- 1Centre for Evidence-Based Medicine, Nuffield Department of Primary Care Health Sciences, Radcliffe Observatory Quarter, University of Oxford, Oxford, United Kingdom
- 2Trip Database Ltd., Newport, United Kingdom
Introduction: Respiratory viral pathogens are a major cause of morbidity and mortality, and there is a need to understand how to prevent their transmission.
Methods: We performed a scoping review to assess the amount and scope of published research literature on environmental factors, including meteorological factors and pollution, that affect the transmission of respiratory viral pathogens. We used Joanna Briggs Institute methodology for conducting a scoping review. We searched the electronic databases: MEDLINE, Register of Controlled Trials (Cochrane CENTRAL), TRIP database, WHO Covid-19 Database, Global Index Medicus, LitCovid, medRxiv, and Google Scholar. We included studies on environmental exposures and transmission of respiratory viruses (including but not restricted to: influenza, respiratory syncytial virus (RSV), human coronaviruses, viral pneumonia).
Results: The searches identified 880 studies for screening; after screening we included 481 studies, including 395 primary studies and 86 reviews. Data were extracted by one reviewer (ES) and independently checked by a second reviewer for accuracy (AP). All primary studies were observational, mostly using an ecological design; 2/395 primary studies were prospective cohorts. Among the primary studies, 241/395 were on SARS-CoV-2/COVID-19; 95 focussed on influenza; the remaining 59 reported on RSV, other coronaviruses, and other respiratory viruses. Exposures were most commonly temperature (306 primary studies) and humidity (201 primary studies); other commonly reported exposures were air pollution, wind speed, precipitation, season, and UV radiation. It was frequently reported, but not consistently, that temperature, humidity and air pollution were positively correlated with COVID-19 cases/deaths; for influenza, season/seasonality was commonly reported to be associated with cases/deaths.
Discussion: The majority of studies reported on SARS-CoV-2/COVID-19 and were of ecological design. Few prospective cohort studies have been done for any respiratory virus and environmental exposures. Understanding the role of environmental factors on transmission is limited by the lack of prospective cohort studies to inform decision making.
Systematic Review Registration: https://osf.io/ntdjx/, identifier: 10.17605/OSF.IO/NTDJX.
1 Introduction
Environmental factors including temperature and humidity, climate and weather, pollution, and UV radiation are thought to impact on transmission of respiratory viruses such as rhinoviruses, adenoviruses, and coronaviruses. For example, studies have shown that temperature and humidity affect influenza and coronavirus transmission (1, 2) and sunlight may inactivate the SARS-CoV-2 virus on surfaces (3). There are no up-to-date systematic reviews, using comprehensive literature searches and assessment of the risk of bias in included studies, that assess environmental effects on respiratory virus transmission as a whole. Recent systematic reviews have focused on COVID-19 and single environmental factors, such as climate variables and seasonality (4, 5), temperature and humidity (6), with one systematic review focusing on seasonal patterns of influenza (7). However, there was no review collating all the published evidence on the effect of environmental factors on respiratory virus transmission. Environmental factors could have significant consequences on severity of infection and transmission and therefore it is critical to understand how the environment impacts person-to-person spread and therefore which public health interventions might reduce transmission.
Due to the heterogeneous nature of existing research publications in this area, including case series, prospective and retrospective cohort studies, randomised controlled trials, and reviews, the most appropriate methodology was to conduct a scoping review. In doing this review, we aimed to collate and present studies assessing the relationship between environmental factors and the transmission of respiratory pathogens, to describe the extent and range of the research in this area, to describe the approaches that have been used thus far, and to identify gaps in research. The methodology followed that published by the Joanna Briggs Institute (8).
2 Methods
We used the five steps described by the Joanna Briggs Institute methodology for conducting a scoping review: 1. Set the research question 2. Search strategy 3. Selection of studies 4. Charting the data 5. Collating and reporting. The review was conducted according to PRISMA guidance for Scoping reviews (9).
2.1 The research question
Our research question was: What are the environmental factors that affect respiratory viral pathogen transmission and outcomes? The exposure (E) of interest was therefore environmental factors and their effect on respiratory virus transmission (O) in the general population (P).
