- 1Beijing Institute of Occupational Disease Prevention and Control, Beijing, China
- 2School of Public Health, Peking University, Beijing, China
- 3School of Public Health, North China University of Science and Technology, Tangshan, China
- 4School of Public Health and the Beijing Key Laboratory of Environmental Toxicology, Capital Medical University, Beijing, China
Introduction: Long working hours are likely associated with the decreased of kidney function, while physical activity (PA) was linked to improvements in kidney function. However, whether PA can offset the negative impact of long working hours on kidney function was unclear, which is the focus of this study.
Methods: A cross-sectional study was conducted. Three approaches were adopted to distinguish the association between long working hours and regular working hours. Moderate to vigorous physical activity (PA) was assessed by a structured questionnaire. eGFR and chronic kidney disease (CKD) or not were utilized to evaluate the kidney function. Linear and logistic regression analyses were conducted to assess the association between weekly working hours, PA, and kidney function.
Results: A total of 18,431 adults were enrolled in this study, including 9981 males (54.2%) and 8450 females (45.8%). The average eGFR was (99.54 ± 17.55 mL/min/1.73 m2). The people worked more than 40 h/wk (98.89 ± 17.06 mL/min/1.73 m2) had lower eGFR compared to those worked less than 40 h/wk (99.93 ± 17.83 mL/min/1.73 m2) (p < 0.05). Individuals working longer hours exhibited lower eGFR (β = -0.772, 95% CI: -1.241, -0.303, for > 40 h/wk compared to working ≤ 40 h/wk). Engagement in moderate to vigorous PA was associated with higher eGFR values (β = 1.159, 95% CI: 0.699, 1.619) compared to low PA (< 150 minutes/wk), but this association did not reach statistical significance for the prevalence of CKD. Furthermore, PA was insufficient to reverse the decline of eGFR related to prolonged working hours.
Discussion: Prolonged working hours were associated with a decline in eGFR, while PA was found to have a protective effect on kidney function. However, PA alone may not fully mitigate the negative impact of prolonged working hours on renal health. More robust measures to protect renal function should be implemented to mitigate the damage caused by prolonged working hours.
1 Introduction
Extended working hours were on the rise in contemporary society, prompting apprehensions regarding the potential ramifications on diverse facets of health. The mean weekly working time worldwide stood at approximately 43 hours, with approximately 36.1% of workers clocking in more than 48 h/wk in 2014 reported by the International Labour Organization (ILO) (1). Based on population-based surveys and the Sixth European Working Conditions Survey, the prevalence of working 48 or more hours per week was notably high in 2010, with 19% of Americans working such hours (2). In comparison, in 2015, 15% of Europeans reported working similar hours (2). Consistent exposure to prolonged work hours has been consistently associated with an array of safety and health risks, such as cardiovascular diseases, hypertension, depression, and occupational injury (3–5), while renal function stands out as a vital parameter, given its pivotal role in maintaining metabolic (6) balance and waste excretion. Some evidences from Asia showed that long working hours were associated with decreased kidney function and increased prevalence of chronic kidney disease (CKD) (7, 8), while whether this pattern existed in other ethnic groups remains unclear.
Epidemiological studies indicated a global CKD prevalence ranging from 8% to 16%, affecting approximately 850 million individuals globally (9). In 2017, approximately 1.2 million (with a 95% uncertainly interval ranging from 1.2 to 1.3 million) individuals succumbed to CKD worldwide, leading to 35.8 million (with a 95% uncertainly interval ranging from 33.7 to 38.0 million) disability-adjusted life-years (DALYs) (10). Notably, CKD was a major risk factor for cardiovascular diseases, the leading cause of death globally, amplifying its association on public health (10, 11). Given its multifactorial etiology and complex pathophysiology, effective strategies for the prevention and management of CKD required a comprehensive approach, encompassing early detection, risk factor modification, and timely interventions to mitigate disease progression. Understanding the risk factors of CKD was crucial for informing public health policies and strategies aimed at reducing its burden and improving the overall health outcomes of affected individuals globally, while long working hours probably be a potential risk factor for CKD.
Physical activity (PA) played a crucial role in maintaining overall health and preventing various diseases. Numerous studies have consistently demonstrated the beneficial effects of regular PA on reducing the risk of chronic conditions such as depression, cardiovascular disease, diabetes, obesity, and certain cancers (12–15). Regarding CKD, emerging evidence suggested that PA probably be also play a protective role in kidney health (16–19). We therefore considered it necessary to evaluate the relationship of kidney function with long working hours, as well as whether PA has sufficiently protective effect on it, to reveal the adverse effects of long working hours, draw attention to the harms of prolonged work periods, and ultimately reduce working hours. As estimated glomerular filtration rate (eGFR) testing was affordable and widely accessible globally, diminished eGFR may serve as a valuable indicator for predicting kidney disease and its implications (20). The hypothesis of this study is that long working hours are associated with a decline in kidney function, while physical activity is associated with improvements in kidney function, and physical activity may be able to offset this damage. The objective of this study was to explore the correlation between weekly work hours and declining kidney function, as measured by eGFR, and further evaluate the association of PA, among the long working individuals in U.S.
