
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Endocrinol. , 03 April 2024
Sec. Bone Research
Volume 15 - 2024 | https://doi.org/10.3389/fendo.2024.1320468
This article is part of the Research Topic Organ System Crosstalk in Degenerative Musculoskeletal Diseases View all 11 articles
 Mobin Azami1
Mobin Azami1 Asra Moradkhani1
Asra Moradkhani1 Maryam Afraie2
Maryam Afraie2 Lotfolah Saed3
Lotfolah Saed3 Mohammad Amin Tapak1
Mohammad Amin Tapak1 Kimya Khoramipoor1
Kimya Khoramipoor1 Sorour Khateri4*
Sorour Khateri4* Yousef Moradi5*
Yousef Moradi5*Background: Despite the fact that DM patients are living longer, research on the prevalence of MSDs and other related illnesses is still lacking compared to that of other comorbidities. This study systematically reviewed and meta-analyzed cohort studies to determine the association between diabetes mellitus (DM) and musculoskeletal disorders (MSDs).
Methods: A comprehensive search of international databases, including Medline (PubMed), Web of Science, Scopus, and Embase, was conducted up to June 2023 to identify relevant studies investigating the association between MSDs and DM.
Results: The meta-analysis included ten cohort studies with a total of 308,445 participants. The pooled risk ratio (RR) estimate for the association between MSDs and DM was 1.03 (95% CI 1.00-1.06). Based on subgroup analysis, the association between longer duration (more than 7), European, below the age of 70, and female patients was higher than the others.
Conclusion: In conclusion, the results of this meta-analysis suggest that there may be an association between MSDs and diabetes in people with diabetes. These findings add to the existing knowledge on this topic and highlight the importance of recognition and management of MSDs in people with DM. There is a need for further research to investigate the underlying mechanisms and to develop targeted interventions for the prevention and management of MSDs in this population.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=381787, identifier CRD42022381787.
Diabetes mellitus (DM) is a chronic disorder defined as persistent hyperglycemia (1). The prevalence of DM in 2011 was 366 million worldwide, which will rise to 552 million by 2030 (2). DM is associated with a range of complications, including both microvascular and macrovascular conditions. Microvascular complications of DM involve damage to the small blood vessels, particularly in the eyes (retinopathy) and nerves (neuropathy). Retinopathy can lead to vision impairment or even blindness, while neuropathy can result in numbness, tingling, or pain in the extremities. In severe cases, it may lead to foot ulcers or amputation. On the other hand, macrovascular complications of DM are related to large blood vessels and can affect various organs. Ischemic heart disease, in which blood flow to the heart muscles is reduced, and stroke, in which blood flow to the brain is interrupted, are two of the most common macrovascular problems that can happen because of DM. These conditions increase the risk of heart attacks and strokes in individuals with diabetes. Both microvascular and macrovascular complications contribute significantly to the morbidity and mortality associated with DM. Therefore, managing and preventing these complications are essential aspects of diabetes care and require comprehensive strategies targeting blood glucose control, blood pressure management, lipid control, and lifestyle modifications (3). Signs of MSDs associated with DM include muscle pain, joint pain or stiffness, reduced joint mobility, joint swelling, deformities, and a sensation of pins and needles in the arms or legs. Some MSDs are unique to individuals with diabetes. These complications significantly impact the quality of life and life expectancy of diabetic patients. Despite the increasing life expectancy of DM patients due to the availability of new antidiabetic drugs, the prevalence of MSDs and related disorders remains understudied compared to other complications (4–7).
The exact mechanism of MSDs in DM is unclear, but changes in collagen deposition and progressive non-enzymatic glycosylation in the connective tissue may be the cause (8, 9). MS complications affect different parts of the body. Soft tissue disorders such as cheiroarthropathy, carpal tunnel syndrome, trigger finger, Dupuytren’s contracture, and frozen shoulder can occur. Charcot arthropathy and gouty arthritis are examples of joint disease in people with diabetes. Bone involvement, such as osteoporotic and non-osteoporotic fractures and idiopathic skeletal hyperostosis, is seen (10, 11). Different places in patients with DM, such as the wrist, neck, spine, and knee, are involved (12). Diabetes duration, glucose level control, sex, and age are some risk factors for musculoskeletal complications (13, 14). Various studies, such as case-control or cohort studies, have been conducted around the world, but the results of these studies are controversial. This condition has implications for clinical and public health decision-making worldwide, particularly in developing countries. Determining the exact association between DM and MSDs may help clinicians and specialists reduce the impact and improve the quality of life of people with DM. As well as the results of this meta-analysis help develop and update clinical guidelines and improve evidence-based medicine (EBM) knowledge and policy in this field. Also, based on this information and the results of previous studies, DM is associated with musculoskeletal disorders (MSDs) and is often clinically underdiagnosed and undertreated. There have also been no systematic reviews of the literature to determine the association between DM and MSDs in the general population. Therefore, this study aimed to review systematically and meta-analyses the association between DM and MSDs by combining cohort studies.
This systematic review and meta-analysis were based on the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) (15). The study protocol was registered in PROSPER with the code CRD42022381787 (https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=381787).
