- 1Department of Endocrinology, Air Force Medical Center, Beijing, China
- 2Department of Graduate School, China Medical University, Shenyang, China
Objective: To compare the efficacy, safety and patients’ quality of life of radiofrequency ablation (RFA) and surgery in the treatment of papillary thyroid microcarcinoma (PTMC).
Methods: MEDLINE, EMBASE, Cochrane, CNKI and other databases were searched for studies on radiofrequency ablation versus traditional surgery for PTMC up to October 2022. RevMan5.4 software was used for Meta-analysis.
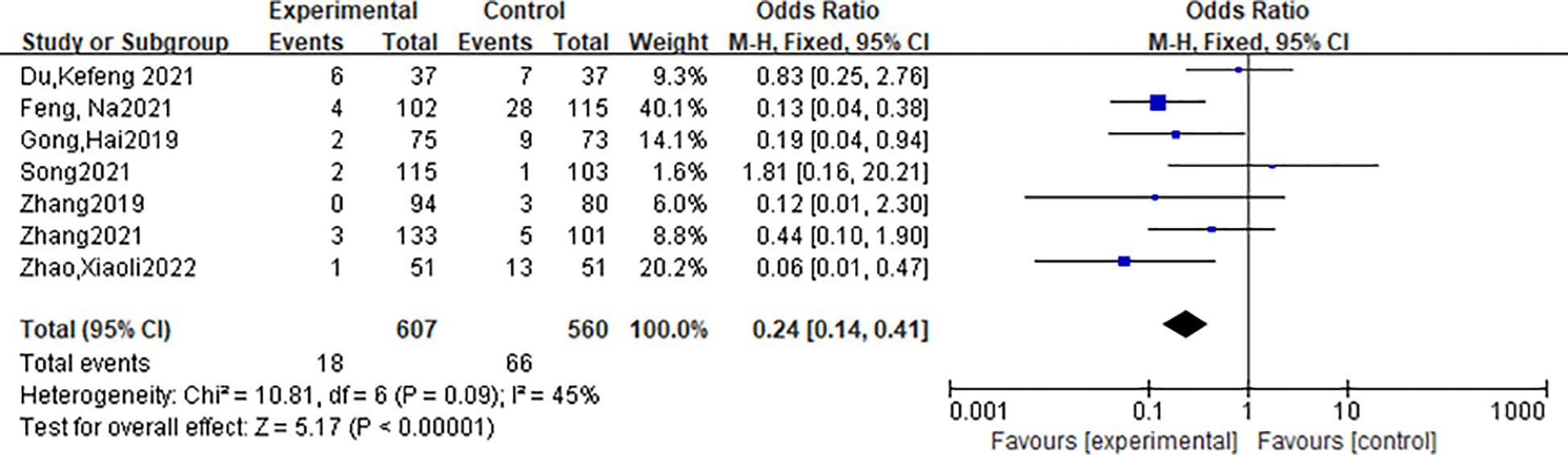
Results: 10 articles were selected from 392 articles, including 873 cases of radiofrequency ablation and 781 cases of open surgery. After meta-analysis, the incidence of postoperative complications in the radiofrequency ablation group was lower than that in the surgery group, and the difference was statistically significant [OR=0.24, 95%CI (0.14,0.41), P<0.001]. There were no significant differences in lymph node metastasis rate, local recurrence rate, and new tumor rate between the two groups [OR=1.6, 95%CI (0.21, 12.41), P>0.05; OR=0.85, 95%CI (0.05, 13.8), P>0.05; OR=0.12, 95%CI (0.01, 0.98), P>0.05]. The treatment time and hospital stay in the radiofrequency ablation group were shorter than those in the open surgery group [MD=-49.99, 95%CI (-62.02, -37.97), P<0.001; MD=-5.21, 95%CI(-7.19,-3.23),P<0.001], and the cost was significantly lower than that of the traditional surgery group [SMD=-14.97, 95%CI (-19.14, -10.81), P<0.001]. The quality of life of patients in the radiofrequency ablation group was higher than that in the surgery group [MD=-1.61, 95%CI (-2.06, -1.17), P<0.001].
Conclusion: Compared with traditional open surgery, radiofrequency ablation for papillary thyroid microcarcinoma has the advantages of less trauma, fewer complications, faster recovery and higher quality of life. The indications need to be strictly controlled in the treatment.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/, identifier (CRD42022374987).
1 Introduction
In recent years, the incidence of thyroid cancer has increased dramatically, among which the main type is papillary thyroid microcarcinoma (PTMC) with a diameter of ≤10mm. The situation in China is similar to that abroad (1). According to the Guidelines for the Diagnosis and Treatment of Thyroid Cancer (2022 Edition) (2), surgery is the preferred treatment for thyroid cancer in China, but not all patients are candidates for surgery or choose to undergo surgery. Therefore, minimally invasive treatment of thyroid microcarcinoma has attracted much attention. In this paper, the efficacy, safety and quality of life satisfaction of radiofrequency ablation and surgery were comprehensively evaluated.
2 Materials and methods
2.1 Search strategy
The study was registered in the International Prospective Register of Systematic Reviews (PROSPERO) (registration number CRD42022374987). This study searched MEDLINE, EMBASE, Cochrane, CNKI and other databases by subject headings + free words. The English search term is Thyroid Cancer, Papillary thyroid microcarcinoma, Papillary Thyroid Carcinoma, Papillary Thyroid Cancers, Radiofrequency ablation, surgery, etc. The Chinese search terms were papillary thyroid carcinoma, thyroid microcarcinoma, radiofrequency ablation, surgery, etc. The search time was up to October 2022.
2.2 Inclusion and exclusion criteria
Inclusion criteria: 1) studies on low-risk PTMC patients and 2) studies comparing treatment outcomes between thermal ablation and surgery.
