- 1Department of Endocrine Ward, Huadong Hospital Affiliated to Fudan University, Shanghai, China
- 2Department of Nursing, Huadong Hospital Affiliated to Fudan University, Shanghai, China
- 3Department of Geriatrics, Affiliated with Huadong Hospital of Fudan University, Shanghai, China
- 4Department of Dermatology, Affiliated Huadong Hospital, Fudan University, Shanghai, China
Objective: The aim of this study is to assess the effectiveness of foot skin protection technology in elderly patients with diabetic peripheral neuropathy.
Methods: The foot skin protection technology was developed based on a comprehensive literature review and preliminary research conducted by our research team. Subsequently, 88 elderly patients with diabetic peripheral neuropathy and experiencing foot skin problems were recruited from two community health service centers in Shanghai. Using a random number table, the participants were randomly assigned to either the control group or the experimental group. Patients in the experimental group received foot skin protection technology interventions, while those in the control group received standard community nursing guidance for a duration of 3 months. The incidence, severity, and discomfort associated with foot skin problems were evaluated before and after the intervention period in both groups.
Results: The incidence, severity, and discomfort of foot skin problems notably reduced in the experimental group (all P< 0.05).
Conclusion: The foot skin protection technology demonstrates significant potential in enhancing foot skin condition.
1 Introduction
The population of elderly patients with diabetes in China is steadily rising alongside the aging demographic. Among the chronic complications affecting this demographic, diabetic foot ulcer (DFU) stands out as particularly prevalent, with peripheral neuropathy emerging as a significant independent risk factor for its development (1–3). Diabetic peripheral neuropathy (DPN) is a commonly encountered chronic complication in elderly patients with diabetes, characterized by neurological symptoms such as paresthesia, pain, and numbness (4). Roughly 30% to 40% of patients with diabetes, and up to 50% of those over 60 years old, experience peripheral neuropathy, which often leads to various foot skin problems and contributes significantly to the occurrence of DFU (5, 6). International guidelines emphasize the importance of regular assessment of foot skin condition and temperature to prevent DFU (7). Elderly individuals are more susceptible to skin damage compared to the general population. Given the chronic and insidious nature of DPN symptoms, early identification of foot skin problems in elderly patients is challenging but crucial for effective treatment and prognosis (8). Therefore, proactive nursing interventions aimed at early detection and management of skin problems in elderly patients with DPN are vital for preventing DFU.
Foot skin protection technology is a multidisciplinary collaboration involving departments such as endocrinology, dermatology, vascular surgery, orthopedics, specialized diabetic foot care clinics, and rehabilitation. This multidisciplinary team develops and applies the following specific techniques: (1) Biomechanics-based techniques to reduce foot pressure, such as pressure transfer techniques, callus trimming techniques, and the use of new dressings. (9) (2) Maintaining skin moisture, as diabetic peripheral neuropathy leads to issues like dry and cracked foot skin, which are risk factors for diabetic foot. For these issues, the care clinic and dermatology personnel conduct regular inspections and evaluations of patients and provide guidance on proper medication use. (3) Correction techniques for deformed toenails, involving trimming, filing, or reshaping the nails to make them more normal in shape, thereby reducing pressure and friction on surrounding tissues. (4) Individualized treatment, guidance, and medication for other emerging issues, including the three mentioned above (10). The skin problems are dynamically assessed, and intervention strategies are adjusted promptly. Ryder et al. (11) found that the occurrence of DFU is associated with autonomic nervous system damage. There is a close interaction between the autonomic nerves and skin keratinocytes and immune cells, playing an important regulatory role in skin physiological functions (12). Autonomic neuropathy can lead to reduced secretion of sweat glands and sebaceous glands, causing sweat dysfunction. When the skin moisture content is chronically low, haptens can more easily penetrate the skin, increasing the likelihood of sensitization. Additionally, reduced sweat can cause various skin issues such as dryness and scaling, compromising the skin’s integrity, damaging its barrier function, and increasing infection risk (13). Motor neuropathy can cause bone and joint damage and deformities, such as clawfoot deformity and Charcot joint deformity. The resulting dorsal and plantar flexion contractures create significant pressure points, altering the patient’s gait and leading to instability while walking. These changes can damage the skin on the feet, leading to ulcers. Motor neuropathy-induced muscle atrophy and deformity in the feet can continuously increase plantar pressure and cause abnormal pressure distribution, which are key factors in callus formation (14). Without timely intervention, persistent mechanical pressure may lead to DFU, and motor neuropathy can increase the risk of DFU in diabetic patients by up to 2.45 times (11). Sensory neuropathy causes positive symptoms such as tingling, burning, or pain, leading patients to scratch repeatedly. Concurrent ataxia or retinopathy increases the likelihood of falls. Negative signs mainly include the loss of protective sensation, with patients losing the ability to feel pain, pressure, and temperature in their feet, lacking self-protective awareness when injured, and being less likely to notice lesions. These abnormal sensations (either hypersensitivity or loss) can damage the skin on the feet, leading to ulcers (15). Currently, there are numerous protective measures for the foot skin of diabetic patients, but most interventions focus on single symptoms with limited consideration of disease-related factors. There are few targeted skin interventions for DPN, and there is a lack of comprehensive skin protection plans. Specific issues such as increased local skin tension due to motor neuropathy, hyperkeratosis caused by sensory neuropathy, and dryness and cracking resulting from impaired sweating function due to autonomic neuropathy are often not adequately addressed. The aim of this study is to evaluate and diagnose foot skin issues in elderly patients with DPN and explore the effectiveness of foot skin protection technology as an intervention method.
