- 1School of Traditional Chinese Medicine, Hunan University of Chinese Medicine, Changsha, Hunan, China
- 2Department of Endocrinology, The First Hospital of Hunan University of Chinese Medicine, Changsha, Hunan, China
Objective: This study aimed to explore the clinical efficacy and acupoint combinations of auricular pressure for treating type 2 diabetes.
Methods: Eight common databases were searched for publications related to auricular pressure in type 2 diabetes as of November 2023. A meta-analysis was performed to assess the efficacy and safety of auricular pressure therapy. Data mining was used to analyze the core acupoints for auricular pressure.
Results: Meta-analysis demonstrated that compared with the conventional treatment group, the combined auricular pressure and conventional treatment group had significantly reduced fasting blood glucose (mean difference [MD]: -0.93; 95% confidence interval [CI]: -1.17 to -0.68; p < 0.00001), 2-hour postprandial blood glucose (MD: -1.58; 95% CI: -2.04 to -1.12; p < 0.00001), glycated hemoglobin A1c (MD: -0.83; 95% CI: -1.19 to -0.48; p < 0.00001), total cholesterol (MD: -0.43; 95% CI: -0.72 to -0.14; p = 0.004), triglycerides (MD: -0.33; 95% CI: -0.64 to -0.03; p < 0.00001), systolic blood pressure (MD: -14.75; 95% CI: -24.46 to -5.05; p = 0.003), diastolic blood pressure (MD: -10.32; 95% CI: -20.14 to -0.50; p = 0.04), and body mass index (MD: -1.74; 95% CI: -2.61 to -0.87; p < 0.0001), while adverse events were comparable (RR: 0.84; 95% CI: 0.43 to 1.66; p = 0.61). Egger’s test revealed no publication bias (p = 0.715). Data mining identified AH6a, TF4, AT4, CO18, and CO10 as core acupoints for treating type 2 diabetes with auricular pressure.
Conclusion: Auricular pressure safely improves blood glucose and lipid levels, blood pressure, and body mass index in patients with type 2 diabetes. A regimen consisting of AH6a, TF4, AT4, CO18, and CO10 is expected to serve as a complementary treatment for type 2 diabetes.
Systematic review registration: www.crd.york.ac.uk/prospero/display_record.php?RecordID=524887, identifier CRD42024524887.
1 Introduction
Type 2 diabetes is a metabolic disease characterized by tissue-specific insulin resistance and pancreatic β-cell dysfunction (1). Epidemiological studies indicate that approximately 537 million people worldwide have diabetes, 90%–95% of whom have type 2 diabetes (2). Type 2 diabetes poses a significant threat to human health, leading to a series of complications such as diabetic nephropathy, retinopathy, cardiomyopathy, and peripheral neuropathy, which seriously jeopardize the physical and mental well-being of patients (3). The global health expenditure for diabetes and its complications was reported to be as high as $760 billion in 2019, placing a huge economic burden on patients, their families, and society (4). Although oral hypoglycemic drugs and insulin help in glycemic control (5), a small number of patients still experience poor glycemic control, and the potential adverse effects of these drugs remain a concern (6); as such, exploring safe, effective, and inexpensive adjuvant therapy for type 2 diabetes is important.
Acupuncture is a traditional Chinese medical technique with a long history of treating diseases by applying stimulation or pressure to specific acupoints. With greater interest in health management and natural therapies in recent years, the role of acupuncture in promoting health and treating diseases has received increasing attention (7, 8). Previous studies have shown that traditional acupuncture therapies, such as moxibustion, cupping, acupoint catgut embedding, acupoint application, and auricular pressure, help improve overall health outcomes (9–13). Auricular pressure is a treatment in which Wangbuliuxing seeds are applied to a patient’s auricular acupoints. It plays a role in treating diseases and strengthening the body through continuous acupoint stimulation (14). Auricular pressure is easy to perform, very safe, and well-tolerated (13); it is widely used in traditional Chinese medicine to treat various diseases such as allergic rhinitis, pain, and insomnia (13–15). Reports indicate that auricular pressure lowers blood glucose, reduces weight, and regulates lipid metabolism (16), indicating that it may be a potential supplementary therapy for type 2 diabetes. However, because of the lack of high-quality evidence, the specific benefits and risks of auricular pressure use in type 2 diabetes are still unclear. In addition, the acupoint selection scheme for auricular pressure treatment of type 2 diabetes has always been controversial. This study aimed to conduct a meta-analysis to assess the efficacy and safety of auricular pressure for type 2 diabetes and to explore a selection scheme of auricular acupoints through data mining.
2 Methods
This study strictly adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (17) and was registered in Prospero (CRD42024524887, www.crd.york.ac.uk/prospero/display_record.php?RecordID=524887).
2.1 Literature retrieval
A literature search was conducted by combining subject terms with extra terms. The subject terms included “auricular pressure” and “type 2 diabetes.”, and extra terms were obtained using MeSH and Sinomed. Relevant literature on the treatment of type 2 diabetes with auricular pressure published before November 2023 was queried in four English databases (Embase, PubMed, the Cochrane Library, and Web of Science) and four Chinese databases (China National Knowledge Infrastructure, China Science and Technology Journal Database, Wanfang, and Sinomed). No language restrictions were imposed.
2.2 Inclusion and exclusion criteria
Inclusion criteria: (і) Subjects meeting the 1999 World Health Organization diagnostic criteria for type 2 diabetes: Fasting blood glucose (FBG) ≥ 7.0 mmol/L or 2-hour postprandial blood glucose (2h-PBG) in oral glucose tolerance tests ≥ 11.1 mmol/L. (іі) The experimental group received conventional treatment combined with auricular pressure, while the control group received conventional treatment. Conventional treatment includes lowering blood glucose and blood pressure as well as regulating blood lipids, among others. (ііі) The efficacy endpoints included blood glucose (FBG, 2h-PBG, glycated hemoglobin A1c [HbA1c]), blood lipids (total cholesterol [TC], triglycerides [TG]), blood pressure (systolic blood pressure [SBP], diastolic blood pressure [DBP]), and body mass index (BMI). The safety endpoint was adverse events. (іv) The study design was a randomized controlled trial.
Exclusion criteria: (і) Duplicate data publication. (іі) Incomplete data. (ііі) Data not deemed usable.
2.3 Literature screening, data collection, and bias risk assessment
All literature was imported into the literature manager, and the included literature was selected based on the inclusion and exclusion criteria. The included literature was then classified, and basic information was extracted into a characteristics table. The risk of bias in the included studies was evaluated using the tools provided in Revman5.3. These tasks were independently completed by Qin Xiang and Xiu Liu, with any objections ruled upon by Yu.
2.4 Statistical analysis
Meta-analysis was performed using Revman5.3. The mean difference (MD) and risk ratio (RR) were used as effect sizes for continuous and dichotomous variables, respectively. Heterogeneity was assessed using the I2 test; when I2 < 50%, a fixed-effect model was used for analysis, while when I2 ≥ 50%, a random-effect model was used. A leave-one-out sensitivity analysis was used to assess the robustness of the results. Egger’s test was performed using Stata15.0 to evaluate publication bias, with p > 0.1 indicating no publication bias. Frequency analysis was performed to obtain common acupoints for auricular pressure treating type 2 diabetes using Traditional Chinese Medicine Case Cloud V2.3, with a frequency threshold of ≥ 30%. The common acupoints were imported into SPSS Modeler 18.0 for association rule analysis, and the following parameters were set to obtain the core auricular acupoint combinations for type 2 diabetes: Apriori model, support ≥ 50%, confidence ≥ 80%, and lift ≥ 1.0. The acupoints that comprised these core acupoint combinations were defined as core acupoints.
3 Results
3.1 Literature screening
The database contained 1570 relevant studies. Ultimately, 14 articles were included (18–31) after 987 were excluded because of duplication, and 569 were excluded because they did not meet the inclusion criteria (Figure 1).