2 Materials and methods
2.1 Participants and study design
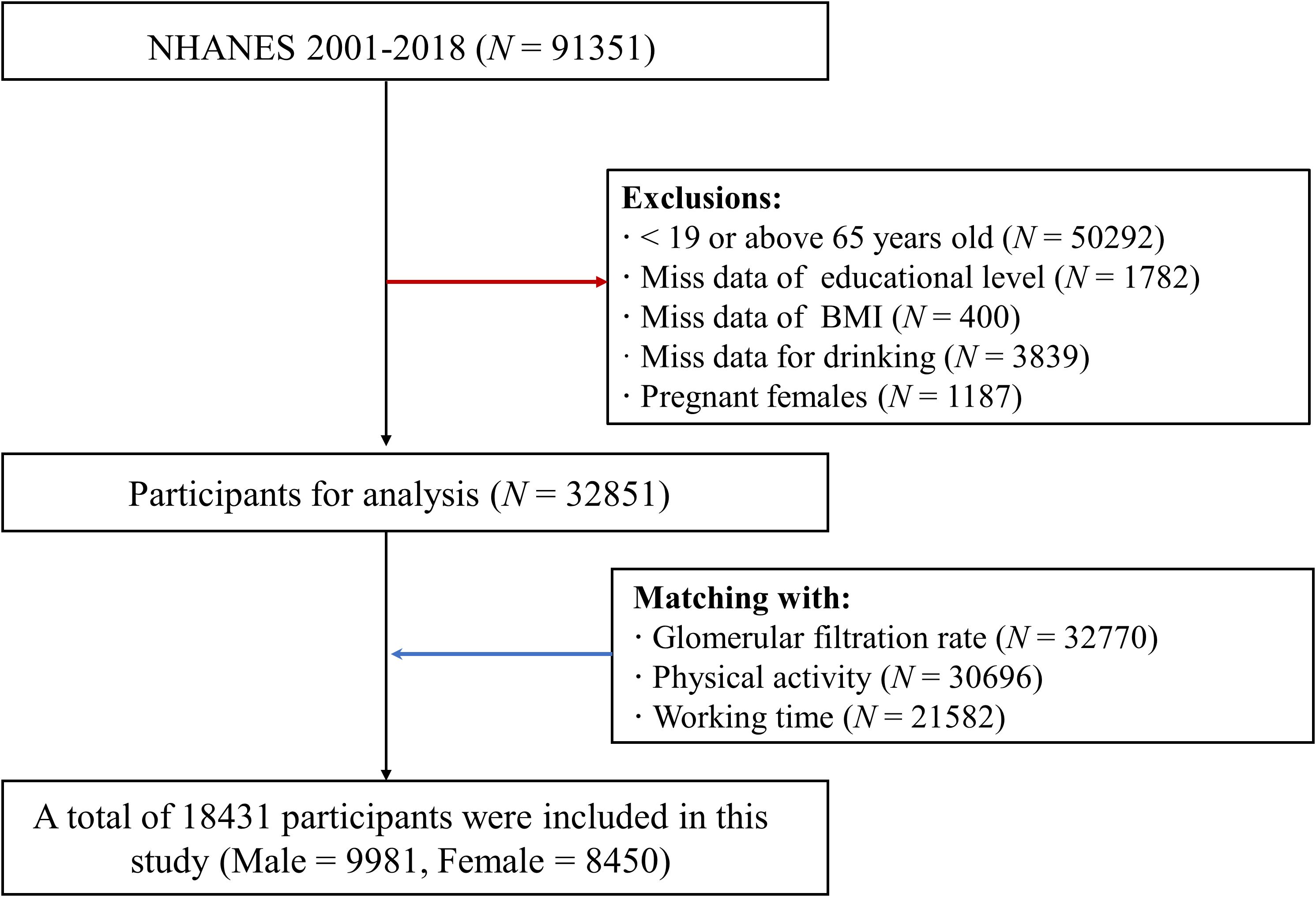
The research leveraged the dataset from the NHANES, a representative cross-sectional study conducted in the U.S. The NHANES study protocol has been approved by the National Center for Health Statistics (NCHS) Institutional Research Ethics Review Board (ERB). In this study, data was utilized in the nine cycle years, including 2001 – 2002, 2003 - 2004, 2005 - 2006, 2007 - 2008, 2009 - 2010, 2011 - 2012, 2013 – 2014, 2015 - 2016, and 2017 - 2018. A total of 91,351 individuals were enrolled in primary. And 50,529 participants were excluded for < 19 or above 65 years old. 1748, 400, and 3839 individuals were excluded for missing data of educational level, BMI, and drinking information, respectively. And 1187 pregnant females were also excluded. Furthermore, based on participants’ code, demographic and sociological information with data on eGFR, PA, and working time was matched. In final, 18,431 individuals were included, consistent of 9981 males (54.2%) and 8450 (45.8%) females (Figure 1).
2.2 Working hours
The assessment of weekly working hours was conducted via a questionnaire, available at https://wwwn.cdc.gov/nchs/nhanes/Default.aspx. All the participants were questioned “How many hours did [you/SP] work last week at all jobs or businesses [OCQ180]”. Due to the inconsistent classification criteria for long working hours among different international organizations, while there was no research to show which is better, three distinct categorizations were employed for weekly working hours in this study (4, 21). Category 1: ≤ 40 h/wk and > 40 h/wk; Weekly working hours category 2: ≤ 48 h/wk and 48 h/wk; Weekly working hours category 3: ≤ 30 h/wk, 31 - 40 h/wk, 41 - 48 h/wk, 49 – 54 h/wk, and ≥ 55 h/wk.
2.3 Kidney function
The blood for all the participants were collected by trained nurses, centrifuged and shipped to – 80 °C environment until test. The Jaffe rate method was used to analyzed serum creatine. Furthermore, according to the indicator of serum creatine, age, sex, and race/ethnicity, the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation was applied for eGFR estimation (22). Additionally, individuals whose eGFR was below 60 mL/min/1.73 m² were classified as cases of CKD (23).
2.4 Physical activity (PA)
Within the NHANES dataset, the moderate to vigorous PA levels in leisure-time were assessed using the following questionnaire items: PADLEVEL (Activity level), PADTIMES (# of times did activity in the past 30 days), which included activity type and time. The moderate intensity to vigorous PA have a set of fixed and clear evaluation methods and were widely accepted by most scholars, including swimming, walking, bicycling et al. (24, 25) PADDURAT (Average duration of activity in minutes). Utilizing this data, the moderate to vigorous PA was computed as PADTIMES (# of times did activity in the past 30 days) × PADDURAT (Average duration of activity in minutes). We defined engagement in moderate to vigorous PA for less than 150 minutes per week in leisure-time as high-risk group, whereas participation in moderate to vigorous PA for 150 minutes or more per week was categorized as low-risk group (24).