2 Participants and methods
2.1 Research participants
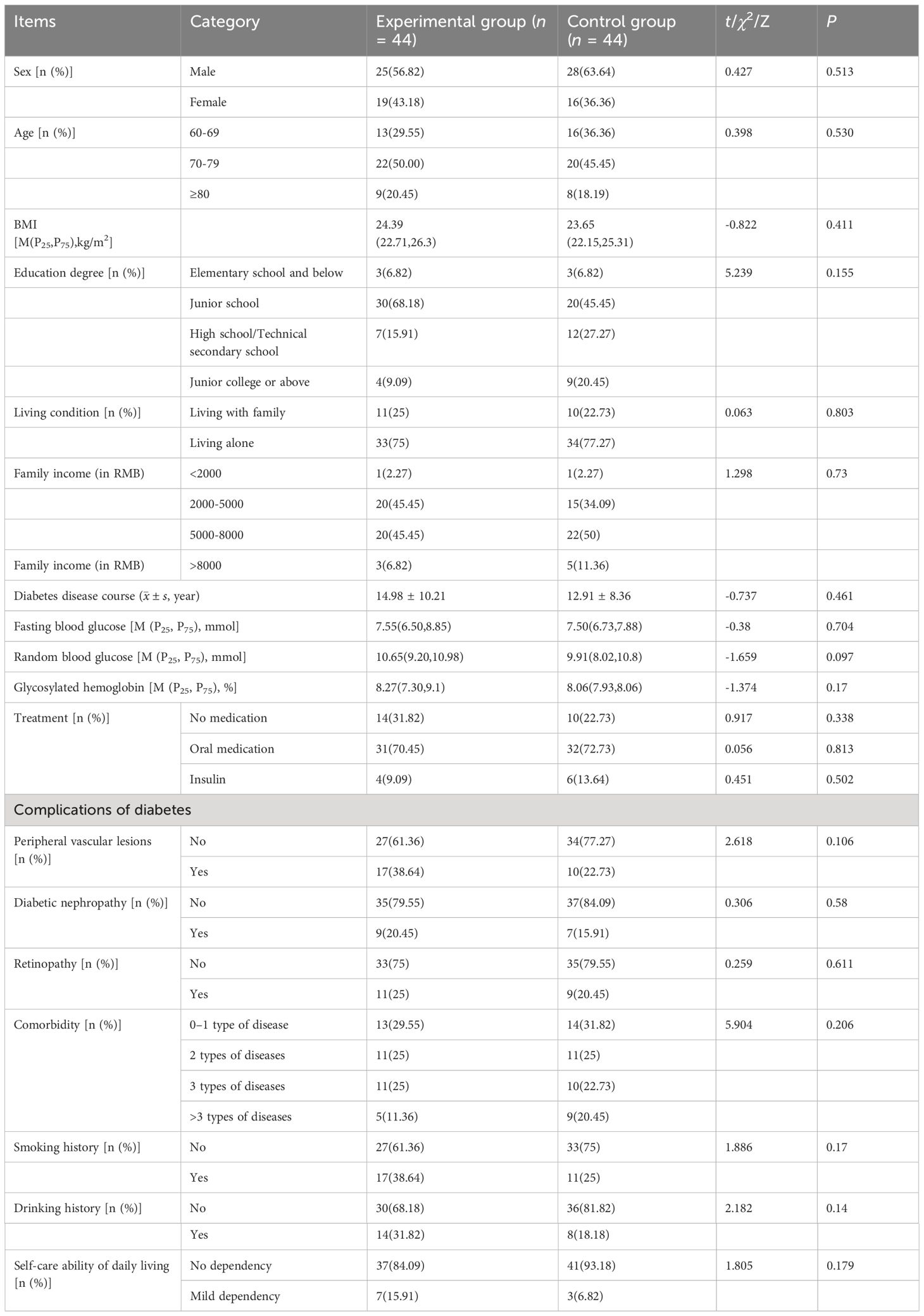
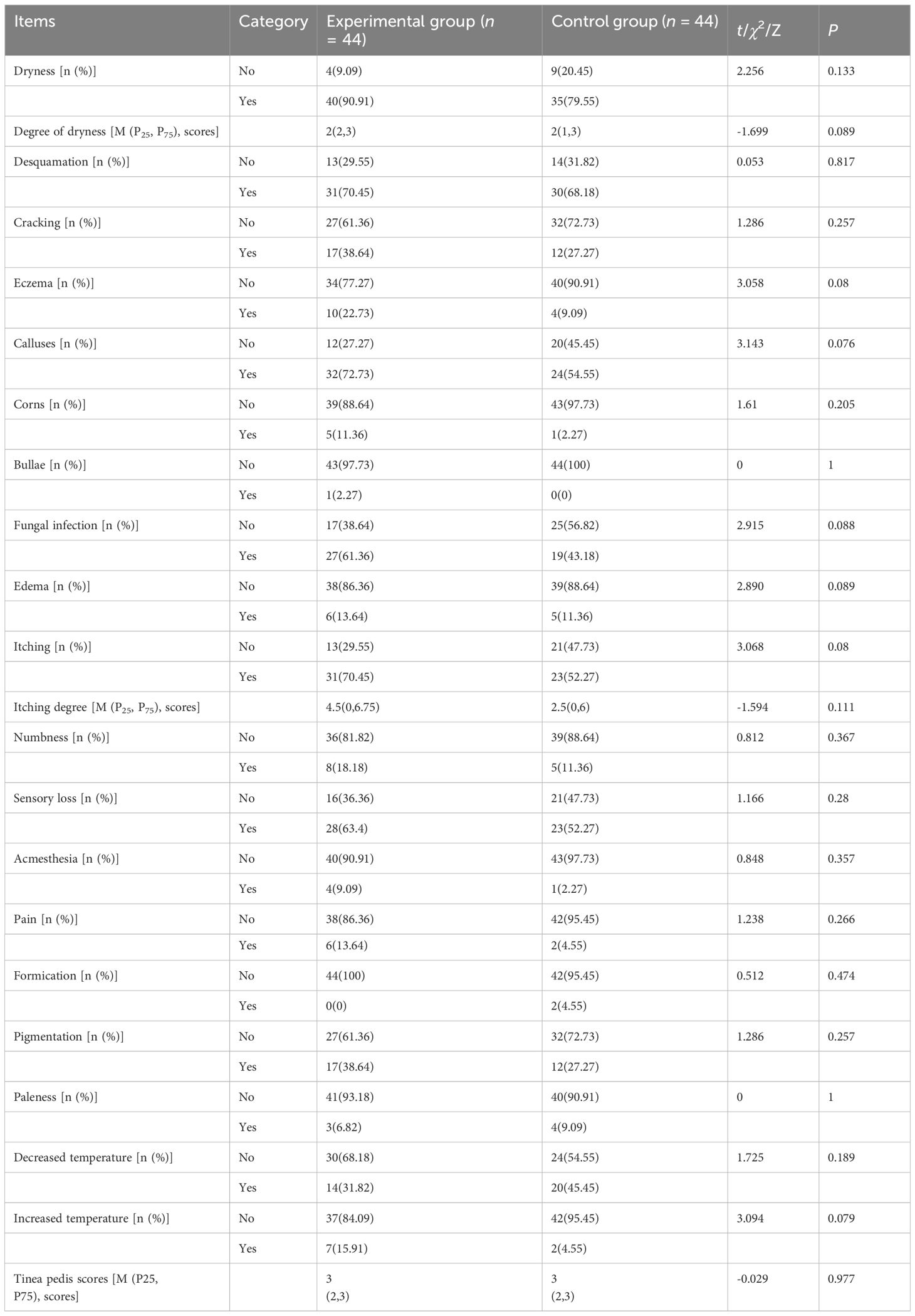
From June to August 2022, a total of 88 elderly patients with DPN were recruited from Shanghai Jiangsu Road Community Health Service Center and Xinhua Road Community Health Service Center. Inclusion criteria for participation were: (1) aged 60 years or older; (2) diagnosed with type 2 diabetes mellitus according to the 1999 WHO criteria; (3) diagnosed with diabetic peripheral neuropathy based on the 2013 Consensus on DPN Diagnosis and Treatment (16); (4) presence of one or more foot skin problems associated with DPN; (5) voluntary participation and signed the informed consent form. Exclusion criteria were: (1) presence of diabetic foot ulcers; (2) severe lower limb vascular problems related to diabetes mellitus; (3) history of amputation; (4) acute infections, severe musculoskeletal disorders, and so on; (5) unconsciousness, mental disorders, or non-cooperation with the research. Using a random number table, the participants were randomly assigned into two groups, with 44 patients in each group. However, 3 patients from each group were lost to follow-up, leaving a final cohort of 41 patients in the experimental group and 41 patients in the control group. Baseline data analysis revealed no significant differences between the two groups (all P > 0.05), ensuring comparability (see Tables 1–3). This study was registered in the Chinese Clinical Trials Registry with registration number ChiCTR2200066360 (detailed in Appendix 1). The study protocol, informed consent form, and relevant participant information were reviewed and approved by East China Hospital, with approval number 20220104 (detailed in Appendix 2), before commencement of the study.
The random grouping was conducted using SPSS software with the following steps: (1) Study subjects were assigned numbers; (2) A fixed starting value of 20220608 was set in the random number generator; (3) A random number sequence was generated by computing variables; (4) The generated random numbers were randomly divided into two groups in a 1:1 ratio and labeled as groups “1” and “2”; (5) The SPSS-generated random numbers and their corresponding group assignments were noted on cards, which were then placed in opaque, sealed envelopes, and the envelopes were labeled with serial numbers. The envelopes were handed