- 1Department of Nephrology, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan, China
- 2College of First Clinical Medicine, Shandong University of Traditional Chinese Medicine, Jinan, China
Background: 25-hydroxyvitamin D is the body’s main storage form of vitamin D and is internationally recognized as the best indicator of vitamin D status in the human body. There is a scarcity of research investigating the interrelationship between serum 25-hydroxyvitamin D (25(OH)D) levels and mortality among elderly individuals with hyperlipidemia. To address this knowledge gap, we examined the association between serum 25(OH)D levels and mortality in an older hyperlipidemic population from NHANES, while controlling for other influential factors. The study sought to elucidate the correlation between serum 25(OH)D levels and mortality about all-cause mortality, cardiovascular disease (CVD), malignant neoplasms, and mortality from other causes.
Methods: The data from NHANES 2001-2016, including 9,271 participants were analyzed to examine the association between serum 25(OH)D levels and mortality. The interrelationship was illustrated using Kaplan-Meier curves and restricted cubic splines, while the Cox proportional hazards model was utilized to estimate the multifactor adjusted hazard ratio (HR).
Results: This study included 9,271 participants (43.28% male) with an average age of 69.58 years, and the average duration of participant follow-up was 88.37 months. Kaplan-Meier curves demonstrated that lower serum 25(OH)D levels were associated with increased risks of all-cause mortality, cardiovascular mortality, malignant neoplasm mortality, and mortality from other causes. This negative association was further confirmed by the Cox proportional hazards models. Additionally, restricted cubic splines not only revealed this negative association but also highlighted the saturated serum 25(OH)D levels. Moreover, subgroup analyses indicated that the inverse correlation between serum 25(OH)D levels and all-cause mortality was more pronounced in the non-obese and smoking population. And the inverse correlation with mortality from other causes was even stronger in the non-obese population.
Conclusions: In the elderly population with hyperlipidemia, 25(OH)D serum levels were negatively correlated with both cause-specific mortality and all-cause mortality. Moreover, there was a threshold effect in this negative association.
1 Introduction
Hyperlipidemia is a metabolic disorder characterized by dysregulated lipid metabolism. It can result in elevated cholesterol or triglycerides in the bloodstream, which are usually associated with reduced levels of high-density lipoprotein (1). There are numerous studies demonstrated that elevated serum cholesterol, increased low-density lipoprotein (LDL) or triglyceride levels, and reduced serum high-density lipoprotein (HDL) levels are strongly associated with the increased risk of CVD in patients (2). In recent studies, it has been demonstrated that hyperlipidemia is also significantly associated with heightened mortality risk across multiple conditions, including diabetes, malignancies, systemic autoimmune diseases, and renal diseases (3–6). Currently, hyperlipidemia continues to present significant challenges to the global population, with a considerable proportion of patients receiving lipid-lowering treatment failing to achieve optimal control (7). Elderly individuals are a high-risk group for developing hyperlipidemia, which further amplifies their susceptibility to mortality from diverse pathological conditions (1).
Vitamin D is one of the most essential micronutrients of humans. 25(OH)D represents the primary form of vitamin D synthesized by the human body and serves as a key marker to evaluate the absorption and metabolism of vitamin D (8). However, its optimal level remains controversial. The current regulations consider that 25(OH)D laboratory analyses should be monitored for performance through an external quality assessment scheme that provides target reference values for standardized measurement procedures (9). Notably, serum levels of 25(OH)D are closely associated with various health conditions and prognoses. Extensive evidence suggests that lower levels of 25(OH)D are linked to an increased risk of developing conditions such as osteoporosis, chronic kidney diseases, autoimmune disorders, nervous system diseases, and specific types of cancers (10–13). Moreover, numerous research studies have consistently demonstrated a significant correlation between reduced 25(OH)D levels and elevated mortality risk. Similarly, serum levels of 25(OH)D exert an impact on the occurrence and progression of CVD and diabetes. Adequate levels of 25(OH)D have been shown to protect the cardiovascular system and help prevent illnesses such as hypertension, coronary artery disease, and stroke (14). Conversely, insufficient levels of 25(OH)D can contribute to insulin resistance and the development of diabetes, given its vital role in insulin secretion, the maturation of insulin-secreting cells, and overall insulin function. In summary, 25(OH)D serum levels have a significant impact on the overall health of populations.
In conclusion, we hypothesized that there might be a potential association between serum levels of 25(OH)D and mortality in the elderly population with hyperlipidemia. Therefore, this study aimed to investigate this potential association, thus contributing to improving the health status of older adults affected by hyperlipidemia.
2 Method
2.1 Study design and participants
NHANES (https://www.cdc.gov/nchs/nhanes/index.htm), conducted by the Centers for Disease Control and Prevention (CDC), is a survey research program based on the population and cross-sectional, which was used to evaluate the nutritional conditions and the overall health of the entire population in American through a complex survey method. The database includes a wide range of data, including demographic, dietary, examination, laboratory, and questionnaire information. The study procedures were authorized by the Ethical Review Committee of the National Health Statistical Research Center and all individuals agreed to join the study. Data collection was carried out over eight periods between 2001 and 2016. Additionally, the NHANES Public-Use Linked Mortality Files were linked with the NHANES database from 2001 to 2016, enabling researchers to identify participant deaths up until December 31, 2019.
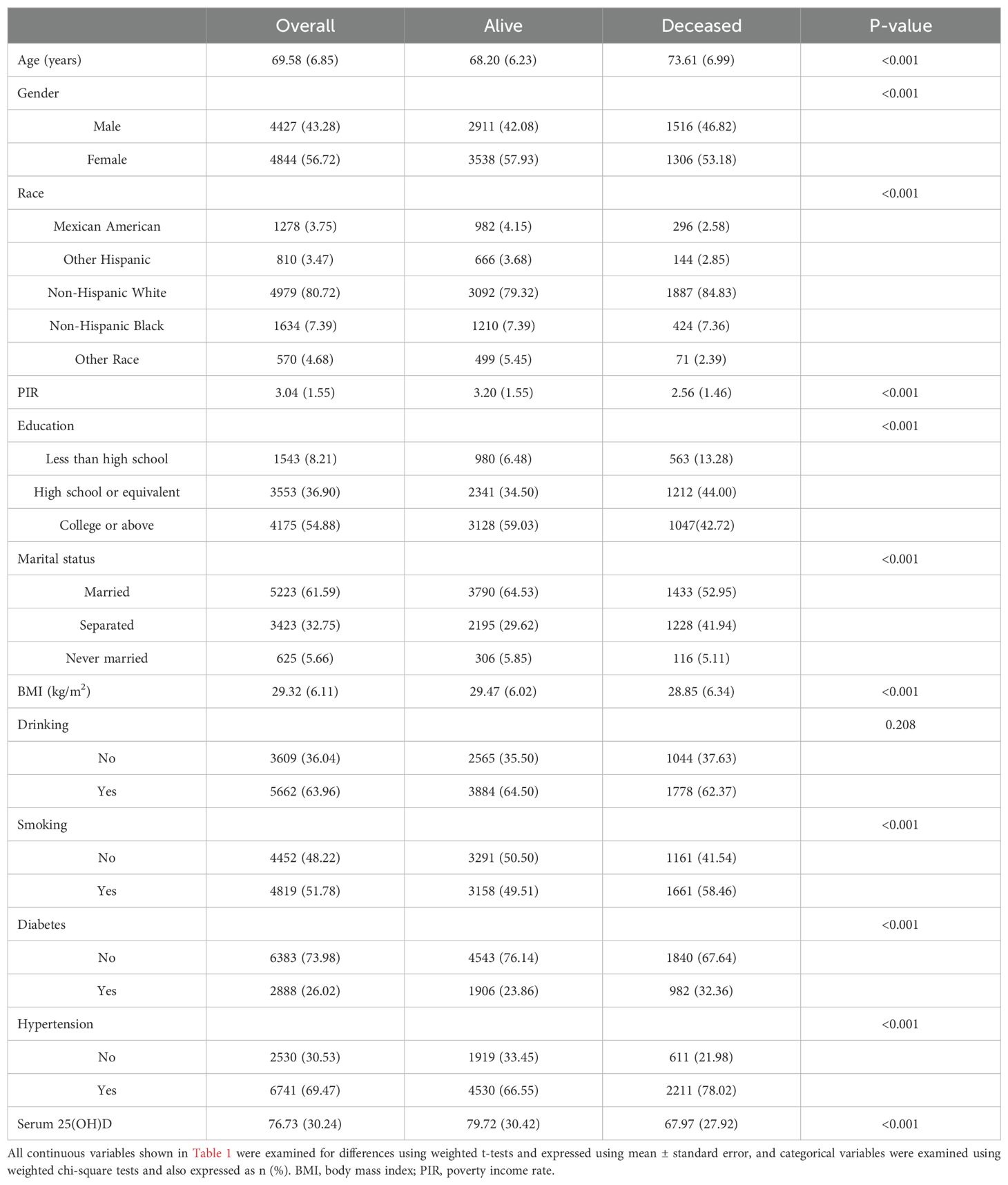
In this cohort study, a total of 91,352 subjects were initially included. After including participants aged 60 years or older, we excluded participants with missing 25(OH)D information (n=2,166), participants with undiagnosed hyperlipidemia (n=2,664), and participants with missing mortality data (n=1,160). Subsequently, we further excluded participants with missing information on covariates, including those with missing information on poverty income rate (PIR), education information, body mass index (BMI), and information on drinking and smoking. A final analysis cohort of 9271 individuals was obtained (shown in Figure 1).