Exclusion criteria: 1) case report or case series included <20 patients; 2) Letters, editorials, conference abstracts, consensus statements, guidelines, and review articles; 3) articles that do not focus on specific topics.
2.3 Data extraction and quality assessment
Two reviewers used a standard data extraction form to extract the following data from the included studies (1): study characteristics: first author’s name, publication year, study design, sample size (2); Demographic and clinical characteristics of patients: mean age, sex distribution, tumor diameter (3); Postoperative characteristics: volume reduction rate, tumor complete disappearance rate, postoperative hospital stay, perioperative cost, complication rate, operation time, recurrence rate and Thyroid Health-related Quality of Life (THYCA-QOL) (4). Postoperative complications.
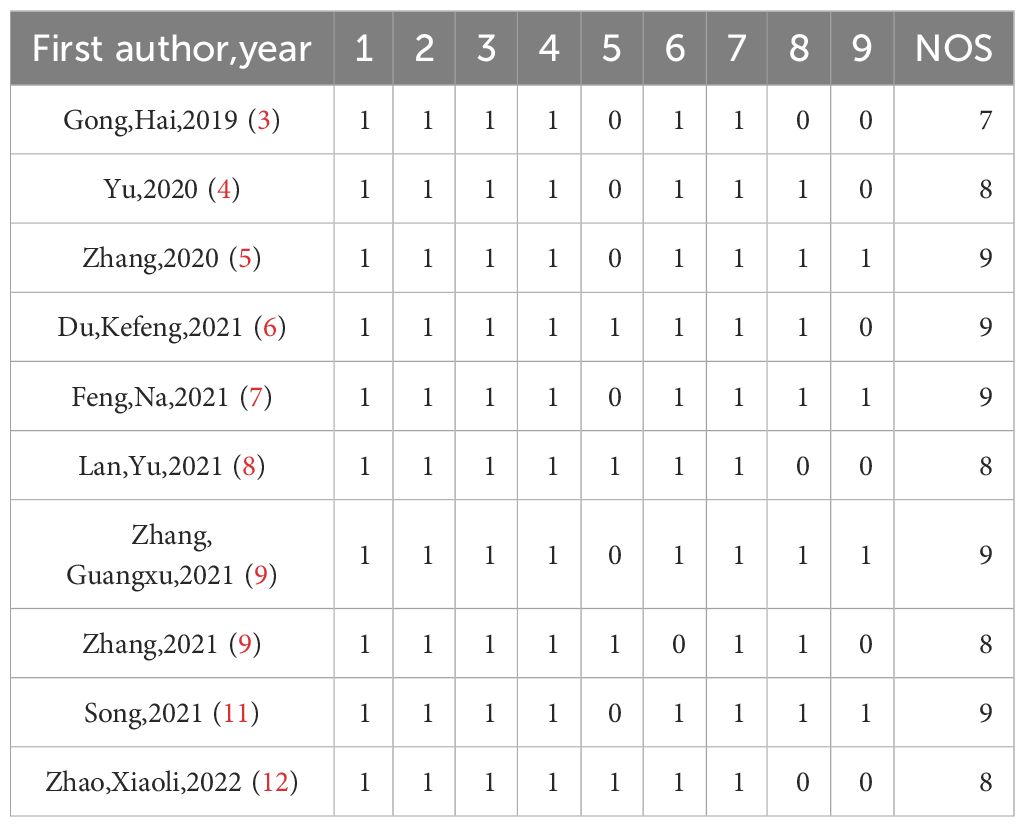
Two reviewers independently assessed the methodological quality of the included studies using the Newcastle-Ottawa Scale (NOS), and disagreements were resolved with a third reviewer. The NOS scale is suitable for evaluating case-control studies and cohort studies. It has 8 items in 3 parts to evaluate cohort studies and case-control studies. These include:
Selection:
1) Representative of exposed group (1 point)
2) Representative of the non-exposed group (1 point)
3) Identification of exposure factors (1 point)
4) Confirm the outcome indicators not to be observed at the beginning of the study (1 point)
Comparability:
1) The comparability of exposed group and non-exposed group was considered in design and statistical analysis (2 points)
Outcome:
1) Evaluation of outcome indicators (1 point)
2) Long enough follow-up time (1 point)
3) Integrity of exposed group and non-exposed group (1 point)
2.4 Statistical analysis
RevMan 5.4 software was used to analyze the indicators, and chi-square test was used to test the heterogeneity of the indicators included in the study. If the heterogeneity test was not statistically significant (I2<50%, P≥0.05), the fixed effect model was used. The count data were analyzed by Odds Ratio (OR) (95% confidence interval), and the measurement data were analyzed by Mean Difference (MD) (95% confidence interval). If the heterogeneity test showed significant heterogeneity (I2≥50%, P<0.05), then sensitivity analysis was used to find the source of heterogeneity and Meta-analysis was performed using the random effect model. P<0.05 was considered statistically significant.