to another research team member who was unaware of the grouping details. This member distributed the envelopes according to the order in which the subjects were included in the study. After the baseline measurements, the envelopes were opened on the spot. Patients with cards marked “1” received the foot skin protection plan based on elderly DPN patients, while those with cards marked “2” received the standard community foot skin care guidance for elderly DPN patients.
The flow diagram of the study process is shown in Supplementary Figure S1.
2.2 Methods
2.2.1 Development of foot skin protection technology in elderly patients with DPN
Following the principles of evidence-based medicine and drawing from previous clinical studies, alongside insights from real-world clinical practice, the foot skin protection technology tailored for elderly patients with DPN was developed. This technology encompasses various strategies, including biomechanics-based plantar decompression techniques, foot callus treatment methods, and management techniques for diabetic bullae (17).
2.2.2 Intervention methods
Patients in both the control and experimental groups received diabetic medication, nursing care, and health education regarding diabetic foot management. In the control group, patients attended community outpatient clinics where their concerns were addressed by outpatient specialist nurses. Conversely, patients in the experimental group were provided with the foot skin protection technology specifically tailored for elderly patients with DPN, developed by the podiatry clinic of East China Hospital. They were instructed to attend follow-up visits every 2 weeks at the integrated podiatry clinic of East China Hospital, with specific follow-up times determined accordingly. After a 3-month intervention period, the patients’ adherence to the skin protection plan, foot care practices, occurrence of foot problems, and the efficacy of the intervention were monitored and assessed during follow-up visits.
The standard community nursing guidance provided to the control group was as follows:
(1) Health Education: Conducted through foot care knowledge lectures and distribution of health education guidebooks. This included daily foot skin inspections, daily care routines, exercise precautions, proper selection of shoes and socks, toenail trimming prevention, and daily prohibitions for peripheral neuropathy.