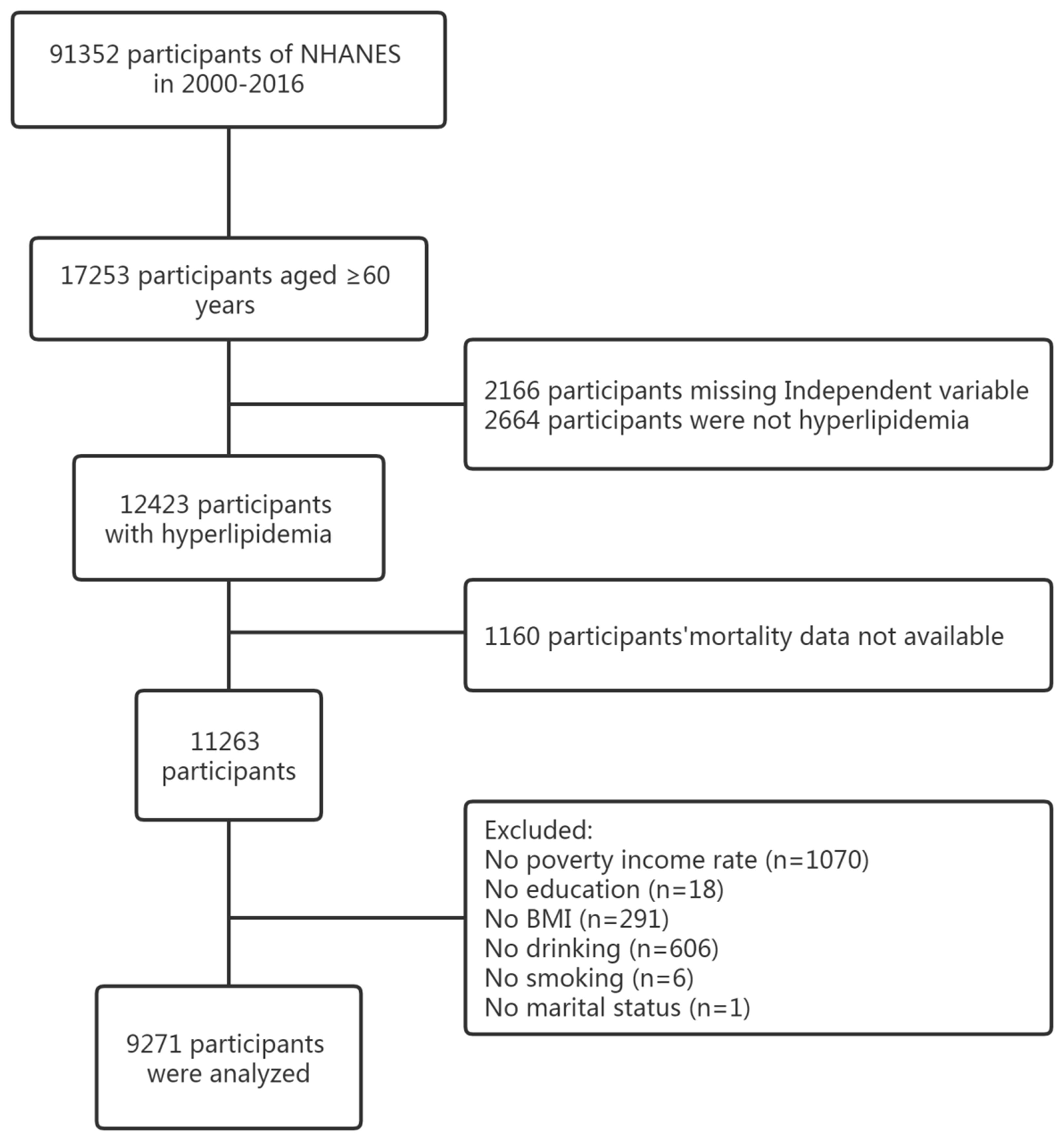
Figure 1. Flow chart of this study design from NHANES. NHANES, National Health and Nutrition Examination Survey.
2.2 Determination of 25(OH)D serum levels
In the NHANES 2001-2006 study, 25(OH)D serum levels were measured by the CDC using radioimmunoassay (DiaSorin Assay Kit). Serum samples from 2007 to 2016 were analyzed using a standardized liquid chromatography-tandem mass spectrometry (LC-MS/MS) to estimate the 25(OH)D serum levels. The 25(OH)D serum levels of participants who took part in NHANES 2001-2006 were transformed into equivalent values derived from the standardized LC-MS/MS technique using regression. This transformation was performed to facilitate the utilization and evaluation of 25(OH)D serum levels by researchers. The unit of measurement for 25(OH)D serum levels is nmol/L.
2.3 Covariates
The study incorporated data from the NHANES database, which encompasses details on demographics, examination information, laboratory information, and questionnaire information. The following categories composed the demographic data: age, gender, ethnicity (Mexican American, Other Hispanic, Non-Hispanic Black, Non-Hispanic White, or Other Race), level of education (less than high school, high school or equivalent, and college or above), the status of marital (never married, married, and separated), and PIR. Age and PIR were treated as continuous variables, while race, education, and marital status were considered categorical variables. Examination information included diastolic blood pressure (DBP), systolic blood pressure (SBP), weight, and height information. BMI was calculated by dividing the participant’s weight in kilograms by the square of their height in meters. Laboratory information contained measurements for fasting plasma glucose, hemoglobin A1c (HbA1c), total cholesterol, triglycerides, HDL, and LDL. The questionnaire section contained information about drug use, alcohol consumption, and smoking habits.
