- 1Research Center for Economy of Upper Reaches of the Yangtse River/School of Economics, Chongqing Technology and Business University, Chongqing, China
- 2School of Economics and Management, Huzhou University, Huzhou, China
Background: More than 80% of sewage generated by human activities is discharged into rivers and oceans without any treatment, which results in environmental pollution and more than 50 diseases. 80% of diseases and 50% of child deaths worldwide are related to poor water quality.
Methods: This paper selected 85 relevant papers finally based on the keywords of water pollution, water quality, health, cancer, and so on.
Results: The impact of water pollution on human health is significant, although there may be regional, age, gender, and other differences in degree. The most common disease caused by water pollution is diarrhea, which is mainly transmitted by enteroviruses in the aquatic environment.
Discussion: Governments should strengthen water intervention management and carry out intervention measures to improve water quality and reduce water pollution’s impact on human health.
Introduction
Water is an essential resource for human survival. According to the 2021 World Water Development Report released by UNESCO, the global use of freshwater has increased six-fold in the past 100 years and has been growing by about 1% per year since the 1980s. With the increase of water consumption, water quality is facing severe challenges. Industrialization, agricultural production, and urban life have resulted in the degradation and pollution of the environment, adversely affecting the water bodies (rivers and oceans) necessary for life, ultimately affecting human health and sustainable social development (Xu et al., 2022a). Globally, an estimated 80% of industrial and municipal wastewater is discharged into the environment without any prior treatment, with adverse effects on human health and ecosystems. This proportion is higher in the least developed countries, where sanitation and wastewater treatment facilities are severely lacking.
Sources of Water Pollution
Water pollution are mainly concentrated in industrialization, agricultural activities, natural factors, and insufficient water supply and sewage treatment facilities. First, industry is the main cause of water pollution, these industries include distillery industry, tannery industry, pulp and paper industry, textile industry, food industry, iron and steel industry, nuclear industry and so on. Various toxic chemicals, organic and inorganic substances, toxic solvents and volatile organic chemicals may be released in industrial production. If these wastes are released into aquatic ecosystems without adequate treatment, they will cause water pollution (Chowdhary et al., 2020). Arsenic, cadmium, and chromium are vital pollutants discharged in wastewater, and the industrial sector is a significant contributor to harmful pollutants (Chen et al., 2019). With the acceleration of urbanization, wastewater from industrial production has gradually increased. (Wu et al., 2020). In addition, water pollution caused by industrialization is also greatly affected by foreign direct investment. Industrial water pollution in less developed countries is positively correlated with foreign direct investment (Jorgenson, 2009). Second, water pollution is closely related to agriculture. Pesticides, nitrogen fertilizers and organic farm wastes from agriculture are significant causes of water pollution (RCEP, 1979). Agricultural activities will contaminate the water with nitrates, phosphorus, pesticides, soil sediments, salts and pathogens (Parris, 2011). Furthermore, agriculture has severely damaged all freshwater systems in their pristine state (Moss, 2008). Untreated or partially treated wastewater is widely used for irrigation in water-scarce regions of developing countries, including China and India, and the presence of pollutants in sewage poses risks to the environment and health. Taking China as an example, the imbalance in the quantity and quality of surface water resources has led to the long-term use of wastewater irrigation in some areas in developing countries to meet the water demand of agricultural production, resulting in serious agricultural land and food pollution, pesticide residues and heavy metal pollution threatening food safety and Human Health (Lu et al., 2015). Pesticides have an adverse impact on health through drinking water. Comparing pesticide use with health life Expectancy Longitudinal Survey data, it was found that a 10% increase in pesticide use resulted in a 1% increase in the medical disability index over 65 years of age (Lai, 2017). The case of the Musi River in India shows a higher incidence of morbidity in wastewater-irrigated villages than normal-water households. Third, water pollution is related to natural factors. Taking Child Loess Plateau as an example, the concentration of trace elements in water quality is higher than the average world level, and trace elements come from natural weathering and manufacture causes. Poor river water quality is associated with high sodium and salinity hazards (Xiao et al., 2019). The most typical water pollution in the middle part of the loess Plateau is hexavalent chromium pollution, which is caused by the natural environment and human activities. Loess and mudstone are the main sources, and groundwater with high concentrations of hexavalent chromium is also an important factor in surface water pollution (He et al., 2020). Finally, water supply and sewage treatment facilities are also important factors affecting drinking water quality, especially in developing countries. In parallel with China rapid economic growth, industrialization and urbanization, underinvestment in basic water supply and treatment facilities has led to water pollution, increased incidence of infectious and parasitic diseases, and increased exposure to industrial chemicals, heavy metals and algal toxins (Wu et al., 1999). An econometric model predicts the impact of water purification equipment on water quality and therefore human health. When the proportion of household water treated with water purification equipment is reduced from 100% to 90%, the expected health benefits are reduced by up to 96%.. When the risk of pretreatment water quality is high, the decline is even more significant (Brown and Clasen, 2012).
To sum up, water pollution results from both human and natural factors. Various human activities will directly affect water quality, including urbanization, population growth, industrial production, climate change, and other factors (Halder and Islam, 2015) and religious activities (Dwivedi et al., 2018). Improper disposal of solid waste, sand, and gravel is also one reason for decreasing water quality (Ustaoğlua et al., 2020).
Impact of Water Pollution on Human Health
Unsafe water has severe implications for human health. According to UNESCO 2021 World Water Development Report, about 829,000 people die each year from diarrhea caused by unsafe drinking water, sanitation, and hand hygiene, including nearly 300,000 children under the age of five, representing 5.3 percent of all deaths in this age group. Data from Palestine suggest that people who drink municipal water directly are more likely to suffer from diseases such as diarrhea than those who use desalinated and household-filtered drinking water (Yassin et al., 2006). In a comparative study of tap water, purified water, and bottled water, tap water was an essential source of gastrointestinal disease (Payment et al., 1997). Lack of water and sanitation services also increases the incidence of diseases such as cholera, trachoma, schistosomiasis, and helminthiasis. Data from studies in developing countries show a clear relationship between cholera and contaminated water, and household water treatment and storage can reduce cholera (Gundry et al., 2004). In addition to disease, unsafe drinking water, and poor environmental hygiene can lead to gastrointestinal illness, inhibiting nutrient absorption and malnutrition. These effects are especially pronounced for children.