(2) Clinic Visits for Foot Problems: When patients encountered foot problems, they visited the foot clinic where specialized nurses addressed their issues. The main content included assessing changes in foot skin, such as dryness, calluses, infections, damage, and abnormal sensations. Individualized treatment and health guidance were provided for existing skin problems.
(3) Monthly Telephone Follow-Ups: Conducted once a month, each call lasting 10–15 minutes. The primary focus was to understand any abnormal issues with the patient’s foot skin and provide guidance over the phone for any skin problems that occurred.
The foot skin protection technology provided to the experimental group was as follows:
(1) Individualized Education and Professional Support: Based on the overall and foot skin care assessment results, patients were provided with personalized education and professional technical support. Specific content included daily foot skin inspection, daily care, exercise precautions, proper selection of shoes and socks, standard toenail trimming, and daily prohibitions for peripheral neuropathy. A health education guidebook was distributed.
(2) Patient Involvement in Decision-Making: Patients were encouraged to actively participate in the decision-making process of the care intervention plan, enhancing their sense of health responsibility. This included daily skin care plans, exercise plans, and dietary aspects.
(3) Knowledge Lectures: Knowledge lectures were conducted in the 1st, 5th, and 9th weeks, focusing on the dangers of diabetic foot complications and how to prevent them, foot cleaning and moisturizing, proper toenail trimming, and selection and wearing of shoes and socks. Each lecture lasted 30 minutes. During the lectures, on-site interactions with patients were conducted, including a Q&A session to help patients recognize the importance of timely addressing foot skin problems and improve their awareness of foot protection.
(4) Emotional Support: Emotional support was provided through face-to-face and telephone communication and establishing a WeChat group to stay in contact with patients, listen to their feelings, and provide timely feedback. For elderly patients living alone, communication frequency was increased as needed. Monthly psychological counseling sessions were provided, offering emotional support. Three additional counseling sessions, each lasting 30 minutes, were scheduled in the 2nd, 7th, and 11th weeks. The themes were “The Impact of Diabetic Foot Skin Issues on Life and Emotional Reactions,” “Positive Ways to Cope with Foot Complications,” and “Emotional Management and Self-Regulation Techniques.”
(5) Follow-Up Appointments: Patients were guided to visit the Integrated Foot Clinic at Huadong Hospital every two weeks for a follow-up. Specific follow-up times were determined. During these visits, the execution of the patient’s skin protection plan, foot care behaviors, occurrence of foot problems, and the effectiveness of the application were tracked and evaluated.
(6) Adjustment of Intervention Plan: The content of the skin intervention care plan was adjusted promptly, and patients’ questions were answered.
To keep consistency during the implementation process, during the intervention period, participants regularly received clinical monitoring and guidance, including assessments of foot skin condition, monitoring of intervention effectiveness, and training in foot care techniques. This ensured participants correctly understood and executed the intervention plan, with timely adjustments made to the interventions to suit individual situations.
2.2.3 Quality control measures
Drawing from evidence-based medicine principles and prior clinical research findings, the foot skin protection technology for elderly patients with DPN was developed, and was meticulously refined through expert consultation to ensure its scientific rigor and safety. To mitigate selective bias, the randomization scheme was concealed. Standardized assessment and intervention protocols were established through unified training for all participating medical personnel. Regular follow-up visits were conducted biweekly to monitor progress. Additionally, a monthly 30-minute knowledge lecture covering diabetic foot complications, preventive measures, foot hygiene practices, proper toenail trimming techniques, footwear selection, and usage precautions was organized. During these sessions, interactive discussions were facilitated to engage patients directly, fostering an environment for queries and clarifications, thereby enhancing patients’ awareness of foot protection and the importance of timely treatment for foot skin issues.
2.2.4 Effect evaluation
2.2.4.1 Process indicators
Foot care behavior: The Foot Skin Self-Management Behavior Questionnaire consists of 8 items: “Daily skin inspection,” “Daily skin cleaning,” “Use of mild bath soap,” “Drying skin with a soft towel,” “Daily application of moisturizer,” “Wearing soft and breathable socks,” “Taking measures when exposed to sunlight,” and “Adhering to doctor’s guidance.” Scoring is based on a Likert 5-point scale, with scores ranging from 0–4 for each item, totaling a maximum of 20 points. Higher scores indicate better foot skin care by the patient.
Health-promoting behavior: This scale is based on the Health Promoting Lifestyle Profile (HPLP) developed and revised by Walker et al. (18) The scale uses a Likert 4-point scoring method (Never, Sometimes, Usually, Always). The overall Cronbach’s α coefficient for the scale is 0.94, with Cronbach’s α coefficients for the six dimensions ranging from 0.79 to 0.87. The Cronbach’s α coefficient for this dimension is 0.87.
2.2.4.2 Outcome indicators
Incidence and severity of foot skin problems: Common clinical measurement tools were used, including the Overall Dry Skin Score (19), Visual Analog Scale (20), Total Symptom Score (21) for athlete’s foot symptoms and signs, and the Diabetic Foot Comfort Assessment Plate (22).
Service Satisfaction (Client Satisfaction Tool): This scale is a patient satisfaction survey designed by Bear et al., using the Cox Health Behavior Interaction Model as a framework. This study uses the translated version by Bai Yating. The Cronbach’s α value and test-retest reliability of this scale are 0.938 and 0.974, respectively. The Pearson correlation coefficients for each item range from 0.630 to 0.919, and the Item-Level Content Validity Index for each item is 1.
