
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol. , 21 May 2024
Sec. Clinical Diabetes
Volume 15 - 2024 | https://doi.org/10.3389/fendo.2024.1347396
 Ayoub Ali Alshaikh1
Ayoub Ali Alshaikh1 Faisal Saeed Al-Qahtani1
Faisal Saeed Al-Qahtani1 Saif Aboud M. Alqahtani2
Saif Aboud M. Alqahtani2 Ahmad Ali AlFarhan3
Ahmad Ali AlFarhan3 Ali Mushabbab Al Nuwayhidh3
Ali Mushabbab Al Nuwayhidh3 Ayman Mohammed Madkhali3
Ayman Mohammed Madkhali3 Riyad Saeed AlQahtani3
Riyad Saeed AlQahtani3 Ali Fayez AlAsmari3
Ali Fayez AlAsmari3 Abdulaziz Saeed Alserhani3
Abdulaziz Saeed Alserhani3 Hatim Ahmed Alqubaisi4
Hatim Ahmed Alqubaisi4 Ziyad Saad Saeed Aldawh3
Ziyad Saad Saeed Aldawh3 Abdulmalik Khalid Al Bin Ahmad3
Abdulmalik Khalid Al Bin Ahmad3 Ramy Mohamed Ghazy1,5*
Ramy Mohamed Ghazy1,5*Background: Self-efficacy is a popular psychological concept that refers to an individual’s perception or belief in his ability to perform specific actions. This study aimed to assess the predictive value of self-efficacy, measured using the Self-Efficacy for Managing Chronic Disease 6-Item Scale (SEM6S) questionnaire, for diabetes management and overall well-being in patients with diabetes.
Subject and methods: An anonymous online cross-sectional study was conducted to evaluate the self-efficacy of diabetic patients in the Asser region of Saudi Arabia. The participants were requested to upload their most recent glycated hemoglobin A1C (HbA1C) measurements taken in the last three months, which helped in the accurate categorization of their diabetes as either controlled or uncontrolled. We used the valid Arabic version of the SEM6S and WHO-5 well-being questionnaires to assess patient self-efficacy and well-being.
Results: A cohort of 342 patients was enrolled in the study, 67.25% were married, their mean age was 43.17 ± 17.61 years, and 52.69% had university-level or higher education. Among the participants, 46.0% exhibited well-being, while 24.9% reported poor well-being, including 9.4% who were identified as experiencing depression. The mean scores of self-efficacy and well-being were significantly higher among those with controlled diabetes versus uncontrolled diabetes (40.86 ± 13.26 vs. 36.48 ± 13.26) and (67.35 ± 21.22 vs. 60.93 ± 25.05), respectively. The predictors of glycemic control were self-efficacy [Odds ratio (OR)=1.03 (95%CI, 1.01-1.06, P=0.002], having other chronic diseases [OR=3.25 (95%CI), P<0.001], having type 1 diabetes [OR=7.16, 95%CI, P=0.005], being Saudi [OR=7.67, (95%CI, P=0.027], working in a public sector [OR=0.15, (95%CI, 0.05-0.44), P=0.005], being unemployed [OR=0.19, (95%CI, 0.06-0.59), P=0.005], being a smoker [OR=0.44, 95%CI, 0.19-0.98, P=0.048], and duration of diabetes between 6-10 years [OR= 0.33, 95%CI, 0.11-0.95), P=0.043] or more than 10 years OR=0.32, 95%CI, 0.12-0.86), P=0.026]. The main determinants of well-being were having self-efficacy [OR=1.07 (95%CI, 1.04-1.09), P = 0.0001], having public health insurance [OR=4.36 (95%CI, P=0.015], and education level (read and write) [OR=0.13 (95%CI,.02-.70), P=0.021].
Conclusions: The study reveals that non-modifiable and modifiable factors, including self-efficacy, play a crucial role in diabetes control. The study recommends providing targeted educational interventions, using different social media platforms, psychosocial support programs, and inclusive healthcare policies to improve diabetes control and mental well-being among diabetic patients.
The prevalence of diabetes mellitus (DM) in Saudi Arabia ranks second highest in the Middle East and seventh worldwide. (1) It is estimated that over 7 million people are diabetic, with nearly 3 million having pre-diabetes. (1) In Saudi Arabia, a comprehensive epidemiological health study was conducted, focusing on adults aged 30 to 70 years who live in selected households. The survey found that diabetes was diagnosed in 4,004 of the 16,917 survey participants, accounting for approximately 23.7% of the population. (2) This substantial increase, exceeding ten times in the last three decades, has led to elevated rates of mortality and morbidity, contributing to compromised health and a reduced quality of life (QoL) (1).
Self-efficacy is a popular psychology concept that refers to an individual’s perception or belief in his ability to perform specific actions. (3) Recognizing the importance of self-efficacy as a fundamental requirement for successful self-care of chronic diseases, there is growing recognition of its importance in managing DM. Self-care for diabetes encompasses a spectrum that spans from increased awareness of people living with DM to more engaged and proactive participation in the overall management process (4) Estimating self-efficacy for self-care routines in diabetic patients is a crucial step toward better diabetes control. According to self-efficacy theory, the effective completion of the action plan is more important than the plan itself. (5) Promoting a higher level of self-efficacy has been associated with improved DM self-care practices in nutrition, exercise, medication adherence, blood glucose testing, risk reduction behaviors (e.g., smoking cessation), and foot care, which leads to better glycemic control and QoL. (6) The Self-Efficacy for Managing Chronic Disease 6-Item Scale (SEM6S) is a validated, brief questionnaire designed for use in research and clinical settings. This simple assessment tool helps patients evaluate their confidence in managing chronic conditions. The questionnaire assesses one’s self-efficacy in dealing with fatigue, discomfort, pain, mental distress, and other symptoms associated with chronic disease treatment (7) Figure 1.