3.2 Basic characteristics of included studies
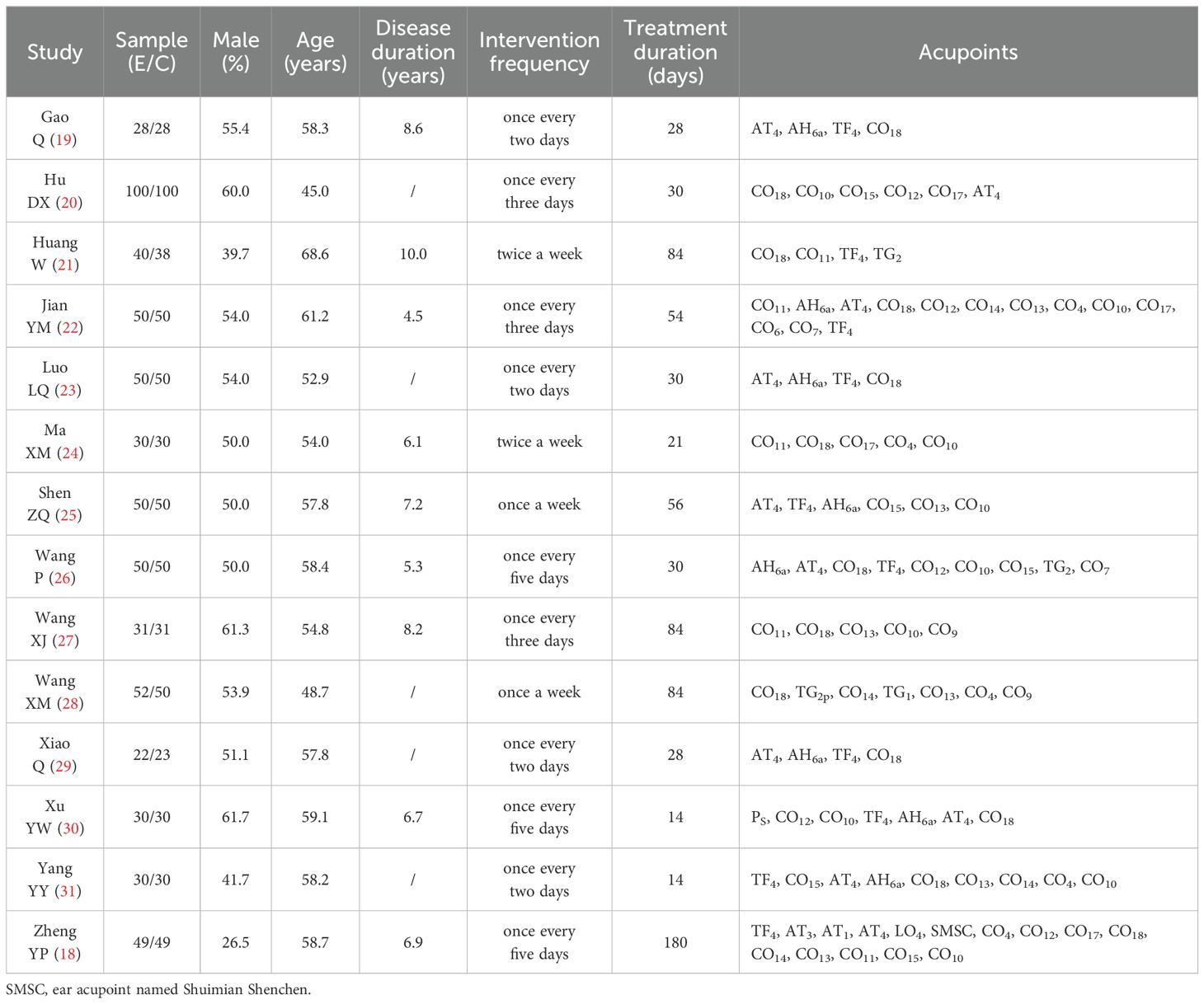
Fourteen clinical trials were included (18–31) with a total sample size of 1221 cases, all conducted in China with publication years ranging from 2014 to 2022. A total of 612 cases received auricular pressure in combination with conventional treatment, while 609 received conventional treatment alone (Table 1).
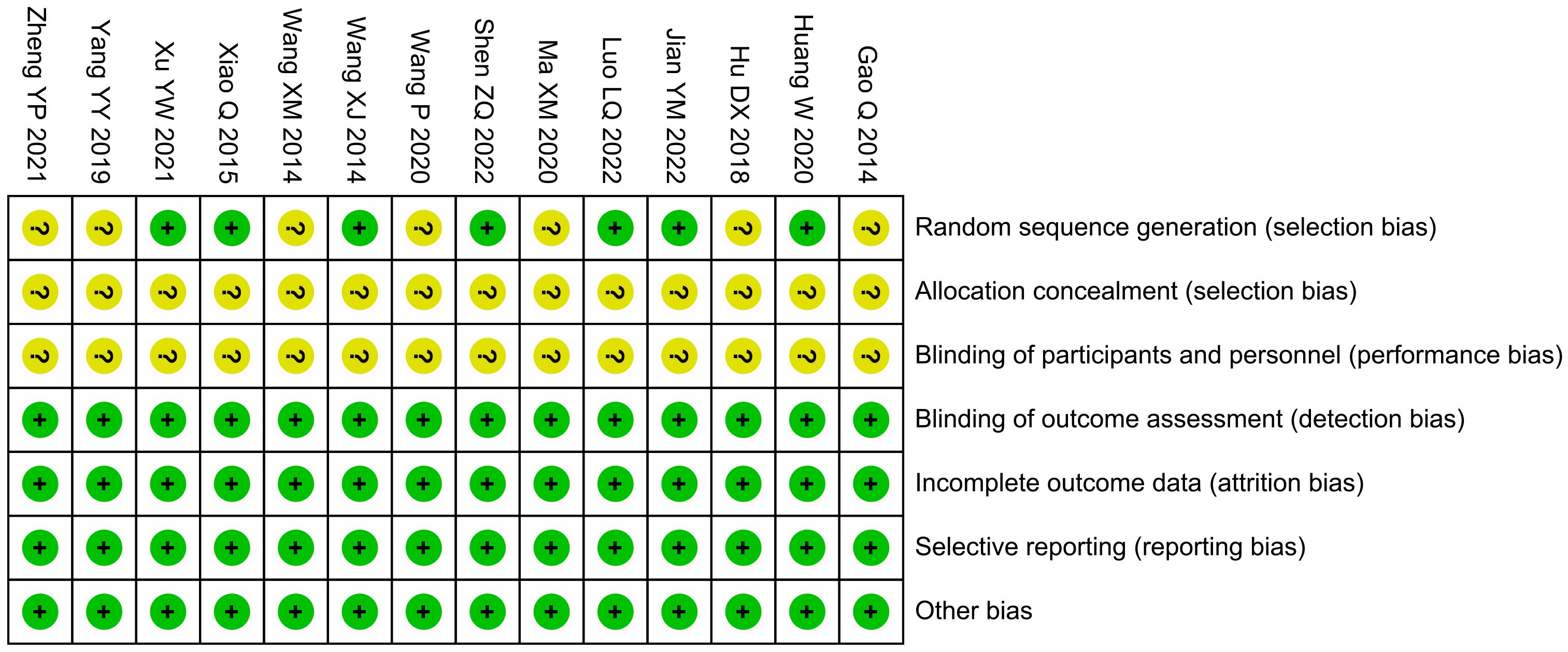
3.3 Bias risk assessment
The bias risk of randomization in seven studies was unclear, while that of allocation concealment, as well as blinding of participants and personnel, was unclear in 14 studies. The risk of bias in other areas was low (Figure 2).
3.4 Efficacy endpoint
3.4.1 Blood glucose
Meta-analysis showed that combined treatment significantly reduced FBG by 0.93 mmol/L (MD: -0.93, 95% confidence interval [CI]: -1.17 to -0.68; p < 0.00001), 2h-PBG by 1.58 mmol/L (MD: -1.58, 95% CI: -2.04 to -1.12; p < 0.00001), and HbA1c by 0.83% (MD: -0.83, 95% CI: -1.19 to -0.48: p < 0.00001) compared with the conventional treatment group (Figure 3). Sensitivity analysis showed that the results were robust.
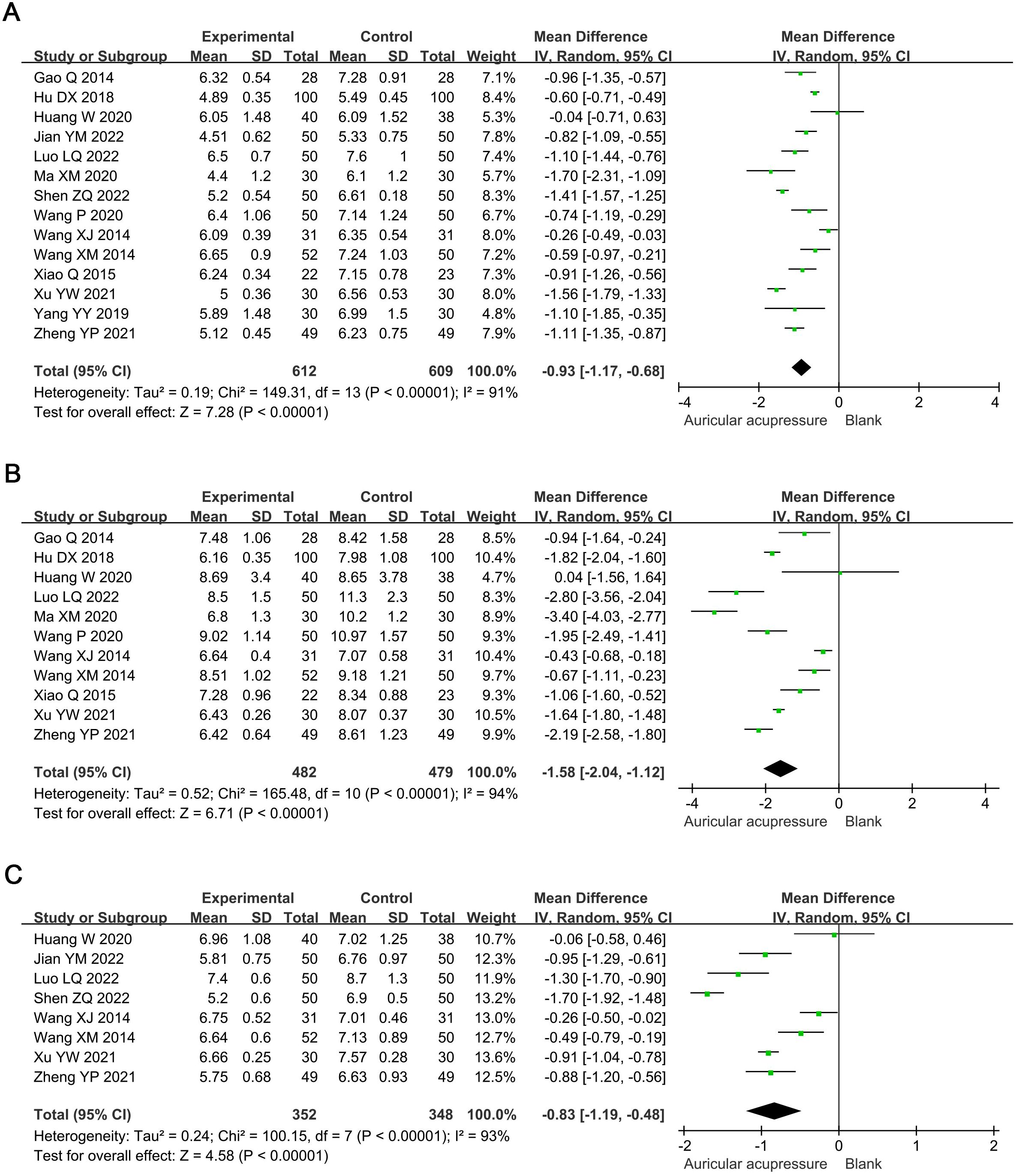
Figure 3. Meta-analysis results of blood glucose in T2D treated with auricular pressure. (A) FBG; (B) 2h-PBG; (C) HbA1c. FBG, fasting blood glucose; PBG, postprandial blood glucose; HbA1c, glycosylated hemoglobin A1c.