Purpose of This Paper
More than two million people worldwide die each year from diarrhoeal diseases, with poor sanitation and unsafe drinking water being the leading cause of nearly 90% of deaths and affecting children the most (United Nations, 2016). More than 50 kinds of diseases are caused by poor drinking water quality, and 80% of diseases and 50% of child deaths are related to poor drinking water quality in the world. However, water pollution causes diarrhea, skin diseases, malnutrition, and even cancer and other diseases related to water pollution. Therefore, it is necessary to study the impact of water pollution on human health, especially disease heterogeneity, and clarify the importance of clean drinking water, which has important theoretical and practical significance for realizing sustainable development goals. Unfortunately, although many kinds of literature focus on water pollution and a particular disease, there is still a lack of research results that systematically analyze the impact of water pollution on human health and the heterogeneity of diseases. Based on the above background and discussion, this paper focuses on the effect of water pollution on human health and its disease heterogeneity.
Materials and Methods
Search Process
This article uses keywords such as “water,” “water pollution,” “water quality,” “health,” “diarrhea,” “skin disease,” “cancer” and “children” to search Web of Science and Google Scholar include SCI and SSCI indexed papers, research reports, and works from 1990 to 2021.
Inclusion-Exclusion Criteria and Data Extraction Process
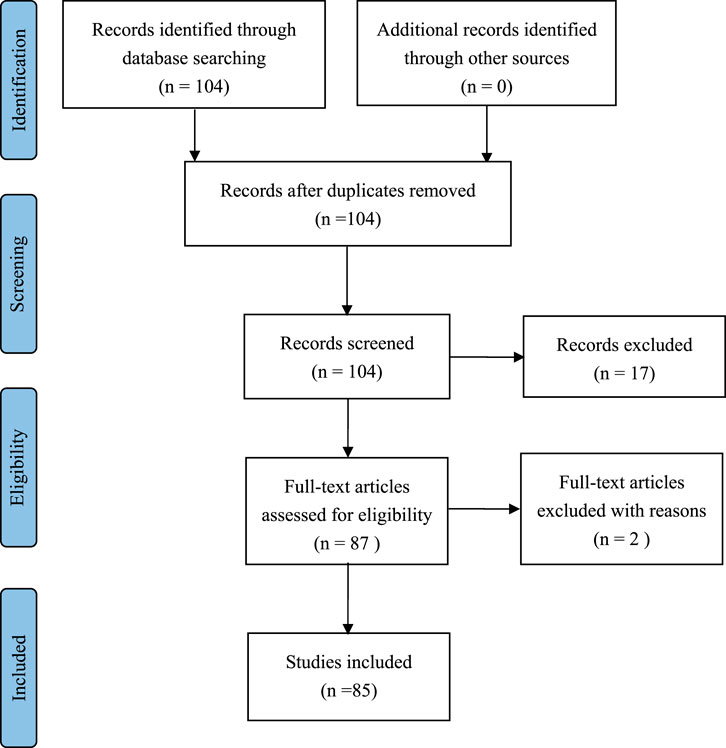
The existing literature shows that water pollution and human health are important research topics in health economics, and scholars have conducted in-depth research. As of 30 December 2021, 104 related literatures were searched, including research papers, reviews and conference papers. Then, according to the content relevancy, 19 papers were eliminated, and 85 papers remained. The purpose of this review is to summarize the impact of water pollution on human health and its disease heterogeneity and to explore how to improve human health by improving water pollution control measures.
Information extracted from all included papers included: author, publication date, sample country, study methodology, study purpose, and key findings. All analysis results will be analyzed according to the process in Figure 1.
The relevant information of the paper is exported to the Excel database through Endnote, and the duplicates are deleted. The results were initially extracted by one researcher and then cross-checked by another researcher to ensure that all data had been filtered and reviewed. If two researchers have different opinions, the two researchers will review together until a final agreement is reached.
Quality Assessment of the Literature
The JBI Critical Appraisal Checklist was used to evaluate the quality of each paper. The JBI (Joanna Briggs Institute) key assessment tool was developed by the JBI Scientific Committee after extensive peer review and is designed for system review. All features of the study that meet the following eight criteria are included in the final summary:1) clear purpose; 2) Complete information of sample variables; 3) Data basis; 4) the validity of data sorting; 5) ethical norms; (6); 7) Effective results; 8) Apply appropriate quantitative methods and state the results clearly. Method quality is evaluated by the Yes/No questions listed in the JBI Key Assessment List. Each analysis paper received 6 out of 8.
Results
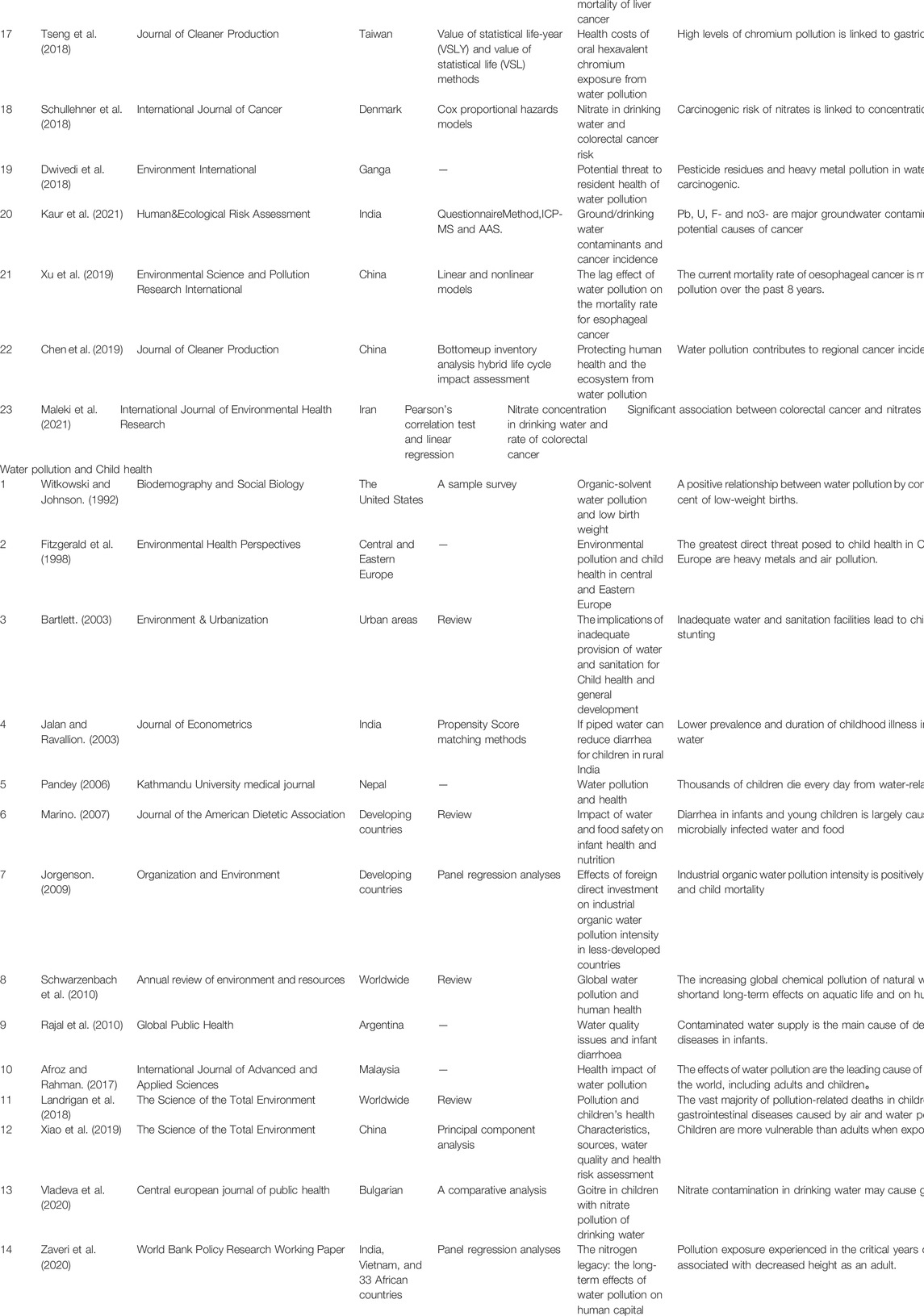
The quality of drinking water is an essential factor affecting human health. Poor drinking water quality has led to the occurrence of water-borne diseases. According to the World Health Organization (WHO) survey, 80% of the world’s diseases and 50% of the world’s child deaths are related to poor drinking water quality, and there are more than 50 diseases caused by poor drinking water quality. The quality of drinking water in developing countries is worrying. The negative health effects of water pollution remain the leading cause of morbidity and mortality in developing countries. Different from the existing literature review, this paper mainly studies the impact of water pollution on human health according to the heterogeneity of diseases. We focuses on diarrhea, skin diseases, cancer, child health, etc., and sorts out the main effects of water pollution on human health (Table 1).