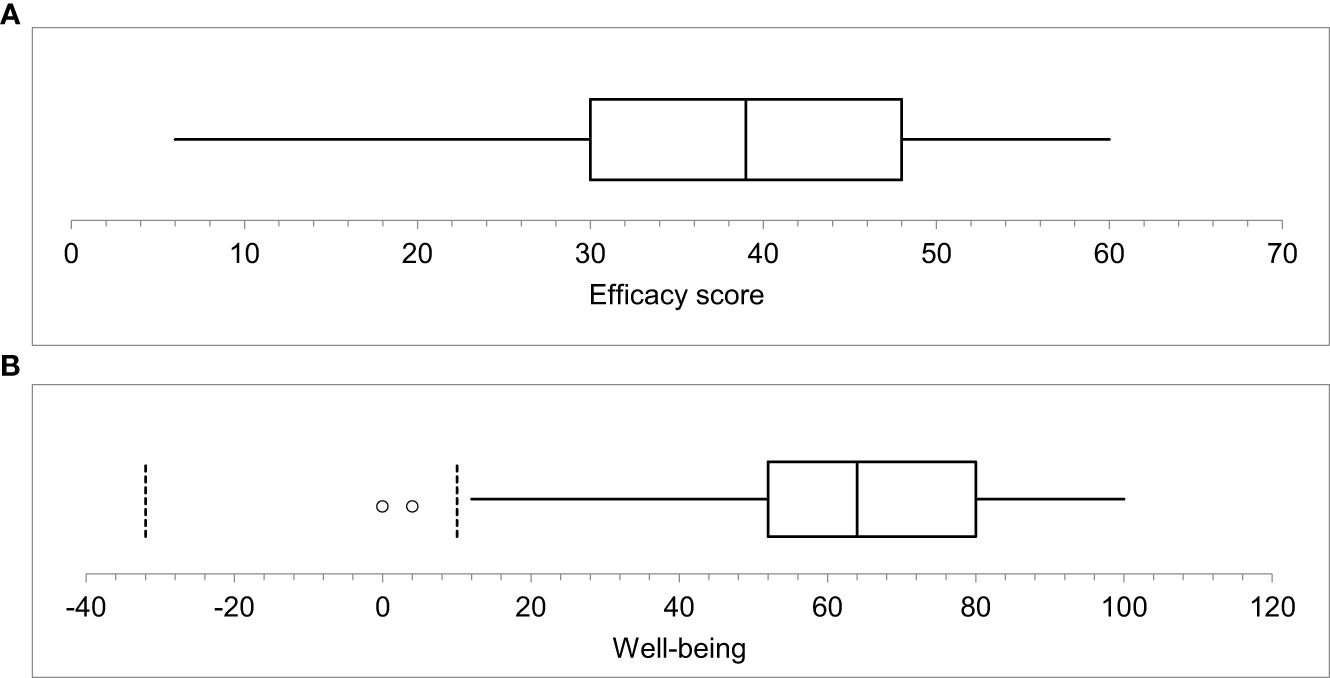
Figure 1 (A, B) show the summary statistics of the self-efficacy and wellbeing scores. The maximum score of the self-efficacy is 60, and the maximum score of wellbeing is 100. The mean of the efficacy score was 38.4 ± 13.3, the median was 390. Additionally, the wellbeing mean was 63 ± 23.1 and the median score was 64.0.
Patients with diabetes exhibit a higher prevalence of depression, estimated to be two to three times higher than that observed in the general population, thus negatively impacting both their QoL and diabetes-related outcomes. (8, 9) In light of this, routine screening for depression is recommended for diabetic patients. The World Health Organization-Five Well-Being Index (WHO-5) appears as a concise and positively framed instrument designed to evaluate emotional well-being over a 14-day span. Extensive research in adults, both with and without diabetes, using the Structured Clinical Interview for the Diagnostic and Statistical Manual (DSM)-IV as a benchmark, has demonstrated the WHO-5’s excellent sensitivity (94–100%) and specificity (78%). Due to its brevity and emphasis on positive affect, the WHO-5 holds promise as a suitable screening tool for assessing low emotional well-being and depressive tendencies in patients with diabetes (10, 11) Figure 1.
In this study, we hypothesize that higher levels of self-efficacy among patients with diabetes would be associated with better diabetes management and overall well-being. The main objective of this study was to explore the association between self-efficacy, assessed through the SEM6S questionnaire, and glycemic control in Saudi Arabian diabetic patients. Additionally, our focus expanded to evaluating the well-being of diabetic individuals and determining the role of self-efficacy as a predictor of overall well-being. This study may provide useful insights for healthcare interventions to improve the QoL for diabetic patients in Saudi Arabia.
An anonymous online cross-sectional study was used to assess self-efficacy and well-being among diabetic patients in the Asser region of Saudi Arabia. Participants were selected using convenience and snowball sampling methods. Using G*power software (version 3.1, Franz Faul, Universitat Kiel, Germany), the minimum required sample size was 210 (105 having glycated hemoglobin A1C (HbA1C) > 7%, and 105 having HbA1C ≤ 7%), presuming an effect size of 0.5, an alpha error of 5%, and a power of 95% based on a prior study, to detect a difference in self-efficacy scale of 0.98. (12) Our study included adult participants aged 18 years or older residing in the Aseer Region, Saudi Arabia, with Internet access. To accurately categorize them into controlled and uncontrolled diabetes, we requested participants to upload their most recent HbA1C laboratory result conducted within the past 3 months. Responders who were unable to provide an accurate report of their latest laboratory HbA1C result were excluded. Additionally, we excluded participants with incomplete and inconsistent data from the analysis.
Before actual data collection, data collectors were asked to collect five responses to assess the time needed to complete the questionnaire, the clarity of the language, and the response rate. The response rate was 84%, the time to complete the questionnaire ranged from 5 to 12 minutes and a few rewordings were made to improve the language of the questionnaire. The data of the pilot study was excluded from the final data set.