In this study, hypertension was identified as a self-reported high blood pressure diagnosis, currently receiving treatment for hypertension, with SBP (average) ≥140 mmHg or DBP (average) ≥90 mmHg. Diabetes was characterized by either self-reported diagnosis, self-reported utilization of medication or insulin to reduce glucose, HbA1c levels of 6.5%, or glucose levels of fasting plasma ≥ 7.0 mmol/L. Hyperlipidemia was characterized by triglycerides at or above 150 mg/dl, total cholesterol at or above 200 mg/dl, LDL at or above 130 mg/dl without using cholesterol-lowering drugs, and HDL lower than 40 mg/dl in men or 50 mg/dl in women.
According to the results of the survey, participants were divided into two groups: nonsmokers and smokers. Smoker status refers to individuals who reported smoking more than 100 cigarettes in their lifetime. The drinking status (yes or no) was determined based on whether alcohol consumption exceeded 12 drinks in the past year.
2.4 Statistical analysis
Considering the potential linear or nonlinear association between 25(OH)D serum levels and various mortality outcomes (including all-cause mortality, cardiovascular disease fatality, malignant neoplasm mortality, and other-cause mortality), subjects were categorized into four groups based on quartiles of 25(OH)D serum levels: Q1 (<49.50 nmol/L), Q2 (49.5-67.50 nmol/L), Q3 (67.5-86.7 nmol/L), and Q4 (>86.7 nmol/L).
Continuous variables are presented as mean (standard error, SE), while categorical data is expressed as frequencies (percentages). Kaplan-Meier curves were used to illustrate survival rates based on 25(OH)D serum levels. To visualize the nonlinear correlation between 25(OH)D serum levels and mortality, restricted cubic splines were employed. Cox proportional hazard models were utilized to calculate adjusted hazard ratios (HRs) and their corresponding 95% confidence intervals for different mortality rates associated with 25(OH)D serum levels. Model 1 represents unadjusted results, while Model 2 adjusts for age, sex, race, and PIR. Model 3, which includes all covariates from Model 2, additionally adjusts for education, marital status, BMI, drinking, smoking, diabetes, and hypertension. Finally, a subgroup analysis was utilized to investigate the robust relationship between 25(OH)D serum levels and fatality rate across different populations.
Every result produced from the data was calculated utilizing a weighted data analysis that was founded on intricate sampling. All statistical analyses were performed using R version 4.0.4 (R-project.org), incorporating weighted data analysis based on complex sampling. Statistical significance was indicated by a P-value below 0.05 in all studies.
3 Results
3.1 Baseline characteristics and demographic information of participants
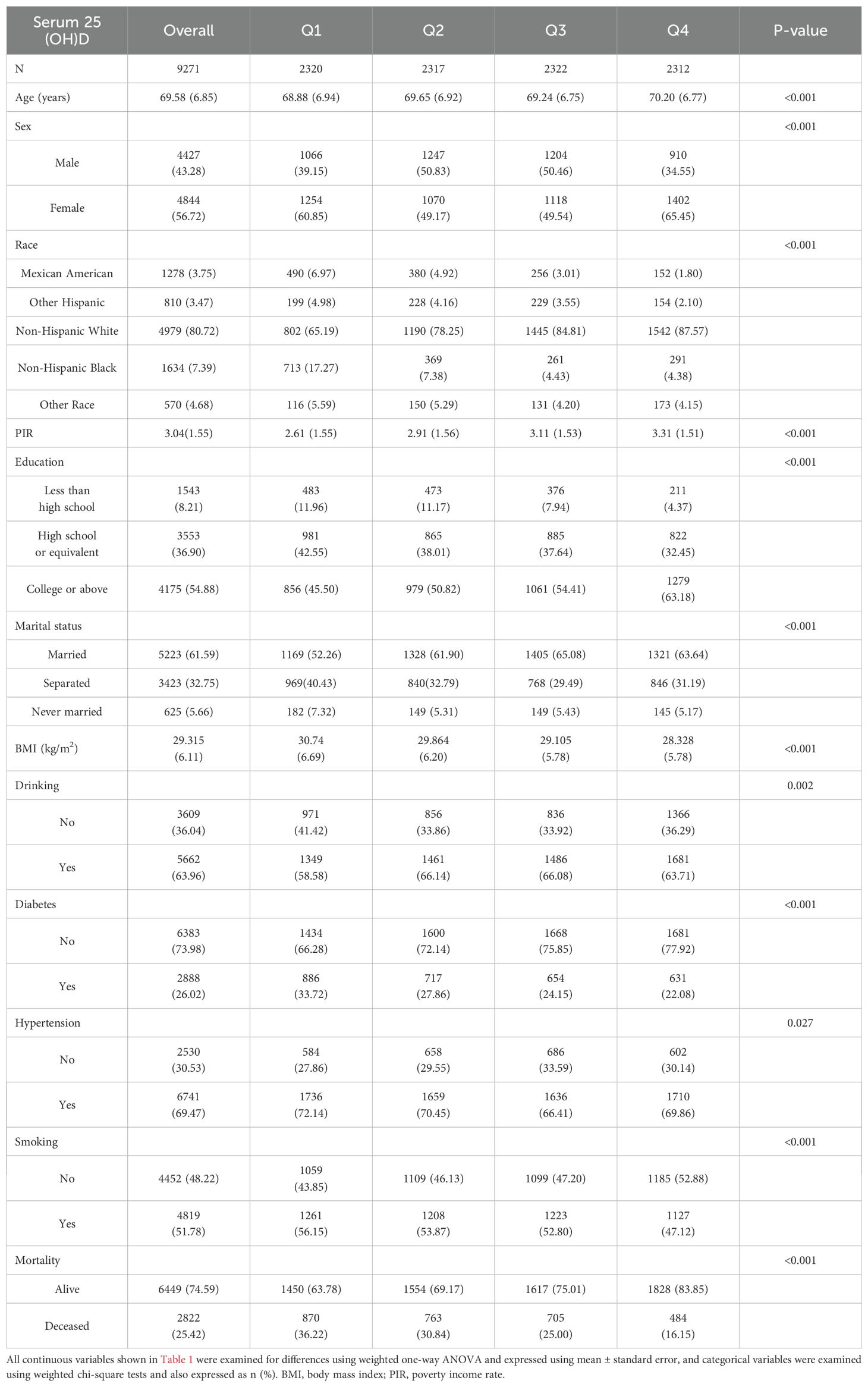
Based on the final cohort study, a total of 9,271 participants were included, with males representing 43.28% of the cohort. The average age of participants was 69.58 years, and the mean follow-up period was 88.37 months. Table 1 provides detailed information on survival and mortality rates among the subjects in this study. Age, gender, race, PIR, education level, marital status, BMI, smoking, diabetes, hypertension, and 25(OH)D serum levels were found to have statistically significant associations with mortality rates (P < 0.05). However, no correlation was observed between drinking status and mortality rates. Table 2 examines the relationship between the aforementioned variables and the independent variable, 25(OH)D serum levels. Higher 25(OH)D serum levels were frequently related to increased survival and reduced mortality rates.
3.2 The relationship between mortality and 25(OH)D serum levels
The cumulative Kaplan-Meier curve of the quartiles of 25(OH)D levels is presented in Figure 2. Regarding the overall mortality rate, the cumulative survival probability was significantly lower in the lowest 25(OH)D levels group (P < 0.001). This pattern was consistent for CVD mortality, malignant neoplasm mortality, and other causes of mortality (P < 0.001).
