
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Endocrinol. , 26 February 2024
Sec. Renal Endocrinology
Volume 15 - 2024 | https://doi.org/10.3389/fendo.2024.1273265
Objective: The specific benefit and selection of acupoints in acupuncture for diabetic kidney disease (DKD) remains controversial. This study aims to explore the specific benefits and acupoints selection of acupuncture for DKD through meta-analysis and data mining.
Methods: Clinical trials of acupuncture for DKD were searched in eight common databases. Meta-analysis was used to evaluate its efficacy and safety, and data mining was used to explore its acupoints selection.
Results: Meta-analysis displayed that compared with the conventional drug group, the combined acupuncture group significantly increased the clinical effective rate (risk ratio [RR] 1.35, 95% confidence interval [CI] 1.20 to 1.51, P < 0.00001) and high-density lipoprotein cholesterol (mean difference [MD] 0.36, 95% CI 0.27 to 0.46, P < 0.00001), significantly reduced the urinary albumin (MD –0.39, 95% CI –0.42 to –0.36, P < 0.00001), urinary microalbumin (MD –32.63, 95% CI –42.47 to –22.79, P < 0.00001), urine β2-microglobulin (MD –0.45, 95% CI –0.66 to –0.24, P < 0.0001), serum creatinine (MD –15.36, 95% CI –21.69 to –9.03, P < 0.00001), glycated hemoglobin A1c (MD –0.69, 95% CI –1.18 to –0.19, P = 0.006), fasting blood glucose (MD –0.86, 95% CI –0.90 to –0.82, P < 0.00001), 2h postprandial plasma glucose (MD –0.87, 95% CI –0.92 to –0.82, P < 0.00001), total cholesterol (MD –1.23, 95% CI –2.05 to –0.40, P = 0.003), triglyceride (MD –0.69, 95% CI –1.23 to –0.15, P = 0.01), while adverse events were comparable. Data mining revealed that CV12, SP8, SP10, ST36, SP6, BL20, BL23, and SP9 were the core acupoints for DKD treated by acupuncture.
Conclusion: Acupuncture improved clinical symptoms, renal function indices such as uALB, umALB, uβ2-MG, and SCR, as well as blood glucose and blood lipid in patients with DKD, and has a favorable safety profile. CV12, SP8, SP10, ST36, SP6, BL20, BL23, and SP9 are the core acupoints for acupuncture in DKD, and this program is expected to become a supplementary treatment for DKD.
Diabetic kidney disease (DKD) is a metabolic disease characterized by systemic metabolic disturbance (1) and is the most common and severe complication of diabetes (2). DKD manifests as hyperfiltration and proteinuria in the early stage and end-stage renal disease in the late stage (3). Epidemiological studies have shown that the number of patients with DKD is increasing year by year, and it is estimated that there will be 592 million patients with DKD by 2035, accounting for about 8%–10% of the global population (4, 5). Renal failure in patients with advanced DKD often requires renal replacement therapy or renal transplantation, which seriously jeopardizes the physical and mental health of patients and imposes a substantial economic burden on families and society (6). Currently, the main therapeutic options for DKD include hypoglycemia, antihypertensive, regulation of lipid metabolism disorders, reduction of urinary protein, and renal replacement therapy for end-stage renal disease (7). Although these treatment regimens reduce complications, delay the progression of DKD, and improve long-term survival, it remains unsatisfactory (8). Therefore, it is essential to explore a safe and effective treatment that can improve the prognosis of DKD.
Acupuncture is a traditional Chinese medicine practice that works by stimulating specific sites (acupoints) on the surface of the body (9) and is a widely accepted complementary and alternative therapy (10). Previous studies have indicated that acupuncture can attenuate insulin resistance in patients with type 2 diabetes, implying that it may have the potential to improve the prognosis of type 2 diabetes and its complications (11). In recent years, more and more studies have demonstrated the unique advantages of acupuncture combined with conventional medications in treating DKD (12). Acupuncture has been reported to reduce proteinuria, glycemia, and lipids and improve patients’ quality of life with DKD (13). However, the specific benefits and acupoints selection of acupuncture for DKD is still controversial. Therefore, this study used meta-analysis to assess the efficacy and safety of acupuncture in DKD to explore its specific benefits and risks and used data mining to explore the core acupuncture points for acupuncture in DKD.
This study strictly followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) (14).
China National Knowledge Infrastructure Database (CNKI), China Biomedical Literature, China Science and Technology Journal Database, Wanfang Database, Embase, PubMed, the Cochrane Library, and Web of Science were searched for clinical studies on acupuncture for DKD up to June 2023, with subject terms covering acupuncture and DKD. Based on the subject words, the free words were expanded with the help of CNKI and Mesh databases, and then the subject words and free words were combined for retrieval. The English search formula was: ([“acupuncture” OR “acupressure” OR “needling” OR “needle therapy” OR “meridian therapy”] AND [“diabetic kidney disease” OR “diabetic kidney diseases” OR “diabetic nephropathies” OR “diabetic nephropathy” OR “diabetic glomerulosclerosis” OR “diabetic renal disease” OR “diabetic kidney injury” OR “diabetic renal injury”]). The Chinese search formula is: ([“针刺” OR “针灸” OR “针法”] AND [“糖尿病肾病” OR “糖尿病性肾病” OR “糖尿病肾小球硬化症” OR “糖尿病性肾小球硬化症”]).
Inclusion criteria: (1) Randomized controlled trials; (2) The subjects included were patients with DKD (15); (3) Patients in the control group received conventional treatment, and patients in the experimental group received acupuncture and conventional treatment; (4) Efficacy endpoints included clinical effective rate, renal function (urinary albumin [uALB], urinary microalbumin [umALB], urine β2 microglobulin [uβ2-MG], serum creatinine [SCR]), blood glucose (glycated hemoglobin A1c [HbA1c], fasting blood glucose [FBG], 2h postprandial plasma glucose [2h PPG]), blood lipid (total cholesterol [TC], triglyceride [TG], high-density lipoprotein cholesterol [HDL-C]). The clinical effective rate was defined as the percentage of symptoms and signs relieved out of the total number. Safety endpoints were adverse events.
Exclusion criteria: (1) The literature had been published repeatedly; (2) The data was incomplete; (3) The data was not available.
First, the basic literature was imported into Reference Aid for Medicine, and the included literature was obtained by screening layer by layer according to the inclusion and exclusion criteria. Second, the included literature was sorted out, and the baseline data of each study was entered into the basic characteristics table. Furthermore, the risk of bias was assessed using the Cochrane risk of bias assessment tool. These works were completed independently by Yunfeng Yu and Xinyu Yang, and any objection was decided by Keke Tong.
Meta-analysis was performed using Revman 5.3, with risk ratio (RR) as effect sizes for dichotomous variables and mean difference (MD) for continuous variables. Heterogeneity analysis was conducted by I2 test. Fixed-effects models were used when I2 < 50%, and the methodological quality and clinical design of the included studies were similar. A random-effects model was used when I2 ≥ 50% or there was significant methodologic heterogeneity or clinical heterogeneity. Leave-one-out sensitivity analysis was used to assess the robustness of the combined results and to check for the presence of individual studies that significantly affected the results. Subgroup sensitivity analysis was used to assess the effects of gender, age, and number of acupuncture points on the combined results. Stata15.0 was used to perform Harbord regression to evaluate publication bias, and if P > 0.1, it indicated no publication bias.