2.2.5 Data collection
The data collection procedures were as follows: (1) Secured support for the study from the hospital and two community health service centers. (2) Community general practitioners were responsible for recruiting subjects who met the inclusion and exclusion criteria. Researchers provided detailed explanations and training on these criteria. (3) Researchers provided informed consent forms to the study subjects. These forms had been approved by the ethics committee and included detailed explanations of the study’s purpose, process, voluntariness, confidentiality, and harmlessness. The study commenced after the subjects signed the informed consent forms. (4) Before the study began, researchers collected general and disease-related information from the patients. After collecting the data, research members carefully checked and verified the information. If there were any missing items, they promptly inquired about the reasons and filled in the missing information; otherwise, the sample was considered invalid, ensuring the data was qualified. (5) Researchers assessed the patients’ foot skin problems, health behaviors, and service satisfaction twice: before the intervention began and three months after the intervention.
2.2.6 Statistic analysis
Statistical analysis was performed using SPSS 25.0 software.
To calculate the sample size, if estimating sample size using Pearson’s Chi-squared test, the formular is . If Fisher’s exact test or a corrected Chi-squared test for continuity was used, the formular is , in which α and β represent the probabilities of type I and type II errors, conventionally set at: two-sided α = 0.05, β = 0.1, Uα/2 = 1.96, Uβ = 1.282. Referring to the study by Yang et al. (23), the index of abnormal skin sensation changed from P1 = 0.51 to P2 = 0.15 with intervention, applying the formula yields: for Pearson’s Chi-squared test, each group requires 35 cases, adjusted for 10% loss to follow-up, totaling 78 cases with 39 per group; for Fisher’s exact test or corrected Chi-squared test for continuity, each group requires 38 cases, adjusted for 10% loss to follow-up, totaling 88 cases with 44 per group.
Continuous variables following a normal distribution are presented as mean ± standard deviation, while those not conforming to normal distribution are described as median and quartile. Categorical data are expressed as frequency and percentage. For normally distributed continuous data, independent samples t-test was employed to compare between the two groups. For non-normally distributed continuous data or ordinal categorical data, the Mann–Whitney U test, a non-parametric test, was utilized. The chi-squared test was applied to compare differences between the two groups for categorical data. Continuity correction in the chi-squared test was implemented when the theoretical frequency was ≥ 1 and< 5, and the Fisher’s exact probability method was used when the theoretical frequency was< 1. Paired sample t-test was utilized to compare pre- and post-intervention data within each group for normally distributed continuous variables, while the Wilcoxon test, a paired non-parametric test, was used in other cases. A significance level of P< 0.05 was considered statistically significant.
3 Results
3.1 Comparison of foot skin problems between the two groups
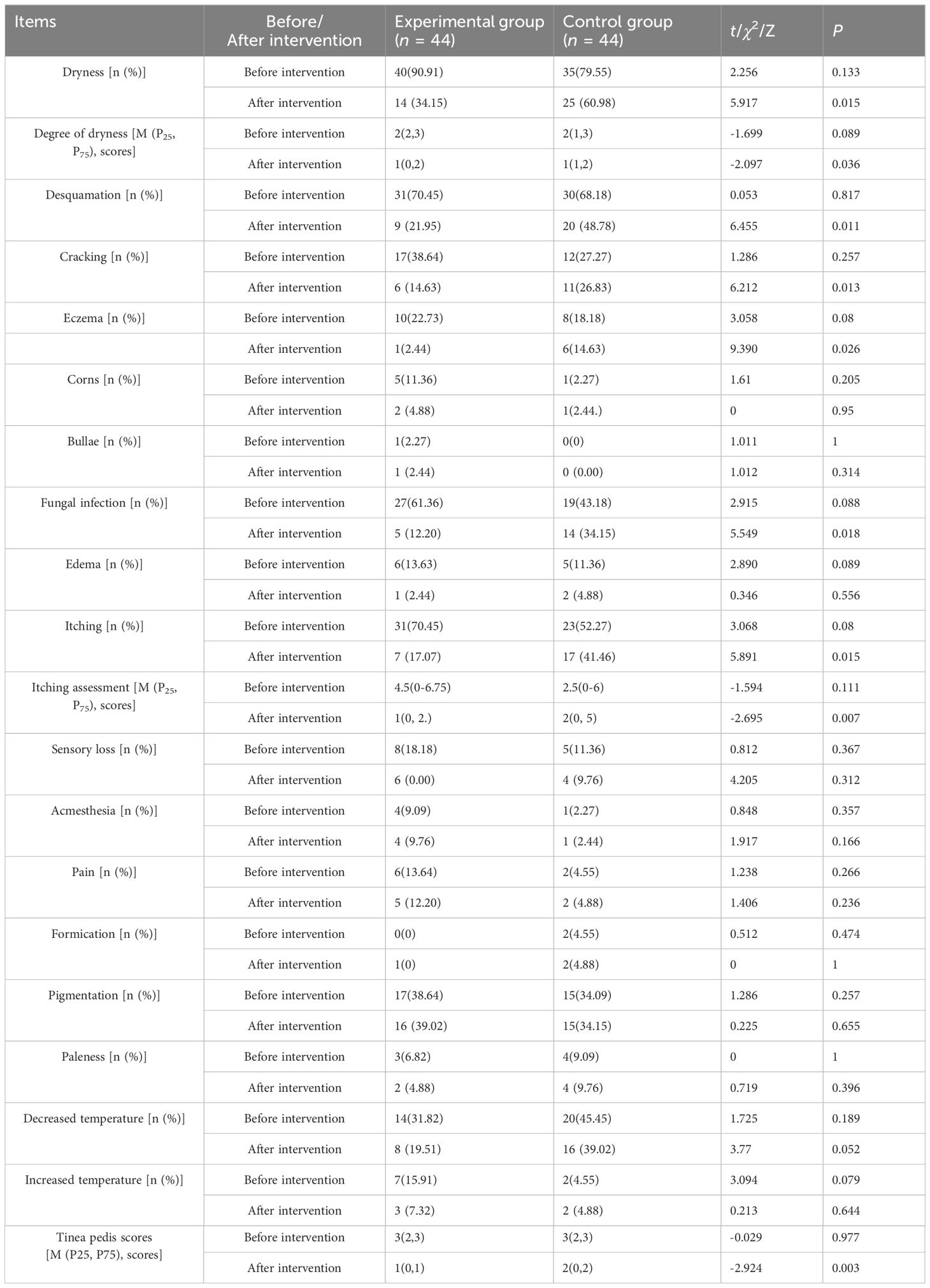
After three months of intervention, the experimental group exhibited lower incidences of various foot skin problems compared to the control group. Specifically, the incidence rates in the experimental group for skin dryness, desquamation, skin cracking, eczema, fungal infection, and itching were 34.15% (14 cases), 21.95% (9 cases), 14.63% (6 cases), 2.44% (1 case), 12.2% (5 cases), and 17.07% (7 cases), respectively. In contrast, the control group had higher incidence rates for these issues: 60.98% (25 cases), 48.78% (20 cases), 26.83% (11 cases), 14.63% (6 cases), 34.15% (14 cases), and 41.46% (17 cases), respectively. These differences were statistically significant (χ2 = 5.917, 6.455, 6.212, 9.390, 5.549, 5.891; P = 0.015, 0.011, 0.013, 0.026, 0.018, 0.015) (See Table 4 for details).