Water Pollution and Diarrhea
Diarrhea is a common symptom of gastrointestinal diseases and the most common disease caused by water pollution. Diarrhea is a leading cause of illness and death in young children in low-income countries. Diarrhoeal diseases account for 21% of annual deaths among children under 5 years of age in developing countries (Waddington et al., 2009). Many infectious agents associated with diarrhea are directly related to contaminated water (Ahmed and Ismail, 2018). Parasitic worms present in non-purifying drinking water when is consumed by human beings causes diseases (Ansari and Akhmatov., 2020) . It was found that treated water from water treatment facilities was associated with a lower risk of diarrhea than untreated water for all ages (Clasen et al., 2015). For example, in the southern region of Brazil, a study found that factors significantly associated with an increased risk of mortality from diarrhoea included lack of plumbed water, lack of flush toilets, poor housing conditions, and overcrowded households. Households without access to piped water had a 4.8 times higher risk of infant death from diarrhea than households with access to piped water (Victora et al., 1988)
Enteroviruses exist in the aquatic environment. More than 100 pathogenic viruses are excreted in human and animal excreta and spread in the environment through groundwater, estuarine water, seawater, rivers, sewage treatment plants, insufficiently treated water, drinking water, and private wells (Fong and Lipp., 2005). A study in Pakistan showed that coliform contamination was found in some water sources. Improper disposal of sewage and solid waste, excessive use of pesticides and fertilizers, and deteriorating pipeline networks are the main causes of drinking water pollution. The main source of water-borne diseases such as gastroenteritis, dysentery, diarrhea, and viral hepatitis in this area is the water pollution of coliform bacteria (Khan et al., 2013). Therefore, the most important role of water and sanitation health interventions is to hinder the transmission of diarrheal pathogens from the environment to humans (Waddington et al., 2009).
Meta-analyses are the most commonly used method for water quality and diarrhea studies. It was found that improving water supply and sanitation reduced the overall incidence of diarrhea by 26%. Among Malaysian infants, having clean water and sanitation was associated with an 82% reduction in infant mortality, especially among infants who were not breastfed (Esrey et al., 1991). All water quality and sanitation interventions significantly reduced the risk of diarrhoeal disease, and water quality interventions were found to be more effective than previously thought. Multiple interventions (including water, sanitation, and sanitation measures) were not more effective than single-focus interventions (Fewtrell and Colford., 2005). Water quality interventions reduced the risk of diarrhoea in children and reduced the risk of E. coli contamination of stored water (Arnold and Colford., 2007). Interventions to improve water quality are generally effective in preventing diarrhoea in children of all ages and under 5. However, some trials showed significant heterogeneity, which may be due to the research methods and their conditions (Clasen et al., 2007).
Water Pollution and Skin Diseases
Contrary to common sense that swimming is good for health, studies as early as the 1950s found that the overall disease incidence in the swimming group was significantly higher than that in the non-swimming group. The survey shows that the incidence of the disease in people under the age of 10 is about 100% higher than that of people over 10 years old. Skin diseases account for a certain proportion (Stevenson, 1953). A prospective epidemiological study of beach water pollution was conducted in Hong Kong in the summer of 1986–1987. The study found that swimmers on Hong Kong’s coastal beaches were more likely than non-swimmers to complain of systemic ailments such as skin and eyes. And swimming in more polluted beach waters has a much higher risk of contracting skin diseases and other diseases. Swimming-related disease symptom rates correlated with beach cleanliness (Cheung et al., 1990).
A study of arsenic-affected villages in the southern Sindh province of Pakistan emphasized that skin diseases were caused by excessive water quality. By studying the relationship between excessive arsenic in drinking water caused by water pollution and skin diseases (mainly melanosis and keratosis), it was found that compared with people who consumed urban low-arsenic drinking water, the hair of people who consumed high-arsenic drinking water arsenic concentration increased significantly. The level of arsenic in drinking water directly affects the health of local residents, and skin disease is the most common clinical complication of arsenic poisoning. There is a correlation between arsenic concentrations in biological samples (hair and blood) from patients with skin diseases and intake of arsenic-contaminated drinking water (Kazi et al., 2009). Another Bangladesh study showed that many people suffer from scabies due to river pollution (Hanif et al., 2020). Not only that, but water pollution from industry can also cause skin cancer (Arif et al., 2020).
Studies using meta-analysis have shown that exposure to polluted Marine recreational waters can have adverse consequences, including frequent skin discomfort (such as rash or itching). Skin diseases in swimmers may be caused by a variety of pathogenic microorganisms (Yau et al., 2009). People (swimmers and non-swimmers) exposed to waters above threshold levels of bacteria had a higher relative risk of developing skin disease, and levels of bacteria in seawater were highly correlated with skin symptoms.