The study questionnaire was uploaded to Google Form and circulated through commonly used social media platforms (Instagram, Facebook, and Twitter). The study collected demographic information like age, sex, marital status, employment status, occupation, residence, nationality, education, health insurance, and monthly income. In the second section, we asked about the comorbid conditions (cardiovascular diseases, cerebrovascular diseases, and cancer). We asked about the type of diabetes (Type 1 diabetes mellitus or Type 2 diabetes mellitus). Furthermore, we collected data regarding glycemic control based on the latest HbA1c. Lastly, we asked about the disease’s duration, participants were categorized as follows: (less than 1 year, 1- 2 years, 3- 5 years, 6-10 years, and more than 10 years). (7).
To measure patient self-efficacy, we used the validated Arabic version of SEM6S. This questionnaire consists of six items, employing a 10-step Likert scale ranging from 1 (‘not at all confident’) to 10 (‘totally confident’). The maximum self-efficacy score achievable is 60. When two consecutive numbers are circled, code the lower number to reflect lower self-efficacy. The overall scale score was determined by calculating the mean score of the six items. We established the median score of all respondents as the cutoff point to categorize patients into those with or without self-efficacy. (13) If more than two items are missing, the scale should not be scored (7).
We measured the patient’s well-being using the validated Arabic version of the WHO well-being questionnaire. WHO-5 is a concise self-administered well-being measure that covers the past two weeks. Comprising five positively framed items, respondents rate their experiences on a 6-point Likert scale, ranging from 0 (at no time) to 5 (all the time). The raw scores were then transformed into a scale from 0 to 100, where lower scores signify poorer well-being. A wellbeing score equal to or less than 50 signals suboptimal mental health and prompts a need for additional exploration of potential symptoms of depression. A score of 28 or lower specifically points towards the presence of depressive symptoms (14, 15).
All collected data were numerically coded, processed using Microsoft Excel, and analyzed using Statistical Package for the Social Sciences (SPSS) version 27. Descriptive statistics were used to summarize the study variables, with percentages and frequencies for categorical data and mean and standard deviation for numerical data. The Z test was used to assess the association between SEM6S and demographic characteristics. To detect the association between glycemic control and independent variables, we performed the Chi-square test. We developed two binary logistic regression models; the first was used to identify the determinant of glycemic control. The second model was used to assess the determinants of well-being. Statistical significance was set at P < 0.05.
Participants were made fully aware of the research’s goals prior to the study’s start. Each participant was then asked for their written informed consent. The study was approved by the King Khalid University Research Ethics Committee (IRB ECM#2023-3105). The Helsinki Declaration’s tenets were strictly followed throughout the research procedure.
The initial sample comprised 410 diabetic respondents. However, we excluded the responses of 68 patients who did not upload their Hb1C test results. Nearly two-thirds of the participants were male (67.25%), 59.0% were married, and their mean age was 43.17 ± 17.61 years. Furthermore, 36.55% had income exceeding 10,000 SAR, 76.32% were not employed in the healthcare sector, and 42.69% had a university degree or higher. Furthermore, a large proportion of participants reported having diabetic relatives (70.18%) and 92.69% were aware of their type of diabetes. Over two-thirds of respondents had glycated hemoglobin levels greater than 7% (61.40%), and 54.0% had other chronic conditions. For more detailed information, refer to Table 1.
The distribution among respondents was relatively balanced, with 47.0% (n=161) exhibiting self-efficacy and 53.0% (n=181) lacking self-efficacy. Figure 2A Well-being was reported by more than three-quarters of the participants, accounting for 75.1%, while 24.9% reported poor (suboptimal) well-being, including 9.4% who were identified as experiencing depressive symptoms Figure 2B.
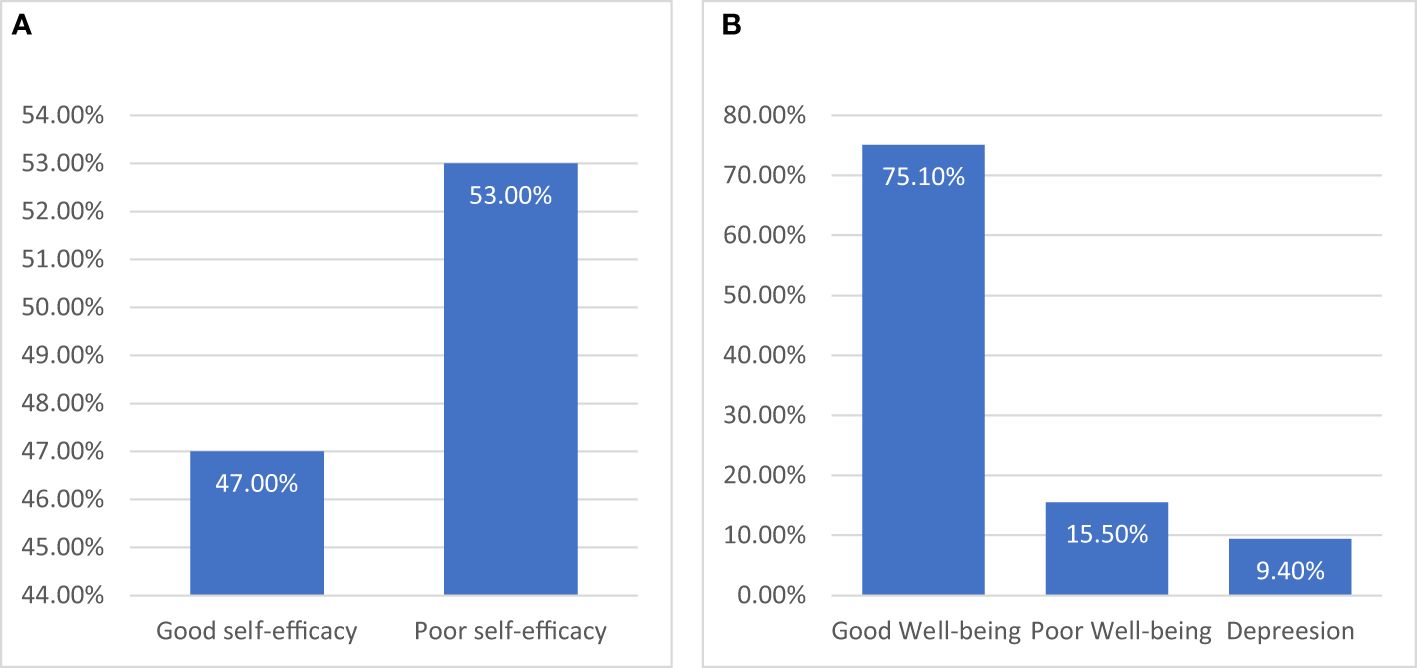
Figure 2 (A), the distribution of study participants is presented, categorized according to self-efficacy, with the median score serving as the cutoff point. (B) illustrates the distribution of participants based on their well-being score. Individuals with scores of 28 or below were classified as experiencing depression, and those with scores of 50 or below were categorized as having poor well-being.
