- 1Department of Neurosurgery, Nanchong Central Hospital, The Second Clinical Medical College, North Sichuan Medical College, Nanchong, Sichuan, China
- 2Nanchong Institute of Cerebrovascular Diseases, Nanchong, Sichuan, China
- 3Sichuan Clinical Research Center for Neurological Disease, Nanchong, Sichuan, China
- 4Department of Neurosurgery, Chongqing General Hospital, Chongqing University, Chongqing, China
Objective: While infertility affects about 15% of women during their reproductive years, its long-term impact on stroke mortality after this period remains unclear. This study aims to investigate the association between infertility and stroke mortality in women using data from the Prostate, Lung, Colorectal, and Ovarian (PLCO) cancer screening trial.
Methods: We analyzed data from 75,778 female participants aged 55–74 years with a median follow-up of 16.84 years. Cox proportional hazard models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for stroke mortality, adjusting for potential confounders.
Results: Among participants, 14.53% reported infertility. During follow-up, 1,159 women died from stroke. Compared to women without infertility, those with infertility had a higher risk of stroke mortality (HR 1.21, 95% CI 1.04–1.41, p = 0.016). This association remained statistically significant after adjusting for age, race, education level, marital status, smoking status, body mass index, history of hypertension, history of heart attack, history of diabetes mellitus, birth control pill use, hormone replacement therapy, endometriosis, first menstrual period and pregnancy history (HR 1.20, 95% CI 1.02–1.42, p = 0.029). Sensitivity and subgroup analyses yielded consistent results.
Conclusion: The findings of this study indicate that infertility is associated with an increased risk of stroke mortality in women. Further research is needed to confirm these findings and elucidate the underlying mechanisms.
Introduction
Stroke is a leading cause of death among women globally, with the aging population significantly contributing to the increasing incidence of this disease. In 2019, an estimated 12 million individuals suffered strokes globally, with more than 6.5 million succumbing to this devastating condition (1).
Infertility, defined as the inability to conceive after one year of unprotected, regular and timed intercourse, is increasingly recognized as a significant public health issue, affecting approximately 15% of women (2, 3). This condition is often linked to premature ovarian insufficiency, polycystic ovary syndrome (PCOS), endometriosis, and uterine fibroids, which are associated with low levels of ovarian hormones, hyperandrogenism, insulin resistance, and systemic inflammation. These factors contribute to endothelial dysfunction and promote atherosclerosis (4–6). Moreover, infertility and stroke share common risk factors, such as hypertension, obesity, and diabetes. Additionally, treatments for infertility, such as in vitro fertilization or hormone therapy, can increase the likelihood of blood clot formation, which may, in turn, elevate the risk of stroke (7, 8). Beyond physical health concerns, infertility can also lead to psychological distress, including depression, anxiety, and interpersonal difficulties, which may further contribute to stroke risk. The combination of these psychological factors with the underlying physiological disturbances may create a unique risk profile for stroke in infertile women. Previous research has indicated that infertility is a marker of increased long-term risk for all-cause mortality in women (9–11), as well as mortality from late-stage cancer and cardiovascular events (10–14). However, the specific relationship between infertility and stroke mortality remains inconclusive.
In this cohort study, we aim to explore the potential association between infertility and stroke mortality by utilizing data from the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial. Understanding this connection is crucial for identifying high-risk individuals, developing effective preventive strategies, and uncovering the common biological mechanisms underlying both conditions.
Methods
Data set
The PLCO Cancer Screening Trial was a large randomized controlled trial designed to assess the impact of specific cancer screening tests on mortality rates for prostate, lung, colorectal, and ovarian cancers (15). Conducted between November 1993 and July 2001, the study recruited approximately 155,000 participants aged 42–78 years from 10 different centers across the United States, including Birmingham, Detroit, Denver, Honolulu, Marshfield, Minneapolis, Pittsburgh, Salt Lake City, St. Louis, and Washington D.C. Detailed inclusion and exclusion criteria are available on the National Cancer Institute’s website (https://cdas.cancer.gov/learn/plco/trial-summary). Participants were randomly allocated to either the intervention arm, where they underwent cancer screening tests, or the control arm, where they received standard medical care without cancer screenings. Data were collected through a baseline questionnaire detailing demographic and health-related information, including age, sex, race, education, body measurements, medical history, smoking habits, and reproductive factors such as infertility.
This study utilized data from the PLCO Cancer Screening Trial to explore the associations between infertility and stroke mortality.
Participant screening
According to the study design, 76,678 male participants were excluded, and 78,209 female participants were included. Of the female participants, 2,094 were excluded due to missing baseline questionnaires, and 337 were excluded due to missing data on infertility. After applying the inclusion and exclusion criteria, the final sample for the infertility study comprised 75,778 women, including women who later became pregnant. Figure 1 illustrates the screening process.