2.2 Search strategy
The search strategy was developed with an information specialist (JB). We conducted a literature search in electronic databases including MEDLINE, Register of Controlled Trials (Cochrane CENTRAL), TRIP database, WHO Covid-19 Database, Global Index Medicus, LitCovid, medRxiv, and Google Scholar. The search was conducted from inception of the databases up until 20 November 2022. We searched the reference lists of included studies. We based the search on Medical Subject Heading (MeSH) terms for databases utilising MeSH. For non-MeSH databases we based the search on keywords and synonyms to identify: household pollution; household damp; household mould; waste disposal services; climate; temperature; vapour pressure; humidity; precipitation; wind speed; indoor ventilation; altitude; population density; respiratory pathogen; respiratory disease; respiratory infection; respiratory mortality; pneumonia; bronchitis; influenza; coronavirus; common cold; bronchiolitis; tonsillitis; laryngitis; sinusitis; chest infection; respiratory hospital admissions; respiratory diagnoses.
The literature search strategy can be viewed in Supplementary Data Sheet 1.
2.3 Selection of studies for inclusion
Studies were independently screened for inclusion by two reviewers (JB, ES) and duplicate screened by a third reviewer (AP).
2.3.1 Eligibility criteria
Prospective or retrospective observational studies including case series and ecological designs (that is studies looking at patterns of rates of disease and environment factor observations such as daily meteorological records) or interventional including randomised trials and clinical reports, outbreak reports, case-control studies, experimental studies, and reviews were eligible to be included. Studies incorporating models to describe observed data were eligible to be included, while studies reporting models based on simulated data were excluded. Studies reporting solely predictive modelling were excluded as the focus of the review was not on the prediction of future events. Studies were restricted to those related to transmission in humans. No language restrictions were imposed.
2.4 Charting the data
We charted the data, including data on study design, population characteristics, environmental exposures under investigation, and outcomes of interest. Data were extracted by one reviewer (ES) and independently checked by a second reviewer for accuracy (AP). We present a description of studies, with a summary of the evidence they present. This is in table form, including the exposures as sub categories, i.e., altitude, air pollution, air temperature, temperature and humidity, seasonality, and multiple meteorlogical variables with or without additional variables such as pollution. As is recognised practice within scoping review methodology, no formal assessment of study quality was conducted (8).
2.5 Collating and reporting the data
To show the distributions of numbers of studies reporting certain outcomes, and numbers of studies reporting certain exposures, we created figures to illustrate the data. We described the findings of the scoping review narratively.
3 Results
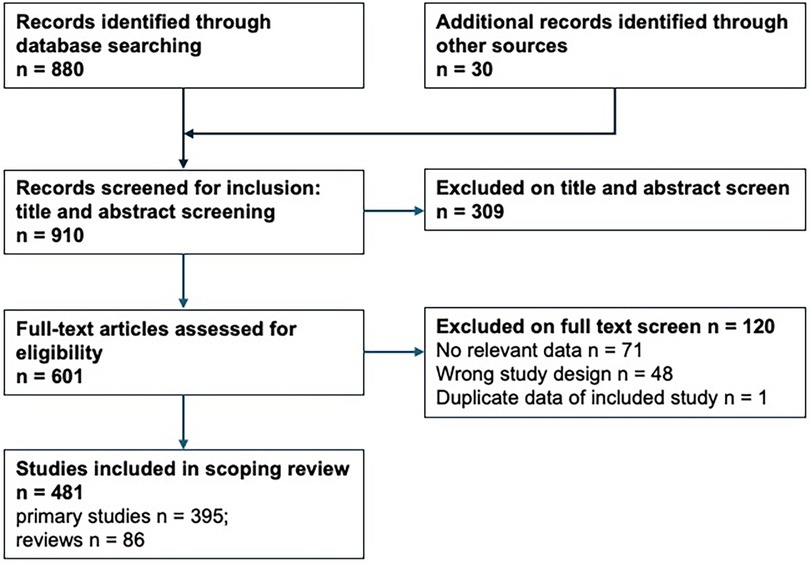
The literature search identified 880 studies for screening and 30 additional possible studies were identified from additional sources, which included screening reference lists of included reviews. After title and abstract screening, 601 studies were reviewed in full text. Figure 1 summarises the search results and the inclusion and exclusion of studies.