3 Outcome
3.1 Results of literature search
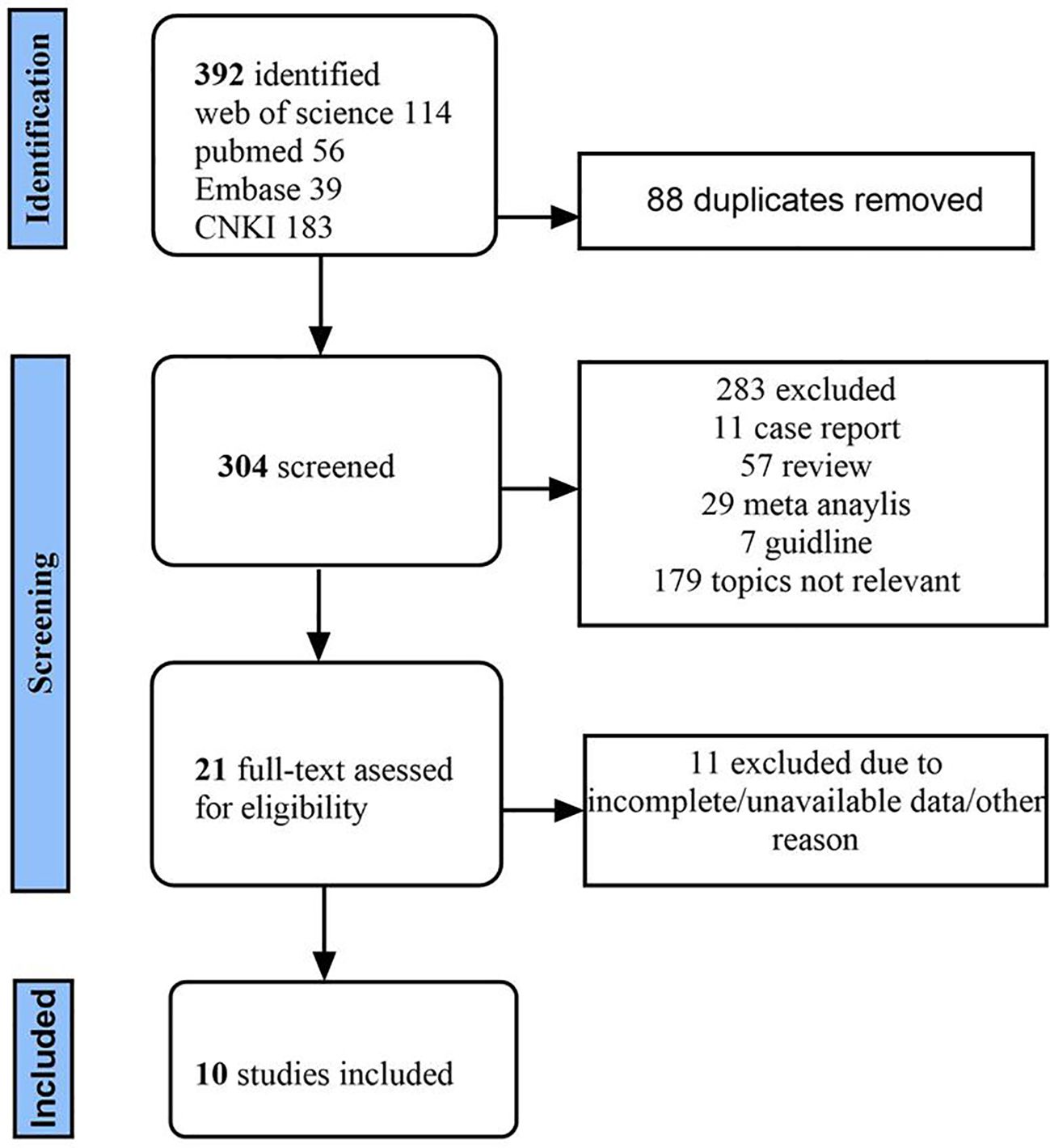
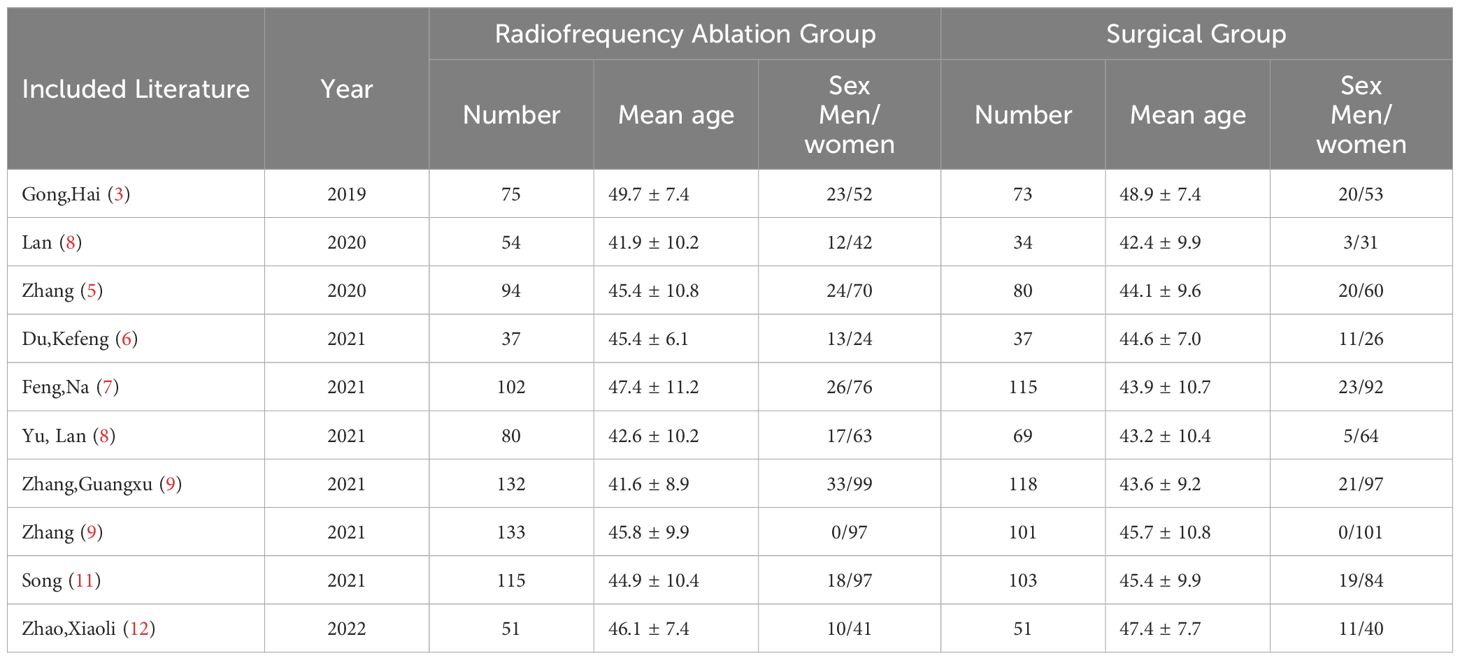
A total of 392 literatures were retrieved from the database by means of subject headings + free words, and 88 duplicate literatures were screened out. By reading titles and abstracts, 178 unrelated studies were removed, and articles such as meta-analysis, case report and guidelines were removed. Twenty-one articles were read in full, and 10 articles were finally included according to the inclusion and exclusion criteria (3–12), The screening flow chart is shown Figure 1. The basic characteristics of each included article are shown in Table 1. According to the criteria of the NOS scale, the quality of the studies was within the acceptable range, as shown in Table 2.