The literature search strategy was the same as the meta-analysis part.
Inclusion criteria:
(1) Randomized controlled trials or case-control studies; (2) The included subjects were patients with DKD; (3) The experimental group was treated with acupuncture, and the acupoint records were complete; (4) The efficacy of acupuncture was definite.
Exclusion criteria:
(1) Duplicate publication; (2) Data were not available; (3) External treatments other than acupuncture were used.
The names of acupoints included in the studies were standardized based on the “Nomenclature and location of meridian points” (16). For example, “Yishu” was standardized as “EX-B3”, and “Zhongjixue” was standardized as “CV3”.
First, the Traditional Chinese Medicine Case Cloud V2.3 was utilized to conduct frequency analysis, with a frequency threshold set at >20% to identify common acupoints for treating DKD through acupuncture. Second, the identified common acupoints were inputted into SPSS Modeler 18.0 for association rule analysis. The analysis employed the Apriori model with parameters set at support ≥ 30%, confidence ≥ 100%, and lift ≥ 1.0. Support measured the frequency of an itemset appearing in the dataset. Confidence represented the likelihood of another subsequent itemset occurring given a set of prerequisite items. Lift was used to determine whether a rule has practical application value. Based on this parameter, the association rule analysis could obtain core acupoint combinations with practical significance consisting of acupoints with a high frequency of occurrence and close connection with each other. The acupoints that make up the core acupoint combinations were defined as core acupoints. Third, the core acupoints were imported into SPSS Statistics 25.0 for factor analysis. The factor analysis, employing principal component analysis and the rotation maximum variance method, aimed to clarify the grouping of these core acupuncture points. Factor analysis was a commonly utilized technique for reducing data dimensions, aiding in the discovery of the latent structures behind observed variables. Furthermore, factor analysis based on principal component analysis could transform multiple correlated observed variables into a few independent principal components, thereby simplifying the data structure and uncovering the inherent connections between variables. It contributed to understanding how core acupoints are grouped and subsequently analyzing the efficacy of different acupoint groups in treating DKD.
A total of 789 relevant studies were obtained, and 325 were excluded due to duplication or other reasons. After reading the title and abstract, 443 studies were eliminated. After reading the complete text, 12 studies were removed. Nine clinical studies were finally included, as shown in Figure 1.
A total of nine clinical studies (17–25) (all study centers were in China) were included with a total sample size of 659 cases, of which 270 cases received conventional treatment and 389 cases received acupuncture combined with conventional treatment. Baseline information such as gender, age, and disease duration were comparable between the experimental and control groups in each included study. The basic characteristics of the included studies are listed in Table 1.
The risk of bias was unclear for the randomization method in two studies, the risk of bias for allocation concealment and blinding of interventions to patients and participants was unclear in nine studies, and the risk of bias was low in the remaining areas, as shown in Figure 2.
Compared with the conventional treatment group, the combined acupuncture group significantly increased the clinical effective rate by 35% (RR 1.35, 95% confidence interval [CI] 1.20 to 1.51, P < 0.00001), as shown in Figure 3.

Figure 3 Meta analysis of clinical effective rate in acupuncture combined group vs conventional drug group in the treatment of DKD. DKD, diabetic kidney disease.
Compared with the conventional treatment group, the combined acupuncture group significantly decreased uALB by 0.39g (MD –0.39, 95% CI –0.42 to –0.36, P < 0.00001), umALB by 32.63mg (MD –32.63, 95% CI –42.47 to –22.79, P < 0.00001), uβ2-MG by 0.45μg/ml (MD –0.45, 95% CI –0.66 to –0.24, P < 0.0001), and SCR by 15.36μmol/L, as shown in Figure 4.
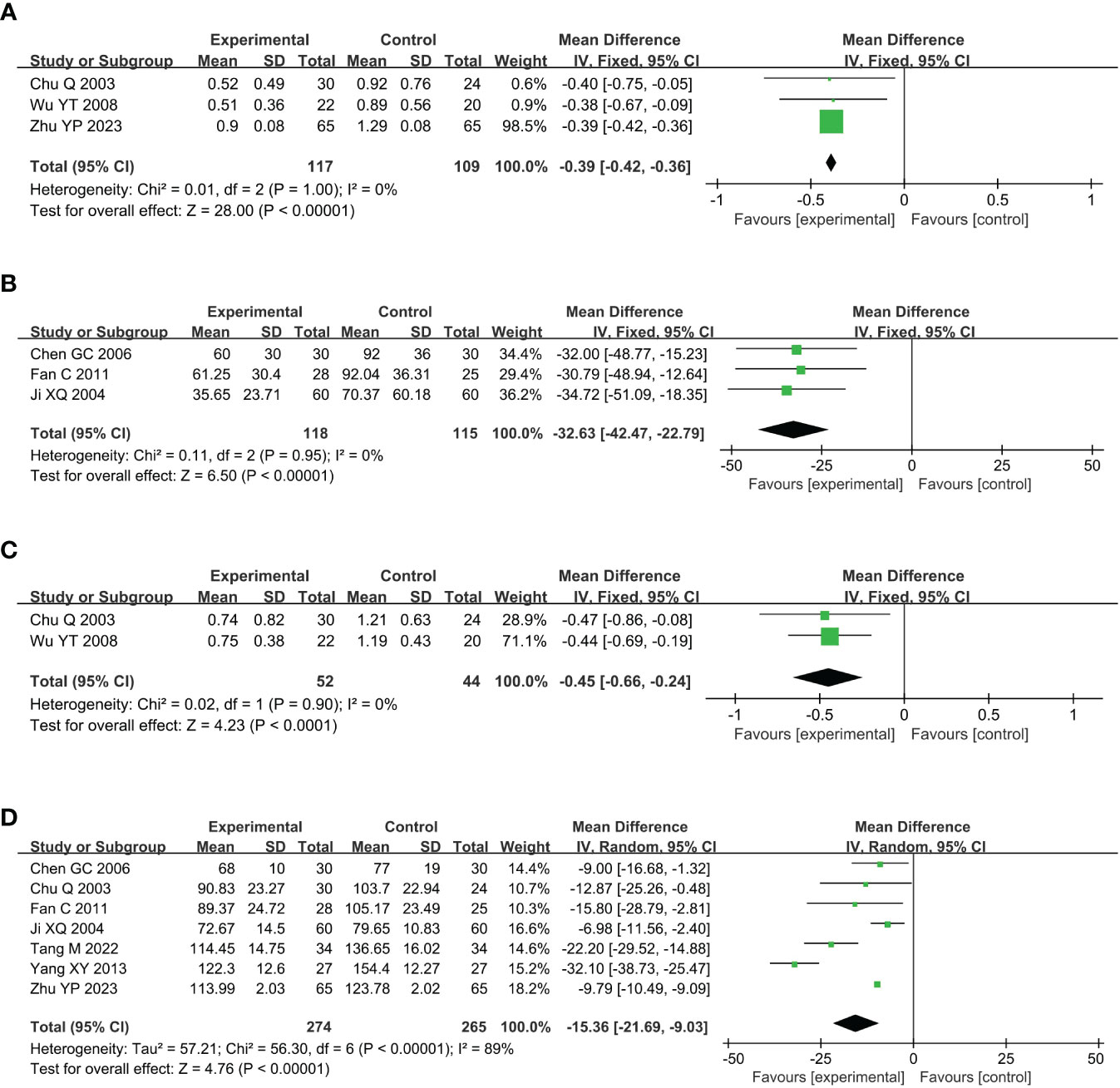
Figure 4 Meta analysis of renal function in acupuncture combined group vs conventional drug group in the treatment of DKD. (A) uALB, (B) umALB, (C) uβ2-MG; (D) SCR. DKD, diabetic kidney disease; uALB, urinary albumin; umALB, urinary microalbumin; uβ2-MG, urine β2 microglobulin; SCR, serum creatinine.