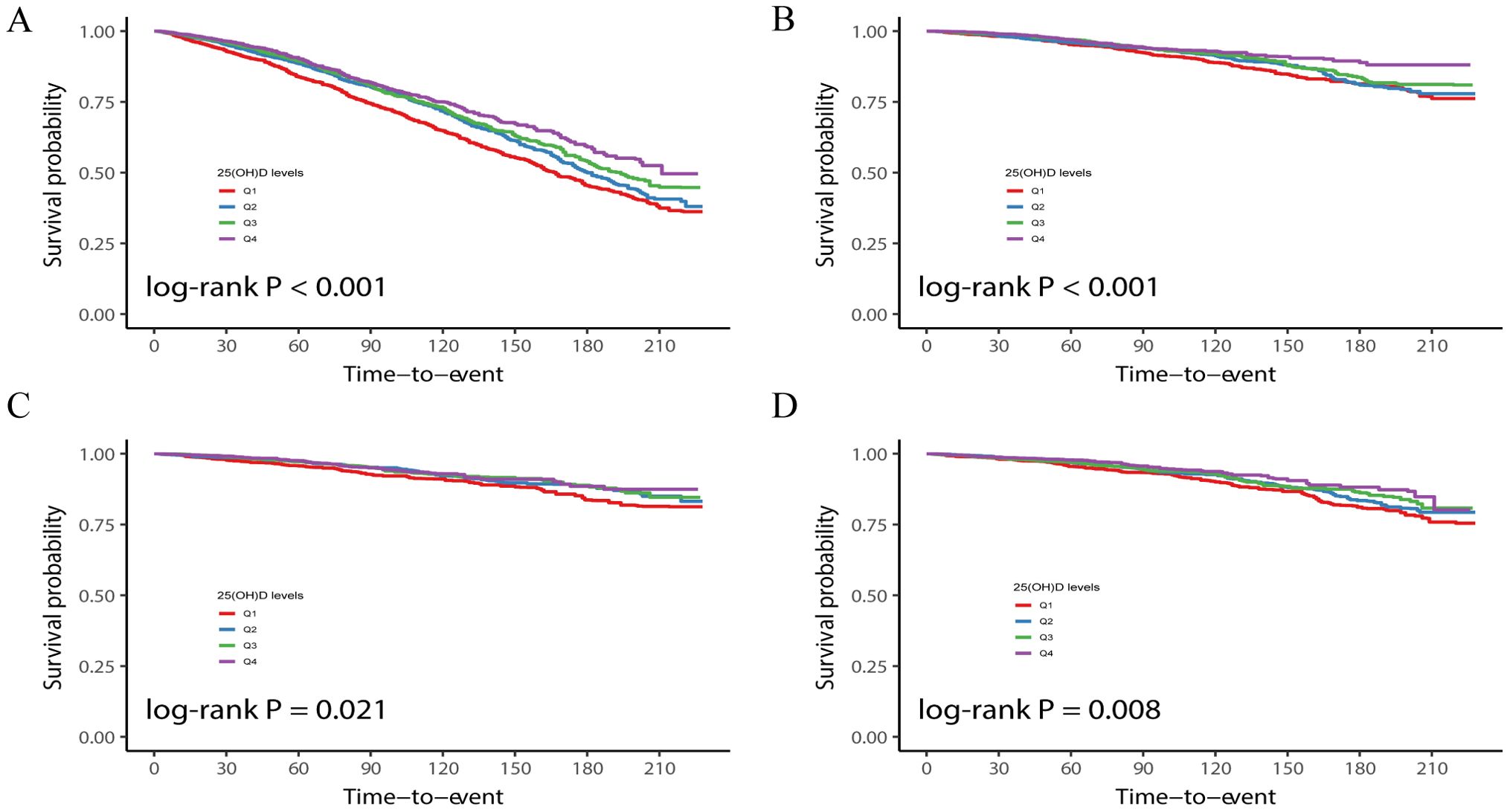
Figure 2. Kaplan-Meier curves showing the relationship between serum 25(OH)D levels quartiles and all-cause (A), CVD (B), malignant neoplasms (C), and other-cause (D) mortality.
To further investigate the impact of serum 25(OH)D levels on mortality, three Cox regression models were constructed. These models accounted for various factors, including age, sex, ethnicity, education attainment, poverty income rate (PIR), marital status, BMI, smoking status, drinking habits, and history of diabetes or hypertension (Model 3). The adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated as follows: 0.996 (0.994, 0.998), 0.995 (0.991, 0.999), 0.997 (0.993, 1.002), and 0.994 (0.989, 0.999) for all-cause mortality, CVD mortality, malignant neoplasm mortality, and other-cause mortality, respectively.
The HRs and 95% CIs in Table 3 calculated for the quartiles of 25(OH)D serum levels, ranging from the lowest to highest categories, were as follows: 1.000 (reference), 0.776 (0.679, 0.887), 0.784 (0.682, 0.901), and 0.697 (0.590, 0.822) for all-cause mortality (P trend <0.001); 1.00 (reference), 0.796 (0.624, 1.015), 0.776 (0.602, 1.001), and 0.673 (0.508, 0.892) for CVD mortality (P trend = 0.007); 1.00 (reference), 0.699 (0.527, 0.927), 0.714 (0.538, 0.947), and 0.712 (0.520, 0.975) for malignant neoplasm mortality (P trend = 0.028); and 1.00 (reference), 0.788 (0.605, 1.028), 0.825 (0.621, 1.097), and 0.649 (0.456, 0.926) for other-cause mortality (P trend = 0.058).
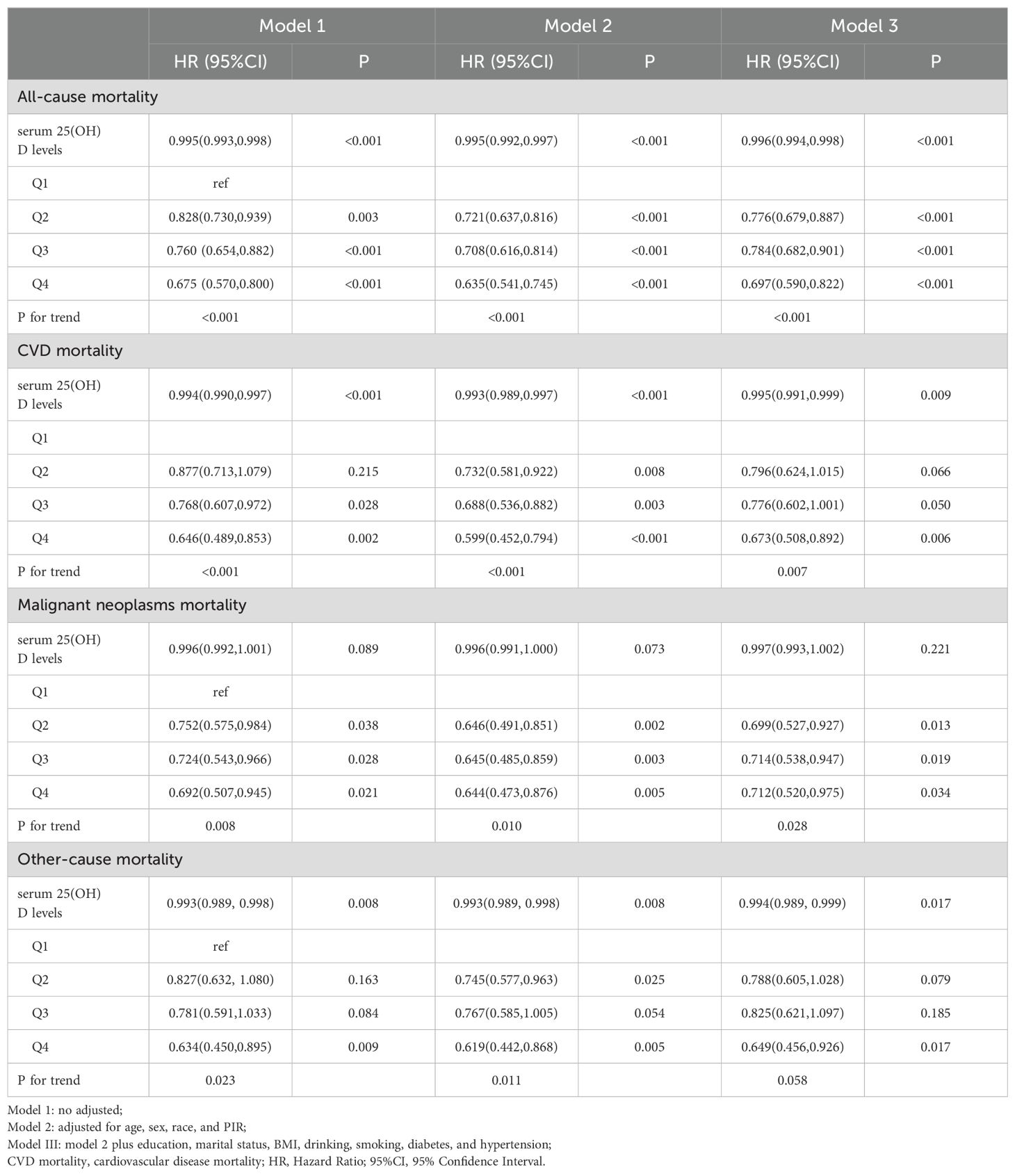
Table 3. Cox regression analysis between serum 25(OH)D levels and all-cause and cause-specific mortality.