A comprehensive search strategy was used to identify relevant trials for this meta-analysis. International databases, including Scopus, Web of Science, PubMed (Medline), and Embase, were searched using specific search terms and MeSH terms for ‘diabetes mellitus’ and ‘musculoskeletal disorders’. Supplementary Table 1 provides detailed information on the systematic search. The search strategy for this meta-analysis covered the period up to July 2023. To ensure a comprehensive search, synonyms, and additional terms were included by reviewing other studies in the field. The first ten pages of Google Scholar were also searched, and related articles were selected. In addition, a manual search was conducted by reviewing the references to relevant articles. The collected articles were managed using Endnote software version 9. Duplicate articles were identified and removed based on the software’s default settings. Considering the predefined inclusion criteria, the remaining articles were evaluated based on their title, abstract, and full text. Two authors (MA and AM) independently and separately screened the articles based on their titles, abstracts, and full text. In cases of disagreement, the supervisor (YM) reviewed the results to reach a consensus.
In this meta-analysis, we specifically included cohort studies that examined the association between DM and the occurrence of MSDs. The PECO structure was used to define the inclusion criteria:
Population: All patients with DM.
Exposure: Presence of MSDs.
Comparison: DM patients without MSDs.
Outcomes: Occurrence of MSDs and associated risk factors.
Cohort studies were selected for this meta-analysis because they can investigate causal associations in observational research. To maintain the focus on relevant studies, we excluded review articles, case reports, case series, clinical trials, other interventional studies, and letters to the editor. This exclusion criterion ensured that the included studies were cohort designs explicitly examining the relationship between DM and MSDs. By employing these inclusion and exclusion criteria, we aimed to conduct a meta-analysis using cohort studies to provide valuable insights into the association between DM and the occurrence of MSDs and their related risk factors.
A checklist was developed to guide the data extraction process for this meta-analysis. The checklist included the first author’s name, country where the study was conducted, type of study (cohort study), study population, sample size, race/ethnicity of the study population, type of diabetes mellitus (DM), age of participants (mean and dispersion, if available), gender distribution (number of males), duration of DM, HbA1c levels, site(s) of involvement, type of MSDs, effect size (RR). Based on the checklist, two authors (MA and AM) independently performed the data extraction process. In cases where conflicts or disagreements arose, a third person (YM) was involved to resolve them and reach a consensus. This systematic data extraction approach collected the relevant information from each included study consistently and comprehensively, ensuring accuracy and minimizing bias in the subsequent analysis.
Two authors (MA and YM) assessed the quality of the included studies using the Joanna Briggs Institute (JBI) checklist for cohort and case-control studies. The JBI checklist is a validated tool that assesses the methodological quality of studies and the potential for bias in their design, conduct, and analysis. The JBI checklist consists of eleven cohort and ten case-control study questions. Each question is answered with ‘yes,’ ‘no,’ ‘not applicable,’ or ‘unclear’ to indicate whether the study adequately addressed the specific methodological criteria. Assessing the studies using the JBI checklist helped the authors determine the quality of the studies and decide whether to include or exclude them based on their quality assessment. It is worth noting that the JBI checklist has undergone extensive peer review and has been endorsed by the JBI Scientific Committee, further validating its usefulness for assessing the methodological quality of research studies (16, 17).
The effect size in this meta-analysis was based on the risk ratio (RR) with a 95% confidence interval. Meta-set commands were used to assess the logarithm and log standard deviation of the RR. Cochrane I2 and Q tests were used to assess heterogeneity between trials. The Egger test was used to calculate publication bias. Subgroup analyses were performed based on the duration of DM, continent, fracture site, type of MSDs, age, and sex. Meta-regression analysis was also performed to determine the effect of age and BMI on the association of interest. Statistical analysis was performed using STATA 17.0, and a P value < 0.05 was considered.
Based on the completion of the international database search, 4,095 studies were retrieved from PubMed, Scopus, Web of Science, and Embase databases. Following the removal of 538 duplicate studies, 3,557 studies remained. Subsequently, a screening process based on titles and abstracts resulted in 37 studies that met the eligibility criteria. Finally, after a thorough review of the full texts and consideration of inclusion and exclusion criteria, ten studies were included in our meta-analysis (Figure 1). The characteristics of the studies included in this meta-analysis have been reported in Table 1.
The present meta-analysis included 10 cohort studies comprising 69,979 patients with diabetes mellitus (DM) and 236,435 healthy controls. These studies aimed to assess the association between diabetes and MSDs. Gue et al. reported the highest RR of 1.26 (95% CI 1.05–1.51), while Schwartz et al. reported the lowest RR of 0.69 (95% CI 0.62–0.76). Upon combining these findings, the pooled RR estimate was 1.03 (95% CI 1.00–1.06), as depicted in Figure 2. The analysis revealed a substantial heterogeneity rate of 91.31 percent. Furthermore, an evaluation of publication bias in the included studies was conducted. The funnel plot showed significant publication bias across studies. However, the Egger's test results did not (B=-4.31; SE=3.645; P value=0.237), as shown in Figure 2.