Compared with the conventional treatment group, the combined acupuncture group significantly reduced HbA1c by 0.69% (MD –0.69, 95% CI –1.18 to –0.19, P = 0.006), FBG by 0.86mmol/L (MD –0.86, 95% CI –0.90 to –0.82, P < 0.00001) and 2h PPG by 0.87mmol/L (MD –0.87, 95% CI –0.92 to –0.82, P < 0.00001), as shown in Figure 5.
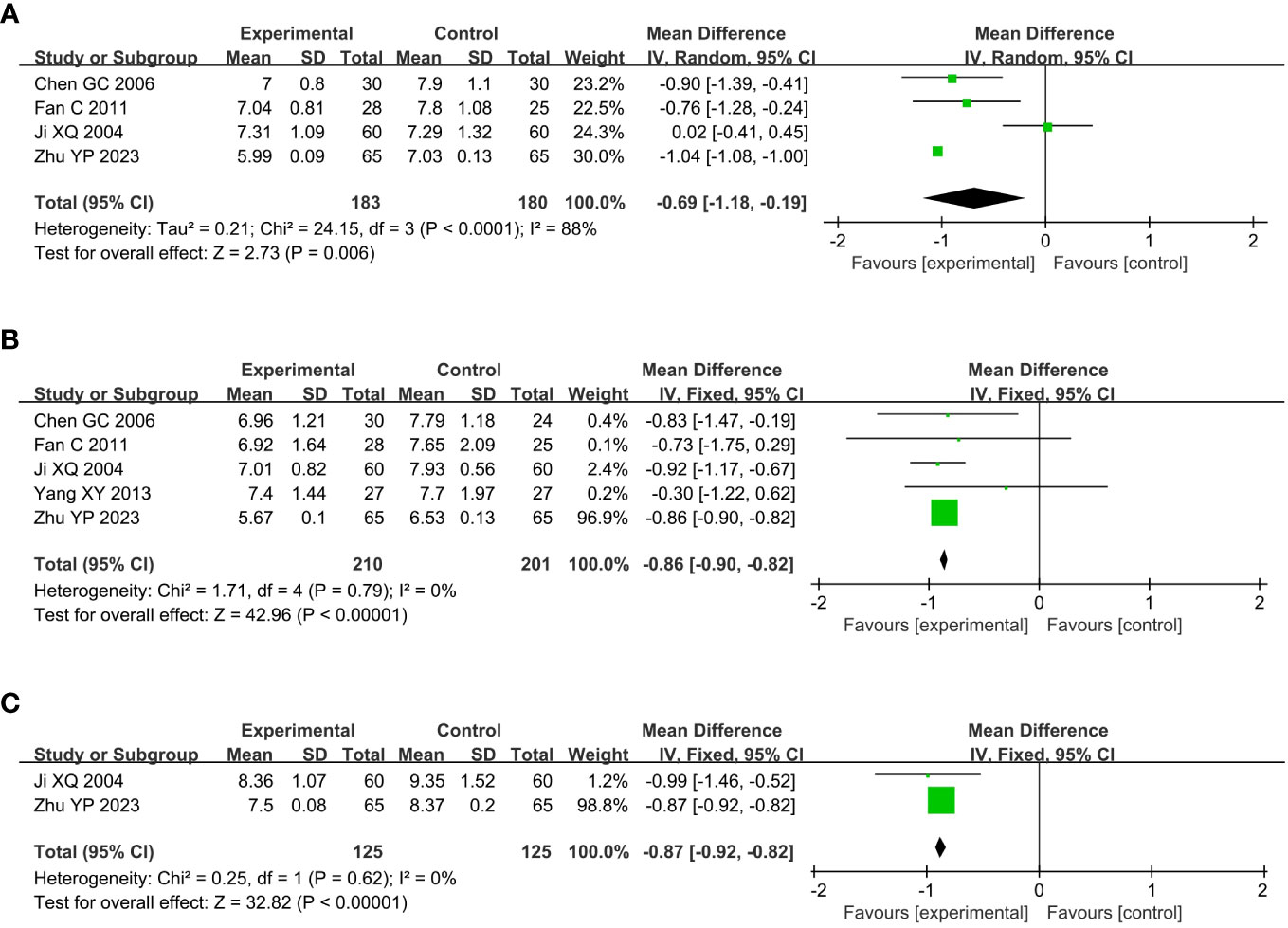
Figure 5 Meta analysis of blood glucose in acupuncture combined group vs conventional drug group in the treatment of DKD. (A) HbA1c, (B) FBG, (C) 2h PPG. DKD, diabetic kidney disease; HbA1c, glycated hemoglobin A1c; FBG, fasting blood glucose; 2h PPG, 2h postprandial plasma glucose.
Compared with the conventional treatment group, the combined acupuncture group significantly reduced TC by 1.23mmol/L (MD –1.23, 95% CI –2.05 to –0.40, P = 0.003) and TG by 0.69mmol/L (MD –0.69, 95% CI –1.23 to –0.15, P = 0.01), and increased HDL-C by 0.36mmol/L (MD 0.36, 95% CI 0.27 to 0.46, P < 0.00001), as shown in Figure 6.