3.4.2 Blood lipids
Compared with the conventional treatment group, the combined treatment significantly reduced TC by 0.43 mmol/L (MD: -0.43, 95% CI: -0.72 to -0.14; p = 0.004) and TG by 0.33 mmol/L (MD: -0.33, 95% CI: -0.64 to -0.03; p = 0.03) (Figure 4). Sensitivity analysis showed that the results for TC were robust, whereas those for TG were not; the significance of TG changes disappeared after excluding Jian YM 2022 (MD: -0.29, 95% CI: -0.74 to 0.16; p = 0.21) or Xu YW 2021 (MD: -0.21, 95% CI: -0.47 to 0.04; p = 0.09).
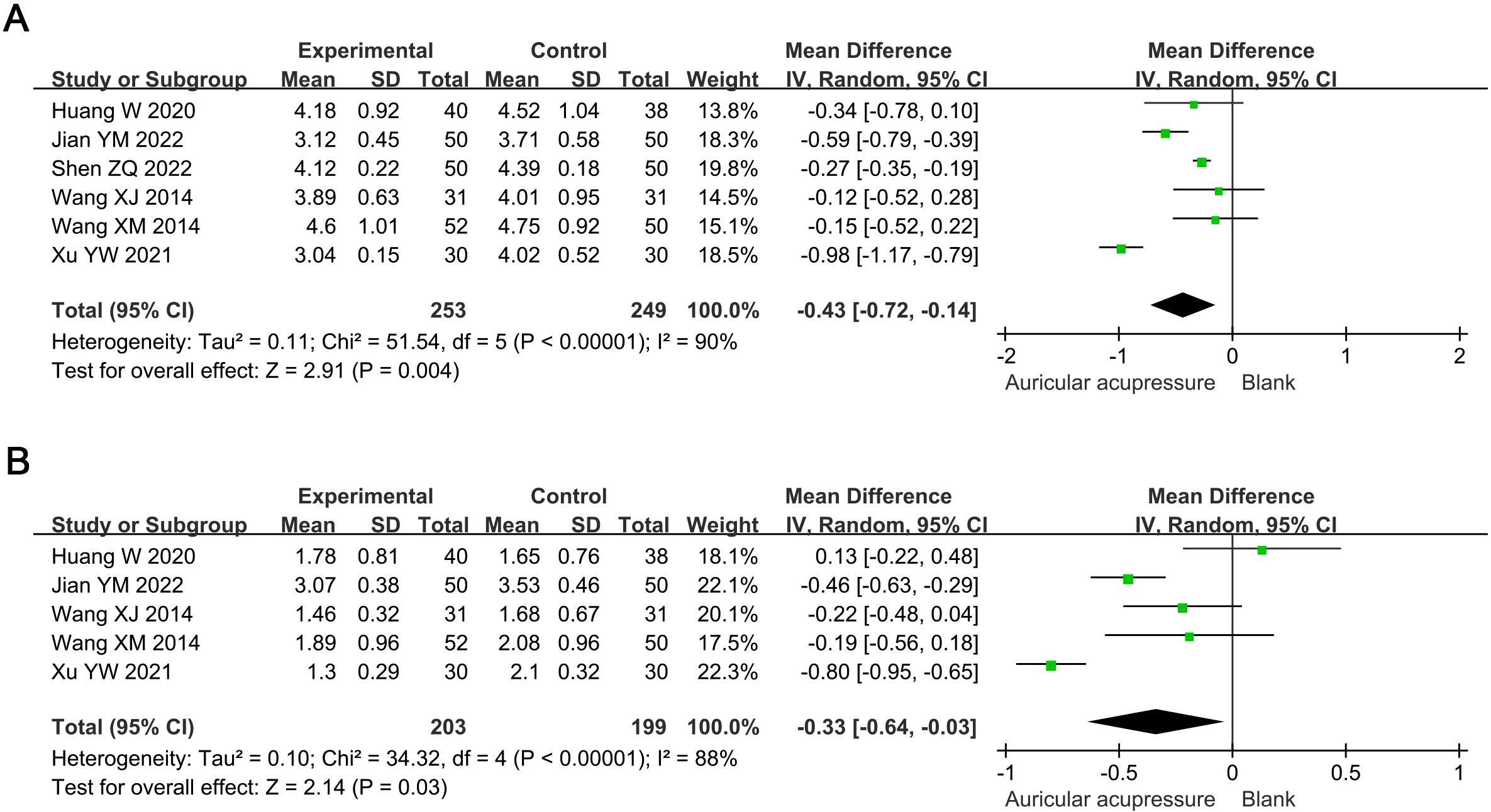
Figure 4. Meta-analysis results of blood lipids in T2D treated with auricular pressure. (A) TC; (B) TG. TC, total cholesterol; TG, triglyceride.
3.4.3 Blood pressure
The combined treatment significantly reduced SBP by 14.75 mmHg (MD: -14.75, 95% CI: -24.46 to -5.05; p = 0.003) and DBP by 10.32 mmHg (MD: -10.32, 95% CI: -20.14 to -0.50; p = 0.04) compared to the conventional treatment group (Figure 5). Sensitivity analysis indicated these results were robust.
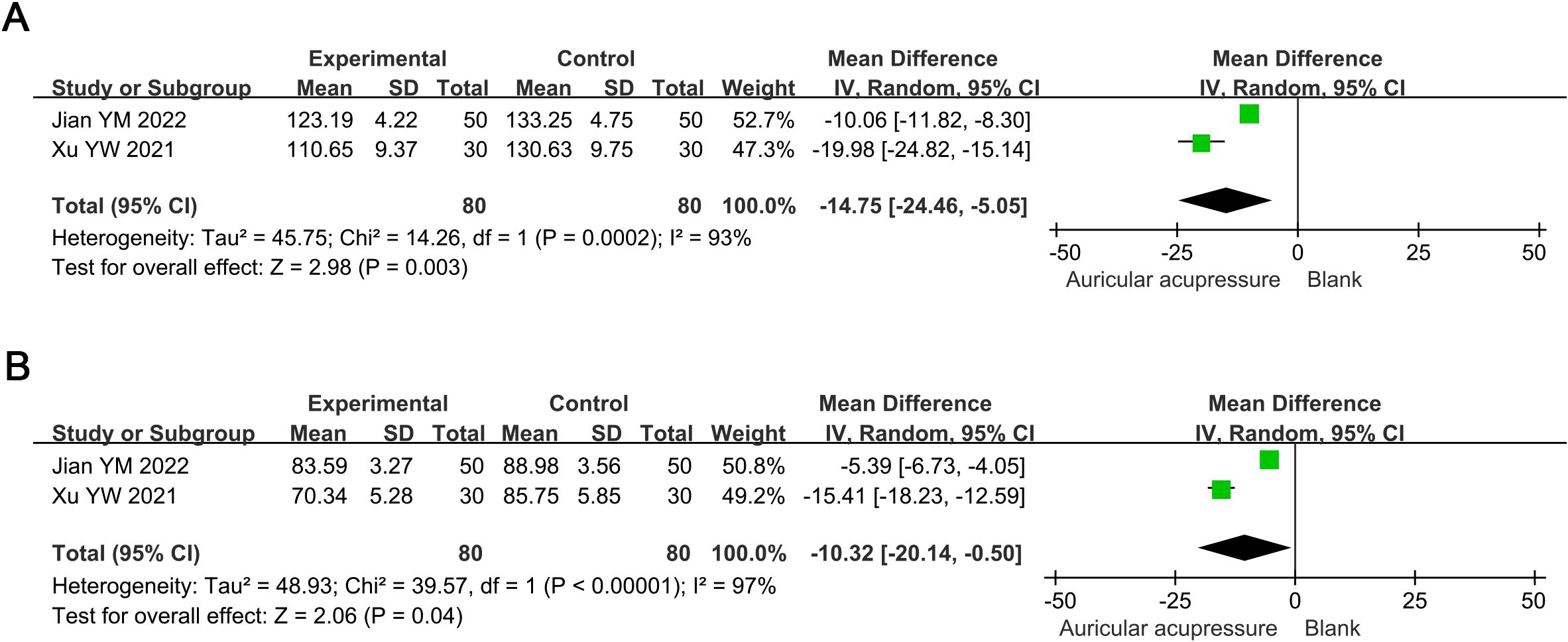
Figure 5. Meta-analysis results of blood pressure in T2D treated with auricular pressure. (A) SBP; (B) DBP. SBP, systolic blood pressure; DBP, diastolic blood pressure.