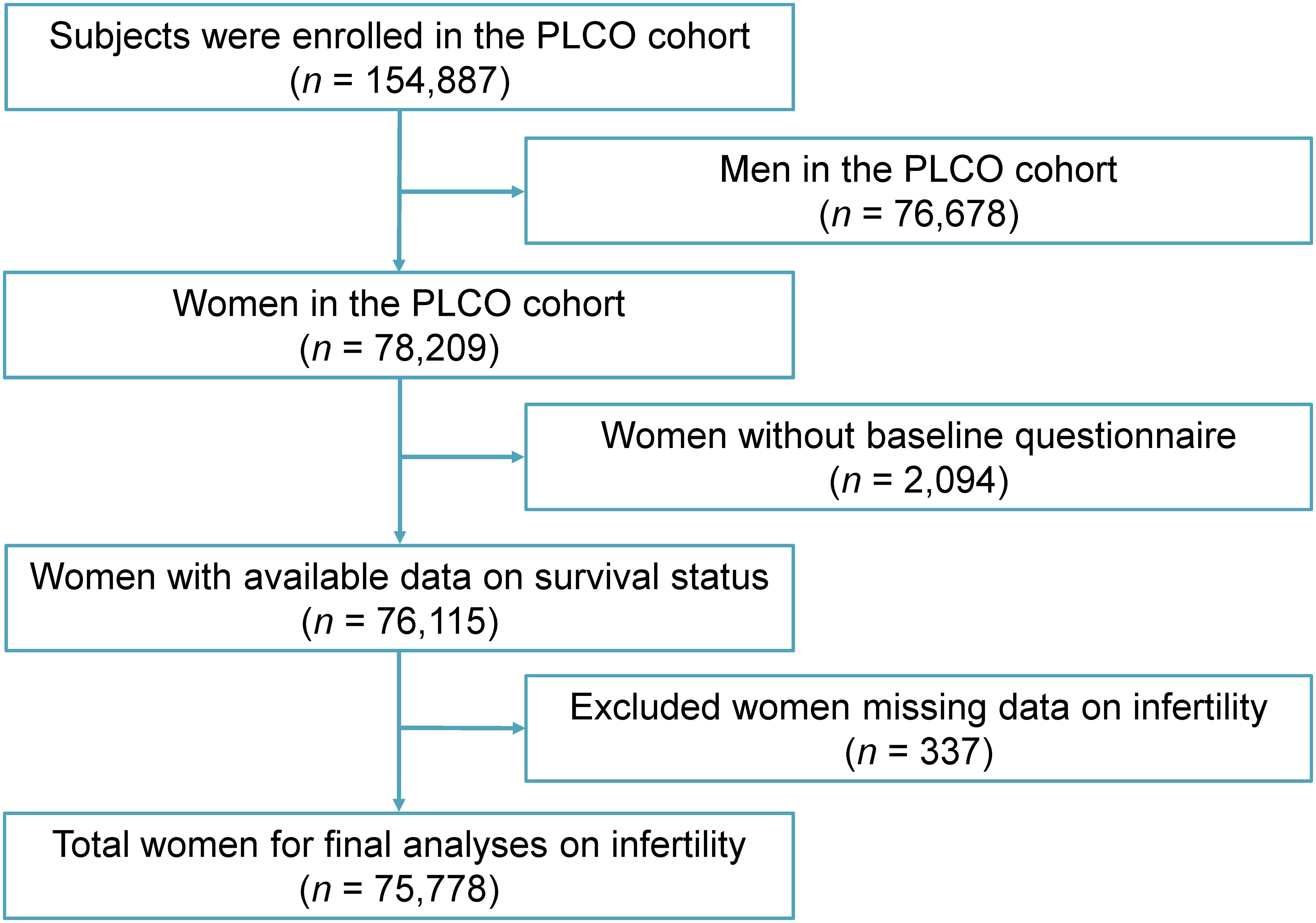
Figure 1. Flow chart of the screening process. PLCO, Prostate, Lung, Colorectal and Ovarian cancer screening trial.
Exposure assessment
Infertility is defined as the inability to conceive after one year or more of regular, unprotected sexual intercourse. In the self-reported baseline questionnaire of the PLCO study, female infertility was assessed using the following reproductive health question: “Have you ever tried to become pregnant for a year or more without success?”. Participants who responded “yes” were classified into the “infertility” group. Participants with missing data on infertility were excluded from all analyses.
Outcome assessment
The PLCO Cancer Screening Trial Centers implemented a multifaceted approach to ensure complete ascertainment of deaths. This included annual study update forms, reports from relatives or obituaries, and exhaustive searches of the Social Security Death Index and National Death Index for all participants. Underlying causes of death were ascertained using the 9th edition of the International Classification of Diseases from death certificates obtained from state vital statistics bureaus. To guarantee the validity of trial outcomes, a Death Review Process was established, involving a meticulous review of medical records for all decedents. This information was then used for statistical analyses of primary endpoints. Survival time was defined as the interval between randomization and either stroke-related death or the pre-defined follow-up cutoff date.