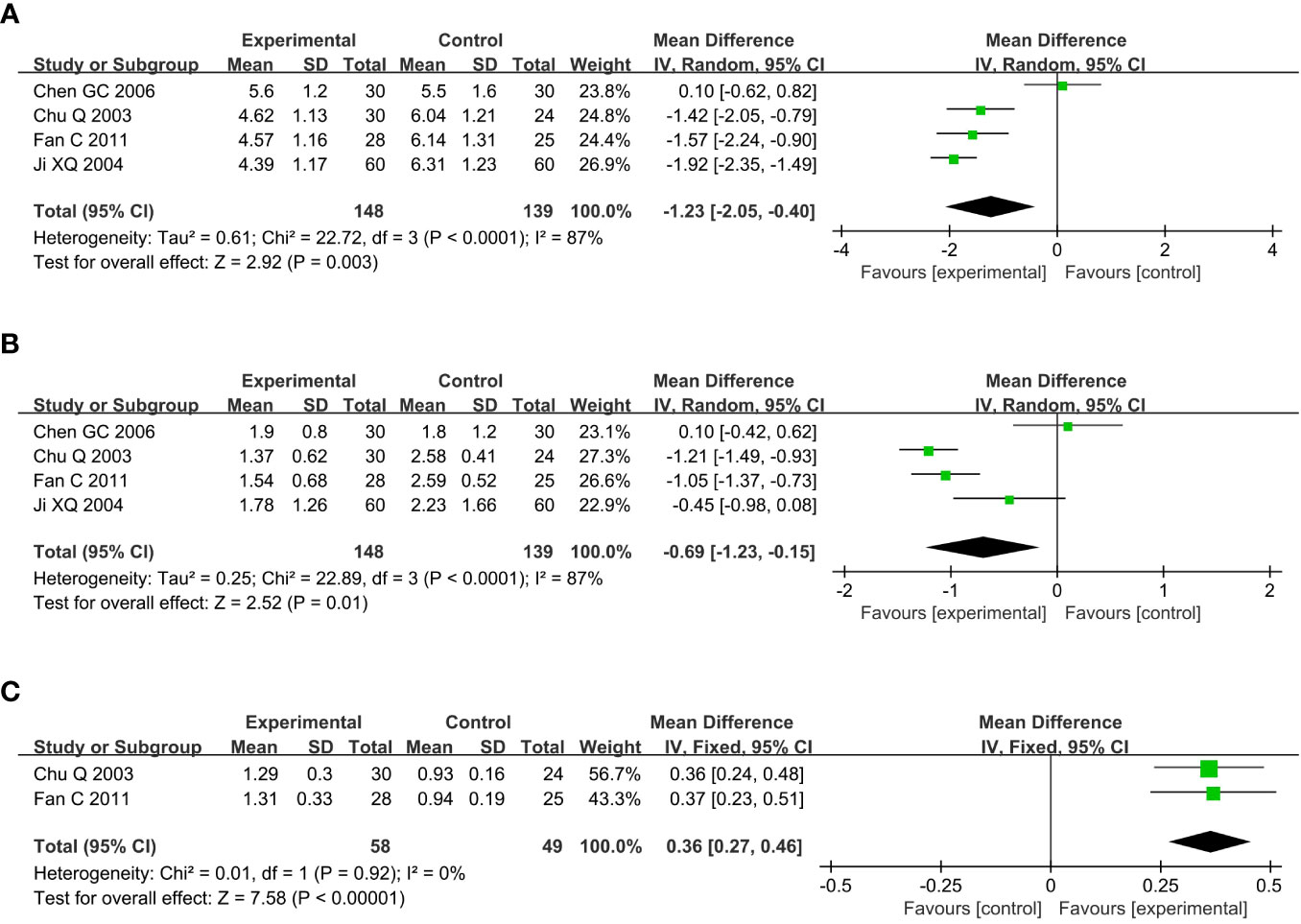
Figure 6 Meta analysis of blood lipid in acupuncture combined group vs conventional drug group in the treatment of DKD. (A) TC, (B) TG, (C) HDL-C. DKD, diabetic kidney disease; TC, total cholesterol; TG, triglyceride; HDL-C, high-density lipoprotein cholesterol.
Adverse events occurred in two patients in the combined acupuncture group, both of which were local hematomas caused by insufficient pressing time after needle withdrawal. There were six adverse events in the conventional treatment group, including three cases of vomiting and three cases of dyspepsia. There was no significant difference in adverse events between the combined acupuncture group and the conventional treatment group (RR 0.60, 95% CI 0.01 to 36.95, P = 0.81), as shown in Figure 7.
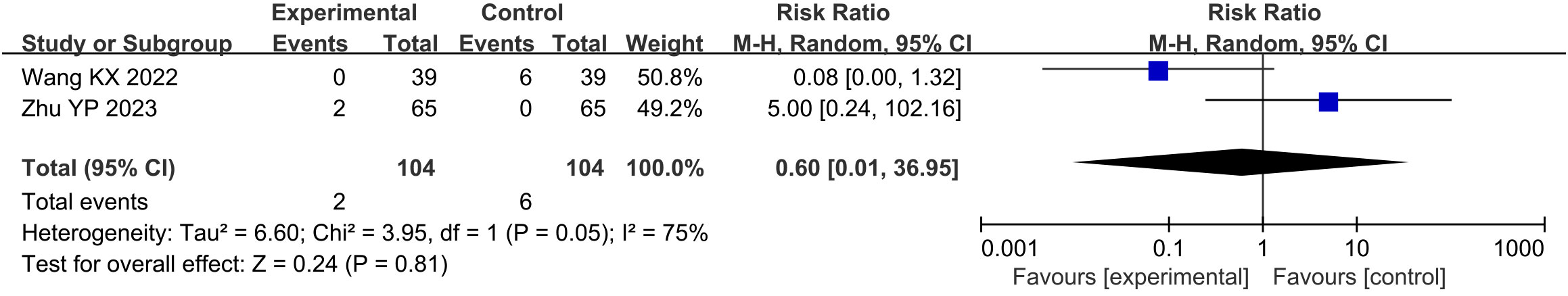
Figure 7 Meta analysis of adverse events in acupuncture combined group vs conventional drug group in the treatment of DKD. DKD, diabetic kidney disease.
The leave-one-out sensitivity analysis showed that the results of clinical effective rate, uALB, umALB, SCR, HbA1c, FBG, TC, and TG had low sensitivity and high confidence. Due to uβ2-MG, 2h PPG, HDL-C, and adverse events were only assessed in two of the included studies, their leave-one-out sensitivity analysis cannot be performed.
The subgroup sensitivity analysis, with creatinine as the outcome, explored the effects of factors such as gender, age, and number of acupoints on the combined outcome. In terms of gender, acupuncture significantly reduced creatinine in the group of DKD with a male ratio of 41–50% (MD –14.27, 95% CI –23.23 to –5.30, P = 0.002), 51–60% (MD –14.18, 95% CI –22.47 to –5.89, P = 0.0008) and 61–70% (MD –22.20, 95% CI –29.52 to –14.88, P < 0.00001). In terms of age, acupuncture significantly reduced creatinine in the group of DKD with an average age of 41–50 years (MD –22.20, 95% CI –29.52 to –14.88, P < 0.00001), 51–60 years (MD –15.98, 95% CI –31.85 to –0.11, P = 0.048) and 61–70 years (MD –9.82, 95% CI –10.51 to –9.12, P < 0.00001). In terms of the number of acupoints, acupuncture significantly reduced creatinine in the group of DKD with 1–10 acupoints (MD –15.65, 95% CI –28.59 to –2.72, P = 0.02) and 10–20 acupoints (MD –15.28, 95% CI –23.31 to –7.26, P = 0.0002), as shown in Table 2.
The Harbord regression of the clinical effective rate showed P = 0.953, suggesting no significant publication bias (Figure 8).
A total of 789 relevant studies were obtained, and 51 clinical trials were included after stratified screening, containing 77 acupoints with a total frequency of 483.