The surgery group included lobectomy or total thyroidectomy combined with lymph node dissection. Among them, Du Ke-feng, Feng Na and Zhao Xiao-li studied thyroid lobectomy combined with central cervical lymph node dissection (TL+CLD), and Song et al. performed total thyroidectomy combined with central cervical lymph node dissection (TT+CLD). The surgical methods of Yu Lan, Zhang2021, Zhang2020, Zhang Guangxu were determined according to ATA guidelines. The surgical group of LAN Yu et al. was divided into lobectomy group and total resection group, without mention of lymph node dissection. Gong Hai et al. did not mention the extent of surgery and the presence or absence of lymph node dissection.
3.2 Results of meta-analysis
3.2.1 Efficacy of radiofrequency ablation and tumor progression
A total of four articles reported the efficacy of radiofrequency ablation for thyroid microcarcinoma. The efficacy was evaluated by the volume reduction rate. The patients were followed up at 1, 3, 6, 12 months and every 6 months thereafter. Feng Na (7) followed up 102 patients in the radiofrequency ablation group for 12 months, and evaluated that 100% of the nodules were completely ablated without signs of recurrence or metastasis. The effective rate of the same group was 100%, and the difference was not statistically significant. Similarly, Zhang Guangxu (9) followed up 121 of 132 patients in the ablation group, and the volume of the thyroid ablation area increased significantly on the first day and 1 month after surgery, and gradually decreased in the subsequent process. At 6 months, the ablation zone had disappeared in 37 patients (30.6%). At 12 months, the ablation zone had disappeared in 75 patients (62.0%). At the latest follow-up, the ablation area of 121 patients disappeared, and the volume reduction rate was 100%. Du Kefeng (6) et al., 37 patients in the observation group, had a preoperative tumor volume of (0. 14 ± 0. 04) mm3, the tumor volume at 1 month and 3 months after surgery was (0. 27 ± 0. 13) mm3, (0. 11 ± 0. 05) mm3. The tumor volume at 6 months after operation was (0. 07 ± 0. 04) mm3, the tumor volume at 12 months after operation was (0. 01 ± 0. 01) mm3, the tumor volume before and after operation was statistically significant (F = 74. 472, P < 0. 001). The final tumor volume reduction rate in the observation group was (93. 05 ± 3. 27) %. Zhang (10) observed the volume of ablation zone in 133 cases of ablation group at each follow-up time point, and calculated the volume reduction rate. At 18 months after the last follow-up time point, the volume reduction rate was 99.98%. A number of studies and a large number of data show that radiofrequency ablation is effective in the treatment of papillary thyroid microcarcinoma, and the tumor nodules that reach or close to the surgical group disappear completely.
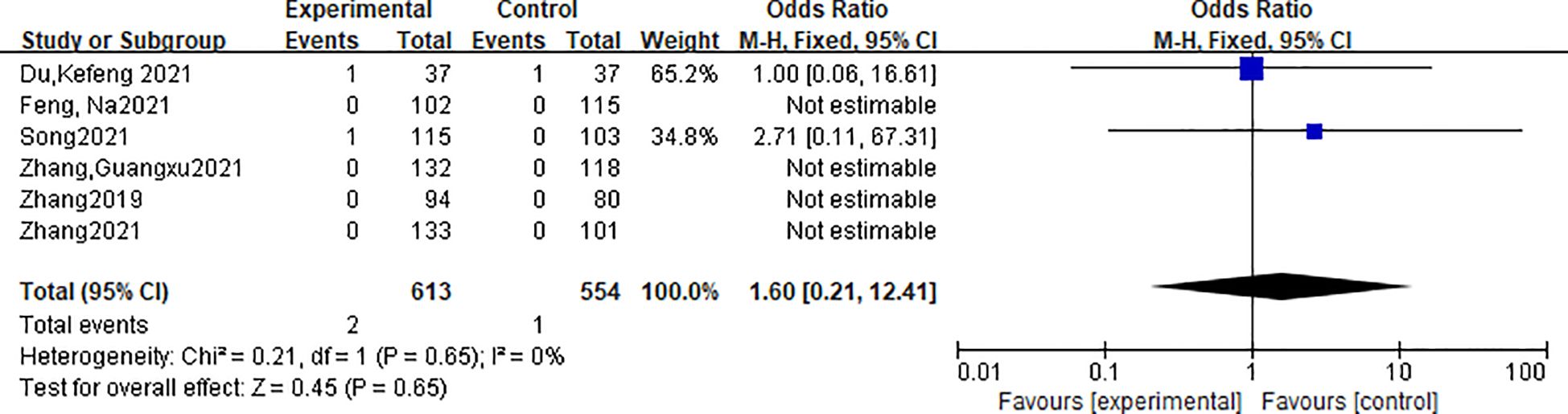
A total of 6 studies reported the local recurrence rate of tumors. A total of 1167 patients were included in the literature, including 613 patients in the radiofrequency ablation group and 554 patients in the traditional thyroid surgery group. There was no heterogeneity in the indicators of the included studies (P=0.65, I2 = 0.0%), and the fixed effect model was used for analysis. Meta-analysis showed that there was no significant difference in local recurrence rate between the radiofrequency ablation group and the traditional surgery group [OR=1.6, 95%CI (0.21, 12.41), P > 0.05]. The forest plot is shown in Figure 2.