3.3 Dose-response correlation between mortality and 25(OH)D serum levels
Figure 3 illustrates the depiction of the association between mortality and 25(OH)D serum levels using a restricted cubic spline. For all-cause mortality, a notable decrease in mortality was observed initially, followed by a stabilization effect as 25(OH)D serum levels gradually increased. The nonlinear relationship demonstrated a saturation point at approximately 67.5 nmol/L. This nonlinear pattern was similarly observed for CVD mortality, malignant neoplasm mortality, and other-cause mortality, with the saturation point consistently around 67.5 nmol/L. Table 4 provides further evidence supporting the nonlinear correlation between 25(OH)D serum levels and mortality.
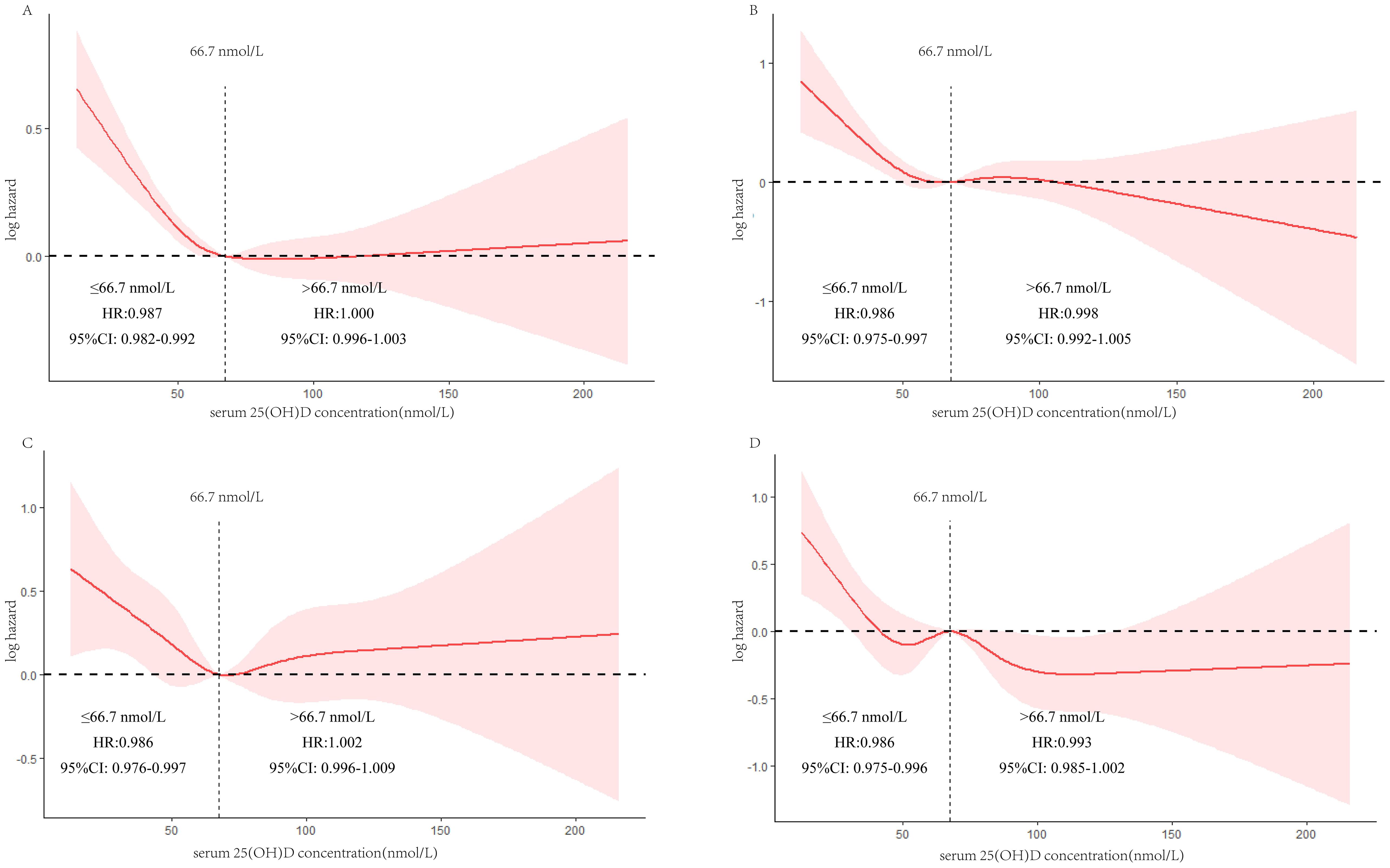
Figure 3. Restricted cubic spline showing the relationship between serum 25(OH)D levels and all-cause (A), CVD (B), malignant neoplasms (C), and other-cause (D) mortality.

Table 4. Saturation effect between serum 25(OH)D concentration and all-cause and cause-specific mortality.
3.4 Subgroup analysis of the correlation between mortality and 25(OH)D levels
Finally, to investigate the correlation between mortality and 25(OH)D serum levels in greater detail, subgroup analyses were performed on elderly individuals with hyperlipidemia, considering various characteristics. Notably, the robustness of the negative correlation between all-cause mortality and 25(OH)D serum levels was evident across different subgroups, including age, sex, alcohol consumption, hypertension, and diabetes. Interestingly, among non-obese (BMI < 30 kg/m2) and smoking elderly individuals with hyperlipidemia, this negative correlation was particularly significant (Table 5). Furthermore, robust associations were observed between 25(OH)D serum levels and mortality due to CVD or malignant neoplasms across different subgroups, including age, gender, BMI, tobacco use, alcohol consumption, high blood pressure, and diabetes (Supplementary Tables S1, S2). In the smoking population, a more pronounced negative relationship was found between other-cause mortality and 25(OH)D serum levels (Supplementary Table S3).