Around 40% of males and females were controlling their diseases, no significant difference in HbA1C test results and gender (P = 0.949). Marital status had no significant differences in any control of diabetes (P = 0.996). There was no significant difference in glycemic control according to income levels (P = 0.161). Similarly, there was no significant difference in glycemic control between health and non-health workers (P = 0.559). Individuals with higher education showed significantly better glycemic control (46.7%, P = 0.018). The study found a significant difference in glycemic control based on the type of social insurance. Patients with private insurance had the highest percentage of glycemic control (P = 0.002). There was also a significant difference in glycemic control based on occupation (P = 0.009), place of residence (cities and villages) (P = 0.030), presence of other chronic diseases (P = 0.034), and self-efficacy (P = 0.011). However, no significant association was found between smoking, nationality, type of diabetes, duration of disease, having diabetic relatives, and glycemic control (P = 1.000, 0.495, 0.200, 0.156, 1.000) Table 2.
There was a statistically significant difference in the mean self-efficacy scores between the controlled and uncontrolled diabetes groups (P = 0.031). similarly, the was a statistically significant difference in mean of well-being score across the studied group (P = 0.040) Table 3.
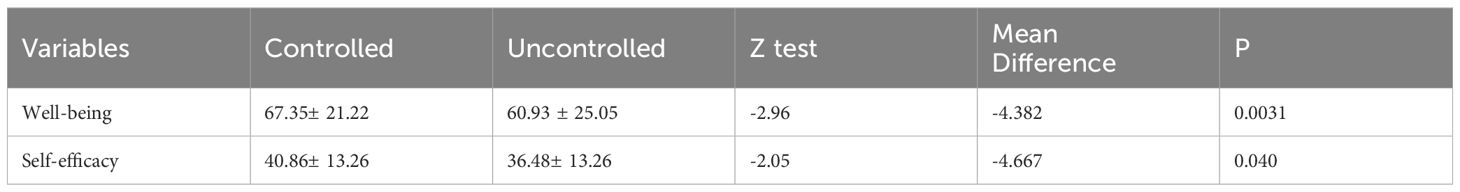
Table 3 The difference between patients with controlled and uncontrolled diabetes in wellbeing and self-efficacy.
Table 4 shows the odds of having controlled diabetes in each category with respect to the reference category. The significant categories were self-efficacy score [OR=1.03(95%CI, 1.01-1.06, P = 0.002], having self-efficacy increased the odds of controlling diabetes than the reference category by 3%. Having other chronic diseases increased the odds of having control diabetes by 3.25 times compare with the reference category [OR = 3.25 (95%CI, 1.83-5.93), P <0.001]. Type 1 diabetes increased the odds of diabetes control [OR = 7.16, 95%CI, 1.96-30.71, P = 0.005]. Finally, being of Saudi nationality improved diabetes control [OR = 7.67, (95%CI, 1.37 – 53.84), P = 0.027]. However, the duration of diabetes between 6 and 10 years, and more than 10 years, was significantly associated with lower odds of diabetes control [OR = 0.33, 95% CI, 0.11-0.95), P = 0.043] and [OR = 0.32, 95% CI, 0.12-0.86), P = 0.026], respectively. Unemployment [OR = 0.19 (95% CI, 0.06-0.59), P = 0.005], working in the public sector [OR = 0.15 (95% CI, 0.05-0.44), P = 0.005], and being a smoker [OR = 0.44, 95% CI, 0.19-0.98, P = 0.048] also decreased the odds of having controlled diabetes. Tables 4, 5 shows the odds of having well-being in each category with respect to the reference category. The predictors of well-being were self-efficacy [OR=1.07 (95%CI, 1.04-1.09), P = 0.0001], education level (read and write), [OR=0.12 (95%CI,.02-.71), P = 0.021], and having public health insurance [OR=4.36 (95%CI, 1.36- 14.89), P = 0.015].
This study focused on assessing how self-efficacy influences diabetes control, measured by evaluating HbA1c levels in the previous three months. Alongside this, we investigated the well-being of the participants, aiming to establish the predictive role of self-efficacy in determining well-being. By exploring the association between self-efficacy, diabetes control, and well-being, our goal was to contribute valuable insights that could inform strategies and interventions for improving the comprehensive health outcomes of individuals managing diabetes.