Statistical analysis
All statistical evaluations were performed utilizing R software (version 4.1.3). The baseline attributes were expressed as counts and percentages for categorical variables, which were compared using the chi-square test. Continuous variables were represented as median (interquartile range, IQR) and compared using the Kruskal-Wallis test.
Women without reported infertility were designated as the reference group, while those reporting infertility were considered as the exposed group. Stroke death was designated as the primary outcome. We first performed univariable survival analysis to assess the association between infertility and stroke mortality, using the Kaplan-Meier method to estimate the survival probability curves. Multivariable analysis was based on a Cox proportional hazards regression model, adjusted for age, race, marital status, education level, smoking status, body mass index, history of hypertension, history of heart attack, history of diabetes mellitus, birth control pill use, hormone replacement therapy, endometriosis, first menstrual period and pregnancy history. We constructed multiple multivariable models to perform sensitivity analyses. Additionally, this study carries out subgroup analyses, accounting for potential confounding factors, to explore the relationship between infertility and stroke mortality, with the goal of assessing result consistency.
Covariates were selected based on prior literature examining associations with infertility and cardiovascular health (14, 16, 17). Age (continuous, in years) was adjusted alongside the following baseline variables: race (white or other), education level (below or at least university degree), marital status (ever married/living with partner or never married), smoking status (never, former or current), body mass index (BMI) categories (underweight/normal [less than 25kg/m²], overweight [25 to less than 30kg/m²], obese [greater than or equal to 30kg/m²]), history of hypertension (yes or no), history of heart attack (yes or no), history of diabetes mellitus (yes or no), birth control pill use (yes or no), hormone replacement therapy (yes or no), endometriosis (yes or no), first menstrual period (≤11 years, 12–13 years, or ≥14 years) and pregnancy history (yes or no). Subgroup analyses were conducted based on these potential confounders to evaluate the consistency of results. All tests were two-sided with a significance level of α = 0.05.
Results
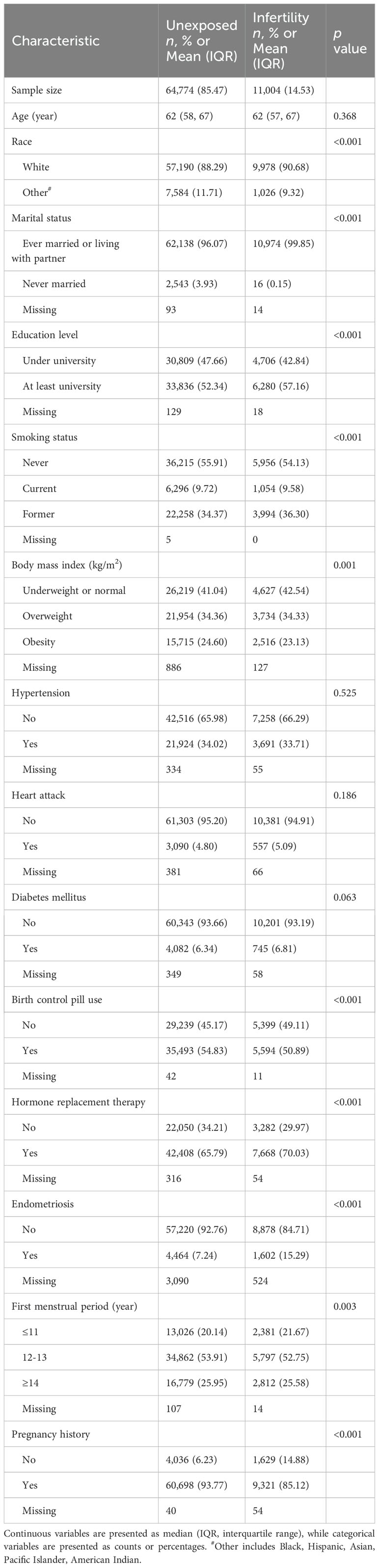
Among 75,778 participants, 14.53% (n = 11,004) self-reported infertility, while 85.47% (n = 64,774) reported no infertility. The baseline characteristics of the participants are summarized in Table 1. During a follow-up period of 16.84 (14.77–18.78) years, 17,209 women died, including 1,159 from stroke and 16,050 from other causes (Supplementary Table 1).
Kaplan-Meier survival analysis was utilized to assess the survival disparity between infertile and non-infertile women. The findings revealed a statistically significant difference in survival probability between the two groups, as illustrated in Figure 2. Table 2 presents the results of unadjusted and adjusted analyses for the hazard ratios of stroke mortality. Unadjusted analysis showed that women with infertility had a higher risk of stroke death than those without infertility (HR 1.21, 95% CI 1.04–1.41, p = 0.016). After adjusting for potential confounders, the associations were slightly attenuated but remained statistically significant (HR 1.20, 95% CI 1.02–1.42, p = 0.029). Sensitivity analysis was conducted using multiple models incorporating different confounding factors, and the findings remained consistent (Table 2). Subgroup analyses based on pre-defined confounding factors suggested no significant differences in the results (Figure 3).