At full text screening, 120 studies were excluded, these are listed in Supplementary Data Sheet 2. Studies excluded at full text. Reasons for exclusion were: no relevant data, n = 71 (including some studies from which relevant data could not be separated from non-relevant data); wrong study design, n = 48 (including laboratory experimental, predictive modelling, studies describing solely hypotheses rather than observations); duplicate data of already included study, n = 1). After full text screening, we included 481 studies: 395 relevant primary studies and 86 reviews.
Essential characteristics of included studies were extracted and are presented in Supplementary Data Sheet 3 (Supplementary Tables S1A–S1F) and Supplementary Data Sheet 4 (Supplementary Table S2. Reviews).
The design and methods used by the studies were not always clear and therefore study methods are outlined in the table, noting the study design where possible. No primary study was an intervention study; thus all studies were observational. Most used an ecological design looking at patterns of rates of disease and environment factor observations (such as daily meteorological records); many of these studies can be described as cross-sectional or retrospective, often using data collected as part of surveillance systems for infectious disease; some can be described as longitudinal, in recording infections over a period of time and examining associations with rates and types over that period of time.
Two of the 395 primary studies were prospective cohort studies (Flight et al. 2014 and Gordon et al. 2009), i.e., recruited individuals without relevant respiratory infections at baseline and followed up the cohort over a period of time, observing incident respiratory infections. Associations with environmental factors and infection rates and types were reported for the follow-up period. One was a study of participants with cystic fibrosis followed over a period of one year, that showed that rhinovirus peaked in summer and autumn, and non-rhinovirus respiratory viral infection peaked in winter and spring (Flight et al. 2014). One was a study of dengue over two years that reported that influenza-like illness showed strong seasonality (Gordon et al. 2009).
Some studies reported multiple outcomes, so tallies of study outcomes may not total to 481. Whilst studies of any respiratory viral infectious disease were eligible for inclusion, 241/395 (61%) included primary studies (and 54/86 [63%] reviews) investigated SARS-CoV-2/COVID-19 and were published within the last three years. The remaining 154 primary studies looked at influenza (unspecified and specified influenza virus subtypes, 95 studies) or influenza-like illness (8 studies); SARS (8 studies); MERS (3 studies); human coronaviruses other than SARS, MERS, SARS-CoV-2 (5 studies); pneumonia (19 studies); respiratory syncytial virus (26 studies); rhinovirus (13 studies); other respiratory diseases combined, including but not necessarily restricted to viral respiratory diseases (23 studies). The 32 non-COVID-19/SARS-CoV-2 reviews looked at influenza (10 reviews), or other diseases including pneumonia, and/or overall respiratory morbidity and/or mortality (22 reviews).
Supplementary Table S1A–1F show the primary studies categorised according to the main focus of the studies: 7 focussed solely or mainly on altitude (Supplementary Table S1A), and overall reported decreased case numbers at higher altitude. Twenty-two studies focussed solely or mainly on air pollution (Supplementary Table S1B), and tended to report higher case numbers associated with regions or time periods of higher air pollution. Twenty-six studies focussed solely or mainly on air temperature (Supplementary Table S1C), most often reporting decreased case numbers at higher temperatures, but there was variability in the time periods, geographical regions, and temperature ranges of the study settings and results varied across the studies. Forty studies reported on air temperature and humidity (Supplementary Table S1D), mainly reporting that case rates were higher at lower temperatures and lower humidity, but there was heterogeneity of the studies’ settings and methods and the results varied.
Supplementary Table S1E shows the 39 studies that reported on season or seasonality (potentially not considered as an exposure per se, but related to meteorological factors and thus included in this scoping review); these tended to show marked patterns of case numbers associated with season, and repeated cycle of case increases and decreases across consecutive years, i.e., seasonality patterns.
Supplementary Table S1F shows the 261 primary studies that reported on combinations of meteorological factors, often including temperature and humidity, with or without air pollution, season, altitude and other factors. As within the studies above, case numbers tended to be observed as higher during higher temperature and humidity, higher pollution, winter and early spring season; the observational nature of the studies made it difficult to establish the relative importance of these factors and whether they were causal, interrelated, or confounding.
Among the reviews, shown in Supplementary Table S2, 24 reviewed studies of air pollution; 19 reviewed studies of temperature with or without humidity; 11 reviewed studies of season or seasonality; and 32 reviewed studies of combinations of meteorological and pollution exposures. The conclusions these reviews drew were in line with the findings of the primary studies included in this scoping review, and since they were all based on observational data, they were unable to establish firm conclusions.