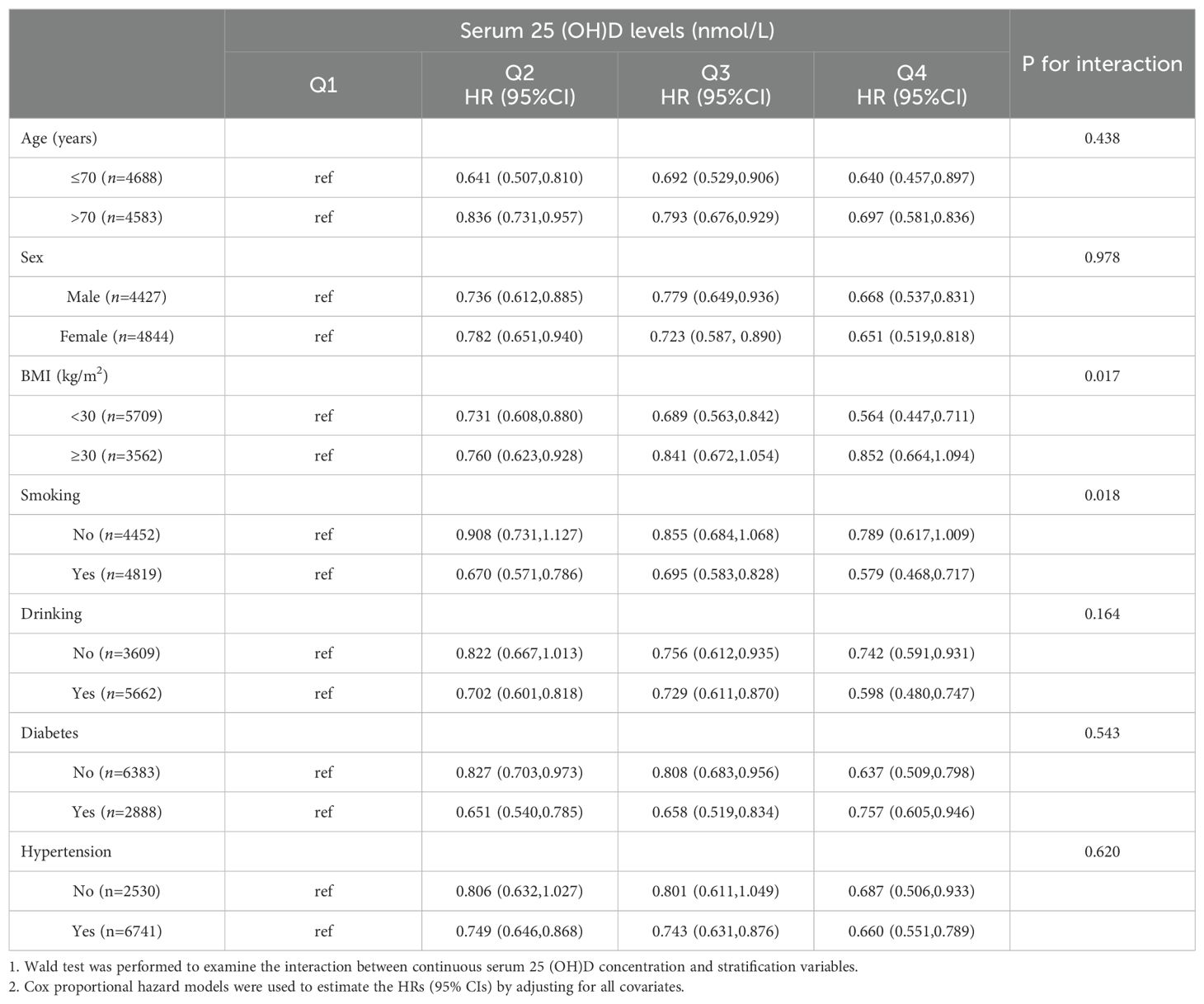
Table 5. Subgroup analysis of the associations between serum 25 (OH)D levels and all-cause mortality among elderly with hyperlipidemia.
4 Discussion
In this nationally representative cohort study, an L-shaped relationship was observed between the risk of 25(OH)D serum and the risk of cardiovascular disease (CVD), malignant neoplasms, all-cause mortality, and other-cause mortality. Specifically, an increase in 25(OH)D serum levels was associated with a decreased risk of mortality from various causes, including CVD, malignant neoplasms, and other causes. These relationships were independent of conventional risk factors such as age, lifestyle factors, BMI, diabetes, and hypertension. We visualized the correlation between 25(OH)D serum levels and different causes of mortality using restricted cubic splines and determined the optimal levels of 25(OH)D to reduce mortality rates through threshold analysis. Subgroup analysis further confirmed the consistent negative relationship between 25(OH)D serum levels and mortality. This study is the initial investigation that focuses on the correlation between 25(OH)D serum levels and cause-specific or all-cause mortality within the hyperlipidemic geriatric population.
To date, numerous studies have already established a close association between 25(OH)D serum levels and overall mortality in populations with diverse characteristics. Large-scale studies conducted on American elderly individuals have independently demonstrated a negative correlation between 25(OH)D serum levels and CVD and all-cause mortality (15). Similar findings were subsequently found in another study of a large national cohort from different regions (16–19). Subsequently, growing attention has been given to the association between 25(OH)D serum levels and mortality in populations with various characteristics. Notably, negative associations between 25(OH)D serum levels and mortality have been reported in individuals with diabetes, osteoarthritis patients, those in the prediabetic population, patients with fatty liver and metabolic dysfunction, rectal cancer patients, and individuals with severe diseases (20–27). However, studies focusing on hyperlipidemic populations remain limited.
Hyperlipidemia is a prevalent condition in modern society, which is considered the most critical risk factor for CVD, making it the primary contributor to adult mortality in the United States (28). Multiple studies have identified the associations between hyperlipidemia and CVD, including induction of oxidative stress, inflammatory cardiac fibrosis, reduced autophagy, decreased microvascular density, and altered mitochondrial function in cardiomyocytes (29, 30), which provide insights into the mechanisms underlying hyperlipidemia induced increase of CVD risk. Consequently, our study mainly focused on the elderly population with hyperlipidemia, who are known to be particularly susceptible to CVD. A retrospective research study found that increasing serum 25(OH) D concentration may help treat hyperlipidemia in vitamin D deficiency (31). In this study, a close relationship was discovered between increased levels of serum 25(OH)D and decreased CVD mortality among elderly individuals with hyperlipidemia. This effect may be attributed to the anti-inflammatory, antioxidative, and enhanced mitochondrial respiration properties of 25(OH)D (32). Apart from its well-established association with CVD, hyperlipidemia has also been linked to an elevated risk of various types of cancer (33–36), which indicates that hyperlipidemia is a risk factor for tumor development. In this study, the correlation between elevated 25 (OH)D serum levels and reduced mortality from tumors has also been discovered.
While numerous public health studies have established an association between vitamin D deficiency and increased risks of all-cause mortality and cause-specific mortality, few have guided the appropriate levels of 25(OH)D to mitigate these risks. The Endocrine Society has outlined a reliable clinical practice guideline categorizing vitamin D levels into four groups: severely deficient (<25.00 nmol/L), moderately inadequate (25.00-49.99 nmol/L), insufficient (50.00-74.99 nmol/L), and adequate (>75.00 nmol/L) (37). However, the optimal level remains controversial for several reasons. Lack of standardization of testing is the cause of this problem, and measures should be taken to overcome it. It is important to note that this classification focuses on individuals at risk of vitamin D insufficiency and does not recommend routine screening for deficiency in low-risk individuals. Considering the potential adverse effects of vitamin D deficiency on bone and overall health, especially when serum 25(OH)D levels are less than 30 nmol/L (<12 ng/mL), it may be useful to prioritize screening of at-risk populations (9). In two large cohort studies involving individuals with diabetes and prediabetes, approximately 80% of the population exhibited vitamin D deficiency. Similarly, within a Chinese cohort study of 1,834 elderly adults, only 3.7% of participants met the Endocrine Society’s recommended threshold for adequate 25(OH)D serum levels (>75 nmol/L) (38). Moreover, several studies have suggested that the current thresholds for 25(OH)D sufficiency may be too stringent for certain populations, highlighting the need for more appropriate guidelines to inform population health. In this study, participant 25(OH)D serum levels were divided into quartiles to explore their linear or nonlinear relationships with cause-specific and all-cause mortality. A nonlinear relationship was observed, and an optimal 25(OH)D level of 67.5 nmol/L was identified, providing valuable insights into the role of 25(OH)D serum levels in reducing mortality rates.