3.4.4 BMI
The combined treatment significantly decreased BMI by 1.74 kg/m2 (MD: -1.74, 95% CI: -2.61 to -0.87; p < 0.0001) compared with the conventional treatment group (Figure 6). Sensitivity analysis demonstrated the robustness of this result.
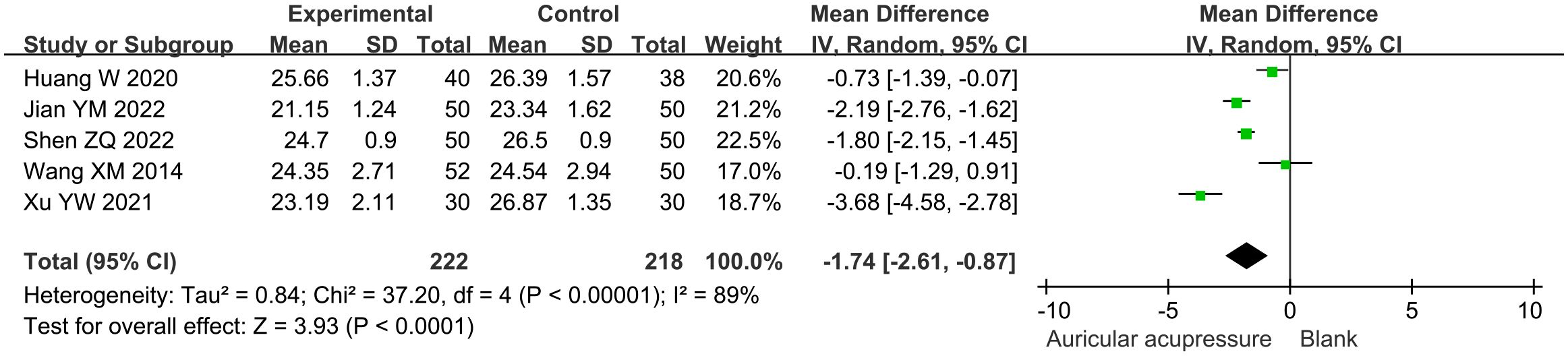
Figure 6. Meta-analysis results of BMI in T2D treated with auricular pressure. BMI, body mass index.
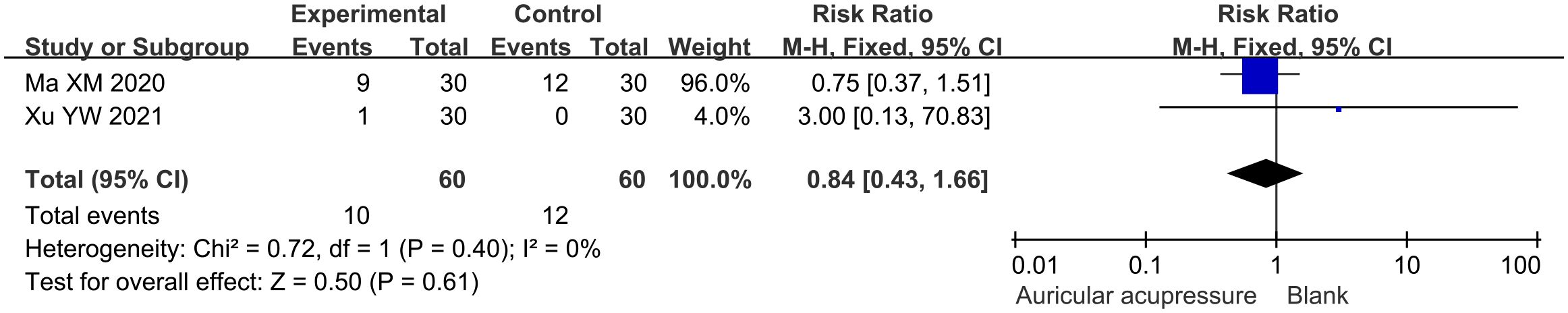
3.5 Safety endpoints
The incidence of adverse events in the combined treatment group was 16.7%, while that in the conventional treatment group was 20.0%. The adverse events in both groups were comparable (RR: 0.84, 95% CI: 0.43 to 1.66; p = 0.61) (Figure 7). Sensitivity analysis confirmed the robustness of this result.
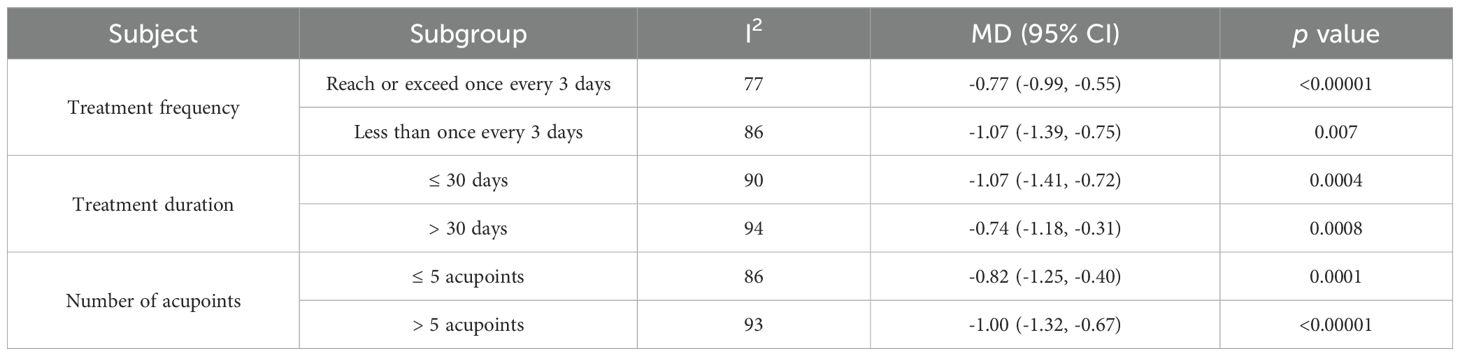
3.6 Subgroup analysis
Subgroup analysis with FBG as the outcome indicator was used to investigate the impact of factors such as treatment frequency, treatment duration, and number of acupoints on the efficacy of auricular pressure treatment for type 2 diabetes. Frequencies of ≤ 3 days (MD: -0.77, 95% CI: -0.99 to -0.55; p < 0.00001) and > 3 days per session (MD: -1.07, 95% CI: -1.39 to -0.75; p = 0.007) significantly reduced FBG. Auricular pressure treatment durations of ≤ 30 (MD: -1.07, 95% CI: -1.41 to -0.72; p = 0.0004) and > 30 days (MD: -0.74, 95% CI: -1.18 to -0.31; p = 0.0008) significantly lowered FBG. Five or less (MD: -0.82, 95% CI: -1.25 to -0.40; p = 0.0001) and > 5 acupoints (MD: -1.00, 95% CI: -1.32 to -0.67; p < 0.00001) of auricular pressure significantly reduced FBG (Table 2).
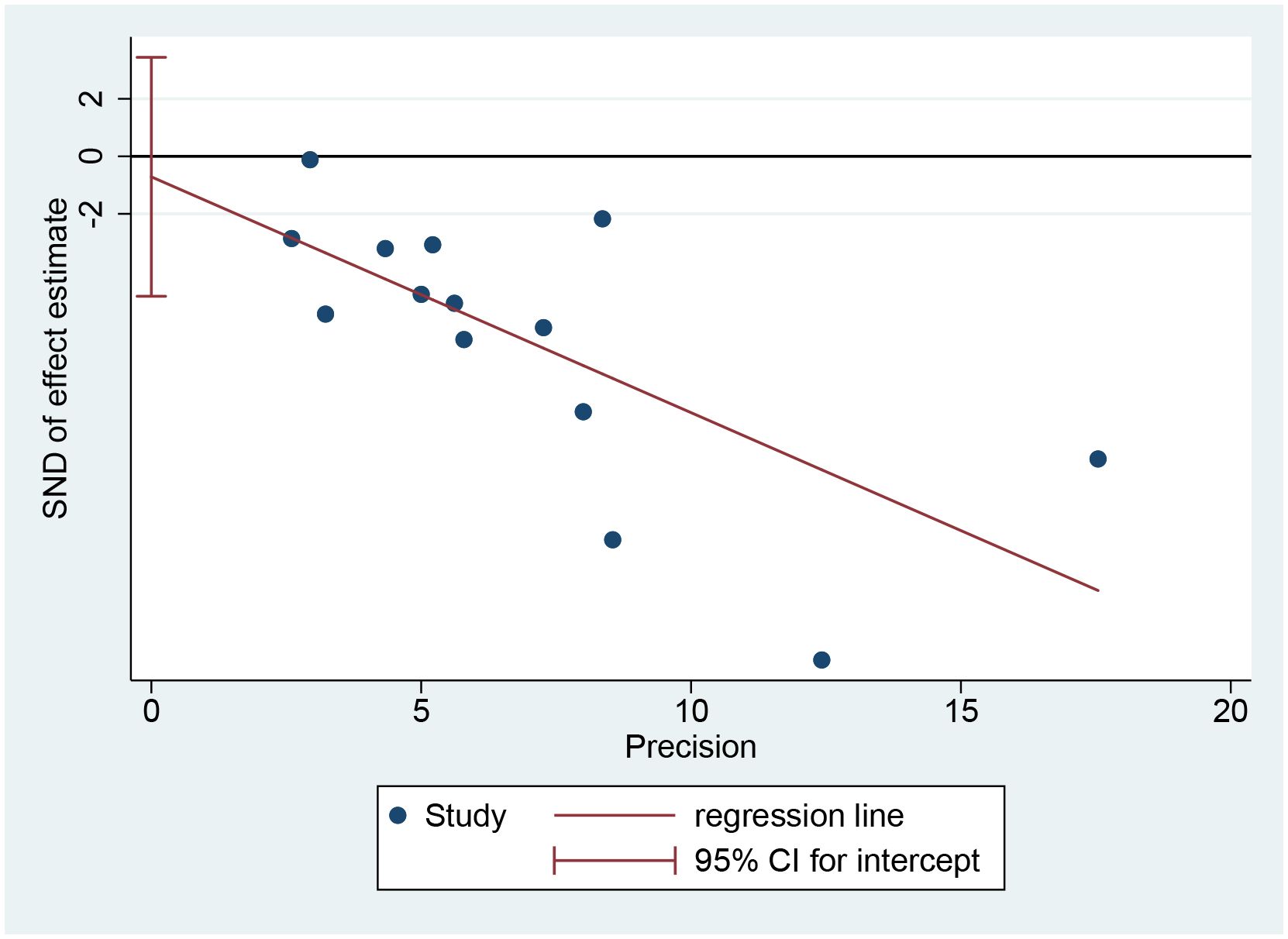
3.7 Publication bias
When FBG level was defined as the primary efficacy endpoint, Egger’s test showed a p-value of 0.715, indicating no significant publication bias (Figure 8).