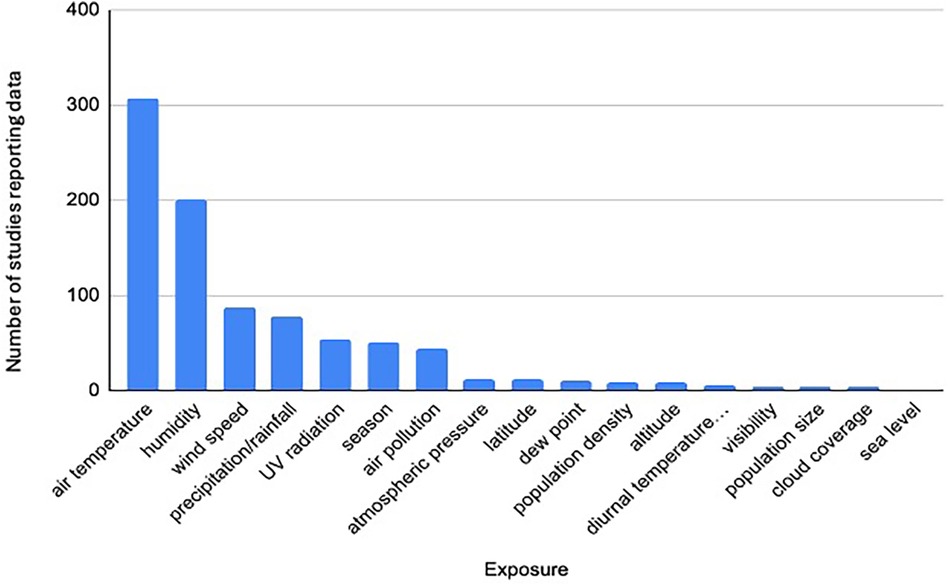
To indicate the topics on which research has been focussed, Figure 2 shows the number of primary studies reporting data for each exposure (not solely considering the main focus of the study). Exposures were most commonly meteorological: 226 primary studies reported on air temperature; 201 on humidity; 88 on wind speed; 78 on precipitation; 54 on UV radiation; 44 on air pollution; 143 studies reported on other exposures including a range of meteorological and geographical exposures.
Of the included studies, 241/395 (61%) primary studies included focussed on SARS-CoV-2/COVID-19 and were published within the last three years. Ninety-five primary studies looked at influenza (unspecified and specified viruses, 16 studies; 26 studies reported on RSV; 19 on pneumonia; 18 on human metapneumovirus; 13 on rhinovirus; 8 on influenza-like illness; 8 on SARS; 8 on human bocavirus; 5 on human coronavirus (other than SARS, SARS-CoV-2; including 229E, NL63, OC43, or HKU1); 4 on acute respiratory infection, not otherwise specified; 3 on MERS; 3 on bronchiolitis; 3 on respiratory disease not otherwise specified; 2 on adenovirus.
Figure 3 shows the number of primary studies reporting data for each respiratory outcome (some studies reported data for multiple outcomes).
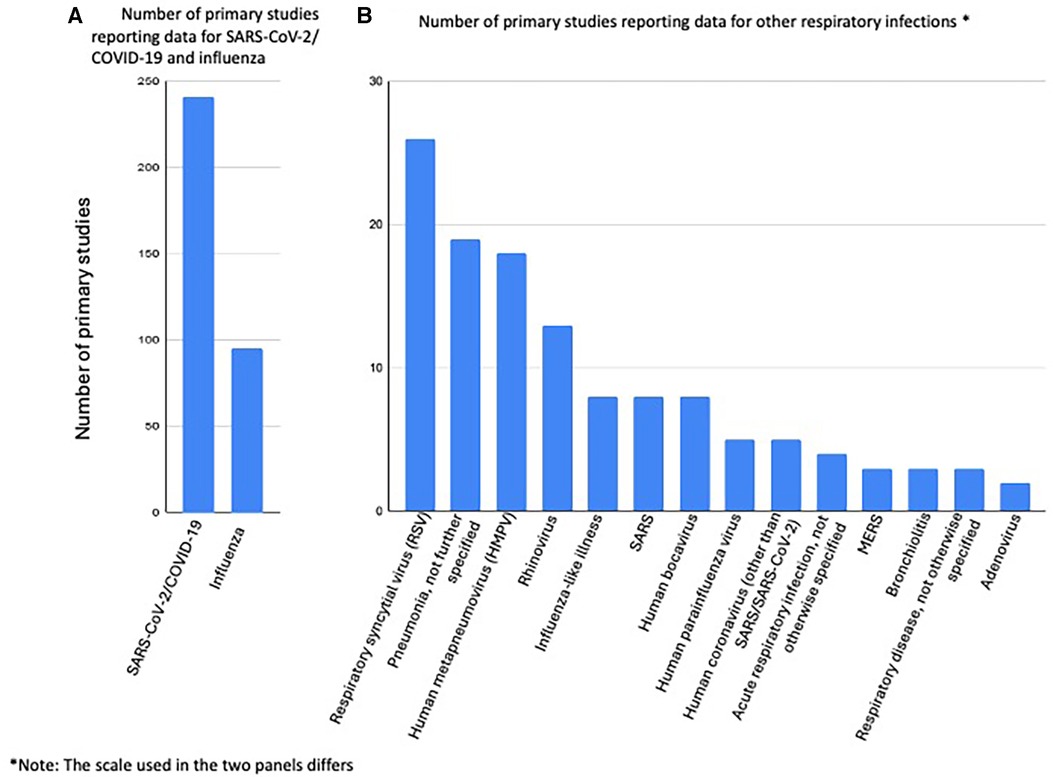
Figure 3. Bar chart showing the number of primary studies reporting data for each respiratory disease investegated. (A) Number of primary studies reporting data for SARS-CoV-2/COVID-19 and influenza. (B) Number of primary studies reporting data for other respiratory infections*. Note: The scale used in the two panels differs.
Among the 86 reviews, the number of COVID outcome reviews was 54; 10 looked at studies of influenza; 5 reviews looked at RSV; 39 reviews looked at other respiratory disease including pneumonia; 34 reviews address air pollution and respiratory disease; 25 looked at temperature, or temperature & humidity; and 25 reported on studies of various climate and meteorological factors.
4 Discussion
In this scoping review of the published literature, the findings of the included primary studies and reviews showed that in general, cold and dry weather conditions were associated with more rapid increase in numbers of identified SARS-CoV-2 infections. Air pollution was repeatedly associated with higher levels of respiratory disease, and data for identifying specific relationships between air pollutants and viral respiratory outcomes were very limited.