In the present study, we observed a stronger negative correlation between serum 25(OH)D levels and all-cause mortality in older adults with hyperlipidemia who had a BMI less than 30. This may be due to the fact that lower BMI indicative of better overall health and lifestyle is associated with better vitamin D status as lower body fat percentage may increase vitamin D bioavailability (39). Thus, the protective effect of vitamin D may be more pronounced in individuals with lower BMI. In addition, we found a more significant negative correlation between serum 25(OH)D levels and all-cause mortality in the smoking hyperlipidemic elderly population. This observation may be related to the increased oxidative stress and inflammation induced by smoking, biological processes that can be mitigated by the anti-inflammatory and antioxidant properties of vitamin D (40, 41). Furthermore, since smoking is a strong predictor of cardiovascular disease and vitamin D has been shown to have positive effects on cardiovascular health, including lowering blood pressure and improving endothelial function (42), this may be more pronounced in smokers.
4.1 Strengths and limitations
Our study was based on NHANES 2001-2016 data covering 9,271 hyperlipidemic elderly participants, which provided us with sufficient statistical power to detect the association between serum 25(OH)D levels and mortality. In addition, the long follow-up period of our study (mean 88.37 months) allowed us to observe more stable long-term results, increasing the reliability of our findings. Although the reported findings yield intriguing conclusions, it is important to acknowledge certain limitations within this research. Firstly, as an observational study, establishing a causal relationship is not feasible. Secondly, 25(OH)D serum levels were assessed based on a single measurement, failing to capture participants’ status consistently throughout the follow-up period. Thirdly, despite meticulous adjustment for numerous confounding factors, the presence of unmeasured or unknown residual confounders cannot be entirely ruled out. Fourthly, the investigation did not delve into the specific effects of distinct vitamin D supplements on the association between 25(OH)D levels and mortality rates. Therefore, further research is imperative to elucidate the potential role of vitamin D supplementation in this domain. Finally, it is noteworthy that African-American and Hispanic adults are more susceptible to 25(OH)D insufficiency (37), but the subgroup analysis did not account for the potential impact of race on the observed association.
5 Conclusion
Within a cohort study comprising elderly individuals with hyperlipidemia, there exists a significant independent association between higher serum levels of 25(OH)D and a decreased risk of cause-specific mortality as well as all-cause mortality.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by National Center for Health Statistics. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
GP: Conceptualization, Methodology, Software, Writing – original draft. JZ: Conceptualization, Methodology, Software, Writing – original draft. YYS: Methodology, Software, Visualization, Writing – review & editing. YHS: Data curation, Validation, Writing – review & editing. FZ: Data curation, Methodology, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2024.1382419/full#supplementary-material
References
1. Ducharme N, Radhamma R. Hyperlipidemia in the elderly. Clinics geriatric Med. (2008) 24:471–487, vi. doi: 10.1016/j.cger.2008.03.007
2. Bozkurt B, Aguilar D, Deswal A, Dunbar SB, Francis GS, Horwich T, et al. Contributory risk and management of comorbidities of hypertension, obesity, diabetes mellitus, hyperlipidemia, and metabolic syndrome in chronic heart failure: A scientific statement from the American heart association. Circulation. (2016) 134:e535–78. doi: 10.1161/CIR.0000000000000450
3. Fan D, Li L, Li Z, Zhang Y, Ma X, Wu L, et al. Effect of hyperlipidemia on the incidence of cardio-cerebrovascular events in patients with type 2 diabetes. Lipids Health Dis. (2018) 17:102. doi: 10.1186/s12944-018-0676-x
4. Chen X, Zhou M, Yan H, Chen J, Wang Y, Mo X. Association of serum total 25-hydroxy-vitamin D concentration and risk of all-cause, cardiovascular and Malignancies-specific mortality in patients with hyperlipidemia in the United States. Front Nutr. (2022) 9:971720. doi: 10.3389/fnut.2022.971720
5. Yu HH, Chen PC, Yang YH, Wang LC, Lee JH, Lin YT, et al. Statin reduces mortality and morbidity in systemic lupus erythematosus patients with hyperlipidemia: A nationwide population-based cohort study. Atherosclerosis. (2015) 243:11–8. doi: 10.1016/j.atherosclerosis.2015.08.030
6. Feng X, Zhan X, Wen Y, Peng F, Wang X, Wang N, et al. Hyperlipidemia and mortality in patients on peritoneal dialysis. BMC Nephrol. (2022) 23:342. doi: 10.1186/s12882-022-02970-w
8. Byrn MA, Sheean PM. Serum 25(OH)D and cognition: A narrative review of current evidence. Nutrients. (2019), 11(4):729. doi: 10.3390/nu11040729
9. Giustina A, Bilezikian JP, Adler RA, Banfi G, Bikle DD, Binkley NC, et al. Consensus statement on vitamin D status assessment and supplementation: whys, whens, and hows. Endocrine Rev. (2024) 45(5):625–54. doi: 10.1210/endrev/bnae009
10. Yuan C, Wang J, Zhang W, Yi H, Shu B, Li C, et al. Effects of obesity with reduced 25(OH)D levels on bone health in elderly Chinese people: a nationwide cross-sectional study. Front Immunol. (2023) 14:1162175. doi: 10.3389/fimmu.2023.1162175
11. Duan S, Lu F, Wu B, Zhang C, Nie G, Sun L, et al. Association of serum 25 (OH) vitamin D with chronic kidney disease progression in type 2 diabetes. Front Endocrinol (Lausanne). (2022) 13:929598. doi: 10.3389/fendo.2022.929598
12. Pelajo CF, Lopez-Benitez JM, Miller LC. Vitamin D and autoimmune rheumatologic disorders. Autoimmun Rev. (2010) 9:507–10. doi: 10.1016/j.autrev.2010.02.011
13. Navale SS, Mulugeta A, Zhou A, Llewellyn DJ, Hypponen E. Vitamin D and brain health: an observational and Mendelian randomization study. Am J Clin Nutr. (2022) 116:531–40. doi: 10.1093/ajcn/nqac107
14. Emerging Risk Factors Collaboration E-CVDVDSC. Estimating dose-response relationships for vitamin D with coronary heart disease, stroke, and all-cause mortality: observational and Mendelian randomisation analyses. Lancet Diabetes Endocrinol. (2024) 12(1):e2–e11. doi: 10.1016/S2213-8587(23)00287-5
15. Ginde AA, Scragg R, Schwartz RS, Camargo CA Jr. Prospective study of serum 25-hydroxyvitamin D level, cardiovascular disease mortality, and all-cause mortality in older U.S. adults. J Am Geriatr Soc. (2009) 57:1595–603. doi: 10.1111/j.1532-5415.2009.02359.x