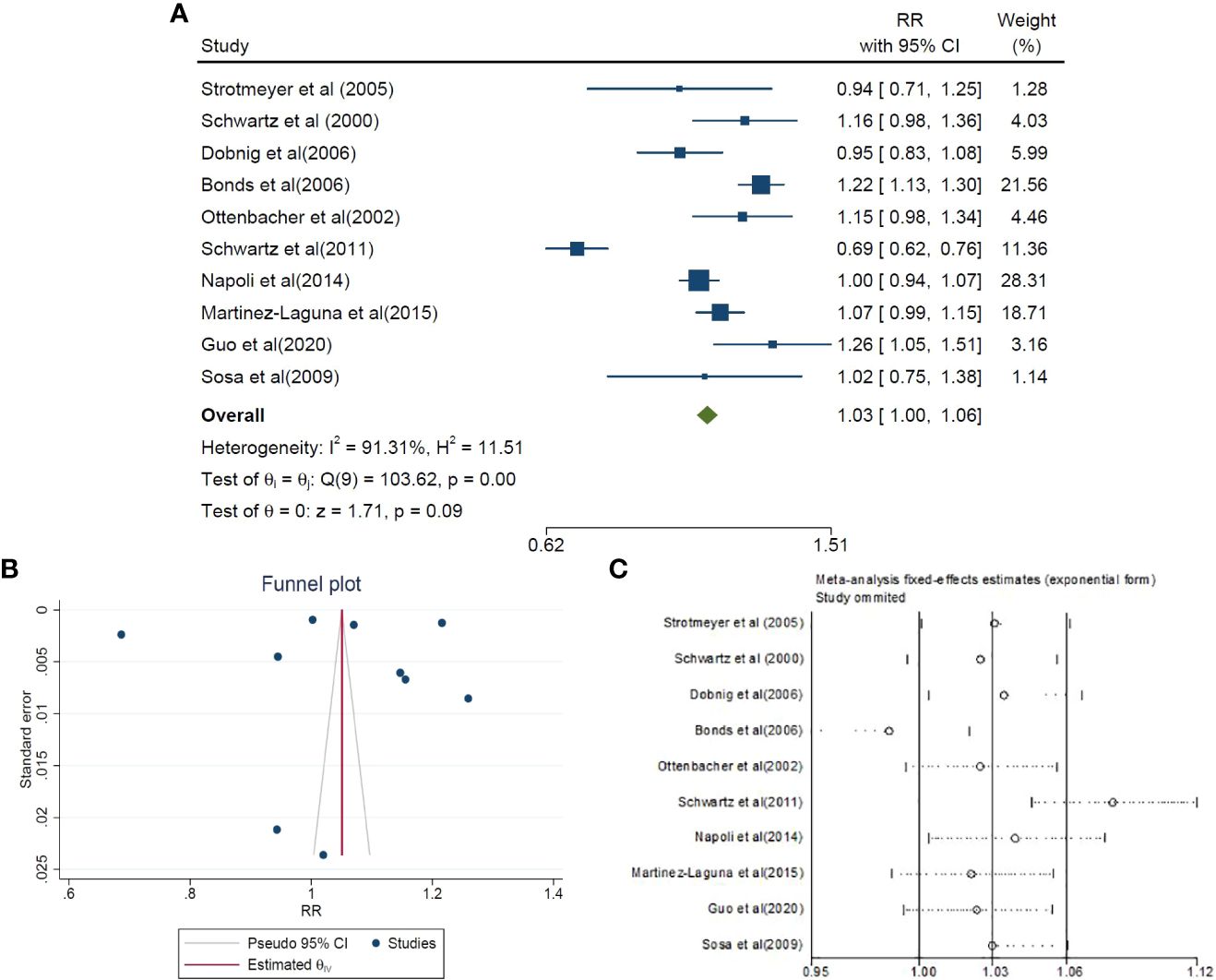
Figure 2 The risk ratio (RR) between DM and MSDs, (A: forest plot) sensitivity analysis (C) and publication bias (B) using a combination of the results of cohort studies (CI, Confidence Interval).
Additionally, a subgroup analysis was performed in our study, considering various factors such as the duration of DM, continent, place of fracture, type of musculoskeletal disorder, age, and sex. The results of this subgroup analysis are summarized in Table 2.
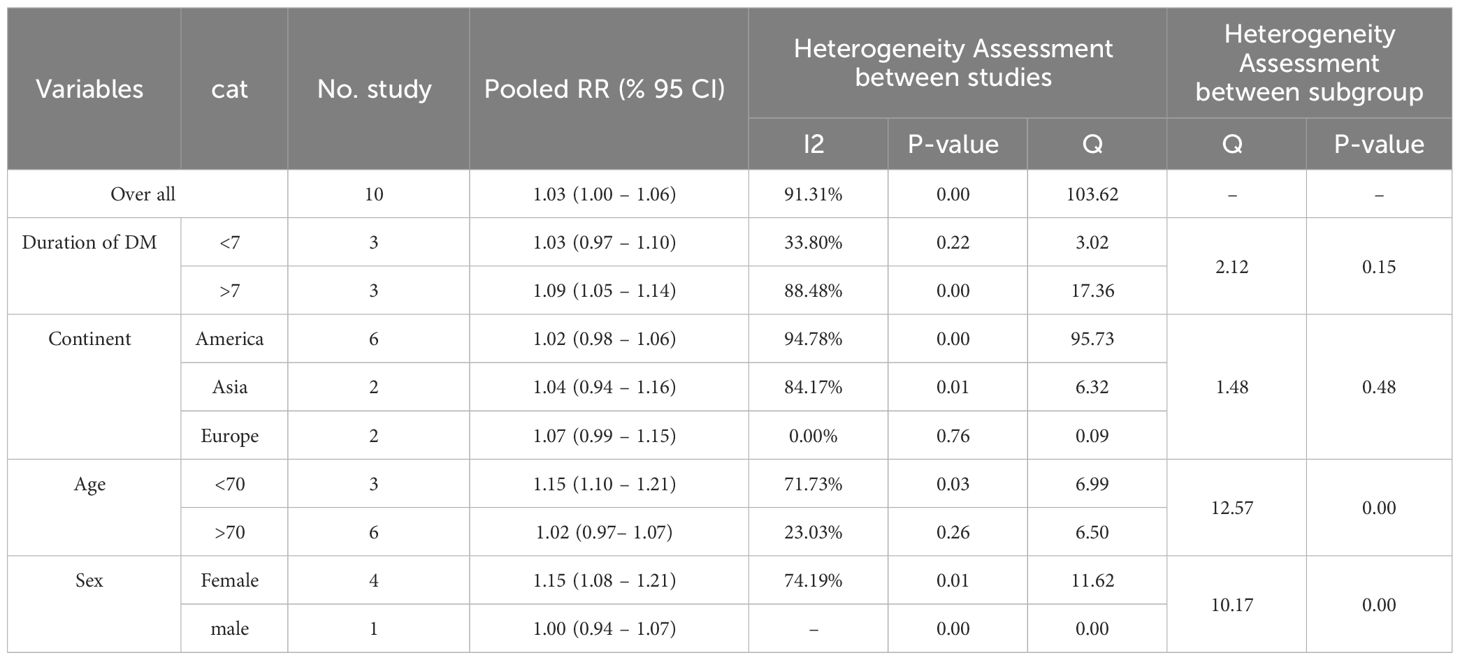
Table 2 The subgroups analysis of association between DM and MSDs by combining cohort studies based on duration of DM, continents, age, and gender.