2.5 Covariates
The demographic characteristics extracted from the NHANES survey encompassed a range of variables, including sex, age, race/ethnicity (categorized as Mexican American, Other Hispanic, Non-Hispanic White, Non-Hispanic Black, and Other race), body mass index (BMI), smoking habits, alcohol consumption habits, and hypertension. Age was stratified into two groups: 20-45 years and 46-65 years. The race/ethnicity was further subdivided into two group: White or other race and Black groups, as the CKD-EPI equation calculates the eGFR separately based on whether the individual belongs to the Black race (22). BMI was computed as weight (in kilograms) divided by height squared (in meters), and categorized into three levels: < 25, 25 to 30, and ≥ 30 kg/m2. Participants were identified as drinkers if they reported consuming alcohol more than 14 g (women) or 28 g (men). Individuals were defined as smoker if they reported smoking more than 100 cigarettes in their lifetime. In this study, hypertension was defined based on systolic blood pressure, diastolic blood pressure, and physician diagnosis of hypertension. Participants were considered to have hypertension (26) if their (1) systolic blood pressure was greater than 140 mmHg, (2) or if the diastolic blood pressure was greater than 90 mmHg, (3) or if they had received a diagnosis of hypertension from a physician. Meeting any one of these criteria led to classification as hypertensive.
2.6 Statistical analysis
Statistical analyses were conducted using SPSS 26.0 (SPSS Inc., Chicago, USA) for Windows and R software (version 4.0.4; R Core Team). Continuous variables were presented as mean ± standard deviation (SD), while categorical parameters were expressed as n (%). To compare differences of eGFR between different sub-groups participants, Student’s t-test or analysis of variance (ANOVA) were employed for continuous variables, while the chi-square test was utilized for categorical variables. Linear and logistic regression analyses were performed to assess the association of longer working hours with the decreased of eGFR and the risk of CKD, with three categories of working hours serving as the reference category, respectively. To ensure the robustness of the results, three levels of adjustment were applied. Initially, the crude model was analyzed, followed by Model 1, which was adjusted for age, gender, BMI, and race/ethnicity, related with the kidney function previously (27, 28). Model 2 further adjusted for smoking & alcohol habits, and hypertension, which were reported related with kidney function previously (28–30). Statistical significance was defined as α < 0.05 for two-tailed p-values.
3 Results
3.1 The general demographic characteristics of participants
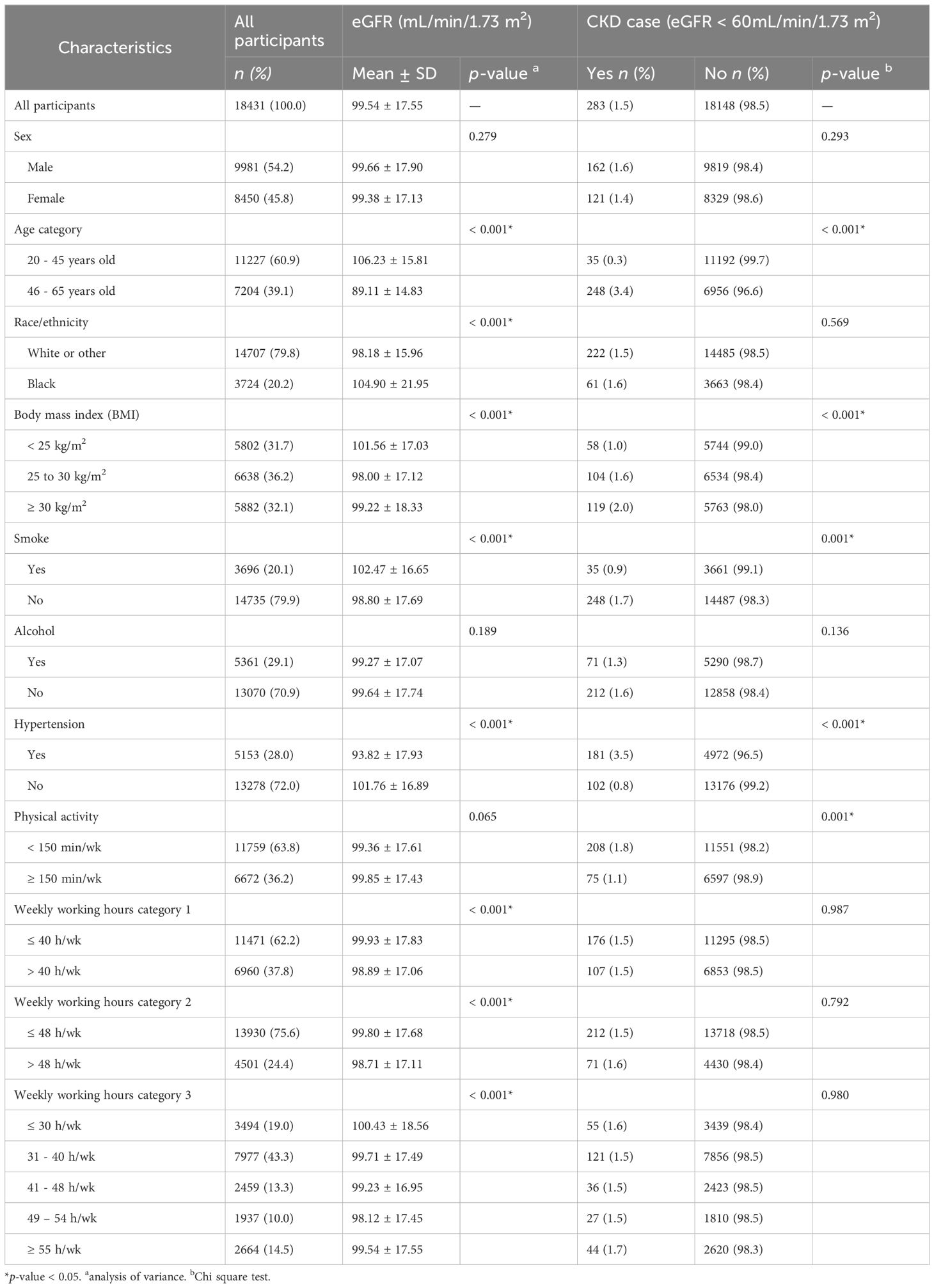
The general demographic characteristics of participants of the 18,431 participants included in the study was outlined in Table 1. The study consisted of 9,981 (54.2%) males and 8,450 (45.8%) females, providing a balanced representation of both sexes. The participants were categorized into two age groups. The majority, comprising 11,227 (60.9%), fell within the 20-45 years age range, while 7,204 (39.1%) were in the 46-65 years age category. There were 14707 (79.8%) white or other race individuals and 3724 (20.2%) included in this study. The BMI categories were delineated as follows: 31.7% (n = 5,802) had a BMI of <no><</no> 25 kg/m2, 36.2% (n = 6,638) fell within the 25 to 30 kg/m2 range, and 32.1% (n = 5,882) had a BMI ≥ 30 kg/m2. Smoking was reported by 3,696 of participants (20.1%), while the majority, 14,735 (79.9%), were non-smokers. Approximately 29.1% of participants (n = 5,361) reported alcohol consumption, with the remaining 70.9% (n = 13,070) abstaining. Hypertension was present in 28.0% of participants (n = 5,153), while 72.0% (n = 13,278) did not exhibit hypertension. A breakdown of physical activity levels revealed that 36.2% (n = 6,672) engaged in more than 150 minutes per week, whereas 63.8% (n = 11,759) participated in physical activity for less than 150 minutes per week. Participants were divided into two categories based on their weekly working hours. In the first category, 62.2% (n = 11,471) worked 40 hours or fewer per week, while 37.8% (n = 6,960) worked more than 40 hours. In the second category, working hours ranged from ≤ 48 h/wk to > 48 h/wk. The third category detailed working hours from ≤ 30 h/wk to ≥ 55 h/wk.