3.2 Comparison of the severity of foot skin problems between the two groups
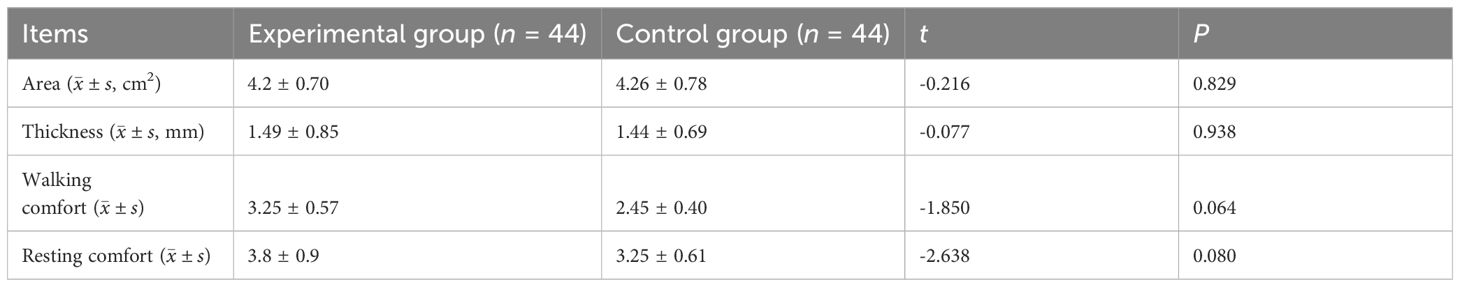
Based on statistical analysis, it was found that the area, thickness, and comfort levels of plantar calluses in the experimental group were significantly better than those in the control group (t =-2.486, -2.816, -2.693, -2.875; P = 0.013, 0.005, 0.007, 0.004) (Table 5). Additionally, the scores for dryness, itching, and tinea pedis in the experimental group were significantly lower compared to the control group (Z = -2.097, -2.695, -2.924; P = 0.036, 0.007, and 0.003, respectively) (Table 4).
4 Discussion
4.1 Diabetic peripheral neuropathy can cause a variety of skin problems
Ryder et al. (24) discovered a significant interplay between autonomic nerves, skin keratinocytes, and immune cells, which holds pivotal importance in regulating the physiological functions of skin (12). Autonomic neuropathy can trigger reduced secretion from sweat and sebaceous glands, resulting in dysfunction in perspiration, dryness, scaling, and various other skin issues (9). This can disrupt skin integrity, compromise barrier function, and heighten the risk of infections (13). Motor neuropathy-induced muscle atrophy and foot deformities can elevate plantar pressure and cause abnormal pressure distribution, crucial factors contributing to callus formation (14). Sensory neuropathy primarily manifests as a loss of protective sensation, rendering patients unable to perceive pain, pressure, or temperature changes in their feet. Consequently, patients may lack awareness of injuries and struggle to detect lesions, which can predispose them to foot skin damage (25).
4.2 Foot skin protection technology can reduce the occurrence of foot skin problems in elderly patients with DPN
Skin issues like dryness, cracking, eczema, itching, and fungal infections are common precursors to ulcers in diabetic patients, necessitating timely identification and treatment to prevent foot skin damage and subsequent infection (26). This study’s findings revealed a significant reduction in the incidence of these foot skin problems, including dryness, scaling, cracking, eczema, itching, and fungal infections, after a three-month intervention in the experimental group compared to the control group (P< 0.05). This suggests that foot skin protection technology can effectively lower the occurrence of such issues. Elderly patients with DPN often experience foot paresthesia, making it difficult for them to detect foot skin damage promptly, thus increasing their susceptibility to skin damage (24). Consequently, early detection and treatment of foot skin issues represent effective measures to prevent the onset and progression of foot ulcers (27).