Studies have also suggested that swimmers are 3.5 times more likely to report skin diseases than non-swimmers. This difference may be a “risk perception bias” at work on swimmers, who are generally aware that such exposure may lead to health effects and are more likely to detect and report skin disorders. It is also possible that swimmers exaggerated their symptoms, reporting conditions that others would not classify as true skin disorders (Fleisher and Kay. 2006).
Water Pollution and Cancer
According to WHO statistics, the number of cancer patients diagnosed in 2020 reached 19.3 million, while the number of deaths from cancer increased to 10 million. Currently, one-fifth of all global fevers will develop cancer during their lifetime. The types and amounts of carcinogens present in drinking water will vary depending on where they enter: contamination of the water source, water treatment processes, or when the water is delivered to users (Morris, 1995).
From the perspective of water sources, arsenic, nitrate, chromium, etc. are highly associated with cancer. Ingestion of arsenic from drinking water can cause skin cancer and kidney and bladder cancer (Marmot et al., 2007). The risk of cancer in the population from arsenic in the United States water supply may be comparable to the risk from tobacco smoke and radon in the home environment. However, individual susceptibility to the carcinogenic effects of arsenic varies (Smith et al., 1992). A high association of arsenic in drinking water with lung cancer was demonstrated in a northern Chilean controlled study involving patients diagnosed with lung cancer and a frequency-matched hospital between 1994 and 1996. Studies have also shown a synergistic effect of smoking and arsenic intake in drinking water in causing lung cancer (Ferreccio et al., 2000). Exposure to high arsenic levels in drinking water was also associated with the development of liver cancer, but this effect was not significant at exposure levels below 0.64 mg/L (Lin et al., 2013).
Nitrates are a broader contaminant that is more closely associated with human cancers, especially colorectal cancer. A study in East Azerbaijan confirmed a significant association between colorectal cancer and nitrate in men, but not in women (Maleki et al., 2021). The carcinogenic risk of nitrates is concentration-dependent. The risk increases significantly when drinking water levels exceed 3.87 mg/L, well below the current drinking water standard of 50 mg/L. Drinking water with nitrate concentrations lower than current drinking water standards also increases the risk of colorectal cancer (Schullehner et al., 2018).
Drinking water with high chromium content will bring high carcinogenicity caused by hexavalent chromium to residents. Drinking water intake of hexavalent chromium experiments showed that hexavalent chromium has the potential to cause human respiratory cancer. (Zhitkovich, 2011). A case from Changhua County, Taiwan also showed that high levels of chromium pollution were associated with gastric cancer incidence (Tseng et al., 2018).
There is a correlation between trihalomethane (THM) levels in drinking water and cancer mortality. Bladder and brain cancers in both men and women and non-Hodgkin’s lymphoma and kidney cancer in men were positively correlated with THM levels, and bladder cancer mortality had the strongest and most consistent association with THM exposure index (Cantor et al., 1978).
From the perspective of water treatment process, carcinogens may be introduced during chlorine treatment, and drinking water is associated with all cancers, urinary cancers and gastrointestinal cancers (Page et al., 1976). Chlorinated byproducts from the use of chlorine in water treatment are associated with an increased risk of bladder and rectal cancer, with perhaps 5,000 cases of bladder and 8,000 cases of rectal cancer occurring each year in the United States (Morris, 1995).
The impact of drinking water pollutants on cancer is complex. Epidemiological studies have shown that drinking water contaminants, such as chlorinated by-products, nitrates, arsenic, and radionuclides, are associated with cancer in humans (Cantor, 1997). Pb, U, F- and no3- are the main groundwater pollutants and one of the potential causes of cancer (Kaur et al., 2021). In addition, many other water pollutants are also considered carcinogenic, including herbicides and pesticides, and fertilizers that contain and release nitrates (Marmot et al., 2007). A case from Hebei, China showed that the contamination of nitrogen compounds in well water was closely related to the use of nitrogen fertilizers in agriculture, and the levels of three nitrogen compounds in well water were significantly positively correlated with esophageal cancer mortality (Zhang et al., 2003).
In addition, due to the time-lag effect, the impact of watershed water pollution on cancer is spatially heterogeneous. The mortality rate of esophageal cancer caused by water pollution is significantly higher downstream than in other regions due to the impact of historical water pollution (Xu et al., 2019). A study based on changes in water quality in the watershed showed that a grade 6 deterioration in water quality resulted in a 9.3% increase in deaths from digestive cancer. (Ebenstein, 2012).
Water Pollution and Child Health
Diarrhea is a common disease in children. Diarrhoeal diseases (including cholera) kill 1.8 million people each year, 90 per cent of them children under the age of five, mostly in developing countries. 88% of diarrhoeal diseases are caused by inadequate water supply, sanitation and hygiene (Team, 2004). A large proportion of these are caused by exposure to microbially infected water and food, and diarrhea in infants and young children can lead to malnutrition and reduced immune resistance, thereby increasing the likelihood of prolonged and recurrent diarrhea (Marino, 2007). Pollution exposure experienced by children during critical periods of development is associated with height loss in adulthood (Zaveri et al., 2020). Diseases directly related to water and sanitation, combined with malnutrition, also lead to other causes of death, such as measles and pneumonia. Child malnutrition and stunting due to inadequate water and sanitation will continue to affect more than one-third of children in the world (Bartlett, 2003). A study from rural India showed that children living in households with tap water had significantly lower disease prevalence and duration (Jalan and Ravallion, 2003).
In conclusion, water pollution is a significant cause of childhood diseases. Air, water, and soil pollution together killed 940,000 children worldwide in 2016, two-thirds of whom were under the age of 5, and the vast majority occurred in low- and middle-income countries (Landrigan et al., 2018). The intensity of industrial organic water pollution is positively correlated with infant mortality and child mortality in less developed countries, and industrial water pollution is an important cause of infant and child mortality in less developed countries (Jorgenson, 2009). In addition, arsenic in drinking water is a potential carcinogenic risk in children (García-Rico et al., 2018). Nitrate contamination in drinking water may cause goiter in children (Vladeva et al.., 2000).
Discussions
This paper reviews the environmental science, health, and medical literature, with a particular focus on epidemiological studies linking water quality, water pollution, and human disease, as well as studies on water-related disease morbidity and mortality. At the same time, special attention is paid to publications from the United Nations and the World Health Organization on water and sanitation health research. The purpose of this paper is to clarify the relationship between water pollution and human health, including: The relationship between water pollution and diarrhea, the mechanism of action, and the research situation of meta-analysis; The relationship between water pollution and skin diseases, pathogenic factors, and meta-analysis research; The relationship between water pollution and cancer, carcinogenic factors, and types of cancer; The relationship between water pollution and Child health, and the major childhood diseases caused.