16. Schottker B, Haug U, Schomburg L, Kohrle J, Perna L, Muller H, et al. Strong associations of 25-hydroxyvitamin D concentrations with all-cause, cardiovascular, cancer, and respiratory disease mortality in a large cohort study. Am J Clin Nutr. (2013) 97:782–93. doi: 10.3945/ajcn.112.047712
17. Virtanen JK, Nurmi T, Voutilainen S, Mursu J, Tuomainen TP. Association of serum 25-hydroxyvitamin D with the risk of death in a general older population in Finland. Eur J Nutr. (2011) 50:305–12. doi: 10.1007/s00394-010-0138-3
18. Lin SW, Chen W, Fan JH, Dawsey SM, Taylor PR, Qiao YL, et al. Prospective study of serum 25-hydroxyvitamin D concentration and mortality in a Chinese population. Am J Epidemiol. (2012) 176:1043–50. doi: 10.1093/aje/kws285
19. Park KY, Han K, Hwang HS, Park HK, Park K. Serum 25-hydroxyvitamin D concentrations are inversely associated with all-cause mortality among Koreans: a nationwide cohort study. Nutr Res. (2023) 113:49–58. doi: 10.1016/j.nutres.2023.02.008
20. Wan Z, Guo J, Pan A, Chen C, Liu L, Liu G. Association of serum 25-hydroxyvitamin D concentrations with all-cause and cause-specific mortality among individuals with diabetes. Diabetes Care. (2021) 44:350–7. doi: 10.2337/dc20-1485
21. Xiao Q, Cai B, Yin A, Huo H, Lan K, Zhou G, et al. L-shaped association of serum 25-hydroxyvitamin D concentrations with cardiovascular and all-cause mortality in individuals with osteoarthritis: results from the NHANES database prospective cohort study. BMC Med. (2022) 20:308. doi: 10.1186/s12916-022-02510-1
22. Lu Q, Wan Z, Guo J, Liu L, Pan A, Liu G. Association between serum 25-hydroxyvitamin D concentrations and mortality among adults with prediabetes. J Clin Endocrinol Metab. (2021) 106:e4039–48. doi: 10.1210/clinem/dgab402
23. Zhang P, Guo D, Xu B, Huang C, Yang S, Wang W, et al. Association of serum 25-Hydroxyvitamin D with cardiovascular outcomes and all-Cause mortality in individuals with prediabetes and diabetes: results from the UK biobank prospective cohort study. Diabetes Care. (2022) 45:1219–29. doi: 10.2337/dc21-2193
24. Zhang JJ, Yu HC, Li Y, Zhang YB, Geng TT, Lu Q, et al. Association between serum 25-hydroxy vitamin D concentrations and mortality among individuals with metabolic dysfunction-associated fatty liver disease: a prospective cohort study. Am J Clin Nutr. (2022) 116:1409–17. doi: 10.1093/ajcn/nqac260
25. Zhou J, Ge X, Fan X, Wang J, Miao L, Hang D. Associations of vitamin D status with colorectal cancer risk and survival. Int J Cancer. (2021) 149:606–14. doi: 10.1002/ijc.v149.3
26. Dai L, Liu M, Chen L. Association of serum 25-hydroxyvitamin D concentrations with all-cause and cause-specific mortality among adult patients with existing cardiovascular disease. Front Nutr. (2021) 8:740855. doi: 10.3389/fnut.2021.740855
27. Arnson Y, Gringauz I, Itzhaky D, Amital H. Vitamin D deficiency is associated with poor outcomes and increased mortality in severely ill patients. QJM. (2012) 105:633–9. doi: 10.1093/qjmed/hcs014
28. Nie Y, Luo F. Dietary fiber: an opportunity for a global control of hyperlipidemia. Oxid Med Cell Longev. (2021) 2021:5542342. doi: 10.1155/2021/5542342
29. Yao YS, Li TD, Zeng ZH. Mechanisms underlying direct actions of hyperlipidemia on myocardium: an updated review. Lipids Health Dis. (2020) 19:23. doi: 10.1186/s12944-019-1171-8
30. Lai M, Peng H, Wu X, Chen X, Wang B, Su X. IL-38 in modulating hyperlipidemia and its related cardiovascular diseases. Int Immunopharmacol. (2022) 108:108876. doi: 10.1016/j.intimp.2022.108876
31. Cheng YL, Lee TI, Chien YM, Lee TW, Chen YJ. Vitamin D level regulates serum lipids discrepantly in adults with and without dyslipidemia. Endocr Connect. (2023) 12(9):e230013. doi: 10.1530/EC-23-0013
32. Wimalawansa SJ. Vitamin D deficiency: effects on oxidative stress, epigenetics, gene regulation, and aging. Biol (Basel). (2019) 8(2):30. doi: 10.3390/biology8020030
33. Chowdhury FA, Islam MF, Prova MT, Khatun M, Sharmin I, Islam KM, et al. Association of hyperlipidemia with breast cancer in Bangladeshi women. Lipids Health Dis. (2021) 20:52. doi: 10.1186/s12944-021-01480-2
34. Shih HJ, Lin KH, Wen YC, Fan YC, Tsai PS, Huang CJ. Increased risk of bladder cancer in young adult men with hyperlipidemia: A population-based cohort study. Med (Baltimore). (2021) 100:e28125. doi: 10.1097/MD.0000000000028125
35. Islam D, Islam MS, Jesmin. Association of hypertension, hyperlipidemia, obesity, and demographic risk factors with breast cancer in Bangladeshi women. Med (Baltimore). (2022) 101:e31698. doi: 10.1097/MD.0000000000031698
36. Zhang D, Xi Y, Feng Y. Ovarian cancer risk in relation to blood lipid levels and hyperlipidemia: a systematic review and meta-analysis of observational epidemiologic studies. Eur J Cancer Prev. (2021) 30:161–70. doi: 10.1097/CEJ.0000000000000597
37. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. (2011) 96:1911–30. doi: 10.1210/jc.2011-0385
38. Jin X, Xiong S, Ju SY, Zeng Y, Yan LL, Yao Y. Serum 25-hydroxyvitamin D, albumin, and mortality among chinese older adults: A population-based longitudinal study. J Clin Endocrinol Metab. (2020) 105(8):dgaa349. doi: 10.1210/clinem/dgaa349
39. Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. (2000) 72:690–3. doi: 10.1093/ajcn/72.3.690
40. Caliri AW, Tommasi S, Besaratinia A. Relationships among smoking, oxidative stress, inflammation, macromolecular damage, and cancer. Mutat Res Rev Mutat Res. (2021) 787:108365. doi: 10.1016/j.mrrev.2021.108365
41. Chen J, Tang Z, Slominski AT, Li W, Zmijewski MA, Liu Y, et al. Vitamin D and its analogs as anticancer and anti-inflammatory agents. Eur J Med Chem. (2020) 207:112738. doi: 10.1016/j.ejmech.2020.112738
Keywords: 25(OH)D serum levels, hyperlipidemia, the elderly, mortality, NHANES
Citation: Pan G-h, Zhang J-q, Sun Y-y, Shi Y-h and Zhang F-r (2024) Saturation association between serum 25-hydroxyvitamin D levels and mortality in elderly people with hyperlipidemia: a population-based study from the NHANES (2001-2016). Front. Endocrinol. 15:1382419. doi: 10.3389/fendo.2024.1382419
Received: 05 February 2024; Accepted: 06 September 2024;
Published: 02 October 2024.
Edited by:
Andrzej Bartke, Southern Illinois University School of Medicine, United StatesReviewed by:
Sara Menotti, Vita-Salute San Raffaele University, ItalyLiyun He, Sun Yat-sen University Cancer Center (SYSUCC), China
Copyright © 2024 Pan, Zhang, Sun, Shi and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fa-rong Zhang, ZmFyb25nemhhbmdAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Guang-hui Pan
Guang-hui Pan Jun-qing Zhang
Jun-qing Zhang Yi-yan Sun
Yi-yan Sun Yue-hui Shi2
Yue-hui Shi2 Fa-rong Zhang
Fa-rong Zhang