We divided the studies into two categories: more than seven years and less than seven years. Six trials were assessed, and each group contained three trials. In the more than seven-years group, the pooled estimate of RR was 1.09 (95% CI 1.05-1.14), but in the less than seven-years group, it was 1.03 (95% CI 0.97-1.10; P-value=0.00, 0.22) with heterogeneity (I2) of 88.48% and 33.80%, respectively (Table 2).
Studies have been conducted on three continents: six in America, two in Asia, and two in Europe. Our findings revealed that the combined RR estimate was 1.02 (95% CI 0.98–1.06; P-value=0.00) in America, 1.04 (95% CI 0.94–1.16; P-value=0.01) in Asia, and 1.07 (95% CI 0.99–1.15; P-value=0.76) in Europe, accompanied by heterogeneity (I2) rates of 94.78%, 84.17%, and 0.00% respectively. Notably, the risk of MSDs in patients with diabetes mellitus (DM) was found to be higher in Europe compared to America. At the same time, no significant association was observed in Asia (Table 2).
We categorized the studies based on age, specifically comparing those below 70 with those above it. Three articles were analyzed for the lower age group, revealing a pooled RR estimate of 1.15 (95% CI 1.10–1.21; P-value=0.03, I2 = 71.73%). However, in the higher age group comprising six articles, the pooled RR estimate was 1.02 (95% CI 0.97–1.07; P-value=0.26, I2 = 23.03%). These findings indicate that the risk of MSDs is higher in individuals below the age of 70 (Table 2).
Furthermore, we observed differences based on sex. Four studies were included in the analysis of the pooled RR estimate for females, resulting in a value of 1.15 (95% CI 1.08–1.21; P-value=0.01). Conversely, only one study evaluated the RR for males, which was 1.00 (95% CI 0.94–1.07) (Table 2).
Among the articles that examined fractures, they were categorized into four groups based on the specific location. Six of these articles specifically investigated hip, pelvis, and upper leg fractures, resulting in a pooled RR estimate of 1.53 (95% CI 1.42–1.65). No significant differences were observed in other locations (Table 3). In six of the articles, the focus was specifically on hip disorders. The study by Dobing et al. reported the lowest RR of 1.07 (95% CI 0.79-1.45), whereas the study by Schwartz et al. reported the highest RR of 2.01 (95% CI 1.79-2.25). The pooled RR estimate for hip involvement was 1.53 (95% CI 1.42–1.65; P-value=0.00, I2 = 88.73%) (Table 3). In addition to these results, 2 studies reported the outcomes of interest based on the inclusion criteria for arm/wrist/hand fracture and 2 studies also reported lower leg/ankle/knee fracture. After combining these results, the meta-analysis showed that the association between the presence of diabetes and arm/wrist/hand fracture was 0.96 (% 95 CI 0.83 - 1.10) and for lower leg/ankle/knee fracture was 1.22 (% 95 CI 1.07 - 1.38). Similarly, the association between diabetes and foot fracture was 1.28 (% 95 CI 1.11 - 1.48) (Table 3).
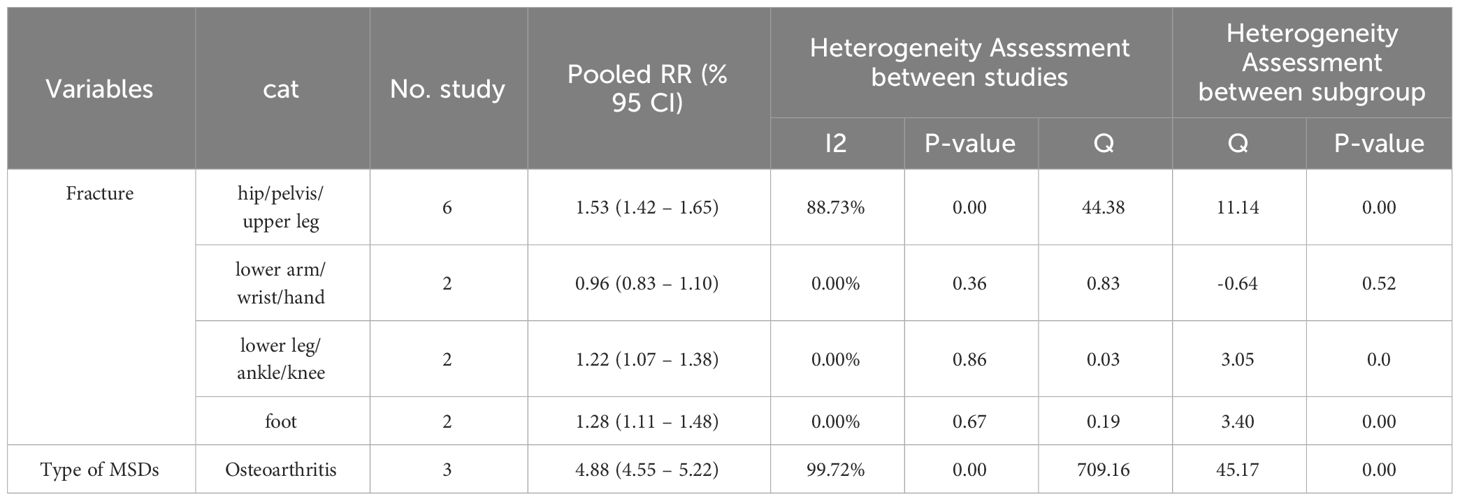
Table 3 The subgroups analysis of association between DM and MSDs by combining cohort studies based on place of fracture, type of MSDs.