A study of more than 100 literatures found that although factors such as country, region, age, and gender may have different influences, in general, water pollution has a huge impact on human health. Water pollution is the cause of many human diseases, mainly diarrhoea, skin diseases, cancer and various childhood diseases. The impact of water pollution on different diseases is mainly reflected in the following aspects. Firstly, diarrhea is the most easily caused disease by water pollution, mainly transmitted by enterovirus existing in the aquatic environment. The transmission environment of enterovirus depends on includes groundwater, river, seawater, sewage, drinking water, etc. Therefore, it is necessary to prevent the transmission of enterovirus from the environment to people through drinking water intervention. Secondly, exposure to or use of heavily polluted water is associated with a risk of skin diseases. Excessive bacteria in seawater and heavy metals in drinking water are the main pathogenic factors of skin diseases. Thirdly, water pollution can pose health risks to humans through any of the three links: the source of water, the treatment of water, and the delivery of water. Arsenic, nitrate, chromium, and trihalomethane are major carcinogens in water sources. Carcinogens may be introduced during chlorine treatment from water treatment. The effects of drinking water pollution on cancer are complex, including chlorinated by-products, heavy metals, radionuclides, herbicides and pesticides left in water, etc., Finally, water pollution is an important cause of children’s diseases. Contact with microbiologically infected water can cause diarrhoeal disease in children. Malnutrition and weakened immunity from diarrhoeal diseases can lead to other diseases.
This study systematically analyzed the impact of water pollution on human health and the heterogeneity of diseases from the perspective of different diseases, focusing on a detailed review of the relationship, mechanism and influencing factors of water pollution and diseases. From the point of view of limitations, this paper mainly focuses on the research of environmental science and environmental management, and the research on pathology is less involved. Based on this, future research can strengthen research at medical and pathological levels.
In response to the above research conclusions, countries, especially developing countries, need to adopt corresponding water management policies to reduce the harm caused by water pollution to human health. Firstly, there is a focus on water quality at the point of use, with interventions to improve water quality, including chlorination and safe storage (Gundry et al., 2004), and provision of treated and clean water (Khan et al., 2013). Secondly, in order to reduce the impact of water pollution on skin diseases, countries should conduct epidemiological studies on their own in order to formulate health-friendly bathing water quality standards suitable for their specific conditions (Cheung et al., 1990). Thirdly, in order to reduce the cancer caused by water pollution, the whole-process supervision of water quality should be strengthened, that is, the purity of water sources, the scientific nature of water treatment and the effectiveness of drinking water monitoring. Fourthly, each society should prevent and control source pollution from production, consumption, and transportation (Landrigan et al., 2018). Fifthly, health education is widely carried out. Introduce environmental education, educate residents on sanitary water through newspapers, magazines, television, Internet and other media, and enhance public health awareness. Train farmers to avoid overuse of agricultural chemicals that contaminate drinking water.
Author Contributions
Conceptualization, XX|; methodology, LL; data curation, HY; writing and editing, LL; project administration, XX|.
Funding
This article is a phased achievement of The National Social Science Fund of China: Research on the blocking mechanism of the critical poor households returning to poverty due to illness, No: 20BJY057.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Afroz, R., Rahman, A., and Rahman, A. (2017). Health Impact of River Water Pollution in Malaysia. Int. J. Adv. Appl. Sci. 4 (5), 78–85. doi:10.21833/ijaas.2017.05.014
Ahmed, S., and Ismail, S. (2018). Water Pollution and its Sources, Effects and Management: a Case Study of Delhi. Int. J. Curr. Adv. Res. 7 (2), 10436–10442. doi:10.24327/ijcar.2018.10442.1768
Ansari, Z. Z., and Akhmatov, S. V. (2020). Impacts of Water Pollution on Human Health: A Case Study of Delhi.
Arif, A., Malik, M. F., Liaqat, S., Aslam, A., Mumtaz, K., and Afzal, A. (2020). 3. Water Pollution and Industries. Pure Appl. Biol. (PAB) 9 (4), 2214–2224. doi:10.19045/bspab.2020.90237
Arnold, B. F., and Colford, J. M. (2007). Treating Water with Chlorine at Point-Of-Use to Improve Water Quality and Reduce Child Diarrhea in Developing Countries: a Systematic Review and Meta-Analysis. Am. J. Trop. Med. Hyg. 76 (2), 354–364. doi:10.4269/ajtmh.2007.76.354
Bartlett, S. (2003). Water, Sanitation and Urban Children: the Need to Go beyond “Improved” Provision. Environ. Urbanization 15 (2), 57–70. doi:10.1177/095624780301500220
Bessong, P. O., Odiyo, J. O., Musekene, J. N., and Tessema, A. (2009). Spatial Distribution of Diarrhoea and Microbial Quality of Domestic Water during an Outbreak of Diarrhoea in the Tshikuwi Community in Venda, South Africa. J. Health Popul. Nutr. 27 (5), 652–659. doi:10.3329/jhpn.v27i5.3642
Boldo, E., MartÍN-Olmedo, P., Medina, S., Pirard, P., Mouly, D., and Beaudeau, P. (2006). Towards the Quantification of Health Impacts Caused by Drinking-Water Pollution in European Countries. Epidemiology 17 (6), S447. doi:10.1097/00001648-200611001-01198