3.2 Kidney function
The kidney function across different groups of the participants were showed in Table 1. For all participants, the mean eGFR was (99.54 ± 17.55) mL/min/1.73 m2. Out of the total, 283 participants (1.5%) were identified as chronic CKD cases with eGFR < 60 mL/min/1.73 m2, while 18,148 participants (98.5%) had an eGFR above this threshold. No significant difference was observed in eGFR between males (99.66 ± 17.90 mL/min/1.73 m2 and females (99.38 ± 17.13 mL/min/1.73 m²). The prevalence of CKD cases among males and females was 1.6% and 1.4%, respectively. A substantial age-related variation in mean eGFR was found (p < 0.05). Participants aged 20-45 years had a higher mean eGFR (106.23 ± 15.81 mL/min/1.73 m²) and a lower CKD prevalence (0.3%) compared to those aged 46-65 years (eGFR 89.11 ± 14.83 mL/min/1.73 m2; CKD prevalence 3.4%). The eGFR of black man (104.90 ± 21.95 mL/min/1.73 m²) was higher than that of white or other race individuals (98.18 ± 15.96 mL/min/1.73 m²) (p < 0.05), while the CKD prevalence was without significance between the two ethnic groups. BMI categories exhibited a significant association on both mean eGFR (p < 0.05) and CKD prevalence. Lower mean eGFR and higher CKD prevalence were associated with higher BMI categories. Participants who smoked demonstrated a significantly higher mean eGFR (102.47 ± 16.65 mL/min/1.73 m2) and a lower CKD prevalence (0.9%) compared to non-smokers. No significant differences were observed in mean eGFR or CKD prevalence between participants who consumed alcohol and those who did not. Participants with hypertension had a lower mean eGFR (93.82 ± 17.93 mL/min/1.73 m²) and a higher CKD prevalence (3.5%) compared to those without hypertension. Higher physical activity levels were associated with a lower CKD prevalence, although the mean eGFR difference was not statistically significant. The results showed that the eGFR was (98.87 ± 17.06 mL/min/1.73 m2) in low PA group and (98.94 ± 17.03 mL/min/1.73 m2) in high PA group, which showed that in the context of long working hours, increased physical activity did not improve kidney function.
3.3 Associations of kidney function and long working hours
Weekly working hours significantly influenced kidney function. Individuals with longer working hours showed lower eGFR, although the CKD prevalence was not statistically significant (Table 1). The linear regression was performed in three levels models, which all indicated that individuals working longer hours tend to exhibit lower eGFR, after adjust three series of confounder factors (Table 2). After adjust variables of sex, age, race/ethnicity, BMI category, smoking and alcohol habits, and hypertension, working hours > 40 h/wk was negatively associated with decreased eGFR compared to those ≤ 40 h/wk [β = -0.772, 95% CI (-1.241, -0.303)]. Weekly working hours > 48 h/wk was negatively associated with decreased eGFR compared to those ≤ 48 h/wk [β = -0.838 (-1.365, -0.310)]. And the regression analysis of categorized working hours into five groups, further indicated a significant association between longer working hours and a decrease in eGFR (p trend < 0.05). The estimated associations of CKD across different working hour categories were further analyzed using three levels multiple logistic regression analysis (Supplementary Table 1). No significant difference was found in all the analysis.