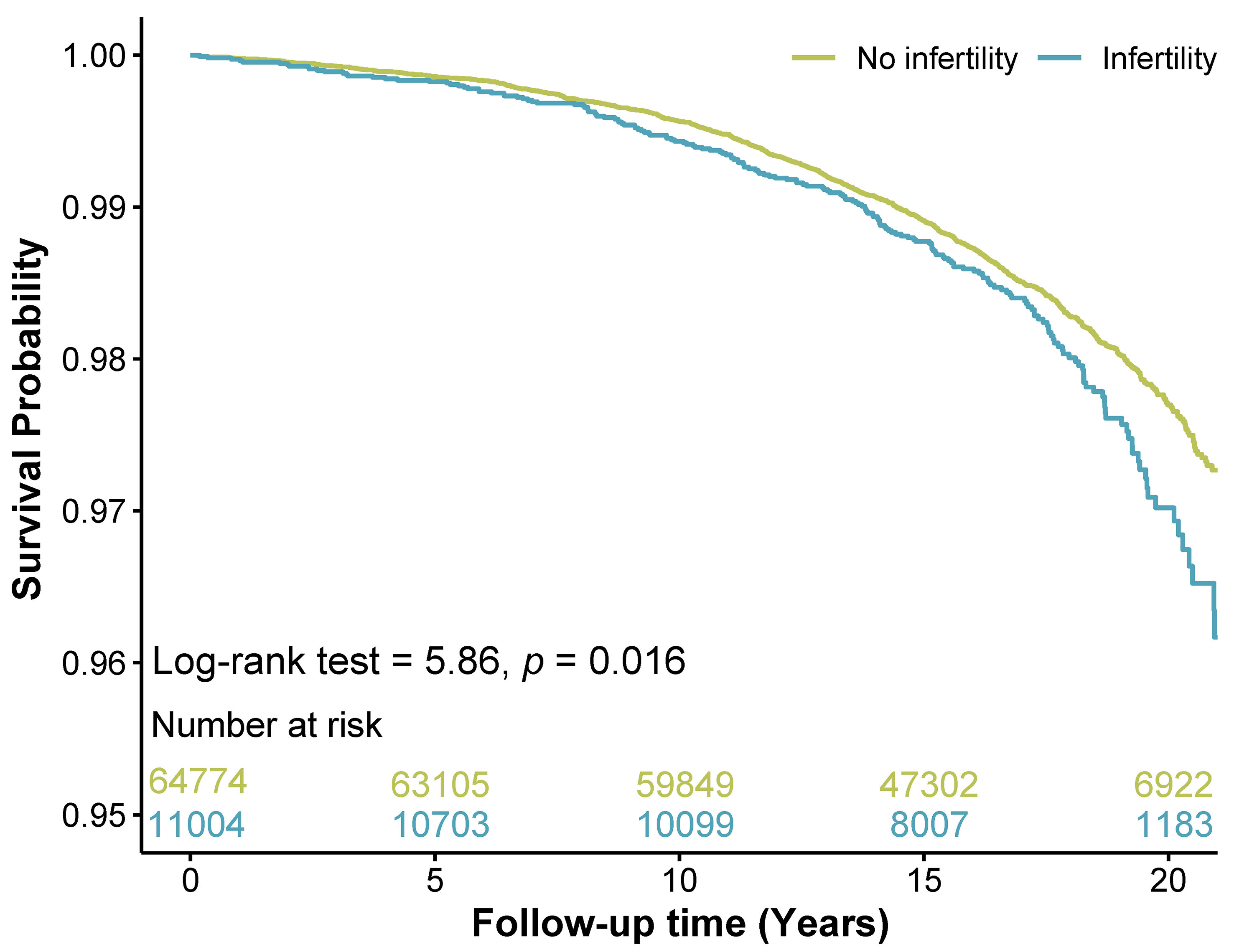
Figure 2. Kaplan-meier survival curves for stroke mortality in women with and without infertility. The cyan line represented the survival rate of women with infertility, and the yellow line represented the survival rate of women without infertility. The survival table details the number of women available for analysis at each time point.