Osteoarthritis was among the disorders examined in several studies. The combined RR estimate for the three studies was 4.88 (95% CI 4.55–5.22; P-value=0.00, I2 = 99.72%). This finding indicates that DM could be a significant risk factor for osteoarthritis (Table 3).
This analysis examined the relationship between our results and three variables: age, BMI, and year. The regression coefficients and statistical significance for each variable were as follows: age (B: -0.009, SE: 0.005, P: 0.096), BMI (B: -0.007, SE: 0.022, P: 0.746), and year (B: -0.001, SE: 0.01, P: 0.890). The age variable demonstrated a weakly decreasing relationship but did not reach statistical significance. The variables of BMI and year did not show any significant associations with our results.
The quality of 10 cohort studies was evaluated using the Joanna Briggs Institute (JBI) critical appraisal tools. The assessment revealed that the majority of the cohort studies received high-quality scores, indicating a high level of methodological rigor (Table 4).
This meta-analysis aimed to evaluate the association between DM and MSDs. Various categories were considered in the analysis, including the duration of DM, continent, place of fracture, type of MSDs, age, and sex. The results consistently indicated that individuals with DM have a higher risk of developing musculoskeletal complications than the general population. These findings align with previous studies and further support the association between DM and MSDs. Indeed, studies have demonstrated that DM affects the human body in various ways, although the exact mechanisms are not fully understood. One proposed mechanism involves increased levels of advanced glycation end-products (AGEs), which can trigger fibroproliferative complications. When the receptor for AGEs (RAGE) is turned on, it activates several signaling pathways, such as the MAPK/ERK, TGF-β, JNK, and NF-κB pathways (28). This activation leads to two main complications. Firstly, it induces oxidative stress in the endoplasmic reticulum (ER) (29). Secondly, it upregulates the expression of inflammatory cytokines such as IL-1β, IL-6, and TNFα (28, 30–32). These pathways can influence proteins like collagen, making them more susceptible to glycation (33). Histologic studies have revealed that this mechanism affects individuals with diabetes, as changes in AGE pathways can lead to decreased elasticity and load-bearing capacity of tendons (34, 35). Additionally, chondrocytes, the cells responsible for cartilage maintenance, can adapt their expression of glucose transporters (GLUT-1, GLUT-3, and GLUT-9) in response to blood glucose levels. However, this adaptive mechanism may be absent in MSDs such as osteoarthritis. TNFα and IL-1β can make IL-6, PGE2, and phosphokinase C work, which controls the amount of expressed GLUT transporters (36–38). Therefore, hyperglycemia and insulin resistance in diabetes can alter these pathways and impact the musculoskeletal system.
In the subgroup analysis, the association between DM and MSDs was found to vary across different categories. Specifically, diabetic patients with a longer duration of DM were observed to have a higher risk of developing musculoskeletal complications. This finding can be attributed to the cumulative effects of prolonged exposure to diabetes, which can lead to both microvascular and macrovascular complications. Over time, diabetes can adversely affect the small blood vessels (microvascular) and larger blood vessels (macrovascular) throughout the body. These vascular complications can impair blood flow, nutrient delivery, and oxygen supply to the musculoskeletal system, increasing the risk of musculoskeletal problems. It is important to note that the longer the duration of DM, the higher the likelihood of developing microvascular complications such as diabetic neuropathy, retinopathy, and nephropathy. These complications can contribute to the development of musculoskeletal issues by affecting nerve function, blood supply, and overall tissue health. As a result, the subgroup analysis shows that the length of DM is strongly related to the risk of musculoskeletal complications. The longer the DM, the higher the risk, as the microvascular and macrovascular complications increase over time (39). Our results were confirmed in the study of Bonds et al. in 2006 (21). Indeed, age and sex differences have been identified as potential risk factors for MSDs in diabetic patients. Their study found musculoskeletal complications were more prevalent in younger and female individuals. This observation aligns with the existing literature and can be explored from different perspectives, including the influence of sex hormones. Sex hormones, such as estrogen, play a role in regulating the health and function of tendons and ligaments. Estrogen has been shown to have a protective effect on these connective tissues, promoting their strength and elasticity. In females, the decline in estrogen levels during menopause can contribute to changes in tendon and ligament properties, making them more susceptible to injury or degeneration. Moreover, hormonal differences between males and females can also impact the inflammatory response and immune function, which may contribute to the development and progression of MSDs. Additionally, differences in body composition, muscle mass, and biomechanics between sexes may influence the distribution of forces and loading patterns on the musculoskeletal system, potentially increasing the risk of certain conditions. Considering age, it is essential to note that younger individuals may be more susceptible to musculoskeletal complications due to longer exposure to diabetes-related metabolic abnormalities and prolonged disease duration. Furthermore, age-related factors such as decreased tissue regeneration capacity, increased oxidative stress and cumulative damage over time can contribute to a higher risk of MSDs in older individuals. By considering these age and sex-related factors, a more comprehensive understanding of the underlying mechanisms and risk factors associated with MSDs in diabetic patients can be achieved (40). Second is diversity in muscle fibers; for example, women have more type I fibers than others (41). Third, lower pain thresholds in females can be the other cause (42). One of the specific diseases investigated in the diabetic population was osteoarthritis, and our study revealed a heightened risk of its occurrence. This increased risk can be attributed to elevated levels of pro-inflammatory cytokines, oxidative stress, obesity, and higher secretion of adipokines in individuals with diabetes. These factors play significant roles in the development and progression of osteoarthritis (43, 44). Our findings approved Courties et al.’s previous study 2016 (45).