This scoping review is not intended to evaluate the content of the included studies in detail, nor to assess quality of the identified studies. It does highlight the range and amount of published literature on the relationship between environmental factors and transmission of respiratory viral infections: whilst there are a considerable number of studies on SARS-CoV-2/COVID-19, there are far fewer on any other respiratory infections, such as RSV, pneumonia, human metapneumovirus, rhinovirus, SARS, and human bocavirus. Findings of studies on SARS-CoV-2 are not consistent, but do support there being relationships between environmental factors such as air temperature and humidity, air pollution and virus transmission. Studies of influenza indicate seasonal patterns and more detailed information on environmental exposures is more limited. Influenza typically exhibited a mid-winter peak in both the Northern and Southern hemisphere. Other respiratory viruses have only limited research evidence on environmental factors and transmission.
Most primary studies used ecological approaches and/or surveillance data to investigate relationships between environmental factors and respiratory disease. Only two of the 395 included primary studies used a prospective cohort design.
We acknowledge that extracting data from this large number of studies may be incomplete; in addition, categorising exposures was challenging due to reporting variability, with studies lacking detail as to the exposures that were investigated, particularly when multiple exposures were considered, such as meteorological factors, pollution, temperature, weather variables and population size. The reviews identified and included in this scoping review may also incorporate some of the included primary studies.
The large number of studies published on SARS-CoV-2/COVID-19 reflects the interest and concern in the first years since the pandemic began. This is notable in contrast to the small number of studies on environmental exposures and SARS (2003) or MERS (2015), outbreaks of which posed serious public health challenges at the time. Despite the large volume of studies on the SARS-CoV-2 virus, they are all observational in nature and lack detailed information on how risk factors relate to documented transmission; therefore, public health advice about environmental influences and risk of transmission based on these data would still be unclear. It is worth considering this in the context of concern about research waste (10), with many primary studies not referring to existing systematic review literature and reviews conducted without using systematic methodology.