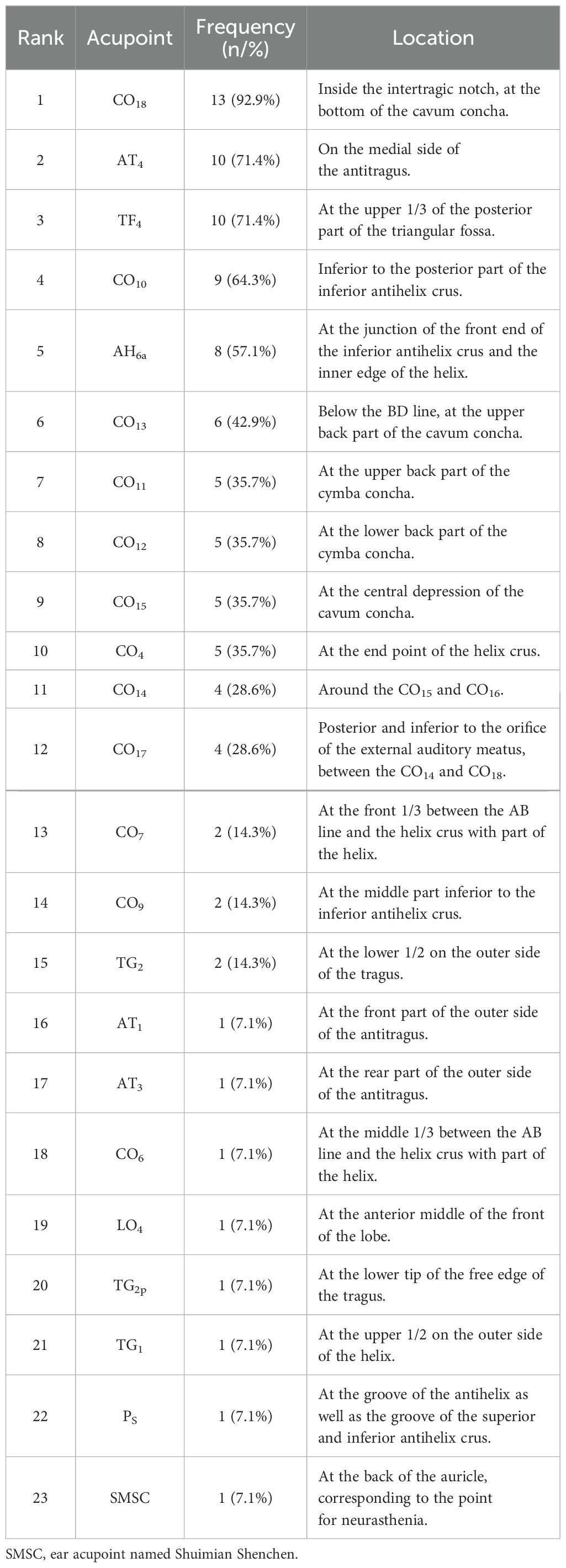
3.8 Frequency analysis
Fourteen auricular pressure protocols were included in the frequency analysis, with a total frequency of 98. The protocol involved 23 auricular acupoints (Table 3). The frequencies of CO18 (92.9%), AT4 (71.4%), TF4 (71.4%), CO10 (64.3%), AH6a (57.1%), CO13 (42.9%), CO11 (35.7%), CO12 (35.7%), CO15 (35.7%), and CO4 (35.7%) were all above 30.0%, making them common acupoints in the treatment of type 2 diabetes using auricular pressure.
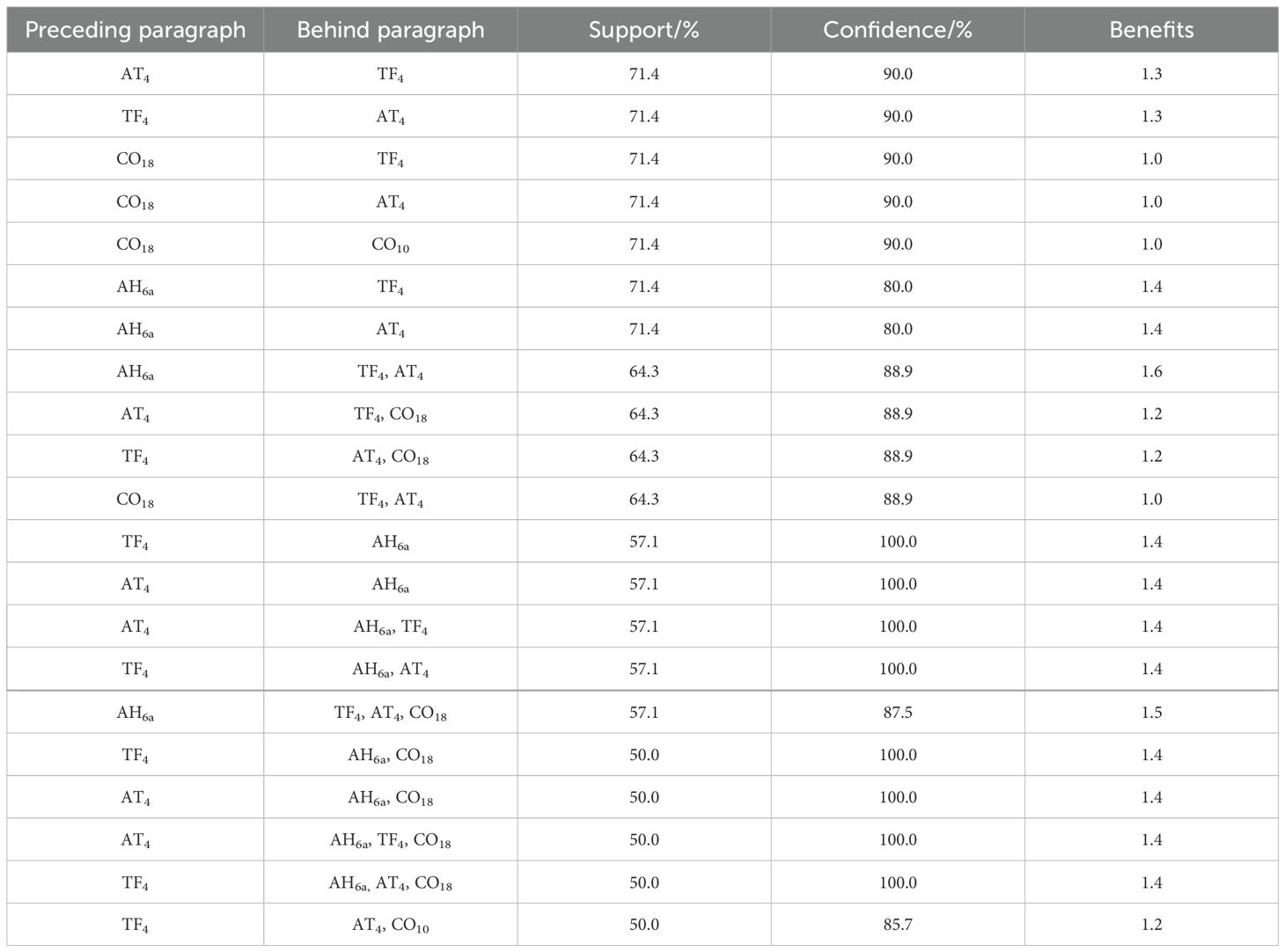
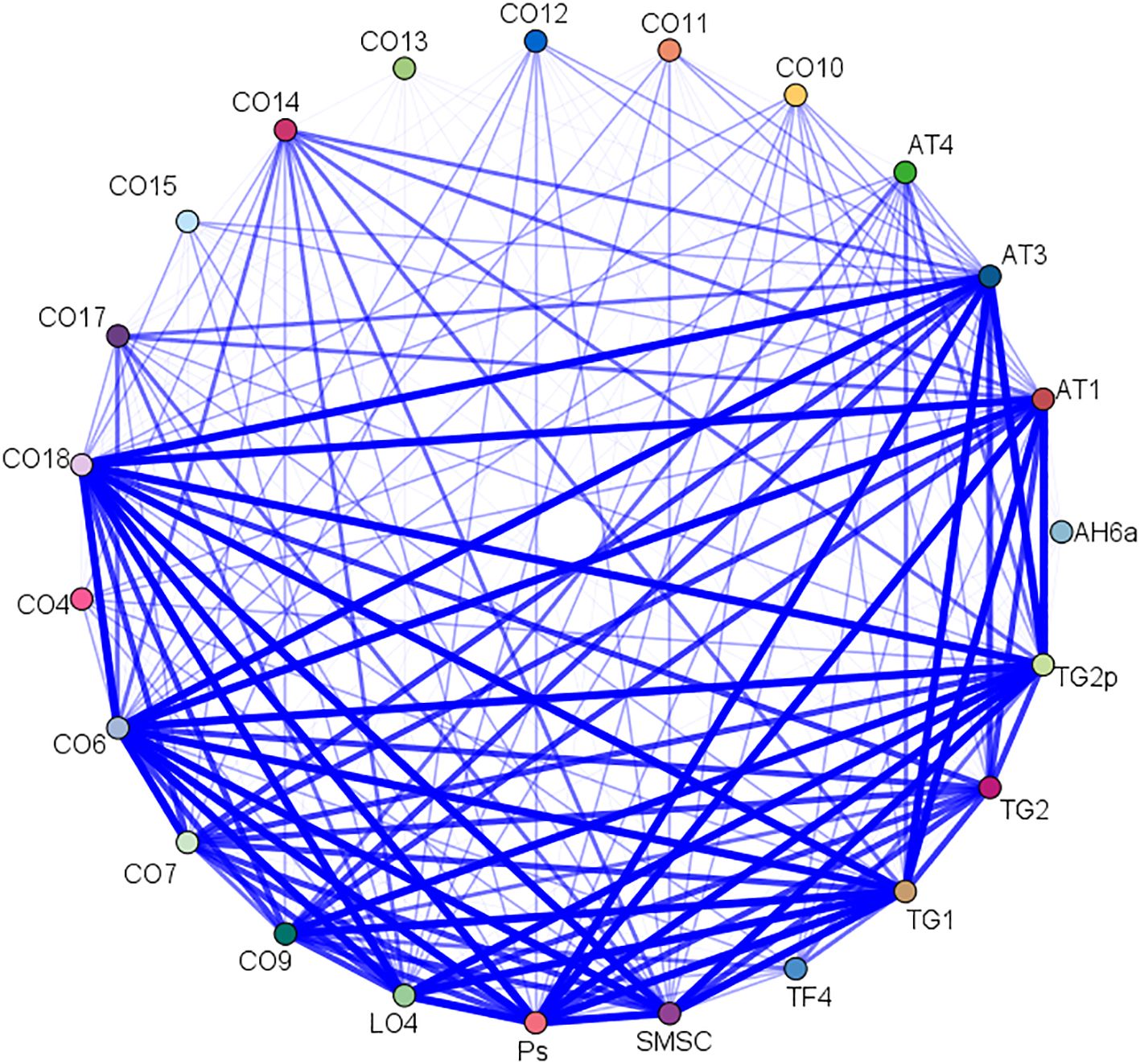
3.9 Association rule analysis
A total of 21 acupoint combinations were obtained through association rule analysis (Table 4). The AT4-TF4 combination had the highest support, confidence, and lift values, while the AH6a-TF4-AT4-CO18 combination had the largest number of acupoints. These core acupoint combinations were composed of acupoints AH6a, TF4, AT4, CO18, and CO10. The network relationships are shown in Figure 9.
4 Discussion
4.1 Background and significance
Auricular pressure is a treatment that applies Wangbuliuxing seeds to the auricle acupoints under the guidance of traditional Chinese medicine theory (32). Owing to its simplicity and high safety, it has been utilized by traditional Chinese medicine practitioners to treat various conditions such as insomnia, pain, and allergic rhinitis (13–15). In 1994, Chen H and colleagues (33) first reported the application of auricular pressure in patients with diabetes in a clinical trial, finding that auricular pressure promoted insulin secretion and lowered blood glucose in patients with diabetes. Since then, many studies have suggested that auricular pressure may be a potential adjunct treatment for type 2 diabetes. However, because of the lack of high-quality evidence, the benefits and risks of auricular pressure use in type 2 diabetes remain uncertain. To the best of our knowledge, this is the first meta-analysis and data mining study examining auricular pressure for type 2 diabetes, aiming to provide evidence-based support for its clinical application.
4.2 Efficacy evaluation
Meta-analysis demonstrated that auricular pressure combined with conventional treatment significantly reduced FBG by 0.93 mmol/L, 2h-PBG by 1.58 mmol/L, and HbA1c by 0.83% compared with conventional treatment alone. FBG is an indicator used to diagnose and monitor diabetes, reflecting the basal insulin secretion function of pancreatic β-cells. 2h-PBG is an important indicator that reflects postprandial insulin secretion and predicts changes in renal function. HbA1c is an important indicator of blood glucose status and cardiovascular risk over the past 90 days. The benefits of auricular pressure on FBG, 2h-PBG, and HbA1c levels indicate that it regulates blood glucose levels and improves prognosis. In addition, Shen et al. (25) found that auricular pressure significantly reduced fasting insulin and C-peptide levels in patients, and Huang et al. (21) reported that auricular pressure significantly reduced the homeostasis model assessment-insulin resistance index (HOMA-IR) in patients. Fasting insulin and HOMA-IR are key indicators for assessing insulin resistance in patients with diabetes, while C-peptide levels reflect the secretory function of pancreatic β-cells. These findings indicate that auricular pressure may reduce blood glucose levels by increasing insulin sensitivity and regulating pancreatic β-cell function.