Future research should focus on identifying additional factors contributing to the increased risk of MSDs in diabetic individuals, such as specific treatment modalities, comorbidities, lifestyle factors, or genetic predisposition. By expanding our knowledge of the risk factors and underlying mechanisms, healthcare providers can develop more targeted strategies for prevention, early detection, and effective management of musculoskeletal complications in individuals with diabetes. This will ultimately improve patient outcomes and contribute to the development of evidence-based guidelines for clinical practice.
The study possesses several strengths that contribute to its significance. Firstly, it stands as the first systematic review and meta-analysis to investigate and analyze the association between DM and MSDs comprehensively. This approach enhances the overall understanding of the topic and provides a valuable synthesis of existing evidence. Secondly, the study employed diverse studies that investigated various outcomes related to MSDs. This allowed for a subgroup analysis based on different specifications, enabling a more nuanced association examination. The high homogeneity observed in the results indicates that the included articles were appropriately chosen, further strengthening the validity of the findings. Thirdly, using cohort studies for meta-analysis provides a foundation for exploring causal associations between DM and MSDs. This approach allows for incorporating genetic and molecular science studies, which can shed light on underlying mechanisms and potential pathways. However, it is important to acknowledge certain limitations of the study. One such limitation is the lack of analysis based on confounding variables. MSDs can develop and advance as a result of factors like the type of treatment diabetic patients receive and the presence of other underlying diseases. The absence of consideration for these confounders restricts the ability to explain the study results fully and may leave room for alternative interpretations. Despite these limitations, the study’s strengths, including its systematic and comprehensive approach, subgroup analysis, and utilization of cohort studies, contribute to its valuable insights into the association between diabetes and musculoskeletal disorders. Despite study limitations, further research is crucial to understand the underlying mechanisms, potentially informing targeted interventions that can mitigate MSDs prevalence and impact in the diabetic population. This underscores the importance of an integrated healthcare approach, ultimately enhancing the overall quality of life for affected individuals.
In conclusion, our findings shed light on an understudied aspect of diabetes-related comorbidities, emphasizing the nuanced nature of this relationship, particularly in specific subgroups. Importantly, they highlight the need for a holistic approach to diabetes management, addressing both glycemic control and musculoskeletal health.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
MAz: Conceptualization, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. AM: Data curation, Writing – original draft. MAf: Formal analysis, Methodology, Writing – original draft. LS: Data curation, Investigation, Writing – original draft. MT: Data curation, Writing – original draft. KK: Data curation, Investigation, Writing – original draft. SK: Conceptualization, Data curation, Investigation, Project administration, Writing – original draft, Writing – review & editing. YM: Conceptualization, Data curation, Investigation, Methodology, Software, Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2024.1320468/full#supplementary-material
1. Alam U, Asghar O, Azmi S, Malik RA. General aspects of diabetes mellitus. Handb Clin Neurol. (2014) 126:211–22. doi: 10.1016/B978-0-444-53480-4.00015-1
2. Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. (2011) 94:311–21. doi: 10.1016/j.diabres.2011.10.029
3. Chawla A, Chawla R, Jaggi S. Microvasular and macrovascular complications in diabetes mellitus: Distinct or continuum? Indian J Endocrinol Metab. (2016) 20:546–51. doi: 10.4103/2230-8210.183480
4. Majjad A, Errahali Y, Toufik H, H Djossou J, Ghassem MA, Kasouati J, et al. Musculoskeletal disorders in patients with diabetes mellitus: a cross-sectional study. Int J Rheumatol. (2018) 2018:3839872. doi: 10.1155/2018/3839872
5. Mustafa KN, Khader YS, Bsoul AK, Ajlouni K. Musculoskeletal disorders of the hand in type 2 diabetes mellitus: prevalence and its associated factors. Int J rheumatic Dis. (2016) 19:730–5. doi: 10.1111/1756-185X.12617
6. Arkkila PET, Gautier J-F. Musculoskeletal disorders in diabetes mellitus: an update. Best Pract Res Clin Rheumatol. (2003) 17:945–70. doi: 10.1016/j.berh.2003.11.001
7. Harding JL, Pavkov ME, Magliano DJ, Shaw JE, Gregg EW. Global trends in diabetes complications: a review of current evidence. Diabetologia. (2019) 62:3–16. doi: 10.1007/s00125-018-4711-2
8. Rosenbloom AL, Silverstein JH. Connective tissue and joint disease in diabetes mellitus. Endocrinol Metab Clinics. (1996) 25:473–83. doi: 10.1016/S0889-8529(05)70335-2
9. Goldberg BA, Scarlat MM, Harryman Ii DT. Management of the stiff shoulder. J orthopaedic Sci. (1999) 4:462–71. doi: 10.1007/s007760050131
10. Sözen T, Başaran NÇ, Tınazlı M, Özışık L. Musculoskeletal problems in diabetes mellitus. Eur J Rheumatol. (2018) 5:258. doi: 10.5152/eurjrheumatol.