Approximately 25.0% of the respondents reported a poor well-being, 9.4% experienced depression, while 47.0% indicated self-efficacy. Factors that contributed to improved glycemic control included self-efficacy, the presence of chronic health conditions, being Saudi, and having Type 1 diabetes. On the contrary, longer durations of diabetes, working in the public sector, unemployment, and smoking were associated with lower odds of controlling diabetes. Regarding well-being, individuals with basic education (read and write) showed lower odds, whereas patients with higher self-efficacy and having public health insurance exhibited higher odd of well-being.
We found that having diabetes for a duration longer than 6 years was significantly associated with worse glycemic control. In the same vein, Juarez et al. (16) Shamshirgaran et al. (17), and Mamo et al. (18) reported that glycemic control tends to worsen with the duration of diabetes. The longer duration of diabetes, especially uncontrolled diabetes, was found to be associated with mortality from other diseases as well. (19) The poor control of diabetes with increasing diseases duration could be attributed to a decrease in insulin secretion or an elevated level of insulin resistance among those patients (20).
Notably, individuals without comorbidities exhibit significantly better glycemic control, with an OR of 3.25 compared to those with comorbid conditions. In line with our findings, several studies showed a significant association between the number of chronic conditions and glycemic control. (21, 22) The observed association between multimorbidity and improved glycemic control could be attributed to more effective healthcare management for patients with multiple chronic conditions. In simple terms, the presence of comorbidities may open opportunities for a more comprehensive treatment approach, which may help to achieve the desired level of glycemic control. However, previous research has produced inconclusive results. For example, Haghighatpanah et al. (20) found that the presence of comorbidity was comparable in people with good and bad glycemic control. We found that the Saudi population has a higher probability of managing diabetes compared to other nationalities. This may be due to ongoing intervention programs that targets general population and medical students to raise their knowledge about diabetes and obesity (23, 24) and their complications (25).
Our findings indicated a significant association between smoking and poorer glycemic control. Consistently, data from the Swedish National Diabetes Registry covering the years 1996–2001 revealed that smokers exhibited higher mean HbA1c levels compared to non-smokers. (26) Similarly, the Fukuoka Diabetes Registry findings highlighted that Japanese men with Type 2 diabetes mellitus who smoked experienced a significant increase in mean HbA1c levels compared to non-smokers. (27) Further supporting this trend, in a study involving 10,551 men with diabetes in China, smoking was associated with an elevated risk of poor glycemic control. (28) In another Chinese study, male heavy smokers with Type 2 diabetes mellitus undergoing medical treatment exhibited a mean HbA1c increase of 0.38% compared to non-smokers. (29) These collective findings underscore the consistent association between smoking and compromised glycemic outcomes across diverse populations. Smoking can potentially impact glucose regulation directly by engaging various mechanisms, including the elevation of insulin resistance, reduction in insulin secretion, or impairment of pancreatic beta cell function (30, 31).
Self-efficacy plays a significant role in the self-management of diabetes and serves as a predictor of its outcomes. In this study we found that self-efficacy was significantly associated with glycemic control in bivariate and multivariate analysis. In a similar vein, Dehghan et al. (32) revealed that self-efficacy played a noteworthy role by accounting for a considerable portion of the variability in diabetes self-care (11.4%) and influencing a significant part of the variance in behavioral intention related to diabetes self-care (31.3%). Sarkar et al. (33) found that with each 10% rise in self-efficacy score, patients demonstrated an increased probability of reporting adherence to an optimal diet, heightened involvement in exercise, and more frequent self-monitoring of blood glucose and foot care. Nevertheless, no notable association was detected with medication adherence. Moreover, a study involving 200 diabetic patients in Nigeria revealed that self-efficacy emerged as the most influential predictor associated with glycemic control, surpassing factors such as age, adherence to treatment, and engagement in physical exercise. (34) In a meta-analysis conducted by Jiang et al. (35), it was determined that educational interventions emphasizing self-efficacy are probable to reduce HbA1C levels, elevate self-efficacy, regulate self-management behaviors, improve knowledge, and ultimately contribute to an improved QoL for individuals with diabetes. Importantly, the association between self-efficacy and self-management remained consistent between different groups of race/ethnicity and levels of health literacy. (34, 36, 37). This finding addresses the importance of implementing programs to increase self-efficacy to improve glycemic control. On the contrary, Dehghan et al. (32) did not identify a significant association between self-efficacy and glycemic control among Iranians. In their study, the only significant predictor of glycemic control was the duration of the disease. Numerous studies have also indicated the absence of a link between self-efficacy and the management of metabolic syndrome (38, 39).
In this study, it was observed that the well-being of individuals with uncontrolled diabetes was significantly lower compared to those with controlled diabetes. Additionally, the study identified self-efficacy as a significant predictor of well-being, alongside the presence of health insurance and education. Similarly, Çalli and Kartal (34) found that self-efficacy was the strongest predictor of well-being. Psychological well-being indicators, such as optimism, positive affect, self-efficacy, and gratitude, have consistently been associated with better health outcomes in various medical conditions. These associations have been observed prospectively, irrespective of sociodemographic and medical factors. (33) Mental distress and depression seem to exert a significant influence on health behavior and medical outcomes, particularly among patients with diabetes (40, 41). For instance, distress is correlated with reduced treatment adherence (42), while depression is associated with compromised glucose control (43), end organs complications (43), and increased mortality (43–45).
This study has important implications for healthcare care, suggesting the need for comprehensive approaches to diabetes care. The prevalence of poor well-being highlights the importance of integrating mental health support into the management of diabetes. Factors that influence glycemic control, such as self-efficacy, age, occupation, and duration of diabetes, provide targeted areas for interventions. Tailoring education to individuals with higher odds of non-controlled diabetes and enhancing self-efficacy may improve diabetes outcomes.