4.3 Foot skin protection technology can reduce the severity of foot skin problems in elderly patients with DPN
Foot calluses can greatly impact a patient’s comfort, especially during walking, leading to a sensation of discomfort akin to having a foreign object present (28). These uncomfortable sensations can evoke negative emotions like anxiety and depression, fostering a sense of helplessness that hinders the adoption of healthy behavior. Following a three-month intervention, the experimental group exhibited significantly lower comfort scores associated with foot calluses compared to the control group (P< 0.05). It is important to note that the comfort score is inversely proportional to the level of comfort, with a lower score signifying an enhanced level of comfort. Employing evidence-based methods for timely and standardized treatment of foot calluses can mitigate the risk of skin damage and infection. Callus excision proves effective in relieving pressure on the plantar surface for patients. Research by Xu et al. (29) demonstrated that prompt callus treatment in 60 patients with diabetes effectively curbed the incidence of foot ulcers, enhanced quality of life, and reduced anxiety levels. Additionally, scores for foot skin dryness, itching, and athlete’s foot were markedly diminished in the experimental group compared to the control group (P< 0.05), indicating that foot skin protection technology not only reduces the occurrence of foot skin issues but also alleviates dryness, itching, and symptoms of athlete’s foot. Through standardized interventions, effective maintenance of skin moisture and oil secretion can be achieved, reducing the occurrence of skin problems related to dryness. Customized interventions based on individual and environmental characteristics are designed to meet specific needs. These interventions include guiding the elderly on proper foot inspection, cleaning, selection of suitable shoes and socks, nail trimming, appropriate exercise, choosing suitable moisturizing products, using proper pressure-relief footwear/assistive devices, and following medical advice. This approach helps patients understand health-related information and emphasizes the importance of foot skin care. By employing engaging methods such as “on-site demonstrations,” “hands-on teaching,” “on-site assessments,” and “prize quizzes,” elderly patients or their caregivers are taught essential foot care knowledge and skills. For issues that patients cannot resolve on their own, timely and appropriate handling and protection are provided. Patients are informed about when and how to seek medical attention, ensuring that they receive prompt and proper treatment for foot problems.
There are some limitations in this study. First, due to time constraints, the long-term care outcomes of patients were not discussed, and the long-term effects of interventions cannot be determined. Second, this study included subjects from only two community hospitals, thus the representativeness of the study is limited. Future research should be conducted in different regions and hospitals of various levels to broaden the sample sources, increase the overall sample size, and enhance the representativeness of the research results. In addition, the follow-up period should be expanded to continuously track the intervention effects of foot skin protection in elderly DPN patients and analyze the long-term impact of the protective measures on patients.
5 Conclusion
In this study, we elucidated the extent of foot skin issues among patients with DPN and investigated the efficacy of foot skin protection technology. Through the comparison of results from the experimental and control groups, it is evident that the utilization of this technology markedly diminishes both the occurrence and severity of skin issues, leading to improved patient comfort and overall well-being. This study offers a crucial theoretical and practical foundation for nursing care in elderly patients with diabetes. Future research should delve into the operational complexities and long-term impacts of foot skin protection technology, alongside its dissemination and implementation in clinical settings, to furnish more efficacious strategies for caring for elderly patients with diabetes.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Huadong Hospital Affiliated to Fudan University (No.20220104). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LZ: Conceptualization, Formal analysis, Writing – original draft. P-FS: Formal analysis, Writing – original draft. WQ: Data curation, Formal analysis, Writing – review & editing. QJ: Data curation, Formal analysis, Writing – review & editing. FM: Conceptualization, Writing – review & editing. J-JB: Conceptualization, Formal analysis, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by Clinical Research Project of Huadong Hospital Affiliated to Fudan University “The key to promote muscle strength rehabilitation in elderly patients with diabetes Research and transformation of technology” (No.HDLC2022008); Key Special Disease Construction Project of Huadong Hospital Affiliated to Fudan University (No.ZDZB2224); Fudan University Fuxing Nursing Research Fund Key Project, titled “Mechanism of Health Behavior Degradation and Early Warning Strategies in Elderly Diabetic Patients with Dangerous Feet from the Perspective of Ego Depletion Theory” (No.FNF202301); Fudan University-Fosun Nursing Research Fund Project "Health Resource Utilization Status of Elderly Diabetic Foot Patients" (No.FNF202463); Shanghai Clinical Research Center for Rehabilitation Medicine (No.21MC1930200).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2024.1411657/full#supplementary-material
Supplementary Figure 1 | A flow diagram of study process.
Abbreviations
DPN, Diabetic Peripheral Neuropathy; DFU, Diabetic Foot Ulcers.
References
1. Bacarin TA, Sacco IC, Hennig EM. Plantar pressure distribution patterns during gait in diabetic neuropathy patients with a history of foot ulcers. Clinics (Sao Paulo). (2009) 64:113–20. doi: 10.1590/S1807-59322009000200008
2. Oguejiofor OC, Odenigbo CU, Oguejiofor CB. Evaluation of the effect of duration of diabetes mellitus on peripheral neuropathy using the United Kingdom screening test scoring system, bio-thesiometry and aesthesiometry. Niger J Clin Pract. (2010) 13:240–7.
3. Xia C, Xu J, Wu WX. Health status of the elderly population in China and analysis of influencing factors. Chin Nurs Res. (2016) 30:2580–3.
4. Jaiswal M, Divers J, Dabelea D, Isom S, Bell RA, Martin CL, et al. Prevalence of and risk factors for diabetic peripheral neuropathy in youth with type 1 and type 2 diabetes: SEARCH for diabetes in youth study. Diabetes Care. (2017) 40:1226–32. doi: 10.2337/dc17-0179
5. Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. (2011) 94:311–21. doi: 10.1016/j.diabres.2011.10.029
6. Iqbal Z, Azmi S, Yadav R, Ferdousi M, Kumar M, Cuthbertson DJ, et al. Diabetic peripheral neuropathy: Epidemiology, diagnosis, and pharmacotherapy. Clin Ther. (2018) 40:828–49. doi: 10.1016/j.clinthera.2018.04.001
7. Schaper NC, van Netten JJ, Apelqvist J, Bus SA, Hinchliffe RJ, Lipsky BA, et al. Practical Guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes Metab Res Rev. (2020) 36 Suppl 1:e3266. doi: 10.1002/dmrr.3266
8. Fore J. A review of skin and the effects of aging on skin structure and function. Ostomy Wound Manage. (2006) 52:24–35.