A total of 4 studies reported the incidence of new cancer. A total of 908 patients were included in the literature, including 461 patients in the radiofrequency ablation group and 447 patients in the traditional thyroid surgery group. There was no heterogeneity in the indicators of the included studies (P=0.91, I2 = 0.0%), and the fixed effect model was used for analysis. Meta-analysis showed that there was no significant difference in the incidence of new tumors between the thermal ablation group and the conventional surgery group. [OR=0.85, 95%CI (0.05, 13.8), P > 0.05].
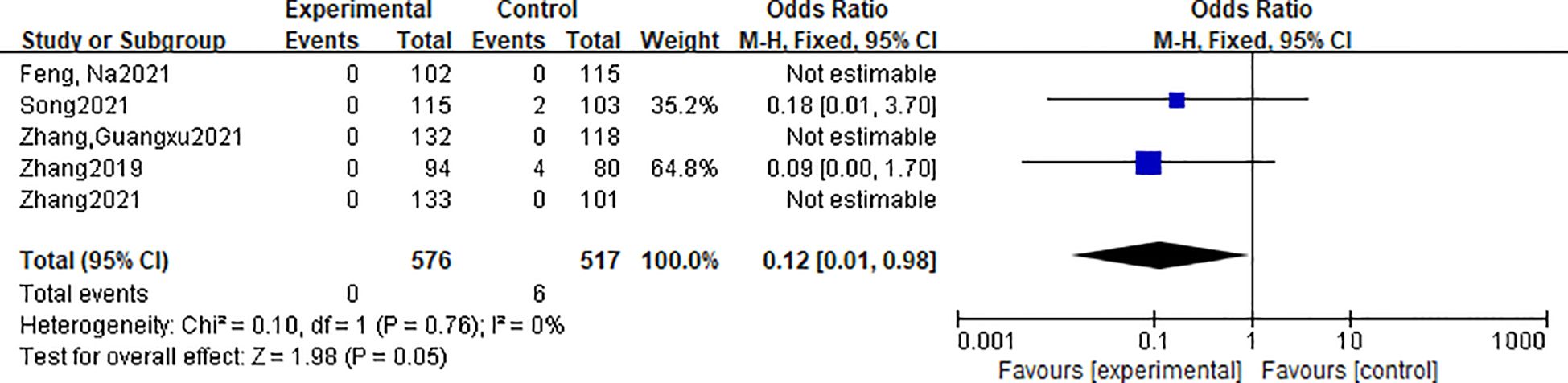
A total of 5 studies reported the lymph node metastasis rate. They indicated that the mode of follow-up and lymph node metastasis was 1, 3, 6, 9, and 12 months after surgery, with reexamination of thyroid ultrasound, and patients after 12 months after surgery were followed up every 6 to 12 months according to the patient’s condition. If suspicious nodules or lymph nodes were detected by ultrasound, aspiration cytology and thyroglobulin in the eluate were performed if necessary. A total of 1093 patients were included in the literature, including 576 patients in the radiofrequency ablation group and 517 patients in the traditional thyroid surgery group. There was no heterogeneity in the indicators of the included studies (P=0.05, I2 = 0.0%), and the fixed effect model was used for analysis. Meta-analysis showed that there was no significant difference in local recurrence rate between the thermal ablation group and the traditional surgery group [OR=0.12, 95%CI (0.01, 0.98), P > 0.05]. The forest plot is shown in Figure 3.
3.2.2 Safety comparison
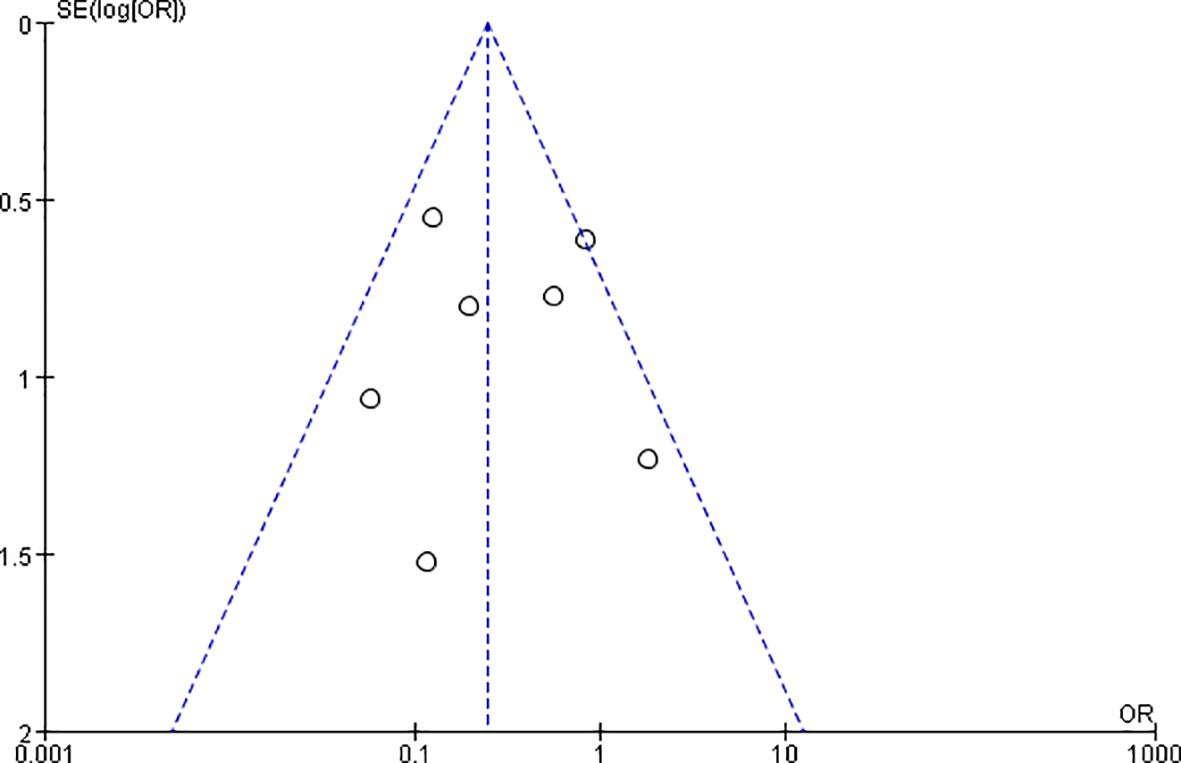
A total of 8 articles reported the postoperative complications of radiofrequency ablation and surgery group, including hoarseness, drinking cough, permanent recurrent laryngeal nerve damage, peripheral tissue damage, convulsions, incision bleeding, pain, incision infection, anesthesia vomiting, hypothyroidism, hyperthyroidism, etc. Severe complications included recurrent laryngeal nerve injury, tracheal injury, and hypoparathyroidism, while minor complications included pain, transient hoarseness, and wound infection. The impact on thyroid function was not included in the comparison, because all patients in the surgical group had permanent hypothyroidism and scar after surgery. In a study by Zhang Guangxu (9) et al., the number of patients with complications such as pain and hoarseness in the two groups was not listed. It was only reported that 1 of 132 patients in the ablation group had hypothyroidism and 3 had hyperthyroidism due to the use of Euthyroxine, while all 118 patients in the surgery group had hypothyroidism. After its removal, the heterogeneity is less than 50%, and the funnel plot is shown in Figure 4, with approximate symmetry on both sides indicating that the synthesized results are robust. The incidence of postoperative complications in the radiofrequency ablation group was lower than that in the surgery group, and the difference was statistically significant [OR=0.24,95%CI(0.14,0.41),P < 0.001].The forest plot is shown in Figure 5.
3.2.3 Comparison of time and economic benefits
A total of 5 studies reported the treatment time and postoperative hospital stay. A total of 1291 patients were included in the literature, including 481 patients in the radiofrequency ablation group and 436 patients in the traditional thyroid surgery group. There was heterogeneity in the indicators of the included studies (P < 0.001, I2 > 50%), and the random effect model was used for analysis. Meta-analysis showed that the treatment time and postoperative hospital stay in the thermal ablation group were less than those in the traditional surgery group, and the difference was statistically significant [MD=-49.99, 