This study has several strengths that contribute to the validity of its findings. The extensive nature of data collection, which includes variables ranging from demographics to self-efficacy and well-being, provides a comprehensive understanding of the factors that influence diabetes management. Furthermore, the use of validated Arabic measurement tools, such as the SEM6S and the WHO-5 questionnaire, ensures the data’s reliability and validity. Furthermore, the exclusion of respondents who were unable to accurately report the HbA1C results reduces the study’s potential bias. Despite its strengths, the study has notable limitations that should be considered. The use of convenient and snowball sampling methods may introduce selection bias, potentially limiting the generalizability of findings to the Asser region’s larger diabetic population. Furthermore, while employing an online survey is convenient, it may inadvertently exclude individuals without internet access, potentially impacting the inclusivity and representativeness of the sample. However, it’s noteworthy that a substantial segment of the Saudi population actively uses social media platforms such as TikTok, Facebook, Telegram, Snapchat, and YouTube, which could help mitigate this bias (46). The cross-sectional design restricts the study to capturing a single point in time, preventing the establishment of causal relationships. Finally, we did not ask about dietary habits, treatment regimen, and complications like frequency of hypoglycemic and hyperglycemic attacks.
This study provides valuable insights into diabetes control, shedding light on both non-modifiable and modifiable factors influencing its management. Among these factors, self-efficacy emerges as a significant determinant. Demographic factors such as sex, marital status, and income did not show significant associations with glycemic control, but non-modifiable risk factors such as nationality and modifiable risk factors such as self-efficacy, occupation, and smoking emerged as a key factor in glycemic control. The distribution of reported self-efficacy is nearly balanced among diabetic patients. A noteworthy proportion report a suboptimal well-being, shedding light on the prevalent mental health challenges within diabetic patients. To address these findings, it is recommended to implement targeted educational interventions aimed at enhancing awareness of diabetes management. These interventions can be delivered through the community-based participation approach, a method that has been proven to be economically effective in diabetes management. (47) Additionally, the use of social media platforms could serve as another effective approach to providing such services. Moreover, psychosocial support programs should be integrated to improve self-efficacy, potentially improving disease control and mental well-being. Finally, inclusive healthcare policies are essential, considering factors like smoking, occupation, nationality, and the presence of other chronic conditions. Implementing these recommendations will enable healthcare practitioners and policymakers to design more effective and tailored interventions, ultimately enhancing diabetes control and well-being in the surveyed population.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Ethical Committee of King Khalid University, Abha, Saudi Arabia (IRB ECM#2023-3005). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
AyA: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing, Funding acquisition, Supervision. FA-Q: Data curation, Writing – review & editing, Resources. SA: Resources, Investigation, Supervision, Writing – original draft. AhA: Investigation, Methodology, Software, Writing – review & editing. AMN: Data curation, Methodology, Supervision, Writing – original draft. AM: Methodology, Data curation, Supervision, Writing – review & editing. RA: Conceptualization, Investigation, Software, Writing – review & editing. AFA: Data curation, Methodology, Conceptualization, Writing – review & editing. ASA: Conceptualization, Investigation, Software, Writing – review & editing. HA: Conceptualization, Investigation, Software, Writing – original draft. ZSS: Conceptualization, Investigation, Writing – review & editing. AKA: Data curation, Methodology, Writing – original draft, Supervision. RG: Data curation, Methodology, Writing – original draft, Conceptualization, Formal analysis, Investigation, Software, Validation, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The author extends their appreciation to the Deanship of Research and Graduates studies at King Khalid University for funding this work through small under grant number group research RGP1/180/45.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Al Dawish AM, Robert AA, Braham R, Al Hayek AA, Saeed AA, Ahmed AR, et al. Diabetes mellitus in Saudi Arabia: A review of the recent literature. Curr Diabetes Rev. (2016) 12:359–68. doi: 10.2174/1573399811666150724095130
2. Alqurashi KA, Aljabri KS, Bokhari SA. Prevalence of diabetes mellitus in a Saudi community. Ann Saudi Med. (2011) 31:19–23. doi: 10.5144/0256-4947.2011.19
3. Shorey S, Lopez V. Self-efficacy in a nursing context. In: Haugan G, Eriksson M, editors. Health Promotion in Health Care – Vital Theories and Research. Springer International Publishing (2021). p. 145–58. doi: 10.1007/978-3-030-63135-2_12
4. Du S, Yuan C. Evaluation of patient self-management outcomes in health care: a systematic review. Int Nurs Rev. (2010) 57:159–67. doi: 10.1111/j.1466-7657.2009.00794.x
5. Bandura A. Health promotion by social cognitive means. Health Educ Behav. (2004) 31:143–64. doi: 10.1177/1090198104263660
6. Tan CCL, Cheng KKF, Hwang SW, Zhang N, Holroyd E, Wang W. Effect of a diabetes self-efficacy enhancing program on older adults with type 2 diabetes: a randomized controlled trial. Clin Nurs Res. (2020) 29:293–303. doi: 10.1177/1054773818792480
7. Allam MM, El-Zawawy HT, Ibrahim Ismail I, Ghazy RM. Cross-cultural reliability of an arabic version of the self-efficacy for managing chronic disease 6-item scale in Arab patients with diabetes mellitus. Primary Care Diabetes. (2020) 14:305–10. doi: 10.1016/j.pcd.2019.11.001
8. Bădescu SV, Tătaru C, Kobylinska L, Georgescu EL, Zahiu DM, Zăgrean AM, et al. The association between Diabetes mellitus and Depression. J Med Life. (2016) 9:120–5.
9. Gómez-Pimienta E, González-Castro TB, Fresan A, Juárez-Rojop IE, Martínez-López MC, Barjau-Madrigal HA, et al. Decreased quality of life in individuals with type 2 diabetes mellitus is associated with emotional distress. Int J Environ Res Public Health. (2019) 16:2652–57. doi: 10.3390/ijerph16152652
10. Löwe B, Spitzer RL, Gräfe K, Kroenke K, Quenter A, Zipfel S, et al. Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. J Affect Disord. (2004) 78:131–40.