11. Choi JH, Kim HR, Song KH. Musculoskeletal complications in patients with diabetes mellitus. Korean J Intern Med. (2022) 37(6):1099–110. doi: 10.3904/kjim.2022.168
12. Smith L, Burnet S, McNeil J. Musculoskeletal manifestations of diabetes mellitus. Br J sports Med. (2003) 37:30. doi: 10.1136/bjsm.37.1.30
13. Henry RR, Genuth S. Forum one: current recommendations about intensification of metabolic control in non-insulin-dependent diabetes mellitus. Ann Internal Med. (1996) 124:175–7. doi: 10.7326/0003-4819-124-1_Part_2-199601011-00019
14. Aydeniz A, Gursoy S, Guney E. Which musculoskeletal complications are most frequently seen in type 2 diabetes mellitus? J Int Med Res. (2008) 36:505–11. doi: 10.1177/147323000803600315
15. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. (2021) 10:1–11. doi: 10.1186/s13643-021-01626-4
16. Moola S, Munn Z, Sears K, Sfetcu R, Currie M, Lisy K, et al. Conducting systematic reviews of association (etiology): The Joanna Briggs Institute's approach. Int J Evid Based Healthc. (2015) 13:163–9. doi: 10.1097/XEB.0000000000000064
17. Pollock D, Tricco AC, Peters MDJ, Mclnerney PA, Khalil H, Godfrey CM, et al. Methodological quality, guidance, and tools in scoping reviews: a scoping review protocol. JBI Evid Synth.. (2022) 20(4):1098–105. doi: 10.11124/JBIES-20-00570
18. Strotmeyer ES, Cauley JA, Schwartz AV, Nevitt MC, Resnick HE, Bauer DC, et al. Nontraumatic fracture risk with diabetes mellitus and impaired fasting glucose in older white and black adults: the health, aging, and body composition study. Arch Internal Med. (2005) 165:1612–7. doi: 10.1001/archinte.165.14.1612
19. Schwartz AV, Sellmeyer DE, Ensrud KE, Cauley JA, Tabor HK, Schreiner PJ, et al. Study of Osteoporotic Fractures Research G. Older women with diabetes have an increased risk of fracture: a prospective study. J Clin Endocrinol Metab. (2001) 86:32–8. doi: 10.1210/jcem.86.1.7139
20. Dobnig H, Piswanger-Sölkner JC, Roth M, Obermayer-Pietsch B, Tiran A, Strele A, et al. Type 2 diabetes mellitus in nursing home patients: effects on bone turnover, bone mass, and fracture risk. J Clin Endocrinol Metab. (2006) 91:3355–63. doi: 10.1210/jc.2006-0460
21. Bonds DE, Larson JC, Schwartz AV, Strotmeyer ES, Robbins J, Rodriguez BL, et al. Risk of fracture in women with type 2 diabetes: the Women’s Health Initiative Observational Study. J Clin Endocrinol Metab. (2006) 91:3404–10. doi: 10.1210/jc.2006-0614
22. Ottenbacher KJ, Ostir GV, Peek MK, Goodwin JS, Markides KS. Diabetes mellitus as a risk factor for hip fracture in Mexican American older adults. Journals Gerontology Ser A: Biol Sci Med Sci. (2002) 57:M648–53. doi: 10.1093/gerona/57.10.M648
23. Schwartz AV, Vittinghoff E, Bauer DC, Hillier TA, Strotmeyer ES, Ensrud KE, et al. Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes. Jama. (2011) 305:2184–92. doi: 10.1001/jama.2011.715
24. Napoli N, Strotmeyer ES, Ensrud KE, Sellmeyer DE, Bauer DC, Hoffman AR, et al. Fracture risk in diabetic elderly men: the MrOS study. Diabetologia. (2014) 57:2057–65. doi: 10.1007/s00125-014-3289-6
25. Martinez-Laguna D, Tebe C, Javaid MK, Nogues X, Arden NK, Cooper C, et al. Incident type 2 diabetes and hip fracture risk: a population-based matched cohort study. Osteoporosis Int. (2015) 26:827–33. doi: 10.1007/s00198-014-2986-9
26. Guo Y, Wang Y, Chen F, Wang J, Wang D. Assessment of risk factors for fractures in patients with type 2 diabetes over 60 years old: a cross-sectional study from Northeast China. J Diabetes Res. (2020) 2020. doi: 10.1155/2020/1508258
27. Sosa M, Saavedra P, Jódar E, Lozano-Tonkin C, Quesada JM, Torrijos A, et al. Bone mineral density and risk of fractures in aging, obese post-menopausal women with type 2 diabetes. The GIUMO Study. Aging Clin Exp Res. (2009) 21:27–32. doi: 10.1007/BF03324895
28. Khalid M, Petroianu G, Adem A. Advanced glycation end products and diabetes mellitus: mechanisms and perspectives. Biomolecules. (2022) 12:542. doi: 10.3390/biom12040542
29. Guerrero-Hernández A, Leon-Aparicio D, Chavez-Reyes J, Olivares-Reyes JA, DeJesus S. Endoplasmic reticulum stress in insulin resistance and diabetes. Cell calcium. (2014) 56:311–22. doi: 10.1016/j.ceca.2014.08.006
30. Monnier VM, Sell DR, Gao X, Genuth SM, Lachin JM, Bebu I. Plasma advanced glycation end products and the subsequent risk of microvascular complications in type 1 diabetes in the DCCT/EDIC. BMJ Open Diabetes Res Care. (2022) 10:e002667. doi: 10.1136/bmjdrc-2021-002667