In summary, a considerable number of studies have been published reporting on a range of environmental exposures and transmission of a number of respiratory viruses, with the large majority utilising ecological observational study designs. Whilst there continues to be a lack of prospective or interventional data, it is difficult from these data to draw conclusions. This scoping review may form a basis for further investigation into respiratory virus transmission and potential to slow or reduce the impact of outbreaks of respiratory viral infections by understanding the role of environmental factors on transmission. High quality prospective studies are required to better understand the role of environmental factors on transmission of respiratory viruses.
4.1 Protocol availability
The protocol for this review can be accessed at Open Science Framework (11).
4.2 Registration
The review is accessible at Open Science Framework.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
ES: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. JB: Data curation, Investigation, Methodology, Writing – review & editing. AP: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This study/project is funded by the National Institute for Health and Care Research (NIHR) School for Primary Care Research (project 569). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Conflict of interest
AP receives funding from the National Institute for Health and Care Research (NIHR) School for Primary Care Research. JB is a major shareholder and employee of the Trip Database search engine www.tripdatabase.com.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fenvh.2024.1345403/full#supplementary-material
References
1. Chin AWH, Perera MRA, Hui KPY, Yen H-L, Chan MCW, Peiris M, et al. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe. (2020) 1(e10). doi: 10.1016/S2666-5247(20)30003-3
2. Marr LC, Tang JW, Van Mullekom J, Lakdawala SS. Mechanistic insights into the effect of humidity on airborne influenza virus survival, transmission and incidence. J R Soc Interface. (2019) 16:20180298. doi: 10.1098/rsif.2018.0298
3. Ratnesar-Shumate S, Williams G, Green B, Krause M, Holland B, Wood S, et al. Simulated sunlight rapidly inactivates SARS-CoV-2 on surfaces. J Infect Dis. (2020) 222:214–22. doi: 10.1093/infdis/jiaa274
4. Zheng HL, Guo ZL, Wang ML, Yang C, An SY, Wu W. Effects of climate variables on the transmission of COVID-19: a systematic review of 62 ecological studies. Environ Sci Pollut Res Int. (2021) 28(39):54299–316. doi: 10.1007/s11356-021-15929-5
5. Li Y, Wang X, Nair H. Global seasonality of human seasonal coronaviruses: a clue for postpandemic circulating season of severe acute respiratory syndrome coronavirus 2? J Infect Dis. (2020) 222(7):1090–7. doi: 10.1093/infdis/jiaa436
6. Mecenas P, Bastos RTDRM, Vallinoto ACR, Normando D. Effects of temperature and humidity on the spread of COVID-19: a systematic review. PLoS One. (2020) 15(9):e0238339. doi: 10.1371/journal.pone.0238339
7. Iribhogbe OI, Samuel SO, Ohaju-Obodo JO. Human influenza viruses in south-east and east Asia: a systematic review of seasonal patterns, viral types/subtypes, and antiviral susceptibility pattern in the past two decades. Int J Basic Clin Pharmacol. (2020) 9(9):1444–53. doi: 10.18203/2319-2003.ijbcp20203634
8. Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. (2020) 18(10):2119–26. doi: 10.11124/JBIES-20-00167
9. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for scoping reviews (PRISMAScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
10. Chalmers I, Glasziou P. Avoidable waste in the production and reporting of research evidence. Lancet. (2009) 374(9683):86–9. doi: 10.1016/S0140-6736(09)60329-9
Keywords: respiratory viral pathogen, environmental factors, influenza virus, coronavirus, pollution, transmission, weather, climate
Citation: Spencer E, Brassey J and Pluddemann A (2024) What are the environmental factors that affect respiratory viral pathogen transmission and outcomes? A scoping review of the published literature. Front. Environ. Health 3:1345403. doi: 10.3389/fenvh.2024.1345403
Received: 27 November 2023; Accepted: 31 January 2024;
Published: 15 February 2024.
Edited by:
Reginald Quansah, University of Ghana, GhanaReviewed by:
Sorina Eftim, ICF, United StatesAnn Grimm, United States Environmental Protection Agency, United States
© 2024 Spencer, Brassey and Pluddemann. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Annette Pluddemann YW5uZXR0ZS5wbHVkZGVtYW5uQHBoYy5veC5hYy51aw==
 Elizabeth Spencer1
Elizabeth Spencer1 Annette Pluddemann
Annette Pluddemann