Brown, J., and Clasen, T. (2012). High Adherence Is Necessary to Realize Health Gains from Water Quality Interventions. PLoS ONE 7 (5), e36735–9. doi:10.1371/journal.pone.0036735
Cantor, K. P., Hoover, R., Mason, T. J., and McCabe, L. J. (1978). Associations of Cancer Mortality with Halomethanes in Drinking Water. J. Natl. Cancer Inst. 61 (4), 979
Cantor, K. P. (1997). Drinking Water and Cancer. Cancer Causes Control CCC 8 (3), 292–308. doi:10.1023/a:1018444902486
Chen, B., Wang, M., Duan, M., Ma, X., Hong, J., Xie, F., et al. (2019). In Search of Key: Protecting Human Health and the Ecosystem from Water Pollution in China. J. Clean. Prod. 228, 101–111. doi:10.1016/j.jclepro.2019.04.228
Cheung, W. H. S., Chang, K. C. K., Hung, R. P. S., and Kleevens, J. W. L. (1990). Health Effects of Beach Water Pollution in Hong Kong. Epidemiol. Infect. 105 (1), 139–162. doi:10.1017/s0950268800047737
Cheung, W. H. S., Hung, R. P. S., Chang, K. C. K., and Kleevens, J. W. L. (1991). Epidemiological Study of Beach Water Pollution and Health-Related Bathing Water Standards in Hong Kong. Water Sci. Technol. 23 (1-3), 243–252. doi:10.2166/wst.1991.0422
Chowdhary, P., Bharagava, R. N., Mishra, S., and Khan, N. (2020). Role of Industries in Water Scarcity and its Adverse Effects on Environment and Human Health. Environ. Concerns Sustain. Dev., 235–256. doi:10.1007/978-981-13-5889-0_12
Clasen, T. F., Alexander, K. T., Sinclair, D., Boisson, S., Peletz, R., Chang, H. H., et al. (2015). Interventions to Improve Water Quality for Preventing Diarrhoea. Cochrane Database Syst. Rev. 10, CD004794. doi:10.1002/14651858.CD004794.pub3
Clasen, T., Schmidt, W.-P., Rabie, T., Roberts, I., and Cairncross, S. (2007). Interventions to Improve Water Quality for Preventing Diarrhoea: Systematic Review and Meta-Analysis. Bmj 334 (7597), 782. doi:10.1136/bmj.39118.489931.be
Conroy, R. M., Elmore-Meegan, M., Joyce, T., McGuigan, K. G., and Barnes, J. (1996). Solar Disinfection of Drinking Water and Diarrhoea in Maasai Children: a Controlled Field Trial. Lancet 348 (9043), 1695–1697. doi:10.1016/s0140-6736(96)02309-4
Dasgupta, P. (2004). Valuing Health Damages from Water Pollution in Urban Delhi, India: a Health Production Function Approach. Envir. Dev. Econ. 9 (1), 83–106. doi:10.1017/s1355770x03001098
Dwivedi, S., Mishra, S., and Tripathi, R. D. (2018). Ganga Water Pollution: A Potential Health Threat to Inhabitants of Ganga Basin. Environ. Int. 117, 327–338. doi:10.1016/j.envint.2018.05.015
Ebenstein, A. (2012). The Consequences of Industrialization: Evidence from Water Pollution and Digestive Cancers in China. Rev. Econ. Statistics 94 (1), 186–201. doi:10.1162/rest_a_00150
El-Kowrany, S. I., El- Zamarany, E. A., El-Nouby, K. A., El-Mehy, D. A., Abo Ali, E. A., and Othman, A. A. (2016). Water Pollution in the Middle Nile Delta, Egypt: an Environmental Study. J. Adv. Res. 7 (5), 781–794. doi:10.1016/j.jare.2015.11.005
Enrique Biagini, R. (1975). Chronic Arsenic Water Pollution in the Republic of Argentina. Med. Cutan. Ibero Lat. Am. 3 (6), 423
Esrey, S. A., Potash, J. B., Roberts, L., and Shiff, C. (1991). Effects of Improved Water Supply and Sanitation on Ascariasis, Diarrhoea, Dracunculiasis, Hookworm Infection, Schistosomiasis, and Trachoma. Bull. World Health Organ 69 (5), 609
Ferreccio, C., González, C., Milosavjlevic, V., Marshall, G., Sancha, A. M., and Smith, A. H. (2000). Lung Cancer and Arsenic Concentrations in Drinking Water in Chile. Epidemiology 11 (6), 673–679. doi:10.1097/00001648-200011000-00010
Fewtrell, L., and Colford, J. M. (2005). Water, Sanitation and Hygiene in Developing Countries: Interventions and Diarrhoea-A Review. Water Sci. Technol. A J. Int. Assoc. Water Pollut. Res. 52 (8), 133–142. doi:10.2166/wst.2005.0244
Fitzgerald, E. F., Schell, L. M., Marshall, E. G., Carpenter, D. O., Suk, W. A., and Zejda, J. E. (1998). Environmental Pollution and Child Health in Central and Eastern Europe. Environ. Health Perspect. 106 (6), 307–311. doi:10.1289/ehp.98106307
Fleisher, J. M., and Kay, D. (2006). Risk Perception Bias, Self-Reporting of Illness, and the Validity of Reported Results in an Epidemiologic Study of Recreational Water Associated Illnesses. Mar. Pollut. Bull. 52 (3), 264–268. doi:10.1016/j.marpolbul.2005.08.019
Fong, T.-T., and Lipp, E. K. (2005). Enteric Viruses of Humans and Animals in Aquatic Environments: Health Risks, Detection, and Potential Water Quality Assessment Tools. Microbiol. Mol. Biol. Rev. 69 (2), 357–371. doi:10.1128/mmbr.69.2.357-371.2005
Froom, P. (2009). Water Pollution and Cancer in Israeli Navy Divers. Int. J. Occup. Environ. Health 15 (3), 326–328. doi:10.1179/oeh.2009.15.3.326
Gundry, S., Wright, J., and Conroy, R. (2004). A Systematic Review of the Health Outcomes Related to Household Water Quality in Developing Countries. J. water health 2 (1), 1–13. doi:10.2166/wh.2004.0001
Halder, J., Islam, N., and Islam, N. (2015). Water Pollution and its Impact on the Human Health. Eh 2 (1), 36–46. doi:10.15764/eh.2015.01005
Hanif, M., Miah, R., Islam, M., and Marzia, S. (2020). Impact of Kapotaksha River Water Pollution on Human Health and Environment. Prog. Agric. 31 (1), 1–9. doi:10.3329/pa.v31i1.48300
Haseena, M., Malik, M. F., Javed, A., Arshad, S., Asif, N., Zulfiqar, S., et al. (2017). Water Pollution and Human Health. Environ. Risk Assess. Remediat. 1 (3), 20. doi:10.4066/2529-8046.100020
Henry, F. J., Huttly, S. R. A., Patwary, Y., and Aziz, K. M. A. (1990). Environmental Sanitation, Food and Water Contamination and Diarrhoea in Rural Bangladesh. Epidemiol. Infect. 104 (2), 253–259. doi:10.1017/s0950268800059422
Jalan, J., and Ravallion, M. (2003). Does Piped Water Reduce Diarrhea for Children in Rural India? J. Econ. 112 (1), 153–173. doi:10.1016/s0304-4076(02)00158-6