95%CI(-62.02, -37.97),P<0.001; MD=-5.21, 95%CI(-7.19,-3.23),P<0.001]. Four studies reported the cost of treatment. There was heterogeneity in the indicators of the included studies, and the random effect model was used for analysis. Meta-analysis showed that the treatment cost of the thermal ablation group was lower than that of the traditional surgery group, and the difference was statistically significant [SMD=-14.97, 95%CI (-19.14, -10.81), P < 0.001]. The greater heterogeneity may be related to the different hospitals and geographic locations in which treatment was performed, but the results consistently showed that radiofrequency ablation was associated with shorter hospital stay, shorter treatment duration, and lower costs than surgery.
3.2.4 Comparison of quality of life scores
A total of 4 studies reported the thyroid-specific quality of life score of tumors. The indicators of the included studies were heterogeneous (I2 = 99%). Sensitivity analysis excluded the literature with large heterogeneity of Song2021, and no heterogeneity was found. The THYQOL score of the RFA group was lower than that of the traditional surgery group, that is, the quality of life of the RFA group was higher than that of the surgery group, and the difference was statistically significant [MD=-1.61, 95%CI (-2.06, -1.17), P < 0.001]. The forest plot is shown in Figure 6.
4 Discussion
Due to the widespread use of ultrasound-guided fine needle aspiration cytology, the detection rate of primary papillary thyroid carcinoma (PTMC) is increasing, accounting for 50% of papillary thyroid carcinoma (13, 14). The World Health Organization (WHO) defines PTMC as thyroid microcarcinoma or less than 10 mm in diameter (1). The American Joint Committee on Cancer (AJCC) TNM system classifies T1 category (T; 1: ≤2 cm) were divided into T1a: ≤1 cm and T1b: ≤2 cm (15). There are three treatments for papillary thyroid microcarcinoma: follow-up, surgery, or minimally invasive thyroid surgery. Although several landmark studies have suggested that the prognosis of papillary thyroid microcarcinoma is good, even if the long-term survival rate of patients without intervention is not statistically different from that of patients with immediate surgery (13, 16, 17), the diagnosis of cancer may affect the quality of life of patients, and the majority of patients will choose intervention. Chinese guidelines for primary thyroid cancer (2)recommend surgery as the first-line treatment, and RFA can be applied as the preferred alternative for patients who are not suitable for surgery or refuse surgery. Although the curative effect of RFA is very good, it will lead to a variety of postoperative complications such as permanent hypothyroidism, recurrent laryngeal nerve injury, surgical scar and other shortcomings, as well as aesthetic impact. More and more studies have proved the safety and efficacy of RFA in PTMC (18–22). For example, One of the largest cohort studies to date found that Yan et al. followed 414 patients with single-focus PTMC for long-term tumor efficacy after RFA treatment after 42.15 ± 11.88 months (range, 24–69 months) (10). After RFA, 366 of 414 tumors (88.41%) completely disappeared, with a volume reduction rate of 98.81 ± 6.41%, indicating long-term efficacy in this large cohort (22).What’s more, a meta-analysis of three 5-year follow-up PTMC patients who underwent RFA involved 207 patients and 219 PTMCS, none of whom had local tumor recurrence, lymph node metastasis, or distant metastasis, or underwent delayed surgery during a mean follow-up of 67.8 months. Five new tumors developed in the remaining thyroid in four patients, four of which were successfully treated by repeated thermal ablation. The mean combined major complication rate was 1.2%, and no patient had life-threatening or delayed complications. The long-term safety of RFA has been demonstrated (20).
