
Xing, B., Lin, J. T., Tang, H. P., Yang, L., Yuan, Y. D., Gu, Y. H., et al. (2018). A retrospective study of the inducing factors and clinical characteristics of patients hospitalized for asthma exacerbation in China in 2013-2014. Zhonghua nei ke za zhi 57 (1), 21–26. doi:10.3760/cma.j.issn.0578-1426.2018.01.004
Keywords: asthma hospitalization, climatic changes, geographical factors, land cover, GIS
Citation: Kanannejad Z, Shokri Y, Alyasin S, Ghatee MA and Soleimanian S (2023) Geo-climatic variability and adult asthma hospitalization in Fars, Southwest Iran. Front. Environ. Sci. 11:1085103. doi: 10.3389/fenvs.2023.1085103
Received: 31 October 2022; Accepted: 28 March 2023;
Published: 10 April 2023.
Edited by:
Yanfang Sang, Institute of Geographic Sciences and Natural Resources (CAS), ChinaReviewed by:
Chaitanya B. Pande, Mahatma Phule Krishi Vidyapeeth, IndiaCopyright © 2023 Kanannejad, Shokri, Alyasin, Ghatee and Soleimanian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Soheila Alyasin, YWx5YXNpbnNAc3Vtcy5hYy5pcg==; Mohammad Amin Ghatee, Z2hhdGVlYTE5ODBAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.