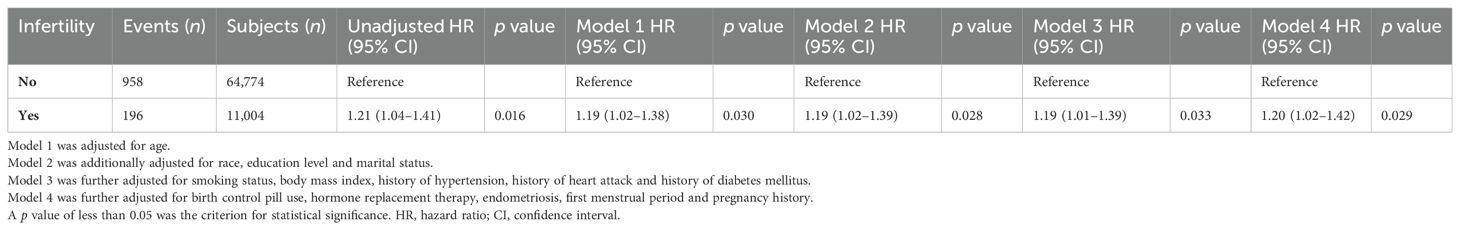
Table 2. Unadjusted and adjusted hazard ratios of the association between infertility and stroke mortality.
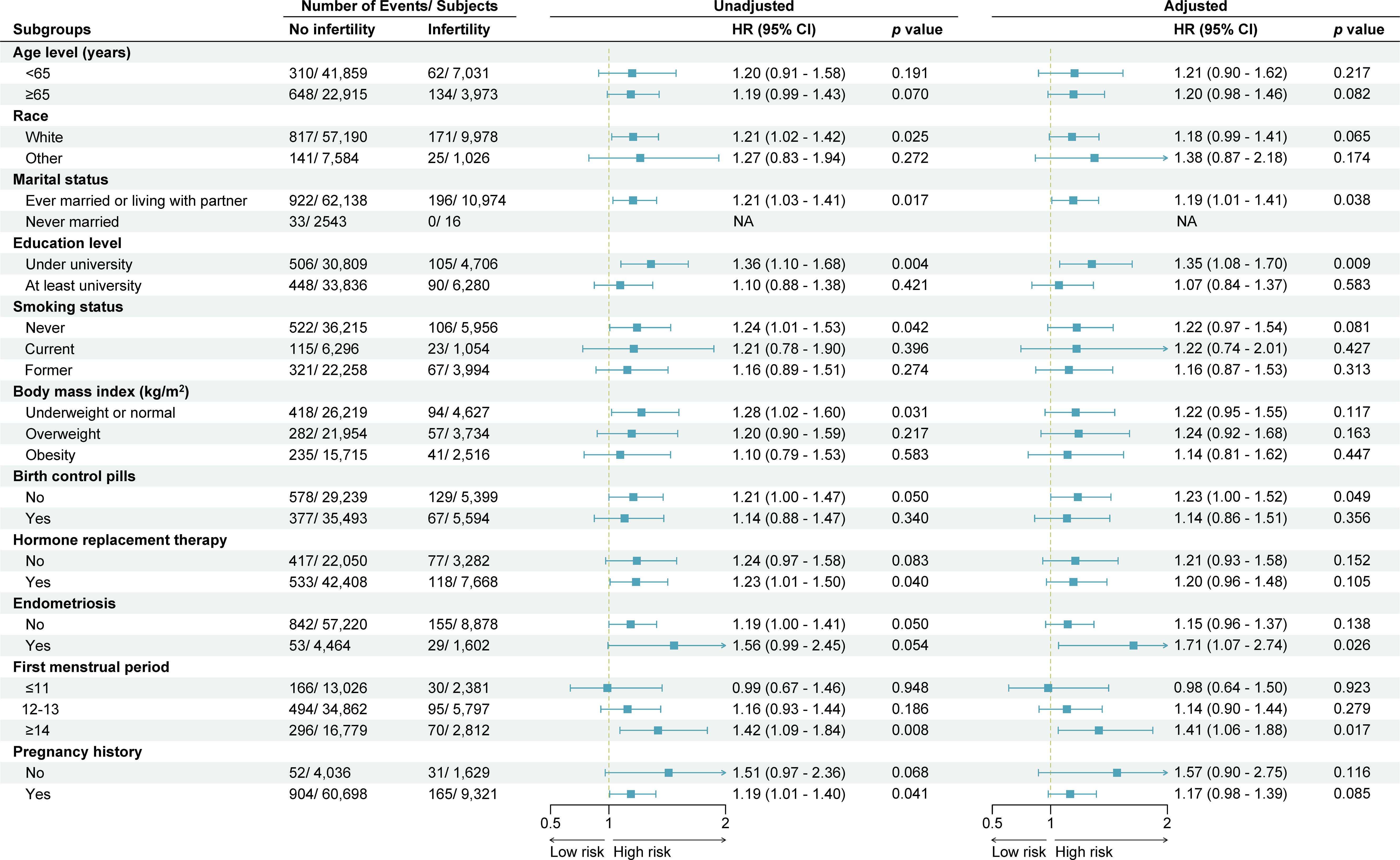
Figure 3. Subgroup analysis and forest plot for stroke-cause mortality in women with and without infertility. This forest plot shows the number of deaths and subjects, unadjusted and adjusted hazard ratios (HR) with 95% confidence interval (CI), according to baseline characteristics. Hazard ratios were adjusted for age, race, marital status, education level, smoking status, body mass index, history of hypertension, history of heart attack, history of diabetes mellitus, birth control pill use, hormone replacement therapy, endometriosis, first menstrual period and pregnancy history. NA, not available.