Frequency analysis was performed to obtain 20 common acupoints with a frequency greater than 20%, including Zusanli (ST36), Shenshu (BL23), Sanyinjiao (SP6), Taixi (KI3), Diji (SP8), Zhongwan (CV12), Yinlingquan(SP9), Pishu (BL20), Xuehai (SP10), Guanyuan (CV4), Tianshu (ST25), Taichong (LR3), Fenglong (ST40), Hegu (LI4), Weiwanxiashu (EX-B3), Baihuanshu (BL30), Quchi (LI11), Ganshu (BL18), Gaohuangshu (BL43), and Zhongji (CV3), as shown in Table 3.
Association rule analysis was used to explore core acupoint combinations consisting of common acupoints. Under the conditions of setting support ≥ 30%, confidence ≥ 100%, and lift ≥ 1.0, a total of 11 core acupoint combinations were obtained, as shown in Table 4 They were formed by combining CV12, SP8, SP10, ST36, SP6, BL20, BL23, and SP9 with each other, indicating that these acupoints were the core acupoints for acupuncture in DKD. The network relationship diagram is shown in Figure 9.
Factor analysis was employed to explore the combinatorial relationship between the core acupoints, as shown in Figure 10. A total of two common factors were obtained, and the cumulative variance contribution was 65.30%. Common factor 1 consisted of CV12, SP8, and SP10, which accounted for 35.66% of the total variance. Common factor 2 consisted of ST36, SP6, BL20, BL23, and SP9, accounting for 29.64% of the total variance.
DKD is a major cause of end-stage renal disease (26). Patients with DKD have a higher mortality rate compared to diabetic patients without renal disease (27), and their prevalence has shown a gradual increase (28). Currently, there are no specific drugs for DKD, and strict control of blood glucose and blood pressure remains the primary strategy in treating DKD (29). Although these therapeutic strategies have delayed the progression of DKD to some extent, some patients still eventually develop end-stage renal disease (30). Acupuncture has been reported to have unique efficacy and a favorable safety profile in treating diabetes and its complications (31). In 1983, Li RC et al. (32) confirmed for the first time through animal experiments that acupuncture promotes insulin secretion and improves glucose tolerance, which has since opened the study of acupuncture for diabetes and its complications. Subsequent researchers have found that acupuncture not only reduces glycemia (33) but also has a combined effect of regulating lipids and hemodynamics (34, 35). In 2001, Zhang YL et al. (36) first reported the efficacy of acupuncture in the treatment of DKD, and they found that acupuncture could reduce 24-hour urine protein quantification and SCR in patients with DKD. Since then, there has been increasing evidence of the role of acupuncture in improving the prognosis of DKD (37). Nevertheless, the specific benefits and acupoint selection schemes of acupuncture for DKD are still controversial. Therefore, this study aimed to review and collect clinical trials of acupuncture for DKD, elaborate on the specific benefits of acupuncture for DKD through meta-analysis, and then explore the acupoint selection of acupuncture for DKD through data mining.
The study results showed that the clinical effective rate of the combined acupuncture group was significantly higher than that of the conventional treatment group, suggesting that acupuncture could effectively reduce the symptoms and signs of DKD patients. In terms of renal function, compared with the conventional treatment group, the combined acupuncture group significantly reduced 15.36μmol/L SCR, 0.39g uALB, 32.63mg umALB and 0.45μg/ml uβ2-MG. SCR is an essential indicator that reflect the function of the kidney to remove metabolic waste (38). uβ2-MG is often used to evaluate renal tubular function (39). ALB reflects glomerular injury and glomerular permeability to macromolecules (40). mALB is an indicator of renal and systemic endothelial dysfunction (41). This evidence suggests that acupuncture effectively improves renal function in patients with DKD, thereby bettering the prognosis of DKD.
On the glycemic-related endpoints, the combined acupuncture group significantly reduced 0.69% HbA1c, 0.86 mmol/L FBG, and 0.87 mmol/L 2h PPG compared with the conventional treatment group, implying that acupuncture has a glycemic lowering effect. Actually, hyperglycemia, hypertension, obesity, and dyslipidemia are major risk factors for the development and progression of DKD (42). It has been reported that chronic persistent hyperglycemia can cause abnormal glucose and lipid metabolism, hemodynamic changes, and oxidative stress in the body, which can lead to renal dysfunction and DKD (43, 44). Studies have shown that the incidence of diabetic complications is directly related to blood glucose levels (45), and the risk of microvascular complications increases by 40% for every 1% increase in HbA1c levels (46). The rate of renal impairment in patients with DKD is also controlled by blood glucose (47). Nosadini R et al. (48) noted that when HbA1c is consistently greater than 7.5% and postprandial glucose is more significant than 200 mg/dl, the risk of a rapid decline in glomerular function is significantly increased. On lipid-related endpoints, compared with the conventional treatment group, the combined acupuncture group significantly reduced 1.23 mmol/L TC and 0.69 mmol/L TG and significantly increased 0.36 mmol/L HDL-C, suggesting that acupuncture has an additional benefit in lipid modulation. In addition, considering that cardiovascular events are one of the main causes of death in DKD patients, regulating blood lipids can help improve the cardiovascular prognosis of DKD patients (27).
On the safety endpoints, adverse events in the combined acupuncture group were not significantly different from those in the conventional treatment group, suggesting that acupuncture has a good safety profile and does not additionally increase the risk of adverse events.
Although meta-analysis showed that acupuncture was a safe treatment for DKD, it is still essential to be aware of potential adverse events such as hematoma, pain, infection, and needle-sickness that may be associated with acupuncture (49, 50). (1) Hematoma: Hematoma is one of the most prevalent untoward incidents following needle insertion. In this study, both adverse events observed in the acupuncture group were hematoma, typically arising from inadequate post-needle removal compression time. Applying gentle pressure with a cotton swab for approximately 30 seconds upon needle extraction effectively prevents hematoma formation. Hematomas formed by minimal bleeding generally resolve independently without requiring specific interventions. In cases where excessive subcutaneous bleeding induces intense pain, initial hemostasis through cold compression is recommended, followed by warm compression 24 hours later to facilitate hematoma absorption. (2) Pain: As an invasive therapeutic modality, acupuncture may induce localized pain at the needling site. Clinical practitioners should rigorously control needle insertion angles, depths, and stimulation levels in adherence to guidelines to alleviate the patient’s pain burden. Additionally, severe pain is commonly attributable to hematoma formation; hence, averting hematoma development effectively reduces the incidence of pain. (3) Infection: Infections typically arise from inadequate disinfection during operation. Given the slower wound healing in diabetic patients compared to the general population, infections are more prone to occur in patient with DKD. Strict adherence to standardized disinfection protocols significantly mitigates the risk of infection. (4) Needle-sickness: Needle-sickness refers to symptoms such as dizziness, palpitations, nausea, and sweating during the needling process. The precise mechanism of it remains not entirely elucidated, but it is generally associated with factors such as psychological tension, hunger, improper positioning, and excessive stimulation. Pre-needling education and effective doctor-patient communication contribute to reducing occurrences of needle-sickness. In the event of needle-sickness, immediate cessation of the procedure is necessary, allowing the patient to recover gradually.