Therefore, ten studies were included in this study, and the radiofrequency ablation group was compared with the surgery group. In terms of efficacy, the tumor volume reduction rate of the radiofrequency ablation group was close to or reached 100% after a long enough follow-up, which was close to the efficacy of the surgery group. However, the concern that RFA treatment may affect tumor progression, such as lymph node metastasis, local recurrence, and increase in new tumors, occurred in a small number of cases among the thousands of cases in the literature, and the difference between the radiofrequency ablation group and the surgery group was not statistically significant. In terms of safety, the incidence of postoperative complications in the radiofrequency ablation group was lower than that in the surgery group, and the difference was statistically significant. The efficacy of radiofrequency ablation in the treatment of papillary thyroid microcarcinoma is similar to that of surgery, with low incidence of complications and good safety.
The study found that the treatment time and length of hospital stay in the radiofrequency ablation group were less than those in the surgery group, and the cost was lower, which was helpful to reduce the economic burden of disease. In terms of quality of life, this paper uses the thyroid specific Quality of Life scale score, which is an internationally used quality of life scale for thyroid cancer (23, 24). It was sinicized by Liu Jie et al., a Chinese expert (25) in 2019. It has been confirmed that it has good reliability and validity, and can be used as an assessment tool for the quality of life of Chinese thyroid cancer patients. It includes 24 questions summarized into seven symptom domains (neuromuscular, voice, attention, sympathetic symptoms, throat or mouth, psychological, and sensory problems) and six single items (scarring, feeling cold, tingling in hands or feet, weight gain, headache, and decreased libido). All items were scored on a 4-point scale (none, somewhat, fairly, very good). A higher score indicates that the patient complains more about the symptom. The results of meta-analysis showed that the THYQOL score of the RFA group was lower than that of the traditional surgery group, that is, the quality of life was higher than that of the surgery group, and the difference was statistically significant.
Our meta-analysis also has shortcomings, for example, there are few studies included in the quality of life score. In the future, we hope that more studies will focus on the quality of life of patients, rather than only the efficacy and safety of treatment, especially the proportion of women in patients with thyroid cancer is high, and the scar caused by surgery will affect the quality of life of patients. In addition, the surgical methods of the included studies were different, which would affect the study results. However, study heterogeneity is acceptable in the comparison of outcome measures. If there are more studies on the comparison of radiofrequency ablation and surgery in the treatment of PTMC in the future, the surgery group can be further divided into TT group and TL group for comparison.
In conclusion, RFA can fill the gap between surgery and follow-up in a minimally invasive manner. Radiofrequency ablation is the first choice for patients who are not suitable for surgery or refuse surgery. In addition, if more studies support the efficacy and safety of radiofrequency ablation, radiofrequency ablation may become the preferred treatment for patients with thyroid microcarcinoma in the future.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Author contributions
XK: Writing – original draft. CY: Writing – review & editing. DZ: Writing – review & editing. LW: Writing – review & editing. YS: Data curation, Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Clinical Research Program of Air Force Medical Center (Grant No. 2021LC016) and Chuying Project of Air Force Medical University (Grant No.KT2021DX005).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Tufano RP, Pace-Asciak P, Russell JO, Suárez C, Randolph GW, López F, et al. Update of radiofrequency ablation for treating benign and Malignant thyroid nodules. The future is now. Front Endocrinol (Lausanne). (2021) 12:698689. doi: 10.3389/fendo.2021.698689
2. People HCOT, #39, National sROC. National guidelines for diagnosis and treatment of thyroid cancer (2022 edition). Chin J Pract Surg. (2022) 42:1343–57+63. doi: 10.21147/J.ISSN.1000-9604.2022.03.01
3. Gong H, Liu W, Yao Z. Efficacy of ultrasound-guided microwave ablation, radiofrequency ablation and surgical resection in the treatment of papillary thyroid microcarcinoma. Chin J Cancer Clinic Rehabil. (2019) 26:781–4. doi: 10.13455/j.cnki.cjcor.2019.07.04
4. Yu L, Yukun L, Mingbo Z, Zhuang J, Jing X, Lin Y, et al. Quality of life in papillary thyroid microcarcinoma patients undergoing radiofrequency ablation or surgery: A comparative study. Front Endocrinol. (2020) 11. doi: 103389/fendo.2020.00249
5. Zhang M, Tufano RP, Russell JO, Zhang Y, Zhang Y, Qiao Z, et al. Ultrasound-guided radiofrequency ablation versus surgery for low-risk papillary thyroid microcarcinoma: results of over 5 years’ Follow-up. Thyroid. (2020) 30:408–17. doi: 10.1089/thy.2019.0147
6. Du KF, Dong G. Clinical efficacy and safety of ultrasound-guided radiofrequency ablation in the treatment of papillary thyroid microcarcinoma. Cancer Basic Clinic. (2021) 34:378–81.