Discussion
In the PLCO Cancer Screening Trial study of 78,209 women with a median follow-up of 16.84 years, 1,159 died of stroke. Our study found that women with infertility had a higher risk of stroke death compared to women without infertility.
Prior studies investigating the association between infertility and stroke incidence have yielded mixed results, with some studies reporting an increased risk of stroke in infertile women (10, 18), while others have found no such association (14, 19, 20). Two studies examined mortality in relation to infertility, with consistent findings indicating an elevated all-cause mortality risk in infertile women, while demonstrating no association with cardiovascular disease mortality (10, 11). Notably, no studies have exclusively investigated the relationship between infertility and stroke mortality. Our present analysis using PLCO Cancer Screening Trial data reveals a 20% higher risk of stroke mortality in infertile women.
Our findings contrast with other studies that found no significantly increased risk of mortality from cardiovascular diseases in infertile women. Several possible explanations may account for for this discrepancy. First, the two previous studies failed to differentiate between stroke, ischemic heart disease, and other circulatory system diseases. Remarkably, approximately three-quarters of all strokes occur in individuals aged 65 years or older. Short follow-up periods may result in an underestimation of stroke mortality. Therefore, further research is needed to clarify this issue.
Several mechanisms might explain our findings. Although transient hormonal fluctuations are common among women, infertile women often experience chronic and persistent hormonal imbalances. These sustained imbalances lead to prolonged vascular dysfunction, which significantly elevated risk of stroke (5). Furthermore, specific causes of female infertility, such as endometriosis and PCOS (21), which were also found to be associated with stroke risk (4, 22–26). Endometriosis induces systemic inflammation through pro-inflammatory cytokines such as IL-1β, IL-6, and TNF-α (23). This chronic inflammatory state can induce a hypercoagulable environment, thereby increasing the risk of cardiovascular complications, such as stroke (5, 27). Our data indicate a significantly higher prevalence of endometriosis among women with infertility (15.29%) compared to those without (7.24%). Further subgroup analysis by history of endometriosis showed women with endometriosis have a significantly higher risk of stroke mortality compared to the general population. PCOS can induce insulin resistance, promoting atherosclerosis and platelet aggregation, all of which elevate ischemic stroke risk (5, 28). Infertility treatments, such as in vitro fertilization or hormone therapy, can induce a hypercoagulable state, increasing the risk of thrombosis and subsequently stroke (7, 8). Due to the absence of data on PCOS and infertility treatments in PLCO study, the impact of PCOS-related infertility and infertility treatments on stroke mortality remains unconfirmed in the current analysis. Therefore, further research should focus more specifically on identifying the underlying causes of female infertility and their potential link to stroke mortality.
This study leverages a large prospective cohort with long-term follow-up, strengthening its generalizability. However, some limitations also exist in the current study. First, the reliance on self-reported data from a retrospective questionnaire on infertility introduces potential bias. Second, the lack of data on male partner fertility may lead to an overestimation of the association between female infertility and stroke mortality, as infertility can be attributed to factors from either or both partners. Third, the absence of detailed stroke subtype and fertility treatment data in the PLCO study impedes the differentiation between hemorrhagic and ischemic stroke mortality and hampers the assessment of risks associated with fertility treatment status. Lastly, this study focused on individuals within the U.S., indicating that future research in other geographic regions is necessary to validate and generalize these findings.
Conclusions
Our findings suggest that infertility might be a potential risk factor for stroke mortality in women, potentially serving as an early indicator of long-term cerebrovascular health. Well-designed prospective cohort studies are crucial to validate these observations. Further research is warranted to elucidate the underlying mechanisms linking infertility and stroke mortality.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: While the current study utilized data from the National Cancer Institute PLCO study group under a data use license, accessing this dataset requires following specific procedures. Requests to access these datasets should be directed to https://cdas.cancer.gov/plco.
Ethics statement
The studies involving humans were approved by the Ethics Committees of all PLCO cancer screening trial centers. The institutional review board of the National Cancer Institute (NCI) approved the study protocol after review (under protocols PLCO-811 and PLCO-836). The participants provided their written informed consent to participate in the PLCO study at study entry. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
HT: Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Supervision, Visualization, Writing – original draft, Writing – review & editing. XY: Formal analysis, Visualization, Writing – original draft, Investigation. ZL: Data curation, Formal analysis, Investigation, Writing – original draft. YZ: Formal analysis, Methodology, Writing – original draft, Investigation. HC: Formal analysis, Investigation, Methodology, Writing – original draft. MD: Data curation, Investigation, Writing – original draft. CS: Data curation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Research and Development Foundation of Bureau of Science & Technology and Intellectual Property Nanchong City (20SXQT0087) and Research Projects of Sichuan Provincial Research Center for Primary Healthcare Development (SWFZ22-Y-14). The funders had no role in study design, data collection and analysis, publication decisions, or manuscript preparation.