Currently, studies on the mechanisms of acupuncture in the treatment of DKD have focused on podocytes. Podocytes are terminally differentiated and highly specialized cells whose foot processes can attach to the glomerular basement membrane and connect to each other through the slit diaphragm (SD) (51). Podocyte injury is one of the earliest pathological changes in DKD (52), which mainly manifests as loss of foot processes and destruction of SD (53). Studies have shown that acupuncture can protect podocytes from damage by restoring SD density, up-regulating the expression of SD proteins (nephrin and CD2 associated protein) and the apical membrane protein podocalyxin, and downregulating the cytoskeletal intermediate filament protein desmin (51). Acupuncture can also up-regulate the expression of podocyte mucin, thereby exerting a protective effect on the top surface of podocytes (51). Liu L et al. (54) found that acupuncture can improve the podocyte damage of rats with DKD and alleviate pathological changes such as glomerular basement membrane thickening by up-regulating the expression of podocalyxin, CD2 associated protein, and nephrin and down-regulating the expression of desmin, thereby delaying the progression of DKD.
Oxidative stress and inflammation are also closely related to podocyte damage (55). Wang M et al. (56) proposed that acupuncture can regulate the oxidative stress state of patients with DKD by down-regulating the contents of malondialdehyde, protein carbonyl, and 8-hydroxyguanine in plasma and up-regulating the activity of superoxide dismutase in patients with DKD. Wang KX et al. (22) found that acupuncture can reduce oxidative stress by up-regulating the expression of forkhead box protein O1 and peroxisome proliIerators-activated receptor γ coactivator lalpha, thereby protecting the kidneys. Zhang J et al. (57) reported that acupuncture can reduce renal inflammatory injury by inhibiting Nod-like receptor thermal protein domain associated protein 3/nuclear factor-kappa B pathway. In addition, acupuncture can also alleviate kidney injury in rats with DKD by promoting renal cell autophagy (58).
The frequency analysis yielded 20 common acupoints for acupuncture in DKD. However, limited by the support and confidence level, common acupoints such as KI3, CV4, ST25, LR3, ST40, LI4, EX-B3, BL30, LI11, BL18, BL43, and CV3 were excluded from the association rule analysis. Although it contained commonly used acupoints for the treatment of diabetes and its complications, such as LI4 and LI11, the association rule analysis showed that these acupoints were underutilized or lacked close association with other acupoints in the database constructed by the included studies. The association rule analysis yielded core acupoint combinations were composed of CV12, SP8, SP10, ST36, SP6, BL20, BL23, and SP9, suggesting that these acupoints were the core acupoints for acupuncture in DKD. The needling methods and location plan for core acupoints are shown in Table 5.
Traditional Chinese medical theory posits that the pathogenesis of DKD is intricate, encompassing both spleen-kidney deficiency as well as phlegm and blood stasis obstruction (59). Given the selection of specific acupoints was based on the Chinese medical pathogenesis, the intricate pathogenesis of DKD dictate the requirement for multiple acupoint combinations in its treatment. In this study, factor analysis categorized the core acupoints into two groups. The first group comprised CV12, SP8, and SP10, primarily functioning to tonify the kidneys and dissipate blood stasis. The second group consisted of ST36, SP6, BL20, BL23, and SP9, primarily acting to tonify the spleen and kidney, and dissipate phlegm. These two sets of acupoints complement each other, collectively exerting the therapeutic effects of tonifying the spleen and kidneys as well as dissipating phlegm and blood stasis, aligning with the Chinese medical pathogenesis of DKD. Hence, acupuncturists must comprehend the significance of these core acupoints and their groupings in the treatment of DKD and fully apply them in clinical practice.
Although the study followed the PRISMA guidelines, there are still some limitations. First, only 659 samples were included in the meta-analysis part of the study, and only 51 programs were included in the data mining part, which may lead to a decrease in the accuracy of the results. Second, Wang KX et al. (22) limited the age to 30–70 years and only included patients with Mogensen stage III, while Chu Q et al. (18) subjectively excluded patients with blood glucose >14 mmol/L. The limitations of these inclusion criteria may reduce the generalizability of the meta-analysis results. Third, the research centers of the nine clinical trials were all in China, and the study subjects were mainly of Chinese descent. This means that the results of this study were mainly used to evaluate the effects of acupuncture in Chinese patients with DKD, and it is not yet clear how the therapy works in Europeans, Americans, and Africans. Fourth, the course of treatment included in the study was between four and 12 weeks, so the meta-analysis results mainly reflected the short-term efficacy of acupuncture in treating DKD, and there was a lack of long-term follow-up data.
Given the limitations of existing research, we expect the future studies will continue to improve: (1) The acupuncture strategy obtained in this study can be used in clinical trials to verify its efficacy and safety in treating DKD. (2) By facilitating the development of multicenter stratified studies, further explore the efficacy of acupuncture in treating patients with DKD of varying age, stage, baseline glucose level, and baseline weight. (3) Research centers can be established in European, American, and African countries to further evaluate the specific benefits of acupuncture in different ethnic populations. (4) Researchers can further evaluate the long-term efficacy of acupuncture in treating DKD by extending the follow-up period to half a year to one year.
Acupuncture improved clinical symptoms, renal function indices such as uALB, umALB, uβ2-MG, and SCR, as well as blood glucose and blood lipid in patients with DKD, and has a favorable safety profile. CV12, SP8, SP10, ST36, SP6, BL20, BL23, and SP9 are the core acupoints for acupuncture in DKD, and this program is expected to become a supplementary treatment for DKD.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
YFY: Conceptualization, Supervision, Writing – original draft. GH: Methodology, Supervision, Writing – original draft. XY: Formal analysis, Methodology, Writing – original draft. YMY: Data curation, Formal analysis, Writing – original draft. KT: Data curation, Formal analysis, Writing – original draft. RY: Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the key support project of the Regional Innovation and Development Joint Fund of the National Natural Science Foundation of China [U21A20411].
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ALB, Albumin; CI, Confidence interval; DKD, Diabetic kidney disease; FBG, Fasting blood glucose Glycated; HbA1c, hemoglobin A1c ; HDL-C, High-density lipoprotein cholesterol; MD, Mean difference ; PRISMA, Preferred Reporting Items for Systematic reviews and Meta-Analyses; SCR, Serum creatinine; SD, Slit diaphragm; TC, Total cholesterol; TG, Triglyceride; uALB, Urinary albumin; umALB, Urinary microalbumin; uβ2-MG, Urine β2 microglobulin; 2h PPG, 2h postprandial plasma glucose.
1. Yang M, Chen W, He L, Liu D, Zhao L, Wang X. Intermittent fasting-A healthy dietary pattern for diabetic nephropathy. Nutrients (2022) 14:3995. doi: 10.3390/nu14193995
2. Wang S, Zhang X, Wang Q, Wang R. Histone modification in podocyte injury of diabetic nephropathy. J Mol Med (Berl) (2022) 100:1373–86. doi: 10.1007/s00109-022-02247-7
3. Farber E, Hanut A, Tadmor H, Ruth A, Nakhoul F, Nakhoul N. [Autophagy and diabetic nephropathy]. Harefuah (2021) 160:740–5.