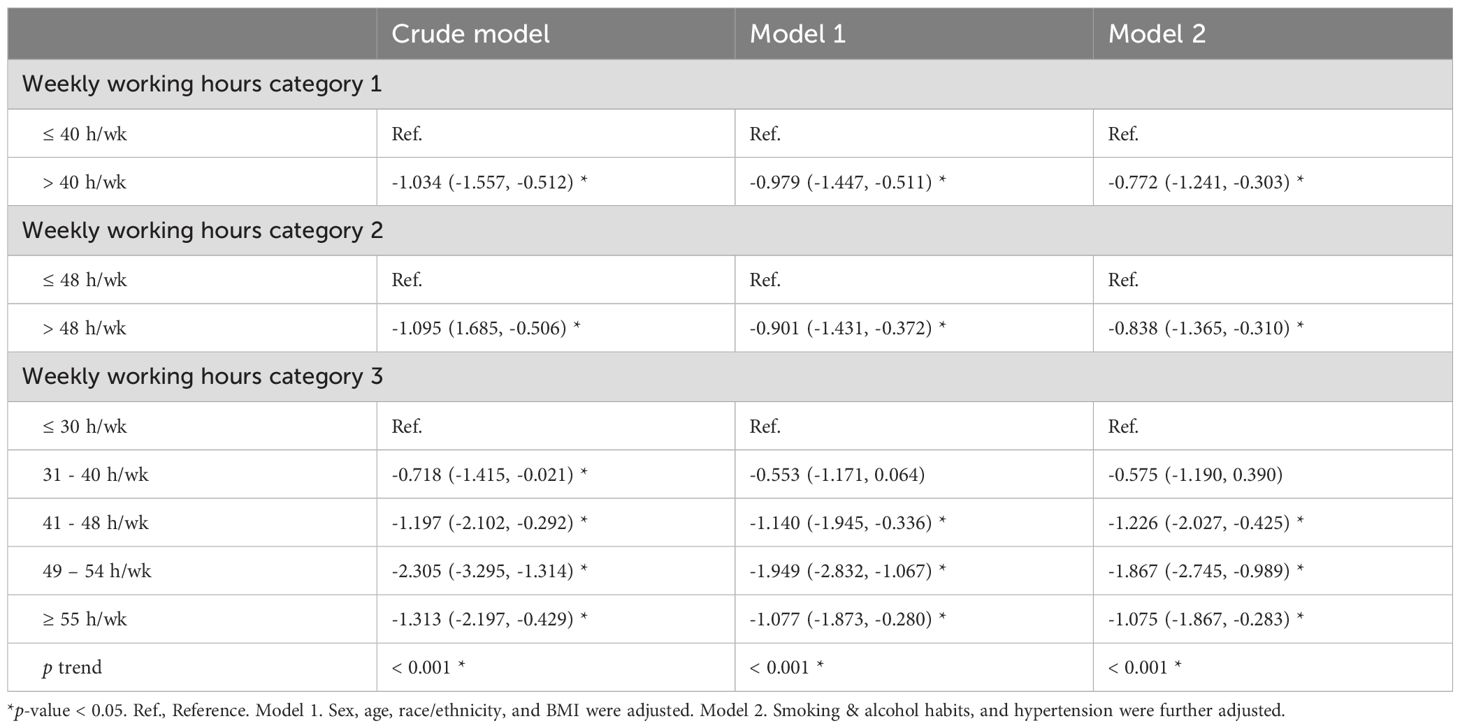
Table 2. Estimated association of eGFR across long working hours performed by linear regression (β, 95% CI).
3.4 Associations of kidney function and physical activity
The association of kidney function and PA was tested by linear regression analyses were showed in Table 3. Individuals who engaged in 150 minutes or more of PA per week showed a higher eGFR values (β = 1.159, 95% CI: 0.699, 1.619). However, this association did not reach statistical significance for the prevalence of CKD (OR = 0.820, 95% CI: 0.625, 1.076) (Supplementary Table 1).
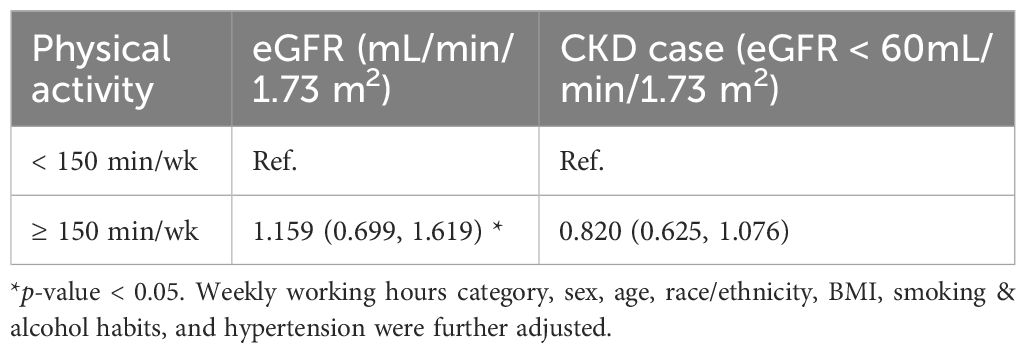
Table 3. Estimated association of eGFR and CKD across physical activity performed by linear regression (β, 95% CI).
3.5 Modification of PA on kidney function and working hours
The estimated associations of eGFR across different weekly working hours categories were analyzed in relation to PA time (Table 4). Adjustment for sex, age, race/ethnicity, BMI, smoking and alcohol habits, and hypertension, the results indicated that the decreased eGFR was more with individuals weekly working hours > 40 h/wk than those weekly working hours ≤ 40 h/wk. And the decreased of eGFR [β = -0.874, 95% CI: (-1.460, -0.288)] was less in the group of < 150 min/wk than those of ≥ 150 min/wk [β = -1.020, 95% CI: (-1.799, -0.242)]. The decreased eGFR was more with individuals weekly working hours > 48 h/wk than those weekly working hours ≤ 48 h/wk. And the decreased of eGFR [β = -0.813, 95% CI: (-1.471, -0.154)] was less in the group of < 150 min/wk than those of ≥ 150 min/wk [β = -0.911, 95% CI: (-1.790, -0.032)]. There were significant found in the other working hour category of eGFR. The estimated associations of CKD across different working hour categories and PA time were further analyzed using logistic regression analysis (Supplementary Table 2). No significant difference was found in all the analysis.