9. Singh AV, Gemmati D, Kanase A, Pandey I, Misra V, Kishore V, et al. Nanobiomaterials for vascular biology and wound management: a review. Veins Lymphatics. (2018) 7:34–47. doi: 10.4081/vl.2018.7196
10. Zhong DY, Li L, Li HJ, Ma RM, Deng YH. Study on the mechanism and molecular docking verification of buyang huanwu decoction in treating diabetic foot. World J Tradit Chin Med. (2023) 9:178–90. doi: 10.4103/2311-8571.370108
11. Ryder RE, Kennedy RL, Newrick PG, Wilson RM, Ward JD, Hardisty CA, et al. Autonomic Denervation may be a Prerequisite of Diabetic Neuropathic Foot Ulceration. Diabetic Med. (2010) 7:726–30. doi: 10.1111/j.1464-5491.1990.tb01477.x
12. Yu S, Yu TZ, Li W. Role of autonomic nerves in immune dysregulation in atopic dermatitis. Chin J Dermatol. (2022) 55:362–5. doi: 10.35541/cjd.20210298
13. Doi T, Mizukawa Y, Shimoda Y, Yamazaki Y, Shiohara T. Importance of water content of the stratum corneum in mouse models for contact hypersensitivity. J Invest Dermatol. (2017) 137:151–8. doi: 10.1016/j.jid.2016.08.031
14. Deli G, Bosnyak E, Pusch G, Komoly S, Feher G. Diabetic neuropathies: diagnosis and management. Neuroendocrinology. (2013) 98:267–80. doi: 10.1159/000358728
16. Chinese diabetes society. Chinese guidelines for the prevention and treatment of type 2 diabetes (Basic edition). Chin J Gen Practitioners. (2013) 12:675–96.
17. Song PF, Zhou QH, Bai JJ, Shui RY. Summary of the best evidence for skin protection in diabetic peripheral neuropathy. Shanghai Nurs. (2021) 21:25–30.
18. Walker SN, Sechrist KR, Pender NJ. The Health-Promoting Lifestyle Profile: development and psychometric characteristics. Nurs Res. (1987) 36:76–81. doi: 10.1097/00006199-198703000-00002
19. Paul C, Maumus-Robert S, Mazereeuw-Hautier J, Guyen CN, Saudez X, Schmitt AM, et al. Prevalence and risk factors for xerosis in the elderly: a cross-sectional epidemiological study in primary care. Dermatol: Int J Clin Invest Dermatol. (2011) 223:260–5. doi: 10.1159/000334631
20. Ständer S, Augustin M, Reich A, Blome C, Ebata T, Phan NQ, et al. Pruritus assessment in clinical trials: consensus recommendations from the International Forum for the Study of Itch (IFSI) Special Interest Group Scoring Itch in Clinical Trials. Acta Derm Venereol. (2013) 93:509–14. doi: 10.2340/00015555-1620
21. Fu MH, Li M, Li RY, Wang AP, Wen H, Guo ZP, et al. A multicentre, randomised, double-blind controlled study of different courses of 1% luliconazole cream in the treatment of tinea pedis. Chin J Dermatol. (2014) 47:453–6. doi: 10.3760/cma.j.issn.0412-4030.2014.07.001
22. Bai JJ, Sun J, Tu XJ, Pan X, Ming Y. Diabetic foot comfort assessment plate. East China Hospital. (2014).
23. Yang H. Impact of focus resolution model nursing on knowledge of diabetic foot patients and changes in foot skin conditions. Dermatol Venereology. (2020) 42:607–8.
24. Ryder RE, Kennedy RL, Newrick PG, Wilson RM, Ward JD, Hardisty CA. Autonomic denervation may be a prerequisite of diabetic neuropathic foot ulceration. Diabetes Med. (1990) 7:726–30. doi: 10.1111/j.1464-5491.1990.tb01477.x
26. Zhou L, Bai JJ, Tao XM, Jia Y. Investigation and analysis of foot skin problems in elderly diabetic patients in community. J Nurs Sci. (2022) 37:102–5.
27. Wu R, Bai JJ, Zhou J, Sun J, Ming Y. Investigation and analysis of pre-hospital diagnosis and treatment of elderly diabetic foot patients. Geriatrics Health Care. (2020) 26:283–6.
28. Liu J, Bai R, Qi X, Lu Q, Yuan GH, Guan H, et al. Progress in intervention and evaluation of foot callus in diabetic patients. Chin J Diabetes. (2020) 28:547–9.
Keywords: diabetic foot, diabetic peripheral neuropathy, elderly diabetes, nursing, skin protection
Citation: Zhou L, Song P-F, Qin W, Jia Q, Miao F and Bai J-J (2024) Effectiveness of foot skin protection technology in elderly patients with diabetic peripheral neuropathy. Front. Endocrinol. 15:1411657. doi: 10.3389/fendo.2024.1411657
Received: 03 April 2024; Accepted: 22 July 2024;
Published: 19 August 2024.
Edited by:
Joanne Paton, University of Plymouth, United KingdomReviewed by:
Ajay Vikram Singh, Federal Institute for Risk Assessment (BfR), GermanyCosmin Mihai Vesa, University of Oradea, Romania
Copyright © 2024 Zhou, Song, Qin, Jia, Miao and Bai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiao-Jiao Bai, YmpqMTYzMTYzQDE2My5jb20=; Fei Miao, bWlhb2ZlaTQ4ODUxMDJAYWxpeXVuLmNvbQ==
†These authors have contributed equally to this work
 Lin Zhou1†
Lin Zhou1† Jiao-Jiao Bai
Jiao-Jiao Bai