Meta-analysis indicated that auricular pressure significantly reduced BMI by 1.74 kg/m2 in type 2 diabetes patients. Given that obesity is one of the most important risk factors for type 2 diabetes (34), weight reduction support using auricular pressure may have powerful potential for the treatment of type 2 diabetes. In addition, auricular pressure also significantly reduced TC by 0.43 mmol/L, TG by 0.33 mmol/L, SBP by 14.75 mmHg, and DBP by 10.32 mmHg in patients with type 2 diabetes. Hyperlipidemia and hypertension are well known common risk factors for type 2 diabetes, and controlling blood lipid and blood pressure helps to reduce the risk of type 2 diabetes and delay disease progression (35). The lipid-regulating and blood pressure-lowering effects of auricular pressure may be effective in improving the prognosis of type 2 diabetes. Notably, the sensitivity analysis showed that significant difference in TG between the combined treatment and conventional treatment groups disappeared after removing the studies by Jian et al. (22) and Xu et al. (30). Out of the five included studies, the study by Jian et al. (22) had a significantly higher baseline TG level than the other studies, which may be an important reason for the difference in the results; we did not find obvious methodological or clinical heterogeneity between the study by Xu et al. (30) and the three other included studies. Given the lack of sufficient clinical evidence, we hope that more high-quality clinical trials will be conducted in the future to explore the effects of auricular pressure on blood lipid levels in patients with type 2 diabetes.
In addition to these outcome indicators, the included studies reported other benefits of auricular pressure. Shen et al. (25) found that auricular pressure significantly reduced Hamilton Anxiety Rating Scale and Hamilton Depression Rating Scale scores in patients with type 2 diabetes; these scales are commonly used to assess anxiety and depression. Previous studies have shown that anxiety and depression are common complications in patients with type 2 diabetes and are important factors affecting their quality of life (36). Depression and anxiety are also potential independent risk factors for type 2 diabetes (37, 38). This suggests that auricular pressure reduces the risk of comorbid anxiety and depression as well as the effects of anxiety and depression in patients with type 2 diabetes. In addition, Yang et al. (31) and Zheng et al. (18) found that auricular pressure effectively reduces the Pittsburgh Sleep Quality Index in patients with type 2 diabetes; the Pittsburgh Sleep Quality Index is commonly used to assess sleep quality, with higher scores indicating poorer sleep. Previous studies have shown that sleep disorders are associated with an increased risk of diabetic complications, and treating sleep disorders can help prevent the progression of diabetes (39). This finding implies that auricular pressure may further reduce the risk of complications in patients with type 2 diabetes by improving their sleep quality. Overall, auricular pressure can potentially reduce mood and sleep disorders in addition to lowering blood glucose, blood pressure, and blood lipids, helping to improve the prognosis of type 2 diabetes.
Subgroup analysis showed that auricular pressure treatment frequency of either less than or equal to once every 3 days and more than once every 3 days both significantly reduced FBG levels, suggesting that its hypoglycemic effect was not limited by treatment frequency. Both ≤ and > 30 days of auricular pressure significantly reduced FBG, suggesting that both short-term and long-term treatment have a hypoglycemic effect. Both ≤ and > 5 acupoints significantly reduced FBG, suggesting that the number of acupoints within the normal range did not limit the hypoglycemic effect of auricular pressure. This evidence suggests that the benefits of auricular pressure are not limited by treatment frequency, treatment duration, or the number of acupoints, implying that it has good variability in frequency, duration, and acupoint number that can allow clinicians to flexibly adjust the treatment plan according to the patient’s tolerance level.