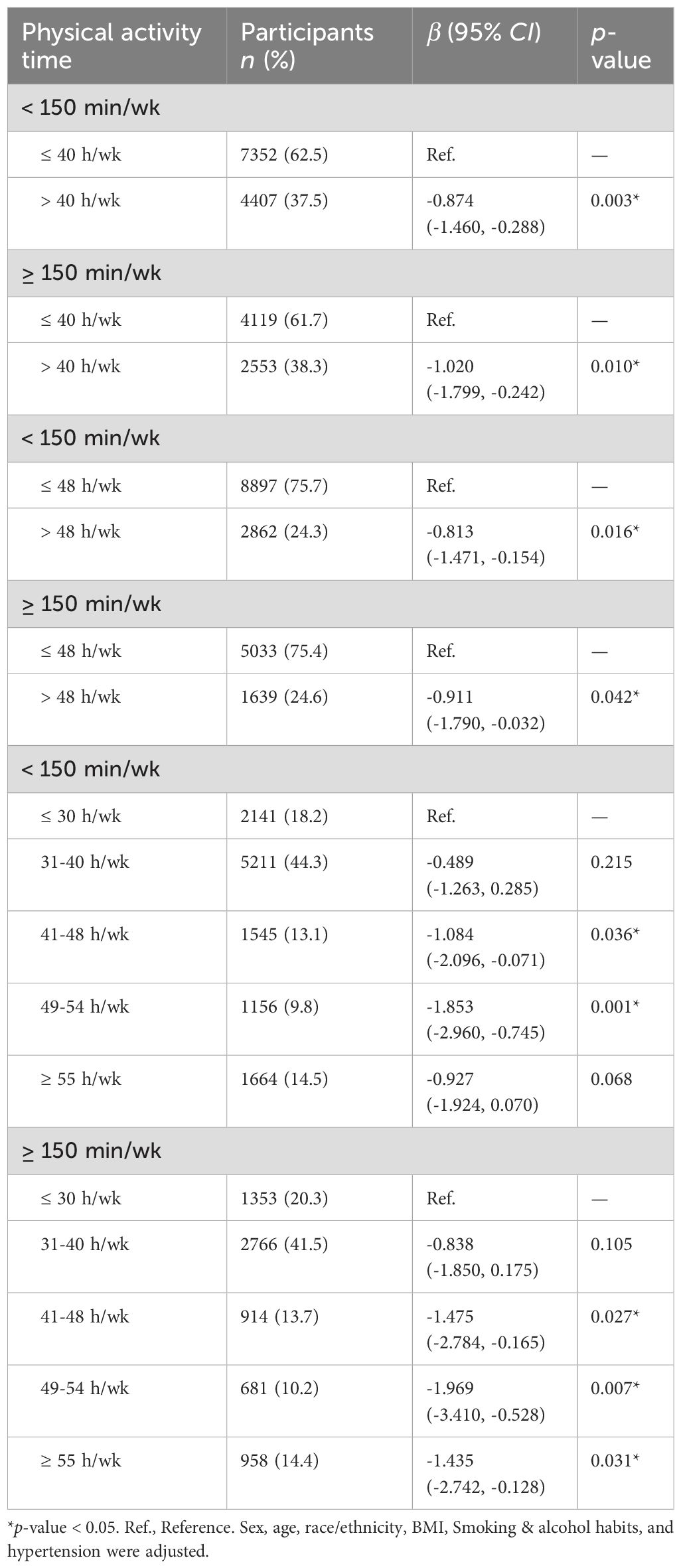
Table 4. Estimated association of eGFR across different weekly working hours category by physical activity time (β, 95% CI).
4 Discussion
This study provided insights into the complex interplay between PA, prolonged working hours, and kidney function among a large sample of participants. We observed that long working hours was associated with decreased kidney function, while PA levels, demonstrated a potential positive association with eGFR. However, when combined with long working hours, PA seems not to offset the adverse association on kidney function.
This study revealed a negative association between prolonged working hours and eGFR among U.S. adults for the first time. These findings were consistent with previous studies suggesting that extended working hours may influence kidney function among other regions. For every additional hour worked per week, there was a corresponding decrease of 0.057 mL/min/1.73 m2 in eGFR among individuals who worked more than 52 hours per week in the Korean population (7). The mechanism behind this association remains unclear, but sporadic studies suggested that the elevation of serum uric acid induced by stress from prolonged working hours probably be linked to the decreased of kidney function (31).
A wealth of evidence has reported that individuals who engaged in regular leisure-time PA have a lower risk of CKD compared to those who did not or engage in minimal PA (16–19). Moreover, enhancing PA has been shown to enhance symptom management, aerobic capacity, muscular strength, physical performance, cardiovascular health, and quality of life (17). In addition, evidences showed that occupational PA were found to increase the risk of poor self-rated health, while leisure-time PA was reverse (32). Furthermore, “weekend warrior” and other leisure-time PA were found both sufficient to reduce all-cause, CVD, and cancer mortality risk (33). The evidences supported the positive value of leisure-time PA. Given the prevalence of kidney inflammation in renal injury (34), leading to fibrosis and irreversible loss of function (35). The mechanism behind exercise’s potent anti-inflammatory effect involved the reduction of visceral fat, leading to decreased secretion of pro-inflammatory adipokines (36), and increased levels of anti-inflammatory cytokines, such as interleukin-6 (IL-6) released from contracting skeletal muscle (36). Elevated IL-6 levels have been shown to slow the increase in tumor necrosis factor-alpha (TNF-a) levels following exposure to an inflammatory stimulus (37). The exercise-induced elevation in IL-6 levels and simultaneous reduction in TNF-a levels suggest the potential therapeutic role of exercise in managing low-grade inflammation, which can exacerbate CKD. To the best of our knowledge, this is the first study to report the complex interplay between prolonged working hours, PA, and eGFR.
There were several inherent limitations in the design of this study. Firstly, its cross-sectional nature precludes the establishment of a causal relationship between exposure and health outcomes. It is plausible that individuals with pre-existing kidney issues may reduce their work hours to alleviate symptoms, potentially leading to an underestimation of the actual risk. Additionally, participants with lower kidney function may reduce working hours, leading to reverse causality. Thus, to ascertain causality, further investigation is warranted through longitudinal studies. Secondly, despite efforts to control for confounding variables, we cannot exclude the influence of other factors such as family history of kidney disease, meat consumption of analgesic medications, job-related stress, and occupation, which could impact the relationship between work hours and kidney function. For example, occupations with manual labor, especially those in high temperature environment, were more likely to develop CKD (38, 39). Higher processed meat consumption was associated with lower kidney function (40). Thirdly, our reliance on a single eGFR measurement introduces the possibility of misclassification of kidney function. According to the CKD definition, abnormalities in kidney structure or function should persist for at least 3 months. However, since our data were collected at a single time point, it was unable to confirm CKD cases according to this definition, potentially leading to the inclusion of patients with acute kidney injury. Forth, evaluating PA through questionnaire was not accurate enough. Additionally, the occupational PA was not collected in the NHANES data bank, resulted that the assessment of physical activity intensity exposure was incomplete. Additionally, varying impacts of different types and intensities of PA was not considered in the analyses. It would be more accurate to collect information through wearing an electronic bracelet.