7. Feng N, Huang PT, Xu D, Liping W. Comparison of radiofrequency ablation and surgery for papillary thyroid microcarcinoma. J Intervent Radiol. (2021) 30:356–60. doi: 10.21147/J.ISSN.1000-9604.2022.03.01
8. Lan Y, Zhang MB, Zhang Y, Qing S, Lin Y, Jing X, et al. Comparison of quality of life in patients with papillary thyroid microcarcinoma treated with different methods. J Chin Acad Med Sci. (2021) 43:328–37. doi: 10.3881/J.ISSN.1000-503X.1334
9. Zhang G. Efficacy comparison of ablation and surgery in the treatment of low-risk papillary thyroid microcarcinoma. Changchun: Jilin University (2021).
10. Chao Z, Jing Y, Chenlu H, Qin Y, Ping W, Pintong H. Comparison of ultrasound guided percutaneous radiofrequency ablation and open thyroidectomy in the treatment of low-risk papillary thyroid microcarcinoma: A propensity score matching study. Clin Hemorheol Microcirc. (2021) 80(20). doi: 10.3233/CH-201087
11. Song Q, Gao H, Ren L, Tian X, Lan Y, Yan L, et al. Radiofrequency ablation versus total thyroidectomy in patients with papillary thyroid microcarcinoma located in the isthmus: a retrospective cohort study. Int J Hyperthermia. (2021) 38(1). doi: 10.1080/02656736.2021.1916625
12. Zhao X, Song M. Efficacy of ultrasound-guided radiofrequency ablation and surgical resection in the treatment of papillary thyroid microcarcinoma and its influence on complications. Clin Med Res Pract. (2022) 7(17):105–7. doi: 10.19347/j.cnki.2096-1413.202217028
13. Bernardi S, Giudici F, Cesareo R, Antonelli G, Cavallaro M, Deandrea M, et al. Five-year results of radiofrequency and laser ablation of benign thyroid nodules: A multicenter study from the Italian minimally invasive treatments of the thyroid group. Thyroid. (2020) 30:1759–70. doi: 10.1089/thy.2020.0202
14. Tumino D, Grani G, Di Stefano M, Di Mauro M, Scutari M, Rago T, et al. Nodular thyroid disease in the era of precision medicine. Front Endocrinol (Lausanne). (2019) 10:907. doi: 10.3389/fendo.2019.00907
15. Perrier ND, Brierley JD, Tuttle RM. Differentiated and anaplastic thyroid carcinoma: Major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. (2018) 68:55–63. doi: 10.3322/caac.21439
16. Wells SA Jr., Asa SL, Dralle H, Elisei R, Evans DB, Gagel RF, et al. Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid. (2015) 25:567–610. doi: 10.1089/thy.2014.0335
17. Oda H, Miyauchi A, Ito Y, Yoshioka K, Nakayama A, Sasai H, et al. Incidences of unfavorable events in the management of low-risk papillary microcarcinoma of the thyroid by active surveillance versus immediate surgery. Thyroid. (2016) 26:150–5. doi: 10.1089/thy.2015.0313
18. Bernardi S, Palermo A, Grasso RF, Fabris B, Stacul F, Cesareo R. Current status and challenges of US-guided radiofrequency ablation of thyroid nodules in the long term: A systematic review. Cancers (Basel). (2021) 13. doi: 10.3390/cancers13112746
19. Ding M, Tang X, Cui D, et al. Clinical outcomes of ultrasound-guided radiofrequency ablation for the treatment of primary papillary thyroid microcarcinoma. Clin Radiol. (2019) 74:712–7. doi: 10.1016/j.crad.2019.05.012
20. Cho SJ, Baek SM, Na DG, et al. Five-year follow-up results of thermal ablation for low-risk papillary thyroid microcarcinomas: systematic review and meta-analysis. Eur Radiol. (2021) 31:6446–56. doi: 10.1007/s00330-021-07808-x
21. Van Dijk SPJ, Coerts HI, Gunput STG, et al. Assessment of radiofrequency ablation for papillary microcarcinoma of the thyroid: A systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg. (2022) 148:317–25. doi: 10.1001/jamaoto.2021.4381
22. Yan L, Lan Y, Xiao J, et al. Long-term outcomes of radiofrequency ablation for unifocal low-risk papillary thyroid microcarcinoma: a large cohort study of 414 patients. Eur Radiol. (2021) 31:685–94. doi: 10.1007/s00330-020-07128-6
23. Husson O, Haak HR, Buffart LM, et al. Health-related quality of life and disease specific symptoms in long-term thyroid cancer survivors: a study from the population-based PROFILES registry. Acta Oncol. (2013) 52:249–58. doi: 10.3109/0284186X.2012.741326
24. Rogers SN, Mepani V, Jackson S, et al. Health-related quality of life, fear of recurrence, and emotional distress in patients treated for thyroid cancer. Br J Oral Maxillofac Surg. (2017) 55:666–73. doi: 10.1016/j.bjoms.2016.09.001
Keywords: papillary thyroid microcarcinoma, radiofrequency ablation, surgery, meta-analysis, life quality
Citation: Kong X, Wang L, Sun Y, Zhu D and Yang C (2024) Comparison of radiofrequency ablation and surgery for thyroid papillary microcarcinoma: efficacy, safety and life quality. Front. Endocrinol. 15:1352503. doi: 10.3389/fendo.2024.1352503
Received: 08 December 2023; Accepted: 24 June 2024;
Published: 12 July 2024.
Edited by:
Maaike van Gerwen, Icahn School of Medicine at Mount Sinai, United StatesCopyright © 2024 Kong, Wang, Sun, Zhu and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Di Zhu, anVkeTM0ODFAMTYzLmNvbQ==; Caizhe Yang, eWFuZ2NhaXpoZTIwMDhAMTYzLmNvbQ==
 Xiaoyan Kong
Xiaoyan Kong Liangchen Wang
Liangchen Wang Yuchen Sun1,2
Yuchen Sun1,2 Di Zhu
Di Zhu Caizhe Yang
Caizhe Yang