4.3 Mechanism analysis
Little literature exists on the mechanisms of auricular pressure in type 2 diabetes. Previous studies have discussed the effects of auricular pressure on increasing insulin sensitivity and promoting insulin secretion. Wang et al. (40) found that auricular pressure directly stimulated the vagus nerve branch of the auricle and adjusted the balance of the autonomic nervous system, promoting insulin sensitivity and secretion. Liu et al. (41) reported that auricular pressure stimulates the thalamic sympathetic-adrenal and vagus insulin pathways by stimulating glucose- and insulin-sensitive neurons of the nucleus tractus solitarius, promoting insulin secretion from pancreatic beta cells.
4.4 Safety evaluation
Our meta-analysis showed that auricular pressure did not increase the incidence of additional adverse events, indicating that it is a relatively safe non-drug treatment. Despite this, clinicians must remain vigilant and prevent potential adverse events such as foreign body sensation, pain, infection, and allergy (42). Certain patients can experience a foreign body sensation, slight pain, or even bleeding when pressing beans on the auricle; this is typically caused by excessive or improper stimulation. Operators must adjust the stimulation intensity and method when performing auricular pressure to ensure patient comfort; when these conditions occur, stopping stimulation immediately will provide relief. Improper disinfection when applying auricular pressure or local skin damage caused by long-term pressure can lead to an infection. Standardized auricle disinfection is key to reducing the occurrence of infections. When an infection occurs, the ear patch should be removed immediately, and the auricle should be disinfected; topical or oral antibacterial drugs should be administered if necessary. Some patients may also experience local redness, swelling, itching, and other symptoms due to allergies to Wangbuliuxing seeds or tape. As this allergic reaction is most commonly caused by tape, replacing the tape with a desensitizing material can help reduce its occurrence. When an allergic reaction occurs, the ear patch should be torn off immediately, and the local skin should be washed with water or saline; antihistamines should be administered if necessary. Given that these potential adverse events are closely related to procedure operation, two suggestions could help to reduce the adverse events caused by operational factors and ensure the safety of auricular pressure; the first is to provide strict and standardized professional training to nursing staff performing auricular pressure measurements, while the second is to provide correct auricular pressure guidance to patients.
Auricular pressure is a form of acupuncture that is safe and reliable. Compared with oral drugs, auricular pressure does not involve hepatic metabolism and renal excretion, reducing the metabolic burden on the liver and kidneys. As a type of acupoint stimulation therapy, auricular pressure exerts a hypoglycemic effect through a neuroendocrine mechanism, which has fewer side effects than oral drugs that act on the whole body (43). In addition, auricular pressure is a relatively noninvasive form of stimulation compared to traditional needling or auricular acupuncture, as it does not involve piercing needles or other tools into the skin (44). A related systematic evaluation noted that the adverse events of auricular pressure were mainly foreign body sensation, pain, and local allergic reactions, and most were mild, short-term, and well-tolerated (42); the incidence of infection was very low.
4.5 Scheme analysis
Data mining revealed that AH6a, TF4, AT4, CO18, and CO10 are the core acupoints for auricular pressure treatment of type 2 diabetes; Auricular Therapy describes their localization and action (45). CO18 has a regulatory role in overall endocrine and immune functions, serving as a pivotal acupoint for rectifying endocrine dysfunction. AT4 is an important acupoint involved in the regulation of endocrine metabolism and digestive functions. CO10 serves as a core acupoint for health preservation, influencing the nervous and endocrine metabolic systems. AH6a regulates autonomic nervous system function and vascular dilation. TF4 plays a role in tranquilizing the mind and regulating cardiovascular function. Together, they form a recommended plan for the treatment of diabetes using auricular pressure. The positioning of the auricular acupoints is shown in Figure 10.
Auricular pressure operations involved localization, disinfection, application of pressure pellets, daily pressure, and replacement of ear patches. The positions of AH6a, TF4, AT4, CO18, and CO10 should first be determined on the basis of an auricular acupoint chart and marked accordingly. Routine disinfection of the surface of acupoints should be performed with complex iodine. Ear patches should be applied to the aforementioned acupoints on one ear using clean tweezers. The patient should then gently press the ear patch with their hand until they experience sensations of soreness, numbness, distension, or warmth at the site; patients should be instructed to press each acupoint for 1 min at a time, 3 times a day. Ear patches should be replaced every 3–7 days; the ear patches should be gently removed, followed by wiping the ear with warm water to avoid allergic reactions caused by the adhesive tape residue.
4.6 Limitations and prospects
This research has some limitations. The included literature did not mention whether blinding of participants and personnel was used, which increases the potential risk of implementation bias. Sensitivity analysis showed that the combined results of TG were not robust, meaning that further verification from similar clinical trials is needed. Due to an insufficient study base, we were also unable to conduct a meta-analysis of effects on insulin, C-peptide, and HOMA-IR; because of this, the impact of auricular pressure on insulin secretion and insulin resistance remains unclear. Since the subjects included in the original studies were all Chinese, this study also may be unable to explain the role of auricular pressure in other ethnicities. Additionally, the auricular pressure scheme recommended in this study was obtained through data mining and required further validation in clinical trials.
In future research, experimental centers in other countries should be established to explore the effects of auricular pressure on patients of different races with type 2 diabetes. Additionally, insulin, C-peptide, and HOMA-IR should be added as outcome indicators to explore the impact of auricular pressure on these indicators in similar clinical trials. Additionally, the auricular pressure scheme recommended in this study should be tested in multicenter clinical trials to verify its efficacy and safety in the treatment of type 2 diabetes.
5 Conclusion
Auricular pressure safely improves blood glucose, lipids, blood pressure, and BMI in patients with type 2 diabetes compared to conventional treatment alone. The auricular pressure protocol developed through data mining that is proposed in this study, consisting of AH6a, TF4, AT4, CO18, and CO10, holds promise as a complementary treatment for type 2 diabetes.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
YFY: Conceptualization, Formal analysis, Methodology, Writing – original draft. QX: Data curation, Writing – original draft. XL: Data curation, Writing – original draft. YMY: Data curation, Writing – original draft. SB: Writing – original draft. RY: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by The Key Support Project of the Regional Innovation and Development Joint Fund of the National Natural Science Foundation of China (U21A20411) and Hunan University of Chinese Medicine Disciplinary Construction' Revealing the List and Appointing Leaders' Project (22JBZ002).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
BMI, Body mass index; CI, Confidence interval; DBP, Diastolic blood pressure; FBG, Fasting blood glucose; HbA1c, Glycated hemoglobin A1c; HOMA-IR, Homeostasis model assessment-insulin resistance index; PRISMA, Preferred Reporting Items for Systematic reviews and Meta-Analyses; MD, Mean difference; RR, Risk ratio; SBP, Systolic blood pressure; TC, Total cholesterol; TG, Triglycerides; 2h-PBG, 2-hour postprandial blood glucose.