31. Holte KB, Juel NG, Brox JI, Hanssen KF, Fosmark DS, Sell DR, et al. Hand, shoulder and back stiffness in long-term type 1 diabetes; cross-sectional association with skin collagen advanced glycation end-products. The Dialong study. J Diabetes its Complications. (2017) 31:1408–14. doi: 10.1016/j.jdiacomp.2017.06.007
32. Sutherland JP, McKinley B, Eckel RH. The metabolic syndrome and inflammation. Metab syndrome related Disord. (2004) 2:82–104. doi: 10.1089/met.2004.2.82
33. Avery NC, Bailey AJ. The effects of the Maillard reaction on the physical properties and cell interactions of collagen. Pathologie Biologie. (2006) 54:387–95. doi: 10.1016/j.patbio.2006.07.005
34. Boivin GP, Elenes EY, Schultze AK, Chodavarapu H, Hunter SA, Elased KM. Biomechanical properties and histology of db/db diabetic mouse Achilles tendon. Muscles ligaments tendons J. (2014) 4:280. doi: 10.11138/mltj/2014.4.3.280
35. Valencia JV, Weldon SC, Quinn D, Kiers GH, DeGroot J, TeKoppele JM, et al. Advanced glycation end product ligands for the receptor for advanced glycation end products: biochemical characterization and formation kinetics. Anal Biochem. (2004) 324:68–78. doi: 10.1016/j.ab.2003.09.013
36. Rosa SC, Gonçalves J, Judas F, Mobasheri A, Lopes C, Mendes AF. Impaired glucose transporter-1 degradation and increased glucose transport and oxidative stress in response to high glucose in chondrocytes from osteoarthritic versus normal human cartilage. Arthritis Res Ther. (2009) 11:1–11. doi: 10.1186/ar2713
37. Shikhman AR, Brinson DC, Valbracht J, Lotz MK. Cytokine regulation of facilitated glucose transport in human articular chondrocytes. J Immunol. (2001) 167:7001–8. doi: 10.4049/jimmunol.167.12.7001
38. Chen YJ, Chan DC, Lan KC, Wang CC, Chen CM, Chao SC, et al. PPARγ is involved in the hyperglycemia-induced inflammatory responses and collagen degradation in human chondrocytes and diabetic mouse cartilages. J Orthopaedic Res. (2015) 33:373–81. doi: 10.1002/jor.22770
39. Ebadi SA, Pajavand H, Asadi A, Asadollahi P, Fatollahzadeh M. Relationship of musculoskeletal diseases with microvascular and macrovascular complications in patients with diabetes in Iran. Diabetes Metab Syndrome: Clin Res Rev. (2021) 15:102272. doi: 10.1016/j.dsx.2021.102272
40. Hart DA, Archambault JM, Kydd A, Reno C, Frank CB, Herzog W. Gender and neurogenic variables in tendon biology and repetitive motion disorders. Clin Orthopaedics Related Research®. (1998) 351:44–56. doi: 10.1097/00003086-199806000-00007
41. Lindman R, Eriksson A, Thornell LE. Fiber type composition of the human male trapezius muscle: Enzyme-histochemical characteristics. Am J Anat. (1990) 189:236–44. doi: 10.1002/aja.1001890306
42. Treaster DE, Burr D. Gender differences in prevalence of upper extremity musculoskeletal disorders. Ergonomics. (2004) 47:495–526. doi: 10.1080/00140130310001638171
43. Yusuf E, Nelissen RG, Ioan-Facsinay A, Stojanovic-Susulic V, DeGroot J, Van Osch G, et al. Association between weight or body mass index and hand osteoarthritis: a systematic review. Ann rheumatic Dis. (2010) 69:761–5. doi: 10.1136/ard.2008.106930
44. Hotamisligil GS, Arner P, Caro JF, Atkinson RL, Spiegelman BM. Increased adipose tissue expression of tumor necrosis factor-alpha in human obesity and insulin resistance. J Clin Invest. (1995) 95:2409–15. doi: 10.1172/JCI117936
Keywords: musculoskeletal disorders, diabetes mellitus, complications, evidence synthesis, meta-analysis
Citation: Azami M, Moradkhani A, Afraie M, Saed L, Tapak MA, Khoramipoor K, Khateri S and Moradi Y (2024) The association between diabetes mellitus and musculoskeletal disorders: a systematic review and meta-analysis. Front. Endocrinol. 15:1320468. doi: 10.3389/fendo.2024.1320468
Received: 23 October 2023; Accepted: 18 March 2024;
Published: 03 April 2024.
Edited by:
Xiaonan Liu, Johns Hopkins Medicine, United StatesReviewed by:
Cristina Hernández-Díaz, Hospital Juárez de México, MexicoCopyright © 2024 Azami, Moradkhani, Afraie, Saed, Tapak, Khoramipoor, Khateri and Moradi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yousef Moradi, WW91c2VmbW9yYWRpMjExQHlhaG9vLmNvbQ==; Sorour Khateri, U29ydXIua2hhdGVyaUB5YWhvby5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.