11. Khosravi A, Mousavi SA, Chaman R, Kish MS, Ashrafi E, Khalili M, et al. Reliability and validity of the Persian version of the World Health Organization-five well-being index. Int J Health Stud. (2015), 17–9.
12. American Diabetes Association Professional Practice Committee. 6. Glycemic targets: standards of medical care in diabetes—2022. Diabetes Care. (2021) 45:S83–96. doi: 10.2337/dc22-S006
13. MacCallum RC, Zhang S, Preacher KJ, Rucker DD. On the practice of dichotomization of quantitative variables. psychol Methods. (2002) 7:19. doi: 10.1037//1082-989X.7.1.19
14. Bech P, Gudex C, Staehr Johansen K. The WHO (Ten) well-being index: validation in diabetes. Psychother psychosomatics. (1996) 65:183–90. doi: 10.1159/000289073
15. Bech P, Olsen LR, Kjoller M, Rasmussen NK. Measuring well-being rather than the absence of distress symptoms: a comparison of the SF-36 Mental Health subscale and the WHO-Five well-being scale. Int J Methods Psychiatr Res. (2003) 12:85–91. doi: 10.1002/mpr.145
16. Juarez DT, Sentell T, Tokumaru S, Goo R, Davis JW, Mau MM. Factors associated with poor glycemic control or wide glycemic variability among diabetes patients in Hawaii 2006-2009. Prev Chronic Dis. (2012) 9:120065. doi: 10.5888/pcd9.120065
17. Shamshirgaran SM, Mamaghanian A, Aliasgarzadeh A, Aiminisani N, Iranparvar-Alamdari M, Ataie J. Age differences in diabetes-related complications and glycemic control. BMC Endocrine Disord. (2017) 17:25. doi: 10.1186/s12902-017-0175-5
18. Mamo Y, Bekele F, Nigussie T, Zewudie A. Determinants of poor glycemic control among adult patients with type 2 diabetes mellitus in Jimma University Medical Center, Jimma zone, south west Ethiopia: a case control study. BMC Endocrine Disord. (2019) 19:91. doi: 10.1186/s12902-019-0421-0
19. Herrington WG, Alegre-Díaz J, Wade R, Gnatiuc L, Ramirez-Reyes R, Hill M, et al. Effect of diabetes duration and glycaemic control on 14-year cause-specific mortality in Mexican adults: a blood-based prospective cohort study. Lancet Diabetes Endocrinol. (2018) 6:455–63. doi: 10.1016/s2213-8587(18)30050-0
20. Haghighatpanah M, Nejad ASM, Haghighatpanah M, Thunga G, Mallayasamy S. Factors that correlate with poor glycemic control in type 2 diabetes mellitus patients with complications. Osong Public Health Res Perspect. (2018) 9:167–74. doi: 10.24171/j.phrp.2018.9.4.05
21. McCoy RG, Lipska KJ, Van Houten HK, Shah ND. Paradox of glycemic management: multimorbidity, glycemic control, and high-risk medication use among adults with diabetes. BMJ Open Diabetes Res Care. (2020) 8:e001007. doi: 10.1136/bmjdrc-2019-001007
22. Dinavari MF, Sanaie S, Rasouli K, Faramarzi E, Molani-Gol R. Glycemic control and associated factors among type 2 diabetes mellitus patients: a cross-sectional study of Azar cohort population. BMC Endocr Disord. (2023) 23:273. doi: 10.1186/s12902-023-01515-y
23. Alshaikh AA, Alqahtani AS, AlShehri FA, Al Hadi AM, Alqahtani MMM, Alshahrani OM, et al. Examining the impact of socioeconomic factors and lifestyle habits on obesity prevalence among male and female adolescent students in asser, Saudi Arabia. Cureus. (2023) 15:e43918. doi: 10.7759/cureus.43918
24. Mahfouz AA, Alsaleem SA, Alsaleem MA, Ghazy RM. Prevalence of Obesity and Associated Dietary Habits among Medical Students at King Khalid University, Southwestern Saudi Arabia. Medicina. (2024) 60:347. doi: 10.3390/medicina60030347
25. Alshaikh AA, Alqarni HM, Assiri HAH, Shlwan MA, AlJebreel MA, Almuaddi AS, et al. Knowledge, attitude, and practice of diabetic foot ulcer care in asser region: A cross-sectional study. Cureus. (2023) 15:e42807. doi: 10.7759/cureus.42807
26. Nilsson P, Gudbjörnsdottir S, Eliasson B, Cederholm J, Register, S. C. o. t. S. N. D. Smoking is associated with increased HbA1c values and microalbuminuria in patients with diabetes—data from the National Diabetes Register in Sweden. Diabetes Metab. (2004) 30:261–8. doi: 10.1016/S1262-3636(07)70117-9
27. Ohkuma T, Iwase M, Fujii H, Kaizu S, Ide H, Jodai T, et al. Dose-and time-dependent association of smoking and its cessation with glycemic control and insulin resistance in male patients with type 2 diabetes mellitus: the Fukuoka Diabetes Registry. PloS One. (2015) 10:e0122023. doi: 10.1371/journal.pone.0122023
28. Peng K, Chen G, Liu C, Mu Y, Ye Z, Shi L, et al. Association between smoking and glycemic control in diabetic patients: R esults from the R isk E valuation of c A ncers in C hinese diabe T ic I ndividuals: A l ON gitudinal (REACTION) study: 吸烟与糖尿病患者血糖控制的相关性研究: 来自中国 2 型糖尿病患者恶性肿瘤发生风险的纵向研究 (REACTION) 的发现. J Diabetes. (2018) 10:408–18. doi: 10.1111/1753-0407.12625