Jensen, P. K., Jayasinghe, G., Hoek, W., Cairncross, S., and Dalsgaard, A. (2004). Is There an Association between Bacteriological Drinking Water Quality and Childhood Diarrhoea in Developing Countries? Trop. Med. Int. Health 9 (11), 1210–1215. doi:10.1111/j.1365-3156.2004.01329.x
Jorgenson, A. K. (2009). Foreign Direct Investment and the Environment, the Mitigating Influence of Institutional and Civil Society Factors, and Relationships between Industrial Pollution and Human Health. Organ. Environ. 22 (2), 135–157. doi:10.1177/1086026609338163
Kaur, G., Kumar, R., Mittal, S., Sahoo, P. K., and Vaid, U. (2021). Ground/drinking Water Contaminants and Cancer Incidence: A Case Study of Rural Areas of South West Punjab, India. Hum. Ecol. Risk Assess. Int. J. 27 (1), 205–226. doi:10.1080/10807039.2019.1705145
Kazi, T. G., Arain, M. B., Baig, J. A., Jamali, M. K., Afridi, H. I., Jalbani, N., et al. (2009). The Correlation of Arsenic Levels in Drinking Water with the Biological Samples of Skin Disorders. Sci. Total Environ. 407 (3), 1019–1026. doi:10.1016/j.scitotenv.2008.10.013
Khan, S., Shahnaz, M., Jehan, N., Rehman, S., Shah, M. T., and Din, I. (2013). Drinking Water Quality and Human Health Risk in Charsadda District, Pakistan. J. Clean. Prod. 60, 93–101. doi:10.1016/j.jclepro.2012.02.016
Kochhar, N., Gill, G. S., Tuli, N., Dadwal, V., and Balaram, V. (2007). Chemical Quality of Ground Water in Relation to Incidence of Cancer in Parts of SW Punjab, India. Asian J. Water, Environ. Pollut. 4 (2), 107 doi:10.1086/114154
Kumar, S., Meena, H. M., and Verma, K. (2017). Water Pollution in India: its Impact on the Human Health: Causes and Remedies. Int. J. Appl. Environ. Sci. 12 (2), 275
Lai, W. (2017). Pesticide Use and Health Outcomes: Evidence from Agricultural Water Pollution in China. J. Environ. Econ. Manag. 86, 93–120. doi:10.1016/j.jeem.2017.05.006
Landrigan, P. J., Fuller, R., Fisher, S., Suk, W. A., Sly, P., Chiles, T. C., et al. (2018). Pollution and Children's Health. Sci. Total Environ. 650 (Pt 2), 2389–2394. doi:10.1016/j.scitotenv.2018.09.375
Lin, H.-J., Sung, T.-I., Chen, C.-Y., and Guo, H.-R. (2013). Arsenic Levels in Drinking Water and Mortality of Liver Cancer in Taiwan. J. Hazard. Mater. 262, 1132–1138. doi:10.1016/j.jhazmat.2012.12.049
Lu, Y., Song, S., Wang, R., Liu, Z., Meng, J., Sweetman, A. J., et al. (2015). Impacts of Soil and Water Pollution on Food Safety and Health Risks in China. Environ. Int. 77, 5–15. doi:10.1016/j.envint.2014.12.010
Marino, D. D. (2007). Water and Food Safety in the Developing World: Global Implications for Health and Nutrition of Infants and Young Children. J. Am. Dietetic Assoc. 107 (11), 1930–1934. doi:10.1016/j.jada.2007.08.013
Marmot, M., Atinmo, T., Byers, T., Chen, J., and Zeisel, S. H. (2007). Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. Nutr. Bull.
Marr, A., and Dasgupta, N. (2009). Industrial Water Pollution in Dhaka, Bangladesh: Strategies and Incentives for Pollution Control in Small and Medium Enterprises. Int. J. Interdiscip. Soc. Sci. Annu. Rev. 3 (11), 97–108. doi:10.18848/1833-1882/cgp/v03i11/52752
Morris, R. D. (1995). Drinking Water and Cancer. Environ. Health Perspect. 103, 225. doi:10.2307/3432315
Moss, B. (2008). Water Pollution by Agriculture. Phil. Trans. R. Soc. B 363 (1491), 659–666. doi:10.1098/rstb.2007.2176
Page, T., Harris, R. H., and Epstein, S. S. (1976). Drinking Water and Cancer Mortality in Louisiana. Science 193 (4247), 55–57. doi:10.1126/science.935854
Pandey, S. (2006). Water Pollution and Health. Kathmandu Univ. Med. J. (KUMJ) 4 (1), 128. doi:10.1016/j.crvi.2013.04.013
Parris, K. (2011). Impact of Agriculture on Water Pollution in OECD Countries: Recent Trends and Future Prospects. Int. J. Water Resour. Dev. 27 (1), 33–52. doi:10.1080/07900627.2010.531898
Payment, P., Siemiatycki, J., Richardson, L., Renaud, G., Franco, E., and Prevost, M. (1997). A Prospective Epidemiological Study of Gastrointestinal Health Effects Due to the Consumption of Drinking Water. Int. J. Environ. Health Res. 7 (1), 5–31. doi:10.1080/09603129773977
Rabbani, M., Chowdhury, M., and Khan, N. A. (2010). Impacts of Industrial Pollution on Human Health: Empirical Evidences from an Industrial Hotspot (Kaliakoir) in Bangladesh. Asian J. Water, Environ. Pollut. 7 (1), 27
Rajal, V. B., Cruz, C., and Last, J. A. (2010). Water Quality Issues and Infant Diarrhoea in a South American Province. Glob. Public Health 5 (4), 348–363. doi:10.1080/17441690802447267
Rampen, F. H. J., Nelemans, P. J., and Verbeek, A. L. (1992). Is Water Pollution a Cause of Cutaneous Melanoma? Epidemiology 3, 263–265. doi:10.1097/00001648-199205000-00013
Royal Commission for Environmental Pollution 1979 Seventh Report. Agriculture and Pollution. London, UK: H.M.S.O.
Rusiñol, M., Fernandez-Cassi, X., Timoneda, N., Carratalà, A., and Abril, J. F. (2015). Evidence of Viral Dissemination and Seasonality in a Mediterranean River Catchment: Implications for Water Pollution Management. J. Environ. Manag. 159, 58–67. doi:10.1016/j.jenvman.2015.05.019
Schullehner, J., Hansen, B., Thygesen, M., Pedersen, C. B., and Sigsgaard, T. (2018). Nitrate in Drinking Water and Colorectal Cancer Risk: A Nationwide Population-Based Cohort Study. Int. J. Cancer 143 (1), 73–79. doi:10.1002/ijc.31306
Schwarzenbach, R. P., Egli, T., Hofstetter, T. B., Von Gunten, U., and Wehrli, B. (2010). Global Water Pollution and Human Health. Annu. Rev. Environ. Resour. 35, 109–136. doi:10.1146/annurev-environ-100809-125342
Sliman, N. A. (1978). Outbreak of Guillain-Barre Syndrome Associated with Water Pollution. Bmj 1 (6115), 751–752. doi:10.1136/bmj.1.6115.751
Smith, A. H., Hopenhayn-Rich, C., Bates, M. N., Goeden, H. M., Hertz-Picciotto, I., Duggan, H. M., et al. (1992). Cancer Risks from Arsenic in Drinking Water. Environ. Health Perspect. 97, 259–267. doi:10.1289/ehp.9297259
Stephens, J. K. (2002). Deterioration of Stored Domestic Water Quality and Diarrhoea in Zenu. University of Ghana.