References
1. Xourafa G, Korbmacher M, Roden M. Inter-organ crosstalk during development and progression of type 2 diabetes mellitus. Nat Rev Endocrinol. (2024) 20:27–49. doi: 10.1038/s41574-023-00898-1
2. Chow E, Wang K, Lim CKP, Tsoi STF, Fan B, Poon E, et al. Dorzagliatin, a dual-acting glucokinase activator, increases insulin secretion and glucose sensitivity in glucokinase maturity-onset diabetes of the young and recent-onset type 2 diabetes. Diabetes. (2023) 72:299–308. doi: 10.2337/db22-0708
3. Demir S, Nawroth PP, Herzig S, Ekim Üstünel B. Emerging targets in type 2 diabetes and diabetic complications. Adv Sci (Weinh). (2021) 8:e2100275. doi: 10.1002/advs.202100275
4. Banday MZ, Sameer AS, Nissar S. Pathophysiology of diabetes: An overview. Avicenna J Med. (2020) 10:174–88. doi: 10.4103/ajm.ajm_53_20
5. Callaghan BC, Little AA, Feldman EL, Hughes RAC. Enhanced glucose control for preventing and treating diabetic neuropathy. Cochrane Database Syst Rev. (2012) 6:CD007543. doi: 10.1002/14651858.CD007543.pub2
6. Yu Y, Yang X, Tong K, Yin S, Hu G, Zhang F, et al. Efficacy and safety of dorzagliatin for type 2 diabetes mellitus: A meta-analysis and trial sequential analysis. Front Cardiovasc Med. (2022) 9:1041044. doi: 10.3389/fcvm.2022.1041044
7. Anastasi JK, Capili B, Neumaier J, Hackett L. Delivery of acupuncture in clinical trials: Research acupuncturists' perspectives. J Integr Med. (2023) 21:315–9. doi: 10.1016/j.joim.2023.03.007
8. de Sousa TR, Mattos S, Marcon G, Furtado T, Duarte da Silva M. Acupuncture techniques and acupoints used in individuals under chemotherapy or radiotherapy treatment of cancer: A systematic review. J Clin Nurs. (2023) 32:6917–33. doi: 10.1111/jocn.16812
9. Jaladat AM, Alizadeh Vaghasloo M, Atarzadeh F, Ayati MH, Kazemi AH, Akin E, et al. Similarities and differences between kaiy in Persian medicine and moxibustion in Chinese medicine. J Integr Med. (2023) 21:354–60. doi: 10.1016/j.joim.2023.05.002
10. Yu Y, Hu G, Yang X, Yin Y, Tong K, Yu R. A strategic study of acupuncture for diabetic kidney disease based on meta-analysis and data mining. Front Endocrinol (Lausanne). (2024) 15:1273265. doi: 10.3389/fendo.2024.1273265
11. Yu Y, Xu X, Tan D, Yin Y, Yang X, Yu R. A study on the use of acupoint catgut embedding in the treatment of pre-diabetes: a meta-analysis and data mining approach. Front Public Health. (2023) 11:1282720. doi: 10.3389/fpubh.2023.1282720
12. Gholamreza K, Mansoor K, Ismaeel N, Mohammad Reza Shams A, Arman Z, Maryam M, et al. Cupping therapy can improve the quality of life of healthy people in Tehran. J Tradit Chin Med. (2017) 37:558–62. doi: 10.1016/S0254-6272(17)30164-4
13. Lan Y, Wu X, Tan HJ, Wu N, Xing JJ, Wu FS, et al. Auricular acupuncture with seed or pellet attachments for primary insomnia: a systematic review and meta-analysis. BMC Complement Altern Med. (2015) 15:103. doi: 10.1186/s12906-015-0606-7
14. Zhong J, Liu S, Lai D, Lu T, Shen Y, Gong Q, et al. Ear acupressure for allergic rhinitis: A systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. (2021) 2021:6699749. doi: 10.1155/2021/6699749
15. Yang Y, Wen J, Hong J. The effects of auricular therapy for cancer pain: A systematic review and meta-analysis. Evid Based Complement Alternat Med. (2020) 2020:1618767. doi: 10.1155/2020/1618767
16. Hsieh CH. The effects of auricular acupressure on weight loss and serum lipid levels in overweight adolescents. Am J Chin Med. (2010) 38:675–82. doi: 10.1142/S0192415X10008147
17. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
18. Zheng YP, Chen ML. Effect of ear point pressing bean on improving sleep quality and blood glucose control of type 2 diabetes mellitus in communit. World J Sleep Med. (2021) 8:609–11. doi: 10.3969/j.issn.2095-7130.2021.04.023
19. Gao Q, Ji L. Clinical observation on 28 cases of type 2 diabetes treated by ear point embedding beans. Chin J Ethnomedicine Ethnopharmacy. (2014) 23:38–9. doi: 10.3969/j.issn.1007-8517.2014.20.zgmzmjyyzz201420021
20. Hu DX. Effects of auricular plaster therapy applied to control blood sugar of the patients with new-onset type two diabetes mellitus. Western J Tradi Chin Med. (2018) 31:124–6. doi: 10.3969/j.issn.1004-6852.2018.01.037
21. Huang W, Liu X, Zhang WX, Yang TT, Lu H. Clinical efficacy of auricular point sticking and pressing of Wangbuliuxingzi combined with conventional treatment in patients with super severe type 2 diabetes. Chin Tradi Patent Med. (2020) 42:3369–71. doi: 10.3969/j.issn.1001-1528.2020.12.053
22. Jian YM. Effect of diet management combined with ear point pressing beans on type 2 diabetes patients. Advice For Health. (2022) 16:153–5.
23. Luo LQ. To observe the effect of ear point pressing bean therapy and its nursing on blood sugar control in newly diagnosed type 2 diabetes patients. Special Health. (2022) 2022:91–2.
24. Ma XM, Wang XM. Effect of auricular point sticking and pressing method on blood glucose control in hospitalized patients with type 2 diabetes. Shanxi Med J. (2020) 49:2885–7. doi: 10.3969/j.issn.0253-9926.2020.20.069
25. Shen ZQ, Zhao HY. The clinical effect of ear-point embedding beans in type 2 diabetes and sleep disorders patients and its influence on sleep quality. Shanxi Med J. (2022) 51:727–30. doi: 10.3969/j.issn.0253-9926.2022.07.002
26. Wang P. Analysis of the influence of auricular acupoint pressure bean on sleep quality in diabetic patients. Chin Community Doctors. (2020) 36:103–4. doi: 10.3969/j.issn.1007-614x.2020.29.050
27. Wang XJ. Clinical research of Aauricular acupressure treatment of early diabetic nephropathy in type 2 diabetes. Shanxi Univ Chin Med. (2015) 1–25.
28. Wang XM, Ji YJ, Li LW. Metformin combined with auricular plaster therapy for 52 newly diagnosed patients with type 2 diabetes. Chin J Tradi Med Sci Technol. (2014) 21:686–7.
29. Xiao Q. Study on the therapeutic effect of auricular acupoint medication therapy on blood glucose in type 2 diabetes patients. Pract Clin J Integrated Tradi Chin Western Med. (2015) 15:43–4. doi: 10.13638/j.issn.1671-4040.2015.02.026
30. Xu YW, Zhang L, Qiu GQ. Observation on the therapeutic effect of auricular point sticking and pressing on type 2 diabetes with hypertension. Zhejiang J Integrated Tradi Chin Western Med. (2021) 31:634–6. doi: 10.3969/j.issn.1005-4561.2021.07.012
31. Yang YY. Effect of auricular point sticking and pressing on sleep quality and blood sugar in type 2 diabetes patients with insomnia. Med Forum. (2019) 23:771–2. doi: 10.19435/j.1672-1721.2019.06.016
32. Jin X, Ding L, Xia D, Chen P. Effects of acupoint catgut embedding combined with auricular point pressure on menopausal syndrome of liver-kidney deficiency type and estradiol. Chin Acupunct Moxibustion. (2017) 37:836–9. doi: 10.13703/j.0255-2930.2017.08.010
33. Chen H, Wang C, Chang FM, Liu ZY, Song ZH. Study on the effect of wangbuliuxing auricular acupoint sticking and pressing on blood glucose and insulin levels in normal and diabetes subjects. Henan Tradi Chin Med. (2017) 4:223–4.
34. Ottosson F, Smith E, Ericson U, Brunkwall L, Orho-Melander M, Di Somma S, et al. Metabolome-defined obesity and the risk of future type 2 diabetes and mortality. Diabetes Care. (2022) 45:1260–7. doi: 10.2337/dc21-2402
35. LeRoith D. Hyperglycemia, hypertension, and dyslipidemia in type 2 diabetes mellitus: goals for diabetes management. Clin Cornerstone. (2008) 9:S8–S16. doi: 10.1016/S1098-3597(09)60021-1
36. Khan P, Qayyum N, Malik F, Khan T, Khan M, Tahir A. Incidence of anxiety and depression among patients with type 2 diabetes and the predicting factors. Cureus. (2019) 11:e4254. doi: 10.7759/cureus.4254
37. Jin H, Lee S, Won S. Mendelian randomization shows depression increases the risk of type 2 diabetes. Front Genet. (2023) 14:1181851. doi: 10.3389/fgene
38. Jiang L, Atasoy S, Johar H, Herder C, Peters A, Kruse J, et al. Anxiety boosts progression of prediabetes to type 2 diabetes: findings from the prospective Cooperative Health Research in the Region of Augsburg F4 and FF4 studies. Diabetes Med. (2020) 37:1737–41. doi: 10.1111/dme.14232
39. Schipper SBJ, Van Veen MM, Elders PJM, Van Straten A, van der Werf YD, Knutson KL, et al. Sleep disorders in people with type 2 diabetes and associated health outcomes: a review of the literature. Diabetologia. (2021) 64:2367–77. doi: 10.1007/s00125-021-05541-0
40. Wang YL, Pei J. Clinical observation on ear acupoint sticking and pressing intervening glucose metabolism of the patients in prediabetic state. Western J Tradi Chin Med. (2014) 11:4–6,7. doi: 10.3969/j.issn.1004-6852.2014.11.002
41. Liu YJ, Mei PX, Shi GY. Application of continuous intervention of auricular points compression and internet information interviewing in diabetic patients nursing. China Modern Med. (2018) 25:161–3. doi: 10.3969/j.issn.1674-4721.2018.28.049
42. Tan JY, Molassiotis A, Wang T. Suen LK Adverse events of auricular therapy: a systematic review. Evid Based Complement Alternat Med. (2014) 2014:506758. doi: 10.1155/2014/506758
43. Li P, Chen H, Fu X, Zhou H, Lai F. Clinical effects and safety of auricular acupressure as an adjunct therapy on postoperative pain among patients with hip fracture: A meta-analysis. Pain Res Manag. (2023) 2023:5077772. doi: 10.1155/2023/5077772
44. Nielsen A, Gereau S, Tick H. Risks and safety of extended auricular therapy: A review of reviews and case reports of adverse events. Pain Med. (2020) 21:1276–93. doi: 10.1093/pm/pnz379
Keywords: acupoints, auricular pressure, type 2 diabetes, meta-analysis, data mining, integrative medicine, traditional Chinese medicine
Citation: Yu Y, Xiang Q, Liu X, Yin Y, Bai S and Yu R (2024) Auricular pressure as an adjuvant treatment for type 2 diabetes: data mining and meta-analysis. Front. Endocrinol. 15:1424304. doi: 10.3389/fendo.2024.1424304
Received: 27 April 2024; Accepted: 30 July 2024;
Published: 05 September 2024.
Edited by:
Bo Zhu, Harvard Medical School, United StatesReviewed by:
Mohammad Hashem Hashempur, Shiraz University of Medical Sciences, IranPeiming Zhang, Foshan Hospital of Traditional Chinese Medicine, China
Copyright © 2024 Yu, Xiang, Liu, Yin, Bai and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rong Yu, eXVyb25nMTk2OTA1QDE2My5jb20=
 Yunfeng Yu
Yunfeng Yu Qin Xiang1
Qin Xiang1 Siyang Bai
Siyang Bai