Acknowledgments
The authors gratefully acknowledge the National Cancer Institute for providing access to data from the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial. We acknowledge the use of generative AI technologies, including Google's Gemini 1.5 and Grammarly, to enhance the clarity and readability of this manuscript. These tools were used for grammar and style checks only and did not generate any original content. Special thanks to Dr. Jing Du from the Beijing Center for Disease Prevention and Control for her invaluable guidance and insightful suggestions on statistical analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2024.1433930/full#supplementary-material
References
1. Collaborators GS. Global, regional, and national burden of stroke and its risk factors, 1990-2019: A systematic analysis for the global burden of disease study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/s1474-4422(21)00252-0
2. Infertility Workup for the Women's Health Specialist. Infertility workup for the women’s health specialist: acog committee opinion, number 781. Obstetrics Gynecology. (2019) 133:e377–e84. doi: 10.1097/aog.0000000000003271
3. Talmor A, Dunphy B. Female obesity and infertility. Best Pract Res Clin Obstet Gynaecol. (2015) 29:498–506. doi: 10.1016/j.bpobgyn.2014.10.014
4. Farland LV, Degnan WJ 3rd, Bell ML, Kasner SE, Liberman AL, Shah DK, et al. Laparoscopically confirmed endometriosis and risk of incident stroke: A prospective cohort study. Stroke. (2022) 53:3116–22. doi: 10.1161/strokeaha.122.039250
5. Liang C, Chung HF, Dobson AJ, Mishra GD. Infertility, miscarriage, stillbirth, and the risk of stroke among women: A systematic review and meta-analysis. Stroke. (2022) 53:328–37. doi: 10.1161/strokeaha.121.036271
6. Scicchitano P, Dentamaro I, Carbonara R, Bulzis G, Dachille A, Caputo P, et al. Cardiovascular risk in women with pcos. Int J Endocrinol Metab. (2012) 10:611–8. doi: 10.5812/ijem.4020
7. Sachdev D, Yamada R, Lee R, Sauer MV, Ananth CV. Risk of stroke hospitalization after infertility treatment. JAMA Netw Open. (2023) 6:e2331470. doi: 10.1001/jamanetworkopen.2023.31470
8. Dayan N, Filion KB, Okano M, Kilmartin C, Reinblatt S, Landry T, et al. Cardiovascular risk following fertility therapy: systematic review and meta-analysis. J Am Coll Cardiol. (2017) 70:1203–13. doi: 10.1016/j.jacc.2017.07.753
9. Murugappan G, Li S, Alvero RJ, Luke B, Eisenberg ML. Association between infertility and all-cause mortality: analysis of us claims data. Am J Obstet Gynecol. (2021) 225:57.e1–.e11. doi: 10.1016/j.ajog.2021.02.010
10. Stentz NC, Koelper N, Barnhart KT, Sammel MD, Senapati S. Infertility and mortality. Am J Obstet Gynecol. (2020) 222:251.e1–.e10. doi: 10.1016/j.ajog.2019.09.007
11. Wang YX, Farland LV, Wang S, Gaskins AJ, Wang L, Rich-Edwards JW, et al. Association of infertility with premature mortality among us women: prospective cohort study. Lancet Reg Health Am. (2022) 7:1–14. doi: 10.1016/j.lana.2021.100122
12. Wang S, Gaskins AJ, Farland LV, Zhang D, Birmann BM, Rich-Edwards JW, et al. A prospective cohort study of infertility and cancer incidence. Fertil Steril. (2023) 120:134–42. doi: 10.1016/j.fertnstert.2023.02.028
13. Gleason JL, Shenassa ED, Thoma ME. Self-reported infertility, metabolic dysfunction, and cardiovascular events: A cross-sectional analysis among U.S. Women. Fertil Steril. (2019) 111:138–46. doi: 10.1016/j.fertnstert.2018.10.009
14. Liang C, Chung HF, Dobson AJ, Hayashi K, van der Schouw YT, Kuh D, et al. Infertility, recurrent pregnancy loss, and risk of stroke: pooled analysis of individual patient data of 618 851 women. Bmj. (2022) 377:e070603. doi: 10.1136/bmj-2022-070603
15. Zhu CS, Pinsky PF, Kramer BS, Prorok PC, Purdue MP, Berg CD, et al. The prostate, lung, colorectal, and ovarian cancer screening trial and its associated research resource. J Natl Cancer Inst. (2013) 105:1684–93. doi: 10.1093/jnci/djt281