Despite these limitations, the study possesses several strengths. Firstly, it is the first of its kind to investigate the relationship of kidney function with work hours and physical activity. Secondly, this study considered three criteria for prolonged working hours, yet the results remained robust. This underscores the urgency of addressing health concerns related to long working hours.
5 Conclusion
Overall, our findings underscore the importance of considering both PA levels and working hours in strategies aimed at preserving kidney function and preventing CKD. Encouraging individuals to engage in regular PA can promote overall health but not help offset the negative association of prolonged working hours on kidney function. This study can have implications for clinical and policy – oriented perspectives. This study may have implications for both clinical practice and policy development of labor. Future longitudinal studies are warranted to further elucidate the causal relationships of kidney function PA and working hours, as well as to identify potential mechanisms underlying these associations.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by The U.S. National Center for Health Statistics (NCHS) Institutional Research Ethics Review Board (ERB). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
TY: Conceptualization, Funding acquisition, Software, Supervision, Writing – original draft, Writing – review & editing. SN: Data curation, Formal analysis, Methodology, Visualization, Conceptualization, Software, Writing – review & editing. XL: Conceptualization, Writing – original draft. BZ: Investigation, Writing – original draft. XS: Software, Writing – original draft. BH: Validation, Writing – original draft. XD: Resources, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Capital’s Funds for Health Improvement and Research (CFH), China (2024-4G-3105).
Acknowledgments
A special thanks to all of participants freely giving their time to make this and other possible studies. We also grateful to all those who helped us in our research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2024.1415713/full#supplementary-material
References
1. Descatha A, Sembajwe G, Baer M, Boccuni F, Di Tecco C, Duret C, et al. WHO/ILO work-related burden of disease and injury: Protocol for systematic reviews of exposure to long working hours and of the effect of exposure to long working hours on stroke. Environ Int. (2018) 119:366–78. doi: 10.1016/j.envint.2018.06.016
2. Alterman T, Luckhaupt SE, Dahlhamer JM, Ward BW, Calvert GM. Prevalence rates of work organization characteristics among workers in the U.S.: data from the 2010 National Health Interview Survey. Am J Ind Med. (2013) 56:647–59. doi: 10.1002/ajim.22108
3. Ishikawa M. Long working hours,depression and suicidality among OB/GYNs in Japan. Occup Med (Lond). (2022) 72:200–6. doi: 10.1093/occmed/kqab191
4. Yan T, Ding X, Xie T, Lan T, Niu D, Li J, et al. Physical activity (PA) influences the risk of depression associated with long working hours. J Affect Disord. (2023) 321:227–33. doi: 10.1016/j.jad.2022.10.043
5. Trudel X, Brisson C, Gilbert-Ouimet M, Vézina M, Talbot D, Milot A. Long working hours and the prevalence of masked and sustained hypertension. Hypertension. (2020) 75:532–8. doi: 10.1161/HYPERTENSIONAHA.119.12926
6. Sarwar N, Gao P, Seshasai SRK, Gobin R, Kaptoge S, Di Angelantonio E, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet (London England). (2010) 375:2215–22. doi: 10.1016/S0140-6736(10)60484-9
7. Lee D-W, Lee J, Kim H-R, Jun KY, Kang M-Y. Long work hours and decreased glomerular filtration rate in the Korean working population. Occup Environ Med. (2020) 77:699–705. doi: 10.1136/oemed-2020-106428
8. Lee Y, Seo E, Mun E, Lee W. A longitudinal study of working hours and chronic kidney disease in healthy workers: The Kangbuk Samsung Health Study. J Occup Health. (2021) 63:e12266. doi: 10.1002/1348-9585.12266
9. Jha V, Garcia-Garcia G, Iseki K, Li Z, Naicker S, Plattner B, et al. Chronic kidney disease: global dimension and perspectives. Lancet (London England). (2013) 382:260–72. doi: 10.1016/S0140-6736(13)60687-X
10. GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease,1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2020) 395:709–33. doi: 10.1016/S0140-6736(20)30045-3
11. Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation. (2003) 108:2154–69. doi: 10.1161/01.CIR.0000095676.90936.80
12. Colberg SR, Albright AL, Blissmer BJ, Braun B, Chasan-Taber L, Fernhall B, et al. Exercise and type 2 diabetes: American College of Sports Medicine and the American Diabetes Association: joint position statement. Exercise Type 2 Diabetes Med Sci Sports Exerc. (2010) 42:2282–303. doi: 10.1249/MSS.0b013e3181eeb61c
13. Lee D, Artero EG, Sui X, Blair SN. Mortality trends in the general population: the importance of cardiorespiratory fitness. J Psychopharmacol. (2010) 24:27–35. doi: 10.1177/1359786810382057
14. Rebar AL, Stanton R, Geard D, Short C, Duncan MJ, Vandelanotte C. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol Rev. (2015) 9:366–78. doi: 10.1080/17437199.2015.1022901
15. Moore SC, Lee I-M, Weiderpass E, Campbell PT, Sampson JN, Kitahara CM, et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern Med. (2016) 176:816–25. doi: 10.1001/jamainternmed.2016.1548
16. Uchiyama K, Adachi K, Muraoka K, Nakayama T, Oshida T, Yasuda M, et al. Home-based aerobic exercise and resistance training for severe chronic kidney disease: a randomized controlled trial. J Cachexia Sarcopenia Muscle. (2021) 12:1789–802. doi: 10.1002/jcsm.12775
17. Chu NM, Hong J, Harasemiw O, Chen X, Fowler KJ, Dasgupta I, et al. Chronic kidney disease, physical activity and cognitive function in older adults-results from the National Health and Nutrition Examination Survey (2011-2014). Nephrol Dial Transplant. (2022) 37:2180–9. doi: 10.1093/ndt/gfab338