4. Gao Y, Ji Y, Song Y, Gong R, Chen C, Chen H. Clinical efficacy and safety of warm acupuncture in the treatment of type 2 diabetic kidney disease: A protocol of a randomized controlled trial. Med (Baltimore) (2022) 101:e32034. doi: 10.1097/MD.0000000000032034
5. Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract (2011) 94:311–21. doi: 10.1016/j.diabres.2011.10.029
6. Campos CS, Ferreira GF, Bastos KV, da Costa Carbogim F, de Brito Poveda V, de Araújo Püschel VA, et al. Immunosuppressive adherence after kidney transplantation in adult patients treated at an outpatient clinic: a better practice implementation project. JBI Evid Implement (2020) 19:306–14. doi: 10.1097/XEB.0000000000000262
7. Bonner R, Albajrami O, Hudspeth J, Upadhyay A. Diabetic kidney disease. Prim Care (2020) 47:645–59. doi: 10.1016/j.pop.2020.08.004
8. Zhang Y, Zhu BB, Chi YF, Liu S, Wang H, Wang YM. Effect of Huangqi decoction on renal function and glucose and lipid metabolism in patients with diabetes nephropathy stage III of qi yin deficiency. Lishizhen Med Materia Medica Res (2022) 33:2435–7.
9. Wang M, Liu W, Ge J, Liu S. The immunomodulatory mechanisms for acupuncture practice. Front Immunol (2023) 14:1147718. doi: 10.3389/fimmu.2023.1147718
10. Zhu Q, Chen J, Xiong J, Lu L, Zhu S, Zhong Z, et al. The efficacy of moxibustion and acupuncture therapy for ankylosing spondylitis: A protocol for an overview of systematic reviews and meta-analysis. Med (Baltimore) (2021) 100:e25179. doi: 10.1097/MD.0000000000025179
11. Liang F, Koya D. Acupuncture: is it effective for treatment of insulin resistance? Diabetes Obes Metab (2010) 12:555–69. doi: 10.1111/j.1463-1326.2009.01192.x
12. Miao YD, Gu WY, Liu ZQ, Ma YT, Deng S. Effectiveness comparisons of acupuncture for diabetic nephropathy proteinuria: A systematic review and meta-analysis: study protocol. Med (Baltimore) (2019) 98:e17819. doi: 10.1097/MD.0000000000017819
13. Yu Z, Zhang W, Li B, Bao P, Wang F, Sun J, et al. Efficacy and safety of acupuncture combined with Chinese Herbal Medicine for diabetic nephropathy: A protocol for systematic review and meta-analysis. Med (Baltimore) (2021) 100):e27087. doi: 10.1097/MD.0000000000027087
14. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematicreviews. BMJ (2021) 372:n71. doi: 10.1136/bmj.n71
15. Mogensen CE, Christensen CK, Vittinghus E. The stages in diabetic renal disease. With emphasis on the stage of incipient diabetic nephropathy. Diabetes (1983) 32:64–78. doi: 10.2337/diab.32.2.S64
16. State Administration for Market Regulation. GBT 12346-2021, Nomenclature and location of meridian points. Beijing: The State Administration for Market Regulation (2021).
17. Chen GC, Chen WD. 30 cases of diabetes nephropathy treated with western medicine and acupuncture. Guangming J Chin Med (2006) 01:36–8. doi: 10.3969/j.issn.1003-8914.2006.01.029
18. Chu Q. Clinical research on the treatment of diabetic nephropathy with acupuncture. Jinan: Shandong University of Traditional Chinese Medicine (2003).
19. Fan C. Acupuncture treatment of diabetic and kidney disease, Probe into acupuncture points in ancient and its modern clinical research. Guangdong: Guangzhou University of Chinese Medicine (2011).
20. Ji XQ, Yu SH, Xue L, Zhang ZL. Effect of acupuncture combined with low protein diet on diabetic early nephropathies. Chin Acupunct Moxibustion (2004) 09:7–9.
21. Tang M, Xu JS. Effect analysis of warm acupuncture and moxibustion in the treatment of diabetic nephropathy with spleen and kidney yang deficiency. Diabetes New World (2022) 25:165–167 + 175. doi: 10.16658/j.cnki.1672-4062.2022.05.165
22. Wang KX, Liang FX, Chen S, Luo ZH, Chen B, Chen ZQ, et al. Effect of electroacupuncture of “Biao-Ben” acupoints on renal function and hemorheology and eNOS level in patients with early diabetic nephropathy. Acupunct Res (2022) 47:46–52. doi: 10.13702/j.1000-0607.20210036
23. Wu YT. Clinical observation on treating diabetic nephropathy with benazepril plus acupuncture. Chin J Pract Chin Modem Med (2008) 21:1236–7.
24. Yang XY. Clinical analysis of 27 cases of diabetes nephropathy treated by acupuncture with the method of supplementing qi and activating blood circulation. Xinjiang J Tradit Chin Med (2013) 31:45–7.
25. Zhu YP, Chen YP, Zhao YY, Ya HJ, Su SH. Clinical observation on the acupuncture for the treatment of peripheral neuropathy of type 2 diabetic nephropathy. J Guangzhou Univ Tradit Chinese Med (2023) 40:899–904. doi: 10.13359/j.cnki.gzxbtcm.2023.04.018
26. Verma A, Patel AB, Upadhyay A, Waikar SS. CREDENCE: significant victory for diabetic kidney disease. Trends Endocrinol Metab (2020) 31:391–3. doi: 10.1016/j.tem.2020.04.002
27. Fox CS, Matsushita K, Woodward M, Bilo HJ, Chalmers J, Heerspink HJ, et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Lancet (2012) 380:1662–73. doi: 10.1016/S0140-6736(12)61350-6
28. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract (2019) 157:107843. doi: 10.1016/j.diabres.2019.107843
29. Xiang E, Han B, Zhang Q, Rao W, Wang Z, Chang C, et al. Human umbilical cord-derived mesenchymal stem cells prevent the progression of early diabetic nephropathy through inhibiting inflammation and fibrosis. Stem Cell Res Ther (2020) 11:336. doi: 10.1186/s13287-020-01852-y
30. Zhang L, Li K, Liu X, Li D, Luo C, Fu B, et al. Repeated systemic administration of human adipose-derived stem cells attenuates overt diabetic nephropathy in rats. Stem Cells Dev (2013) 22:3074–86. doi: 10.1089/scd.2013.0142
31. Zhao Q, Sun LY, Zhen QY, Zhang XX, Jin HN, Chen ML, et al. Meta-analysis of acupuncture as an adjuvant treatment for diabetic kidney disease. Modern Chin Clin Med (2020) 27:41–8. doi: 10.1097/MD.0000000000023821
32. Li RC, She YC. The effect of acupuncture on animal glucose tolerance and insulin secretion response. Jiangxi J Tradit Chin Med (1983) 5:1–4.
33. Zhu XF. Clinical Observation on 246 Cases of diabetes Treated by acupuncture and moxibustion. Chine Acupunct Moxibustion (1991) 1:5.
34. Liang C, An XC, Geng JD, Li JL, Sun MY, Chen J, et al. Effect of acupuncture on serum HDL-C content in experimental diabetes rabbits. Chin J Gerontol (1991) 4:245–6.