29. Lycett D, Nichols L, Ryan R, Farley A, Roalfe A, Mohammed MA, et al. The association between smoking cessation and glycaemic control in patients with type 2 diabetes: a THIN database cohort study. Lancet Diabetes Endocrinol. (2015) 3:423–30. doi: 10.1016/S2213-8587(15)00082-0
30. Śliwińska-Mossoń M, Milnerowicz H. The impact of smoking on the development of diabetes and its complications. Diabetes Vasc Dis Res. (2017) 14:265–76. doi: 10.1177/1479164117701876
31. Maddatu J, Anderson-Baucum E, Evans-Molina C. Smoking and the risk of type 2 diabetes. Transl Res. (2017) 184:101–7. doi: 10.1016/j.trsl.2017.02.004
32. Dehghan H, Charkazi A, Kouchaki GM, Zadeh BP, Dehghan BA, Matlabi M, et al. General self-efficacy and diabetes management self-efficacy of diabetic patients referred to diabetes clinic of Aq Qala, North of Iran. J Diabetes Metab Disord. (2017) 16:8. doi: 10.1186/s40200-016-0285-z
33. Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. (2006) 29:823–9. doi: 10.2337/diacare.29.04.06.dc05-1615
34. Çalli D, Kartal A. The relationship between self-efficacy of diabetes management and well-being in patients with type 2 diabetes. Nigerian J Clin Pract. (2021) 24:393–9. doi: 10.4103/njcp.njcp_280_18
35. Jiang X, Wang J, Lu Y, Jiang H, Li M. Self-efficacy-focused education in persons with diabetes: a systematic review and meta-analysis. Psychol Res Behav Manag. (2019) 12:67–79. doi: 10.2147/prbm.S192571
36. Chih A-H, Jan C-F, Shu S-G, Lue B-H. Self-efficacy affects blood sugar control among adolescents with type I diabetes mellitus. J Formosan Med Assoc. (2010) 109:503–10. doi: 10.1016/S0929-6646(10)60084-8
37. Newton KT, Ashley A. Pilot study of a web-based intervention for adolescents with type 1 diabetes. J telemedicine telecare. (2013) 19:443–9. doi: 10.1177/1357633X13512069
38. Shiu AT-Y, Choi K-c, Wong RY-M. The Chinese version of the Diabetes Empowerment Scale-short form. Patient Educ Couns. (2012) 87:258–60. doi: 10.1016/j.pec.2011.09.008
39. Survonen A, Salanterä S, Näntö-Salonen K, Sigurdardottir AK, Suhonen R. The psychosocial self-efficacy in adolescents with type 1 diabetes. Nurs Open. (2019) 6:514–25. doi: 10.1002/nop2.235
40. Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care. (2001) 24:1069–78. doi: 10.2337/diacare.24.6.1069
41. Celano CM, Beale EE, Moore SV, Wexler DJ, Huffman JC. Positive psychological characteristics in diabetes: A review. Curr Diabetes Rep. (2013) 13:917–29. doi: 10.1007/s11892-013-0430-8
42. Gonzalez JS, Shreck E, Psaros C, Safren SA. Distress and type 2 diabetes-treatment adherence: A mediating role for perceived control. Health Psychol. (2015) 34:505. doi: 10.1037/hea0000131
43. Lustman PJ, Clouse RE. Depression in diabetic patients: The relationship between mood and glycemic control. J Diabetes its Complications. (2005) 19:113–22. doi: 10.1016/j.jdiacomp.2004.01.002
44. Egede LE, Nietert PJ, Zheng D. Depression and all-cause and coronary heart disease mortality among adults with and without diabetes. Diabetes Care. (2005) 28:1339–45. doi: 10.2337/diacare.28.6.1339
45. Zhang X, Norris SL, Gregg EW, Cheng YJ, Beckles G, Kahn HS. Depressive Symptoms and Mortality among Persons with and without Diabetes. Am J Epidemiol. (2005) 161:652–60. doi: 10.1093/aje/kwi089
46. Alshaikhi OAM, Alshaikhi SA, AlZubaidi HAA, Alzubaidi MAA, Alfaqih HMH, Alrezqi AAA, et al. Social media effect on personal self-esteem among the population in Saudi Arabia. Cureus. (2023) 15. doi: 10.7759/cureus.49543
47. Farag Mohamed H, Allam MM, Hamdy NA, Ghazy RM, Emara RH. A community pharmacy-based intervention in the matrix of type 2 diabetes mellitus outcomes (CPBI-T2DM): A cluster randomized controlled trial. Clin Med Insights: Endocrinol Diabetes. (2021) 14:11795514211056307. doi: 10.1177/11795514211056307
Keywords: well-being, self-efficacy, diabetes mellitus, Saudi Arabia, diabetes control
Citation: Alshaikh AA, Al-Qahtani FS, Alqahtani SAM, AlFarhan AA, Al Nuwayhidh AM, Madkhali AM, AlQahtani RS, AlAsmari AF, Alserhani AS, Alqubaisi HA, Saeed Aldawh ZS, Al Bin Ahmad AK and Ghazy RM (2024) Exploring the self-efficacy of patients with diabetes: its role as a predictor of diabetes management and well-being. Front. Endocrinol. 15:1347396. doi: 10.3389/fendo.2024.1347396
Received: 30 November 2023; Accepted: 22 April 2024;
Published: 21 May 2024.
Edited by:
Baojuan Ye, Jiangxi Normal University, ChinaReviewed by:
Triantafyllos Didangelos, University General Hospital of Thessaloniki AHEPA, GreeceCopyright © 2024 Alshaikh, Al-Qahtani, Alqahtani, AlFarhan, Al Nuwayhidh, Madkhali, AlQahtani, AlAsmari, Alserhani, Alqubaisi, Saeed Aldawh, Al Bin Ahmad and Ghazy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ramy Mohamed Ghazy, cmFteV9naGF6eUBhbGV4dS5lZHUuZWc=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.