18. Seidu S, Abdool M, Almaqhawi A, Wilkinson TJ, Kunutsor SK, Khunti K, et al. Physical activity and risk of chronic kidney disease: systematic review and meta-analysis of 12 cohort studies involving 1,281,727 participants. Eur J Epidemiol. (2023) 38:267–80. doi: 10.1007/s10654-022-00961-7
19. Noce A, Tranchita E, Marrone G, Grazioli E, Di Lauro M, Murri A, et al. The possible role of physical activity in the modulation of gut microbiota in chronic kidney disease and its impact on cardiovascular risk: a narrative review. Eur Rev Med Pharmacol Sci. (2023) 27:3733–46. doi: 10.26355/eurrev_202304_32172
20. James MT, Hemmelgarn BR, Wiebe N, Pannu N, Manns BJ, Klarenbach SW, et al. Glomerular filtration rate, proteinuria, and the incidence and consequences of acute kidney injury: a cohort study. Lancet (London England). (2010) 376:2096–103. doi: 10.1016/S0140-6736(10)61271-8
21. Descatha A, Sembajwe G, Pega F, Ujita Y, Baer M, Boccuni F, et al. The effect of exposure to long working hours on stroke: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ Int. (2020) 142:105746. doi: 10.1016/j.envint.2020.105746
22. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. (2009) 150:604–12. doi: 10.7326/0003-4819-150-9-200905050-00006
23. Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. (2003) 139:137–47. doi: 10.7326/0003-4819-139-2-200307150-00013
24. Khurshid S, Al-Alusi MA, Churchill TW, Guseh JS, Ellinor PT. Accelerometer-derived “Weekend warrior” Physical activity and incident cardiovascular disease. JAMA. (2023) 330:247–52. doi: 10.1001/jama.2023.10875
25. Chen F, Du M, Blumberg JB, Ho Chui KK, Ruan M, Rogers G, et al. Association among dietary supplement use, nutrient intake, and mortality among U.S. Adults: A cohort study. Ann Intern Med. (2019) 170:604–13. doi: 10.7326/M18-2478
26. Piper MA, Evans CV, Burda BU, Margolis KL, O’Connor E, Whitlock EP. Diagnostic and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. (2015) 162:192–204. doi: 10.7326/M14-1539
27. Sink KM, Divers J, Whitlow CT, Palmer ND, Smith SC, Xu J, et al. Cerebral structural changes in diabetic kidney disease: African American-Diabetes Heart Study MIND. Diabetes Care. (2015) 38:206–12. doi: 10.2337/dc14-1231
28. Wang L, Xu X, Zhang M, Hu C, Zhang X, Li C, et al. Prevalence of chronic kidney disease in China: results from the sixth China chronic disease and risk factor surveillance. JAMA Intern Med. (2023) 183:298–310. doi: 10.1001/jamainternmed.2022.6817
29. Burnier M, Damianaki A. Hypertension as cardiovascular risk factor in chronic kidney disease. Circ Res. (2023) 132:1050–63. doi: 10.1161/CIRCRESAHA.122.321762
30. Hall ME, Wang W, Okhomina V, Agarwal M, Hall JE, Dreisbach AW, et al. Cigarette smoking and chronic kidney disease in african americans in the jackson heart study. J Am Heart Assoc. (2016) 5:1–6. doi: 10.1161/JAHA.116.003280
31. Uetani M, Suwazono Y, Kobayashi E, Inaba T, Oishi M, Nogawa K. A longitudinal study of the influence of shift work on serum uric acid levels in workers at a telecommunications company. Occup Med (Lond). (2006) 56:83–8. doi: 10.1093/occmed/kqi178
32. Park S, Lee J-H. Associations of occupational and leisure-time physical activity with self-rated health in Korea. Prev Med (Baltim). (2022) 158:107022. doi: 10.1016/j.ypmed.2022.107022
33. Dos Santos M, Ferrari G, Lee DH, Rey-López JP, Aune D, Liao B, et al. Association of the “Weekend warrior” and other leisure-time physical activity patterns with all-cause and cause-specific mortality: A nationwide cohort study. JAMA Intern Med. (2022) 182:840–8. doi: 10.1001/jamainternmed.2022.2488
34. Kawai T, Autieri MV, Scalia R. Adipose tissue inflammation and metabolic dysfunction in obesity. Am J Physiol Cell Physiol. (2021) 320:C375–91. doi: 10.1152/ajpcell.00379.2020
35. Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol. (2011) 11:607–15. doi: 10.1038/nri3041
36. Asad A, Burton JO, March DS. Exercise as a therapeutic option for acute kidney injury: mechanisms and considerations for the design of future clinical studies. BMC Nephrol. (2020) 21:446. doi: 10.1186/s12882-020-02098-9
37. Stump CS. Physical activity in the prevention of chronic kidney disease. Cardiorenal Med. (2011) 1:164–73. doi: 10.1159/000329929
38. Yan T, Yang S, Zhou X, Zhang C, Zhu X, Ma W, et al. Chronic kidney disease among greenhouse workers and field workers in China. Chemosphere. (2022) 302:134905. doi: 10.1016/j.chemosphere.2022.134905
39. Hill NR, Fatoba ST, Oke JL, Hirst JA, O’Callaghan CA, Lasserson DS, et al. Global prevalence of chronic kidney disease - A systematic review and meta-analysis. PloS One. (2016) 11:e0158765. doi: 10.1371/journal.pone.0158765
Keywords: long working hours, estimated glomerular filtration rate (eGFR), chronic kidney diseases, physical activity (PA), modification
Citation: Yan T, Nabi S, Liu X, Zeng B, Song X, Ding X and Hu B (2024) The association of physical activity with kidney function risk among adults with long working hours. Front. Endocrinol. 15:1415713. doi: 10.3389/fendo.2024.1415713
Received: 08 May 2024; Accepted: 09 September 2024;
Published: 30 September 2024.
Edited by:
Lijing Gong, Beijing Sport University, ChinaReviewed by:
Huadong Xu, Hangzhou Medical College, ChinaXiaoli Guo, Henan Cancer Hospital, China
Qian Li, Shanghai Children’s Medical Center, China
Yuntao Hao, Dr. Von Hauner Children’s Hospital, LMU Munich University Hospital, Munich, Germany, in collaboration with reviewer QL
Copyright © 2024 Yan, Nabi, Liu, Zeng, Song, Ding and Hu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tenglong Yan, yantlyan@163.com; Binshuo Hu, hubsh1997@163.com
†These authors have contributed equally to this work
‡ORCID: Tenglong Yan, orcid.org/0000-0002-2424-0223
 Tenglong Yan
Tenglong Yan