35. Shen JF, Wei J. Observation on Hemorheology of diabetes treated by acupuncture. Chine Acupunct Moxibustion (1986) 1:5–8.
36. Zhang YL, Wang GY. 28 cases of diabetes nephropathy treated by integrated traditional Chinese and Western medicine. J Guizhou Med Univ (2001) 05:436–7.
37. Wang AN, Gao H, Yang YF, Shi Y. A systematic review of acupuncture on diabetic kidney disease. Guiding J Tradit Chin Med Pharmacy (2019) 25:81–6. doi: 10.13862/j.cnki.cn43-1446/r.2019.09.024
38. Tan H, Chen J, Li Y, Li Y, Zhong Y, Li G, et al. Glabridin, a bioactive component of licorice, ameliorates diabetic nephropathy by regulating ferroptosis and the VEGF/Akt/ERK pathways. Mol Med (2022) 28:58. doi: 10.1186/s10020-022-00481-w
39. Ekrikpo UE, Effa EE, Akpan EE, Obot AS, Kadiri S. Clinical utility of urinary β2-microglobulin in detection of early nephropathy in african diabetes mellitus patients. Int J Nephrol (2017) 2017:4093171. doi: 10.1155/2017/4093171
40. Brenner BM, Hostetter TH, Humes HD. Molecular basis of proteinuria of glomerular origin. N Engl J Med (1978) 298:826–33. doi: 10.1056/NEJM197804132981507
41. Swärd P, Rippe B. Acute and sustained actions of hyperglycaemia on endothelial and glomerular barrier permeability. Acta Physiol (Oxf) (2012) 204:294–307. doi: 10.1111/j.1748-1716.2011.02343.x
42. Alicic RZ, Rooney MT, Tuttle KR. Diabetic kidney disease: challenges, progress, and possibilities. Clin J Am Soc Nephrol (2017) 12:2032–45. doi: 10.2215/CJN.11491116
43. Wu D, Yu Z, Zhao S, Qu Z, Sun W, Jiang Y. Lipid metabolism participates in human membranous nephropathy identified by whole-genome gene expression profiling. Clin Sci (Lond) (2019) 133:1255–69. doi: 10.1042/CS20181110
44. Tonneijck L, Muskiet MH, Smits MM, van Bommel EJ, Heerspink HJ, van Raalte DH, et al. Glomerular hyperfiltration in diabetes: mechanisms, clinical significance, and treatment. J Am Soc Nephrol (2017) 28:1023–39. doi: 10.1681/ASN.2016060666
45. Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ (2000) 321:405–12. doi: 10.1136/bmj.321.7258.405
46. Zoungas S, Chalmers J, Ninomiya T, Li Q, Cooper ME, Colagiuri S, et al. Association of HbA1c levels with vascular complications and death in patients with type 2 diabetes: evidence of glycaemic thresholds. Diabetologia (2012) 55:636–43. doi: 10.1007/s00125-011-2404-1
47. Dronavalli S, Duka I, Bakris GL. The pathogenesis of diabetic nephropathy. Nat Clin Pract Endocrinol Metab (2008) 4:444–52. doi: 10.1038/ncpendmet0894
48. Nosadini R, Tonolo G. Relationship between blood glucose control, pathogenesis and progression of diabetic nephropathy. J Am Soc Nephrol (2004) 15 Suppl 1:S1–5. doi: 10.1097/01.ASN.0000093372.84929.BA
49. Li YQ, Liu YY, Zhang J, Guo Y. Analysis on the situation of adverse reaction to acupuncture and acupuncture risk. Chin Acupunct Moxibustion (2011) 31:764–8. doi: 10.13703/j.0255-2930.2011.08.017
50. Wang C, Liu BY, Liu Y, He LY, Li HJ, Liu J. Analysis on the concepts related to adverse events and adverse reactions of acupuncture. Chin Acupunct Moxibustion (2018) 38:87–90. doi: 10.13703/j.0255-2930.2018.01.023
51. Zhang Z, Li X, Liu L, Sun J, Wang X, Zhao Z, et al. Tiaolipiwei acupuncture reduces albuminuria by alleviating podocyte lesions in a rat model of diabetic nephropathy. Evid Based Complement Alternat Med (2018) 2018:1913691. doi: 10.1155/2018/1913691
52. Wiggins RC. The spectrum of podocytopathies: a unifying view of glomerular diseases. Kidney Int (2007) 71:1205–14. doi: 10.1038/sj.ki.5002222
53. Tryggvason K, Wartiovaara J. Molecular basis of glomerular permselectivity. Curr Opin Nephrol Hypertens (2001) 10:543–9. doi: 10.1097/00041552-200107000-00009
54. Liu L, Dong CY, Hao H, Hu JH, Shen SH, Tan YQ, et al. Effect of acupuncture for regulating spleen and stomach on the expression of PCX, CD2AP, nephron and desmin in podocytes of rats with type 2 diabetic nephropathy. J Changchun Univ Chin Med (2023) 39:152–5. doi: 10.13463/j.cnki.cczyy.2023.02.009
55. Liu D, Wu M, Li L, Gao X, Yang B, Mei S, et al. Low-protein diet supplemented with ketoacids delays the progression of diabetic nephropathy by inhibiting oxidative stress in the KKAy mice model. Br J Nutr (2018) 119:22–9. doi: 10.1017/S0007114517003208
56. Wang M, Zhang ZL, Ji XQ, Yang YQ, Yang XJ, Li S. [Randomized controlled clinical trial for analyzing effect of “Spleen-stomach regulation nee- dling” on oxidative stress level in patients with diabetic nephropathy]. Acupunct Res (2015) 40:409–14. doi: 10.13702/j.1000-0607.2015.05.013
57. Zhang J, Yang X, Zhang X, Lu D, Guo R. Electro-acupuncture protects diabetic nephropathy-induced inflammation through suppression of NLRP3 inflammasome in renal macrophage isolation. Endocr Metab Immune Disord Drug Targets (2021) 21:2075–83. doi: 10.2174/1871530321666210118161721
58. Huang H, Chen L, Wu H, Jin JS. Effect of electroacupuncture on renal function and expression of autophagy-related proteins in kidney of rats with diabetic nephropathy. Acupunct Res (2022) 47:108–14. doi: 0.13702/j.1000-0607.20210329
Keywords: diabetic kidney disease, meta-analysis, data mining, acupuncture, acupoint
Citation: Yu Y, Hu G, Yang X, Yin Y, Tong K and Yu R (2024) A strategic study of acupuncture for diabetic kidney disease based on meta-analysis and data mining. Front. Endocrinol. 15:1273265. doi: 10.3389/fendo.2024.1273265
Received: 05 August 2023; Accepted: 22 January 2024;
Published: 26 February 2024.
Edited by:
Jeff M. P. Holly, University of Bristol, United KingdomReviewed by:
Sen Li, Beijing University of Chinese Medicine, ChinaCopyright © 2024 Yu, Hu, Yang, Yin, Tong and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rong Yu, eXVyb25nMTk2OTA1QDE2My5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.