Stevenson, A. H. (1953). Studies of Bathing Water Quality and Health. Am. J. Public Health Nations Health 43 (5 Pt 1), 529–538. doi:10.2105/ajph.43.5_pt_1.529
Team, S. H. (2004). Water, Sanitation and Hygiene Links to Health: Facts and Figures. World Health Organization.
Tondel, M., Rahman, M., Magnuson, A., Chowdhury, I. A., Faruquee, M. H., and Ahmad, S. A. (1999). The Relationship of Arsenic Levels in Drinking Water and the Prevalence Rate of Skin Lesions in Bangladesh. Environ. health Perspect. 107 (9), 727–729. doi:10.1289/ehp.99107727
Tseng, C.-H., Lei, C., and Chen, Y.-C. (2018). Evaluating the Health Costs of Oral Hexavalent Chromium Exposure from Water Pollution: A Case Study in Taiwan. J. Clean. Prod. 172, 819–826. doi:10.1016/j.jclepro.2017.10.177
Ustaoğlu, F., Tepe, Y., Taş, B., and Pag, N. (2020). Assessment of Stream Quality and Health Risk in a Subtropical Turkey River System: A Combined Approach Using Statistical Analysis and Water Quality Index. Ecol. Indic., 113. doi:10.1016/j.ecolind.2019.105815
Vartiainen, T., Pukkala, E., Rienoja, T., Strandman, T., and Kaksonen, K. (1993). Population Exposure to Tri- and Tetrachloroethene and Cancer Risk: Two Cases of Drinking Water Pollution. Chemosphere 27 (7), 1171–1181. doi:10.1016/0045-6535(93)90165-2
Victora, C. G., Smith, P. G., Vaughan, J. P., Nobre, L. C., Lombard, C., Teixeira, A. M. B., et al. (1988). Water Supply, Sanitation and Housing in Relation to the Risk of Infant Mortality from Diarrhoea. Int. J. Epidemiol. 17 (3), 651–654. doi:10.1093/ije/17.3.651
Vladeva, S., Gatseva, P., and Gopina, G. (2000). Comparative Analysis of Results from Studies of Goitre in Children from Bulgarian Villages with Nitrate Pollution of Drinking Water in 1995 and 1998. Cent. Eur. J. Public Health 8 (3), 179
Waddington, H., Snilstveit, B., White, H., and Fewtrell, L. (2009). Water, Sanitation and Hygiene Interventions to Combat Childhood Diarrhoea in Developing Countries. New Delhi India Global Development Network International Initiative for Impact Evaluation Aug.
Witkowski, K. M., and Johnson, N. E. (1992). Organic-solvent Water Pollution and Low Birth Weight in Michigan. Soc. Biol. 39 (1-2), 45–54. doi:10.1080/19485565.1992.9988803
Wu, C., Maurer, C., Wang, Y., Xue, S., and Davis, D. L. (1999). Water Pollution and Human Health in China. Environ. Health Perspect. 107 (4), 251–256. doi:10.1289/ehp.99107251
Wu, H., Gai, Z., Guo, Y., Li, Y., Hao, Y., and Lu, Z. N. (2020). Does Environmental Pollution Inhibit Urbanization in China? A New Perspective through Residents' Medical and Health Costs. Environ. Res. 182 (Mar.), 109128–109128.9. doi:10.1016/j.envres.2020.109128
Xiao, J., Wang, L., Deng, L., and Jin, Z. (2019). Characteristics, Sources, Water Quality and Health Risk Assessment of Trace Elements in River Water and Well Water in the Chinese Loess Plateau. Sci. Total Environ. 650 (Pt 2), 2004–2012. doi:10.1016/j.scitotenv.2018.09.322
Xu, C., Xing, D., Wang, J., and Xiao, G. (2019). The Lag Effect of Water Pollution on the Mortality Rate for Esophageal Cancer in a Rapidly Industrialized Region in China. Environ. Sci. Pollut. Res. 26 (32), 32852–32858. doi:10.1007/s11356-019-06408-z
Xu, X., Wang, Q., and Li, C. (2022b). The Impact of Dependency Burden on Urban Household Health Expenditure and its Regional Heterogeneity in China: Based on Quantile Regression Method. Front. Public Health 10, 876088. doi:10.3389/fpubh.2022.876088
Xu, X., Yang, H., and Li, C. (2022a). Theoretical Model and Actual Characteristics of Air Pollution Affecting Health Cost: A Review. Ijerph 19, 3532. doi:10.3390/ijerph19063532
Yassin, M. M., Amr, S. S. A., and Al-Najar, H. M. (2006). Assessment of Microbiological Water Quality and its Relation to Human Health in Gaza Governorate, Gaza Strip. Public Health 120 (12), 1177. doi:10.1016/j.puhe.2006.07.026
Yau, V., Wade, T. J., de Wilde, C. K., and Colford, J. M. (2009). Skin-related Symptoms Following Exposure to Recreational Water: a Systematic Review and Meta-Analysis. Water Expo. Health 1 (2), 79–103. doi:10.1007/s12403-009-0012-9
Zaveri, E. D., Russ, J. D., Desbureaux, S. G., Damania, R., Rodella, A. S., and Ribeiro Paiva De Souza, G. (20203). The Nitrogen Legacy: The Long-Term Effects of Water Pollution on Human Capital. World Bank Policy Research Working Paper.
Zhang, X.-L., Bing, Z., Xing, Z., Chen, Z.-F., Zhang, J.-Z., Liang, S.-Y., et al. (2003). Research and Control of Well Water Pollution in High Esophageal Cancer Areas. Wjg 9 (6), 1187–1190. doi:10.3748/wjg.v9.i6.1187
Keywords: water pollution, human health, disease heterogeneity, water intervention, health cost
Citation: Lin L, Yang H and Xu X (2022) Effects of Water Pollution on Human Health and Disease Heterogeneity: A Review. Front. Environ. Sci. 10:880246. doi: 10.3389/fenvs.2022.880246
Received: 21 February 2022; Accepted: 09 June 2022;
Published: 30 June 2022.
Edited by:
Ahmed El Nemr, National Institute of Oceanography and Fisheries (NIOF), EgyptReviewed by:
Behzad Shahmoradi, Kurdistan University of Medical Sciences, IranAtik Kulakli, American University of the Middle East, Kuwait
Copyright © 2022 Lin, Yang and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaocang Xu, 03122@zjhu.edu.cn
 Li Lin1
Li Lin1 Haoran Yang
Haoran Yang Xiaocang Xu
Xiaocang Xu