16. Cairncross ZF, Ahmed SB, Dumanski SM, Nerenberg KA, Metcalfe A. Infertility and the risk of cardiovascular disease: findings from the study of women’s health across the nation (Swan). CJC Open. (2021) 3:400–8. doi: 10.1016/j.cjco.2020.11.011
17. Nichols AR, Rifas-Shiman SL, Switkowski KM, Zhang M, Young JG, Hivert MF, et al. History of infertility and midlife cardiovascular health in female individuals. JAMA Netw Open. (2024) 7:e2350424. doi: 10.1001/jamanetworkopen.2023.50424
18. Skåra KH, Åsvold BO, Hernáez Á, Fraser A, Rich-Edwards JW, Farland LV, et al. Risk of cardiovascular disease in women and men with subfertility: the trøndelag health study. Fertil Steril. (2022) 118:537–47. doi: 10.1016/j.fertnstert.2022.05.038
19. Udell JA, Lu H, Redelmeier DA. Long-term cardiovascular risk in women prescribed fertility therapy. J Am Coll Cardiol. (2013) 62:1704–12. doi: 10.1016/j.jacc.2013.05.085
20. Bungum AB, Glazer CH, Arendt LH, Schmidt L, Pinborg A, Bonde JP, et al. Risk of hospitalization for early onset of cardiovascular disease among infertile women: A register-based cohort study. Hum Reprod. (2019) 34:2274–81. doi: 10.1093/humrep/dez154
21. Tarín JJ, García-Pérez MA, Hamatani T, Cano A. Infertility etiologies are genetically and clinically linked with other diseases in single meta-diseases. Reprod Biol Endocrinol. (2015) 13:31. doi: 10.1186/s12958-015-0029-9
22. Zheng M, Zheng S. Endometriosis increases the risk of stroke: A mendelian randomization study. Stroke. (2023) 54:e30–e3. doi: 10.1161/strokeaha.122.041163
23. Poeta do Couto C, Policiano C, Pinto FJ, Brito D, Caldeira D. Endometriosis and cardiovascular disease: A systematic review and meta-analysis. Maturitas. (2023) 171:45–52. doi: 10.1016/j.maturitas.2023.04.001
24. Okoth K, Wang J, Zemedikun D, Thomas GN, Nirantharakumar K, Adderley NJ. Risk of cardiovascular outcomes among women with endometriosis in the United Kingdom: A retrospective matched cohort study. Bjog. (2021) 128:1598–609. doi: 10.1111/1471-0528.16692
25. Wekker V, van Dammen L, Koning A, Heida KY, Painter RC, Limpens J, et al. Long-term cardiometabolic disease risk in women with pcos: A systematic review and meta-analysis. Hum Reprod Update. (2020) 26:942–60. doi: 10.1093/humupd/dmaa029
26. Zhou Y, Wang X, Jiang Y, Ma H, Chen L, Lai C, et al. Association between polycystic ovary syndrome and the risk of stroke and all-cause mortality: insights from a meta-analysis. Gynecol Endocrinol. (2017) 33:904–10. doi: 10.1080/09513590.2017.1347779
27. Vazgiourakis VM, Zervou MI, Papageorgiou L, Chaniotis D, Spandidos DA, Vlachakis D, et al. Association of endometriosis with cardiovascular disease: genetic aspects (Review). Int J Mol Med. (2023) 51:1–16. doi: 10.3892/ijmm.2023.5232
Keywords: infertility, stroke, mortality, female, long-term impact
Citation: Tang H, Yang X, Li Z, Zhang Y, Chen H, Dai M and Shao C (2024) Association between female infertility and stroke mortality: evidence from the PLCO cancer screening trial. Front. Endocrinol. 15:1433930. doi: 10.3389/fendo.2024.1433930
Received: 16 May 2024; Accepted: 02 September 2024;
Published: 24 September 2024.
Edited by:
Jan Tesarik, MARGen Clinic, SpainReviewed by:
Izuchukwu Azuka Okafor, Nnamdi Azikiwe University, NigeriaYefang Huang, Hospital of Chengdu University of Traditional Chinese Medicine, China
Copyright © 2024 Tang, Yang, Li, Zhang, Chen, Dai and Shao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chuan Shao, c2NzaGFvY2h1YW5AeWFob28uY29t; c2hhb2NodWFuQG5zbWMuZWR1LmNu
†ORCID: Hui Tang, orcid.org/0000-0002-1979-4715
Zhou Li, orcid.org/0009-0008-3343-4039
Yuan Zhang, orcid.org/0009-0007-3807-3191
Mingjun Dai, orcid.org/0009-0000-1011-7032
Chuan Shao, orcid.org/0000-0001-8260-4761
 Hui Tang
Hui Tang Xueming Yang
Xueming Yang Zhou Li
Zhou Li Yuan Zhang
Yuan Zhang Huaxuan Chen
Huaxuan Chen Mingjun Dai
Mingjun Dai Chuan Shao
Chuan Shao